Abstract
Background
In this systematic review, our objective was to assess inflammatory bowel disease (IBD) patient preferences and perspectives relating to their disease diagnosis, treatment, knowledge needs and telemedicine.
Methods
This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Four databases and conference proceedings were searched between January 1, 1980, and May 1, 2020. The methodological quality of the included studies was assessed using the Standards for reporting qualitative research checklist.
Results
Our search identified 240 citations and 52 studies met the inclusion criteria. The major expectations of the patients are symptomatic and pain control, quality of life and normal endoscopy. Patients’ main concerns are access to information and healthcare, and shared decision making. At the time of diagnosis, patients expressed a greater need for knowledge about their IBD, preferentially by their treating gastroenterologist. The main treatment expectations in active disease are efficacy, safety and convenience. Patients are willing to accept relatively high risks of complications from medical therapy to avoid a permanent ostomy and to achieve durable remission. Patients are more interested in disease monitoring, research and development during the time of remission. Telemedicine and self-management with supervised e-health tools are feasible and acceptable amongst patients with IBD.
Conclusion
This systematic review demonstrates that patients with IBD expect more information about their disease process, shared decision making and symptom control. Further research is needed to help align patient and physician expectations in order to improve the quality of care provided to patients with IBD.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10620-021-07025-y.
Keywords: Patient preferences, Patient perspectives, Access, Shared decision making, Telemedicine, Systematic review
Introduction
Inflammatory bowel diseases (IBD), consisting of ulcerative colitis (UC) and Crohn’s disease (CD), are chronic immune-mediated disorders of the gastrointestinal tract that can negatively impact patients’ physical health and quality of life. Those with extraintestinal manifestations (EIM) irrespective of disease activity showed worse quality of life than those without EIM both physically and psychologically [1]. The incidence and prevalence of IBD is increasing worldwide, placing a significant burden on both patients and the health care system [2].
The approach to management of IBD has evolved in the past years with tight and objective disease monitoring to achieve endoscopic remission [3]. This predicts long-term steroid free remission and lower surgical and hospitalization rates [4–7]. Most recently, STRIDE II confirmed STRIDE I long-term targets of clinical remission and endoscopic healing and further added the absence of disability and normal quality of life as long-term targets [8].
Despite the advancement in pharmacological management of IBD, patients may experience loss of response due to reasons such as antibody formation and development of drug-related complications such as serious infections and malignancies requiring discontinuation [9–13]. Therefore, the management of IBD is complex requiring tight control of disease activity, close monitoring to minimize drug-related side effects, expertise in the field and an interdisciplinary holistic approach to patient care [14].
Herein, the chronic relapsing nature of IBD requires a long-term patient-oriented interaction and effective communication between the patient and the physician. This is important to optimize patient involvement in their care and shared decision-making [15]. Patient satisfaction is thought to be an integral part of high quality of care (QoC) yet complex assessment of perceived QoC from the patients’ perspective is scarce [16]. The European Crohn’s and Colitis Organization (ECCO) developed criteria to summarize optimal standards of care in IBD [14]. In order to provide a high QoC delivery, it is essential for medical providers to evaluate patients’ satisfaction and expectations when providing care.
Patient expectations differ at diagnosis, during a flare, remission as well as across different countries [17]. Studies have shown that at diagnosis, patient education and support are important. During treatment, efficacy, rapid improvement of symptoms, medication safety profile, and convenience with simplicity are key. During follow-up, patients considered cancer risk and management of complications as important measures [18–21]. It is imperative to be aware of these different aspects of patient expectations during IBD management in order to provide optimal patient care.
To our knowledge, there has not been any systematic review published on patient perspectives and expectations in IBD during shared decision making. A narrative review by Bewtra et al. [22] explored patient preferences in IBD therapy. In this review, we aimed to assess IBD patient preferences and perspectives during various stages of their disease, specifically, relating to their disease at diagnosis, both during active disease and in remission, longstanding disease treatment, knowledge needs, and telemedicine.
Methods
Data Sources and Search Strategy
This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA). [23] We searched the Cumulative Index to Nursing and Allied Health Literature, Medline, Embase, BIOSIS, and Web of Science between January 1, 1980, and May 1, 2020. Conference proceedings were searched (World Congress of Gastroenterology, American College of Gastroenterology, Canadian Digestive Disease Week, Digestive disease week and United European Gastroenterology Week) between January 1, 1980, and May 1, 2020. We searched study references and review articles and contacted authors for additional data. Abstracts and brief reports were not included. The search strategies for patient perspectives and expectations in IBD are outlined in Table 1. Studies were independently selected by two reviewers (BB and AK); disagreements were resolved by a third reviewer (PLL).
Table 1.
Search string
| Medline search strategy | |
|---|---|
| #1 (Inflammatory Bowel Disease [MeSH] OR Crohn’s disease [MeSH] OR Ulcerative Colitis [MeSH] OR ‘Crohn’s disease’ [ti] OR ‘Ulcerative Colitis’ [ti]), AND #2 (‘patient’ [ti]), AND #3 (‘preference’ [ti] or ‘satisfaction’ [ti] or ‘education’ [ti] or ‘needs’ [ti] or ‘information’ [ti] or ‘expectations’ [ti] or ‘telemedicine’ [ti] or ‘decision making’ [ti] or ‘quality indicator’ [ti]) |
Study Selection
We included studies that investigated adult IBD populations (diagnosis of UC or CD per conventional definitions); specifically, patient perspectives, expectations or preferences at the time of IBD diagnosis, during remission, related to treatment and telemedicine. We excluded studies if: (1) if they were not related to our outcome of interest, (2) were not written in English, and (3) they were only available as an abstract or brief report. We accepted cohort, case–control and cross-sectional studies.
Data Extraction
We used a standardized data extraction form. Variables extracted included, (1) study characteristics—primary author, time period of study, location, study design, measurement tools, (2) patient characteristics—age, gender, IBD subtype (UC or CD), patient population (3) patient perspectives/preferences/expectations at the time of diagnosis, during remission, regarding treatment and telemedicine and (4) covariates and between group variables evaluated.
The methodological quality of the included studies was assessed using the Standards for reporting qualitative research (SRQR) checklist [24]. Studies were scored across four categories: Introduction (four questions), Methods (eleven questions), Results (two questions) and Discussion (four questions) with one point per question in each category (Supplemental Table 1). Study quality was defined as low, moderate and high, based on scores of 0–7, 8–14 and 15–21, respectively. Two reviewers (BB and AK) extracted data and assessed quality independently; disagreements were resolved by a third reviewer (PLL).
Results
Search Results
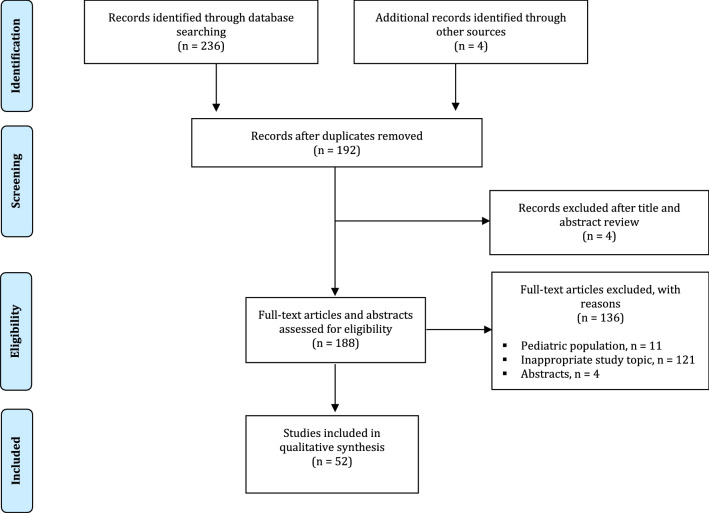
Our search identified 236 citations and fifty-two studies met the inclusion criteria (Fig. 1). The majority of the studies were cross-sectional (43/52). There were three cohort studies, one case–control study and three randomized controlled trials [25–31]. There were two studies that did not state their study design [20, 32]. Twenty-six studies were published in North America, twenty in Europe, four in Asia and two in Oceania. The major expectations of the patients are symptomatic control, pain control, quality of life, and normal endoscopy. Patients’ main concerns are information, access, and shared decision making.
Fig. 1.
Flowchart of study selection
Patient Characteristics
Thirty-five studies included both CD and UC patients. Eleven studies evaluated patients with UC and six studies included only patients with CD.
Patient Perspectives and Expectations at the Time of Diagnosis
There were four studies that evaluated patient perspectives and expectations at the time of diagnosis [33–36]. The conclusion from three of these studies was that patients expressed a greater need for knowledge at the time of diagnosis [34–36]. Table 2 outlines the study characteristics and outcomes. Studies compared variables such as age, sex and severity of disease and information needs at diagnosis varied amongst different patient populations. Patient with more severe, active disease had higher information needs, especially around domains of work-disability, stress-coping and therapy-complications [34]. Patients with a higher level of education than community college had increased desire to participate in self-care [35].
Table 2.
Patient perspectives related to IBD diagnosis
| Author | Study Publication Date | Location | Patient population | IBD | Study size | Female (%) | Variables | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Bernstein [35] | 2011 | Canada | NA | UC + CD | 74 | 53% | Age, sex, diagnosis (UC vs. CD), level of education | 24% of patients reported feeling dissatisfied with the information at the time of diagnosis. Sixty-eight percent preferred information from a medical specialist. Age and diagnosis (CD vs. UC) were not significantly related to desire for information. Desire for participation in self-care was higher among participants with a higher level of education than community college. Sex, age and diagnosis were not significantly associated with desire for self-care |
| Casellas [33] | 2014 | Spain | NA | UC | 8 | 50% | Disease severity | Patients’ main concerns were the delay in diagnosis due to the lack of clinical suspicion by their general practitioner and the delay in obtaining the appropriate diagnostic tests. Patients with moderate versus mild diagnosis are more aware of the need for information due to the impact of their UC |
| Daher [34] | 2019 | Israel | Multi-ethnic | UC + CD | 571 | 46% | Age, sex, diagnosis (UC vs. CD), disease severity | Patients expect more information at the time of diagnosis. Patient with more severe, active disease had higher information needs, especially around domains of work-disability, stress-coping and therapy-complications |
| Lesnovska [36] | 2014 | Sweden | Multi-ethnic | UC + CD | 30 | 53% | None | There was a greater need for knowledge at the time of diagnosis and during relapse. Patients would have preferred a long conversation with their GI specialist at the time of diagnosis |
Patient Perspectives and Expectations Regarding Treatment
There were 18 studies that evaluated patient perspectives and expectations regarding treatment [18, 19, 30, 32, 33, 37–49]. The majority of these studies were conducted in North America (13/18) [18, 19, 32, 37–40, 42–45, 47, 49]. According to the patients’ in multiple studies the most important treatment expectations were related to efficacy, safety and convenience of treatment. [47] There were some differences between CD and UC patients, as UC patients are willing to accept relatively high risks of fatal complications from medical therapy to avoid a permanent ostomy and to achieve durable remission, thus being more efficacy driven [40]. Similarly, CD patients would accept a rare risk of infection or cancer for an increased chance of remission, yet CD patients rated the side effect profile of the medications as very important in their decision making [19, 37, 43, 44]. In contrast, in exchange for improvements from moderate symptoms to remission for the middle-aged patient profile, gastroenterologists were significantly less tolerant than patients of treatment risks of serious infection and lymphoma [44]. An additional factor was the route of administration (intravenous vs. subcutaneous vs. oral) and need for repeated daily dosing [38, 47]. Table 3 outlines the study characteristics and outcomes regarding treatment perspectives and expectations.
Table 3.
Patient perspectives related to IBD treatment
| Author | Study publication date | Location | Patient population | IBD | Study size | Female (%) | Variables | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Almario [37] | 2018 | USA | Non-Hispanic White | UC + CD | 640 | 54% | Age, gender, race/ethnicity, education, marital status, employment status, household income, IBD type, duration, severity | Demographics and IBD characteristics did not predict individual patient preferences, except for IBD type. CD-p reported side effect profile as most important. UC-p were more likely to value therapeutic efficacy |
| Arseneau [32] | 2006 | USA | Caucasian | UC | 48 | 38% | Medical treatment with cyclosporine and/or infliximab, surgical intervention | In the treatment of steroid-refractory UC (defined as the treatment strategy that maximizes a patient’s quality-adjusted life expectancy), 63% of patients maximized their QALYs through medical treatment with infliximab and/or cyclosporine, whereas 37% benefited most from forgoing medical interventions altogether and proceeding directly to total colectomy |
| Boeri [38] | 2019 | USA | NA | UC | 200 | 59% | None | Patients considered symptom control 2.5 times more important than time to symptom improvement. They prefer oral to subcutaneous or intravenous medication administration |
| Bewtra [40] | 2014 | USA | Caucasian | UC | 293 | 57% | None | Patients are willing to accept relatively high risks of fatal complications from medical therapy to avoid a permanent ostomy and to achieve durable remission. Patients view J-pouch surgery, but not permanent ileostomy, as an acceptable therapy for refractory UC where medical therapy is unable to induce remission |
| Bewtra [39] | 2020 | USA | Caucasian | CD | 812 | 75% | Disease duration and severity | Therapy options were strongly influenced by 1) avoidance of active symptoms (61%), 2) avoidance of corticosteroids (25%) and 3) avoidance of risk of cancer, infection or surgery (14%) |
| Casellas [33] | 2014 | Spain | NA | UC | 8 | 50% | None | The main needs of patients related to clinical management of the disease are care on demand and remote care, especially during a flare |
| Casellas [41] | 2016 | Spain | NA | UC | 22 | 32% | Physician versus patient perspective | Patients preferred moderate flare-ups to be followed at the hospital setting rather than in primary care as well as to be informed on aspects, such as diet and impact of UC on their health and lifestyle. Treatment-related efficacy, safety, and improved quality of life were relevant for both patients and physicians. Physicians believed that to reduce pill burden was a crucial aspect to improve patient's satisfaction |
| Gregor [42] | 2018 | Canada | Caucasian | CD + UC | 586 | 48% | Age, sex, education level, presence of symptoms in the past year | Highest ranking attributes included: (1) reducing pain during treatment administration, (2) mucosal healing, and (3) symptom relief. Infusion reactions and risk of hospitalization or surgery were the lowest-ranking attributes. Patient socio-demographics did not affect the rank order of attributes although small differences were observed between asymptomatic and symptomatic patients in the previous year |
| Gray [18] | 2009 | Canada | NA | UC | 100 | 66% | None | Efficacy‐ and safety‐related medication attributes were rated to be more important than those related to dosing regimen (e.g. dosing frequency, number of pills), cost and formulary coverage. When considering a UC medication, patients rated speed of symptom relief and few side effects as the most important factors |
| Hagelund [30] | 2020 | Denmark | NA | UC | 302 | 84% | None | The most important medical treatment attribute was efficacy within eight weeks. Additionally, respondents stated a preference for avoiding taking steroids, for fast onset of effect and for oral formulations |
| Hazlewood [19] | 2020 | Canada | NA | CD | 155 | 68% | None | Patients would accept a rare risk of infection or cancer for a 14% absolute increased chance of remission. All biologic treatments were preferred to azathioprine and methotrexate, based on the balance of benefits and harms. Adalimumab was preferred by 53% of patients, who were motivated by efficacy, and vedolizumab was preferred by 30% who preferred to avoid risks |
| Johnson [43] | 2007 | USA | NA | CD | 580 | 68% | Disease duration and severity | Daily symptom severity was the most important factor in treatment preferences. Patients were willing to accept elevated SAE in exchange for clinical efficacy. The mean acceptable risk was similar across the 3 SAEs (PML, serious infections and lymphoma). Patients with more severe CD are less tolerant of SAE risks than are patients with less severe CD. Patients who have been diagnosed with CD for more than 8 years are generally willing to accept a higher risk of SAEs than patients with a more recent CD diagnosis |
| Johnson [44] | 2010 | USA | NA | CD | 580 | 68% | Age | Gastroenterologists and patients disagreed about how much risk is tolerable for improvements in efficacy. In exchange for improvements from severe to moderate symptoms for the middle-aged patient profile, gastroenterologists were significantly more tolerant than patients of treatment risks of PML and serious infection but not lymphoma. In contrast, in exchange for improvements from moderate symptoms to remission for the same patient profile, patients were significantly more tolerant than gastroenterologists of treatment risks for serious infection and lymphoma but not PML |
| Lai [45] | 2019 | USA | Caucasian | CD + UC | 20 | 50% | None | The main drivers of treatment decision‐making were patients’ perceived clinical status and disease severity, the quality of patient–provider relationships, patients’ knowledge, attitude and beliefs about their treatment, and the social stigma and isolation experienced by IBD patients |
| Lichtenstein [49] | 2012 | USA | NA | CD | 252 | 72% | Medical treatment | The three attributes of greatest importance for patients’ biologic preference were greater proportion of patients achieving lasting remission, decreased frequency of medication administration, and higher proportion of patients responding in 2 weeks |
| Peake [46] | 2011 | UK | NA | CD | 36 | NA | None | The majority of patients preferred adalimumab to infliximab. Reasons included; ‘‘like to give or receive their treatment at home,’’ ‘‘more compatible with lifestyle and/or occupation,’’ and ‘‘difficulties/discomfort obtaining intravenous access’’ |
| Peyrin-Biroulet [48] | 2016 | Europe | NA | UC | 256 | 41% | None | 48% of patients were dissatisfied with their current treatment. Effectiveness, long lasting action, rapid start of action, and fewer side effects were the attributes more frequently considered important or very important |
UC-p ulcerative colitis patients, CD-p Crohn’s disease patients, 5-ASA 5-Aminosalicylate acid, anti-TNF anti-tumor necrosis factor, PML progressive multifocal leukoencephalopathy, SAE serious adverse effects
Patient Perspectives and Expectations During Remission
There were nine studies investigating IBD patient perspectives while in remission (Table 4) [15, 25, 29, 38, 50–54]. Overall, patients are more interested in drug monitoring, access to healthcare as well as research and development during remission [52]. Patients prefer non-invasive stool testing such as fecal calprotectin for monitoring disease activity to colonoscopy as long as the stool test is accurate. [50]. The paper by Morishige et al. [15] demonstrated that patients valued shared decision making concerning their treatment. Patients expected good coordination between specialists and family physicians [29]. Patients considered symptom control more important than the time to symptom control [38]. They also preferred improvement in the quality of life as an important treatment objective over a completely normal colonoscopy [25].
Table 4.
IBD patient perspectives and expectations during remission
| Author | Study publication date | Location | Population | IBD | Study size | Female (%) | Variables | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Barsky [50] | 2020 | USA | N/A | CD + UC | 100 | 54% | None | When choosing between stool-based fecal calprotectin testing and colonoscopy for disease activity assessments, most patients were willing to choose stool-based testing as long as the test was accurate |
| Boeri [38] | 2019 | USA | N/A | UC | 200 | 59% | Physician versus patient preferences | Patients considered symptom control 2.5 times as important as time to symptom improvement and 5-year risk of malignancy almost as important as long-term symptom control. They preferred oral to subcutaneous or intravenous administration. For physicians, symptom control was the most important attribute and was five times as important as the risk of malignancy |
| Casellas [25] | 2017 | Italy | N/A | CD + UC | 117 | 66% | None | The most important treatment objectives were: improving quality of life and completely resolving symptoms. Only 12.8% of patients indicated having a completely normal colonoscopy as a preferred objective |
| Morishige [15] | 2017 | Japan | Japanese | CD + UC | 1035 | 35% | Marital status, comorbidities, surgical history, biologic treatment, and type of hospital | Majority of patients felt that SDM (shared decision making) was very important. There were significant differences between those patients that found it very important to be involved in the decision making concerning their treatment and those that did not. These differences include surgical history or various comorbidities, including dyslipidemia and COPD/asthma. Patients receiving a biologic agent significantly favored SDM in comparison to non-biologic users. Factors affecting UC patients were marital status, diabetes, surgical history, biologic treatment, and type of hospital; in comparison, preferences in CD patients were affected only by type of hospitals |
| Noiseux [51] | 2019 | Canada | N/A | CD + UC | 210 | 81% | None | 78.9% of patients reported a low level of comfort for blood tests. For colonoscopies, 59.7% of the patients reported a high level of concern upon receiving the results. Information about the possibility of false positives or negatives was the least shared with patients |
| Pittet [29] | 2018 | Switzerland | N/A | CD + UC | 1094 | 54% | Gender, primary language, age | Patients expect being good coordination between general practitioners and specialists and information on treatment adverse events. Women had overall higher levels of expectations than men |
| Pittet [52] | 2016 | Switzerland | N/A | CD + UC | 728 | 53% | Gender, primary language, age | Majority had concerns on research and developments; they also searched for information linked to daily disease management |
| Vasudevan [53] | 2013 | Australia | N/A | CD + UC | 187 | 52% | Age, gender, IBD diagnosis (CD vs. UC), disease duration, CRP (≥ 5 mg/L), concurrent biologic therapy | In CD-p, post-resection and longer IBD duration each had lower domain Quality Index (QI) of patient satisfaction of quality of care than their respective counterparts, whereas those on concurrent anti-TNF therapy gave higher QI scores |
| Vaucher [54] | 2016 | Switzerland | N/A | CD + UC | 14 | NA | IBD diagnosis (CD vs. UC), GI physicians versus patients | UC-p agreed more often with gastroenterologists' treatment choices than CD-p. CD-p often considered 5-ASA as a placebo. UC-p saw topical 5-ASA as a temporary solution, neither comfortable nor practical when professionally active. Azathioprine was considered as the treatment for which the risks versus benefits were perceived as the highest. The main risk perceived by patients on anti-TNFs was a potential loss of response |
IBD Patient Information Needs
There were fourteen studies that evaluated information needs amongst patients with IBD (Table 5). Seven studies concluded that patients with IBD were dissatisfied with the information that they received, specifically related to treatment side effect profile, cancer risk and research trials [35, 36, 55–58]. Four studies demonstrated that patients prefer gastroenterologists to be their primary source of information [35, 55, 56, 59]. Information needs varied across variables such as age and disease severity. Patient with more severe, active disease had higher information needs, especially around domains of work-disability, stress-coping and therapy-complications.
Table 5.
IBD Patient information needs
| Author | Study publication Date | Location | Population | IBD | Study size | Female (%) | Variables | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Bernstein [35] | 2011 | Canada | N/A | CD + UC | 74 | 53% | Age, sex, diagnosis (UC vs. CD), level of education | 24% reported feeling dissatisfied with the information they were given at the time of their diagnosis. Sixty-eight percent indicated that they preferred information from a medical specialist |
| Catalan-Serra [57] | 2014 | Spain | N/A | CD + UC | 271 | 61% | Age, sex, diagnosis (UC vs. CD), level of education, previous surgeries, duration of disease | Patients want additional information on treatment (medical and surgical), clinical manifestations, cancer, and mortality risks. Patients feel poorly informed about their social and work rights, risks of cancer and death, and research trials |
| Cullen [55] | 2010 | Ireland | N/A | CD + UC | 100 | 49% | Gender, duration of disease, 5 disease type (CD vs. UC), disease activity, history of adverse events and current medications | 36%, 53% and 79% reported no knowledge regarding safety of corticosteroids, immunomodulators and biologics, respectively. Most patients wish to be informed of all medication side-effects, no matter how rare, and ranked their gastroenterologist as their primary information source |
| Daher [34] | 2019 | Israel | Multi-ethnic | CD + UC | 571 | 46% | Age, sex, diagnosis (UC vs. CD), disease severity | Patient with more severe, active disease had higher information needs, especially around domains of work-disability, stress-coping and therapy-complications. Patients diagnosed after age 50 ranked higher information needs regarding long term complications, nutrition, managing symptoms, therapy-complications |
| Khan [58] | 2016 | USA | Caucasian | CD + UC | 15 | 67% | None | Patients cited a doctor–patient communication divide where there is a continued lack of goal setting when discussing treatments and a lack of objectivity in disease control |
| Lesnovska [36] | 2014 | Sweden | N/A | CD + UC | 30 | 53% | None | There was a greater need for knowledge at the time of diagnosis, during relapse and when the patients had lived with the disease for a long time and realized that they had received insufficient information at diagnosis. They would have preferred a long conversation with their physician at diagnosis |
| McDermott [67] | 2018 | Ireland | N/A | CD + UC | 322 | 51% | Age, sex, diagnosis (UC vs. CD), level of education, duration of disease | Patients were most keen to receive education on medications, ‘what to expect in future’, living with IBD and diet |
| Politi [59] | 2008 | Europe, Israel | N/A | CD + UC | 917 | 49% | Sex, age, diagnosis, educational level, marital status and geographical area | Majority were curious about new fields of research, medical treatment, risks and complications. Sixty-six percent designated the specialist as their primary source of information |
| Probert [20] | 1991 | UK | N/A | CD + UC | 70 | NA | N/A | The majority (75%) of patients with CD and UC wanted to know more about their diseases, with a preference for counseling by hospital doctors or specialty trained nurses in both patient groups |
| Reich [68] | 2019 | USA | Caucasian | CD + UC | 1960 | 75% | Sex, age, remission status, education, IBD type, IBD medication | Patients expressed a substantial interest in using social media to aid in disease management. Use was higher in younger patients, females, and patients with active disease |
| Reich [69] | 2016 | USA | Caucasian | CD + UC | 118 | 56% | Sex, age, remission status, education, IBD type, IBD medication, geographical area | Patients who frequently use social media are highly interested in using social media in the management of their IBD. Most were interested in receiving information from their gastroenterologist and other patient-related organizations through social media. Most are unsure of the quality of IBD information posted on social media |
| Politi [59] | 2008 | Europe, Israel | N/A | CD + UC | 917 | 49% | Sex, age, diagnosis, educational level, marital status and geographical area | Majority were curious about new fields of research, medical treatment, risks and complications. Sixty-six percent designated the specialist as their primary source of information |
| Wong [56] | 2012 | Canada | N/A | CD + UC | 271 | 61% | Sex, age, remission status, education, IBD type | At diagnosis, 80% rated as ‘very important’ information about common symptoms of IBD, possible complications, long-term prognosis, medication side effects, self-management of symptoms and when to involve the doctor. Only 10–36% believed they received the right amount of information about these issues. Dietary guidance was also regarded as important by 80–89%, yet only 8–16% received the correct amount of information. Regarding current needs, a large proportion believed it would be very helpful to have more information about long-term prognosis (66%) and diet (60–68%). The following information sources were regarded as very acceptable: medical specialist (81%); brochure (79%); family doctor (64%); and website (64%), with 51% ranking the medical specialist as the first choice |
| Yoo [70] | 2015 | South Korea | Asian | CD + UC | 313 | 40% | Sex, age, education, IBD type, IBD duration, previous surgeries, employment status | CD-p obtained a higher mean knowledge score, significantly higher scores about complications and patients' information needs than UC-p. Topics of information needed were disease, medication, and diagnosis/operations. CD-p wanted more information than UC-p about medications used for treatment, daily life, and pregnancy |
UC-p ulcerative colitis patients, CD-p Crohn’s disease patients
IBD and Telemedicine
There were eight studies investigating telemedicine in IBD (Table 6). Overall, telemedicine (web or text message based) is acceptable and feasible amongst patients with IBD [26–28, 60, 61]. Telemedicine reduced the number of outpatient visits. In the era of COVID-19, telemedicine has become part of patient expectations. However, compared to conventional management, two studies demonstrated no reduction in the frequency of hospitalizations, whereas two studies showed that there was a reduction in hospitalizations [26–28, 31].
Table 6.
IBD and telemedicine
| Author | Study Publication Date | Location | Population | IBD | Study size | Female (%) | Variables | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Bilgrami [71] | 2020 | USA | Caucasian | CD + UC | 222 | 59% | Age, sex, race, insurance status, IBD type disease duration and activity, study site, baseline knowledge score | Changes in self-efficacy scores were not significantly different between control and experimental groups. Patient activation scores were significantly different between standard care and the TELE-IBD every-other-week group only |
| Cross [31] | 2019 | USA | Caucasian | CD + UC | 348 | 57% | Disease activity, steroid use | Disease activity and QoL, although improved in all participants (standard of care vs. text weekly vs. texts every other week), were not improved further through use of the TELE-IBD system. TELE-IBD participants experienced a decrease in hospitalizations with an associated increase in non-invasive diagnostic tests, telephone calls and electronic encounters |
| De Jong [27] | 2017 | Netherlands | NA | CD + UC | 909 | 58% | Medical center, IBD type, medication (immunosuppressive drugs or biological therapy), age, sex, disease duration, disease activity at baseline, smoking, educational level | The mean number of outpatient visits and hospitalizations were significantly lower in the telemedicine group. At 12 months, both groups reported high mean patient-reported quality of care scores. The mean numbers of flares, corticosteroid courses, emergency visits, and surgeries did not differ between groups |
| Elkjaer [28] | 2010 | Denmark, Ireland | NA | UC | 333 | 50% | None | 88% of patients randomized to receive web-based disease education and self-treatment preferred using the new approach. Adherence to 4 weeks of acute treatment was increased by 31% in Denmark and 44% in Ireland compared to the control groups. In Denmark IBD knowledge and quality of life were significantly improved in web patients. Median relapse duration was lower in the web versus the control group. The number of acute and routine visits to the outpatient clinic was lower in the web than in the control group, resulting in a saving of 189 euro/patient/year. No difference in the relapse frequency, hospitalization, surgery or adverse events |
| Chudy-Onwugaje [72] | 2018 | USA | Caucasian | CD + UC | 193 | 54% | Age, race, sex, health insurance, smoking, IBD type and behavior, age at diagnosis, medication use, inflammatory markers and disease activity scores | Patients with depressive symptoms have high adherence to IBD-specific self-testing when managed in a text messaging-based telemedicine program, specifically in those that were 40 years and younger |
| Li [26] | 2017 | USA | NA | CD + UC | 53 | 69% | None | Over 90% felt the telemedicine visits were of adequate duration and their physician understood their disease state during the visit. Over 75% reported they clearly understood the follow-up plan after the visit. Seventy-seven percent preferred to continue to use telemedicine for follow-up. There were no detectable differences in clinical outcomes before and after telemedicine visits, including current steroid use, biologic exposure or health care utilization |
| McCombie [61] | 2014 | New Zealand | NA | CD + UC | 102 | 48% | Age, sex, time since diagnosis | Patients were more likely to participate in a computer based than face-to-face intervention. Younger females had a significantly higher acceptability of a computerized intervention than older females. Disease duration was not associated with willingness to participate in a computerized intervention |
| Quinn [60] | 2019 | USA | Caucasian | CD + UC | 259 | 47% | None | Patients identified clear benefits of remote monitoring via text messages, including obtaining a better understanding of the disease process, monitoring their symptoms, and feeling connected to their health care provider. They prefer a flexible follow-up system that is personalized, including education messages that can be targeted to individual patients and decreased repetition |
Methodological Quality
Overall, the studies received a high score for methodological quality. Using the SRQR checklist, the average score amongst studies was 17.7. The majority of studies lost points for not including funding sources, conflicts of interest and ethical issues pertaining to human subjects.
Discussion
The results of this systematic review demonstrate that patients with IBD expect overall access, symptom control and more information about their disease and treatment process preferentially by the specialist and to partner with us by shared decision-making. To our knowledge, this is the first systematic review to assess patient perspectives and expectations in IBD during shared decision making.
At the time of diagnosis, patients expected a greater need for knowledge of their condition. The preferred source of information is the treating gastroenterologist [56]. A study by Lesnovska et al. showed that there was a greater need for knowledge at the time of diagnosis and during relapse. Patients would have preferred a long conversation with their gastroenterologist at the time of their diagnosis in order to better understand their disease [36]. Pittet et al. [52] showed that nearly half of patients sought for information, regardless of the disease stage and a quarter of them of them were dissatisfied with information received at the time of first symptoms. Therefore, it is important for patients to be actively involved in the decision-making process from the start [15, 62].
In active disease patients are mainly concerned about their therapy, efficacy, safety, convenience and access [37, 47, 63]. In terms of patient perspectives and expectations during treatment, patients viewed efficacy of therapy to be most important. During flares, 43% were concerned about drugs and therapies in a large study by Pittet et al. [52]. A study by Hazlewood et al. [19] demonstrated that patients would accept a rare risk of infection or cancer for a 14% absolute increase chance of remission Patients were willing to accept elevated serious adverse effects (serious infections, lymphoma) in exchange for clinical efficacy [43]. Convenience (doctor visits, fewer pills) was the third most important aspect of disease management after efficacy and safety. An equally important point is access. In a recent study by our group on assessing patients’ reflection on the quality of care this was highlighted as one of the problem areas [37, 47, 63]. Of note, the availability of rapid access option by email, phone to contact the IBD center with a rapid response has also shown to significantly decrease the burden for the patients with lesser utilization of the emergency units and decreasing costs [37, 47, 63, 64].
Furthermore, Casellas et al. showed that the most important treatment objective from the patients’ perspective was improving quality of life (40% of patients) followed by completely resolving symptoms (33% of patients). Only 12% of patients considered having a completely normal colonoscopy as a preferred objective [25]. Gregor et al. demonstrated that reducing pain during administration, mucosal healing, and symptom relief were the highest-ranking attributes for out of pocket willing-ness to pay. Conversely, infusion reactions and risk of hospitalization or surgery were the lowest-ranking attributes [42]. Patients preferred oral to subcutaneous or intravenous administration (relative importance, 0.47 vs. 0.11 and 0.18, respectively) [38]. When comparing anti TNFs, the majority of patients preferred subcutaneous route to intravenous with ease of use and time required for therapy playing an important role for selection [65]. Interestingly, a study by Almario et al. showed that there was no difference between biologic therapy choice when comparing UC versus CD but UC patients valued therapeutic efficacy more, whereas CD patients valued side effect profile [37]. It is important to be aware of these discrepancies to help with the decision-making process during active disease.
During remission, patients viewed safety, long-term outcomes and novelties in research and development to be important. Boeri et al. demonstrated that patients considered symptom control to be 2.5 times more important than time to symptom improvement and a 5-years risk of malignancy almost as important as long-term symptom control [38]. Nevertheless, for physicians, symptom control was the most important attribute and was five times as important as the risk of malignancy [38]. Furthermore, many patients are concerned about IBD research and development of their illness during remission [52].
Regarding information needs, patients preferred to receive the primary source of information from a gastroenterologist [35, 55]. Pittet et al. [29] looked at patient expectations in IBD and demonstrated that the two most important included good coordination between general practitioners and specialists and information on treatment adverse events. Women had higher level of expectations than men. Other expectations were linked to information, communication, daily care, and disease recognition. In a large study of 728 patients, Pittet et al. [52] showed that information seeking increased in those with active disease and for CD with high levels of perceived stress.
Nevertheless, patients and physicians’ perceptions in IBD may differ and that may hinder high quality care. For instance, physicians estimated the severity of IBD to be lower than patients’ reported disease severity and felt that the disease had lower impact to lead a normal life compared to patients [66]. A study by Casellas et al. showed that only 12.8% of patients indicated having a completely normal colonoscopy as a preferred objective [25]. This is different from physician treatment goals of attaining endoscopic healing. A study by Boeri et al. showed that both patients and physicians considered long-term symptom control the most important attribute relative to others; however, patients were more concerned regarding the risk of malignancy compared to physicians [38].
Amidst this pandemic era, telemedicine has become an alternative option of managing patients with IBD when access to care may be difficult. Telemedicine has shown to be feasible and acceptable in patients with IBD and reduced the number of outpatient visits and consequently healthcare expenditure [27, 28]. IBD and telemedicine existed even before the pandemic era. A paper by Quinn et al., showed clear benefits of remote monitoring by text messages including obtaining a better understanding of the disease process, monitoring their symptoms and feeling connected to the health care provider. It also provided a flexible follow up system that is personalized [60]. Most patients are satisfied with telemedicine and this has helped them to be more involved in their own management. Patients have been able to do their self-management at home and contact the clinic once appropriate. A study by Elkjaer et al. [28] showed that 88% of web patients preferred adhering to either a web-group receiving disease-specific education and self-treatment versus usual care over a 12 months period. In web patients, IBD knowledge, adherence to treatment and QoL improved. Median relapse duration, number of acute and routine visits to the outpatient clinic was lower in the web than in the control group, resulting in a saving of healthcare expenditure [28]. This all reinforces the importance of shared decision-making and self-management. We believe patient expectations would change in the twenty-first century with more emphasis on virtual clinics, telemedicine, patient involvement in their own care including self-monitoring and shared decision-making regarding treatment.
The strength of the present study is focused on harmonized care practices with a high emphasis on delivering quality care to patients with IBD. This systematic review serves as a repertoire for what is available around this important topic and how we can build on shared decision-making in IBD to improve patient care. This systematic review further serves as a comprehensive measure of quality indicators in IBD. The limitation includes that most of the studies discovered in the systematic review are descriptive in nature; nevertheless this is expected when describing quality indicators in IBD. This review includes papers published internationally, but there is no discussion of how differences in healthcare practices across countries (payment, average time with the physician, whether multidisciplinary care is common) may impact findings.
In conclusion, this systematic review demonstrates the importance of patient expectations and perspectives in inflammatory bowel disease. Involving your patient early on with shared decision-making is important to provide optimal patient care despite the misalignment between physician and patient perspectives. Tracking and optimizing quality indicators as well optimizing access to IBD care and self-management are important for developing a model for shared decision-making in IBD. Further research is needed to align patient and physician expectations in order to improve patient care.
Supplementary Information
Below is the link to the electronic supplementary material.
Author’s contributions
AA and BB were involved in data collection and methodological quality assessment. AA, BB and P.L.L were involved in manuscript writing. T.B, W.A, P.L.L and M.A were involved in manuscript editing. P.L.L was involved in study design.
Funding
None.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
5/18/2021
The first name and surname of the first author, 'Alex Al Khoury' has been corrected (First name: Alex; Surname: Al Khoury).
Contributor Information
Alex Al Khoury, Email: alexkhoury88@gmail.com.
Bhairavi Balram, Email: balram@ualberta.ca.
Talat Bessissow, Email: talat.bessissow@gmail.com.
Waqqas Afif, Email: waqqas.afif@mcgill.ca.
Lorant Gonczi, Email: lorantgonczi@gmail.com.
Maria Abreu, Email: mabreu1@med.miami.edu.
Peter L. Lakatos, Email: Peter.Lakatos@muhc.mcgill.ca, Email: peter.lakatos@mcgill.ca, Email: kislakpet99@gmail.com
References
- 1.Barreiro-de Acosta M, et al. P639 Influence of extraintestinal manifestations in health-related quality of life in inflammatory bowel disease patients. J Crohn's and Colitis. 2013;7(Supplement_1):S266–S267. doi: 10.1016/S1873-9946(13)60660-1. [DOI] [Google Scholar]
- 2.Ng SC, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2018;390(10114):2769–2778. doi: 10.1016/S0140-6736(17)32448-0. [DOI] [PubMed] [Google Scholar]
- 3.Colombel JF, et al. Effect of tight control management on Crohn's disease (CALM): a multicentre, randomised, controlled phase 3 trial. Lancet. 2018;390(10114):2779–2789. doi: 10.1016/S0140-6736(17)32641-7. [DOI] [PubMed] [Google Scholar]
- 4.Colombel JF, et al. Early mucosal healing with infliximab is associated with improved long-term clinical outcomes in ulcerative colitis. Gastroenterology. 2011;141(4):1194–1201. doi: 10.1053/j.gastro.2011.06.054. [DOI] [PubMed] [Google Scholar]
- 5.Frøslie KF, et al. Mucosal healing in inflammatory bowel disease: results from a Norwegian population-based cohort. Gastroenterology. 2007;133(2):412–422. doi: 10.1053/j.gastro.2007.05.051. [DOI] [PubMed] [Google Scholar]
- 6.Shah SC, et al. Mucosal healing is associated with improved long-term outcomes of patients with ulcerative colitis: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2016;14(9):1245–1255.e8. doi: 10.1016/j.cgh.2016.01.015. [DOI] [PubMed] [Google Scholar]
- 7.Shah SC, et al. Systematic review with meta-analysis: mucosal healing is associated with improved long-term outcomes in Crohn's disease. Aliment Pharmacol Ther. 2016;43(3):317–333. doi: 10.1111/apt.13475. [DOI] [PubMed] [Google Scholar]
- 8.Turner D et al. STRIDE-II: An Update on the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) Initiative of the International Organization for the Study of IBD (IOIBD): Determining Therapeutic Goals for Treat-to-Target strategies in IBD. Gastroenterology, 2020. [DOI] [PubMed]
- 9.Danese S, et al. Unmet medical needs in ulcerative colitis: an expert group consensus. Dig Dis. 2019;37(4):266–283. doi: 10.1159/000496739. [DOI] [PubMed] [Google Scholar]
- 10.Hindryckx P, et al. Incidence, prevention and management of anti-drug antibodies against therapeutic antibodies in inflammatory bowel disease: a practical overview. Drugs. 2017;77(4):363–377. doi: 10.1007/s40265-017-0693-5. [DOI] [PubMed] [Google Scholar]
- 11.Moss AC, Brinks V, Carpenter JF. Review article: immunogenicity of anti-TNF biologics in IBD - the role of patient, product and prescriber factors. Aliment Pharmacol Ther. 2013;38(10):1188–1197. doi: 10.1111/apt.12507. [DOI] [PubMed] [Google Scholar]
- 12.Rutgeerts P, et al. Efficacy of ustekinumab for inducing endoscopic healing in patients with Crohn's disease. Gastroenterology. 2018;155(4):1045–1058. doi: 10.1053/j.gastro.2018.06.035. [DOI] [PubMed] [Google Scholar]
- 13.D'Amico F et al. Tofacitinib in the treatment of ulcerative colitis: efficacy and safety from clinical trials to real-world experience. Therap Adv Gastroenterol, 2019. 12. [DOI] [PMC free article] [PubMed]
- 14.Fiorino G, et al. Quality of care standards in inflammatory bowel diseases: a European Crohn's and colitis organisation [ECCO] position paper. J Crohns Colitis. 2020;14(8):1037–1048. doi: 10.1093/ecco-jcc/jjaa023. [DOI] [PubMed] [Google Scholar]
- 15.Morishige R, et al. Preferences regarding shared decision-making in Japanese inflammatory bowel disease patients. Adv Therapy. 2017;33(12):2242–2256. doi: 10.1007/s12325-016-0436-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bitton A, et al. Selection of quality Indicators in IBD: integrating physician and patient perspectives. Inflammatory Bowel Diseases. 2019;25(2):403–409. doi: 10.1093/ibd/izy259. [DOI] [PubMed] [Google Scholar]
- 17.Hodgkins P, et al. Patient preferences for first-line oral treatment for mild-to-moderate ulcerative colitis: a discrete-choice experiment. The patient. 2012;5(1):33–44. doi: 10.2165/11595390-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 18.Gray JR, Leung E, Scales J. Treatment of ulcerative colitis from the patient's perspective: a survey of preferences and satisfaction with therapy. Aliment Pharmacol Ther. 2009;29(10):1114–1120. doi: 10.1111/j.1365-2036.2009.03972.x. [DOI] [PubMed] [Google Scholar]
- 19.Hazlewood GS, et al. Patient preferences for maintenance therapy in Crohn's disease: a discrete-choice experiment. PloS one. 2020;15(1):e0227635. doi: 10.1371/journal.pone.0227635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Probert CS, Mayberry JF. Inflammatory bowel disease: patients' expectations in the 1990s. J R Soc Med. 1991;84(3):131–132. doi: 10.1177/014107689108400305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Keil R, et al. Adherence, risk factors of non-adherence and patient's preferred treatment strategy of mesalazine in ulcerative colitis: multicentric observational study. Scand J Gastroenterol. 2018;53(4):459–465. doi: 10.1080/00365521.2018.1451915. [DOI] [PubMed] [Google Scholar]
- 22.Bewtra M, Johnson FR. Assessing patient preferences for treatment options and process of care in inflammatory bowel disease: a critical review of quantitative data. The patient. 2013;6(4):241–255. doi: 10.1007/s40271-013-0031-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moher D, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Int Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 24.O'Brien BC, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 25.Casellas F, et al. Patient preferences for inflammatory bowel disease treatment objectives. Digest Liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study Liver. 2017;49(2):152–156. doi: 10.1016/j.dld.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 26.Li SX, et al. Delivering high value inflammatory bowel disease care through telemedicine visits. Inflamm Bowel Dis. 2017;23(10):1678–1681. doi: 10.1097/MIB.0000000000001210. [DOI] [PubMed] [Google Scholar]
- 27.de Jong MJ, et al. Telemedicine for management of inflammatory bowel disease (myIBDcoach): a pragmatic, multicentre, randomised controlled trial. Lancet. 2017;390(10098):959–968. doi: 10.1016/S0140-6736(17)31327-2. [DOI] [PubMed] [Google Scholar]
- 28.Elkjaer M, et al. E-health empowers patients with ulcerative colitis: a randomised controlled trial of the web-guided 'Constant-care' approach. Gut. 2010;59(12):1652–1661. doi: 10.1136/gut.2010.220160. [DOI] [PubMed] [Google Scholar]
- 29.Pittet V, et al. Patient-reported healthcare expectations in inflammatory bowel diseases. PloS one. 2018;13(5):e0197351. doi: 10.1371/journal.pone.0197351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hagelund LM, Elkjær Stallknecht S, Jensen HH, Quality of life and patient preferences among Danish patients with ulcerative colitis - results from a survey study.Curr Med Res Opin 2020:1–9. [DOI] [PubMed]
- 31.Cross RK, et al. A randomized controlled trial of telemedicine for patients with inflammatory bowel disease (TELE-IBD) Am J Gastroenterol. 2019;114(3):472–482. doi: 10.1038/s41395-018-0272-8. [DOI] [PubMed] [Google Scholar]
- 32.Arseneau KO, et al. Do patient preferences influence decisions on treatment for patients with steroid-refractory ulcerative colitis? Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2006;4(9):1135–1142. doi: 10.1016/j.cgh.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 33.Casellas F, et al. Patients' perceptions, attitudes, and experiences about the management of mild-to-moderate ulcerative colitis. J Crohns Colitis. 2014;8(9):1097–1107. doi: 10.1016/j.crohns.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 34.Daher S, et al. Inflammatory bowel disease patient profiles are related to specific information needs: A nationwide survey. World J Gastroenterol. 2019;25(30):4246–4260. doi: 10.3748/wjg.v25.i30.4246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bernstein KI, et al. Information needs and preferences of recently diagnosed patients with inflammatory bowel disease. Inflamm Bowel Dis. 2011;17(2):590–598. doi: 10.1002/ibd.21363. [DOI] [PubMed] [Google Scholar]
- 36.Lesnovska KP, et al. What do patients need to know? Living with inflammatory bowel disease. J Clin Nurs. 2014;23(11–12):1718–1725. doi: 10.1111/jocn.12321. [DOI] [PubMed] [Google Scholar]
- 37.Almario CV, et al. Optimizing selection of biologics in inflammatory bowel disease: development of an online patient decision aid using conjoint analysis. Am J Gastroenterol. 2018;113(1):58–71. doi: 10.1038/ajg.2017.470. [DOI] [PubMed] [Google Scholar]
- 38.Boeri M, et al. Patient and physician preferences for ulcerative colitis treatments in the United States. Clin Exp Gastroenterol. 2019;12:263–278. doi: 10.2147/CEG.S206970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bewtra M, et al. Variation among patients With Crohn's disease in benefit vs risk preferences and remission time equivalents. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2020;18(2):406. doi: 10.1016/j.cgh.2019.05.010. [DOI] [PubMed] [Google Scholar]
- 40.Bewtra M, et al. Patient preferences for surgical versus medical therapy for ulcerative colitis. Inflamm Bowel Dis. 2014;20(1):103–114. doi: 10.1097/01.MIB.0000437498.14804.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Casellas F, Ginard D, Riestra S. Patient satisfaction in the management of mild-to-moderate ulcerative colitis: Results of a Delphi study among patients and physicians. Digest Liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study Liver. 2016;48(10):1172–1179. doi: 10.1016/j.dld.2016.06.036. [DOI] [PubMed] [Google Scholar]
- 42.Gregor JC, et al. Inflammatory bowel disease patients prioritize mucosal healing, symptom control, and pain when choosing therapies: results of a prospective cross-sectional willingness-to-pay study. Patient Prefer Adherence. 2018;12:505–513. doi: 10.2147/PPA.S152872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Johnson FR, et al. Crohn's disease patients' risk-benefit preferences: serious adverse event risks versus treatment efficacy. Gastroenterology. 2007;133(3):769–779. doi: 10.1053/j.gastro.2007.04.075. [DOI] [PubMed] [Google Scholar]
- 44.Johnson FR, et al. Are gastroenterologists less tolerant of treatment risks than patients? Benefit-risk preferences in Crohn's disease management. J Manage Care Pharm JMCP. 2010;16(8):616–628. doi: 10.18553/jmcp.2010.16.8.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lai C, et al. Patient decision-making in severe inflammatory bowel disease: the need for improved communication of treatment options and preferences. Colorectal Dis Off J Assoc Coloproctol Great Brit Ireland. 2019;21(12):1406–1414. doi: 10.1111/codi.14759. [DOI] [PubMed] [Google Scholar]
- 46.Peake STC, et al. Patient preference in choosing biological therapy in Crohn's disease. Inflamm Bowel Dis. 2011;17(7):E79. doi: 10.1002/ibd.21767. [DOI] [PubMed] [Google Scholar]
- 47.Loftus EV., Jr A practical perspective on ulcerative colitis: patients' needs from aminosalicylate therapies. Inflamm Bowel Dis. 2006;12(12):1107–1113. doi: 10.1097/01.mib.0000235831.01682.8d. [DOI] [PubMed] [Google Scholar]
- 48.Peyrin-Biroulet L, et al. Treatment satisfaction, preferences and perception gaps between patients and physicians in the ulcerative colitis CARES study: A real world-based study. Digest Liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study Liver. 2016;48(6):601–607. doi: 10.1016/j.dld.2016.01.013. [DOI] [PubMed] [Google Scholar]
- 49.Lichtenstein G, Kelly J, McDonald SS, Zanutto EL, Hendricks D, Rahman MI. Assessing drug treatment preferences of patients with Crohn’s disease. PatientPatient-Cent Outcomes Res. 2010;3:113–123. doi: 10.2165/11314880-000000000-00000. [DOI] [Google Scholar]
- 50.Barsky M et al, understanding determinants of patient preferences between stool tests and colonoscopy for the assessment of disease activity in inflammatory bowel disease.Dig Dis Sci 2020. [DOI] [PMC free article] [PubMed]
- 51.Noiseux I et al. Inflammatory bowel disease patient perceptions of diagnostic and monitoring tests and procedures.BMC Gastroenterology 2019;19(1):N.PAG-N.PAG. [DOI] [PMC free article] [PubMed]
- 52.Pittet V, et al. Information needs and concerns of patients with inflammatory bowel disease: what can we learn from participants in a Bilingual Clinical Cohort? PloS one. 2016;11(3):e0150620. doi: 10.1371/journal.pone.0150620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vasudevan A, Arachchi A, van Langenberg DR. Assessing patient satisfaction in inflammatory bowel disease using the QUOTE-IBD survey: a small step for clinicians, a potentially large step for improving quality of care. J Crohn's Colitis. 2013;7(9):e367–e374. doi: 10.1016/j.crohns.2013.02.012. [DOI] [PubMed] [Google Scholar]
- 54.Vaucher C, et al. Patients and gastroenterologists' perceptions of treatments for inflammatory bowel diseases: do their perspectives match? Scand J Gastroenterol. 2016;51(9):1056–1061. doi: 10.3109/00365521.2016.1147065. [DOI] [PubMed] [Google Scholar]
- 55.Cullen G, et al. Perceptions of medication safety among patients with inflammatory bowel disease. Scand J Gastroenterol. 2010;45(9):1076–1083. doi: 10.3109/00365521.2010.490595. [DOI] [PubMed] [Google Scholar]
- 56.Wong S, et al. The information needs and preferences of persons with longstanding inflammatory bowel disease. Can J Gastroenterol. 2012;26(8):525–531. doi: 10.1155/2012/735386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Catalán-Serra I, et al. Information resources used by patients with inflammatory bowel disease: satisfaction, expectations and information gaps. Gastroenterol Hepatol. 2015;38(6):355–363. doi: 10.1016/j.gastrohep.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 58.Khan S et al., Unmet communication and information needs for patients with IBD: implications for mobile health technology. Brit J Med Med Res, 2016;12(3). [DOI] [PMC free article] [PubMed]
- 59.Politi P, et al. Communication of information to patients with inflammatory bowel disease: A European Collaborative Study in a multinational prospective inception cohort. J Crohn's and Colitis. 2008;2(3):226–232. doi: 10.1016/j.crohns.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 60.Quinn CC, et al. The telemedicine for patients with inflammatory bowel disease (TELE-IBD) clinical trial: qualitative assessment of participants' perceptions. J Med Int Res. 2019;21(6):e14165. doi: 10.2196/14165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McCombie A, Gearry R, Mulder R. Preferences of inflammatory bowel disease patients for computerised versus face-to-face psychological interventions. J Crohn's and Colitis. 2014;8(6):536–542. doi: 10.1016/j.crohns.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 62.Baars JE, et al. Patients' preferences regarding shared decision-making in the treatment of inflammatory bowel disease: results from a patient-empowerment study. Digestion. 2010;81(2):113–119. doi: 10.1159/000253862. [DOI] [PubMed] [Google Scholar]
- 63.Gonczi L, et al. Quality of care indicators in inflammatory bowel disease in a tertiary referral center with open access and objective assessment policies. Digest Liver Dis Off J Ital Soc Gastroenterol Ital Assoc Study Liver. 2018;50(1):37–41. doi: 10.1016/j.dld.2017.09.137. [DOI] [PubMed] [Google Scholar]
- 64.Nene S, et al. Benefits of implementing a rapid access clinic in a high-volume inflammatory bowel disease center: Access, resource utilization and outcomes. World J Gastroenterol. 2020;26(7):759–769. doi: 10.3748/wjg.v26.i7.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vavricka SR, et al. Systematic assessment of factors influencing preferences of Crohn's disease patients in selecting an anti-tumor necrosis factor agent (CHOOSE TNF TRIAL) Inflamm Bowel Dis. 2012;18(8):1523–1530. doi: 10.1002/ibd.21888. [DOI] [PubMed] [Google Scholar]
- 66.Rubin DT, et al. Impact of ulcerative colitis from patients' and physicians' perspectives: results from the UC: NORMAL survey. Inflamm Bowel Dis. 2009;15(4):581–588. doi: 10.1002/ibd.20793. [DOI] [PubMed] [Google Scholar]
- 67.McDermott E, et al. Patient education in inflammatory bowel disease: a patient-centred, mixed methodology Study. J Crohns Colitis. 2018;12(4):419–424. doi: 10.1093/ecco-jcc/jjx175. [DOI] [PubMed] [Google Scholar]
- 68.Reich J, et al. Social media use and preferences in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2019;25(3):587–591. doi: 10.1093/ibd/izy280. [DOI] [PubMed] [Google Scholar]
- 69.Reich J, et al. A survey of social media use and preferences in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2016;22(11):2678–2687. doi: 10.1097/MIB.0000000000000951. [DOI] [PubMed] [Google Scholar]
- 70.Yoo YS, Cho OH, Cha KS. Disease-related knowledge and information needs among inflammatory bowel disease patients in Korea. Gastroenterol Nurs. 2015;38(6):455–463. doi: 10.1097/SGA.0000000000000063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bilgrami Z, et al. Effect of telemedicine for inflammatory bowel disease on patient activation and self-efficacy. Digest Dis Sci. 2020;65(1):96–103. doi: 10.1007/s10620-018-5433-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chudy-Onwugaje K, et al. Age modifies the association between depressive symptoms and adherence to self-testing with telemedicine in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2018;24(12):2648–2654. doi: 10.1093/ibd/izy194. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.