Abstract
Introduction
The role of tourniquet during knee arthroplasty is controversial. The present study compares various tourniquet protocols using a Bayesian network meta-analysis of peri-operative data.
Material and methods
The present study was conducted in accordance with the PRISMA extension statement for reporting systematic reviews incorporating network meta-analyses of health interventions. The literature search was conducted in September 2020. All clinical trials investigating the role of tourniquet in knee arthroplasty were considered for inclusion. Methodological quality was assessed using Review Manager 5.3. A Bayesian hierarchical random-effects model analysis was used in all comparisons.
Results
Ultimately, pooled data from 68 studies (7413 procedures) were analysed. Significant inconsistency was found in the data relating to total estimated blood lost; no assumption could be made on this outcome. Full-time tourniquet resulted in the shortest surgical duration and lowest intra-operative blood lost, in both cases followed by incision-to-suture. The incision-to-suture protocol achieved the smallest drop in haemoglobin during the first 72 h post-operatively and the lowest rate of blood transfusion, both followed by full-time tourniquet. Hospitalisation was shortest in the absence (no-tourniquet) group, followed by the cementation-to-end group.
Conclusion
For knee arthroplasty, longer tourniquet use is associated with the shorter duration of surgery, lower intra-operative blood lost, lower drops in haemoglobin and fewer transfusion units. The shortest average hospitalisation was associated with no tourniquet use.
Keywords: Bayesian network meta-analysis, Knee arthroplasty, Tourniquet
Introduction
The use of pneumatic tourniquet in surgery was first described by Sir Harvey Cushing in 1904. [1] Tourniquets are used frequently in orthopaedic procedures. The American Association of Hip and Knee Surgeons has reported that approximately 95% of surgeons use tourniquets in some form during knee arthroplasty [2]. Using a tourniquet reduces intraoperative blood loss [3, 4] and optimizes visualisation, thereby shortening surgical duration [5, 6]. It has been also hypothesized that the use of tourniquet may improve cement penetration, but results from clinical trials are controversial [7–9]. Between no tourniquet and full-time use of tourniquet, various timing protocols are routinely advocated: from skin incision to cement hardening, only during the cementation phase, from cement hardening to the end of procedure, from incision to wound closure. Despite the high number of clinical trials and reviews addressing tourniquet use, no consensus has been reached regarding the optimal tourniquet protocol for knee arthroplasty [10–14]. To date, no studies have been performed comparing peri-operative outcomes associated with the most common tourniquet protocols during knee arthroplasty. The present Bayesian network meta-analysis was therefore conducted to study the following outcomes: duration of surgery, intraoperative blood loss, total estimated blood loss, haemoglobin drop, blood units transfused, length of hospitalisation.
Material and methods
Search strategy
The present Bayesian network meta-analysis was conducted in accordance with the PRISMA extension statement for reporting systematic reviews incorporating network meta-analyses of health interventions [15]. The PICO algorithm was defined as.
P (Population): primary knee arthroplasty;
I (Intervention): effect of tourniquet;
C (Comparison): tourniquet duration;
O (Outcomes): peri-operative data.
Literature search
The literature search was performed independently by two authors (FM, AB). In September 2020, the main online databases were accessed: Pubmed, Google Scholar, Scopus, EMBASE. The following keywords were used in combination: knee, arthroplasty, replacement, prosthesis, outcomes, treatment, surgery, therapy, tourniquet, surgical, hospitalisation, length duration, transfusion, blood lost, hb, haemoglobin. Resulting titles were screened and their abstracts read. If the study was of interest, the full text was accessed. Bibliographies were also screened. Disagreements between reviewers were solved by a third author (MT).
Eligibility criteria
All clinical trials evaluating the role of tourniquets during knee arthroplasty were considered. Following the Oxford Centre for Evidenced-Based Medicine (OEBM) [16], only articles with level I to III evidence were included for analysis. The search was limited to articles in English, Italian, German, French and Spanish, according to the language capabilities of the authors. Various types of implant were considered (e.g., cemented or uncemented, uni-compartimental or total component, cruciate retaining or bi-retaining or sacrificing), as were all common surgical approaches (e.g. medial parapatellar, quadriceps sparing, mid-vastus, sub-vastus). No distinction was made between minimally invasive and standard surgery. Different types of tourniquets and inflation pressures, as well as interventions incorporating navigation systems, were also considered. Reviews, case series, editorials, letters and expert opinions were not considered, nor were biomechanical, animal and cadaveric studies. Also excluded were data from knee arthroplasties following any kind of trauma, revision surgeries, and articles missing quantitative data concerning the outcomes of interest.
Outcomes of interest
Two independent authors (FM, AB) extracted the data of interest. The following demographics were collected: author, year, journal, type of study, type of implant, tourniquet protocol, tourniquet pressure, number of procedures, mean age and BMI, percentage of female gender. Outcomes of interest were hospitalisation length, duration of surgery, intraoperative and total estimated blood loss, haemoglobin (Hb) values, transfusion rate of packed red blood cells.
Methodological quality assessment
The methodological quality assessment was performed using Review Manager 5.3 (Nordic Cochrane Collaboration, Copenhagen) and its risk-of-bias summary tool. Six items from each study were evaluated: randomization (selection bias), allocation (selection bias), blinding method (detection bias), selective reporting (attrition bias), incomplete data (reporting bias), and unknown source of bias.
Statistical analysis
Statistical analyses were performed by the main author (FM). To evaluate the demographic baseline of the included studies an analysis of variance (ANOVA) was performed using IBM SPSS Software, with values of P > 0.5 considered satisfactory. For the Bayesian network meta-analysis of comparisons and related effect, we used STATA Software/MP 14.1 (2015. Stata Corporation, College Station, TX: Stata LP). Network comparisons were performed using a hierarchical random-effects model analysis. Dichotomic variables were analysed through the log odds-ratio (LOR) method and continuous variables through the inverse variance method with a standardised mean difference (SMD) effect measure. Inconsistency was measured using the equation for global linearity via the Wald test. If P value ≥ 0.5, the null hypothesis could not be rejected and the consistency assumption could be accepted at the overall level of each treatment. The confidence interval (CI) and percentile interval (PrI) were set at 95%. An edge plot was drawn for each comparison to display both direct and indirect comparisons, contribution weights and network connections. The final effect of each treatment was displayed in the interval plot, while funnel plots were performed for each comparison to evaluate the risk of publication bias.
Results
Search result
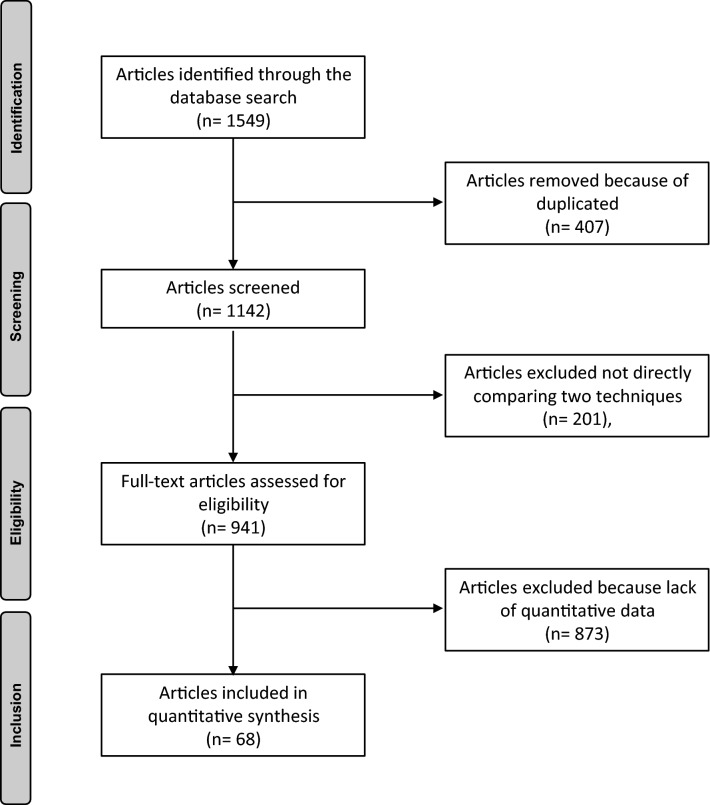
The initial search resulted in 1549 articles. 407 were duplicates. A further 1074 studies were excluded because of no direct comparison (N = 201), language limitations (N = 47), level of evidence (N = 388), type of study (N = 185), revision setting (N = 53), traumatology (N = 61), lack of quantitative data under the outcomes of interest (N = 113), uncertain data (N = 19) or other (N = 7). Finally, 68 studies were included: 45 randomized clinical trials, 9 prospective and 14 retrospective cohort studies. The flowchart of the literature search is shown in Fig. 1.
Fig. 1.
Flow-chart of the literature search
Methodological quality assessment
The Cochrane risk of bias summary evidenced some important strengths and limitations of our meta-analysis. Approximately 65% of the included articles provided randomization, the most strength in the present study. The main limitation was the reduced number of studies using a blinding method. Risk of detection, attrition and reporting biases were all low. The overall methodological quality score was very good. The Cochrane risk of bias summary is shown in Fig. 2.
Fig. 2.
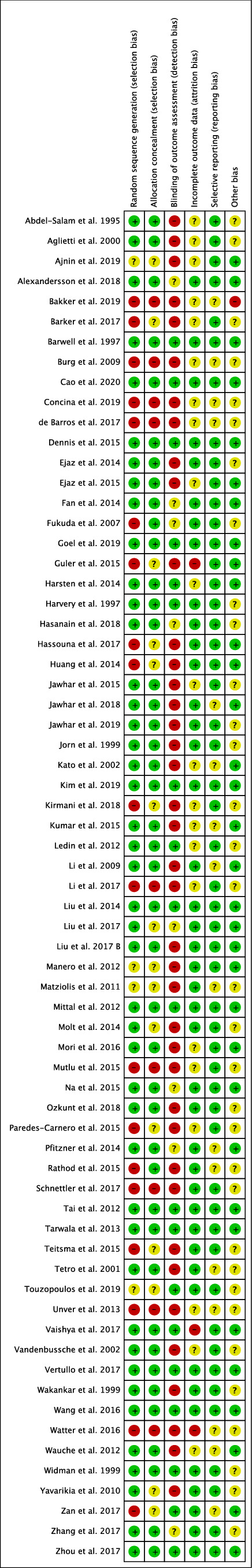
Cochrane risk of bias summary
Patient demographics
In total, data from 7413 procedures were analysed including 2330 procedures where no tourniquet was used. The mean age in this group was 67.87 ± 3.5 years, mean BMI was 28.89 ± 2.6 kg/m2, and 64% (N = 2330) were females. In the incision-to-cementation group, 953 procedures were analysed. The mean age was 68.27 ± 3.3 years, mean BMI 29.05 ± 2.9 kg/m2; 71% (N = 679) were females. In the cementation-to-end group, 782 procedures were analysed. The mean age was 66.94 ± 3.3 years, mean BMI 29.16 ± 2.3 kg/m2; 68% (N = 782) were females. In the incision-to-wound closure group, 455 procedure were analysed. The mean age was 71.21 ± 5.1 years, mean BMI 29.09 ± 1.0 kg/m2; 64% (N = 292) were females. In the full-time tourniquet group 2695 procedure were analysed. The mean age was 68.24 ± 2.9 years, the mean BMI 28.62 ± 2.4 kg/m2; 66% (N = 1775) were females. The ANOVA test detected optimal baseline comparability between the patient demographics according to age (P = 0.7), BMI (P = 0.8) and gender (P = 0.6). Demographics are shown in Table 1.
Table 1.
Generalities and demographics of included studies
| Author, year | Journal | Type of study | Type of implant | Tourniquet protocol | Tourniquet pressure (mmHg) | Samples (n) | Mean Age (years) | Female (%) | BMI (g/m2) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Abdel-Salam et al. [17] | J Bone Joint Surg | RCT | PS | Cemented | Absence | 40 | 72.00 | 57.50 | ||
| Full-time | SBP doubled | 40 | 74.00 | 62.50 | ||||||
| Aglietti et al. [18] | Cin Orthop Rel Res | RCT | Cemented | Incision to cementation | 10 | 70.00 | 70.00 | |||
| Absence | 10 | 68.00 | 60.00 | |||||||
| Ajnin et al. [19] | J Clin Orthop Trauma | PCS | CR | Cemented | Absence | 29 | 73.00 | 33.00 | ||
| Full-time | 300 | 29 | 73.00 | 33.00 | ||||||
| Alexandersson et al. [20] | Knee Surg Sports Traumatol Arthrosc | RCT | Mixed | Cemented | Absence | 43 | 69.70 | 48.83 | 27.90 | |
| Full-time | 300 | 38 | 68.00 | 52.63 | 28.60 | |||||
| Ayik et al. [21] | J Knee Surg | RCT | PS | Cemented | Absence | 33 | 64.90 | 57.57 | 30.31 | |
| Full-time | SBP + 100 | 32 | 65.39 | 56.25 | 31.38 | |||||
| Bakker et al. [22] | Turk J Anaesthesiol Reanim | RCS | Full-time | SBP + 50 | 300 | 65.00 | 64.33 | 28.90 | ||
| Absence | 300 | 65.00 | 58.33 | 29.20 | ||||||
| Barker et al. [23] | J Orthop Traumatol | RCS | Uncemented | Absence | 53 | 62.00 | 52.83 | 33.20 | ||
| Incision to cementation | 300 | 51 | 63.00 | 64.70 | 34.40 | |||||
| de Barros et al. [24] | Rev Bras Ortop | RCS | CR | Cemented | Full-time | 75 | 67.00 | 73.30 | ||
| Absence | 42 | 67.00 | 71.43 | |||||||
| Barwell et al. [25] | J Bone Joint Surg | RCT | Mixed | Cemented | Full-time | 44 | 71.00 | 65.90 | ||
| Incision to cementation | 44 | 69.00 | 72.72 | |||||||
| Burg et al. [26] | J Musc Res | RCS | CR | Cemented | Full-time | 49 | 71.60 | 79.22 | ||
| Cementation to end | 28 | 72.50 | 79.22 | |||||||
| Cao et al. [27] | J Orthop Surg | RCT | PS | Cemented | Full-time | 51 | 64.90 | 72.54 | 24.36 | |
| Cementation to end | 51 | 65.20 | 74.51 | 24.52 | ||||||
| Concina et al. [28] | Acta Biomed | RCS | PS | Cemented | Incision to wound suture | 51 | 73.00 | 61.76 | ||
| Cementation | 50 | 70.00 | 68.00 | |||||||
| Dennis et al. [29] | Clin Orthop Relat Res | RCT | Full-time | 250 | 28 | 62.00 | 42.85 | 29.00 | ||
| Absence or cementation | 250 | 28 | 62.00 | 42.85 | 29.00 | |||||
| Ejaz et al. [30] | Acta Orthop | RCT | CR | Cemented | Absence | 31 | 68.00 | 45.16 | 25.00 | |
| Full-time | 250 | 33 | 68.00 | 45.45 | 25.00 | |||||
| Ejaz et al. [31] | Arthroplasty J | RCT | CR | Cemented | Absence | 28 | 68.20 | 46.43 | 25.20 | |
| Full-time | 250 | 29 | 68.30 | 55.17 | 25.10 | |||||
| Fan et al. [32] | Knee | RCT | PS | Cemented | Full-time | SBP + 100 | 30 | 65.37 | 76.66 | 27.24 |
| Cementation | SBP + 100 | 30 | 63.27 | 70.00 | 26.26 | |||||
| Fukuda et al. [33] | Arch Orthop Trauma Surg | PCS | Cemented | Absence | 21 | 73.10 | 85.71 | 26.50 | ||
| Full-time | 350 | 27 | 71.20 | 85.19 | 26.10 | |||||
| Goel et al. [34] | J Bone Joint Surg | RCT | CR | Cemented | Absence | 100 | 65.50 | 52.00 | 31.30 | |
| Full-time | 225–300 | 100 | 66.00 | 50.00 | 30.90 | |||||
| Guler et al. [35] | Knee Surg Sports Traumatol Arthrosc | RCS | PS | Cemented | Full-time | 70 | 67.40 | 85.71 | ||
| Absence | 78 | 65.80 | 82.05 | |||||||
| Harsten et al. [36] | Knee | RCT | CR | Cemented | Absence | 32 | 66.00 | 43.75 | 28.39 | |
| Full-time | 32 | 68.00 | 46.87 | 27.41 | ||||||
| Harvery et al. [37] | Arthroplasty J | RCT | Cemented | Absence | 28 | 73.40 | ||||
| Cementation | 16 | 72.40 | ||||||||
| Full-time | 36 | 68.30 | ||||||||
| Hasanain et al. [38] | Arthroplasty J | RCT | PS | Cemented | Full-time | 54 | 62.93 | 63.00 | 32.41 | |
| Cementation | SBP + 100–150 | 54 | 62.93 | 63.00 | 32.41 | |||||
| Hassouna et al. [39] | EC Orthop | PCS | CR | Cemented | Full-time | 300 | 48 | 69.00 | 66.66 | 29.30 |
| Cementation to end | 104 | 69.00 | 55.33 | 28.80 | ||||||
| Huang et al. [40] | Arch Orthop Trauma Surg | PCS | Cemented | Full-time | SBP + 100 | 30 | 66.20 | 66.66 | 26.10 | |
| Incision to cementation | 30 | 66.10 | 66.66 | 25.90 | ||||||
| Cementation | 30 | 66.30 | 63.33 | 26.50 | ||||||
| Jawhar et al. [41] | Knee Surg Sports Traumatol Arthrosc | RCT | Cemented | Full-time | 380 | 15 | 70.60 | 53.33 | 32.10 | |
| Absence | 15 | 70.60 | 53.33 | 33.80 | ||||||
| Jawhar et al. [42] | Knee Surg Sports Traumatol Arthrosc | RCT | Cemented | Full-time | 360 | 43 | 70.00 | 62.79 | 31.90 | |
| Absence | 43 | 71.00 | 62.79 | 31.90 | ||||||
| Jawhar et al. [43] | Knee Surg Sports Traumatol Arthrosc | RCT | Cemented | Full-time | 360 | 50 | 69.30 | 34.00 | 31.90 | |
| Absence | 49 | 68.30 | 61.22 | 31.40 | ||||||
| Jorn et al. [44] | Acta Orthop Scand | RCT | PS | Mixed | Full-time | 300 | 35 | 71.00 | 57.14 | 27.96 |
| Incision to wound suture | 42 | 71.00 | 78.57 | 28.78 | ||||||
| Kato et al. [45] | Anesthesiology | RCT | Absence | 24 | 63.00 | |||||
| Full-time | 350 | 22 | 65.00 | |||||||
| Kim et al. [46] | BMC Musc Dis | RCT | mixed | Cemented | Incision to cementation | 255 | 80 | 71.00 | 91.00 | 27.10 |
| Incision to cementation | 233.9 | 80 | 71.80 | 85.00 | 27.40 | |||||
| Kirmani et al. [47] | Int J Res Orthop | PCS | Cemented | Full-time | 52 | 69.80 | 67.30 | |||
| Absence | 146 | 73.00 | 65.80 | |||||||
| Kumar et al. [48] | J Clin Orthop Trauma | RCT | Incision to wound suture | SBP + 100 | 30 | 58.00 | 70.00 | |||
| Absence | 30 | 58.00 | 70.00 | |||||||
| Ledin et al. [49] | Acta Orthop | RCT | CR | Cemented | Full-time | 275 | 25 | 70.00 | 29.00 | |
| Absence | 23 | 71.00 | 28.00 | |||||||
| Li et al. [50] | Int Orthop | RCT | PS | Cemented | Full-time | SBP + 100 | 40 | 71.00 | 27.30 | |
| Absence | 40 | 70.00 | 26.80 | |||||||
| Li et al. [51] | Medicine | RCS | Full-time | 94 | 65.34 | 90.40 | 24.50 | |||
| Absence | 36 | 65.08 | 83.30 | 25.00 | ||||||
| Liu et al. [52] | Knee Surg Relat Res | RCT | PS | Cemented | Full-time | 300 | 10 | 67.00 | 30.00 | 25.57 |
| Absence | 10 | 70.00 | 10.00 | 27.09 | ||||||
| Liu et al. [53] | Int J Clin Exp Med | RCT | PS | Cemented | Full-time | SBP + 125 | 26 | 65.80 | 69.23 | 28.20 |
| Absence | 26 | 65.80 | 69.23 | 28.20 | ||||||
| Liu et al. [54] | Orthop Surg | RCT | PS | Cemented | Full-time | SBP + 125 | 52 | 67.00 | 28.10 | |
| Absence | 52 | 67.00 | 28.10 | |||||||
| Manero et al. [55] | Rev Esp Anestesiol Reanim | PCS | Cemented | Incision to wound suture | 280 | 48 | 72.69 | 62.50 | ||
| Full-time | 48 | 71.54 | 70.80 | |||||||
| Matziolis et al. [56] | Orthopäde | RCS | Cemented | Absence | 300 | 285 | 67.70 | 58.24 | ||
| Full-time | 262 | 68.50 | 59.92 | |||||||
| Mittal et al. [57] | J Surg | RCT | Cemented | Cementation | 300 | 31 | 67.50 | 81.00 | 32.50 | |
| Incision to cementation | 300 | 34 | 66.60 | 74.00 | 32.60 | |||||
| Molt et al. [58] | Knee | RCT | Mixed | Cemented | Full-time | 300 | 30 | 70.00 | 53.30 | 28.00 |
| Absence | 30 | 67.00 | 53.30 | 28.00 | ||||||
| Mori et al. [59] | Knee | RCT | PS | Cemented | Full-time | 250 | 51 | 72.80 | 88.23 | 27.70 |
| Absence | 52 | 74.60 | 82.69 | 29.20 | ||||||
| Mutlu et al. [60] | Int J Surg | RCS | PS | Cemented | Incision to cementation | SBP + 150 | 61 | 67.20 | 78.10 | |
| Absence | 65 | 65.80 | 72.20 | |||||||
| Na et al. [61] | Knee Surg Sports Traumatol Arthrosc | RCT | PS | Cemented | Incision to cementation | 253 | 105 | 72.00 | 94.00 | 26.80 |
| Short deflation before capsule closure | 256 | 101 | 73.00 | 93.00 | 26.90 | |||||
| Ozkunt et al. [8] | Medicine | RCT | CR | Cemented | Full-time | 24 | 65.05 | 100.00 | ||
| Cementation | 20 | 65.05 | 100.00 | |||||||
| Absence | 25 | 65.05 | 100.00 | |||||||
| Paredes-Carnero et al. [62] | Rev Esp Cir Ortop Traumatol | RCS | PS | Cemented | Incision to wound suture | 250–370 | 101 | 73.52 | 30.00 | |
| Full-time | 250–370 | 100 | 75.62 | 30.00 | ||||||
| Pfitzner et al. [63] | Knee Surg Sports Traumatol Arthrosc | RCT | PS | Cemented | Full-time | 350 | 45 | 69.30 | 53.33 | 27.80 |
| Absence | 45 | 70.50 | 75.55 | 26.00 | ||||||
| Rathod et al. [64] | J Knee Surg | PCS | PS | Cemented | Full-time | 40 | 64.10 | 57.50 | 31.60 | |
| Cementation | 40 | 63.60 | 50.00 | 29.10 | ||||||
| Schnettler et al. [65] | J Bone Joint Surg | RCS | Cemented | Cementation | 250 | 45 | 64.69 | 67.00 | 30.24 | |
| Absence | 36 | 65.60 | 69.00 | 31.39 | ||||||
| Tai et al. [66] | J Bone Joint Surg | RCT | Cemented | Incision to wound suture | SBP + 100 | 36 | 72.10 | 75.00 | 28.60 | |
| Absence | 36 | 72.50 | 77.77 | 27.90 | ||||||
| Tarwala et al. [67] | Clin Orthop Relat Res | RCT | PS | Cemented | Incision to cementation | 250 | 39 | 66.10 | 56.41 | 29.90 |
| Cementation | 250 | 40 | 64.60 | 55.00 | 31.40 | |||||
| Teitsma et al. [68] | Orthop Muscular Syst | PCS | PS | Cemented | Absence | 47 | 65.00 | 51.06 | 27.10 | |
| Full-time | 250 | 49 | 63.00 | 67.34 | 28.39 | |||||
| Tetro et al. [69] | Canadian J Surg | RCT | Incision to cementation | SBP + 125–150 | 33 | 69.80 | 54.54 | |||
| Absence | 30 | 69.80 | 63.33 | |||||||
| Touzopoulos et al. [70] | Eur J Orthop Surg Traumatol | RCS | CR | Cemented | Absence | 50 | 69.92 | 84.00 | 31.32 | |
| Full-time | 350 | 50 | 70.73 | 84.00 | 31.04 | |||||
| Unver et al. [71] | Orthop Nur | PCS | CR | Cemented | Full-time | AOP | 17 | 68.00 | 82.35 | 30.80 |
| Full-time | 300 | 21 | 67.30 | 85.71 | 32.00 | |||||
| Vaishya et al. [72] | J Clin Orthop Trauma | RCT | Cemented | Incision to cementation | SBP + 150 | 40 | ||||
| Cementation | SBP + 150 | 40 | ||||||||
| Vandenbussche et al. [73] | Int Orthop | RCT | PS | Cemented | Full-time | 350 | 40 | 72.50 | 77.50 | |
| Absence | 40 | 68.50 | 60.00 | |||||||
| Vertullo et al. [7] | J Orthop Surg | RCT | PS | Cemented | Cementation | 300 | 20 | 67.85 | 50.00 | 30.43 |
| Absence | 20 | 65.65 | 45.00 | 31.00 | ||||||
| Wakankar et al. [74] | J Bone Joint Surg | RCT | Cemented | Full-time | SBP doubled | 37 | 72.50 | 70.27 | ||
| Absence | 40 | 71.80 | 65.00 | |||||||
| Wang et al. [75] | Knee Surg Sports Traumatol Arthrosc | RCT | Cemented | Incision to cementation | SBP + 100 | 25 | 72.30 | 80.00 | 28.80 | |
| Cementation | SBP + 100 | 25 | 72.50 | 84.00 | 29.10 | |||||
| Watter et al. [76] | Reconstr Rev | RCS | Cemented | Absence | 100 | 63.80 | 57.00 | 29.80 | ||
| Cementation | 100 | 67.30 | 65.00 | 28.40 | ||||||
| Incision to cementation | 100 | 63.00 | 63.00 | 31.90 | ||||||
| Wauche et al. [77] | Arch Orthop Trauma Surg | RCT | Uncemented | Full-time | SBP + 100 | 19 | 63.20 | |||
| Absence | 18 | 61.40 | ||||||||
| Widman et al. [78] | Acta Orthop Scand | RCT | CR | Cemented | Incision to wound suture | 300–350 | 46 | 72.00 | 76.08 | |
| Full-time | 300–350 | 39 | 71.00 | 71.79 | ||||||
| Yavarikia et al. [79] | Pak J Biol Sci | RCT | CR | Cemented | Absence | 220–275 | 31 | 66.00 | 75.86 | |
| Incision to cementation | 220–275 | 36 | 64.00 | 72.72 | ||||||
| Zan et al. [80] | Bone Joint Res | RCS | PS | Cemented | Full-time | 220–275 | 29 | 68.00 | 72.72 | |
| Incision to cementation | 250 | 196 | 69.40 | 57.14 | 25.70 | |||||
| Full-time | 250 | 200 | 69.60 | 60.50 | 26.10 | |||||
| Zhang et al. [81] | Ir J Med Sci | RCT | Cemented | Full-time | 317 | 50 | 70.30 | 52.00 | 29.30 | |
| Incision to cementation | 316 | 50 | 71.00 | 60.00 | 29.10 | |||||
| Osteotomy to end | 322 | 30 | 68.20 | 83.33 | 29.60 | |||||
| Zhou et al. [82] | J Orthop Surg Res | RCT | PS | Cemented | Absence | 68 | 69.10 | 89.71 | 25.70 | |
| Full-time | 72 | 66.80 | 81.94 | 26.10 | ||||||
SBP systolic blood pressure, AOP arterial occlusion pressure
Outcomes of interest
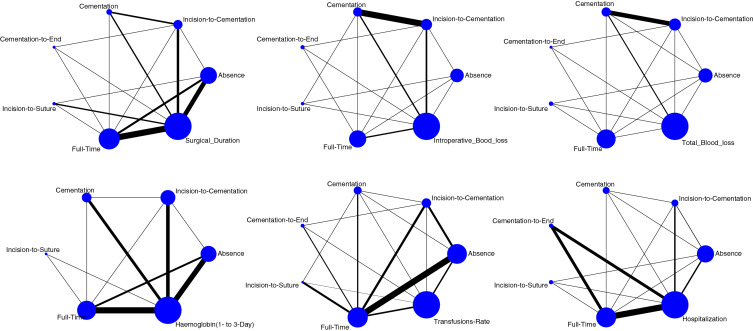
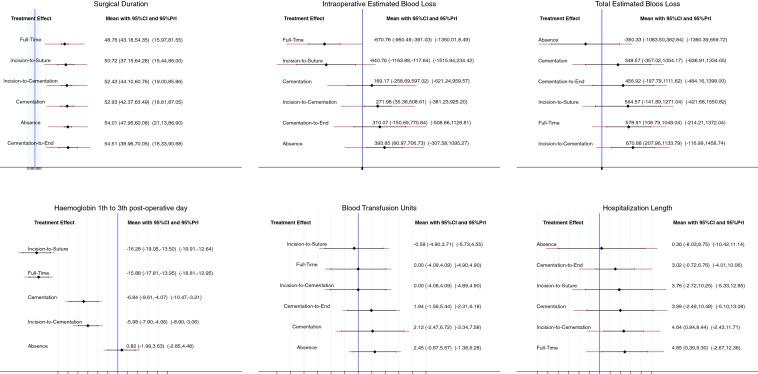
Edge, interval and funnel plots are shown in Figs. 3, 4, 5, respectively. The shortest average duration of surgery was observed in the full-time tourniquet group (SMD: 48.76; 95% CI 43.18–54.35), followed by the incision-to-suture group (SMD: 50.72; 95% CI 37.15–64.28). The cementation-to-end group showed the longest operation time (SMD: 54.51; 95% CI 38.96–70.05), followed by the absence-of-tourniquet group (SMD: 54.01; 95% CI 47.95–60.08). The test for overall inconsistency was not significant (P = 0.7).
Fig. 3.
Edge plots of the comparisons
Fig. 4.
Interval plots of comparisons
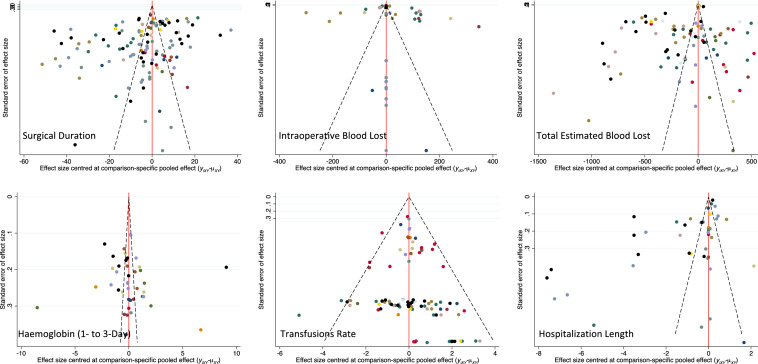
Fig. 5.
Funnel plots of the comparisons
Intraoperative blood lost was lowest in the full-time tourniquet group (SMD: -670.76; 95% CI – 950.49 to – 391.03), followed by the incision-to-suture group (SMD: – 640.76; 95% CI – 1163.88 to – 117.64). The absence of tourniquet group reported the highest intraoperative blood loss (SMD: 393.85; 95% CI 80.97–706.73), followed by the cementation-to-end group (SMD: 310.07; 95% CI – 150.69 to 770.84). The test for overall inconsistency was not significant (P = 0.8).
The absence of tourniquet group showed the lowest amount of total estimated blood lost (SMD: – 350.33; 95% CI – 1083.50 to 382.84), followed by the cementation only group (SMD: 348.57; 95% CI – 357.02 to 1054.17). The incision-to-cementation group had the highest amount of total estimated blood loss (SMD: 670.88; 95% CI 207.96–1133.79), followed by the full-time group (SMD: 578.91; 95% CI 108.79–1049.04). The test for overall inconsistency was significant and the consistency assumption could not be accepted (P = 0.009).
The incision-to-suture group showed the lowest haemoglobin drop 72 h after surgery (SMD: – 16.28; 95% CI – 19.05 to – 13.50), followed by the full-time group (SMD: – 15.88; 95% CI – 17.81 to – 13.95). The absence group of tourniquet showed the highest haemoglobin drop 72 h after surgery (0.82; 95% CI – 1.99 to 3.63), followed by the incision-to-cementation group (SMD: – 5.98; 95% CI – 7.90 to – 4.06). The test for overall inconsistency was not significant (P = 0.7).
The transfusion rate of packed red blood cells was lowest in the incision-to-suture group (LOR: – 0.59; 95% CI – 4.90 to 3.71), followed by the full-time group (LOR: 0.00; 95% CI – 4.09 to 4.09). The absence of tourniquet group showed the highest rate of blood transfusion (LOR: 2.45; 95% CI – 0.67 to 5.57), followed by the cementation only group (LOR: 2.12; 95% CI – 2.47 to 6.72). The test for overall inconsistency was not significant (P = 0.6).
The length of hospital stay was shortest in the absence of tourniquet group (SMD: 0.36; 95% CI – 8.03 to 8.75), followed by the cementation-to-end group (SMD: 3.02; 95% CI – 0.72 to 6.76). The longest hospitalisation length was reported for the full-time tourniquet group (SMD: 4.85; 95% CI 0.39–9.30), followed by the incision-to-cementation group (SMD: 4.64; 95% CI 0.84–8.44). The test for overall inconsistency was not significant (P = 0.5).
Discussion
According to the main findings of the present Bayesian network meta-analysis, longer tourniquet associated with shorter surgery duration, lower intra-operative blood lost, higher post-operative haemoglobin values, and lower rates of blood transfusion units following knee arthroplasty. A shorter average hospitalisation was found in the absence of tourniquet group. Regarding the endpoint total estimated blood loss, statistically significant inconsistency was found, and no assumption could be drawn.
The shorter surgery duration found in the full-time tourniquet group, followed by the incision-to-suture group was expected. Impaired visualization of anatomical structures and the need to constantly wipe the surgical field can lead to longer operating times. In a recent meta-analysis, Cai et al. [83] investigated the difference in surgical duration between absence of tourniquet and full-time tourniquet protocols, finding statistically significant shorter durations in the full-time group across 11 studies. Similar results were reported by Zhang et al. [3] in 2017 from eight studies comparing incision-to-suture versus a full-time tourniquet regime. Likewise, in 2019, Liu et al. [84] analysed operating times across several tourniquet protocols, evidencing significantly longer surgeries in the absence group compared to the full-time tourniquet group (P = 0.005). On the other hand, Wang et al. [12] found no difference in surgical duration between shorter tourniquet use during cementation only and longer tourniquet use across 338 procedures; however, their findings were compromised by a high level of heterogeneity across the data. Tie et al. [11] also found no significant difference between early versus late tourniquet release in over 930 procedures, but their findings too were compromised by a high level of heterogeneity.
Intra-operative blood loss was significantly less with longer tourniquet protocols. Since the purpose of the tourniquet is to limit intra-operative blood loss, these results are expected, and previous meta-analyses observed similar results. In 2019, Cai et al. [83] analysed intra-operative blood loss in a meta-analysis of 234 procedures, and found significantly less bleeding with full-time tourniquet use compared to the absence group. In 2018, Wang et al. [12] performed a meta-analysis comparing cementation only versus longer tourniquet use, and found significantly less intraoperative blood loss with long-term tourniquet use. Intraoperative blood loss was also analysed by Liu et al., in 2019, [84], who found that full-time tourniquet use was correlated with lower intraoperative blood loss compared to absence (1011 samples, P < 0.0001) and cementation only groups (323 samples, P < 0.0001). Previous meta-analyses have reported similar findings [85, 86].
Regarding the endpoint of total estimated blood lost, the equation for global linearity detected statistically significant inconsistency. Therefore, the assumption must be refused at the overall level of each treatment. This result must be interpreted in light of the limitations of the present study. Current evidences concerning total estimated blood lost are controversial. In 2019, Cai et al. [83] performed a meta-analysis of full-time tourniquet use compared to its absence. Across 98 patients, no differences found and a high level of heterogeneity was detected. Zhang et al. [3] found lower values of total blood loss with incision-to-suture tourniquet use compared to the full-time group. Wang et al. [12] found statistically significant lower total blood loss with long-term tourniquet use compared to the cementation group. Liu et al. [84] found no statistically significant differences concerning total estimated blood loss by comparing absence versus full-time and incision-to-suture versus full-time tourniquet use. Tie et al. [11] found lower blood loss in the late tourniquet release compared to early release across approximately thousand patients; this result was statistically significant, but a high level of heterogeneity was also detected.
In the present network analysis, haemoglobin values remained higher in the longer tourniquet procedures. This result can be explained by a lower amount of intra-operative blood loss. Recent meta-analyses have shown no differences among different protocols of tourniquet use during knee arthroplasty. Huang et al. [87] analysed full-time versus incision-to-suture protocols and found no difference in Hb level and Hb drop across 511 procedures. Haemoglobin drop was also evaluated in a recent meta-analysis of Tie et al. [11] over 518 procedures, with no differences between early and late tourniquet release.
In patients with Hb values under 6 g/dL, a blood transfusion is almost always required [88–90]. In patients with Hb values between 6 and 10 g/dL, with concomitant presence of symptoms indicative of hypoxia (e.g., tachycardia, hypotension, fatigue, sleepiness, dizziness), a transfusion may be required [88–90]. Patients with values over 10 g/dL very rarely need transfusion [88–90]. Transfusion of blood units was more frequent in the shorter tourniquet procedures compared to the longer ones. This analysis showed heterogeneity across studies; however, the overall results are consistent and reliable. Results from previous meta-analyses were not statistically significant. However, the blood transfusion rate and consumption of blood units were higher in the short tourniquet procedures than the longer ones. In 2019, Cai et al. [83] performed a meta-analysis comparing absence versus full-time tourniquet over eleven RCTs. They found any statistically significant difference in the rate of blood transfusion. Wang et al. [12] found no difference between the cementation and long-term tourniquet (P = 1) across 167 procedures. The 2019 meta-analysis by Liu et al. [84] found no statistical difference concerning transfusion rates. However, shorter tourniquet time resulted in a higher rate of transfusion (23.5%) compared with incision-to-suture (17.7%) and full-time tourniquet (20.4%). In 2017, Zhang et al. [3] compared incision-to-suture versus full-time tourniquet over 1010 procedures and found an increased rate of transfusion in the full-time group (13.4% versus 7.42%); however, these results were not statistically significant. Huang et al. [87] found no statistically significant difference concerning the transfusion rate between full-time (18.4% versus 22.1%) and incision-to-suture in over 256 patients.
Length of hospital stay was shorter in the absence of tourniquet group. This endpoint involved a large number of studies and was characterized by high heterogeneity with the equation for global linearity yielding a narrow result. The ranking showed a mix of short and long tourniquet protocols with wide CI and Prl; thus, the real effect of this endpoint must be considered with caution. The endpoint hospitalisation length has been included in only a few meta-analyses. The latest meta-analysis, performed by Huang et al. [87] in 2015, found no difference between incision-to-suture versus full-time tourniquet. Since shorter tourniquet time lead to less damage to the quadriceps, the post-operative function and pain without the use of a tourniquet may well be improved, consequently shortening the hospitalization length. However, this endpoint requires further investigations.
The present Bayesian network meta-analysis has several limitations and strengths. The analyses were performed with no regard for antifibrinolytic drugs (e.g., tranexamic acid) and thromboembolic prophylaxes (e.g., unfractionated heparin, oral anticoagulants). Furthermore, the utilisation of drains was not considered in the analyses. The use of tranexamic acid and the avoidance of drainages has been supposed to eradicate the use of tourniquet. However, this is still controversial [91, 92]. The effects of different tourniquet applications on cement penetration and implant anchorage were not evaluated, nor were type of prosthesis, technique, surgical approach, or length of skin incision. These limitations arise mostly from the lack of data in the literature. Therefore, no comprehensive analyses could be performed. Moreover, there was heterogeneity across articles concerning exclusion and inclusion criteria. For example, some differences in type of tourniquet and tourniquet pressure were detected. However, given the insufficient data, a separate analysis could not be performed. In conclusion, considering these limitations, the data from the present Bayesian network meta-analysis must be interpreted with caution. Points of strength of the present work are represented by the comprehensive nature of the literature search, the rigor of our eligibility criteria, good baseline comparability and the good quality of the methodological assessment. Further studies are required to more reliably define the role of the tourniquet during TKA, evaluating the impact of the several tourniquet application regimes on clinical and functional outcomes and clarify the association with thromboembolic event.
Conclusion
For knee arthroplasty longer tourniquet use is associated with shorter surgical duration, lower intra-operative blood lost, higher post-operative haemoglobin values and fewer transfused blood units. The shortest average hospitalisation was associated with no tourniquet use.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study informed consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
3/13/2021
A Correction to this paper has been published: 10.1007/s00402-021-03844-w
References
- 1.Arthur JR, Spangehl MJ. Tourniquet use in total knee arthroplasty. J Knee Surg. 2019;32(8):719–729. doi: 10.1055/s-0039-1681035. [DOI] [PubMed] [Google Scholar]
- 2.Berry DJ, Bozic KJ. Current practice patterns in primary hip and knee arthroplasty among members of the American Association of Hip and Knee Surgeons. J Arthroplasty. 2010;25(6 Suppl):2–4. doi: 10.1016/j.arth.2010.04.033. [DOI] [PubMed] [Google Scholar]
- 3.Zhang P, Liang Y, He J, Fang Y, Chen P, Wang J. Timing of tourniquet release in total knee arthroplasty: A meta-analysis. Medicine (Baltimore) 2017;96(17):e6786. doi: 10.1097/MD.0000000000006786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yi S, Tan J, Chen C, Chen H, Huang W. The use of pneumatic tourniquet in total knee arthroplasty: a meta-analysis. Arch Orthop Trauma Surg. 2014;134(10):1469–1476. doi: 10.1007/s00402-014-2056-y. [DOI] [PubMed] [Google Scholar]
- 5.Zan PF, Yang Y, Fu D, Yu X, Li GD. Releasing of tourniquet before wound closure or not in total knee arthroplasty: a meta-analysis of randomized controlled trials. J Arthroplasty. 2015;30(1):31–37. doi: 10.1016/j.arth.2014.07.034. [DOI] [PubMed] [Google Scholar]
- 6.Tai TW, Lin CJ, Jou IM, Chang CW, Lai KA, Yang CY. Tourniquet use in total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1121–1130. doi: 10.1007/s00167-010-1342-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vertullo CJ, Nagarajan M. Is cement penetration in TKR reduced by not using a tourniquet during cementation? A single blinded, randomized trial. J Orthop Surg (Hong Kong) 2017;25(1):2309499016684323. doi: 10.1177/2309499016684323. [DOI] [PubMed] [Google Scholar]
- 8.Ozkunt O, Sariyilmaz K, Gemalmaz HC, Dikici F. The effect of tourniquet usage on cement penetration in total knee arthroplasty: A prospective randomized study of 3 methods. Medicine (Baltimore) 2018;97(4):e9668. doi: 10.1097/MD.0000000000009668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dincel YM, Sari A, Cetin MU, Gunaydin B, Agca E, Dogan AH, Varol R. The effect of tranexamic acid and tourniquet use on tibial cement penetration in Primary Total Knee arthroplasties. Arthroplast Today. 2020;6(3):422–426. doi: 10.1016/j.artd.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCarthy Deering E, Hu SY, Abdulkarim A. Does tourniquet use in TKA increase postoperative pain? a systematic review and meta-analysis. Clin Orthop Relat Res. 2019;477(3):547–558. doi: 10.1097/CORR.0000000000000572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tie K, Hu D, Qi Y, Wang H, Chen L. Effects of tourniquet release on total knee arthroplasty. Orthopedics. 2016;39(4):e642–650. doi: 10.3928/01477447-20160606-03. [DOI] [PubMed] [Google Scholar]
- 12.Wang C, Zhou C, Qu H, Yan S, Pan Z. Comparison of tourniquet application only during cementation and long-duration tourniquet application in total knee arthroplasty: a meta-analysis. J Orthop Surg Res. 2018;13(1):216. doi: 10.1186/s13018-018-0927-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jiang FZ, Zhong HM, Hong YC, Zhao GF. Use of a tourniquet in total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. J Orthop Sci. 2015;20(1):110–123. doi: 10.1007/s00776-014-0664-6. [DOI] [PubMed] [Google Scholar]
- 14.Leurcharusmee P, Sawaddiruk P, Punjasawadwong Y, Chattipakorn N, Chattipakorn SC. The possible pathophysiological outcomes and mechanisms of tourniquet-induced ischemia-reperfusion injury during total knee arthroplasty. Oxid Med Cell Longev. 2018;2018:8087598. doi: 10.1155/2018/8087598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, Ioannidis JP, Straus S, Thorlund K, Jansen JP, Mulrow C, Catala-Lopez F, Gotzsche PC, Dickersin K, Boutron I, Altman DG, Moher D. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–784. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 16.Howick J CI, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M (2011) The 2011 oxford levels of evidence. Oxford centre for evidence-based medicine
- 17.Abdel-Salam KS AE. Effects of tourniquet during total knee arthroplasty. A prospective randomized study. J Bone Joint Surg. 1995;77:250–253. doi: 10.1302/0301-620X.77B2.7706340. [DOI] [PubMed] [Google Scholar]
- 18.Aglietti P, Baldini A, Vena LM, Abbate R, Fedi A, Falciani M. Effect of tourniquet use on activation of coagulation in total knee arthropalsty. Clin Orthop Relat Res. 2000;371:169–177. doi: 10.1097/00003086-200002000-00021. [DOI] [PubMed] [Google Scholar]
- 19.Ajnin S, Fernandes R. Reduced length of stay and faster recovery after total knee arthroplasty without the use of tourniquet. J Clin Orthop Trauma. 2020;11(1):129–132. doi: 10.1016/j.jcot.2019.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alexandersson M, Wang EY, Eriksson S. A small difference in recovery between total knee arthroplasty with and without tourniquet use the first 3 months after surgery: a randomized controlled study. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1035–1042. doi: 10.1007/s00167-018-5196-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ayik O, Demirel M, Birisik F, Ersen A, Balci HI, Sahinkaya T, Batibay SG, Ozturk I. The effects of tourniquet application in total knee arthroplasty on the recovery of thigh muscle strength and clinical outcomes. J Knee Surg. 2020 doi: 10.1055/s-0040-1701454. [DOI] [PubMed] [Google Scholar]
- 22.Bakker SMK, Kosse NM, Crnic S, Scheffer GJ, Stienstra R. Influence of a tourniquet on opioid consumption after local infiltration analgesia for total knee arthroplasty. Turk J Anaesthesiol Reanim. 2019;47(2):107–111. doi: 10.5152/TJAR.2019.30906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barker T, Rogers VE, Brown KB, Henriksen VT, Rasmussen GL. Tourniquet use during total knee arthroplasty does not modulate the neutrophil-to-lymphocyte ratio, pain, or activity. J Orthop Traumatol. 2017;18(3):283–287. doi: 10.1007/s10195-016-0435-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barros M, Ribeiro EJC, Dias RG. Blood level changes in total knee arthroplasty with and without a tourniquet. Rev Bras Ortop. 2017;52(6):725–730. doi: 10.1016/j.rboe.2017.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barwell J, Anderson G, Hassa A, Rawlins I. The effects of early tourniquet release during total knee arthroplasty. J bone Joint Surg. 1997;79:265–268. doi: 10.1302/0301-620X.79B2.0790265. [DOI] [PubMed] [Google Scholar]
- 26.Burg A, Dudkiewicz I, Heller S, Salai M, Velkes S. The effect of using a tourniquet in total knee arthroplasty: a study of 77 patients. J Musculoskelet Res. 2009;12:137–142. doi: 10.1142/S0218957709002286. [DOI] [Google Scholar]
- 27.Cao Q, He Z, Fan Y, Meng J, Yuan T, Zhao J, Bao N. Effects of tourniquet application on enhanced recovery after surgery (ERAS) and ischemia-reperfusion post-total knee arthroplasty: Full- versus second half-course application. J Orthop Surg (Hong Kong) 2020;28(1):2309499019896026. doi: 10.1177/2309499019896026. [DOI] [PubMed] [Google Scholar]
- 28.Concina C, Crucil M, Fabbro S, Gherlinzoni F (2019) Do tourniquet and drainage influence fast track in total knee arthroplasty? Our results on 151 cases. Acta Biomed 90(1-S):123–129. 10.23750/abm.v90i1-S.8080 [DOI] [PMC free article] [PubMed]
- 29.Dennis DA, Kittelson AJ, Yang CC, Miner TM, Kim RH, Stevens-Lapsley JE. Does tourniquet use in TKA affect recovery of lower extremity strength and function? a randomized trial. Clin Orthop Relat Res. 2016;474(1):69–77. doi: 10.1007/s11999-015-4393-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ejaz A, Laursen AC, Kappel A, Laursen MB, Jakobsen T, Rasmussen S, Nielsen PT. Faster recovery without the use of a tourniquet in total knee arthroplasty. Acta Orthop. 2014;85(4):422–426. doi: 10.3109/17453674.2014.931197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ejaz A, Laursen AC, Jakobsen T, Rasmussen S, Nielsen PT, Laursen MB. Absence of a tourniquet does not affect fixation of cemented TKA: a randomized RSA study of 70 patients. J Arthroplasty. 2015;30(12):2128–2132. doi: 10.1016/j.arth.2015.05.058. [DOI] [PubMed] [Google Scholar]
- 32.Fan Y, Jin J, Sun Z, Li W, Lin J, Weng X, Qiu G. The limited use of a tourniquet during total knee arthroplasty: a randomized controlled trial. Knee. 2014;21(6):1263–1268. doi: 10.1016/j.knee.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 33.Fukuda A, Hasegawa M, Kato K, Shi D, Sudo A, Uchida A. Effect of tourniquet application on deep vein thrombosis after total knee arthroplasty. Arch Orthop Trauma Surg. 2007;127(8):671–675. doi: 10.1007/s00402-006-0244-0. [DOI] [PubMed] [Google Scholar]
- 34.Goel R, Rondon AJ, Sydnor K, Blevins K, O'Malley M, Purtill JJ, Austin MS. Tourniquet use does not affect functional outcomes or pain after total knee arthroplasty: a prospective, double-blinded, randomized controlled trial. J Bone Joint Surg Am. 2019;101(20):1821–1828. doi: 10.2106/JBJS.19.00146. [DOI] [PubMed] [Google Scholar]
- 35.Guler O, Mahirogullari M, Isyar M, Piskin A, Yalcin S, Mutlu S, Sahin B. Comparison of quadriceps muscle volume after unilateral total knee arthroplasty with and without tourniquet use. Knee Surg Sports Traumatol Arthrosc. 2016;24(8):2595–2605. doi: 10.1007/s00167-015-3872-5. [DOI] [PubMed] [Google Scholar]
- 36.Harsten A, Bandholm T, Kehlet H, Toksvig-Larsen S. Tourniquet versus no tourniquet on knee-extension strength early after fast-track total knee arthroplasty; a randomized controlled trial. Knee. 2015;22(2):126–130. doi: 10.1016/j.knee.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 37.Harvey EJ, Leclerc J, Brooks CE, D.L. B, Effect of tourniquet use on blood loss and incidence of deep vein thrombosis in total knee arthroplasty. J Arthroplasty. 1997;12(3):291–296. doi: 10.1016/S0883-5403(97)90025-5. [DOI] [PubMed] [Google Scholar]
- 38.Hasanain MS, Apostu D, Alrefaee A, Tarabichi S. Comparing the effect of tourniquet vs tourniquet-less in simultaneous bilateral total knee arthroplasties. J Arthroplasty. 2018;33(7):2119–2124. doi: 10.1016/j.arth.2018.02.013. [DOI] [PubMed] [Google Scholar]
- 39.Hassouna HZ, Butt U, Kamal B, Appado R, Qureshi A. Tourniquet use in TKR: a potential predictor of postoperative pain scores in males and females. EC Orthop. 2017;7:188–194. [Google Scholar]
- 40.Huang ZY, Pei FX, Ma J, Yang J, Zhou ZK, Kang PD, Shen B. Comparison of three different tourniquet application strategies for minimally invasive total knee arthroplasty: a prospective non-randomized clinical trial. Arch Orthop Trauma Surg. 2014;134(4):561–570. doi: 10.1007/s00402-014-1948-1. [DOI] [PubMed] [Google Scholar]
- 41.Jawhar A, Hermanns S, Ponelies N, Obertacke U, Roehl H. Tourniquet-induced ischaemia during total knee arthroplasty results in higher proteolytic activities within vastus medialis cells: a randomized clinical trial. Knee Surg Sports Traumatol Arthrosc. 2016;24(10):3313–3321. doi: 10.1007/s00167-015-3859-2. [DOI] [PubMed] [Google Scholar]
- 42.Jawhar A, Stetzelberger V, Kollowa K, Obertacke U. Tourniquet application does not affect the periprosthetic bone cement penetration in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019;27(7):2071–2081. doi: 10.1007/s00167-018-5330-7. [DOI] [PubMed] [Google Scholar]
- 43.Jawhar A, Skeirek D, Stetzelberger V, Kollowa K, Obertacke U. No effect of tourniquet in primary total knee arthroplasty on muscle strength, functional outcome, patient satisfaction and health status: a randomized clinical trial. Knee Surg Sports Traumatol Arthrosc. 2019 doi: 10.1007/s00167-019-05646-5. [DOI] [PubMed] [Google Scholar]
- 44.Jorn LP, Lindstrand A, Toksvig-Larsen S. Tourniquet release for hemostasis increases bleeding. A randomized study of 77 knee replacements. Acta Orthop Scand. 1999;70(3):265–267. doi: 10.3109/17453679908997804. [DOI] [PubMed] [Google Scholar]
- 45.Kato N, Kazuhiro N, Shinichi Y. Abnormal Echogenic Findings Detected by Transesophageal Echocardiography and Cardiorespiratory Impairment during Total Knee Arthroplasty with Tourniquet. Anesthesiology. 2002;97:1123–1128. doi: 10.1097/00000542-200211000-00014. [DOI] [PubMed] [Google Scholar]
- 46.Kim TK, Bamne AB, Sim JA, Park JH, Na YG. Is lower tourniquet pressure during total knee arthroplasty effective? A prospective randomized controlled trial. BMC Musculoskelet Disord. 2019;20(1):275. doi: 10.1186/s12891-019-2636-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kirmani SJ, Middleton M, Fontalis A, Srivastava R. A comparison of blood loss and the need for transfusion following primary total knee replacement with or without the use of a tourniquet. Int J Res Orthop. 2018;4(4):532–537. doi: 10.18203/issn.2455-4510.IntJResOrthop20182034. [DOI] [Google Scholar]
- 48.Kumar N, Yadav C, Singh S, Kumar A, Vaithlingam A, Yadav S. Evaluation of pain in bilateral total knee replacement with and without tourniquet; a prospective randomized control trial. J Clin Orthop Trauma. 2015;6(2):85–88. doi: 10.1016/j.jcot.2015.01.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ledin H, Aspenberg P, Good L. Tourniquet use in total knee replacement does not improve fixation, but appears to reduce final range of motion. Acta Orthop. 2012;83(5):499–503. doi: 10.3109/17453674.2012.727078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li B, Wen Y, Wu H, Qian Q, Lin X, Zhao H. The effect of tourniquet use on hidden blood loss in total knee arthroplasty. Int Orthop. 2009;33(5):1263–1268. doi: 10.1007/s00264-008-0647-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu PL, Li DQ, Zhang YK, Lu QS, Ma L. Influence of tourniquet on wound healing in total knee arthroplasty: a randomized and paired clinical trial. Int J Clin Exp Med. 2017;10(2):3653–3660. [Google Scholar]
- 52.Liu D, Graham D, Gillies K, Gillies RM. Effects of tourniquet use on quadriceps function and pain in total knee arthroplasty. Knee Surg Relat Res. 2014;26(4):207–213. doi: 10.5792/ksrr.2014.26.4.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li Z, Liu D, Long G, Ke G, Xiao A, Tang P, Dong J. Association of tourniquet utilization with blood loss, rehabilitation, and complications in Chinese obese patients undergoing total knee arthroplasty: A retrospective study. Medicine (Baltimore) 2017;96(49):e9030. doi: 10.1097/MD.0000000000009030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu PL, Li DQ, Zhang YK, Lu QS, Ma L, Bao XZ, Zhang M. Effects of unilateral tourniquet used in patients undergoing simultaneous bilateral total knee arthroplasty. Orthop Surg. 2017;9(2):180–185. doi: 10.1111/os.12329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Urbano Manero EM, Miguelena Bobadilla JM. Timing of tourniquet release in total knee arthroplasty doesn't affect on transfusion needs. Rev Esp Anestesiol Reanim. 2012;59(10):556–561. doi: 10.1016/j.redar.2012.07.020. [DOI] [PubMed] [Google Scholar]
- 56.Matziolis D, Perka C, Hube R, Matziolis G. Influence of tourniquet ischemia on perioperative blood loss after total knee arthroplasty. Orthopade. 2011;40(2):178–182. doi: 10.1007/s00132-010-1727-9. [DOI] [PubMed] [Google Scholar]
- 57.Mittal R, Ko V, Adie S, Naylor J, Dave J, Dave C, Harris IA, Hackett D, Ngo D, Dietsch S. Tourniquet application only during cement fixation in total knee arthroplasty: a double-blind, randomized controlled trial. ANZ J Surg. 2012;82(6):428–433. doi: 10.1111/j.1445-2197.2012.06083.x. [DOI] [PubMed] [Google Scholar]
- 58.Molt M, Harsten A, Toksvig-Larsen S. The effect of tourniquet use on fixation quality in cemented total knee arthroplasty a prospective randomized clinical controlled RSA trial. Knee. 2014;21(2):396–401. doi: 10.1016/j.knee.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 59.Mori N, Kimura S, Onodera T, Iwasaki N, Nakagawa I, Masuda T. Use of a pneumatic tourniquet in total knee arthroplasty increases the risk of distal deep vein thrombosis: A prospective, randomized study. Knee. 2016;23(5):887–889. doi: 10.1016/j.knee.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 60.Mutlu S, Guler O, Mutlu H, Karaman O, Duymus TM, Parmaksizoglu AS. Tourniquet use during total knee arthroplasty does not offer significant benefit: A retrospective cohort study. Int J Surg. 2015;18:123–127. doi: 10.1016/j.ijsu.2015.04.054. [DOI] [PubMed] [Google Scholar]
- 61.Na YG, Bamne AB, Won HH, Kim TK. After early release of tourniquet in total knee arthroplasty, should it be reinflated or kept deflated? A randomized trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2769–2777. doi: 10.1007/s00167-015-3710-9. [DOI] [PubMed] [Google Scholar]
- 62.Paredes-Carnero X, Rosero-Ruiz GL, Centeno-Garcia JJ, Pombo-Taboada FJ. Effect of removing the ischaemia tourniquet on the transfusion needs of the patient undergoing primary knee arthroplasty. Rev Esp Cir Ortop Traumatol. 2015;59(6):394–399. doi: 10.1016/j.recot.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 63.Pfitzner T, von Roth P, Voerkelius N, Mayr H, Perka C, Hube R. Influence of the tourniquet on tibial cement mantle thickness in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):96–101. doi: 10.1007/s00167-014-3341-6. [DOI] [PubMed] [Google Scholar]
- 64.Rathod P, Deshmukh A, Robinson J, Greiz M, Ranawat A, Rodriguez J. Does tourniquet time in primary total knee arthroplasty influence clinical recovery? J Knee Surg. 2015;28(4):335–342. doi: 10.1055/s-0034-1388654. [DOI] [PubMed] [Google Scholar]
- 65.Schnettler T, Papillon N, Rees H. Use of a tourniquet in total knee arthroplasty causes a paradoxical increase in total blood loss. J Bone Joint Surg Am. 2017;99(16):1331–1336. doi: 10.2106/JBJS.16.00750. [DOI] [PubMed] [Google Scholar]
- 66.Tai TW, Chang CW, Lai KA, Lin CJ, Yang CY. Effects of tourniquet use on blood loss and soft-tissue damage in total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am. 2012;94(24):2209–2215. doi: 10.2106/JBJS.K.00813. [DOI] [PubMed] [Google Scholar]
- 67.Tarwala R, Dorr LD, Gilbert PK, Wan Z, Long WT. Tourniquet use during cementation only during total knee arthroplasty: a randomized trial. Clin Orthop Relat Res. 2014;472(1):169–174. doi: 10.1007/s11999-013-3124-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tetisma XM, Tamminga R, Snoeker BAM, Lucas C, Van der Hart CP, Felizer QGB. Effect of tourniquet application on post-operative functional outcome following total knee arthroplasty: a prospective cohort study. Orthop Muscular Syst. 2015;4(3):1–7. [Google Scholar]
- 69.Tetro AM. The effects of a pneumatic tourniquet on blood loss in total knee arthroplasty. Canadian Med Ass. 2001;44(2):33–38. [PMC free article] [PubMed] [Google Scholar]
- 70.Touzopoulos P, Ververidis A, Mpogiatzis C, Chatzigiannakis A, Drosos GI. The use of tourniquet may influence the cement mantle thickness under the tibial implant during total knee arthroplasty. Eur J Orthop Surg Traumatol. 2019;29(4):869–875. doi: 10.1007/s00590-019-02369-8. [DOI] [PubMed] [Google Scholar]
- 71.Unver B, Karatosun V, Tuncali B. Effects of tourniquet pressure on rehabilitation outcomes in patients undergoing total knee arthroplasty. Orthop Nurs. 2013;32(4):217–222. doi: 10.1097/NOR.0b013e31829aef2a. [DOI] [PubMed] [Google Scholar]
- 72.Vaishya R, Agarwal AK, Vijay V, Tiwari MK. Short term outcomes of long duration versus short duration tourniquet in primary total knee arthroplasty: A randomized controlled trial. J Clin Orthop Trauma. 2018;9(1):46–50. doi: 10.1016/j.jcot.2017.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Vandenbussche E, Duranthon LD, Couturier M, Pidhorz L, Augereau B. The effect of tourniquet use in total knee arthroplasty. Int Orthop. 2002;26(5):306–309. doi: 10.1007/s00264-002-0360-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wakankar HM, Nicholl JE, Koka R, Darcy JC. The tourniquet in total knee arthroplasty. A prospective, randomised study. J Bone Joint Surg Br. 1999;81(1):30–33. doi: 10.1302/0301-620x.81b1.8971. [DOI] [PubMed] [Google Scholar]
- 75.Wang K, Ni S, Li Z, Zhong Q, Li R, Li H, Ke Y, Lin J. The effects of tourniquet use in total knee arthroplasty: a randomized, controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(9):2849–2857. doi: 10.1007/s00167-015-3964-2. [DOI] [PubMed] [Google Scholar]
- 76.Watters T, Levy D, Kim R, Miner T, Dennis D. Arthroplasty does not benefit perioperative blood loss or transfusion requirement with the routine use of tranexamic acid. Reconstr Rev. 2016;6(3):43–47. [Google Scholar]
- 77.Wauke K, Nagashima M, Kato N, Ogawa R, Yoshino S. Comparative study between thromboembolism and total knee arthroplasty with or without tourniquet in rheumatoid arthritis patients. Arch Orthop Trauma Surg. 2002;122(8):442–446. doi: 10.1007/s00402-002-0404-9. [DOI] [PubMed] [Google Scholar]
- 78.Widman J, Isacson J. Surgical hemostasis after tourniquet release does not reduce blood loss in knee replacement. A prospective randomized study of 81 patients. Acta Orthop Scand. 1999;70(3):268–270. doi: 10.3109/17453679908997805. [DOI] [PubMed] [Google Scholar]
- 79.Yavarikia A, Amjad GG, Davoudpour K. The influence of tourniquet use and timing of its release on blood loss in total knee arthroplasty. Pakistan J Bio Sci. 2010;13(5):249–252. doi: 10.3923/pjbs.2010.249.252. [DOI] [PubMed] [Google Scholar]
- 80.Zan P, Mol MO, Yao JJ, Fan L, Yang D, Liu K, Li G. Release of the tourniquet immediately after the implantation of the components reduces the incidence of deep vein thrombosis after primary total knee arthroplasty. Bone Joint Res. 2017;6(9):535–541. doi: 10.1302/2046-3758.69.BJR-2017-0149.R2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhang Y, Li D, Liu P, Wang X, Li M. Effects of different methods of using pneumatic tourniquet in patients undergoing total knee arthroplasty: a randomized control trial. Ir J Med Sci. 2017;186(4):953–959. doi: 10.1007/s11845-017-1585-0. [DOI] [PubMed] [Google Scholar]
- 82.Zhou K, Ling T, Wang H, Zhou Z, Shen B, Yang J, Kang P, Pei F. Influence of tourniquet use in primary total knee arthroplasty with drainage: a prospective randomised controlled trial. J Orthop Surg Res. 2017;12(1):172. doi: 10.1186/s13018-017-0683-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cai DF, Fan QH, Zhong HH, Peng S, Song H. The effects of tourniquet use on blood loss in primary total knee arthroplasty for patients with osteoarthritis: a meta-analysis. J Orthop Surg Res. 2019;14(1):348. doi: 10.1186/s13018-019-1422-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Liu Y, Si H, Zeng Y, Li M, Xie H, Shen B. More pain and slower functional recovery when a tourniquet is used during total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019 doi: 10.1007/s00167-019-05617-w. [DOI] [PubMed] [Google Scholar]
- 85.Li X, Yin L, Chen ZY, Zhu L, Wang HL, Chen W, Yang G, Zhang YZ. The effect of tourniquet use in total knee arthroplasty: grading the evidence through an updated meta-analysis of randomized, controlled trials. Eur J Orthop Surg Traumatol. 2014;24(6):973–986. doi: 10.1007/s00590-013-1278-y. [DOI] [PubMed] [Google Scholar]
- 86.Papalia R, Zampogna B, Franceschi F, Torre G, Maffulli N, Denaro V. Tourniquet in knee surgery. Br Med Bull. 2014;11(1):63–76. doi: 10.1093/bmb/ldu012. [DOI] [PubMed] [Google Scholar]
- 87.Huang Z, Ma J, Zhu Y, Pei F, Yang J, Zhou Z, Kang P, Shen B. Timing of Tourniquet Release in Total Knee Arthroplasty. Orthopedics. 2015;38(7):445–451. doi: 10.3928/01477447-20150701-06. [DOI] [PubMed] [Google Scholar]
- 88.American Society of Anesthesiologists Task Force on Perioperative Blood T, Adjuvant T Practice guidelines for perioperative blood transfusion and adjuvant therapies: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and Adjuvant Therapies. Anesthesiology. 2006;105(1):198–208. doi: 10.1097/00000542-200607000-00030. [DOI] [PubMed] [Google Scholar]
- 89.Liumbruno G, Bennardello F, Lattanzio A, Piccoli P, Rossetti G. Recommendations for the transfusion of red blood cells. Blood Transfus. 2009;7(1):49–64. doi: 10.2450/2008.0020-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Liumbruno GM, Bennardello F, Lattanzio A, Piccoli P, Rossetti G, Italian Society of Transfusion M, Immunohaematology Working P Recommendations for the transfusion management of patients in the peri-operative period. III. The post-operative period. Blood Transfus. 2011;9(3):320–335. doi: 10.2450/2011.0076-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rosenstein AD, Michelov YA, Thompson S, Kaye AD. Benefits of limited use of a tourniquet combined with intravenous tranexamic acid during total knee arthroplasty. Ochsner J. 2016;16(4):443–449. [PMC free article] [PubMed] [Google Scholar]
- 92.Patel NK, Johns W, Vedi V, Langstaff RJ, Golladay GJ. Tourniquet and tranexamic acid use in total knee arthroplasty. Arthroplast Today. 2020;6(2):246–250. doi: 10.1016/j.artd.2020.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]