Abstract
Purpose
Patellofemoral instability is a common cause of knee pain and dysfunction in paediatric and adolescent patients. The purpose of the study was to evaluate the frequency of patellar dislocations seen in emergency departments (EDs) and the rates of surgical procedures for patellar instability at paediatric hospitals in the United States between 2004 and 2014.
Methods
The Pediatric Health Information System database was queried for all paediatric patients who underwent surgery for patellar instability or were seen in the ED for acute patellar dislocation between 2004 and 2014. This was compared with the annual numbers of overall orthopaedic surgical procedures.
Results
Between 2004 and 2014, there were 3481 patellar instability procedures and 447 285 overall orthopaedic surgical procedures performed at the included institutions, suggesting a rate of 7.8 per 1000 orthopaedic surgeries. An additional 5244 patellar dislocations treated in EDs were identified. Between 2004 and 2014, the number of patellar instability procedures increased 2.1-fold (95% confidence interval (CI) 1.4 to 3.0), while orthopaedic surgical procedures increased 1.7-fold (95% CI 1.3 to 2.0), suggesting a 1.2-fold relative increase in patellar instability procedures, compared with total paediatric orthopaedic surgeries.
Conclusion
This study shows a significant rise in the rate of acute patellar instability treatment events in paediatric and adolescent patients across the country. Surgery for patellar instability also increased over the study period, though only slightly more than the rate of all paediatric orthopaedic surgical procedures. This may suggest that increasing youth sports participation may be leading to a spectrum of increasing injuries and associated surgeries in children.
Level of Evidence
IV
Keywords: patellar instability, pediatrics, adolescent, Pediatric Health Information System
Introduction
Patellofemoral instability, defined as the inability of the patella to remain in appropriate alignment throughout the normal arc of knee movement as a result of structural compromise to the bony and soft-tissue restraints of the patellofemoral joint, is a common cause of knee pain and dysfunction in paediatric and adolescent patients.1-3 Specific patellofemoral instability conditions include acute patellar dislocation, patellar subluxation and recurrent subjective instability.
Patellofemoral instability is challenging to treat, as there are varied forms of instability and a wide range of symptomatology and pathology.1,4 Historically, nonoperative treatment has been the standard of care for first-time or ‘primary’ episodes of acute patellar instability in the absence of chondral loose body or osteochondral fracture. However, there is a variable yet significant rate of recurrent instability with nonoperative care in a young population.5,6 Newer surgical techniques for patellar stabilization have become popular and have been adapted for younger populations. Advances in understanding of the relevant anatomy have contributed to improved surgical treatment as well.6 Medial patellofemoral ligament (MPFL) reconstruction is one of several surgical procedures used. Studies have found that operative treatment may be associated with a lower risk of recurrent dislocation, high percentage of return to sport and higher health-related quality of life and sporting function than nonoperative treatment, with some investigated cohorts including first-time dislocators.7-9 All of these trends may contribute to an increased rate of surgical treatment for patellar dislocation, but this concept remains incompletely explored or quantified.
The purpose of this study is to identify trends in patellar instability injuries and treatment at paediatric hospitals in the United States. The study is designed to assess trends in the frequency of patellar dislocation reductions that occur in the emergency department (ED) as well as trends in surgical intervention for patellar instability to determine whether there has been an increase in the rate of surgical treatment for this injury. Our hypothesis is that there has been an increase in frequency of patellar dislocation injuries and an increase in the rate of operative treatment for patellar instability in children over the study period.
Materials and methods
Data from the Pediatric Health Information System (PHIS) database were used for this study. The PHIS is an administrative database that contains inpatient, ED, ambulatory surgery and observation encounter-level data from 48 not-for-profit, tertiary-care paediatric hospitals in the United States, which are affiliated with the Children’s Hospital Association (Overland Park, Kansas). Data quality and reliability are assured through a joint effort between the Children’s Hospital Association and participating hospitals. Participating hospitals provide discharge/encounter data including demographics, diagnoses, procedures and resource utilization data. Data are de-identified at time of submission. Because all data were obtained from a de-identified administrative database, this study was exempt from institutional review board approval. Permission to report de-identified data from the PHIS database was obtained from the Children’s Hospital Association.
The PHIS database was queried for all patients 18 years or younger who underwent orthopaedic surgery procedures between January 1st 2004 and December 31st 2014 using the associated PHIS preferred service line (PSL), PSL 520 “Orthopedics-Surgical”, which is a comprehensive set of all surgeries performed by the orthopaedic services at these PHIS contributing centres. This time period was chosen in order to obtain an entire decade of data without cross-over from International Classification of Diseases (ICD)-9 to ICD-10 (which occurred in 2015) due to differences in coding. This aligns with the Tepolt et al14 study on trends in anterior cruciate ligament (ACL) reconstruction, which used similar exclusion criteria as this study. Data from 25 of the 48 paediatric hospitals participating in the PHIS initiative reported comprehensive patient data consistently for the study time period and were included in the analysis. These 25 centres include two in the Northeast, eight in the Midwest, nine in the South and six in the West. The 23 centres excluded from the current analysis reported gaps in comprehensive patient data reporting for some portion of the study period.
Two different cohorts for each year were identified. The first cohort consisted of patients who underwent a surgical procedure with one or both associated ICD-9 codes for patellar instability (836.3: closed dislocation of patella; 718.36: recurrent dislocation of patella/knee).10 The Current Procedural Terminology, Fourth Revision (CPT-4)11 was used to confirm the procedures by checking the reported codes for each case and determining that they fell within the appropriate category. The second cohort was comprised of patients seen in the ED with one or both of the same ICD-9 codes in addition to CPT codes 27560 or 27562, which indicate that a closed reduction of a patellar dislocation with or without anaesthesia was performed. The database was further queried for patients using the associated PHIS PSL 520 “Orthopedics-Surgical” and PSL 510 “Orthopedics-Medical” who also had the diagnosis codes.
The volume of total orthopaedic surgical procedures and the volume of patellar instability surgeries in each year were evaluated. The volume of surgical procedures for patellar instability was analyzed over the 11-year study period and the annual rate reported as the number of patellar instability surgeries per 1000 paediatric orthopaedic surgeries. Linear modelling was used to assess the overall relative trends in total orthopaedic and patellar dislocation specific surgeries. The n-fold increases in surgery rates were estimated for all subjects and across sex subgroups along with 95% confidence intervals (CIs) to quantify trends over time. Additional analyses were conducted for patellar dislocations treated with reduction in the ED, including trends in treatment and n-fold change in rates of treatment for all subjects by patient sex. Analyses were performed using R statistical software version 3.5.2 (R Core Team, 2020). A p-value < 0.05 was considered statistically significant.
Results
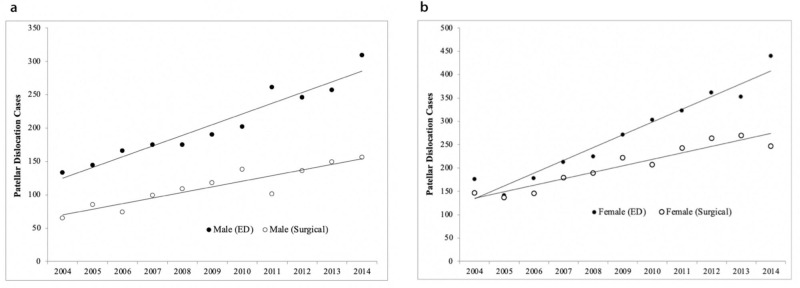
Between January 1st 2004 and December 31st 2014, there were 447 285 orthopaedic surgical procedures at 25 institutions that consistently reported data from the specified time period (Fig. 1a). There were 3481 patellar instability surgical procedures during this time period, for a rate of 7.8 per 1000 orthopaedic surgical procedures. In all, 65% (2251/3481) of these procedures were for female patients. The mean age of the patients who underwent patellar instability surgical procedures was 14.2 years (sd 2.61) (Table 1). In 2004 there were 212 patellar instability surgical procedures; this number increased to 403 in 2014 (Fig. 1b). The rate per 1000 orthopaedic surgical procedures increased from 7.4 to 8.3 during this time period; the highest yearly rate was 8.8 in 2013 and the lowest was 6.9 in 2006 (Fig. 1c).
Fig. 1.
a) Total paediatric orthopaedic surgical procedures beween 2004 and 2014; b) paediatric emergency department (ED) patellar dislocation versus patellar instability surgical procedures between 2004 and 2014; c) paediatric patellar instability surgical procedures per 1000 orthopaedic surgical procedures.
Table 1.
Paediatric patellar cohort characteristics
| Surgical procedures (n = 3481) | ED cases (n = 5244) | |
|---|---|---|
| Gender, n (%) | ||
| Female | 2251 (65) | 2983 (57) |
| Male | 1230 (35) | 2258 (43) |
| Unknown | 0 (0) | 3 (0.06) |
| Mean age, yrs (sd) | 14.2 (2.61) | 13.6 (2.52) |
ED, emergency department
Additionally, 5244 patellar dislocations were treated with reductions in the ED (Table 1). In all, 43% (2258/5244) of the ED visits were for male patients, and 57% were for female patients. The mean age of the patients with ED visits was 13.6 years (sd 2.52). ED visits increased from 309 in 2004 to 749 in 2014 (Fig. 1b), for an overall 2.7-fold increase in ED treatment of patellar dislocation (95% CI 1.7 to 9.5; p < 0.001).
The rate of overall orthopaedic surgical procedures increased 1.7-fold (95% CI 1.3 to 2.0; p < 0.001) over the study period (Table 2). During the same time period, the number of patellar instability surgical procedures increased 2.1-fold (95% CI 1.4 to 3.0; p < 0.001). There was a 1.2-fold (95% CI 1.1 to 1.2; p = 0.003) increase in patellar instability surgical procedures relative to total paediatric orthopaedic surgical procedures (Table 2).
Table 2.
Increase in surgical procedures over the 11-year study period for all subjects and by patient sex
| n | n-fold change | 95% confidence interval | p-value | |
|---|---|---|---|---|
| All orthopaedic surgical procedures | 447 285 | 1.73 | 1.28 to 1.97 | < 0.001 |
| Patellar instability surgical procedures | 3481 | 2.09 | 1.44 to 3.01 | < 0.001 |
| Rate per 1000 orthopaedic procedures | 1.19 | 1.08 to 1.22 | 0.003 | |
| ED patellar dislocation reductions | 5244† | 2.68 | 1.68 to 9.50 | < 0.001 |
| Female | ||||
| Patellar instability surgical procedures | 2251 | 2.03 | 1.40 to 2.86 | < 0.001 |
| ED patellar dislocation reductions | 2983 | 3.04 | 2.32 to 4.14 | < 0.001 |
| Male | ||||
| Patellar instability surgical procedures | 1230 | 2.22 | 1.53 to 4.32 | < 0.001 |
| ED patellar dislocation reductions | 2258 | 2.29 | 1.51 to 4.29 | < 0.001 |
three subjects did not have data on sex
ED, emergency department
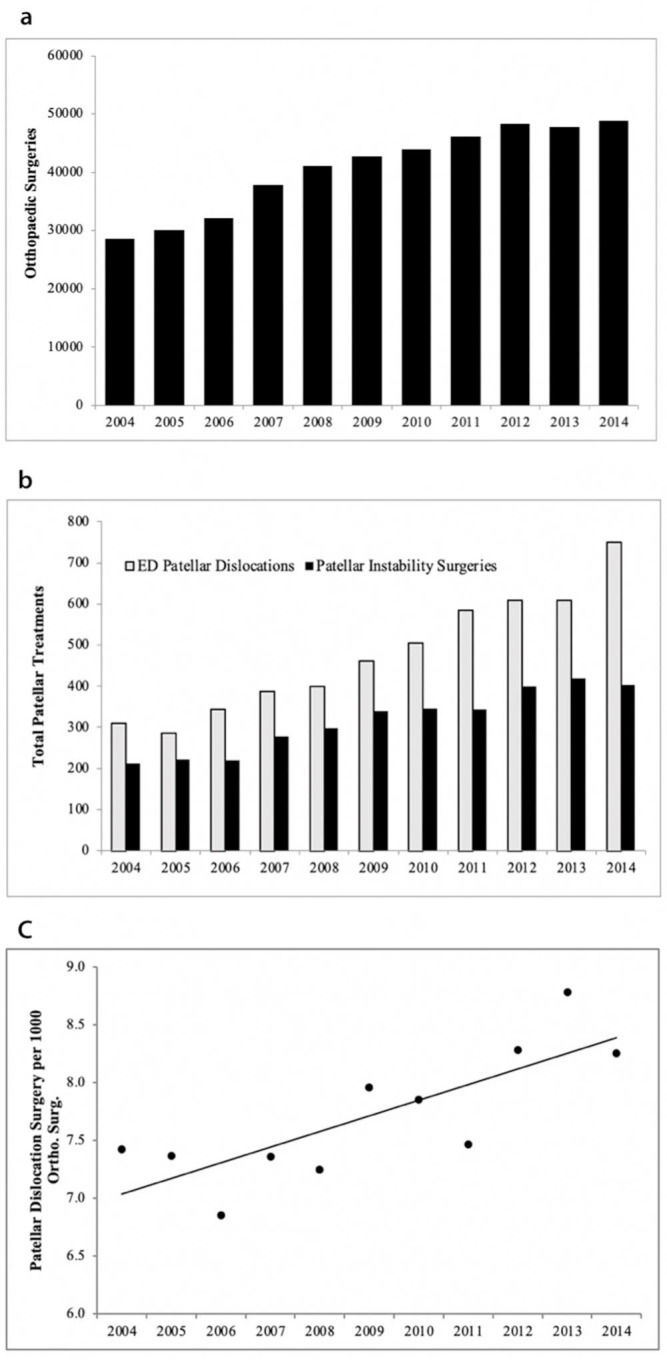
With regards to trends by sex, male patients yielded similar trends between ED cases and operative cases for patellar instability, with a 2.3-fold (95% CI 1.5 to 4.3; p < 0.001) increase in ED cases and 2.2-fold (95% CI 1.5 to 4.3; p < 0.001) increase in operative cases (Fig. 2a). Female patients experienced a higher increase in the ED cases compared with operative cases, with a 3.0-fold (95% CI 2.3 to 4.1, p < 0.001) increase and 2.0-fold (95% CI 1.4 to 2.9; p < 0.001) increase, respectively (Fig. 2b). There was no significant difference detected in the rate increase of surgical procedures between male and female patients. However, female patients had a higher overall rate of surgical procedures, compared with male patients, when analyzed as a percentage of overall patellar instability ‘care’ events (43% versus 35%; p < 0.001).
Fig. 2.
a) Male patellar dislocation emergency department (ED) treatment versus surgery; b) female patellar dislocation ED reductions versus surgical procedures.
Discussion
This study shows a significant rise in the rate of patellar dislocation reductions and patellar instability surgical procedures in paediatric hospitals across the country, between 2004 and 2014. ED treatment for patellar dislocation increased 2.7-fold over the time period studied, and patellar instability surgical procedures increased 2.1-fold. Interestingly, surgical procedures for patellar instability increased only slightly more than the rate of all paediatric orthopaedic surgical procedures, which increased 1.7-fold. This significant increase in patellar instability care at paediatric orthopaedic centres is cause for increased awareness and investigation regarding how to continue improving treatment of children and adolescents with these increasingly common sports-related injuries.
Prior studies have examined the increasing incidence of overall orthopaedics injuries among children and adolescents and have hypothesized a direct connection to increased sports participation.12-19 In a recent review article, Trentacosta15 discusses the increasing number of injuries seen in the paediatric and adolescent athlete population in the context of increased participation in organized youth sports and early specialization in single sports. Field et al17 found total hours per week of vigorous activity to be predictive of developing injury, and girls who engaged in sports specialization to be at increased risk of injury. Fridman et al14 conducted a retrospective study examining the epidemiology of sports-related injuries in children between 2007 and 2010 and found a significant increase in the number of injuries. Recently, Tepolt et al16 reported a 5.7-fold increase, nearly equivalent across sexes, in the number of paediatric ACL reconstruction surgeries between 2004 and 2014, treating a condition typically associated with sports participation.
Regarding patellar instability events, there are previous studies that have looked at the incidence and specific risk factors for this common knee condition. However, there are no studies of this magnitude that report specifically on the increased incidence in patellar instability events and discuss implications for prevention and treatment. In this study, we were able to evaluate a nationwide trend over a lengthy time period. In a similar study in 2018 within a closed healthcare system within one county, Sanders et al20 reported on a cohort of 609 patients over a 20-year period between 1990 and 2010 and found the overall incidence to be relatively stable, with a greater than previously reported incidence among adolescents. Sanders et al21 also examined the incidence of recurrent patellar dislocation in skeletally immature patients and found increased rates of recurrent ipsilateral and contralateral dislocations. In contrast, our study specifically examines the paediatric population and includes a far wider geographic range, as well as a more recent time frame.
Acknowledging patellar instability as a condition that most significantly affects children and adolescents, with significant rates of surgical treatment, is important, given potential long-term consequences for joint health and mobility in such young patients. Multiple studies have discussed the complex nature of these injuries. Going back to 1988, congenital abnormalities have been associated with a predisposition to instability events.22 More recently, Lewallen et al23 described risk factors for recurrent patellar instability to include immature physes, patella alta and trochlear dysplasia. During the same time period of Sanders et al’s aforementioned study (1990 to 2010), 232 skeletally immature patients were examined and a high rate of recurrent instability was found to be associated with structural abnormalities such as patella alta and trochlear dysplasia.21 Keyes et al4 detailed the varied forms of instability and risk factors that should be considered in treatment, as well as varied surgical techniques currently available to surgeons for treating this condition. Koh and Stewart6 also outlined the potential long-term consequences of patellar instability and emphasized the importance of advances in anatomical understanding in successful surgical management. Increasing awareness on the prevalence of this condition and critically examining how we are treating these patients is beneficial to ensure we are providing the highest level of care possible and minimizing long-term complications.
The issue of operative versus nonoperative management of patellar instability remains an area of significant controversy. Various authors24-28 have done significant work analyzing the anatomy of the medial soft-tissue stabilizers implicated in patellofemoral instability and involved in reconstruction. In kind, surgical treatment has made significant advances in the last two decades and now includes high success rates with soft-tissue realignment procedures used in skeletally immature patients, such as MPFL reconstruction.29-32 There are also multiple bony realignment procedures, including but not limited to tibial tubercle transfers, used for correction of anatomical bony defects that predispose to patellofemoral injury.3,33,34 A recent systematic review in 2015 examined 11 studies, pooling the results of 470 conservatively managed and 157 operatively managed knees, and found surgical treatment of first-time patella dislocation in children and adolescents was associated with a lower risk of recurrent dislocation and higher health-related quality of life and sporting function. However, the authors acknowledged the limited evidence on MPFL reconstruction for first time traumatic patella dislocation.8 In a separate study, Lewallen et al35 found nonoperative treatment for first time patellar dislocation resulted in a 62% success rate. In a separate study, Liu et al7 found MPFL reconstruction to be a safe and effective treatment for patellofemoral instability. Nelitz et al36reported combined MPFL reconstruction and trochleoplasty improved stability in patients with trochlear dysplasia. As newer, more advanced surgical techniques become available for treating these injuries, it is important to analyze how this affects treatment patterns and outcomes. This study included all reconstruction techniques over this time frame, but due to the limitations of the database we are unable to comment on increasing frequency of newer surgical techniques such as MPFL reconstruction versus repair or medial plication, or increasing frequency of trochleoplasty in this age group.
Our study noted sub-trends within the data as well, specifically with regards to sex differences. Female patients had a higher rate of increase in ED treatment compared with operative treatment, demonstrating 3.0-fold and 2.0-fold increases over the time period, respectively. In comparison, male patients saw a similar increase in ED and operative treatment, with 2.3-fold and 2.2-fold, respectively. The larger increase in ED treatment among female patients may relate to an increase in girls playing sports since the early 2000s, or may relate to variation in the mechanism of injury between male and female children/adolescents with overall increasing sports participation.19,37 A previous study by Stracciolini et al38 showed girls are more likely to have injuries to the lower extremity compared with boys in a sports-related context. Luhmann39 found female patients to be more likely to have patellofemoral pathology compared with male patients. There was no significant difference detected in the rate of increase of surgical procedures between male and female cases. However, female patients had a higher overall rate of surgical procedures when analyzed as a percentage of their overall patellar instability ‘care’ events (ED reductions plus surgical procedures), compared with male patients (43% versus 35%; p < 0.001). This provides new insights into potential treatment discrepancies. The comparative rates between ED and operative treatment among female and male patients with patellar dislocation are interesting trends that may provide opportunity for further study.
Limitations of this study include those inherent to retrospective studies and those reliant upon large administrative databases. We do not have access to data on the mechanism of injury, clinical course or functional outcomes. Similarly, we do not have data on the nature of the surgical techniques used or any concurrent surgical procedures. Surgical decision-making factors, such as radiological findings, the number of prior instability events and incidence of osteochondral fractures, are unknown. While we know the age of patients involved, the relative skeletal maturity is unknown. It is not known if the patients who sustained a patellar instability event with ED treatment subsequently went on to have surgical treatment at outside hospitals. In addition, we are unable to gain any insights on patients who may have had an instability event but were not seen in the ED nor required operative intervention, such as those who may experience patellar dislocation and reduction without ever coming to the ED. There are likely a significant number of patients who are seen in clinic or never seen for less traumatic subluxations who are not captured in this study. However, we wanted to ensure that everyone included truly had an instability event and thus the CPT codes were used. Lastly, the PHIS database only includes tertiary-care referral paediatric hospitals, therefore, these same trends may not be present at community or non-specialty hospitals. As the subspecialty of paediatric sports medicine has increased, the rate of paediatric patellofemoral surgery may relate to more of these cases being seen in paediatric hospitals versus other sectors. We were only able to use 25 of the 48 centres in the PHIS database due to exclusions for incomplete data entry across the years included in the study, however, this hopefully ensures that the study accurately captures year to year changes at centres that had more complete data entry.
Strengths of this study include the large sample size, with massive data sets from 25 paediatric hospitals that spans the major geographic regions of the United States. This is the largest study of patellofemoral instability in this young age group. Moreover, a denominator of over 400 000 orthopaedic surgeries provides perspective on the relative place of patellar instability surgery within the spectrum of paediatric orthopaedic procedures. Another strength is the longitudinal nature of the study, with consistent data reported from these hospitals for the entire 11-year time period between 2004 and 2014. This enables us to clearly see significant trends over time. The specificity of the study design is important as well. Both cohorts consist solely of patients who have one or both of the ICD-9 codes for patellar instability (836.3: closed dislocation of patella; 718.36: recurrent dislocation of patella/knee). The ED cohort only includes patients who were billed for a reduction manoeuvre with or without anaesthesia (CPT codes 27560 and 27562). The specificity of this inclusion criteria leads to confidence in the diagnosis of patellofemoral instability for the patients included in this study.
Further research is needed to evaluate the link between the clinical significance of increasing rates of acute patellar instability events and the potential need for surgical intervention. More dislocation events suggested by the study are likely reflective of more young athletes with more exposures in today’s increasingly intense culture of youth sports. However, it may instead reflect persistent failures of nonoperative, or even operative, interventions to prevent recurrent episodes. Prospective studies examining longer-term outcomes among patients with patellar instability events are warranted to compare surgical versus nonoperative treatment. While similar studies have been done in the past, retrospective methodology and small sample sizes have limited impactful conclusions. Nonoperative treatment remains the mainstay of treatment for first occurrence patellar dislocation without significant intra-articular injury, however, randomized controlled trials and long-term outcomes data on newer surgical techniques may generate more sophisticated management algorithms.40 Newer surgical techniques and improved understanding of knee anatomy, as well as improved surgical techniques for paediatric patients with open physes, may lead to improved surgical outcomes. Research regarding preventative measures may be warranted as well.
In conclusion, there has been a significant rise in the rate of acute patellar instability events in paediatric and adolescent patients across the country. Moreover, surgery for patellar instability increased more than the rate of all paediatric orthopaedic procedures. Given these increasing rates, along with advances in surgical technique for operative treatment, more research on nonoperative versus operative management is warranted. Paediatric orthopaedic surgeons should be aware of this increasing rate of patellar instability events and continue to develop expertise in treatment for paediatric and adolescent age groups, given the correlation with ongoing increases in youth sports participation in this country.
Open access
This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent was not required for this study as no identifying information about participants is available in the article.
ICMJE Conflict of interest statement
The authors declare that they have no conflict of interest pertaining to this study.
Author Contributions
KHMcF: Assistance with data interpretation for the work, Drafting the work, Final approval of the version to be published, Agreement to be accountable for all aspects of the work.
RPC: Assistance with data interpretation for the work, Critical review of the work, Final approval of the version to be published, Agreement to be accountable for all aspects of the work.
LF: Acquisition of data for the work, Assistance with data interpretation for the work, Critical review of the work, Final approval of the version to be published, Agreement to be accountable for all aspects of the work.
PEM: Analysis of the data for the work, Critical review of the work, Final approval of the version to be published, Agreement to be accountable for all aspects of the work.
BEH: Conception of the work, Critical review of the work, Approval of the version to be published, Agreement to be accountable for all aspects of the work.
DEK: Conception of the work, Critical review of the work, Final approval of the version to be published, Agreement to be accountable for all aspects of the work.
MSK: Conception of the work, Critical review of the work, Final approval of the version to be published, Agreement to be accountable for all aspects of the work.
Y-MY Conception of the work, Critical review of the work, Final approval of the version to be published, Agreement to be accountable for all aspects of the work.
MDM: Conception and design of the work, Critical review of the work, Final approval of the version to be published, Agreement to be accountable for all aspects of the work.
References
- 1. Bessette M, Saluan P. Patellofemoral pain and instability in adolescent athletes. Sports Med Arthrosc Rev 2016;24:144-149. [DOI] [PubMed] [Google Scholar]
- 2. DeFroda SF, Gil JA, Boulos A, Cruz AI Jr. Diagnosis and management of traumatic patellar instability in the pediatric patient. Orthopedics 2017;40:e749-e757. [DOI] [PubMed] [Google Scholar]
- 3. Surendran S. Patellar instability - changing beliefs and current trends. J Orthop 2014;11:153-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Keyes S, Price M, Green DW, Parikh SN. Special considerations for pediatric patellar instability. Am J Orthop 2018;47. [DOI] [PubMed] [Google Scholar]
- 5. Krebs C, Tranovich M, Andrews K, Ebraheim N. The medial patellofemoral ligament: review of the literature. J Orthop 2018;15:596-599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Koh JL, Stewart C. Patellar instability. Orthop Clin North Am 2015;46:147-157. [DOI] [PubMed] [Google Scholar]
- 7. Liu JN, Brady JM, Kalbian IL, et al. Clinical outcomes after isolated medial patellofemoral ligament reconstruction for patellar instability among patients with trochlear dysplasia. Am J Sports Med 2018;46:883-889. [DOI] [PubMed] [Google Scholar]
- 8. Nwachukwu BU, So C, Schairer WW, Green DW, Dodwell ER. Surgical versus conservative management of acute patellar dislocation in children and adolescents: a systematic review. Knee Surg Sports Traumatol Arthrosc 2016;24:760-767. [DOI] [PubMed] [Google Scholar]
- 9. Schneider DK, Grawe B, Magnussen RA, et al. Outcomes after isolated medial patellofemoral ligament reconstruction for the treatment of recurrent lateral patellar dislocations: a systematic review and meta-analysis. Am J Sports Med 2016;44:2993-3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Centers for Medicare & Medicaid Services . ICD-9-CM Diagnosis and Procedure Codes: Abbreviated and Full Code Titles. Updated April 4, 2020. (Date last accessed 10 January 2021). https://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes
- 11. American Medical Association . AMA CPT® Professional 2021. American Medical Association; 2020. [Google Scholar]
- 12. Logan K, Cuff S, Council On Sports Medicine and Fitness . Organized sports for children, preadolescents, and adolescents. Pediatrics 2019;143:e20190997. [DOI] [PubMed] [Google Scholar]
- 13. Pasulka J, Jayanthi N, McCann A, Dugas LR, LaBella C. Specialization patterns across various youth sports and relationship to injury risk. Phys Sportsmed 2017;45:344-352 [DOI] [PubMed] [Google Scholar]
- 14. Fridman L, Fraser-Thomas JL, McFaull SR, Macpherson AK. Epidemiology of sports-related injuries in children and youth presenting to Canadian emergency departments from 2007-2010. BMC Sports Sci Med Rehabil 2013;5:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Trentacosta N. Pediatric sports injuries. Pediatr Clin North Am 2020;67:205-225. [DOI] [PubMed] [Google Scholar]
- 16. Tepolt FA, Feldman L, Kocher MS. Trends in pediatric ACL reconstruction from the PHIS database. J Pediatr Orthop 2018;38:e490-e494. [DOI] [PubMed] [Google Scholar]
- 17. Smucny M, Parikh SN, Pandya NK. Consequences of single sport specialization in the pediatric and adolescent athlete. Orthop Clin North Am 2015;46:249-258. [DOI] [PubMed] [Google Scholar]
- 18. Beck NA, Patel NM, Ganley TJ. The pediatric knee: current concepts in sports medicine. J Pediatr Orthop B 2014;23:59-66. [DOI] [PubMed] [Google Scholar]
- 19. Field AE, Tepolt FA, Yang DS, Kocher MS. Injury risk associated with sports specialization and activity volume in youth. Orthop J Sports Med 2019;7:2325967119870124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sanders TL, Pareek A, Hewett TE, et al. Incidence of first-time lateral patellar dislocation: a 21-year population-based study. Sports Health 2018;10:146-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sanders TL, Pareek A, Hewett TE, et al. High rate of recurrent patellar dislocation in skeletally immature patients: a long-term population-based study. Knee Surg Sports Traumatol Arthrosc 2018;26:1037-1043. [DOI] [PubMed] [Google Scholar]
- 22. Cash JD, Hughston JC. Treatment of acute patellar dislocation. Am J Sports Med 1988;16:244-249. [DOI] [PubMed] [Google Scholar]
- 23. Lewallen L, McIntosh A, Dahm D. First-time patellofemoral dislocation: risk factors for recurrent instability. J Knee Surg 2015;28:303-309. [DOI] [PubMed] [Google Scholar]
- 24. Tanaka MJ, Chahla J, Farr J II, et al. Recognition of evolving medial patellofemoral anatomy provides insight for reconstruction. Knee Surg Sports Traumatol Arthrosc 2019;27:2537-2550. [DOI] [PubMed] [Google Scholar]
- 25. Tanaka MJ, Tompkins MA, Fulkerson JP. Radiographic landmarks for the anterior attachment of the medial patellofemoral complex. Arthroscopy 2019;35:1141-1146. [DOI] [PubMed] [Google Scholar]
- 26. Tanaka MJ, Voss A, Fulkerson JP. The anatomic midpoint of the attachment of the medial patellofemoral complex. J Bone Joint Surg [Am] 2016;98:1199-1205. [DOI] [PubMed] [Google Scholar]
- 27. Fulkerson JP, Edgar C. Medial quadriceps tendon-femoral ligament: surgical anatomy and reconstruction technique to prevent patella instability. Arthrosc Tech 2013;2:e125-e128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Loeb AE, Tanaka MJ. The medial patellofemoral complex. Curr Rev Musculoskelet Med 2018;11:201-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shubin Stein BE, Gruber S, Brady JM. MPFL in first-time dislocators. Curr Rev Musculoskelet Med 2018;11:182-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ellis HB Jr, Dennis G, Wilson PL. Patellofemoral instability in the skeletally immature patient: a review and technical description of medial patellofemoral ligament reconstruction in patients with open physes. Am J Orthop (Belle Mead NJ) 2018;47. [DOI] [PubMed] [Google Scholar]
- 31. Bryant J, Pandya N. Medial patellofemoral ligament repair restores stability in pediatric patients when compared to reconstruction. Knee 2018;25:602-608. [DOI] [PubMed] [Google Scholar]
- 32. Clark D, Metcalfe A, Wogan C, Mandalia V, Eldridge J. Adolescent patellar instability: current concepts review. Bone Joint J 2017;99-B:159-170. [DOI] [PubMed] [Google Scholar]
- 33. Feller JA. Distal realignment (tibial tuberosity transfer). Sports Med Arthrosc Rev 2012;20:152-161. [DOI] [PubMed] [Google Scholar]
- 34. Bollier M, Fulkerson JP. The role of trochlear dysplasia in patellofemoral instability. J Am Acad Orthop Surg 2011;19:8-16. [DOI] [PubMed] [Google Scholar]
- 35. Lewallen LW, McIntosh AL, Dahm DL. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med 2013;41:575-581. [DOI] [PubMed] [Google Scholar]
- 36. Nelitz M, Dreyhaupt J, Lippacher S. Combined trochleoplasty and medial patellofemoral ligament reconstruction for recurrent patellar dislocations in severe trochlear dysplasia: a minimum 2-year follow-up study. Am J Sports Med 2013;41:1005-1012. [DOI] [PubMed] [Google Scholar]
- 37. Simon AE, Uddin SFG. Sports team participation among US high school girls, 1999-2015. Clin Pediatr (Phila) 2018;57:637-644. [DOI] [PubMed] [Google Scholar]
- 38. Stracciolini A, Casciano R, Levey Friedman H, et al. Pediatric sports injuries: a comparison of males versus females. Am J Sports Med 2014;42:965-972. [DOI] [PubMed] [Google Scholar]
- 39. Luhmann SJ. Acute traumatic knee effusions in children and adolescents. J Pediatr Orthop 2003;23:199-202. [PubMed] [Google Scholar]
- 40. Liu JN, Steinhaus ME, Kalbian IL, et al. Patellar instability management: a survey of the International Patellofemoral Study Group. Am J Sports Med 2018;46:3299-3306. [DOI] [PubMed] [Google Scholar]