Abstract
BACKGROUND: Intra-arterial therapies for acute ischemic stroke are increasingly available. Intravenous therapy (IV) followed immediately by intra-arterial therapy (IA) has been shown to be safe, but such therapy is resource intensive. Selecting the best patients for this therapy may be accomplished with the use of baseline neuroimaging.
METHODS: We used data from the IMS-1 and National Institute for Neurological Disorders and Stroke tissue plasminogen activator (tPA) stroke studies to compare outcomes among IV-IA tPA, IV-tPA, and placebo treatment stratified by the baseline CT scan appearance. The CT scans were scored using the Alberta Stroke Program Early CT (ASPECT) score and dichotomized into ASPECT score > 7 (favorable scan) and ASPECT score ≤ 7 (unfavorable scan). Logistic regression was used to assess for an ASPECT score by treatment interaction.
RESULTS: A total of 460 patients was included. Age and sex were similar among the 3 groups. The IV-IA tPA cohort had a higher median National Institutes of Health stroke scale (NIHSS) score (18 versus 17) compared with the IV tPA cohort. The proportion of patients with favorable CT scans (ASPECT score > 7) was lowest in the IV-IA tPA group. A multiplicative interaction effect was shown indicating that patients with an ASPECT score > 7 in the IV-IA cohort were more likely to have a good outcome compared with IV tPA and with placebo. Harm may accrue to patients treated with IV-IA therapy who have an unfavorable baseline CT scan appearance.
CONCLUSIONS: Patients with a favorable baseline CT scan appearance are the most likely to benefit from IV-IA therapy. This hypothesis will be tested in the IMS-3 study.
Intra-arterial therapies for acute ischemic stroke now include chemical and mechanical methods.1,2 The Prolyse in Acute Cerebral Thromboembolism (PROACT)-2 study demonstrated the efficacy of intra-arterial pro-urokinase among patients with proved middle cerebral artery (MCA) occlusion.3 Furthermore, although combination intravenous (IV) followed immediately by intra-arterial (IA) therapy has been shown to be safe, a larger efficacy trial of the combined IV-IA approach is under way (IMS-3 trial).4 It remains unclear which patients particularly benefit from this aggressive and labor- and cost-intensive approach to acute stroke management.
Brain imaging may be one tool to identify stroke patients who will benefit from reperfusion therapy. Perfusion and diffusion MR imaging showing a substantial perfusion deficit and small diffusion lesion may define such patients. This approach, taken in the Desmoteplase in Acute Ischemic Stroke Trial (DIAS)-1 study, appears to be safe.5 However, recent work suggests that even “matched” lesions have substantial positron-emission tomography (PET) defined penumbral tissue.6 This implies that perfusion-diffusion mismatch on MR may have a high specificity but low sensitivity for identifying patients who would benefit from reperfusion. Methods for choosing patients using plain CT imaging have more immediate pragmatism given the widespread use of plain CT for imaging acute stroke patients. We have used the Alberta Stroke Program Early CT (ASPECT) score to rate ischemic change on the acute plain CT scan and shown it to be an excellent prognostic tool.7–9
A post hoc analysis of the PROACT-2 study has demonstrated that patients with a favorable appearance on their baseline CT scan, defined by an ASPECT score greater than 7, were 3 times more likely to achieve an independent functional outcome with treatment compared with placebo, even when those patients were treated approximately 5 hours from symptom onset.10 Patients with a baseline ASPECT score of less than or equal to 7, on average, did not benefit from intra-arterial pro-urokinase. However, although reanalysis of the National Institute for Neurological Disorders and Stroke (NINDS) tPA trial using ASPECT scores shows a trend to reduced mortality among patients with favorable baseline CT scans, no clear interaction between the baseline ASPECT score and treatment could be demonstrated.11
We sought to determine whether the baseline ASPECT score could predict which patients would particularly benefit from intravenous followed by intra-arterial tPA in the IMS-1 study.
Methods
The IMS-1 trial results and methods have been reported previously.4 In brief, the study used a safety and futility design, comparing historical control subjects from the NINDS tPA Stroke Study. A total of 80 patients with NIHSS scores ≥10 at baseline and aged ≤80 years were treated with IV followed by IA tPA. All patients received IV tPA at 0.6 mg/kg and all were treated within 3 hours of symptom onset. At angiography, 62 received additional IA tPA to a maximum dose of 22 mg. The study demonstrated the safety of this approach with a symptomatic intracerebral hemorrhage (ICH) rate of 6.3% (95% confidence interval [CI95] 2.1 to 14.0) and 90-day mortality of 16.3% (CI95 8.9 to 26.2). Although the direction of effect favored the combined IV-IA approach, there was no significant difference in 3-month outcome measures between the IMS-1 cohort and historical IV tPA-treated subjects from the NINDS tPA Stroke Study.
CT scans were acquired using contiguous noncontrast axial 5-mm sections. A minority of CT images were acquired using 10-mm axial sections. The power (kV and mA) and scan obliquity were not prespecified. All CT scans were acquired within 3 hours of stroke onset. ASPECT score is assessed by systematically scoring each of 10 regions on the CT scan and assigning a score of 1 for normal and 0 for a region showing signs of ischemia.7,8 Signs of ischemia are defined as X-ray hypoattenuation, loss of the gray-white boundary (which is due to X-ray hypoattenuation of the gray matter), and/or effacement of cortical sulci. Only new areas of acute ischemia are scored. All images from skull base to vertex are reviewed. The lower regions include the subcortical structures, which are allotted 3 points (C, caudate nucleus; L, lentiform nucleus; and IC, internal capsule—genu and posterior limb only) and the MCA cortex, which is allotted 4 points (insular cortex, M1, 2, 3). The upper regions are defined above the head of the caudate nucleus and include the MCA cortex, which is allotted 3 points (M4, 5, and 6). The score combines localization in the brain and volume into a semiquantitative topographic score. A score of 10 implies no evidence of new early signs of ischemia in the MCA territory and a progressively lower score indicates more extensive ischemic changes. ASPECTS was scored on all baseline and follow-up CT scans using a 3-person panel consensus method. Two stroke neurologists and 1 neuroradiologist jointly reviewed each baseline scan blind to all clinical outcomes and blind to the follow-up scan. A consensus score on each region of the ASPECT scoring system was reached with discussion. For the NINDS tPA Stroke Study, 2 panels of 3 readers each were constituted, and each panel reviewed half the scans (Fig 1). The reviewers were given knowledge of patient symptom side (ie, left or right hemiparesis, aphasia, or unknown) only, to mimic real-life clinical practice.
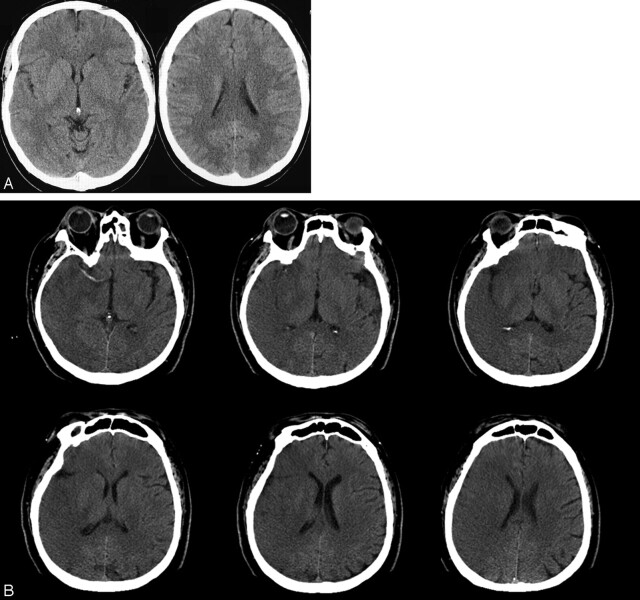
Fig 1.
A, Baseline CT scan at 100 minutes from stroke onset showing a left middle cerebral artery infarct with an ASPECT score of 8. Points are taken off for hypoattenuation of the head of caudate and the lentiform nuclei. Based upon our data, this patient would be an ideal candidate for IV-IA therapy.
B, Baseline CT scan at 175 minutes from stroke onset showing a well-evolved right middle cerebral artery infarct with an ASPECT score of 0. Based upon our data, this patient could be harmed by IV-IA therapy.
Symptomatic hemorrhage was scored by the trial neuroradiologists separately to the review of ASPECT score. Outcomes at 90 days on the modified Rankin Scale (mRS) and the National Institutes of Health stroke scale (NIHSS) were determined by trial personnel for each of the IMS-1 and the NINDS tPA Stroke Study.
Data from the IMS-1 patients were compared with a similar cohort from the NINDS tPA Stroke Study. Patients from the NINDS tPA Stroke Study who were ≤80 years of age and who had a baseline NIHSS score ≥10 made up the comparison group. Baseline characteristics are illustrated by using descriptive statistics. The ASPECT score was dichotomized at ≤7 (an “unfavorable” scan) and >7 (a “favorable” scan). The primary outcome was the mRS score dichotomized at mRS 0–1 versus mRS 2–6. Secondary outcome measures included mRS 0–2 versus 3–6, NIHSS 0–1 and 2–42. Safety outcomes were symptomatic ICH and death. A categoric treatment variable with 3 categories (placebo, IV tPA, and IV-IA tPA) was used with appropriate dummy variables in a logistic regression model. An interaction term, ASPECT score by tPA treatment was assessed within the logistic regression model. To better understand any interaction, simpler logistic regression models were constructed to examine the relationship between IV-IA tPA versus IV tPA treatment, IV-IA tPA versus placebo and IV tPA versus placebo. Logistic regression models were constructed using treatment allocation, ASPECT score dichotomized at 7, and the interaction between dichotomized ASPECT score and treatment assignment as forced variables. Adjustment for known predictors of outcome and potential confounders was done by considering age, sex, onset-to-treatment time, glucose, and baseline NIHSS score as principal covariables. Interaction terms for treatment by sex and treatment by onset-to-treatment time were also assessed based upon published literature.12,13 All analyses were by intention to treat so that patients in the IMS-1 group who received only IV therapy were considered part of the IV-IA group. Statistical significance was considered relevant at P = .05 for main effects variables and P = .10 for interaction terms.14 Analyses were conducted using STATA 8.2 (StataCorp, College Station, Tex).
Results
All patients from the IMS-1 (n = 80) and 380 patients from the NINDS tPA Stroke Study were included in this analysis (Table 1). From 393 patients in the NINDS tPA Stroke Study, the age and baseline NIHSS criteria were met. In an additional 13 patients, CT scan results were not available. One of these patients suffered a symptomatic ICH. Patients in the IV-IA group were more likely to have a lower ASPECT score, a lower glucose level, and a longer onset-to-treatment time. It is noteworthy that there was a gradient in the proportion of patients with favorable CT scans (ASPECT score > 7), with the largest proportion in the placebo group and the lowest in the IV-IA tPA treatment group (P = .001, test for trend). Because a higher ASPECT score is a strong prognostic variable, this could bias against good outcomes in the IV-IA tPA groups.
Table 1:
Baseline patient characteristics
| Placebo (N = 208)* |
IV tPA (N = 172)* |
IV-IA tPA (N = 80)† |
P | |
|---|---|---|---|---|
| Median (iqr) | ||||
| Baseline | ||||
| Age | 66 (58–72) | 69 (59–74) | 65 (54.5–75) | .229 |
| Gender (% female) | 44 | 42 | 50 | .513 |
| bNIHSS | 17 (13–22) | 17 (14–21) | 18 (14–21) | .857 |
| Glucose (mM) | 7.0 (6.0–8.75) | 6.9 (5.8–9.5) | 6.2 (5.6–7.3) | .0098 |
| bASPECTS | 8 (6–10) | 8 (6–10) | 7 (4–9) | .0003 |
| bASPECTS > 7 (%) | 62.5 | 57.0 | 37.5 | .001 |
| Onset-to-treat time (min) | 108.5 (89–150) | 90 (88–149) | 140 (110–158) | <.001 |
| Outcomes | ||||
| Death (%) | 24 | 20 | 16 | .361 |
| mRS 0–1 (%) | 18 | 33 | 30 | .002 |
| mRS 0–2 (%) | 28 | 40 | 43 | .016 |
| NIHSS 0–1 (%) | 15 | 25 | 28 | .013 |
| sICH (%) | 0.96 | 5.2 | 6.3 | .014 |
Note:—tPA indicates tissue plasminogen activator; iqr, interquartile range; bNIHSS, baseline National Institutes of Health Stroke score; ASPECTS, Alberta Stroke Program Early CT score; bASPECTS, baseline ASPECT score; mRS, modified Rankin Scale; sICH, symptomatic intracerebral hemorrhage.
From a subset of the NINDS tPA Stroke Study.
From the IMS-1 Trial.
There was no relationship between the baseline ASPECT score and onset-to-treatment time or age. Patients with unfavorable CT scans tended to have lower glucose (mean, 7.9 mmol/L compared with 8.6 mmol/L), (P = .08). In the entire cohort, patients with an ASPECT score >7 were more likely to have a lower NIHSS score (mean, 17) compared with ASPECT scores ≤7 (mean NIHSS, 19) (P = .0004).
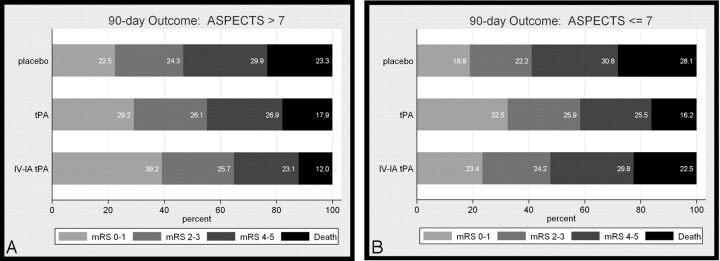
Logistic regression analysis showed a significant interaction between the baseline ASPECT score (dichotomized at 7) and treatment. This was true for multiple outcomes (mRS01, mRS02, NIHSS01) but not for death or symptomatic ICH (Table 2). Exploration of the interaction of treatment by time failed to show an interaction. Similarly, the gender by treatment interaction shown in a recent study was not evident in this group of patients.13 Further analysis to better understand the interaction showed that the major effect modification was with IV-IA tPA and ASPECT score (P = .016, interaction term). After adjustment for baseline NIHSS score, age, glucose, onset-to-treatment time, in the favorable CT scan group (ASPECT score > 7), 10% more of the patients in the IV-IA treatment compared with the IV treatment group achieved a mRS score 0–1. In the unfavorable CT scan group (ASPECT score ≤ 7), 9% fewer patients achieved a mRS score 0–1. As has been shown previously,11 there was no interaction effect of IV tPA alone and ASPECT score (P = .958, interaction term). Adjusted estimates of these proportions along the continuum of the mRS are shown in Fig 2.
Table 2:
Logistic regression analysis of outcome
| Variable | Outcome |
|||
|---|---|---|---|---|
| mRS 0–1 |
NIHSS 0–1 |
|||
| OR (CI) | P | OR (CI) | P | |
| Interaction ASPECTS > 7 by treatment | 1.8 (0.92–3.5) | .084 | 2.1 (1.1–4.2) | .036 |
| Age (y) | 0.95 (0.93–0.97) | <.0001 | 0.95 (0.93–0.97) | <.0001 |
| Baseline NIHSS | 0.86 (0.82–0.91) | <.0001 | 0.86 (0.81–0.91) | <.0001 |
| Onset-to-treatment time (min) | 0.99 (0.99–1.003) | .349 | 0.99–1.001 | .118 |
| Glucose (mM) | 0.95 (0.90–1.01) | .132 | 0.97 (0.90–1.03) | .305 |
Note:—mRS indicates modified Rankin Scale; ASPECTS, Alberta Stroke Program Early CT score; NIHSS, National Institutes of Health Stroke Scale Score; OR, odds ratio. The interpretation of the OR of an interaction term in a logistic regression model is not intuitive or necessarily meaningful clinically. The statistical significance of the interaction term implies that there is a differential treatment effect according to whether the baseline CT scan is favorable or unfavorable. In the presence of an interaction, the OR of the main effects variables are also not clinically meaningful and therefore are excluded from the table. As in previous analyses, age and baseline stroke severity are strong prognostic factors.
Fig 2.
Modified Rankin Scale outcomes at 90 days stratified by the baseline ASPECT score and adjusted using ordered logistic regression for baseline age, NIH Stroke Scale score, onset-to-treatment time, and baseline serum glucose.
We also assessed the cohort with a baseline NIHSS ≥20. A similar interaction effect was observed with the NIHSS 0–1 (P = .038, likelihood ratio test for interaction term) and mRS 0–2 (P = .071, likelihood ratio test for interaction term) outcomes, but not for mRS 0–1 (P = .161, likelihood ratio test for interaction term).
In addition, for the IMS-1 cohort only, we analyzed the baseline ASPECT score according to baseline lesion location (Table 3). There was a good correlation between more proximal arterial occlusion and lower ASPECT scores at baseline (Spearman ρ, 0.43, P < .0001).
Table 3:
ASPECT scores according to intracranial arterial lesion location for the IMS-1 cohort
| Occlusion Location (n) | ASPECTS (median, iqr) | ASPECTS > 7 (%, n/N) | Outcome: mRS 0–1 (%, n/N) |
|
|---|---|---|---|---|
| ASPECTS > 7 | ASPECTS ≤ 7 | |||
| Carotid T (15) | 4 (3–7) | 13% (2/15) | 0% (0/2) | 0% (0/13) |
| M1 (26) | 6 (4–8) | 31% (8/26) | 50% (4/8) | 17% (3/18) |
| M2 (20) | 7 (5–9.5) | 45% (9/20) | 33% (3/9) | 36% (4/11) |
| M3 (6) | 7 (5–9) | 33% (2/6) | 50% (1/2) | 50% (2/4) |
| None (6) | 10 (9–10) | 83% (5/6) | 60% (3/5) | 100% (1/1) |
| ACA (2) | 6.5 (3–10) | 50% (1/2) | 0% (0/1) | 100% (1/1) |
| VB (2) | 8.5 (8–9) | 100% (2/2) | 50% (1/2) | — |
Note:—Three patients did not undergo angiography and thus lesion location was not determined. Intracranial arterial lesion location was determined independent of any extracranial artery occlusion. T indicates carotid T occlusion; M1, M1 segment middle cerebral artery; M2, M2 segment middle cerebral artery; M3, M3 segment middle cerebral artery; ACA, anterior cerebral artery; VB, vertebrobasilar arteries; ASPECTS, Alberta Stroke Program Early CT score; mRS, modified Rankin Scale score; iqr, interquartile range.
Discussion
Comparison of the IMS-1 patient cohort with historical NINDS tPA Stroke Study patients demonstrates that patients with favorable baseline CT scans (ASPECT score >7) do well with IV-IA therapy. The effect size is approximately 10% compared with IV therapy alone, indicating a number-needed-to-treat of 10. Careful review of the data show that the reason for the effect modification is both that patients with favorable scans (ASPECT score >7) do better and that patients with unfavorable scans (ASPECT score ≤7) do worse, without increasing mortality, with IV-IA treatment compared with IV treatment.
The biologic reasons for this effect are not immediately obvious. Patients treated with IV-IA therapy who had more substantial evidence of ischemia on the CT scan (lower ASPECT scores), were slightly more likely to suffer symptomatic ICH (risk ratio [RR] 1.7 [0.4–7.4]) compared with patients treated with IV tPA alone. However, this does not account for the substantially reduced benefit among patients with lower ASPECT scores. Only 5 patients in the IMS-1 cohort suffered symptomatic ICH; 2 had ASPECT scores >7 and 3 had ASPECT scores ≤7. Other factors independent from ischemic volume alone may contribute to ICH.15
There is a theoretic pathobiologic relationship between ASPECT score and time. As time elapses, ischemic processes evolve leading to tissue damage and change on the baseline CT scan. The determinants of infarction include the depth of ischemia (absolute cerebral blood flow), the duration of ischemia and the susceptibility of the individual. ASPECT score measurements are a result of these processes. ASPECT score may therefore serve, in part, as a surrogate for time elapsed since stroke onset and the severity of ischemia. However, in the current dataset, we could not demonstrate a confounding relationship between ASPECT score and time from stroke onset to treatment. This may simply represent a type II error as a result of lack of power.
We noted that the baseline ASPECT score was well correlated with intracranial arterial lesion location. The more proximal the lesion, the more unfavorable was the CT scan appearance. Although this result is intuitive, the outcomes according to lesion location were less so. Internal carotid artery T occlusion (all with unfavorable ASPECT scores) universally had poor outcomes. Patients with M1-MCA occlusion faired nearly 3-fold better if the baseline CT scan was favorable. For M2- and M3-MCA lesions, the baseline scan appearance was not as predictive of outcome. This latter could be a result of the initial bolus of intravenous tPA causing migration of more proximal thrombi into the distal vascular bed. This effect of ASPECT score predicting lesion location is consistent with previous observations.16
Recent data have suggested that the promise of multimodal MR imaging in acute stroke is beginning to be realized.5,17 MR imaging can detect blood more accurately than CT18; MR imaging can identify a measure of penumbra (mean transit time and time to peak to diffusion-weighted imaging mismatch); MRA can detect arterial occlusions as the target for thrombolysis. However, acute MR does remain limited worldwide. A significant minority of acute stroke patients cannot be imaged with MR because of direct contraindications (eg, pacemaker) or indirect contraindications (eg, inability to safely nurse patients because of vomiting or unstable cardiac status).19,20 Although the latter are potentially remediable, the need for CT brain imaging remains. Meanwhile, the relevance of our study is anchored in the fact that CT is faster, is the current standard for prethrombolytic imaging, and is globally more available compared with MR imaging.
This analysis is hypothesis generating. The limitations of comparison with historical rather than contemporary control subjects cannot be overstated. We note that there is a gap of more than decade between the 2 studies. Improvements in CT technology and changes in CT protocols such as the change from 10- to 5-mm section thickness may have biased the assessment of ASPECT score. Nevertheless, the present analysis and previous data from the PROACT II study suggest substantially reduced efficacy of intra-arterial approaches to acute stroke when there is evidence of substantial damage on the baseline CT scan. Confirmation of this observation will be sought in the IMS-3 study, where randomization will ensure balance in time-to-treatment and baseline ASPECT and NIHSS scores between the IV and IV-IA treatment groups.
Acknowledgments
We acknowledge the additional reviewers of the NINDS tPA Stroke Study CT scans: Brian Silver, Steven Levine, Suresh Patel, and Philip A. Barber.
Footnotes
Both the IMS-1 study and the National Institute for Neurological Disorders and Stroke (NINDS) tPA Stroke Study were funded by NINDS at the NIH. M.D.H. was funded by the Heart & Stroke Foundation of Alberta, Northwest Territory, and Nunavut, and the Canadian Institutes for Health Research (CIHR). A.M.D. was funded by the Alberta Heritage Foundation for Medical Research and the CIHR.
References
- 1.Becker KJ, Brott TG. Approval of the MERCI clot retriever: a critical view. Stroke 2005;36:400–03 [DOI] [PubMed] [Google Scholar]
- 2.Gobin YP, Starkman S, Duckwiler GR, et al. MERCI 1: A phase 1 study of mechanical embolus removal in cerebral ischemia. Stroke 2004;35:2848–54 [DOI] [PubMed] [Google Scholar]
- 3.Furlan A, Higashida R, Wechsler L, et al. Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA 1999;282:2003–11 [DOI] [PubMed] [Google Scholar]
- 4.Combined intravenous and intra-arterial recanalization for acute ischemic stroke: the Interventional Management of Stroke Study. Stroke 2004;35:904–11 [DOI] [PubMed] [Google Scholar]
- 5.Hacke W, Albers G, Al-Rawi Y, et al. The Desmoteplase in Acute Ischemic Stroke Trial (DIAS): a phase II MRI-based 9-hour window acute stroke thrombolysis trial with intravenous desmoteplase. Stroke 2005;36:66–73 [DOI] [PubMed] [Google Scholar]
- 6.Guadagno JV, Warburton EA, Aigbirhio FI, et al. Does the acute diffusion-weighted imaging lesion represent penumbra as well as core? A combined quantitative PET/MRI voxel-based study. J Cereb Blood Flow Metab 2004;24:1249–54 [DOI] [PubMed] [Google Scholar]
- 7.Barber PA, Demchuk AM, Zhang J, et al. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score [published erratum appears in Lancet 2000;355:2170]. Lancet 2000;355:1670–74. [DOI] [PubMed] [Google Scholar]
- 8.Pexman JH, Barber PA, Hill MD, et al. Use of the Alberta Stroke Program Early CT Score (ASPECTS) for assessing CT scans in patients with acute stroke. AJNR Am J Neuroradiol 2001;22:1534–42 [PMC free article] [PubMed] [Google Scholar]
- 9.Coutts SB, Demchuk AM, Barber PA, et al. Interobserver variation of ASPECTS in real time. Stroke 2004;35:e103–05 [DOI] [PubMed] [Google Scholar]
- 10.Hill MD, Rowley HA, Adler F, et al. Selection of acute ischemic stroke patients for intra-arterial thrombolysis with pro-urokinase by using ASPECTS. Stroke 2003;34:1925–31 [DOI] [PubMed] [Google Scholar]
- 11.Demchuk AM, Hill MD, Barber PA, et al. Importance of early ischemic computed tomography changes using ASPECTS in NINDS rtPA Stroke Study. Stroke 2005;36:2110–15 [DOI] [PubMed] [Google Scholar]
- 12.Marler JR, Tilley BC, Lu M, et al. Early stroke treatment associated with better outcome: the NINDS rt-PA stroke study. Neurology 2000;55:1649–55 [DOI] [PubMed] [Google Scholar]
- 13.Kent DM, Price LL, Ringleb P, et al. Sex-based differences in response to recombinant tissue plasminogen activator in acute ischemic stroke: a pooled analysis of randomized clinical trials. Stroke 2005;36:62–65 [DOI] [PubMed] [Google Scholar]
- 14.Anonymous. Generalized efficacy of t-PA for acute stroke. Subgroup analysis of the NINDS t-PA Stroke Trial. Stroke 1997;28:2119–25 [DOI] [PubMed] [Google Scholar]
- 15.Khatri P, Broderick J, Khoury J, et al. Microcatheter contrast injections during intraarterial thrombolysis increase intracranial hemorrhage risk. Stroke 2006;37:622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barber PA, Demchuk AM, Hill MD, et al. The probability of middle cerebral artery MRA flow signal abnormality with quantified CT ischaemic change: targets for future therapeutic studies. J Neurol Neurosurg Psychiatry 2004;75:1426–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Furlan AJ, Eyding D, Albers GW, et al. Dose escalation of desmoteplase for acute ischemic stroke (DEDAS): Evidence of safety and efficacy 3 to 9 hours after stroke onset. Stroke 2006;37:1227–31 [DOI] [PubMed] [Google Scholar]
- 18.Kidwell CS, Chalela JA, Saver JL, et al. Comparison of MRI and CT for detection of acute intracerebral hemorrhage. JAMA 2004;292:1823–30 [DOI] [PubMed] [Google Scholar]
- 19.Barber PA, Hill MD, Eliasziw M, et al. Imaging of the brain in acute ischaemic stroke: comparison of computed tomography and magnetic resonance diffusion-weighted imaging. J Neurol Neurosurg Psychiatry 2005;76:1528–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hand PJ, Wardlaw JM, Rowat AM, et al. Magnetic resonance brain imaging in patients with acute stroke: feasibility and patient related difficulties. J Neurol Neurosurg Psychiatry 2005;76:1525–27 [DOI] [PMC free article] [PubMed] [Google Scholar]