Abstract
Lumbar disc herniation (LDH) is a common cause of low back pain (LBP) and/or radicular pain (RP). Over the years, different therapies have been proposed to treat symptomatic LDH, including different minimally invasive techniques and open surgical methods. Recently, percutaneous intradiscal injection of radiopaque gelified ethanol (RGE) DiscoGel® has emerged as an effective therapeutic option in patients with LDH. Nevertheless, only few studies addressed the reliability of this technique. The purpose of this study was to evaluate the efficacy and safety of this procedure. We analysed surgical and outcome data of patients with small or medium LDH treated by DiscoGel between 2012 to 2015. Outcome variables included pain relief, the limitation on physical activity and severity of depression status. Overall, complication rate was defined as the occurrence of any perioperative adverse events. A total of 94 consecutive patients were enrolled in the study. Pain relief was achieved in 90.6% and 88.8% of patients at 1- and 4-year follow-up, respectively. At the last follow-up, at least a satisfactory result was achieved in 92.5% of patients. Similar results were obtained in the limitation on physical activity. Depression status did not significantly change after treatment. There was no mortality, and no patients experienced permanent sequelae. In well-selected patients, DiscoGel has proved effective in maintaining excellent functional results in terms of pain relief and limitation on physical activity while minimizing the overall rate of complications related to these kinds of surgical procedures.
Keywords: Low back pain, lumbar disc herniation, radicular pain, minimally invasive surgery, radiopaque gelified ethanol, DiscoGel® chemonucleolysis
Introduction
Low back pain (LBP) is a common disorder with significant impact on public health.1–3 Lumbar disc herniation (LDH) is a very frequent cause of LBP and is often associated with radicular pains (RPs), due to mechanical compression on the nerve roots together with immunologic and inflammatory changes.4,5
Although, over the years, several treatments have been proposed, including different minimally invasive and percutaneous techniques; among these, microdiscectomy (MD) still remains the gold standard of treatment in symptomatic LBP, when conservative treatment has failed.6–8 Indeed, this surgical procedure allows interrupting the pathophysiological mechanism underlying the pain with rapid relief of symptoms and often with long-lasting clinical benefits.6,8 In the literature, there are several series reporting data on the short-term success rate and long-term outcome of MD.7,9–11 However, despite the improvement in functional short- and long-term outcome, the procedure is still burdened by a series of morbidities, including new or worsening neurological deficit (1–3%), nerve root injury (2.6%), durotomy (3.9%), wound complications (2.1%), wound hematoma (0.5%) and development of the syndrome of failure of lumbar surgery (7–15%).12 Moreover, MD carries the risks of a general anaesthesia, which involves high cost, and re-operation rates ranging between 4–10%.3,12
For these reasons, over the past two decades, several minimally invasive percutaneous techniques have been proposed as alternative treatments to MD. Among these, percutaneous intradiscal injection of radiopaque gelified ethanol (RGE) DiscoGel® has emerged as an effective alternative to MD in selected patients.3,13 DiscoGel acts by dehydrating the nucleus pulposus in the disc with consequent reduction of intradiscal pressure and mechanical compression on the nerve roots. Nevertheless, only few studies reported the efficacy of this procedure in the management of LBP and RP related to LDH. In this study, we evaluated the safety and the efficacy of DiscoGel on pain score and disability in well-selected patient with symptomatic LDH.
Materials and methods
Study design and setting
In this study, we analysed clinical, surgical and outcome data from consecutive patients presenting with symptomatic LDH, operated on from January 2012 to December 2015, by mean of percutaneous intradiscal injection of RGE. All patients, included in this study, signed an informed consent for the scientific use of their data according to the requirements of the local Institutional Review Board.
Participants and study size
A total of 94 consecutive patients were included in the study. After preliminary physical evaluation by an expert neurosurgeon, all patients underwent preoperative neuroradiological examinations, including lumbar X-ray, magnetic resonance imaging (MRI), computed tomography (CT) scan or both. The eligibility criteria were age ⩾ 18 years and patients suffering from LBP and/or RP lasting at least 2 months due to a small or medium size LDH, non-responder to adequate conservative treatments. The exclusion criteria were presence of free disc fragments documented on MRI, significant lumbar and/or intervertebral foramen, degenerative stenosis, multiple LDH, pregnancy, referred allergy to proposed drugs, indication to open MD, sacroiliitis or previous spine surgery.
Variables
We collected demographic and clinical data, including age, sex, fasting glycaemia, duration of symptoms, depression status, smoking, pain intensity and distribution, limitation on physical activity and health-related quality of life (HRQoL) and lumbar level symptoms. Preoperatively, LDH was categorized as small and medium size, respectively, grade 1 A-B and 2 A-B according to Michigan State University (MSU) classification.14
Data sources
Clinical, radiological, treatment and follow-up data were obtained by outpatient clinical evaluation at defined time intervals and collected in a dedicated digital archive. An initial clinical evaluation was obtained at the time of discharge, and patients were then reviewed in our outpatient clinic at 1, 6, 12, 48, and 60 months after surgery.
DiscoGel
‘DiscoGel’ is a sterile viscous solution composed of ethyl alcohol, ethyl cellulose added to tungsten (RGE). The 96% pure ethyl alcohol produces a local necrosis and dehydration of nucleous pulposus, resulting in a reduction of the disc herniation volume. The ethyl cellulose increases the viscosity of the solution, limiting its diffusion into the disc. The tungsten makes the product radiopaque, and the amount of gel injected can be monitored using fluoroscopy. In addition, its hydrophilic properties determine a migration of fluids from the periphery of the disc and a simultaneous precipitation of part of the gel which realizes a sort of ‘soft intradiscal prosthesis’.
Surgical procedure
Procedures were performed in the angiographic room with biplane digital fluoroscopy under local anaesthesia in day surgery and in aseptic conditions. Patients were placed in lateral decubitus on the symptomatic side to allow injection on the opposite side to the structural damage of the herniated disc. We used a coaxial technique approaching the outer border of the disc percutaneously, especially at L5–S1 level, with an 18G × 152 mm needle and thereafter inserting a 22G × 200 mm needle in the centre of nucleus pulposus parallel and at midway between the two end plates. The dose of DiscoGel that is slowly injected at room temperature through the 22G needle in the nucleus pulposus was 0.8–1.6 mL: its radio-opacity facilitates confirmation of the spread of the material within the disc and helps to avoid epidural leakages. No antibiotics were injected intradiscally. In absence of complications, patients were discharged on the day after the procedure on anti-inflammatory drugs for 1 week.
Assessment of outcome and quantitative variables
Using data obtained from a dedicated digital archive, we analysed functional, clinical, radiological, treatment and follow-up data of the 94 patients included in the study. The variables considered to verify the efficacy of the proposed surgical procedure on functional outcome in patients with LDH included pain relief, quality of life, comprised the limitation on physical activity, and severity of depression status. We evaluated pain intensity according to the visual analogue scale (VAS), and limitation on physical activity and HRQoL was assessed using the medical outcome study 36-items short form health survey (SF-36). Data from SF-36 were scored by 0–100 algorithms. To avoid inconsistent interpretation, we categorized functional outcome as excellent (when pain was totally disappeared with full recovery of physical activity); good (when improvement on the VAS score > 70% and no limitation on physical activity), satisfactory (when improvement on the VAS score > 50% and moderate limited physical activity) and poor (when improvement on the VAS score < 50% and very limited physical activity). We also evaluated severity of depression status using the Montgomery-Asberg Depression Rating Scale (MADRS). The overall complication rate was defined as the occurrence of any adverse event occurring during the procedure and/or within a week of the same. Functional outcomes and complications rate were assessed immediately after surgery and by outpatient clinic evaluations at defined time intervals.
Statistical analysis
Data were expressed as mean ± standard deviation (SD). Paired sample t-test that was used to compare the SF-36, VAS and MADRS domain scores before (baseline) and after treatment with DiscoGel was obtained for each patient. P-value of 0.05 was considered statistically significant. IBM R software for Windows was employed for all statistical analyses.
Results
Demographic and clinical features
We selected 94 consecutive patients with symptomatic grade 1 A-B and 2 A-B LDH. They were 40 females and 54 males with a mean age of 53.2 (range 27–79) years. Among them, 30 patients (31.9%) had lumbar back pain, 19 (20.2%) had RP and 45 (47.9%) had both. The average disease duration was 8.7 ± 3.9 months. Lumbar level was L3–L4, L4–L5 and L5–S1, respectively, in 13, 45 and 36 patients. Overall, 49 were smokers. Fasting glycaemia (mg/dl) was 81.6 ± 9.2. Mean body mass index (BMI) was 24 ± 1.8. The average waist circumference was 86.3 ± 1.7 cm. MADRS was 14.3 ± 9.1. The follow-up was 44.18 (range 22–67) months. Demographic and clinical characteristics, including age, sex, HbA1c, disease duration, preoperative pain score, limitation on physical activity, depression rating, smoking, pain type, lumbar level symptoms, and mean follow-up, are reported in Table 1.
Table 1.
Demographic and clinical characteristics of the patients.
| Patients | 94 |
| Mean age (years) | 53.2 (range 27–79) |
| Sex (F/M) | 54/40 |
| Disease duration (months) | 8.7 ± 3.9 |
| Mean preoperative VAS | 8.4 ± 1.04 |
| Mean preoperative SF-36 score | 27.2 ± 12.21 |
| Mean MADRS | 14.3 ± 9.1 |
| Mean HbA1c | 6.8% |
| Mean BMI | 24 ± 1.8 |
| Mean waist circumference (cm) | 86.3 ± 1.7 |
| Smokers | 49/94 |
| Pain: | |
| LBP | 30 (40.5%) |
| LBP + RP | 45 (58.3%) |
| RP | 19 (22.5%) |
| Lumbar level symptom: | |
| L3–L4 | 13 (43%) |
| L4–L5 | 36 (46%) |
| L5–S1 | 45 (58.6%) |
| Mean follow-up (months) | 44.18 (range 22–67) |
BMI: body mass index; VAS: Visual Analogue Scale; SF: short form health survey; MADRS: Montgomery-Asberg Depression Rating Scale; LBP: low back pain; RP: radicular pain.
Pain relief and limitation on physical activity and HRQoL
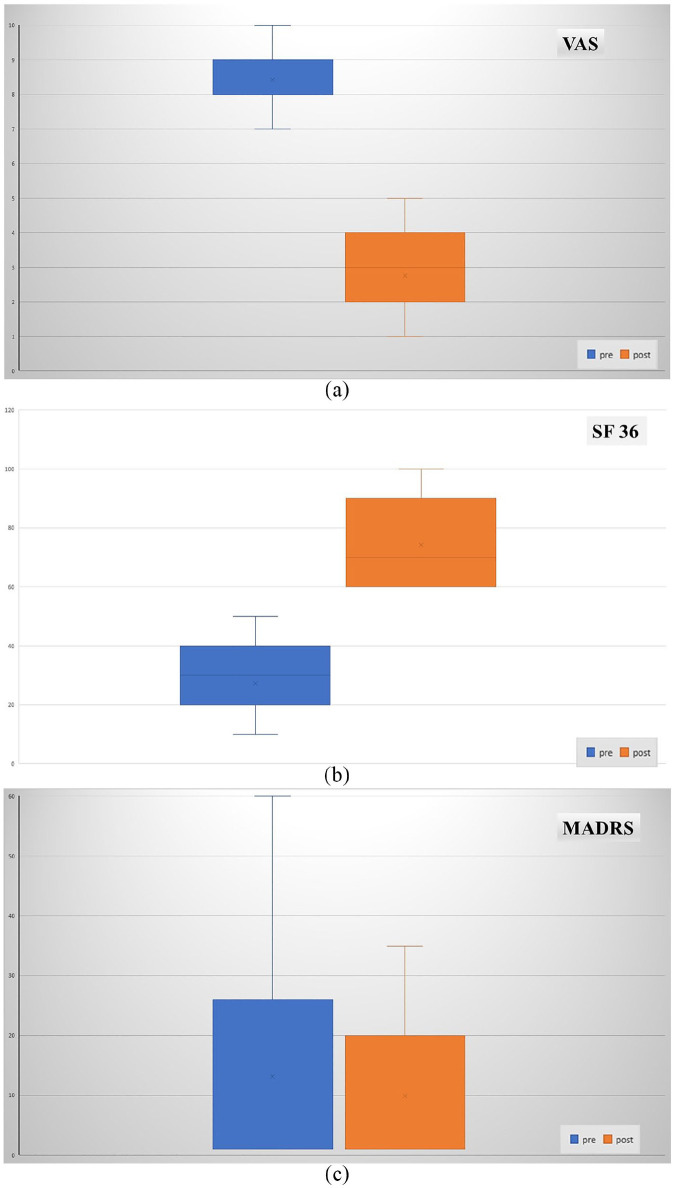
The mean preoperative VAS pain score was 8.4 ± 1.04, while the average postoperative value progressively decreased was 2.8 ± 1.07 at the 1-month follow-up (p < 0.05). (Figure 1(a))
Figure 1.
(a) Box-plot comparing average of VAS pain scores and SF-36, before and after treatment, showing a significant pain relief. (b) Box-plot comparing average of VAS pain scores and SF-36, before and after treatment, showing a significant improvement of the limitation on physical activity and HRQoL. (c) Box-plot showing that the depression status was not significantly changed in the postoperative period.
Notably, in lumbar back pain, relief was achieved immediately after the procedure in 88.3% of patients, while in 10.6% of them a significant improvement of VAS score (> 50%) was obtained in 10 days.
Differently, a significant overall improvement of RP (84.04% of patients) was obtained only 3 weeks after treatments. Similarly, the average preoperative SF-36 score was 27.2 ± 12.21, while the mean postoperative value increased progressively and was 74.3 ± 13.31 at 1-month follow-up (p < 0.05). (Figure 1(b))
Functional outcome and severity of depression status
Excellent or good results were achieved in 77 patients (81.9%), while nine patients (9.6%) had satisfactory results. VAS and SF-36 HRQoL scores remained unchanged along the whole follow-up. At the last follow-up, we recorded at least a satisfactory outcome, (patients with VAS improvement > 50%) in 92.5% of patients. Overall, in nine patients (9.6%), we observed poor results. At first, all these patients underwent conservative treatments with progressive improvement of pain in five out nine patients. The other four patients underwent to open surgery for the persistence of severe pain (VAS = 8/10). The latter, postoperative MRI images showed an unchanged disc herniation.
In 54 out of 94 patients (57%), we noted a slight depression status (mean MADRS 11.7 ± 5.9) that not significantly changed after treatment (mean MADRS 9.8 ± 3.2). (Figure 1(c))
Complications rate
In one case (1.06%), we observed a mild transitory sensory-motor deficit, probably due to the diffusion of local anaesthetic along the introducer needle. The deficit disappeared within 8 hours without any medications. In the immediate postoperative, the onset of an acute RP was detected in one patient (1.06%) but completely recovered in 5 days of corticosteroid therapy. We assumed that this adverse event has been due to an excessive epidural leakage of DiscoGel with irritation of nerve endings. No allergic complications or discitis were observed.
Discussion
In this article, we report the functional outcome and surgical complication of 94 consecutive patients with LBP and/or RP related to a LDH operated on with DiscoGel chemonucleolysis. Using this minimally invasive percutaneous technique, we demonstrated that in well-selected patients, it is possible to obtain good functional outcome and to reduce the spectrum of some complications related to similar procedures. DiscoGel is a percutaneous procedure that, by producing shrinkage of the disc, is thought to relieve pain in patients with symptomatic disc herniation.3,13 In our study, we verified, in a quite large population of patients (n = 94), that DiscoGel chemonucleolysis is an effective treatment, both in the short and long term, in patients with single, small or medium-sized LDH in whom conservative treatments have failed.
LDH is a chronic, expensive and common musculoskeletal disorder responsible for back- and radicular-related pain. Disc herniation is the result of progressive metabolic and structural changes that lead to the loss of mechanical stability and shock absorber function of the intervertebral disc.15 Even if its aetiology and pathogenesis are not fully understood, a correlation between intervertebral disc degeneration and LBP and/or RP has been documented.15,16 LBP and/or RP associated to disc herniation is a multifactorial process characterized by mechanical and inflammatory factors. Mechanical factors are related to a direct compression of LDH on the spinal ganglion associated to the stretching of posterior longitudinal ligament and annulus, resulting in stimulation of the recurrent nerve of Lutschka.13,15,17 While, compression on afferent arterioles and nerve bundle microcirculation causing anoxic demyelination, venous stasis and finally ischaemia are indirect mechanical factors.13,15,17 Other relevant pathogenetic pathway is neural inflammation process, involving an autoimmune cell-mediated response to proteoglycans released from intervertebral disc fragments and bio-humoral immunological response to prostaglandin (PGE2) produced by phospholipase A2, matrix metalloproteinase (MMP-1-2-2-9), IL-1, IL-6 and TNF-alfa.13,15 According with Theron theory,18 we assumed that LBP and RP improvement after the intradiscal ‘DiscoGel’ injection may be related to the reduction of intradiscal pressure and disc shrinkage relays in the reduction of the mechanical compression determined to the nerve roots retraction of the disc herniation.
Functional outcome
Using this minimally invasive technique, we obtained excellent results in terms of pain relief, limitation of physical activity and HRQoL. The average preoperative VAS pain score was 8.4, while the postoperative score was 2.8 (p = 0.5). Likewise, the mean SF-36 score was 27.2 and 74.3, respectively, before and after the procedures (p < 0.05). Moreover, although with slightly lower percentages, good results are also maintained along the whole follow-up period. At the last follow-up, overall, in 87 patients out of 94 (92.5%), we achieved at least a satisfactory result. Our results are similar with those, recently published by Bellini and colleagues3,19 reporting both, good results with significant reduction of VAS score and functional ability (assessed by the Oswestry disability index) after the procedure. However, these studies were conducted on a fairly heterogeneous population, consisting of patients with cervical and LDH; indeed, these two pathological conditions often behave differently. Moreover, they included patients treated at multiple levels and with disc herniation not clearly categorized. In an attempt to avoid confounding variables, in our study, we include only patients with symptomatic MSU grade 1 A-B and 2 A-B LDH and operated on a single level. Furthermore, we inject a higher dose of DiscoGel (0.8–1.6 mL) compared with those utilized in previous studies (0.8 mL of DiscoGel for lumbar discs and 0.3 mL for cervical). In contrast, Léglise et al.20 reported a failure rate of 64% in 25 patients who underwent DiscoGel procedure. The higher rate of failures, reported in the study, was probably due to a different population included in the study and may also be explained by differences in procedure. Furthermore, the relatively small size of the study could lead to a weakness of statistical significance. Stagni et al.21 evaluated clinical results in 32 patients with LDH unresponsive to O2–O3 therapy. DiscoGel treatment was successful in 24 out of 32 patients (75%).
Our overall good results are probably due to a well-selected population of patients, a standardized procedure and to a close multidisciplinary collaboration (neurosurgeons/neuroradiologists/pain therapists).
Complication rate
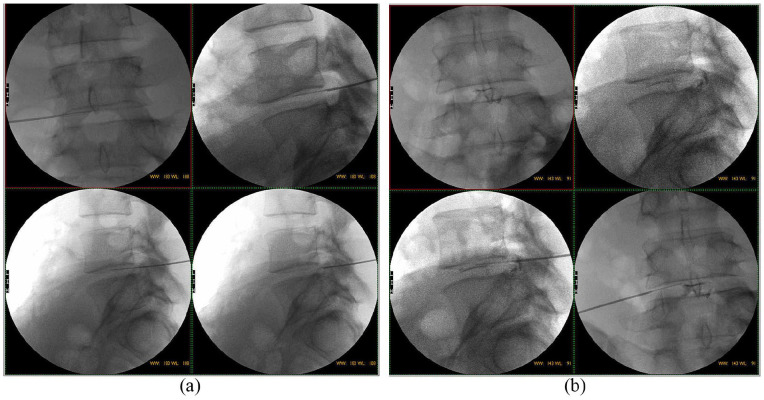
Over the years, different therapies have been proposed to treat symptomatic disc herniation, including different minimally invasive percutaneous techniques and open surgical methods. Among these, MD still remains the gold standard of treatments for the majority of disc herniation patients, even if it is to some extent burdened by a series of morbidities.12,22 For these reasons, several minimally invasive percutaneous procedures had a dramatic increase in utilization, over the years. However, also among these procedures, some complications that may negatively affect the outcome are reported in the literature.2,3,19–21,23 They consist of discitis, anaphylaxis, instability, increased back pain, new numbness and tingling, epidural fibrosis and reherniation.24–28 The overall complication rate for LDH is ranging from 0% to 1.8%.2,3,19,20,29 Recently, DiscoGel chemonucleolysis has emerged as a safe, rapid and effective mini-invasive procedure with a relatively low complication rate.3,19,20 In our study, we only observed a mild transitory sensory-motor deficit in one patient, while another patient with LBP complained a transient onset of intense RP. However, all patients completely recovered in hours or few days. No allergic complications or discitis or other adverse events were observed. Our findings are in agreement with others similar published studies.3,19,20 Indeed, on the basis of the literature review, DiscoGel chemonucleolysis resulted a safe procedure.3,19,20 The procedure can be performed by CT or CT fluoroscopy. However, in our experience, also using the biplanar digital rotational angiographic suite, needle insertion is quite easy, safe and rapid (Figure 2(a)). Moreover, continuous fluoroscopic guidance allows a real-time evaluation of DiscoGel distribution into nucleus pulposus, avoiding possible leakage. (Figure 2(b)).
Figure 2.
(a) Images of biplanar digital rotational angiography of needle insertion. Right percutaneous approach to the L4–L5 intervertebral disc. (b).Intradiscal DiscoGel injection under fluoroscopic guidance.
Limitations
This is a single-centre observational study and along with the relatively small patient population carries the inevitable selection biases typically associated with such study designs. These biases may limit the inferences that we can draw from the results presented herein. However, even if we recognize the limitations that may reduce the generalizability of our findings, to our knowledge, this study is the largest series of patients affected with LDH, operated by means of DiscoGel chemonucleolysis. Moreover, this article provides useful information concerning the possibility, using these minimally invasive procedures, to maintain satisfactory results in terms of functional outcomes, minimizing complication rates in well-selected patients with LDH. To confirm these results, a prospective randomized control study, comparing different percutaneous techniques, will be required.
Conclusion
LBP with or without RP associated to LDH is a major health and economic problem in developed countries, and the number of people affected is increasing worldwide. Recently, percutaneous DiscoGel injection has been proposed as an effective minimally invasive procedure in patients with DH unresponsive to conservative treatments. Our results suggest that DiscoGel chemonucleolysis is a reliable method to achieve satisfactory outcome in terms of pain relief and to minimize the overall rate of complications related to these kinds of surgical procedures and therefore can improve the quality of life of our patients with LBP and/or RP.
Acknowledgments
The authors thank Mr Antonio Iannello for his kind contribution in this research.
Footnotes
Contributorship: D.L.T. ideated and coordinated the study and data collection; D.L.T. wrote the draft of the article; A.L. reviewed and edited the article and approved the final version of the article. All authors provided feedback on the initial draft article and agreed the final changes.
Conflict of interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Institutional Review Board of Catanzaro does not require ethical approval for reporting case series.
Guarantor: Domenico La Torre is the guarantor of this article.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
ORCID iD: Domenico La Torre  https://orcid.org/0000-0002-3918-8798
https://orcid.org/0000-0002-3918-8798
References
- 1. Fouquet N, Descatha A, Ha C, et al. An epidemiological surveillance network of lumbar disc surgery to help prevention of and compensation for low back pain. Eur J Public Health 2016; 26(4): 543–548. [DOI] [PubMed] [Google Scholar]
- 2. Hashemi M, Poorfarokh M, Mohajerani SA, et al. Injection of intradiscal O2-O3 to reduce pain and disability of patients with low back pain due to prolapsed lumbar disk. Anesth Pain Med 2014; 4(5): e19206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Marcia S, Bellini M, Hirsch JA, et al. Efficacy of an ethyl alcohol gel in symptomatic disc herniation. Eur J Radiol 2018; 109: 101–107. [DOI] [PubMed] [Google Scholar]
- 4. Zheng JH, Walters ET, Song XJ. Dissociation of dorsal root ganglion neurons induces hyperexcitability that is maintained by increased responsiveness to cAMP and cGMP. J Neurophysiol 2007; 97: 15–25. [DOI] [PubMed] [Google Scholar]
- 5. Freynhagen R, Baron R. The evaluation of neuropathic components in low back pain. Curr Pain Headache Rep 2009; 13(3): 185–190. [DOI] [PubMed] [Google Scholar]
- 6. Nota per Gli Utilizzatori, http://www.biospina.com/wp-content/uploads/2013/05/LG_ernia_disco1.pdf (accessed 4 March 2019).
- 7. Bostelmann R, Steiger HJ. Comment on: an evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J 2014; 14(9): 2273. [DOI] [PubMed] [Google Scholar]
- 8. Kreiner DS, Hwang SW, Easa JE, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J 2014; 14(1): 180–191. [DOI] [PubMed] [Google Scholar]
- 9. Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical vs nonoperative treatment for lumbar disk herniation. JAMA 2006; 296(20): 2451–2459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pearson AM, Blood EA, Frymoyer JW, et al. SPORT lumbar intervertebral disk herniation and back pain: does treatment, location, or morphology matter? Spine 2008; 33(4): 428–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fisher C, Noonan V, Bishop P, et al. Outcome evaluation of the operative management of lumbar disc herniation causing sciatica. J Neurosurg 2004; 100(4 Suppl. Spine): 317–324. [DOI] [PubMed] [Google Scholar]
- 12. Shriver MF, Xie JJ, Tye EY, et al. Lumbar microdiscectomy complication rates: a systematic review and meta-analysis. Neurosurg Focus 2015; 39(4): E6. [DOI] [PubMed] [Google Scholar]
- 13. Pardatscher K, Volpentesta G, Bombardieri C, et al. Percutaneous treatment of lumbar intervertebral disc hernias with discogel. Neuroradiol J 2011; 24(4): 627–635. [DOI] [PubMed] [Google Scholar]
- 14. Mysliwiec LW, Cholewicki J, Winkelpleck MD, et al. MSU classification for herniated lumbar discs on MRI: toward developing objective criteria for surgical selection. Eur Spine J 2010; 19(7): 1087–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vergroesen YZ, Kingma I, Emanuel KS, et al. Mechanics and biology in intervertebral disc degeneration: a vicious circle. Osteoarthritis Cartilage 2015; 23(7): 1057–1070. [DOI] [PubMed] [Google Scholar]
- 16. Lambeek LC, van Tulder MW, Swinkels IC, et al. The trend in total cost of back pain in the Netherlands in the Period 2002 to 2007. Spine 2011; 36(13): 1050–1058. [DOI] [PubMed] [Google Scholar]
- 17. Ruiz-Fernandez C, Francisco V, Pino J, et al. Molecular relationships among obesity, inflammation and intervertebral disc degeneration: are adipokines the common link. Int J Mol Sci 2019; 20(8): E2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Theron J, Guimaraens L, Casasco A, et al. Percutaneous treatment of lumbar intervertebral disk hernias with radiopaque gelified ethanol: a preliminary study. J Spinal Disord Tech 2007; 20(7): 526–532. [DOI] [PubMed] [Google Scholar]
- 19. Bellini XM, Romano DG, Leonini S, et al. Percutaneous injection of radiopaque gelified ethanol for the treatment of lumbar and cervical intervertebral disk herniations: experience and clinical outcome in 80 patients. AJNR Am J Neuroradiol 2015; 36: 600–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Léglise A, Lombard J, Moufid A. DiscoGel® in patients with discal lumbosciatica. Retrospective results in 25 consecutive patients. Orthop Traumatol Surg Res 2015; 101(5): 623–626. [DOI] [PubMed] [Google Scholar]
- 21. Stagni S, de Santis F, Dall M, et al. A minimally invasive treatment for lumbar disc herniation: DiscoGel ® chemonucleolysis in patients unresponsive to chemonucleolysis with oxygen-ozone. Interv Neuroradiol 2012; 18: 97–104, www.centauro.it (accessed 14 March 2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Aydın Y, Ziyal IM, Duman H, et al. Clinical and radiological results of lumbar microdiskectomy technique with preserving of ligamentum flavum comparing to the standard microdiskectomy technique Surg Neurol 2002; 57: 5–13, https://ac.els-cdn.com/S0090301901006772/1-s2.0-S0090301901006772-main.pdf?_tid=0488af06-c645–44de-81cc-d7ebaaaf51cc&acdnat=1551803970_ca13e1521d158b8fe764420167987a3e (accessed 5 March 2019). [DOI] [PubMed] [Google Scholar]
- 23. Touraine S, Damiano J, Tran O, et al. Cohort study of lumbar percutaneous chemonucleolysis using ethanol gel in sciatica refractory to conservative treatment. Eur Radiol 2015; 25(11): 3390–3397. [DOI] [PubMed] [Google Scholar]
- 24. Crock HV. Internal disc disruption: a challenge to disc prolapse fifty years on. Spine Phila Pa 1976; 11(6): 650–653. [PubMed] [Google Scholar]
- 25. de Sèze M, Saliba L, Mazaux J. Percutaneous treatment of sciatica caused by a herniated disc: an exploratory study on the use of gaseous discography and Discogel® in 79 patients. Ann Phys Rehabil Med 2013; 56: 143–154. [DOI] [PubMed] [Google Scholar]
- 26. Rahimzadeh P, Imani F, Ghahremani M, et al. Comparison of percutaneous intradiscal ozone injection with laser disc decompression in discogenic low back pain. J Pain Res 2018; 11: 1405–1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Smuck M, Benny B, Han A, et al. Epidural fibrosis following percutaneous disc decompression with coblation technology. Pain Physician 2007; 10(5): 691–696. [PubMed] [Google Scholar]
- 28. Bouillet R. Treatment of sciatica: a comparative survey of complications of surgical treatment and nucleolysis with chymopapain. Clin Orthop Relat Res 1990; 251(251): 144–152. [PubMed] [Google Scholar]
- 29. Gibson JN, Grant IC, Waddell G. The Cochrane review of surgery for lumbar disc prolapse and degenerative lumbar spondylosis. Spine 1999; 24(17): 1820–1832. [DOI] [PubMed] [Google Scholar]