Abstract
Context:
Silicosis is a progressive, irreversible and incurable respiratory morbidity and often becomes a cause for pre-mature mortality among occupationally silica dust-exposed workers in India and similar countries. It has a dual problem of associated silico-tuberculosis as a co-morbidity. The present study was done to assess the respiratory morbidity caused by silicosis in sandstone mine of Rajasthan, India.
Methods:
The chest X-rays of 529 subjects having history of employment in stone mines with respiratory morbidity were subjected for this study and evaluated in accordance with ILO Classification 2000. The X-rays were classified into various categories of silicosis and progressive massive fibrosis (PMF) in relation to years of work in stone mines.
Results:
Out of 529 chest radiographs evaluated, 275 (52%) showed radiological evidence of silicosis. Of them, 40 (7.5%) subjects showed large opacities suggestive of progressive massive fibrosis. Both silicosis and progressive massive fibrosis were associated with increasing duration of work in stone mines. Sixty-one (12.4%) subjects with silicosis also had associated pulmonary tuberculosis, termed as silico-tuberculosis.
Conclusion:
The present study showed a high prevalence of silicosis, progressive massive fibrosis and silico-tuberculosis among stone mine workers. It appears that that unless silicosis is controlled, elimination of tuberculosis is far from reality in the country. Hence, states and central authorities must work together towards control of both silicosis as well as silico-tuberculosis. Similarly, there is an urgent need of initiation of national silicosis control programme, similar to existing national tuberculosis control programme, considering the huge burden of silicosis in India
Keywords: Progressive massive fibrosis, silicosis, silico-tuberculosis, stone mine workers
Introduction
Stone mining is carried out in India since ancient times. Stones like sandstone, marble, granite, etc., are used for building houses, carving idols, etc., while masonry stone is used in building roads, bridges, canals etc., Majority of these stone mines are located either in rural areas or outskirt areas adjacent to the cities in order to meet the growing demand of infrastructure sector.[1] A large number of persons are employed in these unorganized small scale stone mines and are exposed to fine dust containing free silica in the range of 70–90% depending on the nature of stone.[2] Most stone mines are seasonal and operated by small entrepreneurs with daily employment ranging from 5 to 20 workers though there are some mines employing more than 100 persons. The working conditions in stone mines are far from satisfactory and rarely comply with health and safety standards. The exposure to silica dust for long duration causes silicosis[3] and is also known to predispose to pulmonary tuberculosis, chronic airflow limitation, lung cancer, renal diseases, etc.[4,5,6,7,8] Many studies have been conducted in past to determine the prevalence of silicosis among stone mine workers. These studies have documented that prevalence of silicosis among these stone quarry workers range from 12% to 50%.[9,10,11,12,13] Silica is cytotoxic to macrophage which is primary defence mechanism to tubercular bacilli and hence exposure to silica dust increases risk for TB.[14] Silica exposed persons are at 2.8 to 39 times greater risk of pulmonary TB in comparison to healthy subjects. Susceptibility of silica exposed persons to TB has been demonstrated in multiple studies.[15,16,17,18,19]
Karauli and Dholpur area of Rajasthan are famous for sandstone that are used for construction, carving and other decorative material. About 15 to 20% of populations in the area are dependent on these small unorganised stone mines for their livelihood. The working in mines is wholly manual with no mechanisation. After removal of overburden of few feet, the stone slabs are manually cut in blocks of stone by making holes with chisels and hammers [Figure 1]. The block of stone so separated is then split into slabs of various thicknesses along natural layers. The split stone layers (patti) are sold as such or cut in small square slabs depending on nature of stone and requirement. Stone slabs are primarily used for making roof and floors. There is a general lack of education and awareness about occupational diseases among the workers, employers and even local medical practitioners. It is not uncommon that most cases of respiratory diseases are treated with anti-tubercular drugs, often without much response as silicosis with/without pulmonary tuberculosis is rampant in the area. Hence, a study was planned to assess the problem of silicosis and it's co-morbidity, silico-tuberculosis in the said stone mine workers.
Figure 1.

Photograph of manual stone cutting in mine
Materials and Method
A local NGO working for the welfare of sandstone mine workers observed that there was high prevalence of pulmonary tuberculosis not responding to anti-TB treatment among workers of Karauli and Dholpur districts, Rajasthan. These workers were exposed to high levels of air borne silica and hence the NGO suspected that the disease could be due to silicosis. Hence, they conducted medical examination of 572 persons with the verbal consent of the participants. Medical examination included detailed history of demography, working in mines, respiratory symptoms, history of treatment for tuberculosis and chest radiographs. For further analysis of the data the NGO collaborated with National Institute of Miners' Health (NIMH), Nagpur. The study was conducted in accordance with the guidelines of Institutional Ethics Committee of NIMH. Out of 572, chest radiograph of 43 persons were of poor quality and were excluded from further analysis. Chest X-rays of remaining 88 persons were considered for evaluation. Analysis of records was carried and chest radiographs were evaluated by doctors proficient in detection of silicosis in accordance with ILO Classification of Radiographs for Pneumoconiosis, 2000.[20]
Based on profusion of small opacities of type p, q or r in chest radiographs, the subjects were classified as Normal when the profusion was 0/-, 0/0 or 0/1; Suspected Silicosis if profusion was 1/0 and confirmed Silicosis if profusion was 1/1 or more. They were further classified as category 1 if profusion was 1/0, 1/1 or 1/2; category 2 if profusion 2/1, 2/2 or 2/3 and category 3 if profusion was 3/2, 3/3 or 3/+. Similarly, progressive massive fibrosis (PMF) was suspected if large opacity of type A, B or C were present. If pulmonary tuberculosis was suspected in presence of small opacities suggestive of silicosis, the subjects were classified as silico-tuberculosis.
Results
The distribution of age-group and duration of work of subjects is given in Figures 2 and 3, respectively. Most workers belonged to the age group of 41-50 year., followed by 31-40 year.', followed by 51-60 year. Similarly, most workers had a working duration of 11–20 years, followed by 21–30 years, followed by >30 years. Out of 529 persons, 453 (85.6%) persons had completed DOTS (Directly Observed Treatment, Short Course) therapy considering the fact that they were suffering from pulmonary tuberculosis. Evaluation of chest X-ray showed presence of small-rounded opacities of 'q' or 'r' type suggestive of silicosis amongst 275 out of 529 persons and are detailed in Table 1. Overall prevalence of silicosis was 52% (275/529) and that of PMF is 7.5% (40/529) [Table 2]. Figure 4 shows photograph of chest radiograph of a subject with category-3 silicosis. The chest radiographs of 40 persons showed large opacities suggestive of PMF. Further analysis of result as in Table 2, showed that occurrence of pneumoconiotic opacities due to silicosis and progressive massive fibrosis were directly related to working duration in stone mine and both were statistically significant as evident by Chi square for linear trends (for silicosis: Chi square = 42.83 & P value = <0.001 and for PMF: Chi square = 12.82 & P value = <0.001). It also showed that profusion category of silicosis and type of large opacity were also related to duration of work in stone mines. Further, 66 (12.4%) subjects with silicosis were associated pulmonary tuberculosis as a co-morbidity, also known as silico-tuberculosis. Chest radiographs of 50 (9.4%) persons had radiological evidence of pulmonary tuberculosis.
Figure 2.
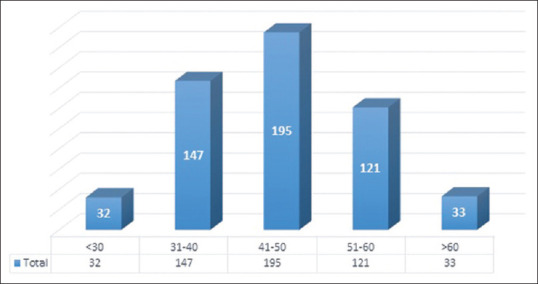
The age wise distribution of persons (N = 529)
Figure 3.
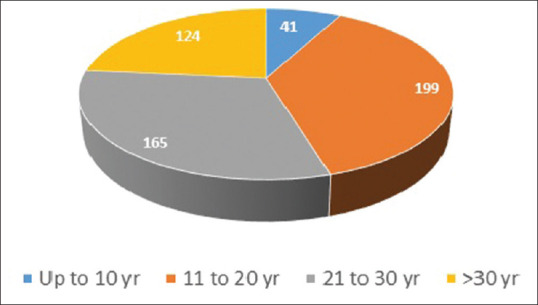
Distribution of person according to working duration in stone mines (N = 529)
Table 1.
Category wise distribution of case with small opacities
| Category | Subcategory | Number of cases | Total |
|---|---|---|---|
| Category- 0 | 0/-, 0/0, 0/1 | 254 | 254 |
| Category- 1 | 1/0 | 36 | 111 |
| 1/1 | 59 | ||
| 1/2 | 16 | ||
| Category- 2 | 2/1 | 19 | 94 |
| 2/2 | 57 | ||
| 2/3 | 18 | ||
| Category- 3 | 3/2 | 17 | 70 |
| 3/3 | 39 | ||
| 3/+ | 14 |
Table 2.
Distribution silicosis and progressive massive fibrosis & work duration (n=529)
| Work duration (yr.) | Silicosis | Linear Trend | Progressive Massive Fibrosis | Linear Trend | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cat-1 | Cat-2 | Cat-3 | Sub. wth X-ray changes | A | B | C | Sub.wth X-ray changes | Total persons examined | |||
| =<10 | 2 | 4 | 1 | 7 (17%) |
χ2=42.83 Df=1 P=<0.001 Significant |
0 | 1 | 0 | 1 (2.4%) | 41 |
χ2=12.82 df=1 P=<0.001 Significant |
| 11-20 | 40 | 24 | 19 | 83 (41.7%) | 0 | 2 | 5 | 7 (3.6%) | 199 | ||
| 21-30 | 43 | 36 | 22 | 101 (61.2%) | 2 | 11 | 2 | 15 (9%) | 165 | ||
| >30 | 26 | 30 | 28 | 84 (67.7%) | 4 | 9 | 4 | 17 (13.7%) | 124 | ||
| Total | 111 | 94 | 70 | 275 (52%) | 6 | 23 | 11 | 40 (7.5%) | 529 | ||
Figure 4.
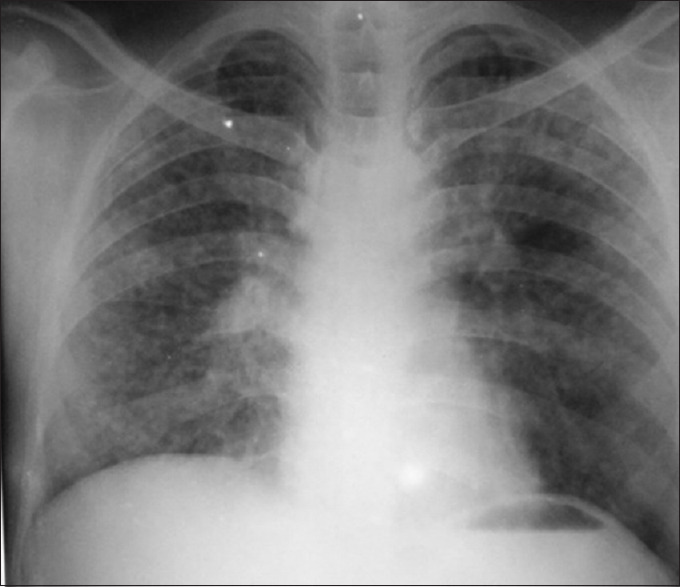
Photograph of Category 3 Silicosis
Discussion
The result showed out of 529 persons with history of working in mines, a total of 275 (52%) had an evidence of silicosis and 40 (7.5%) of them had developed Progressive Massive Fibrosis (PMF). One hundred and sixty-four (31%) persons had silicosis of category 2 or higher indicating advanced stage of the disease. Majority case of PMF showed large opacities of type B or C also indicating of advance stage of the disease. The study showed that silicosis developed even with working duration of 10 year or lesser in stone mines, as shown in Table 2. The study also showed that the prevalence of silicosis increases with increasing duration of work in mines, which is statistically significant. This means working duration is an important risk factor for developing silicosis and possibly due to longer duration exposure of silica dusts causing more damage to lungs. Similarly, the category of silicosis and occurrence of PMF also dependent on duration of work. Seventy-eight percent of subjects with more than 10 years of exposure had profusion of category 2/1 or more. It is known that silicosis tends to predispose to pulmonary tuberculosis due to declined lung immunity and may be a contributing factor towards high prevalence of disease. It was observed that a total of 50 (9.4%) study participants had radiological evidence of pulmonary tuberculosis but was misdiagnosed as silicosis. On the other hand, a total of 66 (12.4%) silicotic study participants had associated pulmonary tuberculosis (silico-tuberculosis). Various other studies conducted among mine workers from time to time, depicted a prevalence of tuberculosis that ranged from 10.7% to 32%.[15,16,17,18] Calvert et al. reported that the prevalence of TB has direct relationship with the concentration of free silica dust in the work environment and risk of TB increased with increased duration of exposure to silica. This is probably due to continuous destruction of lung macrophages caused by free silica particles as mentioned above. Additionally, the study observed that workers developed TB on an average 7 years after discontinuation of silica exposure. This indicates that these workers are at higher risk of TB even after discontinuation of exposure.[19]
The present study confirms that occurrence of advanced stage of silicosis and progressive massive fibrosis is high and related to duration of work apart from silica content of the circulating dusts of work environment, which was not investigated in this study (beyond the scope of this study). Longer the duration of work, higher was the prevalence and advancement of silicosis and PMF. It is possible that some of the subjects who developed silicosis and PMF at early age might have started working in mines at a much younger age. However, the results of this study should not be considered as the community prevalence of silicosis and PMF among stone mine workers as the study population included only those subjects who had been suffering with some respiratory disorders and were symptomatic. This may be considered as the tip of the iceberg and actual community burden of silicosis and PMF might be many folds higher than this present study finding as many of them were in asymptomatic or early symptomatic phase and didn't participate in this study. A well designed community-based study with required sample size & valid selection criteria is required to assess the community burden of silicosis which would detect both symptomatic as well as asymptomatic silicotic cases of both occupational as well as non/para-occupational origin.
Relevance to the practice of primary care physicians
Many studies have documented high prevalence of silicosis among workers exposed to silica.[21,22,23,24,25,26,27] Although silicosis is an irreversible, progressive, incurable disease but it is preventable if intervention is done on time. Hence attempts must be made towards primary and secondary prevention. Stone mines are mostly located in rural or semi-urban areas, often belonging to unorganized sector. Hence, the stone mining industry workers are not covered under any medical scheme like ESIC (Employees State Insurance Corporation, Ministry of Labour & Employment, Govt. of India) or similar facilities offered by state government. Consequently, the workers may approach nearby primary health care physicians for having their healthcare facilities provided it is acceptable to both care givers as well as takers. There is a general lack of awareness about occupational diseases including silicosis among these practicing physicians and silicosis opacities are usually misdiagnosed as pulmonary tuberculosis due to lack of training in detection of silicosis. It is commonly observed that most cases of respiratory disease are treated with anti-tubercular drugs without much response.
Hence, the findings of this paper indicates about need for training of local medical practitioners in understanding of ILO radiography for detection of silicosis. Alternatively, early detection of silicosis can be done at primary health care facilities through annual screening of silica dust exposed workers using a cost-effective bio-marker such as serum CC16. ICMR-National Institute of Occupational Health, Ahmedabad, has already identified such bio-marker – serum club cell protein 16 (CC-16).[28] In this regard, the country requires a suitable legislation to enable all vulnerable workers, particularly those of unorganized workers, for undergoing annual screening for silicosis using novel bio-marker such as serum CC-16 through nearby primary health centers or similar other health establishments. Based on CC-16 cut off value (8 ng/ml), once silicosis is suspected, confirmation might be done by chest x-ray as per ILO radiography. The existing health care delivery system must be prepared adequately towards this. This includes provision of necessary training to the health care workers and necessary logistic supports to be made available in all peripheral health establishments to improve the national occupational health scenario focusing control of silicosis and silico-tuberculosis. It may also be noted that control of silicosis is a crucial and essential step for elimination of TB from the country by 2025 as there is a huge burden of silicosis and silico-tuberculosis, which is not attended adequately so far.
There is an urgent need of formulation of National Silicosis Control Programme that must include following key points involving primary health care services of the country.
Early detection of silicosis by annual screening using serum CC16 biomarker for all silica dust exposed workers of both organised as well as unorganised sector. Similarly, adequate dust control measures and personal protective devices must be implemented in all such industries including household industries
Suitable legislation must be made by the relevant authority for immediate implementation of it
Primary health care physicians/nurses must be trained for assessment of serum CC16 status annually. A suitable training program must be organised to train relevant health personnel of the country. All logistics and other support services must be made available at all primary health centres
Considering huge number of migrant workers, individual serum CC 16 values must be linked with unique identifier such as Adhar no. along with other relevant information to follow up the progress of the disease in relation to time
Whenever serum CC16 value will become around 8 ng/ml, early silicosis may be suspected that needs to be confirmed by chest X-ray for confirmation
Once confirmed, further exposure must be protected by suitable mechanisms including replacement/rehabilitation of job in a non-exposure situation
Since smoking reduces values by 1 to 2 ng/ml (moderate to heavy smokers) compared to non-smokers, smoking must be stopped for at least for 2 months before undergoing for serum CC16. Alternatively, the value may be adjusted accordingly
ICMR-NIOH in collaboration with ICMR-NIV has already developed an indigenous affordable kits for early detection of silicosis. This may be used effectively under national silicosis control initiation
Ministries of Labor, Health, Mines, and Industry etc., must work together considering the fact that silicosis is an interlinked problem and every department's coordinated role is important to mitigate this problem
India is committed to eliminating TB by 2025. But unless silicosis is controlled, eliminating TB will remain a dream. Hence, relevant authorities must understand the complex issues between silicosis and TB and act accordingly
Lastly, post graduate medical curriculum must be developed towards control of common occupational diseases as it is directly linked with country's economy/productivity and existing health care system is totally ignorant about it. India badly needs large number of occupational health experts to improve country's existing situation.
Conclusion
The present study showed that occurrence of silicosis and progressive massive fibrosis was high among stone workers. There is also high prevalence of pulmonary tuberculosis and silico-tuberculosis too. Considering above there is an urgent need of national silicosis control programme.
Ethical approval
The study was conducted in accordance with the guidelines of Institutional Ethics Committee of NIMH.
Informed consent
Informed oral consent was obtained by NGO 'Dang Vikas Sansthan', who provided the medical documents to NIMH.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors gratefully acknowledge the contribution of Dr. P K Sishodiya, Ex-Director of National Institute of Miners' Health and all participating members of 'Dang Vikas Sansthan', a local NGO, for providing necessary logistical assistance. Authors are thankful to National Institute of Miners' Health, Govt. of India, to support for conducting this study. The authors also whole heartedly thank all the study participants for participating in this study.
References
- 1.Indian Bureau of Mines. Indian Minerals Yearbook 2017. 56th ed. Nagpur: IBM; 2017. Available from: http://ibm.gov.in/writereaddata/files/12102018131542Slate_%20S_st%20and%20Other%20Dimension%202017.pdf . Cited 2019 Jun 22. [Google Scholar]
- 2.World Health Organization. Silicosis. 2000. Internet. Available from: http://web.archive.org/web/20070510005843/http://www.who.int/mediacentre/factsheets/fs238/en/ Cited 2019 Jun 17.
- 3.Greenberg MI, Waksman J, Curtis J. Silicosis A review. Dis Mon. 2007;53:394–416. doi: 10.1016/j.disamonth.2007.09.020. [DOI] [PubMed] [Google Scholar]
- 4.Donoghue AM. Occupational health hazards in mining: An overview. Occup Med. 2004;54:283–9. doi: 10.1093/occmed/kqh072. [DOI] [PubMed] [Google Scholar]
- 5.Erren TC, Glende CB, Morfeld P, Piekarski C. Is exposure to silica associated with lung cancer in the absence of silicosis? A meta-analytical approach to an important public health question. Int Arch Occup Environ Health. 2009;82:997–1004. doi: 10.1007/s00420-008-0387-0. [DOI] [PubMed] [Google Scholar]
- 6.Esswein EJ, Breitenstein M, Snawder J, Kiefer M, Sieber WK. Occupational exposures to respirable crystalline silica during hydraulic fracturing. J Occup Environ Hyg. 2013;10:347–56. doi: 10.1080/15459624.2013.788352. [DOI] [PubMed] [Google Scholar]
- 7.Greaves IA. Not-so simple silicosis: A case for public health action. Am J Ind Med. 2000;37:245–51. doi: 10.1002/(sici)1097-0274(200003)37:3<245::aid-ajim1>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 8.Mohner M, Pohrt A, Gellissen J. Occupational exposure to respirable crystalline silica and chronic non-malignant renal disease: Systematic review and meta-analysis. Int Arch Occup Environ Health. 2017;90:555–74. doi: 10.1007/s00420-017-1219-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dhatrak S, Nandi S. Assessment of silica dust exposure profile in relation to prevalence of silicosis among Indian sandstone mine workers: Need for review of standards. Am J Ind Med. 2020;63:277–81. doi: 10.1002/ajim.23077. [DOI] [PubMed] [Google Scholar]
- 10.Malik D. Silicosis – A dusty tale in Rajasthan. 2005 [Internet] Available from: http://www.indiatogether.org/2005/aug/env-lungdust.htm . Cited 2019 Jul 05.
- 11.Mathur ML. Silicosis among sand stone quarry workers of a desert district Jodhpur. Ann Nat Acad Med Sci. 1996;32:113–8. [Google Scholar]
- 12.Kashyap SK. Occupational pneumoconiosis and tuberculosis. Ind J Tub. 1994;41:73–5. [Google Scholar]
- 13.Centre for Occupational and Environmental Health, Maulana Azad Medical College, Delhi. Short Report of Health Survey of Lal kuan Victims [Internet] Available from: www.okinternational.org/docs/LKscan2.pdf . Cited 2019 Jun 12.
- 14.Kasper DL, Longo DL, Fauci AS, Hauser SL, Jameson J, Loscalzo J, editors. Harrison's Principles of Internal Medicine. 19th ed. New York: McGraw-Hill; 2016. [Google Scholar]
- 15.Corbett EL, Churchyard GJ, Clayton TC, Williams BG, Mulder D, Hayes RJ, et al. HIV infection and silicosis: The impact of two potent risk factors on the incidence of mycobacterial disease in South African miners. AIDS. 2000;14:2759–68. doi: 10.1097/00002030-200012010-00016. [DOI] [PubMed] [Google Scholar]
- 16.Health Effects of Occupational Exposure to Respirable Crystalline Silica, No. 2002. Washington DC: National Institute of Occupational Safety and Health (NIOSH); 2002. [Google Scholar]
- 17.Hnizdo E, Murray J. Risk of pulmonary tuberculosis relative to silicosis and exposure to silica dust in South African gold miners. Occup Environ Med. 1998;55:496–502. doi: 10.1136/oem.55.7.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Waternaudete JM, Ehrlich RI, Churchyard GJ, Pemba L, Dekker K, Vermeis M, et al. Tuberculosis and silica exposure in South African gold miners. Occup Environ Med. 2006;63:187–92. doi: 10.1136/oem.2004.018614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Calvert GM, Rice FL, Boiano JM, Sheehy JW, Sanderson WT. Occupational silica exposure and risk of various diseases: An analysis using death certificates from 27 states of the United States. Occup Environ Med. 2003;60:122–9. doi: 10.1136/oem.60.2.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guidelines for the use of ILO International Classification of Radiographs of Pneumoconiosis- Revised Edition 2000, Occupational Safety and Health Series No. 22. ILO. Geneva: International Labour Organization (ILO); 2003. [Google Scholar]
- 21.Sharma N, Kundu D, Dhaked S, Das A. Silicosis and silicotuberculosis in India. Bull World Health Organ. 2016;94:777–8. doi: 10.2471/BLT.15.163550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Siribaddana A, Wickramasekara K, Senevirathna K, Upul A, Pieris M. Prevalence of silicosis among employees of a Silica factory in Sri-Lanka. Eur Respir J. 2013;42:999. [Google Scholar]
- 23.Shtraichman O, Kramer MR. Artificial stone silicosis: The Israel epidemic, current view. Harefuah. 2017;156:517–21. [PubMed] [Google Scholar]
- 24.Reilly MJ, Timmer SJ, Rosenman KD. The burden of silicosis in Michigan: 1988–2016. Ann Am Thorac Soc. 2018;15:1404–10. doi: 10.1513/AnnalsATS.201802-117OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sen S, Mitra R, Mukherjee S, Das PK, Moitra S. Silicosis in current scenario: A review of literature. Curr Respir Med Rev. 2016;12:56–64. [Google Scholar]
- 26.Rose C, Heinzerling A, Patel K, Sack C, Wolff J, Zell-Baran L, et al. Severe silicosis in engineered stone fabrication workers-California, Colorado, Texas, and Washington, 2017-2019. MMWR Morb Mortal Wkly Rep. 2019;68:813–8. doi: 10.15585/mmwr.mm6838a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Koller MF, Scholz SM, Pletscher C, Miedinger D. Silicosis in Switzerland. Int J Occup Med Environ Health. 2018;31:659–76. doi: 10.13075/ijomeh.1896.01272. [DOI] [PubMed] [Google Scholar]
- 28.Naha N, Muhamed JCJ, Pagdhune A, Sarkar B, Sarkar K. Club cell protein 16 as a biomarker for early detection of silicosis. Indian J Med Res. 2020;151:319–25. doi: 10.4103/ijmr.IJMR_1799_18. [DOI] [PMC free article] [PubMed] [Google Scholar]


