Abstract
One of the problems hardly clarified in Coronavirus Disease 2019 (COVID-19) pandemic crisis is to identify factors associated with a lower mortality of COVID-19 between countries to design strategies to cope with future pandemics in society. The study here confronts this problem by developing a global analysis based on more than 160 countries. This paper proposes that Gross Domestic Product (GDP) per capita, healthcare spending and air pollution of nations are critical factors associated with fatality rate of COVID-19. The statistical evidence seems in general to support that countries with a low average COVID-19 fatality rate have high expenditures in health sector >7.5% of GDP, high health expenditures per capita >$2,300 and a lower exposure of population to days exceeding safe levels of particulate matter (PM2.5). Another relevant finding here is that these countries have lower case fatality rates (CFRs) of COVID-19, regardless a higher percentage of population aged more than 65 years. Overall, then, this study finds that an effective and proactive strategy to reduce the negative impact of future pandemics, driven by novel viral agents, has to be based on a planning of enhancement of healthcare sector and of environmental sustainability that can reduce fatality rate of infectious diseases in society.
Keywords: COVID-19, Case fatality rates, Infected people, Health expenditures, Health policy, Health systems, Air pollution, Crisis management, Environmental sustainability
1. The problem and goal of this investigation
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by the novel Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), which appeared in late 2019 (Coccia, 2020). COVID-19 pandemic is still circulating in 2021 with mutations of SARS-CoV-2 that continue to generate high numbers of COVID-19 related infected individuals and deaths in manifold countries worldwide (Johns Hopkins Center for System Science and Engineering, 2021; CDC, 2021). Seligman et al. (2021) show some characteristics of people that are significantly associated with COVID-19 mortality, such as: " mean age 71.6 years, 45.9% female, and 45.1% non-Hispanic white … disproportionate deaths occurred among individuals with nonwhite race/ethnicity (54.8% of deaths … p < .001), individuals with income below the median (67.5% … p < .001), individuals with less than a high school level of education (25.6% … p < .001), and veterans (19.5% … p < .001)". In this context, the fundamental problem is which economic and environmental factors of countries can reduce mortality of COVID-19 and as a consequence decrease the negative impact of COVID-19 pandemic crisis in society (cf., Anser et al., 2020). The study here confronts this problem by developing a global analysis based on more than 160 countries to explain, whenever possible, main factors associated with a lower rate of COVID-19 mortality between countries worldwide. In particular, the main goal of this study is to explore associations among health, economic and environmental factors that have reduced case fatality rate of the COVID-19 in society. The development of this study flows from a recognition that current literature does not clarify the complex interaction of economic, social and institutional factors that can mitigate the mortality of COVID-19 between countries. The assumptions of this study are that wealth of nations, healthcare spending and air pollution are factors associated with fatality rate of COVID-19 in countries. Lessons learned from this study can support effective and proactive strategies for reducing case fatality rates (CFRs) of infectious diseases in the presence of future epidemics similar to the COVID-19. This study is part of a large research project that investigates factors associated with the transmission dynamics of COVID-19 pandemic and socioeconomic effects of the COVID-19 pandemic crisis in society to cope with future epidemics with appropriate policy responses of crisis management (cf., Coccia, 2020, 2021).
2. Theoretical framework
Manifold studies focus on different aspects of COVID-19 pandemic crisis (cf., Hu et al., 2021; Tian et al., 2021). Asirvatham et al. (2020) estimate an adjusted case fatality rate of COVID-19 in India considering some factors of urban environment and population. Results suggest that urban population and population aged more than 60 years were associated with increased adjusted case fatality rate. In this context, healthcare interventions directed to test elderly, people with comorbidities (e.g., having diabetes, cardiovascular diseases, cancer, etc.) and urban population are critical public policies to constrain negative effects of COVID-19 pandemic in society. Siddiqui et al. (2020) also analyze the impact of COVID-19 pandemic in India and show that: “low public health expenditure combined with a lack of infrastructure and low fiscal response implies several challenges to scale up the COVID-19 response and management. Therefore, emergency preparedness and response plan are essential strategies to integrate into the health system of India”. Ahmed et al. (2020) focus on demographic, socioeconomic, lifestyle and health factors of countries to explain different effects of COVID-19 in society. Ahmed et al. (2020) show that countries with high average age of population and high percentage of urban population have also a high fatality of COVID-19. In this research field, Kavitha and Madhavaprasad (2020) maintain that preventive health care measures and policies of social distancing applied on a vast portion of population can constraint the spread of COVID-19. Iyanda et al. (2020) argue that reinforcing public health sector and epidemiological surveillance programs can both reduce the spread of COVID-19 and prevent unnecessary deaths of this infectious disease. The role of health expenditure is also investigated by Gaffney et al. (2020) in the case study of the USA. González-Bustamante (2021) shows that in South America, the social pressure on healthcare system affects interventions of governments to constrain the diffusion of COVID-19. Jin and Qian (2020) analyze the Chinese public-health expenditure at national and provincial levels and suggest that Chinese government should improve the quantity and quality of public-health expenditure in manifold aspects, such as the prevention and control of major public-health emergencies, the reduction of inequity in public-health resource allocation among provinces, the waste of resources in the public-health system, etc. Kapitsinis (2020) investigates the diffusion of the novel coronavirus in nine European countries and pinpoints that health investments play a vital role to alleviate mortality rate of the COVID-19. Instead, Barrera-Algarín et al. (2020) show that in Europe, a lower level of public health investments per capita is associated with high numbers of COVID-19 deaths per million inhabitants; in general, a high mortality of COVID-19 is due to low health expenditure associated with high income inequality. Finally, Perone (2021) analyzes Italy and shows that health care efficiency is one of the factors to be reinforced for the reduction of case fatality rate (CFR); moreover, population aged 70 years and over, and concentration of air pollutants in cities are positively associated with fatality rate in society.
Overall, then, current literature shows that different socioeconomic systems and public policies have generated dissimilar effects of COVID-19 pandemic in society (e.g., in China, India, Italy, the USA, the UK, etc.). However, what is hardly known is to explain and generalize at global level which economic and environment factors of countries are associated with a lower mortality of COVID-19 to design an effective strategy to constrain future epidemics similar to COVID-19.
3. Materials and methods
This study has the primary objective to explore factors associated with a lower fatality rate of the COVID-19 between countries. Results can explain and generalize, whenever possible, vital characteristics of countries for designing an effective public policy to limit negative impacts of future pandemic crisis similar to COVID-19.
3.1. Research setting, sample, and working hypothesis
A main characteristic caused by the novel pathogen of SARS-CoV-2 and its mutations is the severe impact in society, leading to high number of deaths. Fatality rates indicate the severity of an infectious disease and are a main proxy to evaluate the quality of health systems (WHO, 2020). In fact, Lau et al. (2021) argue that confirmed cases of infections are misleading numbers and suggest the mortality rate as the main indicator to evaluate the real effects of COVID-19 in society. In this context, a main measure is case fatality ratio (CFR), which estimates the proportion of deaths among identified confirmed cases. Wilson et al. (2020) argue that SARS-CoV-2 associated with new mutations is expected to further spread globally, and studies have to clarify case-fatality risks of this new infectious disease to support effective public policies. Angelopoulos at al. (2020) maintain that case fatality rates (CFRs) of COVID-19 between countries are critical measures of relative risk that guide policymakers to decide how to allocate medical resource during on-going pandemic crisis. The study here is based on a sample of N = 161 countries that is categorized in two sub-samples having a similar socioeconomic framework, given by countries with a level of Gross Domestic Product (GDP) per capita (wealth of individuals) higher or lower than arithmetic mean of the sample.
The purpose of the present study is to see whether statistical evidence supports the working hypothesis that high GDP per capita, high healthcare spending, and low air pollution can explain the reduction of fatality rate of COVID-19 between countries.
3.2. Measures
The measures for statistical analyses are:
-
⁃
Number of COVID-19 infected individuals (%) is measured with confirmed cases of COVID-19 on December 14, 2020 divided by population of countries under study, per cent. Source of data: Johns Hopkins Center for System Science and Engineering (2021).
-
⁃
Number of COVID-19 deaths (%) is measured with case fatality rate (%) given by deaths on December 14, 2020 divided by total infected individuals in countries, per cent. Source of data: Johns Hopkins Center for System Science and Engineering (2021).
-
⁃
Wealth of population is measured with Gross Domestic Product (GDP) per capita, Purchasing Power Parity (PPP-current international U.S. dollars $) in 2019 (last year available in dataset). GDP per capita is gross domestic product divided by midyear population. GDP is the sum of gross value added by all resident producers in the economy plus any product taxes and minus any subsidies not included in the value of products. It is calculated without making deductions for depreciation of fabricated assets or for depletion and degradation of natural resources. Source of data: World Bank (2020).
-
⁃
The expenditures in health sector are measured by:
-
a)
Level of current health expenditure expressed as a percentage of GDP in 2017 (last year available in dataset). Estimates of current health expenditures include healthcare goods and services consumed during each year. Although this indicator does not include capital health expenditures (e.g., buildings, machinery, IT and stocks of vaccines for emergency or outbreaks), it is a main proxy of investments in health sector; in fact, countries having higher levels of health expenditures as percentage of GDP also tend to have a higher level of Research and Development expenditure (% of GDP)1 : bivariate correlation, using data of 2017, shows a positive coefficient of Pearson equal to r = 0.45 (p-value .01, N = 115 countries) between health expenditures and R&D investments, whereas regression analysis with log-log model reveals that a 1% increase in the Research and Development expenditure (% of GDP), it increases expected current health expenditure (% of GDP) of 0.14% (p-value .001; coefficient R2 indicates that about 20% of the variation of health expenditure can be attributed linearly to Research and Development expenditure). Source of data: World Bank (2020a).
-
b)
Domestic general government health expenditure per capita, PPP (current international $) in 2017 (last year available): Public expenditure on health from domestic sources per capita are expressed in international dollars at purchasing power parity (PPP time series based on ICP2011 PPP). Source of these data is also World Bank (2020b).
-
⁃
Elderly are measured with population aged 65 years and over as a percentage of the total population (population here counts all residents regardless of legal status or citizenship in 2019, last year available). Source: World Bank (2020c). Population aged 65 and over is an important factor in the analyses of infectious diseases because many studies show negative effects of COVID-19 on health of old people (Cohen-Mansfield, 2020; Perone, 2021).
-
⁃
Air pollution in environment is measured by percent of population exposed to ambient concentrations of PM2.5 that exceed the World Health Organization (WHO) guideline value in 2017 (last year available). In particular, it indicates the portion of a country's population living in places where mean annual concentrations of PM2.5 are greater than 10 μg per cubic meter, the guideline value recommended by the WHO as the lower end of the range of concentrations over which adverse health effects due to PM2.5 exposure have been observed. Source: World Bank (2020d). In this context, studies reveal that urban areas with frequently high levels of air pollution — exceeding safe levels of ozone or particulate matter — had higher numbers of COVID-19 related infected individuals and deaths (Coccia, 2020, 2021, 2021a; Martelletti and Martelletti, 2020). Moreover, high concentrations of particulate air pollutant induce serious damages to the immune system of people, weakening human body to cope with infectious diseases of (new) viral agents and other diseases (Glencross et al., 2020).
-
⁃
Containment measures against the spread of COVID-19 are assessed with total days of lockdown across countries in the year 2020 (Coccia, 2021b). Tobías (2020, p. 2) states that: “Lockdown, including restricted social contact and keeping open only those businesses essential to the country's supply chains, has had a beneficial effect”. Flaxman et al. (2020) show that lockdowns seem to have effectively reduced transmission of the COVID-19. Atalan (2020) argues that countries can start lockdown when there is an acceleration of daily confirmed cases beyond a critical threshold and can end it when there is a strong reduction of Intensive Care Unit (ICU) admissions (cf., Chaudhry et al., 2020). Source: COVID-19 pandemic lockdowns (2021).
3.3. Data analysis procedure
The sample of N = 161 countries is divided in two sub-samples (group 1 and 2), each one having similar socioeconomic conditions for a structural comparative analysis:
-
❑
group 1: countries with a Gross Domestic Product per capita higher than arithmetic mean of the sample
-
❑
group 2: countries with a Gross Domestic Product per capita lower and/or equal than arithmetic mean of the sample
Firstly, data are analyzed with descriptive statistics given by arithmetic mean (M) and standard deviation (SD) of variables for a comparative analysis between two groups of countries just mentioned. In addition, the normality of the distribution of variables, to apply correctly parametric analyses, is verified with skewness and kurtosis coefficients; in the presence of not normal distributions, variables are transformed in logarithmic scale to have normality.
Secondly, follow-up investigation is the Independent Samples t-Test that compares the means of two independent groups in order to determine whether there is statistical evidence that the associated population means are significantly different. The assumption of homogeneity of variance in the Independent Samples t-Test -- i.e., both groups have the same variance -- is verified with Levene's Test based on following statistical hypotheses:
H0: σ1 2 - σ2 2 = 0 (population variances of group 1 and 2 are equal).
H1: σ1 2 - σ2 2 ≠ 0 (population variances of group 1 and 2 are not equal).
The rejection of null hypothesis in Levene's Test suggests that variances of the two groups are not equal: i.e., the assumption of homogeneity of variances is violated. If Levene's test indicates that the variances are equal between the two groups (i.e., p-value is large), equal variances are assumed. If Levene's test indicates that the variances are not equal between the two groups (i.e., p-value is small), the assumption is that equal variances are not assumed.
After that, null hypothesis (H′ 0) and alternative hypothesis (H′ 1) of the Independent Samples t-Test are:
H′0: μ1 = μ2, the two population means are equal in countries with a higher and lower level of GDP per capita.
H′1: μ1 ≠ μ2, the two population means are not equal in countries having a higher and lower level GDP per capita.
Statistical analyses are performed with the Statistics Software SPSS® version 26.
4. Results
The arithmetic mean (M) of the GDP per capita in 2019 of the sample (N = 155 valid cases and 6 missing values) is M = $22,794; as consequence the two groups for a comparative analysis are:
-
❑
Countries with a Gross Domestic Product per capita in 2019 > $22,794, N = 58 countries
-
❑
Countries with a Gross Domestic Product per capita in 2019 ≤ $22,794, N = 98 countries
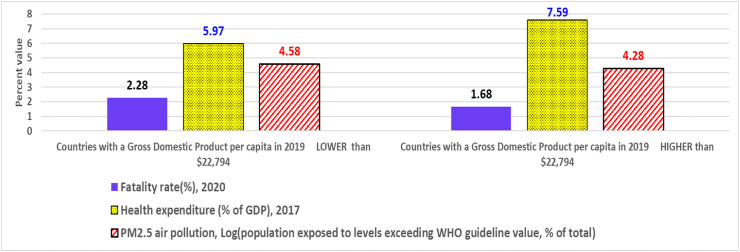
Table 1 shows that fatality rate is lower in richer countries (1.68%) that have an average GDP per capita more than $46,600, a high level of health expenditure of roughly 7.6% of GDP, a high level of government health expenditure of about $2,300 per capita, a lower exposure of population to levels exceeding PM2.5 air pollution according to WHO guidelines, and finally a longer period of lockdown; regardless a higher percentage of population aged 65 years and over, and a higher incidence of confirmed cases on population in these countries (cf., Fig. 1 ).
Table 1.
Descriptive statistics.
| Countries with a Gross Domestic Product per capita in 2019 ≤ $22,794 |
Countries with a Gross Domestic Product per capita in 2019 > $22,794 |
|||
|---|---|---|---|---|
| Description of variables | M | SD | M | SD |
| - Cases/population, % 2020 | 0.81 | 1.11 | 2.39 | 1.66 |
| - Fatality rate, % 2020 | 2.28 | 1.57 | 1.68 | 0.88 |
| - GDP per capita PPP ($), 2019 | $8,538.85 | $6,035.58$ | $46,634.61 | $20,215.07 |
| - Health expenditure % of GDP, 2017 | 5.97 | 2.12 | 7.59 | 2.77 |
| - General government health expenditure per capita, PPP ($), 2017 | $243.72 | $260.29 | $2,323.90 | $1,373.42 |
| - Population aged 65 years and over as a percentage of population, 2019 | 5.83 | 3.85 | 15.07 | 6.41 |
| - PM2.5 air pollution, population exposed to levels exceeding WHO guideline value (% of total), 2017 | 97.70 | 11.95 | 72.34 | 38.23 |
| - COVID-19 pandemic lockdowns (days), 2020 | 55.26 | 51.22 | 96.71 | 85.79 |
Note: M = arithmetic mean; SD= Standard Deviation.
Fig. 1.
Fatality of COVID-19, health expenditure and population exposed to high levels of air pollution in countries with GDP per capita higher/lower than $22,794. Note: log values of PM2.5 air pollution are to have comparable numbers in the bar graph.
Table 2 shows the Independent Samples t-Test, as follow-up inspection, to assess the significance of the difference of arithmetic mean between groups of countries under study. The p-value of Levene's test is significant, and we have to reject the null HP of Levene's test and conclude that the variance in the groups under study is significantly different (i.e., equal variances are not assumed), except variable of lockdown (days) that has p-value<.06 and equal variances are assumed. Table 2 reveals a statistically significant difference of arithmetic mean between groups having GDP per capita lower than $22,794 (group 1) and higher than $22,794 (group 2) as indicated in Table 1.
Table 2.
Independent samples test.
| Levene's Test for equality of variances |
t-test for equality of Means |
|||||||
|---|---|---|---|---|---|---|---|---|
| F | Sig. | t | df | Sig. (2-tailed) | Mean Difference | Std. Error Difference | ||
| Cases/population %, 2020 | •Equal variances assumed | 17.462 | 0.001 | −7.079 | 153.000 | 0.001 | −0.016 | 0.002 |
| •Equal variances not assumed | −6.431 | 88.151 | 0.001 | −0.016 | 0.002 | |||
| Fatality rate %, 2020 |
•Equal variances assumed | 7.842 | 0.006 | 2.671 | 154.000 | 0.008 | 0.006 | 0.002 |
| •Equal variances not assumed | 3.057 | 153.670 | 0.003 | 0.006 | 0.002 | |||
| GDP per capita PPP ($), 2019 | •Equal variances assumed | 46.016 | 0.001 | −17.345 | 153.000 | 0.000 | −38095.761 | 2196.380 |
| •Equal variances not assumed | −13.984 | 63.132 | 0.001 | −38095.761 | 2724.193 | |||
| Health expenditure % of GDP, 2017 | •Equal variances assumed | 4.929 | 0.028 | −4.127 | 154.000 | 0.001 | −1.627 | 0.394 |
| •Equal variances not assumed | −3.859 | 96.660 | 0.001 | −1.627 | 0.422 | |||
| General government health expenditure per capita, PPP ($), 2017 | •Equal variances assumed | 163.442 | 0.001 | −14.446 | 152.000 | 0.001 | −2080.181 | 143.998 |
| •Equal variances not assumed | −11.412 | 59.484 | 0.001 | −2080.181 | 182.286 | |||
| Population ages 65 years and over as a percentage of population, 2019 | •Equal variances assumed | 21.540 | 0.001 | −11.266 | 154.000 | 0.001 | −9.244 | 0.821 |
| •Equal variances not assumed | −9.975 | 81.803 | 0.001 | −9.244 | 0.927 | |||
| Log PM2.5 air pollution, population exposed to levels exceeding WHO guideline value (% of total), 2017 | •Equal variances assumed | 59.944 | 0.001 | 4.311 | 148.000 | 0.001 | 0.518 | 0.120 |
| •Equal variances not assumed | 3.190 | 52.335 | 0.002 | 0.518 | 0.162 | |||
| Log days COVID-19 lockdowns, 2020 | •Equal variances assumed | 3.749 | 0.057 | −2.030 | 70.000 | 0.046 | −0.433 | 0.213 |
| •Equal variances not assumed | −1.999 | 61.106 | 0.050 | −0.433 | 0.217 | |||
In particular, Table 2 substantiates that:
-
•
There was a significant difference in average cases/population % between groups 1 and 2 (t 88.15 = −6.43, p < .001)
-
•
There was a significant difference in average fatality rate % between groups 1 and 2 (t 153.67 = 3.06, p < .01)
-
•
There was a significant difference in average GDP per capita between groups 1 and 2 (t 63.13 = −13.98, p < .001)
-
•
There was a significant difference in average health expenditure as % of GDP between groups 1 and 2 (t 96.66 = −3.86, p < .001)
-
•
There was a significant difference in average government health expenditure per capita between groups 1 and 2 (t 59.48 = −11.41, p < .001)
-
•
There was a significant difference in average population aged 65 years and over as a percentage of total population between groups 1 and 2 (t 81.80 = −9.98, p < .001)
-
•
There was a significant difference in average population exposed to levels of PM2.5 air pollution exceeding WHO guideline value (% of total) between groups 1 and 2 (t 52.34 = 3.19, p < .01)
-
•
There was a significant difference in average days of COVID-19 pandemic lockdowns between groups 1 and 2 (t 70.00 = −2.03, p < .05)
Hence, findings suggest that fatality rate in richer countries (1.7%) is lower than medium-low income per capita countries (2.3%). The statistical evidence above seems in general to support the hypothesis stated that factors associated with the mitigation of the fatality of COVID-19 can be due to a higher level of health expenditure (roughly 7.6% of GDP), higher level of government health expenditure per capita (about $2,300), a lower exposure of population to levels exceeding PM2.5 air pollution according to WHO guidelines and a longer duration of lockdown, though countries with lower CFRs have a higher percentage of population aged 65 years and over (considered as a risk group in population; cf., European Centre for Disease Prevention and Control, 2021)2 and a higher incidence of confirmed cases in population. These statistical analyses provide important, very important results to explain factors associated with reduced effects of COVID-19 pandemic in society. Therefore, an effective strategy to cope with global pandemic crisis has to be based on three main public policies:
□health policy with higher levels of healthcare expenditure as percentage of GDP directed to specific targets of efficiency of overall healthcare sector
□environmental policies based on sustainability for reducing the exposure of population to high levels of air pollution
□and finally, a timely policy response based on containment and mitigation measures in a context of advanced economies.
5. Discussion and policy implications
Lau et al. (2021) argue that in the presence of a continuous global COVID-19 pandemic threat, confirmed cases appear vague numbers and suggest the mortality rate as one of the main indicators to evaluate the real effects of COVID-19 in society (cf., Antony et al., 2020; Liu et al., 2021). In the presence of COVID-19 pandemic crisis and similar infectious diseases, nations endeavor to mitigate the case fatality rate (cf., Coccia, 2020a). Previous studies suggest that measures of containment, such as full lockdown, can reduce the human-to-human transmission dynamics of COVID-19 pandemic in society (Atalan, 2020; Prem et al., 2020; Tobías, 2020).
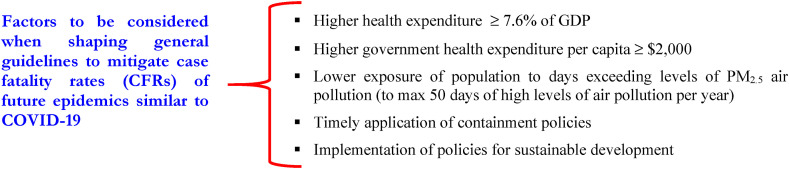
However, restriction policies are necessary but, of course, not sufficient interventions to constraint a negative impact of pandemics in society because many countries with a longer duration of lockdown have also a very high fatality rate, such as Italy (Coccia, 2021); as a consequence, an additional inquiry is needed (Coccia, 2021b). What this study adds to current studies on the COVID-19 pandemic crisis is to explain, with a global analysis between countries, critical factors associated with a lower rate of fatality to support a comprehensive strategy to cope with future epidemics similar to COVID-19. In particular, this study confirms that high GDP per capita, high healthcare spending and low levels of air pollution are factors associated with reduced case fatality rates (CFRs) of COVID-19 between countries. These findings here can suggest factors to be considered when shaping general guidelines to mitigate CFRs of epidemics similar to COVID-19 as schematically summarized in Fig. 2 .
Fig. 2.
Factors associated with a mitigation of case fatality rates of COVID-19 between countries to design general guidelines to constrain pandemic crises of novel viral agents similar to Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) that is the strain of the novel influenza that causes coronavirus disease 2019 (COVID-19).
Hence, follow-up materials to reduce fatality rates of COVID-19 have to be focused on structural public policies to cope with a constant pandemic threat. Especially:
-
❑
Health Policy
This study reveals that countries with lower fatality rates have a high average level of health expenditure given by 7.6% of GDP and average government health expenditure per capita of about $2,300, whereas countries with higher fatality rates of COVID-19 have an average health expenditure of roughly 6% of GDP and very low government health expenditure per capita (a mere average value of about $243 per inhabitants) that indicates a weak healthcare sector to cope with pandemics and also other diseases in society. Scholars, to reduce the risk factors of COVID-19 mortality, also suggest to consider socioeconomic, clinical, physical, biophysiological, and biochemical characteristics of people, which can be affected by the type of nutrition system, toxicity, and ecological footprint (Aljerf and Aljurf, 2020). Other scholars, such as Kapitsinis (2020), argue that investments in health sector are a critical public policy to mitigate mortality rate of COVID-19. In this context, countries should support the expansion of hospital capacity and testing capabilities to reduce diagnostic delays of infectious diseases and foster new technology with the development of effective vaccines, antivirals and other innovative drugs that can counteract future public health threats of new epidemics similar to COVID-19 (Ardito et al., 2021; Coccia, 2019, 2020; Coccia, 2019).
-
❑
Environmental policy
This study finds that sustainable environment plays a vital role for reducing COVID-19 related infected individuals and deaths; in particular, a low rate of fatality is associated with a low level of air pollution (cf., Coccia, 2020, 2020b; 2020c). In fact, average population exposed to levels exceeding WHO guideline value (% of total) is 72% in countries with a lower level of fatality rate, whereas in countries with a higher incidence of mortality of the COVID-19 is almost 98%! Coccia (2020, 2021) shows that number of infected people was higher in Italian cities with more than 100 days per year exceeding limits set for PM10 or ozone. Copat et al. (2020), considering different studies about the relation between air pollution and the spread of COVID-19, suggest that PM2.5 and NO2 can support the spread and lethality of COVID-19, but additional analyses are needed to confirm this relation concerning transmission dynamics and negative effects of the SARS-CoV-2 (cf., Coccia, 2021). Coccia (2020), using a case study of Italy, reveals that: “the max number of days that Italian provincial capitals can exceed per year the limits set for PM10 (particulate matter 10 μm or less in diameter) or for ozone, considering the meteorological conditions, is about 48 days. Beyond this critical point, …environmental inconsistencies, because of the combination between air pollution and meteorological conditions, trigger a take-off of viral infectivity (epidemic diffusion) with damages for health of population, economy and society” (cf. also Aljerf and Aljurf, 2020). In fact, days of high levels of air pollution, associated with climate change, affect the health of population and environment (Coccia, 2020, 2021). In this field of research, Carugno et al. (2018) analyze respiratory syncytial virus (RSV), the primary cause of acute lower respiratory infections in children: bronchiolitis. The study suggests that seasonal weather conditions and concentration of air pollutants seem to influence RSV-related bronchiolitis epidemics in urban areas of North Italy. In particular, airborne particulate matter (PM) may influence the children's immune system and foster the spread of RSV infection. This study also shows a correlation between short- and medium-term PM10 exposures and increased risk of hospitalization because of RSV bronchiolitis among infants. Glencross et al. (2020) discuss that air pollution in the long run can cause diseases by perturbing multicellular immune responses because areas with high levels of air pollution are associated with increased exacerbations of asthma and novel influenza viruses (Coccia, 2020, 2020a, 2021, 2020a). Moreover, in outdoor environments, studies suggest that the concentration of atmospheric pollutants can include also viral agents and likely this concentration is one of the drivers associated with the spread of SARS-CoV-2 (Coccia, 2020; Martelletti and Martelletti, 2020), but a high wind speed sustains clean days from air pollution, reducing whenever possible the spread of COVID-19 and other infectious diseases (cf., Coccia, 2020; Rosario et al., 2020). To put it differently, a low wind speed in cities prevents the dispersion of air pollutants that can include bacteria and viruses, such as SARS-CoV-2, and can increase the incidence of COVID-19 in society, such as in some European regions (Coccia, 2020, 2021). Instead, high wind speed supports the dilution and removal of the droplets, decreasing the concentration of viral agents in the air and the transmission dynamics of viral infectivity among people (cf., Coccia, 2020b, 2020c). In fact, Rosario et al. (2020, p. 4) also show that wind intensity improves the circulation of air and also increases the exposure of the novel coronavirus to the solar radiation effects, a factor having a negative correlation in the diffusion of COVID-19. Guo et al. (2019) argue that haze pollution is a serious environmental problem affecting cities, proposing policies of urban planning that improve natural ventilation and respiratory health of population. In addition, scholars argue that: “besides some high negative externalities associated with COVID-19 pandemic in the form of increasing death tolls and rising healthcare costs, the global world should have to know how to direct high mass carbon emissions and population growth through acceptance of preventive measures, which would be helpful to contain coronavirus pandemic at a global scale” (Anser et al., 2020). Marazziti et al. (2021) point out that the activities of human society do not consider the long-term damages of high air pollution on climate that may increase the diffusion of novel airborne viruses. Reilly et al. (2021) maintain that one of the main effects of COVID-19 pandemic crisis on climate change can be its influence on national commitments to action, such as recovery funds directed to low carbon investments. As a matter of fact, improvements in air quality have been accompanied by demonstrable benefits to human health (Coccia, 2020). In this perspective, countries should introduce organizational, product and process technologies directed to a sustainable development for the improvement of environment, atmosphere, air quality and especially health of population to cope with future epidemics similar to COVID-19 and other diseases that generate different disorders for the health of people (Amoatey et al., 2020; Siafakas et al., 2018, (Coccia, 2019, Coccia, 2020, Coccia and Watts, 2020)).
-
❑
Public policy responses
This study also shows that a lower mortality of COVID-19 is associated with countries having a timely application of containment policies. The model by Balmford et al. (2020) reveals that countries with an immediate application of lockdown reduced deaths of COVID-19 compared to countries that delayed the application of this strong containment measure. Gatto et al. (2020) maintain that restriction to mobility and human interactions can reduce transmission dynamics of the COVID-19 by about 45%. Janssen and van der Voort (2020) show the utility of “smart lockdown” as policy responses based on suggested and not mandated mitigation measures that are focused on responsibility of individuals. In this context, new studies show that specific places have a high risk to be COVID-19 outbreaks (e.g., restaurants, gyms, stadium, discotheques, etc.; cf., Chang et al., 2020); as a consequence, selected measures of containment (e.g., restricting maximum occupancy of specific places, social distancing and wearing of face masks) can be more effective interventions to constrain the spread of COVID-19, without deteriorating economic system, than public policies based on uniformly reduction of the mobility of people and general lockdown (Chang et al., 2020; cf., Coccia, 2021b, 2021c; Renardy et al., 2020). Studies also report that containment measures for COVID-19 pandemic crisis might affect mental health with: “disturbances ranging from mild negative emotional responses to full-blown psychiatric conditions, specifically, anxiety and depression, stress/trauma-related disorders, and substance abuse. The most vulnerable groups include elderly, children, women, people with pre-existing health problems especially mental illnesses, subjects taking some types of medication including psychotropic drugs, individuals with low socio-economic status, and immigrants” (Marazziti et al., 2021). Simon et al. (2021) confirm that: “negative capability well-being, mental health and social support impacts of the Covid-19 lockdown were strongest for people with a history of mental health treatment. Future public health policies concerning lockdowns should pay special attention to improve social support levels in order to increase public resilience”.
***
In general, a continuous pandemic threat can highlight some fragilities, vulnerabilities and weaknesses of ecosystem and society, and the difficulties of countries to cope with unforeseen crises. Hence, pandemic threats originated by novel infectious diseases, such as the COVID-19, need timely policy responses of containment based on agility and adaptive governance of nations supported by high expenditures in health sector and effective environmental policies for reducing air pollution (cf., Coccia, 2020, 2021). In the short run, efficient health systems can support an effective management of COVID-19 vaccinations to constrain negative effects of pandemics in socioeconomic systems (DeRoo et al., 2020; Frederiksen et al., 2020; Harrison and Wu, 2020). Evans and Bahrami (2020) pinpoint that super-flexibility can be an appropriate approach to cope with pandemic threats of COVID-19 and similar infectious diseases in which decision making of policymakers should be oriented to versatility, agility, and resilience.
In short, this study, to reiterate, suggests that to constrain the negative impact in society of constant pandemic threats, nations have to apply public policies directed to increase expenditures in health sector and reduce the sources of air pollution for improving healthcare of population in a context of overall environmental sustainability (Coccia, 2020; Sabat et al., 2020, p. 917).
6. Concluding observations and limitations
This statistical analysis here suggests that high GDP per capita, high healthcare spending and low levels of air pollution are factors associated with reduction of fatality rate of COVID-19 between countries. In particular, this new study here supports the hypothesis that countries with a low average COVID-19 fatality rates have high average expenditures in health sector (>7.5% of GDP), high average health expenditures per capita (>$2,300) and a lower average exposure of population to days exceeding safe levels of particulate matter (PM2.5). Results of the study here also suggest that factors to be considered when shaping general guidelines for a global strategy to cope with pandemic threat have to be based on a public policy that supports health system with effective expenditures and investments, and an environmental policy directed to sustainability that reduces the exposure of population to high levels of air pollution. These public policies can reduce case fatality rates in the presence of pandemics, regardless a higher percentage of elderly in society.
In addition, results here can also suggest ambidexterity strategies of crisis management for more prosperous or less favored countries:
-
•
Rich countries can focus in the short run on measures of containment of shorter duration because of a stronger healthcare sector based on high health expenditures (as % of GDP), whereas in the long run these countries should support environmental policies for reducing air pollution
-
•
Developing countries have to focus in the short run on measures of containment of a longer duration because of a weak healthcare sector based on low health expenditures (as % of GDP) and in the long run have to support policies for enhancing health system and health of population.
These conclusions are, of course, tentative. A main concern is that there can be differences among countries having a similar level of GDP per capita, because they can have different healthcare expenditures, institutional contexts, political regimes and apply different strategies of pandemic management. COVID-19 pandemic also shows broad variations in the estimations of CFR between different geo-economic regions and as a consequence some data are difficult to compare for manifold reasons. In fact, there can be a bias for detecting and reporting all COVID-19 deaths in poor countries. In addition, nations can use different case concepts, testing strategies or counting cases. Variations in CFR may be also due to how time lags are handled, to dissimilar organizations of healthcare systems and/or to interventions applied at different stages of the illness. Finally, structure of population and characteristics of patients (e.g., ethnicity, age, sex, and comorbidities) may vary between countries making comparative analysis in some cases problematic (Angelopoulos et al., 2020; WHO, 2020). Although the study here provides main findings to better design policy responses to cope with pandemic threat, other confounding factors that influence variables under study here (e.g., institutional aspects, culture, religion, political system, investments in hospital sector, in prevention, in medical personnel, etc.) need to be considered for more comprehensive analysis and policy responses of countries (cf., Stribling et al., 2020). The positive side of this study is a global analysis of more than 160 countries to explore and generalize, whenever possible, proposed findings that are prima facie (i.e., accepted as correct until proved otherwise) to support appropriate policy responses of crisis management at country level. However, future studies have also to focus on follow-up materials and questions investigating the role of different organizational and financing modes of healthcare systems and the allocation of financial resources between healthcare activities (e.g., preventive and curative care) or groups of healthcare providers (for example, hospitals and ambulatory centers) because can affect the health system capability of countries to cope with pandemic crises. Hence, results here have to be reinforced with much more follow-up investigations concerning a detailed research into the relations between effects of pandemic in society, health systems, public health capacities and policy responses of countries.
Overall, then, this study suggests that an effective strategy to reduce the negative impact of future pandemic threats in society, similar to COVID-19, in terms of case fatality rates (CFRs), has to be based on high expenditures (and investments) in health system and on policies of sustainable development to improve health of people and protect ecosystems. To conclude, this study here could represent a starting point to analyze further socio-economic factors that may shape and support general guidelines for a strategy to cope with future pandemic crises both in more prosperous and less favored countries.
Author's contributions
Mario Coccia: Conceptualization, Methodology, Investigation, Formal analysis, Data curation, Visualization, Writing - original draft, Writing - review & editing, Funding acquisition, Project administration, Resources, Software, Supervision, Validation
Declaration of competing interest
The author, Mario Coccia, declares that he has no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. No funding was received for this study.
For instance, in this context, at 9 December 2020, fatality rate in Italy as a percentage of the age group was 3% (between people having 60–69 years), 10.2% (70–79 years), 19% (80–89) and finally about 23% in population aged > 90 years (cf., Perone, 2021).
Gross domestic expenditures on research and development (R&D), expressed as a percent of GDP, include both capital and current expenditures in the four main sectors: business enterprise, government, higher education and private non-profit. R&D covers basic research, applied research, and experimental development.
References
- Ahmed A., Haque T., Rahman M.M. Lifestyle acquired immunity, decentralized intelligent infrastructures, and revised healthcare expenditures may limit pandemic catastrophe: a lesson from COVID-19. Frontiers in Public Health. 2020;8:566114. doi: 10.3389/fpubh.2020.566114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aljerf L., Aljurf M. Improvements in the ecological and nutritional aspects of down's Syndrome. Preprints. 2020;2020 doi: 10.21203/rs.3.rs-30313/v1. 2020050512. [DOI] [Google Scholar]
- Amoatey P., Sicard P., De Marco A., Khaniabadi Y.O. Long-term exposure to ambient PM2.5 and impacts on health in Rome, Italy. Clinical Epidemiology and Global Health. 2020;8(2):531–535. doi: 10.1016/j.cegh.2019.11.009. [DOI] [Google Scholar]
- Angelopoulos A.N., Pathak R., Varma R., Jordan M.I. Harvard Data Science Review. 2020. On identifying and mitigating bias in the estimation of the COVID-19 case fatality rate. [DOI] [Google Scholar]
- Anser M.K., Yousaf Z., Khan M.A., Voo X.H., Nassani A.A., Alotaibi S.M., Abro M., Zaman K. Advance online publication; 2020. The Impacts of COVID-19 Measures on Global Environment and Fertility Rate: Double Coincidence. Air Quality, Atmosphere, & Health, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antony S.J., Almaghlouth N.K., Heydemann E.L. Are coinfections with COVID-19 and influenza low or underreported? An observational study examining current published literature including three new unpublished cases. J. Med. Virol. 2020;92(11):2489–2497. doi: 10.1002/jmv.26167. [DOI] [PubMed] [Google Scholar]
- Ardito L., Coccia M., Messeni Petruzzelli A. Technological exaptation and crisis management: evidence from COVID-19 outbreaks. R D Manag. 2021 doi: 10.1111/radm.12455. [DOI] [Google Scholar]
- Asirvatham E.S., Lakshmanan J., Sarman C.J., Joy M. Demystifying the varying case fatality rates (CFR) of COVID-19 in India: lessons learned and future directions. Journal of Infection in Developing Countries. 2020;14(10):1128–1135. doi: 10.3855/jidc.13340. [DOI] [PubMed] [Google Scholar]
- Atalan A. Is the lockdown important to prevent the COVID-19 pandemic? Effects on psychology, environment and economy-perspective. Annals of medicine and surgery. 2020;56:38–42. doi: 10.1016/j.amsu.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balmford B., Annan J.D., Hargreaves J.C., et al. Cross-country comparisons of covid-19: policy, politics and the price of life. Environ. Resour. Econ. 2020;76:525–551. doi: 10.1007/s10640-020-00466-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrera-Algarín E., Estepa-Maestre F., Sarasola-Sánchez-Serrano J.L., Vallejo-Andrada A. vol. 94. Revista espanola de salud publica; 2020. COVID-19, Neoliberalism and Health Systems in 30 European Countries: Relationship to Deceases. [PubMed] [Google Scholar]
- Carugno M., Dentali F., Mathieu G., Fontanella A., Mariani J., Bordini L., Milani G.P., Consonni D., Bonzini M., Bollati V., Pesatori A.C. PM10 exposure is associated with increased hospitalizations for respiratory syncytial virus bronchiolitis among infants in Lombardy, Italy. Environ. Res. 2018;166:452–457. doi: 10.1016/j.envres.2018.06.016. 2018. [DOI] [PubMed] [Google Scholar]
- CDC About variants of the virus that causes COVID-19. 2021. https://www.cdc.gov/coronavirus/2019-ncov/transmission/variant.html
- Chang S., Pierson E., Koh P.W., et al. Mobility network models of COVID-19 explain inequities and inform reopening. Nature. 2020 doi: 10.1038/s41586-020-2923-3. [DOI] [PubMed] [Google Scholar]
- Chaudhry R., Dranitsaris G., Mubashir T., Bartoszko J., Riazi S. A country level analysis measuring the impact of government actions, country preparedness and socioeconomic factors on COVID-19 mortality and related health outcomes. Eclinicalmedicine. 2020 doi: 10.1016/j.eclinm.2020.100464. 100464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M. Why do nations produce science advances and new technology? Technol. Soc. 2019;59:1–9. doi: 10.1016/j.techsoc.2019.03.007. November, 101124. [DOI] [Google Scholar]
- Coccia M. The theory of technological parasitism for the measurement of the evolution of technology and technological forecasting. Technological Forecasting and Social Change. 2019;141:289–304. doi: 10.1016/j.techfore.2018.12.012. [DOI] [Google Scholar]
- Coccia M. A Theory of classification and evolution of technologies within a Generalized Darwinism. Technology Analysis & Strategic Management. 2019;31(5):517–531. doi: 10.1080/09537325.2018.1523385. [DOI] [Google Scholar]
- Coccia M. Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138474. Article Number: 138474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M. vol. 191. Environmental Research; 2020. An Index to Quantify Environmental Risk of Exposure to Future Epidemics of the COVID-19 and Similar Viral Agents: Theory and Practice. December, Article number 110155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M. How (Un)sustainable environments are related to the diffusion of COVID-19: the relation between coronavirus disease 2019, air pollution, wind resource and energy. Sustainability. 2020;12:9709. doi: 10.3390/su12229709. 2020. [DOI] [Google Scholar]
- Coccia M. How do low wind speeds and high levels of air pollution support the spread of COVID-19? Atmospheric Pollution Research, PII. 2020;(20):30293. doi: 10.1016/j.apr.2020.10.002. S1309-1042. 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M. Deep learning technology for improving cancer care in society: New directions in cancer imaging driven by artificial intelligence. Technology in Society. 2020;60 doi: 10.1016/j.techsoc.2019.101198. [DOI] [Google Scholar]
- Coccia M. Effects of the spread of COVID-19 on public health of polluted cities: results of the first wave for explaining the dejà vu in the second wave of COVID-19 pandemic and epidemics of future vital agents. Environ. Sci. Pollut. Control Ser. 2021;28(15):19147–19154. doi: 10.1007/s11356-020-11662-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M. The effects of atmospheric stability with low wind speed and of air pollution on the accelerated transmission dynamics of COVID-19. Int. J. Environ. Stud. 2021;78(1):1–27. doi: 10.1080/00207233.2020.1802937. [DOI] [Google Scholar]
- Coccia M. The relation between length of lockdown, numbers of infected people and deaths of Covid-19, and economic growth of countries: lessons learned to cope with future pandemics similar to Covid-19. Sci. Total Environ. 2021 doi: 10.1016/j.scitotenv.2021.145801. Available online 12 February 2021, 145801. [DOI] [Google Scholar]
- Coccia M. The impact of first and second wave of the COVID-19 pandemic: comparative analysis to support control measures to cope with negative effects of future infectious diseases in society. Environ. Res. 2021;111099 doi: 10.1016/j.envres.2021.111099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M., Watts J. A theory of the evolution of technology: technological parasitism and the implications for innovation management. Journal of Engineering and Technology Management. 2020;55 doi: 10.1016/j.jengtecman.2019.11.003. [DOI] [Google Scholar]
- Cohen-Mansfield J. COVID-19 and older adults in Israel – common challenges and recommendations. Qual. Ageing. 2020;21(4):209–216. [Google Scholar]
- Copat C., Cristaldi A., Fiore M., Conti G.O., Ferrante M. The role of air pollution (PM and NO2) in COVID-19 spread and lethality: a systematic review. Environ. Res. 2020;191:110129. doi: 10.1016/j.envres.2020.110129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID-19 pandemic lockdowns . Wikipidia, Template: COVID-19 Pandemic Lockdowns. 2021. https://en.wikipedia.org/wiki/Template:COVID-19_pandemic_lockdowns accessed 4th January 2021. [Google Scholar]
- DeRoo Schaffer S., Pudalov N.J., Fu L.Y. Planning for a COVID-19 vaccination program. J. Am. Med. Assoc. 2020;323(24):2458–2459. doi: 10.1001/jama.2020.8711. [DOI] [PubMed] [Google Scholar]
- European Centre for Disease Prevention and Control . 2021. Risk Factors and Risk Groups.https://www.ecdc.europa.eu/en/covid-19/latest-evidence/epidemiology [Google Scholar]
- Evans S., Bahrami H. Super-flexibility in practice: insights from a crisis. Global J. Flex. Syst. Manag. 2020;21(3):207–214. doi: 10.1007/s40171-020-00246-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flaxman S., Mishra S., Gandy A., Unwin H.J.T., Mellan T.A., Coupland H., Bhatt S. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020 doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- Frederiksen L., Zhang Y., Foged C., Thakur A. The long road toward COVID-19 herd immunity: vaccine platform technologies and mass immunization strategies. Front. Immunol. 2020;11:1817. doi: 10.3389/fimmu.2020.01817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaffney A., Himmelstein D.U., Woolhandler S. COVID-19 and US health financing: perils and possibilities. Int. J. Health Serv. 2020;50(4):396–407. doi: 10.1177/0020731420931431. [DOI] [PubMed] [Google Scholar]
- Gatto M., Bertuzzo E., Mari L., Miccoli S., Carraro L., Casagrandi R., Rinaldo A. Spread and dynamics of the COVID-19 epidemic in Italy: effects of emergency containment measures. Proceedings of the National Academy of Sciences May. 2020;117:10484–10491. doi: 10.1073/pnas.2004978117. 19. https://doi.org/10.1073/pnas.2004978117, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glencross D.A., Tzer-Ren H., Nuria C., Hawrylowicz C.M., Pfeffer P.E. Air pollution and its effects on the immune system. Free Radic. Biol. Med. 2020 doi: 10.1016/j.freeradbiomed.2020.01.179. (in press) [DOI] [PubMed] [Google Scholar]
- González-Bustamante B. Evolution and early government responses to COVID-19 in South America. World Dev. 2021;137:105180. doi: 10.1016/j.worlddev.2020.105180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo L., Luo J., Yuan M., Huang Y., Shen H., Li T. The influence of urban planning factors on PM2.5 pollution exposure and implications: a case study in China based on remote sensing, LBS, and GIS data. Sci. Total Environ. 2019;659:1585–1596. doi: 10.1016/j.scitotenv.2018.12.448. [DOI] [PubMed] [Google Scholar]
- Harrison E.A., Wu J.W. Vaccine confidence in the time of COVID-19. Eur. J. Epidemiol. 2020;35(4):325–330. doi: 10.1007/s10654-020-00634-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu J., Li C., Wang S., Li T., Zhang H. Genetic variants are identified to increase risk of COVID-19 related mortality from UK Biobank data. Hum. Genom. 2021;15(1):10. doi: 10.1186/s40246-021-00306-7. 2021 Feb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyanda A.E., Adeleke R., Lu Y., et al. A retrospective cross-national examination of COVID-19 outbreak in 175 countries: a multiscale geographically weighted regression analysis (January 11-June 28, 2020) Journal of Infection and Public Health. 2020;13(10):1438–1445. doi: 10.1016/j.jiph.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen M., van der Voort H. Agile and adaptive governance in crisis response: lessons from the COVID-19 pandemic. Int. J. Inf. Manag. 2020;55 doi: 10.1016/j.ijinfomgt.2020.102180. Article number 102180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin H., Qian X. How the Chinese government has done with public health from the perspective of the evaluation and comparison about public-health expenditure. Int. J. Environ. Res. Publ. Health. 2020;17(24):1–16. doi: 10.3390/ijerph17249272. 9272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns Hopkins Center for System Science and Engineering . 2021. Coronavirus COVID-19 Global Cases.https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 [Google Scholar]
- Kapitsinis N. The underlying factors of the COVID-19 spatially uneven spread. Initial evidence from regions in nine EU countries. Regional Science Policy and Practice. 2020;12(6):1027–1045. [Google Scholar]
- Kavitha C., Madhavaprasad D. The trajectory of corona virus: covid 19 around the world. Disaster Advances. 2020;13(10):98. [Google Scholar]
- Lau H., Khosrawipour T., Kocbach P., Ichii H., Bania J., Khosrawipour V. Evaluating the massive underreporting and undertesting of COVID-19 cases in multiple global epicenters. Pulmonology. 2021;27(2):110–115. doi: 10.1016/j.pulmoe.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z., Magal P., Webb G. Predicting the number of reported and unreported cases for the COVID-19 epidemics in China, South Korea, Italy, France, Germany and United Kingdom. J. Theor. Biol. 2021;509:110501. doi: 10.1016/j.jtbi.2020.110501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marazziti D., Cianconi P., Mucci F., Foresi L., Chiarantini I., Della Vecchia A. Climate change, environment pollution, COVID-19 pandemic and mental health. Sci. Total Environ. 2021;773:145182. doi: 10.1016/j.scitotenv.2021.145182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martelletti L., Martelletti P. Air pollution and the novel covid-19 disease: a putative disease risk factor. Sn compr. Clin. Med. 2020:1–5. doi: 10.1007/s42399-020-00274-4. https://doi.org/10.1007/s42399-020-00274-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perone G. The determinants of COVID-19 case fatality rate (CFR) in the Italian regions and provinces: an analysis of environmental, demographic, and healthcare factors. Sci. Total Environ. 2021;755:142523. doi: 10.1016/j.scitotenv.2020.142523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prem K., Liu Y., Russell T.W., Kucharski A.J., Eggo R.M., Davies N., et al. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. The Lancet Public Health, March. 2020;25:2020. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reilly J.M., Chen Y.-H.H., Jacoby H.D. The covid-19 effect on the paris agreement. Humanities & Social Sciences Communications. 2021;8(16) doi: 10.1057/s41599-020-00698-2. [DOI] [Google Scholar]
- Renardy M., Eisenberg M., Kirschner D. Predicting the second wave of COVID-19 in washtenaw county, MI. J. Theor. Biol. 2020;507 doi: 10.1016/j.jtbi.2020.110461. 21 December 2020, Article number 110461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosario Denes K.A., Mutz Yhan S., Bernardes Patricia C., Conte-Junior Carlos A. Relationship between COVID-19 and weather: case study in a tropical country. Int. J. Hyg Environ. Health. 2020;229:113587. doi: 10.1016/j.ijheh.2020.113587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabat I., Neuman-Böhme S., Varghese N.E., Barros P.P., Brouwer W., van Exel J., Schreyögg J., Stargardt T. United but divided: policy responses and people's perceptions in the EU during the COVID-19 outbreak. Health Pol. 2020;124(9):909–918. doi: 10.1016/j.healthpol.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman B., Ferranna M., Bloom D.E. Social determinants of mortality from COVID-19: a simulation study using NHANES. PLoS Med. 2021;18(1) doi: 10.1371/journal.pmed.1003490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siafakas N., Bizymi N., Mathioudakis A., Corlateanu A. EARLY versus MILD chronic obstructive pulmonary disease (COPD) Respir. Med. 2018;140:127–131. doi: 10.1016/j.rmed.2018.06.007. [DOI] [PubMed] [Google Scholar]
- Siddiqui A.F., Wiederkehr M., Rozanova L., Flahault A. Situation of India in the COVID-19 pandemic: India's initial pandemic experience. Int. J. Environ. Res. Publ. Health. 2020;17(23):1–18. doi: 10.3390/ijerph17238994. 8994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon J., Helter T.M., White R.G., van der Boor C., Łaszewska A. Impacts of the Covid-19 lockdown and relevant vulnerabilities on capability well-being, mental health and social support: an Austrian survey study. BMC Publ. Health. 2021;21(1):314. doi: 10.1186/s12889-021-10351-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stribling J., Clifton A., McGill G., de Vries K. Examining the UK Covid-19 mortality paradox: pandemic preparedness, healthcare expenditure, and the nursing workforce. J. Adv. Nurs. 2020;76(12):3218–3227. doi: 10.1111/jan.14562. [DOI] [PubMed] [Google Scholar]
- Tian T., Zhang J., Hu L., Jiang Y., Duan C., Li Z., Wang X., Zhang H. Risk factors associated with mortality of COVID-19 in 3125 counties of the United States. Infectious diseases of poverty. 2021;10(1):3. doi: 10.1186/s40249-020-00786-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobías A. Evaluation of the lockdowns for the SARS-CoV-2 epidemic in Italy and Spain after one month follow up. Sci. Total Environ. 2020;725:138539. doi: 10.1016/j.scitotenv.2020.138539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Who . 2020. Estimating Mortality from COVID-19, Scientific Brief.https://www.who.int/news-room/commentaries/detail/estimating-mortality-from-covid-19 4 August. 6 May 2021. [Google Scholar]
- Wilson N., Kvalsvig A., Barnard L., et al. Case-fatality risk estimates for COVID-19 calculated by using a lag time for fatality. Emerg. Infect. Dis. 2020;26(6):1339–1441. doi: 10.3201/eid2606.200320. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank . 2020. World Development Indicators Database. GDP Per Capita, PPP (Current International $)https://data.worldbank.org/indicator/NY.GDP.PCAP.PP.CD License: CC BY-4.0. [Google Scholar]
- World Bank World health organization global health expenditure database. Domestic general government health expenditure (% of GDP). License: CC BY-4.0. 2020. https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS
- World Bank World Health Organization Global Health Expenditure database. Domestic general government health expenditure per capita, PPP (current international $) 2020. https://data.worldbank.org/indicator/SH.XPD.GHED.PP.CD License: CC BY-4.0.
- World Bank World Bank staff estimates based on age/sex distributions of United Nations Population Division's World Population Prospects: 2019 Revision. Population ages 65 and above (% of total population. License: CC BY-4.0. 2020. https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS
- World Bank . In: 2017, for the Global Burden of Disease Study 2017. License: CC BY-4.0. Brauer M., et al., editors. 2020. PM2.5 air pollution, population exposed to levels exceeding WHO guideline value (% of total)https://data.worldbank.org/indicator/EN.ATM.PM25.MC.ZS [Google Scholar]