Abstract
Purpose
Radial tunnel syndrome is defined as a compressive neuropathy of the posterior interosseus nerve. It is differentiated from posterior interosseus nerve compression by symptom profile. The purpose of this article is to review past and current literature on the topic and determine if there are any emerging treatment options for this condition.
Recent Findings
Traditionally, conservative management of Radial Tunnel syndrome has been relatively unsuccessful. As a result, patients afflicted by this neuropathy require operative intervention. Effectiveness of surgical decompression is variable and can range from 67 to 92% but currently remains the standard treatment. However, there are some conservative treatment options that have been recently reported that show promising results. Such treatments include dry needling of the affected area and ultrasound guided corticosteroid injections to hydro dissect around the posterior interosseus nerve at sites of compression.
Summary
Radial tunnel syndrome is an uncommon and unique peripheral neuropathy. It involves the posterior interosseus nerve however it can be differentiated from PIN syndrome based on the symptom profile. There are various compressive etiologies that can cause a patient to become symptomatic; therefore it is important to critically assess the patient and their symptoms and use appropriate imaging to determine the cause and appropriate treatment. Typically, conservative treatments are attempted first. Traditionally, conservative therapy is unsuccessful and operative decompression is necessary. However, current literature highlights various new nonsurgical options that suggest some promise and could be alternatives to surgical decompression.
Keywords: PIN neuropathy, Radial tunnel syndrome, Posterior interosseous nerve, Proximal forearm pain, Compression
Introduction
Radial tunnel syndrome (RTS) is defined as a compressive neuropathy of the posterior interosseus nerve. It is differentiated from posterior interosseus nerve compression by symptom profile. RTS presents primarily as pain within the mobile wad, approximately 3–5 cm distal to the lateral epicondyle; whereas posterior interosseous nerve (PIN) syndrome is typically painless and is accompanied by motor deficits and weakness. There have been various compressive etiologies described, including fascial bands, radial recurrent vessels, the proximal edge of the supinator, and various space occupying lesions (ganglions, hemangioma, lipoma, synovium, or accessory muscle); however, the most common site of compression is the arcade of Frohse [1]. The incidence of this peripheral compressive neuropathy is much less common than conditions such as carpal or cubital tunnel syndrome. The overall annual incidence of RTS is approximately 0.03% [2] as compared with carpal tunnel which ranges between 0.1 and 0.35% [3]. Patients typically present with RTS around 30–50 years of age and it is often seen in females.
Anatomy
RTS is a compressive neuropathy of the posterior interosseus nerve which is a branch of the radial nerve. The radial nerve is a terminal nerve from the posterior cord of the brachial plexus with contributions from the C5 to C8 nerve roots. The radial nerve and axillary nerve make their division from the posterior cord anterior to the subscapularis muscle. The radial nerve then travels into the arm anterior to the latissimus insertion and then runs along the triceps and travels along the posterior aspect of the humerus along the spiral groove. It is at this landmark that the nerve crosses midline at approximately 15 cm from the distal joint line and travels through the lateral intermuscular septum on average 12.2 cm from the lateral epicondyle. Proximal to the elbow the radial nerve innervates the long, lateral, and medial heads of the triceps and a portion of the brachioradialis muscle (due to its dual innervation). Approximately 3 cm distal to the lateral epicondyle and deep to the brachioradialis the radial nerve splits into 2 branches, the posterior interosseus nerve and the superficial radial nerve [4]. This division occurs ~3 cm proximal to the superior border of the supinator, also known as the arcade for Frohse. The PIN first passes between the two heads of the origin of the supinator muscle (Fig. 1) and then directly contacts the radial neck and passes over the abductor pollicis longus muscle origin towards the interosseous membrane.
Fig. 1.
View of the lateral elbow interval between ECRB (extensor carpi radialis brevis) and EDC (extensor digitorum communis) with underlying supinator. Dotted line indicates the path of the PIN beneath the supinator. Arrowhead indicates the origin of PIN. (Adapted from Knutsen, E. J., & Calfee, R. P. (2013). Uncommon Upper Extremity Compression Neuropathies. Hand Clinics, 29(3), 443–453. 10.1016/j.hcl.2013.04.014)
The radial tunnel is the anatomic boundary of the radial nerve around the elbow joint. It is approximately 5 cm in length and spans from the radiocapitellar joint proximally and to the proximal edge of the supinator distally. The boundaries of the tunnel on the lateral border are the brachioradialis, ECRL, and ECRB. The boundaries on the medial border are the biceps tendon and the brachialis. The floor of the tunnel is the capsule of the radiocapitellar joint [5] (Fig. 2).
Fig. 2.
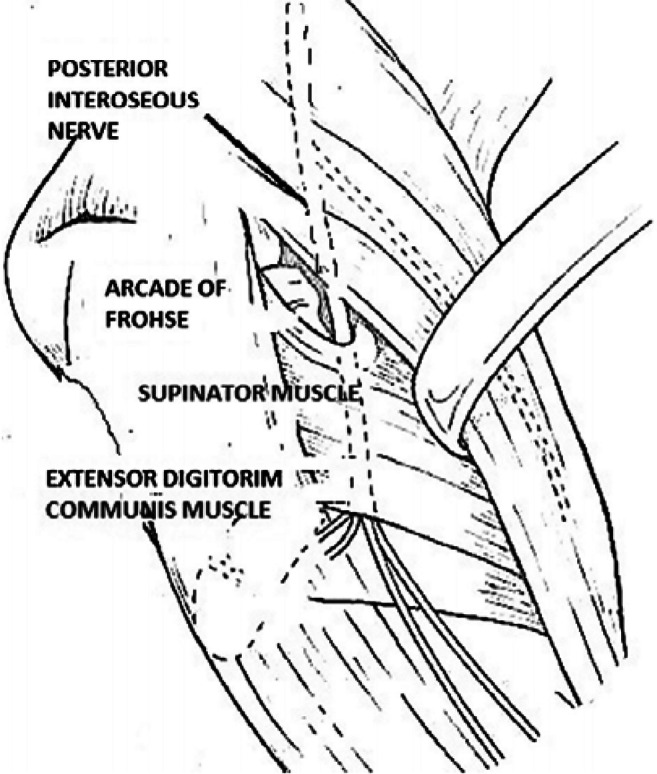
Image demonstrating the path of the posterior interosseous nerve through the radial tunnel (Adapted from Simon Perez, C., García Medrano, B., Rodriguez Mateos, J. I., Coco Martin, B., Faour Martin, O., & Martin Ferrero, M. A. (2014). Radial tunnel syndrome: results of surgical decompression by a postero-lateral approach. International Orthopaedics, 38(10), 2129–2135. 10.1007/s00264-014-2441-8)
Once the nerve exits the radial tunnel, it then continues its course traversing along the posterior interosseous membrane. The terminal branch is located on the floor of the fourth extensor compartment. It provides motor innervation of the extensor compartment including the common extensors (ECRB, EDC, EDM, ECU), the deep extensors (supinator, APL, EPB, EPL, EIP), and finally sensory nerve fibers to the dorsal wrist capsule.
RTS compression can result from one or more of various structures along the PIN nerve path through the radial tunnel. These points of compression include: the superficial supinator muscle (also known as the arcade of Frohse), the tendinous edge of ECRB, vessels from the radial recurrent artery (also known as the leash of Henry), or fibrous bands distal to the radial head [6]. Of these structures, the tendinous edge of the superficial supinator muscles is considered to be the most common site of compression, as seen in a cadaveric study by Konjengbam and Elangbam [7].
Presentation
A detailed history and physical examination are necessary to obtain an accurate diagnosis and an appropriate treatment. It is critical to differentiate RTS from PIN injury, PIN compression, lateral epicondylitis, or other proximal neuropathies.
Symptoms
RTS typically presents with deep aching pain in the dorsoradial proximal forearm. This can span from the lateral elbow to the wrist and increases with forearm rotation and lifting activities. Patients can also present with muscle weakness; however, this is due to pain rather than muscle denervation [8].
Physical Exam
RTS is a condition that is based on clinical findings; therefore the physical exam is of utmost importance. Physical examination involves evaluation of the entire upper extremity. Palpation over the mobile wad about the supinator arch, approximately 3–5 cm distal to the lateral epicondyle, elicits maximal tenderness. The Rule-of-Nine test was proposed in a cadaveric study to help better localize to site of tenderness in RTS. The study demonstrated that by diagraming a 3 × 3 quadrant distal to the elbow crease, the width of the crease used for the length of all sides of the square, and dividing the square 3 × 3, this can be used to localize the a patient’s tenderness and differentiate RTS from other entities. In the cadaveric study, it was determined that the proximal 2 squares of the lateral column most consistently coincided with the location of the PIN nerve compression at the radial tunnel [9] (Fig. 3).
Fig. 3.

Rule of nine test-nine pressure points are marked on the proximal volar aspect of the forearm in 3 columns. Tenderness to palpation over the two proximal lateral points (red) indicates radial nerve irritation. Tenderness over the middle distal points (yellow) indicates proximal median nerve irritation. The remaining points (blue) serve as controls. (Adapted from Moradi A, Ebrahimzadeh MH, Jupiter JB. Radial tunnel syndrome, diagnostic and treatment dilemma. Arch Bone Jt Surg. 2015:3:3:156-162. 10.1155/2012/230679.)
Maneuvers that place the nerve under tension can elicit pain. These maneuvers include elbow extension, passive forearm pronation, and wrist flexion. Other provocative physical exams can also help elicit radial tunnel pain. These physical exams include resisted supination, resisted extension of the wrist, and resisted extension of the long finger [10, 11]. These physical exam tests with will often reproduce pain at the radial tunnel and possible weakness secondary to pain. Evidence shows that passive stretch of the supinator increases pressure inside of the radial tunnel to 250 mmHg, while pressure at baseline is 50 mmHg.
A diagnostic injection with local anesthetic into the radial tunnel will lead to a PIN palsy but also relieve pain [12]. With regard to sensory and motor deficits, patients may present with paresthesia of the first dorsal web space however there are no motor manifestations.
Diagnosis
Imaging
Prior to advanced imaging, it is important to obtain standard radiographs of the elbow and forearm to ensure there are no osseous injuries or abnormalities that could be the cause of a compressive neuropathy.
If radiographs are negative, the next step is MRI imaging. While MRI results are typically negative, it is important to rule out other potential diagnoses. When patients with RTS do have positive MRI findings, the most common finding is usually denervation edema of the musculature innervated by the PIN. This was most commonly seen in the supinator (44%) and less commonly with in the proximal forearm extensors (12%) [13]. MRI could also demonstrate areas of compression, such as a thickened ECRB edge, prominent radial recurrent vessels, also known as the leash of Henry, or swelling of the PIN. Finally, MRI can identify other causes of compression such as space occupying lesions including, tumors, ganglia, radiocapitellar synovitis, bicipital bursitis, and as previously mentioned osseous injuries like radial head fractures and dislocations.
Nerve Conduction Studies
Electrodiagnostic studies (EMG/NCV) are generally inconclusive and nondiagnostic studies for RTS. This is due to the composition of the PIN. It carries unmyelinated fibers (C-fibers) that sense nociception and small myelinated Group IIA afferent fibers that sense temperature. Compression of these fibers produces pain but does not affect motor function and they cannot be evaluated by EMG and NCV. The large myelinated fibers of PIN remain unaffected and thus result in normal EMG/NCV.
While seeking diagnosis, it is also always important to consider the differential diagnosis. There are various other pathologies that can present at a similar location and with similar symptoms, and these include lateral epicondylitis and cervical radiculopathy of C6-7. Lateral epicondylitis will have tenderness directly over the lateral epicondyle while in RTS tenderness is distal to the lateral epicondyle. Furthermore, many patients present with concomitant RTS and lateral epicondylitis, further complicating diagnosis and treatment. With cervical radiculopathy, there will be positive findings in electrodiagnostic studies that demonstrate denervation. Distal biceps insertional tendonitis has also been shown to mimic RTS [14]. A cases series of 13 patients showed that distal biceps insertional tendonitis can present with similar tenderness and provocative symptoms, yet biceps pathology was revealed on MRI. In this study, at final follow-up, all patients had resolutions of their symptoms with conservative management.
These various alternative diagnoses can explain why some patients with suspected RTS may improve with nonoperative treatment and why surgical release can provide unsatisfactory results.
Treatment
Non-operative Intervention
First-line treatment of radial tunnel treatment is non-operative and should be trialed for an extended period of time, often a year. This includes activity modifications, temporary splinting, and non-steroidal anti-inflammatory medications. Activity modifications and positional adjustment may prevent prolonged elbow extension with forearm pronation and wrist extension. Corticosteroid injections may also be trialed and provide a diagnostic and therapeutic effect. Marchese et al. conducted a prospective evaluation of a single corticosteroid injection in patients with RTS. In this study there were 35 patients that matched criteria and were available for analysis. The injection was 0.25 mL of 1% lidocaine and 0.75 mL of Celestone 6 mg/mL, and it was injected at the point of maximal tenderness over the mobile wad. Overall, at the 1-year mark, there was a significant decrease in VAS scores and qDASH scores. With regard to MCID in qDASH, 57% of patients had discernable affect at 1 year. Studies have shown that 70% of patients show improvement at 6 weeks and 60% are pain free at 2 years [15]. This study indicates that a single corticosteroid injection is an effective option that can be trialed prior to operative intervention.
While it is recommended to trial nonoperative intervention prior to proceeding to a release, several studies have shown that conservative treatment tends to not be significantly effective.
Operative Intervention
Operative intervention can be discussed after a trial of nonoperative interventions for at least 1 year. Operative intervention entails radial tunnel release. This release can be managed via a dorsal or anterior approach to the PIN.
The dorsal approach to the PIN has been described through 3 different planes. These 3 planes include the plane between ECRB and EDC, between brachioradialis and ECRL, or via a transmuscular brachioradialis splitting approach. The anterior approach to the PIN utilizes the plane between brachioradialis and the biceps. During this approach, the arm is held in supination and curved incision is made from the lateral epicondyle and directed distally between the biceps and brachioradialis. Once the radial nerve is identified, it is followed to its bifurcation of PIN and superficial radial nerve. Near the bifurcation, the arcade of Frohse is released, potential compressive recurrent radial vessels are ligated, and the supinator muscle is released [16]. Regardless of the approach used, the three different areas of constriction most frequently released are the arcade of Frohse, the distal edge of the supinator, and the recurrent radial artery if necessary. In a prospective study by Perez et al., a posterolateral approach was utilized to achieve PIN release. In this study, using the Roles and Maudsley criteria, 85% of patients achieved good or excellent results after release with a mean follow-up of 22 months [17].
Overall effectiveness of surgical decompression is variable and can range from 67 to 92%, with patient satisfaction rates ranging from 40 to 83% [18•]. Other factors that can lower success rates include concomitant multiple entrapment neuropathies, concomitant lateral epicondylitis and workers’ compensation patients.
Current Literature
In a case report for treating RTS with dry needling, a 45-year-old male patient presented with a 6-month history RTS that was refractory to all other conservative treatments, including therapy, anti-inflammatories, corticosteroid injections, bracing, and several others. The patient underwent 4 sessions of dry needling over 2 weeks through a grade 6 dry needling procedure over the supinator. Grade 6 dry needling indicates deep insertion with needle rotation (unidirectional or bidirectional) and engaging tissue bind, there is no “pistoning,” “in and out,” or “sparrow pecking” performed. A 0.20-mm solid needle, 30 mm in length, was inserted perpendicular into the skin at the supinator where the maximal point was tenderness was localized. After 4 treatments and after 6 months of follow-up, the patient was reported to be pain free and fully functional [19•].
Another case series describes an RTS injection composed of saline, local anesthetic, and corticosteroid guided by ultrasound to achieve improved results when compared to non-ultrasound guided injections. This case series describes hydraulic dissection of the PIN as they use a higher volume of infiltration and ultrasound-guided injection. The volume used in this case series was 1 mL of corticosteroid solution, 2 mL of 2% lidocaine, and 1–2 mL of saline solution. This was injected into the anatomic plane between PIN and the arcade of Frohse under US with the intent to decompress the PIN. Of the 54 patients that underwent injection 100% reported pain prior to injection and only 1.9% reported pain afterwards. While this study shows significant decrease in pain directly after injection there is no long term follow up. However, this study does bring into focus that US-guided injections with a corticosteroid could yield improved results compared to injections of corticosteroid without ultrasound guidance CSI due to a more exact infiltration location [20•].
Author’s Experience/Clinical Examples
It has been our experience that the most critical component of treating patients with radial tunnel syndrome is to make the correct diagnosis. One must rule out any other potential diagnoses and also identify concurrent diagnoses. Once one is certain that a patient has RTS, appropriate treatment can be initiated. Treatment can be successful in the properly indicated patient. The following clinical example (Courtesy of Louis Catalano, MD) demonstrates a patient with radial tunnel syndrome. MRI images in this case demonstrate lateral epicondylitis with additional findings suggestive of radial tunnel syndrome (Figs. 4, 5, and 6).
Fig. 4.
Coronal T2 weighted MRI cuts of the left elbow demonstrating edema secondary to a partial tear of the common extensor tendon origin at the lateral epicondyle (Image Courtesy of Louis Catalano, MD)
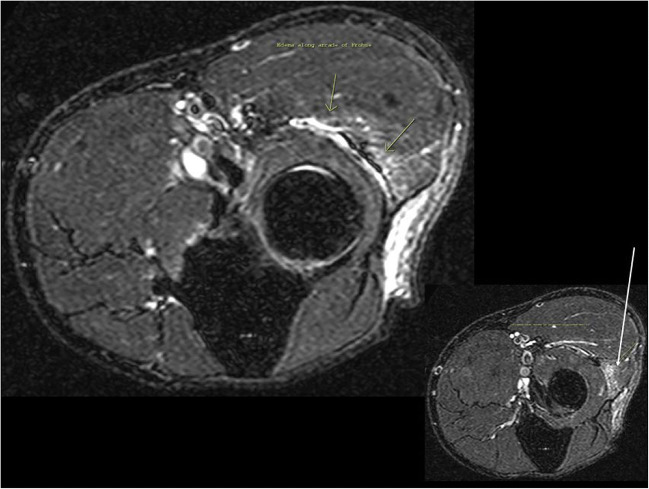
Fig. 5.
Axial T2 weight MRI cut of the distal humerus demonstrating edema adjacent to the lateral epicondyle demonstrating lateral epicondylitis (Image Courtesy of Louis Catalano, MD)
Fig. 6.
Axial T2-weighted MRI cuts of the proximal radius and ulna demonstrating edema from the common extensor tendon tear at the lateral epicondyle tracking along the PIN within the arcade of Frohse (yellow arrow). The white arrow demonstrates intramuscular edema within the extensor digitorum communis (EDC) that may reflect acute denervation; however there is no obvious atrophy of the musculature (Image Courtesy of Louis Catalano, MD)
Intraoperative photos demonstrate the dorsal approach through the interval between the brachioradialis and the ECRL (Figs. 7, 8, 9, and 10).
Fig. 7.
Anterolateral incision over the proximal forearm. Skin incision completed demonstrating structures beneath the skin. Anteriorly is the thin facia (appearing more red) overlying the brachioradialis (BR) and laterally/posteriorly is the thicker fascia overlying the extensor carpi radialis longus (ECRL) (Image Courtesy of Louis Catalano, MD)
Fig. 8.
The inset image in the left upper hand corner demonstrates the brachioradialis (BR) and extensor carpi radialis longus (ECRL) muscle bellies once the facia has been incised. The main image demonstrates the fascial plane between BR and ECRL) (Image Courtesy of Louis Catalano, MD)
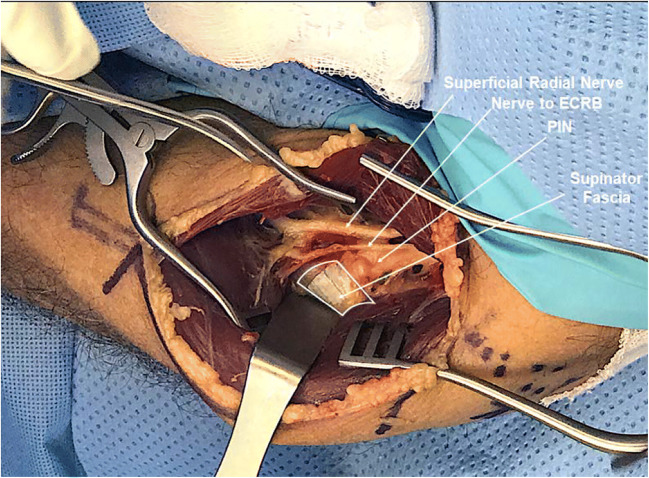
Fig. 9.
This image demonstrates the neural structures between the brachioradialis anteriorly and ECRL posterolaterally. The wide white band deep to the ECRL is the supinator fascia and posterior interosseus nerve (PIN) can be seen diving deep to the supinator fascia. Just anterior to the PIN a branch can be seen which is the nerve to extensor carpi radialis brevis (ECRB). Anterior to this, deep to the brachioradialis is the superficial radial nerve that has branched with the PIN from the radial nerve proximal to this exposure. ) (Image Courtesy of Louis Catalano, MD)
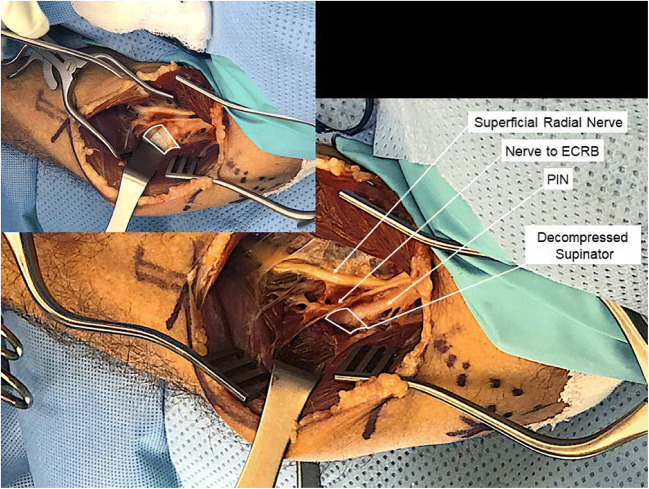
Fig. 10.
The inset in the left upper hand corner demonstrates the same image as that shown in Fig. 9 to reiterate the location of the supinator fascia. The main image shows the supinator fascial incised (white box demonstrates where the fascia was located prior to decompression). The decompressed PIN can now be seen diving deep into the supinator muscle belly. The superficial radial nerve can be seen coursing from proximal to distal along the lateral border of the brachioradialis. Between the PIN and superficial radial nerve, the terminal branch nerve to ECRB can be seen inserting into the muscle belly (Image Courtesy of Louis Catalano, MD)
Conclusion
RTS is an uncommon and unique peripheral neuropathy. It involves the posterior interosseus nerve; however, it should be differentiated from PIN syndrome. Patients with RTS exhibit forearm pain approximately 3–5 cm distal from the lateral epicondyle without any motor manifestations. Any motor weakness is typically related to pain and not true motor findings. PIN syndrome is another compressive peripheral neuropathy of the PIN, but it is characterized by painless motor weakness of the PIN distribution. RTS is a difficult diagnostic entity since it frequently coincides with other compressive conditions, as shown in a study by Sotereanos at el. Their study showed that 20% of their patients had an additional compressive condition and 43% of their patients had associated lateral epicondylitis [21]. Furthermore, RTS is a clinical diagnosis and often a diagnosis of exclusion. Imaging is helpful to rule out other conditions and MRI findings are typically negative. Also, electrodiagnostic studies typically demonstrate negative findings as these studies do not detect the compression of unmyelinated and small myelinated fibers seen in RTS. Once a diagnosis of RTS is suspected, it is important to initiate a trial of conservative treatment that includes rest, activity modification, NSAIDs, and corticosteroid injections. Frequently nonoperative measures are unsuccessful in achieving resolution of RTS and then and only then should operative treatment be considered. Surgical decompression can be accomplished through a variety of different approaches but is important to realize that the surgical treatment of RTS can be variable in its success rate.
Declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no conflict of interest.
Footnotes
This article is part of the Topical Collection on Compressive Neuropathies in the Upper Extremity
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Clavert P, Lutz JC, Adam P, Wolfram-Gabel R, Liverneaux P, Kahn JL. Frohse’s arcade is not the exclusive compression site of the radial nerve in its tunnel. Orthop Traumatol Surg Res. 2009;95(2):114–118. doi: 10.1016/j.otsr.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Dang AC, Rodner CM. Unusual Compression Neuropathies of the Forearm, Part I: Radial Nerve. J Hand Surg Am. 2009;34(10):1906–1914. doi: 10.1016/j.jhsa.2009.10.016. [DOI] [PubMed] [Google Scholar]
- 3.van den Ende KI, Steinmann SP. Radial Tunnel Syndrome. J Hand Surg Am. 2010;35(6):1004–1006. doi: 10.1016/j.jhsa.2010.03.020. [DOI] [PubMed] [Google Scholar]
- 4.Mazurek MT, Shin AY. Upper extremity peripheral nerve anatomy: Current Concepts and Applications. Clinical orthopaedics and related research. 2001;383:7–20. doi: 10.1097/00003086-200102000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Portilla Molina AE, Bour C, Oberlin C, Nzeusseu A, Vanwijck R. The posterior interosseous nerve and the radial tunnel syndrome: an anatomical study. Int Orthop. 1998;22(2):102–106. doi: 10.1007/s002640050218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lister GD, Belsole RB, Kleinert HE. The radial tunnel syndrome. J Hand Surg Am. 1979;4(1):52–59. doi: 10.1016/s0363-5023(79)80105-7. [DOI] [PubMed] [Google Scholar]
- 7.Konjengbam M, Elangbam J. Radial nerve in the radial tunnel: anatomic sites of entrapment neuropathy. Clin Anat. 2003;17(1):21–25. doi: 10.1002/ca.10194. [DOI] [PubMed] [Google Scholar]
- 8.Huisstede BMA, Miedema HS, Opstal T, et al. Interventions for treating the posterior interosseous nerve syndrome: a systematic review of observational studies. J Peripheral Nervous System. 2006;11:101–110. doi: 10.1111/j.1085-9489.2006.00074.x. [DOI] [PubMed] [Google Scholar]
- 9.Loh YC, Lam WL, Stanley JK, Soames RW. A new clinical test for radial tunnel syndrome-the Rule- of-Nine test: a cadaveric study. J Orthop Surg (Hong Kong). 2004;12:83–86. doi: 10.1177/230949900401200115. [DOI] [PubMed] [Google Scholar]
- 10.Bolster MA, Bakker XR. Radial tunnel syndrome: emphasis on the superficial branch of the radial nerve. J Hand Surg Eur. 2009;34(3):343–347. doi: 10.1177/1753193408099832. [DOI] [PubMed] [Google Scholar]
- 11.Hagert CG, Lundborg G, Hansen T. Entrapment of the posterior interosseous nerve. Scand J Plast Reconstr Surg. 1977;11(3):205–212. doi: 10.3109/02844317709025519. [DOI] [PubMed] [Google Scholar]
- 12.Sarhadi NS, Korday SN, Bainbridge LC. Radial tunnel syndrome: diagnosis and management. Journal of Hand Surgery. 1998;23(5):617–619. doi: 10.1016/s0266-7681(98)80015-6. [DOI] [PubMed] [Google Scholar]
- 13.Ferdinand BD, Rosenberg ZS, Schweitzer ME, Stuchin SA, Jazrawi LM, Lenzo SR, Meislin RJ, Kiprovski K. MR Imaging features of radial tunnel syndrome: initial experience. Radiology. 2006;240(1):161–168. doi: 10.1148/radiol.2401050028. [DOI] [PubMed] [Google Scholar]
- 14.Wilson JM, Runner R, McClelland WB, McGillivary G. Misdiagnosis and radial tunnel syndrome: considering the distal biceps tendon. J Surg Orthop Adv. 2019;28(1):35–40. doi: 10.3113/JSOA.2019.0035. [DOI] [PubMed] [Google Scholar]
- 15.Marchese J, Coyle K, Cote M, Wolf JM. Prospective evaluation of a single corticosteroid injection in radial tunnel syndrome. HAND, 155894471878728. 10.1177/1558944718787282 [DOI] [PMC free article] [PubMed]
- 16.Moradi A, Ebrahimzadeh MH, Jupiter JB. Radial tunnel syndrome, diagnostic and treatment dilemma. Arch Bone Jt Surg. 2015;3(3):156–162. doi: 10.1155/2012/230679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Perez CS, Medrano BG, Mateos JIR, Martin BC, Martin OF, Ferrero MAM. Radial tunnel syndrome: results of surgical decompression by a posterolateral approach. International Orthopedics. 2014;38(10):2129–2135. doi: 10.1007/s00264-014-2441-8. [DOI] [PubMed] [Google Scholar]
- 18.• Marchese J, Coyle K, Cote M, Wolf JM. Prospective Evaluation of a Single Corticosteroid Injection in Radial Tunnel Syndrome. HAND. 2018;155894471878728. 10.1177/1558944718787282. This is a notable reference, as it describes a viable alternative treatment to surgical intervention for radial tunnel syndrome. This is a prospective study of improved quality that shows a clinical important difference in qDASH scores after an injection after a year of follow up. This study demonstrates that a single corticosteroid injection is a viable option to attempt prior to choosing operative intervention.
- 19.Anandkumar S. Effect of dry needling on radial tunnel syndrome: A case report. Physiotherapy Theory and Practice. 2019;35(4):1–10. doi: 10.1080/09593985.2018.1443357. [DOI] [PubMed] [Google Scholar]
- 20.Garcia N, Rosales J, Greene C, Droppelmann G, Verdugo MA. Ultrasound guided hydraulic release associated with corticosteroids in radial tunnel syndrome: description of technique and preliminary clinical results. J Ultrasound Med. 2019;00:1–4. doi: 10.1002/jum.15085. [DOI] [PubMed] [Google Scholar]
- 21.Sotereanos DG, Varitimidis SE, Giannakopoulos PN, Westkaemper JG. Results of surgical treatment for radial tunnel syndrome. The Journal of Hand Surgery. 24(3):566–70. 10.1053/jhsu.1999.0566. [DOI] [PubMed]