An effective critical surge response to Mayotte’s second COVID-19 wave
Since the beginning of the COVID-19 outbreak in China in December 2019, nearly 120 million people have been infected, and more than 2,5 million died worldwide by the end of March 2021 [1]. Despite strict public health measures in the most affected countries and a large-scale vaccination strategy, the repetition of epidemic waves still takes its heavy toll partly because of the emergence of virus variants.
In France, as in other countries, the uneven regional distribution between intensive care units (ICU) capacities and the number of COVID-19 cases has led to several hospitals’ saturation, requiring national coordination of resources. The French Military Health Service (FMHS) has thus intervened on several occasions in support of public healthcare structures: deploying mobile military intensive care unit in Mulhouse, Guadeloupe, Mayotte, and French Guiana; and performing collective airborne (plane and helicopter), railroad, and naval transport of critically ill patients [2], [3], [4], [5].
In February 2021, Mayotte island faced a second COVID-19 wave due to the highly contagious SARS-CoV-2 501Y.V2 South African variant, saturating the unique ICU of the Mayotte hospital. On the 3rd of February 2021, the order has been given to deploy a mobile military ICU (Module Militaire de Réanimation du Service de Santé des Armées – MMRSSA) to support the island.
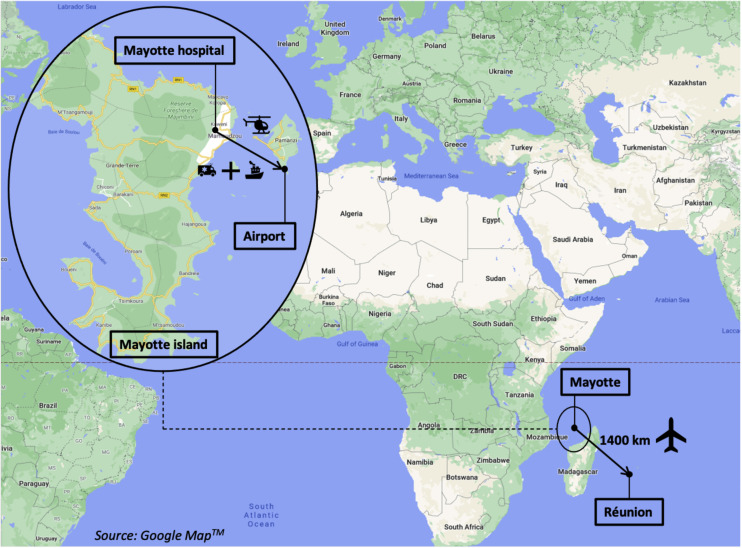
Mayotte is a French overseas department of 280,000 people located southeast of Africa, near Madagascar. The only hospital on the island is a 411-bed structure located in Mamoudzou with a single 16-bed ICU. The closest other ICU is located in the Reunion Island, 1400 km away.
Since the beginning of the pandemic, FMHS identified each month a rapid response ICU team that can be deployed anywhere in France on short notice. The MMRSSA was ordered to deploy in Mayotte on the 3rd of February; the first team of 37 people took off from Paris on the 5th of February, starting work in the ICU on the 8th of February (initial capacity of 5 beds). A second team arrived on the 16th of February to expand the ICU capacity to 10 beds.
Autonomy and complementarity with the Mayotte Hospital
The objective of the MMR was to create a functionally autonomous ICU in terms of human resources. The medical and paramedical staff consisted of personals from the eight French military training hospitals and soldiers from the Régiment Médical (RMED – Medical Regiment). We built four paramedical teams, each staffed by four nurses (including one certified registered nurse anaesthetist), three assistant nurses, and one soldier from the RMED working 12 h shift, following French recommendations on structural and organisational requirements for ICUs. Two anaesthesiologists/intensive care physicians worked in the ICU during the daytime and one at night. A physiotherapist, a pharmaceutical assistant, a medical secretary, and a head nurse also worked during the day. As of the 16th of February, the MMRSSA was fully operational and composed of 54 people in a 10-bed ICU.
A military plane discharged in Mayotte on the 6th of February. The medical equipment needed to open up to 6 ICU beds, including turbine-driven ventilators, one portable ultrasound system and two portable blood gas analysers. Using equipment on loan from the Mayotte hospital, ten beds were successfully opened.
The MMRSSA was placed under the command of a senior anaesthesiologist/intensivist physician, assisted by a head nurse and a RMED officer.
About half of the nurses and assistant nurses came from an intensive care background. The physicians provided ongoing training to all the paramedics of the MMRSSA during the mission on rest days.
The MMRSSA was integrated as a new ICU of the Mayotte hospital; communication was permanent between the medical teams. Civilian intensivists performed medical regulation, including patient assessment in emergency and medical wards, ensuring that each patient was at the right place to receive adequate treatment. If the patient needed extrarenal purification or extracorporeal oxygenation, the patient was transferred to the civilian ICU.
Medical support services, including plain X-ray, CT-scanner, biochemistry, haematology, and microbiology, were provided by the Mayotte hospital.
Patient flow management – avoiding ICU saturation
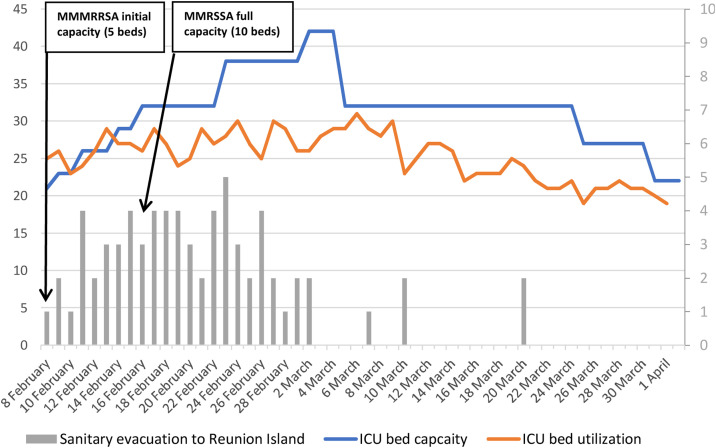
Before the MMRSSA deployment, the Mayotte hospital increased its ICU beds from 16 to 22. The swift reorganisation of ICU capabilities thanks to the MMRSSA and the appointment of civilian healthcare givers from metropolitan France increased ICU bed total capacity by 100%. At the height of the epidemic, four different ICUs were operational: the main 16-bed ICU, a 6-bed ICU in a post-anaesthesia care unit, a 10-bed ICU in the emergency department, and a 10-bed ICU in the ambulatory surgical ward. However, the constant flow of patients needing intensive care (up to 35 in a week), threatening to overwhelm Mayotte ICU capacities, forced us to evacuate as many patients as possible to the Reunion Island. From the 3rd of February to the 5th of March, 74 ICU patients were transported by aeromedical evacuation. Thanks to this rigorous organisation, all the patients requiring intensive care have been taken care of, and the “glass ceiling” of ICU saturation has never been broken (Fig. 1 ).
Fig. 1.
Evolution of ICU capacity in Mayotte Hospital.
Overall activity
From the 8th of February to the 1st of April 2021, 61 critically ill SARS-CoV-2 patients were transferred into the MMRSSA field hospital. Table 1 summarises the main characteristics of the patients, and their outcomes.
Table 1.
Patients’ characteristics and outcomes.
| Characteristics | Patients (n = 61) |
|---|---|
| Age, year, mean (SD) | 58 (12) |
| Sex, male, % | 39 (64) |
| Body mass index, kg/m2, mean (SD) | 31.3 (7) |
| Chronic medical illness, n (%) | |
| Hypertension | 35 (58.3) |
| Diabetes | 26 (43.3) |
| Immunocompromised | 4 (6.7) |
| Chronic obstructive pulmonary disease | 2 (3.3) |
| Pregnancy, n (%) | 2 (3.3) |
| SOFA score on admission, mean (SD) | 3.43 (1.82) |
| SAPS II score, mean (SD) | 34.4 (10.5) |
| Clinical frailty scale, mean (SD) | 2.8 (1.4) |
| Admission location n (%) | |
| Civilian ICU | 35 (57) |
| Emergency department | 14 (23) |
| Ward (medical or surgical) | 12 (20) |
| Ventilation strategy, n (%) | |
| Invasive mechanical ventilation | 50 (82) |
| Non-invasive (NIV or HFOT) | 11 (18) |
| Continuous neuromuscular blocking agents perfusion | 43 (70.5) |
| Prone positioning | 25 (40.9) |
| Nitric oxide inhalation | 3 (4.9) |
| Length of stay in ICU, day, mean (SD) | 8 (7.8) |
| Outcome at MMR ICU discharge, n (%) | |
| Evacuation to Reunion Island | 33 (54.1) |
| Transfer to civilian ICU | 4 (6.5) |
| For ECMO therapy | 2 (3.3) |
| Death | 7 (11.5) |
| Withdrawal of life-sustaining treatment | 3 (4.9) |
| Ward | 17 (27.9) |
SOFA: Sequential organ failure assessment; SAPS II: simplified acute physiology score; NIV: Non-invasive ventilation; OHFT: High-flow oxygen therapy; ECMO: Extracorporeal membrane oxygenation.
The respiratory support strategies driven for these ARDS COVID-19 patients included protective mechanical ventilation, perfusion of neuromuscular blocking agents, prone positioning, recruitment manoeuvres, and inhalation of nitric oxide if indicated for each of these propositions. Figure 2 shows Mayotte Island's geographical location and means of transport used for sanitary evacuations.
Fig. 2.
Geographical location of Mayotte and Reunion Island and means of transport used for sanitary evacuations.
Conclusion
We describe one of the FMHS responses to the COVID-19 pandemic in France. Swift deployment, rapid augmentation of capabilities, adaptability, and good civil-military cooperation were the key elements of a successful mission.
Conflicts of interest
The authors declare no conflict of interest. No funding sources.
Acknowledgments
The authors thank all the teams involved in this operation: Dr. Jean Derely, Dr. Alain Benois, health caregivers, and the RMED personals. Moreover, the authors pay a great tribute to the Mayotte hospital’s ICU teams: Dr. Renaud Blondé, Dr. Yvonnick Boué, and their collaborators.
References
- 1.John Hopkins University Coronavirus Resource Center. 2021. https://coronavirus.jhu.edu/map.html . [Accessed 11 March 2021] [Google Scholar]
- 2.Danguy des Déserts M., Mathais Q., Luft A., Escarment J., Pasquier P. Conception and deployment of a 30-bed field military intensive care hospital in Eastern France during the 2020 COVID-19 pandemic. Anaesth Crit Care Pain Med. 2020;39(June (3)):361–362. doi: 10.1016/j.accpm.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boutonnet M., Turc J., Dupre H.L., Paris R., Muller V. “MoRPHEE” fighting COVID-19. Anaesth Crit Care Pain Med. 2020;39(June (3)):363–364. doi: 10.1016/j.accpm.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turc J., Dupré H.L., Beaussac M., Murris S., Koch L., Paris R. Collective aeromedical transport of COVID-19 critically ill patients in Europe: a retrospective study. Anaesth Crit Care Pain Med. 2020;(November) doi: 10.1016/j.accpm.2020.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nguyen C., Montcriol A., Janvier F., Cungi PJ, Esnault P., Mathais Q. Critical COVID-19 patient evacuation on an amphibious assault ship: feasibility and safety. A case series. BMJ Mil Health. 2020;(August) doi: 10.1136/bmjmilitary-2020-001520. bmjmilitary-2020-001520. Online ahead of print. [DOI] [PubMed] [Google Scholar]