Abstract
Aim:
To assess (1) how far smoking patterns, depression and smoking-related beliefs and intentions predict vaping uptake, current vaping and vaping frequency among daily smokers; and (2) how far the aforementioned predictors and baseline vaping frequency predict current vaping among those who reported ever vaped.
Design:
Analysis of data from six waves of a longitudinal survey over 8 years. Longitudinal associations between predictors and outcomes were examined using multilevel models.
Setting:
UK, US, Canada and Australia.
Participants:
6296 daily smokers (53% females) who contributed data to at least two consecutive survey waves.
Measurements:
The outcome variables were vaping uptake, vaping frequency, and current vaping at follow-up. The key predictor variables, measured in previous waves, were time to first cigarette, cigarettes smoked per day, depressive symptoms, intention to quit smoking, quitting self-efficacy and worry about adverse health effects of smoking.
Findings:
Number of cigarettes smoked daily was associated with (1) subsequent vaping uptake (OR=1.69, 95%CI [1.19, 2.39] for 30+ cigarette per day; Reference category: 0–10 cigarettes) and (2) a higher frequency of current vaping (OR=1.97, 95% CI [1.36, 2.85] for 30+ cigarettes). Intention to quit was associated with a higher frequency of current vaping (OR = 1.48, 95% CI [1.21, 1.82]). Among those who reported ever vaped, higher baseline vaping frequency (OR=11.98, 95% CI [6.00, 23.93] for daily vaping at baseline; reference category: Vaped less than monthly) predicted current vaping.
Conclusion:
Among daily smokers, amount smoked and intention to quit smoking appear to predict subsequent vaping uptake. Vaping frequency at baseline appears to predict current vaping at follow up.
Introduction
In the last decades, the tobacco epidemic has evolved in many high-income countries. Smoking has steadily decreased over the last 50 years (1, 2), while the use of vaping devices, also known as e-cigarettes, has recently emerged. Survey data from 28 European countries show a clear upward trend in vaping, with more than 1 in 10 adults in 2014 reporting having ever vaped (3). Most people who vape are ex-smokers who have recently quit or current smokers. In the UK, where nicotine vaping products (NVPs) are regulated as a consumer product and easily accessible, current vaping amongst current and recent ex-smokers increased from 2% in 2011 to 20% in 2017, with 11% reporting daily vaping. However, the prevalence of vaping in the general population is low, at 5.5% in the UK, a rate that has stabilized in the last 2–3 years (4).
Reasons for vaping are likely to influence how NVPs are used. For example, some smokers may use these products as a short to medium term cessation aid, much like NRT, in which they are an intermediate step between smoking and becoming nicotine-free. A number of studies have reported that the most common reason reported for vaping is to quit smoking (5–7), and a recent report estimated that over six million European Union citizens had quit or reduced smoking with the help of NVPs (3, 8). Evidence from randomized controlled trials also supports the effectiveness of NVPs as cessation aids (9). Unlike pharmaceutical nicotine replacement therapy (NRT), NVPs are not marketed as medicines, but as less harmful substitutes for tobacco cigarettes. Thus, unlike NRT, NVPs are not marketed with any recommended ‘treatment’ schedule. Some smokers may use NVPs as a complete long-term substitute for cigarettes, while others may only experiment with them out of curiosity or vape when smoking is not allowed while continuing to smoke where there are no smoking restrictions. Research suggests that the pattern of vaping is differentially associated with quitting smoking, with quit success associated with frequent use but not with intermittent use (10).
Existing cross-sectional research examining sociodemographic and smoking related factors associated with vaping uptake has found that those who have tried NVPs are more likely to be current smokers (11), younger (12), motivated to quit smoking (13), and to believe that vaping is less harmful than smoking cigarettes (7). In the US, those who smoke a greater number of cigarettes per day are more likely to have vaped (14). A cross-country analysis showed that interest in quitting predicted trial and current use of NVPs in the UK, but only predicted trial in Australia (12). This research, however, did not explore predictors of vaping frequency (i.e., daily versus non-daily) and continuation of vaping over time.
This study expands on existing research by using longitudinal data from daily smokers collected in the US, UK, Canada and Australia as part of the International Tobacco Control (ITC) Project to examine smoking-related predictors of vaping uptake and vaping frequency. These potential predictors include: intention to quit smoking, intensity of smoking, quitting self-efficacy, outcome expectancy of quitting, and concerns about the health impacts of smoking. In addition, most previous studies of NVPs focused on use/non-use, or frequency of use measured at one point in time. These studies provide limited information about the ongoing vaping, given they are a novel product and some people might use them only briefly out of curiosity. Therefore, we also explored predictors of ongoing use among daily smokers who reported ever vaped.
Method
Participants
Data for the current study were from the ITC Four Country Survey, a longitudinal cohort of nationally representative samples of adult smokers in the United States, the United Kingdom, Canada and Australia. This study used data from six waves of data collection, spanning 2008 to 2016 across the four countries. The first five waves (2008–2014) were collected using a mixture of telephone interviews and web survey, but the sixth wave in 2016 (used only for outcomes here) was exclusively a web-based survey known as the ITC Four Country Smoking and Vaping Survey comprise of England, Canada, the US and Australia. Attrition between waves was approximately 30% for the first five waves, and was much higher (around 60%) for the sixth wave as those only responding by phone were largely dropped. The attrition rate of the sixth wave for the UK sample (~80%) was higher than the other three countries because for the first five waves, data were collected from Scotland, Wales, Northern Ireland and England, but only participants from England was followed up in the sixth wave. We have conducted extensive sensitivity analyses to evaluate the impact of high attrition rate of the sixth wave on the overall conclusion (See Analysis and Result section below). In each follow-up wave, new participants were also recruited using the same sampling procedure for initial recruitment to replenish those who dropped out of the study. Details about the initial samples and dropout rate from each country in each wave are presented in Supplementary Table 1. Details of the ITC conceptual model and methodologies for the first five waves are described in detail elsewhere (15, 16). Details of the methodologies of the sixth wave are described in Thompson et al. (17). The analysis sample consisted of 6296 daily smokers who contributed data to at least two consecutive waves.
Measures
Outcome variables
Vaping uptake by follow-up waves was assessed by the question: “Have you ever tried an electronic cigarette? Yes/No” with “Yes” coded as 1 and “No” as 0.
Current vaping frequency use at follow-up waves was measured using the item “How often, if at all, do you currently use an electronic cigarette?” The response scale was “Daily/ Less than daily but at least once a week/ Less than weekly, but at least once a month/ Less than monthly/ Not at all”.
Ongoing use was derived as follows, and only for the last two waves: Among daily smokers who reported ever having vaped (measured with the question, “Have you ever used electronic cigarettes, or e-cigarettes, even one time?”) at the fifth wave and reported any current use at the sixth wave were coded as 1 and those who reported lifetime vaping at the fifth wave but not vaping at the sixth were coded as 0.
Smoking-related predictor variables
Smoking status was based on self-report and was classified into “Daily smoker”, “Non-daily smoker” and “Quitter”.
Intention to quit smoking was measured using the item “Are you planning to quit smoking…” with the response options “Within the next month”, “Within the next 6 months”, “Sometime in the future, beyond 6 months” and “Not planning to quit”. The first three categories were recoded into “Yes – intending to quit” and the last one was recoded into “No – not intending to quit”.
Time to first cigarette was measured using the item “How soon after waking do you usually have your first smoke?” Participants’ responses were recoded into four levels “More than 60 mins/ 31–60 mins/ 6–30 mins/ 5 mins or less”.
Cigarettes per day were derived from participants’ self-reported average number of cigarettes they smoked per day and this variable was recoded into “0–10/ 11–20/ 21–30/ and more than 31”.
Quitting self-efficacy was measured using the item “If you decided to give up smoking completely in the next 6 months, how sure are you that you would succeed?” and the 5-point response scale was “Not at all sure/ Slightly sure/ Moderately sure/ Very sure/ Extremely sure”.
Expectation about life enjoyment after quitting was measured using the item “If you were to quit smoking, would your ability to enjoy life be improved, made worse, or stay the same?” with the 5-point response scale “Improved a lot/ improved a little/ stay the same/ made a little worse/ made a lot worse”.
Worry about future adverse health effects was measured using the item “How worried are you, if at all, that smoking will damage your health in future?” with the 4-point scale “Not at all worried/ A little worried/ Moderately worried/ Very worried”.
Depression symptoms were measured using the two items from the Primary Care Evaluation of Mental Disorders Procedure questionnaire (18) assessing core symptoms of a depressive episode (DSM-IV): “During the last 30 days, have you often been bothered by little interest or pleasure in doing things?” and “During the last 30 days, have you often been bothered by feeling down, depressed or hopeless?”. The responses to these two items were “Yes/ No”.
Overall opinion about smoking was measured using the item “What is your overall opinion of smoking? Is it…?” with the 5-point response scale “Very positive/ Positive/ Neither positive nor negative/ Negative/ Very negative”.
Current health was measured using a 5-point scale item “In general, how would you describe your health? Is it…” with response options “Poor/ Fair/ Good/ Very good/ Excellent”.
Past adverse health effects of smoking was measured using the item “To what extent, if at all, has smoking damaged your health?” with the 4-point scale “Not all all/ Just a little/ A fair amount/ A great deal”.
Demographic and survey specific variables
Demographic variables included gender, age, country, household composition (single adult smoker/ all adult smokers/ mixed adult household), household income (Low/ Moderate/ High) and education level (Low/ Moderate/ High). Survey specific variables included: survey mode (Telephone/ Web) and time between assessments. The effect of these variables were adjusted for in all regression analyses.
Statistical analysis
Two main sets of analyses were conducted:
1. Predicting vaping uptake and current vaping frequency
A series of multilevel binary logistic (for vaping uptake) and multilevel ordinal logistic regressions (for frequency of current vaping) were used to examine the impact of smoking related, demographic and survey specific variables (explanatory variables) on (1) vaping uptake and (2) vaping frequency (outcome variables). All explanatory variables were taken from one wave prior to that of the outcome variables. For the analysis of vaping uptake, we only included observations from participants who reported no vaping in prior wave, and we only used data second waves onwards because lifetime vaping was not measured in the first wave. For the frequency models, we used data from all six waves. Figure 1 shows the number of observations used in different analyses between waves. Multilevel models with random intercept were used to account for the repeated observations on some participants. Because the drop-out rate between the fifth and sixth waves was substantially higher, we conducted a supplementary analysis without using data from the sixth wave to evaluate the robustness of our results.
Figure 1.
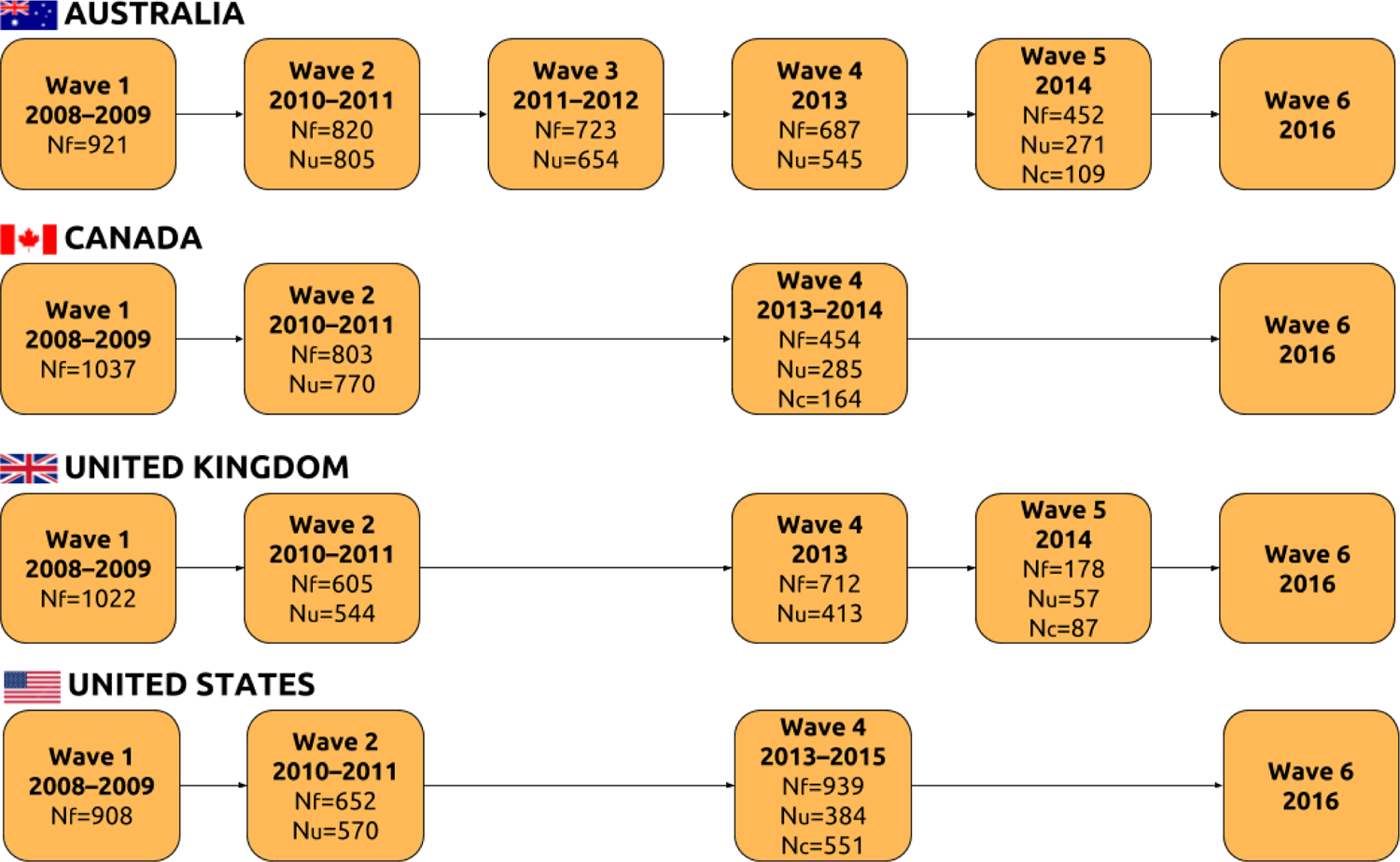
Sample size from each country for each analysis.
Nf : The number of observations in prior wave predicting vaping frequency in the next wave; Nu: The number of observations in prior wave predicting VNPs uptake in the next wave; Nc: The number of observations in prior wave predicting ongoing vaping.
2. Predicting ongoing use among those who reported ever vaped
Because the goal of this analysis was to examine factors that predicted ongoing vaping in the most recent wave among those who have initiated vaping, and the prevalence of vaping was low up until this point, only the subset of participants who reported ever vaping at the fifth wave (collected in 2013–2014) were included. Therefore, the fifth wave served as a baseline wave for this analysis. Logistic regression was used to examine the impact of smoking-related variables on ongoing use, adjusted for demographic and survey-specific variables (e.g., survey mode and time between assessments). To evaluate the robustness of our results, we conducted two sets of supplementary analyses. First, we limited our analyses to those who reported current vaping at the fifth wave (as opposed to ever use). Second, we excluded participants from the UK because the dropout rate in the UK for the sixth was much higher than the other three countries.
All analyses were performed in STATA 13. A partially adjusted model was run first and included only the target smoking-related predictor, demographic and survey-specific variables as predictor variables. Variables that were significant at an alpha level of 0.05 were included in the final adjusted analysis. In the analysis sample, there was less than 10% missing data in each variable. Multiple imputation was used to fill in missing data (19) and all regression analyses were based on 10 imputed datasets.
Results
Of the 6296 participants, 27% from Australia, 22% from Canada, 22% from United Kingdom and 30% from the United States. The mean age was 52, and 53% were female. These participants contributed 10913 observations over the study period. Because only participants who contributed data to at least two consecutive waves were included, differences between participants who remained and dropped out of the study were examined and detailed results were presented in Supplementary Tables 2A and 2B. Although there were statistically significant differences in some analysis variables, the effect sizes were mostly very small (Cramer’s V below 0.1 for categorical variables and Cohen’s D below 0.1 for continuous variable). Therefore, excluding these participants would be unlikely to change or negate our conclusion because the results on which our conclusion were based were highly significant (p < .001; see result section below) and the effect sizes were moderately large.
Table 1A and 1B show descriptive statistics of the sample for smoking-related variables, and demographic and survey-specific variables respectively. The proportion of daily smokers who reported ever vaping was highest in the US, followed by the UK and Canada, and lowest in Australia.
Table 1A.
Descriptive statistics for participants when they first participated in the ITC study.
| Australia | Canada | UK | US | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | |
| Lifetime VNP use | ||||||||||
| No | 1345 | 92.06 | 1174 | 85.44 | 1046 | 81.46 | 1152 | 62.07 | 4717 | 78.95 |
| Yes | 116 | 7.94 | 200 | 14.56 | 238 | 18.54 | 704 | 37.93 | 1258 | 21.05 |
| Frequency of current vaping | ||||||||||
| Not at all | 1439 | 96.90 | 1274 | 92.72 | 1181 | 86.77 | 1543 | 83.14 | 5437 | 89.48 |
| Less than once a month | 12 | 0.81 | 36 | 2.63 | 33 | 2.42 | 114 | 6.14 | 195 | 3.21 |
| Less than weekly | 18 | 1.21 | 13 | 0.95 | 46 | 3.38 | 45 | 2.42 | 122 | 2.01 |
| Less than daily | 1 | 0.07 | 21 | 1.53 | 46 | 3.38 | 69 | 3.72 | 137 | 2.25 |
| Daily | 15 | 1.01 | 30 | 2.18 | 55 | 4.04 | 85 | 4.58 | 185 | 3.04 |
| Intention to quit smoking | ||||||||||
| No | 417 | 28.48 | 321 | 24.32 | 521 | 39.08 | 501 | 30.38 | 1760 | 30.52 |
| Yes | 1047 | 71.52 | 999 | 75.68 | 812 | 60.92 | 1148 | 69.62 | 4006 | 69.48 |
| Time to first cigarette | ||||||||||
| More than 60 mins | 188 | 12.82 | 136 | 10.16 | 186 | 13.82 | 207 | 11.83 | 717 | 12.15 |
| 31–60 mins | 282 | 19.24 | 262 | 19.58 | 249 | 18.50 | 328 | 18.74 | 1121 | 19.00 |
| 6 – 30mins | 708 | 48.29 | 656 | 49.03 | 676 | 50.22 | 853 | 48.74 | 2893 | 49.03 |
| 5mins or less | 288 | 19.65 | 284 | 21.23 | 235 | 17.46 | 362 | 20.69 | 1169 | 19.81 |
| Depressive symptoms – Little interest or pleasure | ||||||||||
| No | 1054 | 73.35 | 994 | 74.35 | 1031 | 79.37 | 1327 | 77.20 | 4406 | 76.07 |
| Yes | 383 | 26.65 | 343 | 26.65 | 268 | 20.63 | 392 | 22.80 | 1386 | 23.93 |
| Depressive symptoms – Feeling down or hopeless | ||||||||||
| No | 1001 | 67.50 | 415 | 30.23 | 956 | 70.66 | 1281 | 71.33 | 4196 | 69.88 |
| Yes | 482 | 32.50 | 958 | 69.77 | 397 | 29.34 | 515 | 28.67 | 1809 | 30.12 |
| M | SD | M | SD | M | SD | M | SD | M | SD | |
| Quitting self-efficacy | 2.28 | 1.21 | 2.44 | 1.17 | 2.16 | 1.25 | 2.42 | 1.24 | 2.33 | 1.22 |
| Enjoy life less after quitting | 2.11 | 1.03 | 2.08 | 0.99 | 2.36 | 1.09 | 2.14 | 1.02 | 2.16 | 1.04 |
| Worry about adverse future health effect | 2.64 | 1.01 | 2.64 | 0.99 | 2.50 | 1.01 | 2.62 | 0.98 | 2.60 | 1.00 |
| Overall opinion about smoking | 3.61 | 0.90 | 3.64 | 0.93 | 3.41 | 0.94 | 3.51 | 0.89 | 3.54 | 0.92 |
| Current health | 3.01 | 0.99 | 3.06 | 0.95 | 2.94 | 1.02 | 2.97 | 0.97 | 2.99 | 0.99 |
| Past adverse health effect of smoking | 2.24 | 0.81 | 2.14 | 0.85 | 2.11 | 0.87 | 2.32 | 0.89 | 2.21 | 0.86 |
Table 1B.
Descriptive statistics for participants when they first participated in the ITC study.
| Australia | Canada | UK | US | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | |
| Gender | ||||||||||
| Female | 816 | 54.55 | 745 | 53.75 | 727 | 52.95 | 951 | 50.91 | 3239 | 52.90 |
| Male | 680 | 45.45 | 641 | 46.25 | 646 | 47.05 | 917 | 49.09 | 2884 | 47.10 |
| Household income | ||||||||||
| Low | 392 | 26.20 | 313 | 22.58 | 415 | 30.23 | 670 | 35.87 | 1790 | 29.23 |
| Moderate | 433 | 28.94 | 491 | 35.43 | 434 | 31.61 | 581 | 31.10 | 1939 | 31.67 |
| High | 572 | 38.24 | 472 | 34.05 | 403 | 29.35 | 538 | 28.80 | 1985 | 32.42 |
| Not reported | 99 | 6.62 | 110 | 7.94 | 121 | 8.81 | 79 | 4.23 | 409 | 6.68 |
| Education level | ||||||||||
| Low | 861 | 57.59 | 577 | 41.78 | 744 | 54.71 | 797 | 42.69 | 2979 | 48.81 |
| Moderate | 387 | 25.89 | 518 | 37.51 | 363 | 26.69 | 705 | 37.76 | 1973 | 32.33 |
| High | 247 | 16.52 | 286 | 20.71 | 253 | 18.60 | 365 | 19.55 | 1151 | 18.86 |
| M | SD | M | SD | M | SD | M | SD | M | SD | |
| Age (in years) | 49.46 | 12.70 | 50.98 | 11.89 | 50.75 | 13.28 | 53.89 | 12.63 | 51.09 | 12.73 |
| Time between assessment (in years) | 1.49 | 0.32 | 1.82 | 0.45 | 1.64 | 0.24 | 1.64 | 0.37 | 1.65 | 0.37 |
1. Predicting vaping uptake and current vaping frequency
Table 2 shows odds ratios and the associated 95% confidence intervals from multilevel analyses predicting vaping uptake and vaping frequency. Overall, the predictors of uptake and frequency of use were similar. Respondents from UK and US were more likely to take up vaping and to have a higher frequency of use, compared to those Australia. Females were more likely to take up vaping and vape more frequently as were those of moderate education. Those of a higher education level reported higher vaping frequency. Those with high incomes were also more likely to have higher frequency of vaping. Turning to smoking-related variables, the more cigarettes the person smoked per day at previous wave, the more likely they were to take up vaping (OR = 1.41, 95% CI [1.12, 1.78] for 21–30 cigarettes; OR = 1.69, 95% CI [1.19, 2.39] for 30 + cigarettes; reference category: 0 – 10 cigarettes) and the greater the frequency of vaping (OR = 1.46, 95% CI [1.12, 1.91] for 20–30 cigarettes; OR = 1.97, 95% CI [1.36, 2.85] for 30+ cigarettes) in next wave. Time to first cigarette was significantly associated in a similar way in the partially adjusted models but this association dropped out in the fully adjusted model when cigarettes per day was included. Those with an intention to quit smoking were more likely to vape at a greater frequency (OR = 1.48, 95% CI [1.21, 1.82]). Finally, those who reported depressive symptoms, particularly feeling down or hopeless were more likely to report a higher frequency of vaping.
Table 2.
Multilevel logistic regression predicting VNP uptake and multilevel ordinal logistic regression predicting vaping frequency (Nobservation = 5296 and Nparticipants = 3797 for the uptake model; Nobservation = 10913 and Nparticipants = 6296 for the frequency model)
| VNP uptake | Frequency of VNP usea | |||||||
|---|---|---|---|---|---|---|---|---|
| Partially adjusted model | Final adjusted model | Partially adjusted model | Final adjusted model | |||||
| Smoking-related variables | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Intention to quit smoking (Ref: No) | ||||||||
| Yes | 1.19* | (1.02, 1.40) | 1.16 | (0.98, 1.39) | 1.53*** | (1.26, 1.84) | 1.48*** | (1.21, 1.82) |
| Time to first cigarette (Ref: More than 60mins) | ||||||||
| 31–60mins | 1.34* | (1.01, 1.78) | 1.27 | (0.96, 1.69) | 1.30 | (0.97, 1.76) | 1.19 | (0.88, 1.61) |
| 6 to 30mins | 1.34* | (1.05, 1.70) | 1.19 | (0.92, 1.54) | 1.52** | (1.17, 1.99) | 1.31 | (0.99, 1.73) |
| 5 min or less | 1.51** | (1.14, 1.99) | 1.22 | (0.91, 1.64) | 1.37* | (1.01, 1.85) | 1.07 | (0.77, 1.48) |
| Cigarette per day (Ref: 0 – 10) | ||||||||
| 11–20 cigarettes | 1.17 | (0.99, 1.38) | 1.13 | (0.95, 1.35) | 1.26* | (1.05, 1.52) | 1.19 | (0.98, 1.46) |
| 21 – 30 cigarettes | 1.47*** | (1.19, 1.84) | 1.41** | (1.12, 1.78) | 1.50*** | (1.17, 1.92) | 1.46** | (1.12, 1.91) |
| More than 31 cigarettes | 1.77*** | (1.28, 2.45) | 1.69** | (1.19, 2.39) | 1.96*** | (1.38, 2.78) | 1.97*** | (1.36, 2.85) |
| Past year alcohol use (Ref: No alcohol use) | ||||||||
| Daily | 1.26 | (0.98, 1.63) | 0.72* | (0.52, 0.99) | 0.72* | (0.53, 0.99) | ||
| Weekly | 1.00 | (0.82, 1.23) | 0.94 | (0.75, 1.18) | 0.97 | (0.77, 1.22) | ||
| Monthly or less frequent | 0.93 | (0.77, 1.13) | 1.01 | (0.82, 1.26) | 1.04 | (0.84, 1.28) | ||
| Quitting self-efficacy | 0.94* | (0.88, 1.00) | 0.96 | (0.90, 1.03) | 0.91* | (0.85, 0.98) | 0.93 | (0.86, 1.00) |
| Enjoy life less after quitting | 0.97 | (0.90, 1.04) | 0.95 | (0.87, 1.02) | ||||
| Worry about adverse health effect in future | 1.11** | (1.04, 1.20) | 1.06 | (0.97, 1.16) | 1.17*** | (1.07, 1.27) | 1.05 | (0.95, 1.16) |
| Depressive symptom - little interest or pleasures | 1.21* | (1.02, 1.44) | 1.02 | (0.82, 1.27) | 1.22* | (1.02, 1.46) | 0.99 | (0.78, 1.23) |
| Depressive symptom - feeling down or hopeless | 1.28*** | (1.10, 1.49) | 1.18 | (0.98, 1.43) | 1.35*** | (1.15, 1.61) | 1.24* | (1.01, 1.52) |
| Overall opinion about smoking | 1.01 | (0.94, 1.10) | 1.06 | (0.97, 1.16) | ||||
| Current health | 0.94 | (0.87, 1.01) | 0.90* | (0.83, 0.98) | 0.98 | (0.89, 1.08) | ||
| Past adverse health effect of smoking | 1.11* | (1.02, 1.21) | 1.02 | (0.92, 1.12) | 1.17*** | (1.06, 1.29) | 1.04 | (0.92, 1.16) |
| Demographic and survey specific variables | ||||||||
| Gender (Ref: Female) | ||||||||
| Male | 0.87 | (0.76, 1.00) | 0.87* | (0.75, 1.00) | 0.79** | (0.67, 0.93) | 0.82** | (0.69, 0.97) |
| Country (Ref: Australia) | ||||||||
| Canada | 1.00 | (0.64, 1.40) | 1.03 | (0.73, 1.45) | 0.96 | (0.71, 1.30) | 0.98 | (0.73, 1.33) |
| US | 1.66*** | (1.22, 2.25) | 1.80** | (1.32, 2.45) | 1.99*** | (1.56, 2.54) | 2.14*** | (1.67, 2.75) |
| UK | 2.85*** | (2.15, 3.78) | 3.18*** | (2.37, 4.28) | 5.19*** | (4.06, 6.67) | 5.63*** | (4.37, 7.25) |
| Household income (Ref: Low) | ||||||||
| Moderate | 1.14 | (0.96, 1.37) | 1.19 | (1.00, 1.43) | 1.15 | (0.93, 1.42) | 1.17 | (0.96, 1.46) |
| High | 1.15 | (0.95, 1.38) | 1.21 | (1.00, 1.46) | 1.30* | (1.05, 1.61) | 1.37** | (1.10, 1.71) |
| Not reported | 1.23 | (0.92, 1.65) | 1.28 | (0.95, 1.71) | 1.28 | (0.90, 1.82) | 1.32 | (0.93, 1.88) |
| Education level (Ref: Low) | ||||||||
| Moderate | 1.27** | (1.08, 1.48) | 1.29** | (1.10, 1.52) | 1.25* | (1.04, 1.51) | 1.25* | (1.04, 1.51) |
| High | 1.08 | (0.89, 1.23) | 1.07 | (0.90, 1.32) | 1.31* | (1.05, 1.64) | 1.36** | (1.08, 1.70) |
| Age (Unit: 10 years) | 0.76*** | (0.71, 0.82) | 0.76*** | (0.71, 0.82) | 0.84*** | (0.78, 0.91) | 0.85** | (0.79, 0.92) |
Survey specific variables, including time between assessment and survey mode, were adjusted for in all models.
p < .005;
p < .01;
p < .05.
Frequency of use was measured in 5-point scale from Daily to Not at all.
Given the higher dropout rate between the last two data collections, we repeated the same analyses using only data from the first five waves. The results were similar and the same conclusion can be drawn.
2. Predicting ongoing vaping among those who tried vaping
Table 3 shows the odds ratios and the associated 95% confidence intervals from the logistic regression predicting ongoing vaping among daily smokers who reported ever vaping in the second last wave (the second last wave served as the baseline wave for this analysis). The more respondents vaped at baseline, the more likely they were to still be vaping at the follow-up (OR = 11.98, 95% CI [6.00, 23.93] for daily vaping; OR = 9.80, 95% CI [5.16, 18.60] for weekly vaping; OR = 4.32, 95% CI [2.71, 6.87]; reference category: vaped less than monthly). Also, compared to those who were daily smokers at follow-up, those who became non-daily smokers were more likely to continue vaping (OR = 4.99, 95% CI [2.39, 10.43]) while those who had quit smoking altogether were significantly less likely to continue to vape (OR = 0.48, 95% CI [0.29, 0.80]).
Table 3.
Logistic regression predicting on-going VNP use among baseline daily smokers who reported ever vaping (N = 911).
| Partially adjusted model | Final adjusted model | |||
|---|---|---|---|---|
| Baseline predictors: | OR | 95% CI | OR | 95% CI |
| Intention to quit smoking (Ref: No) | ||||
| Yes | 1.32 | (0.92, 1.90) | ||
| 31–60mins | 1.07 | (0.66, 1.74) | ||
| 6 to 30mins | 1.24 | (0.81, 1.90) | ||
| 5 min or less | 1.20 | (0.72, 2.00) | ||
| Cigarette per day (Ref: 0 – 10) | ||||
| 11–20 cigarettes | 1.16 | (0.86, 1.58) | ||
| 21 – 30 cigarettes | 1.11 | (0.72, 1.70) | ||
| More than 31 cigarettes | 1.08 | (0.56, 2.08) | ||
| Past year alcohol use (Ref: No alcohol use) | ||||
| Daily | 1.24 | (0.36, 4.28) | ||
| Weekly | 1.12 | (0.48, 2.60) | ||
| Monthly or less frequent | 1.14 | (0.57, 2.28) | ||
| Quitting self-efficacy | 1.01 | (0.90, 1.14) | ||
| Enjoy life less after quitting | 1.00 | (0.86, 1.17) | ||
| Worry about adverse health effect in future | 1.13 | (0.97, 1.31) | ||
| Depressive symptom - little interest or pleasures | 0.94 | (0.69, 1.29) | ||
| Depressive symptom - feeling down or hopeless | 1.25 | (0.91, 1.71) | ||
| Overall opinion about smoking | 0.94 | (0.80, 1.10) | ||
| Current health | 1.07 | (0.92, 1.25) | ||
| Past adverse health effect of smoking | 0.95 | (0.79, 1.14) | ||
| Vaping frequency (Ref: Less than monthly) | ||||
| Daily | 11.93*** | (6.12, 23.25) | 11.98*** | (6.00, 23.93) |
| Weekly | 9.35*** | (4.95, 17.64) | 9.80*** | (5.16, 18.6) |
| Monthly | 4.13*** | (2.60, 6.54) | 4.32*** | (2.71, 6.87) |
| Smoking status at follow-up wave (Ref: Daily smoker) | ||||
| Non-daily smoker | 5.51*** | (2.28, 10.94) | 4.99*** | (2.39, 10.43) |
| Quitter | 0.62* | (0.39, 0.97) | 0.48** | (0.29, 0.80) |
Note: Demographic and survey specific variables were adjusted for in all models;
p < .001;
p < .01;
p <.05.
We repeated these analyses with only participants who reported current vaping at the fifth wave (as opposed to ever vaped) and the results were essentially the same, although standard errors of the estimates were larger due to a reduction of sample size. We have also repeated the analysis without the samples from the UK given its higher dropout rate. The results were similar, and the same conclusion was drawn.
Discussion
Intention to quit smoking was a strong predictor of high frequency of vaping and this finding aligns with cross-sectional research showing that vaping was more likely in those with higher levels of motivation to quit and in those who had made a quit attempt in the last year (13, 20).
After adjusting for other smoking-related variables, more frequent smoking was predictive of vaping uptake and more frequent vaping, but it was not associated with ongoing vaping. It is unclear whether the latter finding is due to successful quitting or giving up on vaping following a failure to quit. It is also possible that the non-significant association between smoking frequency and ongoing vaping was due to reduced power because the sample size in that analysis was substantially lower. Nonetheless, the finding that heavy smokers may be more likely to vape should be considered when evaluating the efficacy of NVPs as cessation aids.
Several smoking related-variables, such as quitting self-efficacy, worrying about future adverse health effects and experience of past adverse health effects of smoking, were significantly associated with vaping uptake and vaping frequency in the partially adjusted models. However, these associations did not persist after adjusting for other smoking variables, such as quit intentions and cigarettes smoked per day. This suggests that their effect may be mediated by those variables that remained in the models.
Having symptoms of depression was significantly associated with vaping uptake and vaping frequency in the partially adjusted models, and it remained significant in predicting vaping frequency in the final adjusted model. Past research has demonstrated a bidirectional effect between depression and smoking (21–24), suggesting that depressed individuals may smoke as a form of self-medication and that smoking may lead to increased depressive symptoms. In our study, we showed that depressive symptoms predicted higher vaping frequency, and this effect was independent of smoking. This finding is consistent with the possibility that some smokers with depressive symptoms may vape as a form of self-medication (25).
Among daily smokers who have ever vaped, ongoing vaping does not appear to be influenced directly by any of the smoking-related factors that were important in predicting uptake and vaping frequency. Instead, vaping frequency in the past was a strong predictor of ongoing use, with those vaping daily more likely to be vaping at follow-up than those who vaped only occasionally. Consistent with previous cross-sectional research (20), this suggests that established vapers are more likely to vape long term than experimenters. The reasons for the continuation and discontinuation of vaping are unclear although past research suggests that product satisfaction, lower harm beliefs and use in smoke-free places motivate smokers to continue to vape (26). Those who have discontinued vaping report that it was because NVPs did not control their cravings, or that they did not “feel” similar enough to smoking cigarettes (20). Our findings also suggest that the extent to which vaping helps daily smokers to manage their smoking by cutting down or quitting also influences ongoing use. Daily smokers who managed to cut down their smoking via vaping were more likely to vape longer term, whereas those who managed to quit smoking were less likely to do so. The latter is consistent with the previous finding that most vapers who no longer smoke intend to discontinue vaping eventually (26).
The study’s strengths were its longitudinal design and data collection in several countries. It also had several limitations. First, the analysis was based on self-report data and the prevalence of vaping might be underestimated. This analysis only looks at vaping over time. We did not analyse smoking status over time because of the relatively small number of vapers whose smoking status changed in the study period (especially in the earlier waves when vaping was less common). We were therefore not able to assess whether those who started vaping and discontinued succeeded in quitting smoking or relapsed. Second, the latest data collection was mainly based on online surveys, rather than the telephone surveys used in earlier waves. It is unclear how this might have affected our findings, if at all.
Conclusion
Among daily smokers, motivation to quit and heaviness of smoking appear to be the main factors influencing vaping uptake and vaping frequency. Ongoing use appears to depend on the initial frequency of use and how helpful vaping has been in managing their smoking. The fact that intention to quit smoking is a strong predictor of vaping accords with other research findings that quitting smoking is one of the primary reasons that smokers vape.
Supplementary Material
Acknowledgement
[ITC 4C Survey:]
The ITC Four Country Survey for Waves 7 to 10 was supported by grants from the US National Cancer Institute (R01 CA100362, P50 CA111236 (Roswell Park Transdisciplinary Tobacco Use Research Center), and P01 CA138389), the Canadian Institutes of Health Research (MOP-79551, MOP-115016, FDN-148477), the National Health and Medical Research Council of Australia (450110, 1005922), and Cancer Research UK (C312/A11039, C25586/A19540).
[ITC 4CV Survey:]
The ITC Four Country Smoking and Vaping Survey was supported by grants from the US National Cancer Institute (P01 CA200512), the Canadian Institutes of Health Research (FDN-148477), and the National Health and Medical Research Council of Australia (APP1106451).
Footnotes
Declarations of competing interest: None
Ethical Approval
ITC 4C Survey (The first five waves)
The survey protocols and all materials, including the survey questionnaires were cleared for ethics by Research Ethics Office, King’s College London, UK; Office of Research Ethics, University of Waterloo, Canada; Human Research Ethics, Cancer Council Victoria, Australia; and Office of Research Subject Protection, Roswell Park Cancer Institute, US.
ITC 4CV Survey (The sixth wave)
The survey protocols and all materials, including the survey questionnaires were cleared for ethics by Research Ethics Office, King’s College London, UK; Office of Research Ethics, University of Waterloo, Canada; and Human Research Ethics, Cancer Council Victoria, Australia.
Reference
- 1.Australian Bureau of Statistics. National Health Survey - First Results. Canberra: Australian Bureau of Statistics; 2015. [Google Scholar]
- 2.Office of National Statistics. Statistical bulletin: Adult smoking habits in the UK: 2016 2017 [Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandlifeexpectancies/bulletins/adultsmokinghabitsingreatbritain/2016.
- 3.Farsalinos KE, Poulas K, Voudris V, Le Houezec J. Electronic cigarette use in the European Union: analysis of a representative sample of 27 460 Europeans from 28 countries. Addiction. 2016;111(11):2032–40. [DOI] [PubMed] [Google Scholar]
- 4.West r, Beard E, Brown J. Trends in electronic cigarette use in England London: University College London; 2017. [Available from: www.smokinginengland.info/latest-statistics. [Google Scholar]
- 5.Rutten LJF, Blake KD, Agunwamba AA, Grana RA, Wilson PM, Ebbert JO, et al. Use of e-cigarettes among current smokers: associations among reasons for use, quit intentions, and current tobacco use. Nicotine & Tobacco Research. 2015;17(10):1228–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cooper M, Harrell MB, Perry CL. Comparing young adults to older adults in e-cigarette perceptions and motivations for use: implications for health communication. Health education research. 2016;31(4):429–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adkison SE, O’Connor RJ, Bansal-Travers M, Hyland A, Borland R, Yong H-H, et al. Electronic nicotine delivery systems: international tobacco control four-country survey. American journal of preventive medicine. 2013;44(3):207–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farsalinos KE, Poulas K, Voudris V, Le Houezec J. E-cigarette use in the European Union: millions of smokers claim e-cigarettes helped them quit. Addiction. 2017;112(3):545–6. [DOI] [PubMed] [Google Scholar]
- 9.Rahman MA, Hann N, Wilson A, Mnatzaganian G, Worrall-Carter L. E-cigarettes and smoking cessation: evidence from a systematic review and meta-analysis. PloS one. 2015;10(3):e0122544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Biener L, Hargraves JL. A longitudinal study of electronic cigarette use among a population-based sample of adult smokers: association with smoking cessation and motivation to quit. Nicotine & Tobacco Research. 2014;17(2):127–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pearson JL, Richardson A, Niaura RS, Vallone DM, Abrams DB. e-Cigarette awareness, use, and harm perceptions in US adults. American journal of public health. 2012;102(9):1758–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yong H-H, Borland R, Balmford J, McNeill A, Hitchman S, Driezen P, et al. Trends in e-cigarette awareness, trial, and use under the different regulatory environments of Australia and the United Kingdom. Nicotine & Tobacco Research. 2014;17(10):1203–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vardavas CI, Filippidis FT, Agaku IT. Determinants and prevalence of e-cigarette use throughout the European Union: a secondary analysis of 26 566 youth and adults from 27 Countries. Tobacco control. 2015;24(5):442–8. [DOI] [PubMed] [Google Scholar]
- 14.Levy DT, Yuan Z, Li Y. The Prevalence and Characteristics of E-Cigarette Users in the US. International Journal of Environmental Research and Public Health. 2017;14(10):1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fong GT, Cummings KM, Borland R, Hastings G, Hyland A, Giovino GA, et al. The conceptual framework of the International Tobacco Control (ITC) policy evaluation project. Tobacco control. 2006;15(suppl 3):iii3–iii11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thompson ME, Fong GT, Hammond D, Boudreau C, Driezen P, Hyland A, et al. Methods of the International Tobacco Control (ITC) four country survey. Tobacco control. 2006;15(suppl 3):iii12–iii8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thompson ME, Fong GT, Boudreau C, Driezen P, Li G, Gravely SM, et al. Methods of the ITC Four Country Smoking and Vaping Survey, Wave 1 (2016). Addiction. 2018;E-cigarette supplement. [DOI] [PMC free article] [PubMed]
- 18.Spitzer RL, Williams JB, Kroenke K, Linzer M, Verloin deGruy F, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 study. Jama. 1994;272(22):1749–56. [PubMed] [Google Scholar]
- 19.Rubin DB. Multiple imputation for nonresponse in surveys. New York: John Wiley & Sons; 2009. [Google Scholar]
- 20.Simonavicius E, McNeill A, Arnott D, Brose LS. What factors are associated with current smokers using or stopping e-cigarette use? Drug and Alcohol Dependence. 2017;173:139–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leung J, Gartner C, Hall W, Lucke J, Dobson A. A longitudinal study of the bi-directional relationship between tobacco smoking and psychological distress in a community sample of young Australian women. Psychological medicine. 2012;42(6):1273–82. [DOI] [PubMed] [Google Scholar]
- 22.Chaiton MO, Cohen JE, O’Loughlin J, Rehm J. A systematic review of longitudinal studies on the association between depression and smoking in adolescents. BMC public health. 2009;9(1):356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cooper J, Borland R, Yong HH, Fotuhi O. The impact of quitting smoking on depressive symptoms: findings from the International Tobacco Control Four-Country Survey. Addiction. 2016;111(8):1448–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cooper J, Borland R, McKee SA, Yong HH, Dugué PA. Depression motivates quit attempts but predicts relapse: differential findings for gender from the International Tobacco Control Study. Addiction. 2016;111(8):1438–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cummins SE, Zhu S-H, Tedeschi GJ, Gamst AC, Myers MG. Use of e-cigarettes by individuals with mental health conditions. Tobacco control. 2014:tobaccocontrol-2013-051511. [DOI] [PMC free article] [PubMed]
- 26.Ma BH, Yong HH, Borland R, McNeill A, Hitchman SC. Factors associated with future intentions to use personal vaporisers among those with some experience of vaping. Drug and Alcohol Review. 2017. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


