Abstract
The coronavirus disease 2019 (COVID-19) pandemic has had a major impact on education at all age levels, including professional schools and health professions programs. We describe the experience of adapting preclinical medical school courses within an integrated curriculum to virtual instruction. A major feature of two of the courses were pathology small groups adapted from pathology courses in the previous medical school curriculum. These small groups were designed to use facilitated groups of 8 to 10 students. With a sudden change to virtual learning, these small groups were shifted to large group virtual sessions. In general, the conversion went well, with ongoing optimization of the format of the large group sessions mainly occurring over the first several sessions. End-of-course student evaluations were generally positive, but with a preference toward returning to live sessions in the future. Scores on 5 multiple choice examinations in the spring 2020 course were essentially identical in mean, standard deviation, and distribution to examinations in the previous 2 years of the course that had similar layout and topic organization. We discuss the challenges and successes of the switch to virtual instruction and of teaching pathology content within an integrated medical school curriculum.
Keywords: COVID-19, course director, disease mechanisms, educational cases, integrated curricula, medical school pathology, pathology education, virtual teaching
Introduction
Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), was officially classified by the World Health Organization as a pandemic on March 11, 2020.1,2 The pandemic has had major impact throughout society, including education throughout all levels.3-5 In conjunction with government actions and recommendations, schools have had to make difficult decisions on whether to continue with in-person classes, adopt hybrid models, or switch completely to virtual teaching. Medical schools and health professions programs faced the difficult task of teaching hands-on skills (including physical examination and interviewing of patients) through virtual or partly virtual models.6-14 The switch to virtual education impacts interaction, role-modeling, and networking among students and faculty. For students, social isolation, financial stress (eg, loss or partial loss of employment by student and/or partner), and impacts on childcare or schooling (for students who are parents) are additional downstream consequences.3,15-19 Faculty and other instructors may struggle with technology used for virtual technology, especially if they have little or no prior experience with virtual instruction.7,20-22
The sudden disruptions to education caused by the COVID-19 pandemic have forced educators throughout the world to come up with creative virtual solutions for curriculum delivery.3-5 In this report, we describe pathology content and delivery in preclinical medical school courses at a public academic medical center that combines medical and physician assistant students in the first 18 months of training. In 2014, our medical school switched from a 24 month subject-based course structure that included a dedicated 2-semester Medical Pathology course to an 18 month integrated curriculum with centrally managed multidisciplinary courses. This change in curriculum follows a broader trend seen within United States allopathic medical schools in the last decade toward integrated curricula.23-25 A major component of the pathophysiology and histopathology education in the preclinical curriculum is delivered via pathology case analysis small groups which are facilitated by pathology faculty and residents. We discuss changes and lessons learned for pathology education in the switch to an integrated curriculum in 2014 and then the adaptations in 2020 for virtual teaching.
Methods
Background on Curriculum
The University of Iowa Carver College of Medicine (CCOM) is currently the only allopathic medical school in the state of Iowa.26,27 The medical school class size is typically around 150 students. A unique aspect within the CCOM is that medical student and physician assistant students are merged for the preclinical courses. There are typically about 25 physician assistant students admitted per year.28 Carver College of Medicine implemented an integrated medical school curriculum starting in autumn of 2013, with the class entering in 2014 completely engaged with the new curriculum.26,29 The theoretical foundation for the current curriculum is described in a separate publication.30 The preclinical curriculum switched from 24 months of courses managed primarily by departments (eg, separate courses for biochemistry, medical genetics, medical pharmacology, medical pathology, etc) to 18 months of a centrally managed curriculum comprised primarily of 3 integrated course series: Mechanisms of Health and Disease (MOHD), Clinical and Professional Skills, and Medicine and Society. In the preclinical curriculum, the MOHD courses are graded on an Honors/Near Honors/Pass/Fail system. The remaining courses are graded on a binary Pass/Fail system. Table 1 summarizes some differences between the previous and current curriculum.
Table 1.
Comparison of Previous and Current Curriculum.
| Curriculum content | Previous curriculum through 2014* | Integrated curriculum (2015-)* |
|---|---|---|
| Preclinical courses | 24 months | 18 months |
| Main Pathology Content | Medical Pathology I and II (M2 year) | MOHD II, III, IV (M1/M2 years) |
| Exposure to Pathology Laboratories | Student selectives (2 hours) | Tour of core clinical laboratories (45 minutes) |
| Forensic/autopsy content |
Participation in autopsy on request Lecture |
Participation in autopsy on request Lecture, 2 hours interactive session |
| Pathology small groups | Throughout both semesters of Medical Pathology (2 hours/session × 23 sessions) | In the MOHD II-IV courses (1.5 hours/session × 15 sessions) |
Abbreviations: M1, first year of medical school; M2, second year of medical school; MOHD, Mechanisms of Health and Disease.
* The new curriculum impacting pathology content began with spring semester of 2015 for M1 students.
The MOHD series comprises much of the normal physiology, disease mechanisms, pathophysiology, and histopathology content of the preclinical curriculum.26,29,30 In the previous curriculum, the pathology-specific content was contained within 2 semester-long Medical Pathology courses in the M2 year. In the new curriculum, most of the pathology content was integrated into the 10-week MOHD III (end of M1 year) and 10-week MOHD IV (beginning of M2 year) courses. Two of the coauthors of the present report (MDK, TJS) have been codirectors of the MOHD III course since it was established in spring 2015. Another of the coauthors (LAB) has the primary role in the oversight, content, and organization of pathology small groups within the MOHD II, MOHD III, and MOHD IV courses.
All CCOM medical school courses have a “Liaison Committee” comprised of 6 students (typically 5 medical students and 1 physician assistant student). This group is in contact with the course directors and serves as the main conduit for information to the rest of the class. The Liaison Committee can bring forward any concerns or suggestions from the students (students can also contact course directors directly, if preferred). After completion of the course, the Liaison Committee prepares a report that summarizes student evaluations of the course and identifies strengths along with areas that might need improvement. These reports are formally presented at a meeting that includes curriculum administrators, student representatives, and all other preclinical course directors. These meetings occur about 3 to 6 months after the end of courses. At these meetings, the course directors are given the opportunity to respond to areas of concerns raised by the student committee and also to outline plans for modifying the course in future years.
Mechanisms of Health and Disease III Course
The MOHD III course covers disease mechanisms and pharmacology for a number of organ systems: fetal and reproductive, endocrine, cardiac, pulmonary, gastrointestinal/liver, hematologic, renal, and head/neck. The course also contains introduction to the principles of laboratory medicine, anatomic pathology, and imaging. The main course content is delivered by lecture and pathology small groups. As with other preclinical courses, all lectures are recorded, with the exception of some content for which video is not recorded due to sensitive images (death scene investigations). A limited number of lectures are prerecorded if the faculty member cannot be available at the preferred time in the schedule. In the event of unexpected unavailability, recorded lectures from a previous year have been used. There are a total of 5 multiple choice examinations in the 10-week course. Organ systems and concepts not included within the MOHD III course are found in the MOHD IV course, which focuses on immunologic, neurologic, psychiatric, infectious disease, musculoskeletal, and dermatologic disorders.
Mechanisms of Health and Disease Pathology Small Groups
The pathology small group content from the Medical Pathology courses in the previous curriculum was adapted and revised for the MOHD courses. The 20 groups are comprised of 8 to 10 students and 1 or 2 pathology facilitators. Physician assistant students are intermixed with the medical students, with 1 or 2 physician assistant students in each small group. In the previous curriculum, each small group session was 2 hours in length with 23 total sessions (46 total student contact hours). The small group sessions were shortened to 1.5 hours in the MOHD courses with 15 total sessions (22.5 total student contact hours) and an additional 45 minutes for each student for the clinical laboratory tour. There are 2 small group sessions in the MOHD II course (covering basic concepts such as cell death, inflammation, and repair), 8 in the MOHD III course (along with the clinical laboratory tours), and 5 in the MOHD IV course. MOHD II and III maintain the same small groups and facilitators, since both courses occur within a single semester. Mechanisms of Health and Disease IV uses a different set of small groups and facilitators.
There are 3 basic formats for pathology small group content. The first format, “Case Analysis,” utilizes internally developed software to present interactive cases via a web-based portal. Each case generally is comprised of a clinical history, imaging, gross pathology images, and a virtual slide. A case unfolds in an iterative fashion and students work through each case by answering questions in pop-up text boxes as they move through the case. Students are expected to completely work through every case each week and be prepared to discuss any aspects of the case when the group meets. Many of these cases also contain a mechanistic diagramming exercise in which the students are asked to arrange a logical sequence of risk factors, inciting events, clinical/pathologic findings, and pathologic mechanisms. These mechanistic diagrams have been used in both preclinical and clinical medical school teaching and evaluation at the University of Iowa.29,31,32
The second format of content delivery used in small groups are LabCAPS (Laboratory—Computer Assisted Patient Simulation) software that allows students to work through cases with a focus on laboratory work-up and testing. For each LabCAPS case, the students are provided a brief clinical history and physical examination findings and are then asked to devise differential diagnoses, order diagnostic testing (laboratory, imaging, and procedural [biopsy, etc]), in one or more iterations. They conclude the case by arriving at a diagnosis and recommending treatment. Students then are provided a comparison of how their work-up and diagnostic test ordering compares to expert consensus, including cost.33 In terms of cost, the students use Medicare reimbursement rates as an approximate surrogate. The students do not currently have a maximal budget on what they order.
The third format for the small groups is a hands-on session examining fixed gross specimens (eg, hearts or brains) or tours of pathology laboratories. In the previous curriculum, in addition to the small groups, all students were required to complete a “pathology selective” where they spent 2 hours in an area of pathology such as clinical chemistry, hematopathology, microbiology, or the gross room. In the current curriculum, this was replaced with a tour of the core clinical laboratories (clinical chemistry, hematopathology, flow cytometry) in the MOHD III course. Students are not required to attend an autopsy but are encouraged to do so at any point in their training.
Impact of COVID-19 on the University of Iowa Preclinical Medical School Courses
In March 2020, University of Iowa restrictions related to the evolving COVID-19 pandemic took effect after the first week of the MOHD III course. The following week was the university spring break, and subsequently most educational activities were moved online. The timing of the restrictions also meant that some students who had traveled for spring break were unable, at least temporarily, to return to Iowa City. A practical challenge was that internet access and bandwidth presented an issue in some cases.
The sudden switch to online teaching had immediate impact on preclinical medical school courses, specifically MOHD III which had just begun. Several decisions were made quickly. These included the following: cancellation of clinical laboratory tours in the second week of the course (impacting half of the students as the other half had already taken the tours), change of grading for MOHD III to Pass/Fail (from Honors/Near Honors/Pass/Fail), preferential use of prerecorded lectures from 2019 unless faculty wished to prerecord a new lecture, and adaptations that allowed students to take examinations off-campus. The 20 pathology small groups were converted to one large virtual group per week as it was not possible to hold in-person small groups due to limited availability of rooms large enough to permit social distancing. Conversion to virtual small groups was considered, but at that point in time, facilitator and curriculum support staff experience with virtual technology was too limited to ensure uniform student experience among the 20 groups. In making the changes to virtual large group format, the session length was increased from 1.5 to 2 hours. The course directors switched to use of the Zoom videoconferencing app/platform.34 Zoom meetings were held with the Liaison Committee. Zoom Question and Answer sessions were also set up on the Wednesdays before Friday examinations. Most meetings with students were also done by Zoom. Table 2 summarizes key changes in the switch to online learning.
Table 2.
Changes in Switch to Online Teaching in Mechanisms of Health and Disease (MOHD) III Course.
| Teaching method | Pre-COVID | Online (mid-March 2020) | Required participation?* |
|---|---|---|---|
| Lectures | Live, recorded | Pre-recorded or live Zoom | No |
| Quizzes | Online | Online | Yes |
| Examinations | Multiple choice, proctored on-campus | Can be taken remotely | Yes |
| Pathology small groups Case analysis LabCAPS Gross specimens |
8-10 students with facilitator† | Single large group Zoom† | Yes |
| Laboratory tours | Attend 45 minutes tour | Cancelled‡ | Yes |
Abbreviation: LabCAPS, Laboratory—Computer Assisted Patient Simulation.
* The participation requirements applied to both pre-COVID and online.
† The spring semester typically has a total of 10 sessions with facilitators. In spring semester 2020, a total of 8 sessions were adapted to large group Zoom format.
‡ Half of the class was able to participate in the live laboratory tours prior to COVID restrictions. The tours were cancelled for the remainder of the class due to timing of COVID restrictions. A virtual format will be used for spring semester 2021.
Adaptation of Small Group Sessions for Online Format
All regular case analysis cases required at least some modification in language and format to be utilized in the large group setting, and design of the Zoom sessions evolved over the subsequent weeks to include more student interaction via poll questions. Adapting the cases and creating the interactive session required a significant investment in faculty preparation time as compared to preparation for a usual live small group session. The LabCAPS cases, which were designed to be worked through beforehand by students, worked best in the large group setting with a presentation that demonstrated key features in the case in a PowerPoint presentation as opposed to trying to work through the LabCAPS software live. In addition, some modifications were made to the software to allow tracking of student preparation for all types of cases. Attendance for each large group session, which was required, was completed utilizing the Report function of Zoom. Table 3 summarizes pathology small groups before and after switch to virtual teaching. Supplemental Appendix 1 shows an example of a case analysis session adapted for the large group virtual session, including polling questions. Supplemental Appendix 2 shows a LabCAPS presentation adapted for large group virtual session.
Table 3.
Pathology Small Group Descriptions.
| Activity | Approximate time/case | Live | Online |
|---|---|---|---|
| Case analysis/LabCAPS | 30 minutes |
|
|
| Gross specimens | 45 mins gross specimens 45 mins gross or histology review |
|
|
Abbreviation: LabCAPS, Laboratory—Computer Assisted Patient Simulation.
Results
Overview of the Switch to Integrated Curriculum: Successes and Challenges
As described above, the University of Iowa CCOM fully implemented an integrated preclinical medical school curriculum with the class entering fall 2014. The majority of the pathology content was incorporated within the MOHD III and MOHD IV courses, with some background concepts such as cell death, inflammation, and tissue repair covered in earlier courses. The software infrastructure and a bank of cases for pathology small groups had been developed in the previous curriculum. A subset of the cases was adapted for the MOHD courses, with a number of cases revised or substituted based on facilitator and student feedback. Throughout the first 6 years of the MOHD III course, pathology small groups were consistently the highest or one of the highest rated aspects of the course. As an example, an end-of-course evaluation item on “Case Analysis was useful in understanding the course material” received 4.64 out of a 5.0 point scale (N = 117) for the 2019 course. The students appreciated the ability to present cases and interact with group facilitators. In addition, a 2-hour interactive session on forensic pathology (basics of death investigation and death certificates) was very highly rated, with a slight drop in ratings for the 2020 online session compared to the previous 2 years that were conducted in-person (2018: 4.51 out of 5.0, N = 123; 2019: 4.66 out of 5.0, N = 98; 2020: 4.27 out of 5.0, N = 101).
One ongoing effort with the MOHD III course has been in recruiting faculty who could teach blocks of material, as opposed to single lectures. A desire for this approach has consistently been indicated in yearly student evaluations. This has required some flexibility with recruiting the main faculty who teach within an organ or function system. For hematologic, gastrointestinal, and cardiovascular disorders, for example, the primary lecturers have been pathologists. For endocrinology and liver/biliary systems, the primary lecturers have been clinicians and basic scientists, with separate pathology lecture(s) included to cover histology and other pathologic aspects. The most consistent challenge with the course has been the integration of pharmacology/therapeutics with the pathophysiological material. This is an ongoing area of optimization.
Lessons Learned From the Mechanisms of Health and Disease III Course
The most immediate lessons learned during the 2020 MOHD III course were related to optimizing the large group Zoom sessions for the pathology case analysis groups. This included recognition that at least one moderator (in addition to the main presenter) was needed to triage questions from the audience. Students were directed to bring questions forward via the Chat function, and questions were far more numerous than usually encountered in small groups of 8 to 10 students. The first two sessions ran into time management challenges and subsequently the moderator took on a greater role in managing questions to determine which should be discussed with the entire group.
The switch to prerecorded lectures somewhat surprisingly resulted in few complaints from students. One benefit was that the lectures and recordings could be organized in the most optimal way that would be difficult to schedule in practice such as a lecturer giving 4 live lectures within a single day. A subset of students indicated appreciation for the lecturers that did new recordings for the 2020 course as opposed to using the 2019 recordings. This was not asked as a formal question on course evaluations but was mentioned in free text by 15 out of 101 students in lecture and end-of-course evaluations for the 2020 course. In soliciting feedback from faculty, questions emailed from students regarding lecture content were at a similar volume to previous years with live lectures. Lecturers were made available for a virtual question/answer session prior to each exam. Interestingly, examination score means and standard deviations were very similar for all 5 examinations for 2018, 2019, and 2020 (prior to 2018, course blocks were in a different arrangement and hard to compare directly; Figure 1).
Figure 1.
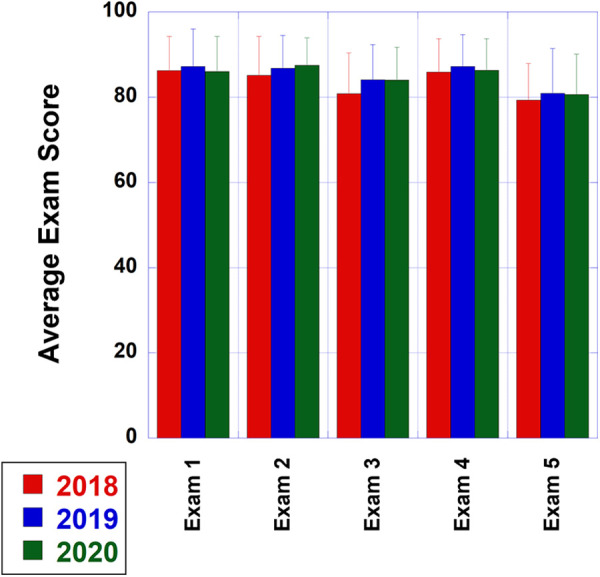
Examination scores (mean ± error bars showing standard deviation) for the 5 multiple-choice examinations for the MOHD III course (N = 174 for the 2018 and 2019 courses; N = 172 for the 2020 course). The course content over the 3 years shown was very similarly divided over the blocks of the course, with the 2019 and 2020 courses virtually identical except that the 2020 course used virtual instruction for all but 1 week of the course. For all examinations, the highest student score was 100% except for 98% in examination #5 in 2018. The lowest scores for the 5 examinations were (values indicate 2018, 2019, 2020, respectively): examination 1 (63%, 43%, 58%), examination 2 (58%, 60%, 67%), examination 3 (55%, 56%, 61%), examination 4 (58%, 60%, 59%), examination 5 (54%, 51%, 57%). MOHD indicates Mechanisms of Health and Disease.
Adjustments for Subsequent Courses
Pathology small groups for the MOHD IV course in fall semester 2020 used a similar approach to the MOHD III course in the previous spring, with a large group format. Additional emphasis was placed on interactive polling due to student feedback from MOHD III. The plan for the MOHD III course in spring 2021 is to return to individual pathology small groups but using Zoom. Interestingly, the Liaison Committee report for the MOHD III course and subsequent discussion indicated that there were a subset of students who appreciated the large group format for the pathology small groups relative to the 2 individual small group sessions in the MOHD II course prior to COVID-19 restrictions on live classes. The most consistent comments in favor of the large group format related to uniformity in presentation to all students. In general, ratings on end-of-course evaluation items covering broad aspects of the course (eg, course fairness, responsiveness of codirectors) were either essentially the same or slightly higher compared to the 2019 course. However, an exception was that the overall feedback on “Case analysis was useful in understanding the course material” dropped to 4.30 out of 5.0 (N = 108) in 2020 compared to 4.64 out of 5.0 in 2019 (N = 117). Students who preferred the individual small groups appreciated the ability to get direct feedback and have more engagement and accountability with the cases and with the other students and the facilitator. In the usual small group format students are expected to present parts of each case to the group, while all the responsibility for presentation was on faculty in the large group setting.
Discussion
Recent trends in medical school curricula in the United States present a challenge and an opportunity for education in laboratory medicine and pathology.35-37 Historically, many medical schools have utilized subject-based courses (eg, Anatomy, Biochemistry, Genetics, Pathology, Pharmacology, Physiology) in the preclinical curriculum. These courses may be managed by basic science or clinical departments related to the subject area. A more recent trend has been toward integrated curricula that feature multidisciplinary courses often managed more centrally.23-25 The University of Iowa CCOM fully implemented an 18-month integrated preclinical curriculum starting with the class entering 2014. Our experience has shown that pathology small groups that utilize knowledge in pathophysiology and histopathology can be an effective component of preclinical integrated courses. In our situation, small group cases developed in the previous traditional curriculum required some modifications for integrated courses.
The logistic changes due to the COVID-19 pandemic offered us an opportunity to see how pathology small groups, intended as facilitated live sessions, could be adapted to a virtual format. In our MOHD III course, the sessions functioned relatively well in a large group Zoom format. Content structure and delivery optimization occurred over the first several sessions. The student feedback on this switch was generally positive, although end-of-course evaluations suggested a preference toward the live small groups.
Overall, the experience enabled us to experiment with different teaching modalities and use this new knowledge in our continuing efforts to improve our preclinical courses. One concrete change has been to expand use of prerecorded sessions in MOHD III to maximize scheduling flexibility. For the 2021 course, the codirectors have offered this option to lecturers who give multiple lectures within a block or who have scheduling conflicts that make ideal placement of lectures challenging. This can be especially useful for back-to-back lectures where the first time slot can be prerecorded and the second one live, allowing for the lecturer to field student questions on both sessions. Lastly, our medical school and physician assistant programs share courses during the first 18 months of training, a unique structure for United States medical schools. The College of Medicine has found this to be an effective combination, with similar performance in the medical and physician assistant students throughout the preclinical course. A future goal is to analyze the outcomes and opportunities associated with this structure.
Supplemental Material
Supplemental Material, sj-pdf-1-apc-10.1177_23742895211015337 for Teaching Pathology in an Integrated Preclinical Medical School Curriculum and Adaptations to COVID-19 Restrictions by Matthew D. Krasowski, John L. Blau, Stephanie J. Chen, Karra A. Jones, Thomas J. Schmidt and Leslie A. Bruch in Academic Pathology
Supplemental Material, sj-pdf-2-apc-10.1177_23742895211015337 for Teaching Pathology in an Integrated Preclinical Medical School Curriculum and Adaptations to COVID-19 Restrictions by Matthew D. Krasowski, John L. Blau, Stephanie J. Chen, Karra A. Jones, Thomas J. Schmidt and Leslie A. Bruch in Academic Pathology
Acknowledgments
The authors thank Laina Edwards and Kim Crist for all their help with the MOHD III course, including the rapid switch to virtual instruction. The authors also thank Drs Fred Dee and Thomas Haugen for development of the software for case analysis, LabCAPS, and mechanistic diagrams and their efforts over the years with integrating these in medical school education.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Matthew D. Krasowski  https://orcid.org/0000-0003-0856-8402
https://orcid.org/0000-0003-0856-8402
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Chu DKW, Pan Y, Cheng SMS, et al. Molecular diagnosis of a novel coronavirus (2019-nCoV) causing an outbreak of pneumonia. Clin Chem. 2020;66:549–555. doi:10.1093/clinchem/hvaa029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi:10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Christakis DA, Van Cleve W, Zimmerman FJ. Estimation of US children’s educational attainment and years of life lost associated with primary school closures during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3:e2028786. doi:10.1001/jamanetworkopen.2020.28786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Masonbrink AR, Hurley E. Advocating for children during the COVID-19 school closures. Pediatrics. 2020;146:e20201440. doi:10.1542/peds.2020-1440 [DOI] [PubMed] [Google Scholar]
- 5. Nearchou F, Flinn C, Niland R, Subramaniam SS, Hennessy E. Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: a systematic review. Int J Environ Res Public Health. 2020;17:8479. doi:10.3390/ijerph17228479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dost S, Hossain A, Shehab M, Abdelwahed A, Al-Nusair L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: a national cross-sectional survey of 2721 UK medical students. BMJ Open. 2020;10:e042378. doi:10.1136/bmjopen-2020-042378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ferrel MN, Ryan JJ. The impact of COVID-19 on medical education. Cureus. 2020;12:e7492. doi:10.7759/cureus.7492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gaur U, Majumder MAA, Sa B, Sarkar S, Williams A, Singh K. Challenges and opportunities of preclinical medical education: COVID-19 crisis and beyond. SN Compr Clin Med. 2020;2:1992–1997. doi:10.1007/s42399-020-00528-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Loda T, Loffler T, Erschens R, Zipfel S, Herrmann-Werner A. Medical education in times of COVID-19: German students’ expectations—A cross-sectional study. PLoS One. 2020;15:e0241660. doi:10.1371/journal.pone.0241660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tabatabai S. COVID-19 impact and virtual medical education. J Adv Med Educ Prof. 2020;8:140–143. doi:10.30476/jamp.2020.86070.1213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tariq EF, Sah PK, Malik A. The plight of COVID-19 pandemic on medical students and residency applicants. Ann Med Surg (Lond). 2020;60:1–4. doi:10.1016/j.amsu.2020.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Teele SA, Sindelar A, Brown D, et al. Online education in a hurry: delivering pediatric graduate medical education during COVID-19. Prog Pediatr Cardiol. 2020;60:101320. doi:10.1016/j.ppedcard.2020.101320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wijesooriya NR, Mishra V, Brand PLP, Rubin BK. COVID-19 and telehealth, education, and research adaptations. Paediatr Respir Rev. 2020;35:38–42. doi:10.1016/j.prrv.2020.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yusoff MSB, Hadie SNH, Mohamad I, et al. Sustainable medical teaching and learning during the COVID-19 pandemic: surviving the new normal. Malays J Med Sci. 2020;27:137–142. doi:10.21315/mjms2020.27.3.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bayham J, Fenichel EP. Impact of school closures for COVID-19 on the US health-care workforce and net mortality: a modelling study. Lancet Public Health. 2020;5:e271–e278. doi:10.1016/S2468-2667(20)30082-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Droit-Volet S, Gil S, Martinelli N, et al. Time and Covid-19 stress in the lockdown situation: Time free, <<Dying>> of boredom and sadness. PLoS One. 2020;15:e0236465. doi:10.1371/journal.pone.0236465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Eilersen A, Sneppen K. Cost-benefit of limited isolation and testing in COVID-19 mitigation. Sci Rep. 2020;10:18543. doi:10.1038/s41598-020-75640-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Jaspal R, Breakwell GM. Socio-economic inequalities in social network, loneliness and mental health during the COVID-19 pandemic [Published online December 7, 2020]. Int J Soc Psychiatry. 2020. doi:10.1177/0020764020976694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pietrabissa G, Simpson SG. Psychological consequences of social isolation during COVID-19 outbreak. Front Psychol. 2020;11:2201. doi:10.3389/fpsyg.2020.02201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Neary S, Van Rhee J, Roman C. The effect of the coronavirus pandemic on physician assistant educators. J Physician Assist Educ. 2020;31:121–125. doi:10.1097/JPA.0000000000000312 [DOI] [PubMed] [Google Scholar]
- 21. Rajab MH, Gazal AM, Alkattan K. Challenges to online medical education during the COVID-19 pandemic. Cureus. 2020;12:e8966. doi:10.7759/cureus.8966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zuo L, Miller Juve A. Transitioning to a new era: future directions for staff development during COVID-19. Med Educ. 2021;55:104–107. doi:10.1111/medu.14387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Brauer DG, Ferguson KJ. The integrated curriculum in medical education: AMEE Guide No. 96. Med Teach. 2015;37:312–322. doi:10.3109/0142159X.2014.970998 [DOI] [PubMed] [Google Scholar]
- 24. Buja LM. Medical education today: all that glitters is not gold. BMC Med Educ. 2019;19:110. doi:10.1186/s12909-019-1535-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Villatoro T, Lackritz K, Chan JSY. Case-based asynchronous interactive modules in undergraduate medical education. Acad Pathol. 2019;6. doi:10.1177/2374289519884715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. MD Program. University of Iowa Health Care Carver College of Medicine. Published 2021. Updated January 1, 2021. Accessed March 15, 2021. https://medicine.uiowa.edu/md/curriculum/about-curriculum
- 27. Ferguson K, Cooper C, Asprey D, Densen P. University of Iowa Carver College of Medicine. Acad Med. 2010;85: S228–232. doi:10.1097/ACM.0b013e3181e8dcb8 [DOI] [PubMed] [Google Scholar]
- 28. Department of Physician Assistant Studies. University of Iowa Health Care Carver College of Medicine. Published 2021. Updated January 1, 2021. Accessed March 15, 2021. https://medicine.uiowa.edu/md/curriculum/about-curriculum
- 29. Ferguson KJ, Kreiter CD, Franklin E, Haugen TH, Dee FR. Investigating the validity of web-enabled mechanistic case diagramming scores to assess students’ integration of foundational and clinical sciences. Adv Health Sci Educ Theory Pract. 2020;25:629–639. doi:10.1007/s10459-019-09944-y [DOI] [PubMed] [Google Scholar]
- 30. Densen P. Challenges and opportunities facing medical education. Trans Am Clin Climatol Assoc. 2011;122:48–58. [PMC free article] [PubMed] [Google Scholar]
- 31. Dee FR, Haugen TH, Kreiter CD. New web-based applications for mechanistic case diagramming. Med Educ Online. 2014;19:24708. doi:10.3402/meo.v19.24708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ferguson KJ, Kreiter CD, Haugen TH, Dee FR. Web-enabled mechanistic case diagramming: a novel tool for assessing students’ ability to integrate foundational and clinical sciences. Acad Med. 2018;93:1146–1149. doi:10.1097/ACM.0000000000002184 [DOI] [PubMed] [Google Scholar]
- 33. Kreiter CD, Haugen T, Leaven T, et al. A report on the piloting of a novel computer-based medical case simulation for teaching and formative assessment of diagnostic laboratory testing. Med Educ Online. 2011;16:5646. doi:10.3402/meo.v16i0.5646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zoom Security Guide. Zoom Video Communications, Inc. San Jose, CA. Published 2016. Updated July 1, 2016. Accessed March 15, 2021. https://d24cgw3uvb9a9h.cloudfront.net/static/81625/doc/Zoom-Security-White-Paper.pdf
- 35. Knollmann-Ritschel BEC, Regula DP, Borowitz MJ, Conran R, Prystowsky MB. Pathology competencies for medical education and educational cases. Acad Pathol. 2017;4. doi:10.1177/2374289517715040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Knollmann-Ritschel BEC, Suarez E, Gilliland W, Conran R, Pock A. Pathology course director perspectives of a recent LCME experience: preparation in an integrated curriculum with the revised standards. Acad Pathol. 2017;4. doi:10.1177/2374289516687070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sadofsky M, Knollmann-Ritschel B, Conran RM, Prystowsky MB. National standards in pathology education: developing competencies for integrated medical school curricula. Arch Pathol Lab Med. 2014;138:328–332. doi:10.5858/arpa.2013-0404-RA [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-apc-10.1177_23742895211015337 for Teaching Pathology in an Integrated Preclinical Medical School Curriculum and Adaptations to COVID-19 Restrictions by Matthew D. Krasowski, John L. Blau, Stephanie J. Chen, Karra A. Jones, Thomas J. Schmidt and Leslie A. Bruch in Academic Pathology
Supplemental Material, sj-pdf-2-apc-10.1177_23742895211015337 for Teaching Pathology in an Integrated Preclinical Medical School Curriculum and Adaptations to COVID-19 Restrictions by Matthew D. Krasowski, John L. Blau, Stephanie J. Chen, Karra A. Jones, Thomas J. Schmidt and Leslie A. Bruch in Academic Pathology


