Abstract
Background:
Given the high incidence of asymptomatic or subclinical SARS-CoV-2 infection, reported cases likely underestimate the overall prevalence and infectivity of COVID-19. Serological test for IgG can provide a better measure of disease activity by identifying asymptomatic or subclinical infection. This study was conducted to estimate the seroprevalence of SARS-CoV-2 infection and to the determinants of SARS-CoV-2 infection in the hotspot area of COVID-19.
Method:
It was a community-based, cross-sectional study using multistage sampling with a sample size of 360. After informed consent, the demographic information, past history of SARI/ILI, contact, COVID-19 status were collected. The blood samples were taken from one family member for anti-SARS-CoV-2 IgG antibody by ELISA testing kit.
Results:
Majority of the study subjects had no history of SARI (86%) or any contact with COVID-19 case (98%). Overall seroprevalence of anti-SARS-CoV-2 of IgG antibody was 40% (95% CI 35–45%), infection fatality rate (IFR) was 0.7%. Seroprevalence varied significantly depending on religious background; with Muslims (53%) seroprevalence compared to other religious groups. Seroprevalence of homemaker/unemployed (49%) and laborer (55%) was significantly higher compared to business (30%) and service occupation (21%). Subjects with overcrowding conditions and poor ventilation was significantly associated with higher seroprevalence with odds ratio of 2.5 and 2.3, respectively.
Conclusion:
The antibody testing detects a large number of asymptomatic cases or previously infected cases which would have been missed by clinical history. Thus, the number of undiagnosed cases was found significantly higher even with rigorous implementation of lockdown.
Keywords: Antibody, anti-SARS-CoV-2 IgG, COVID-19, Malegaon, seroprevalence
Background
A cluster of cases of viral pneumonia of unknown etiology was reported in Wuhan, China in late 2019. It was further characterized as a novel viral pneumonia, COVID-19 (Coronavirus Disease 2019), caused by the novel severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). In short period of 3–4 months, it spread rapidly and developed into a global pandemic. The COVID-19 pandemic has so far affected >216 countries and globally 62,877,71 total confirmed cases and 379,941 deaths are reported till 3 June 2020.[1] In India, total number of cases and deaths were reported 216,919 and 6,075, respectively. In Maharashtra state, it was reported 74,860 and 2,587, respectively, till 3 June 2020.[2] In the state of Maharashtra, the town Malegaon was reported with 789 confirmed COVID-19 cases and it is the only taluka, with one of the highest number of COVID 19 cases till 3 June 2020.[3]
COVID-19 cases show a wide range of symptoms—ranging from asymptomatic to mild symptoms to severe illness. The symptoms may appear 2–14 days after exposure to the virus and comprise of fever, dry cough, fatigue, headache, diarrhoea. Due to the overlapping manifestations, clinical diagnosis becomes challenging, especially during seasonal flu. There is continuous demand for various types of diagnostic tests by countries across the globe. Real-time, that is, RT-PCR test is considered gold standard frontline test for clinical diagnosis of SARS-CoV-2, causing COVID-19. The test is useful only when performed in the acute stage of infection (<7 days).[4] The widespread use of RT-PCR test has been detected in many asymptomatic and atypical cases suggesting that the incidence of COVID-19 may be significantly higher than previously confirmed cases. In a COVID-19 outbreak on a cruise ship, about half of the 619 confirmed COVID-19 cases were asymptomatic at the time of diagnosis and even other studies have reported similar and/or higher proportions of asymptomatic cases.[5,6,7]
Several serological tests for IgG antibodies for COVID-19 have been developed and approved by FDA. As per Indian Council of Medical Research (ICMR) Delhi, IgG antibodies generally start appearing after 2 weeks of onset of infection and after recovery they last for several months. Although these serologic tests cannot be used as the sole test to diagnose or exclude active SARS-CoV-2 infection, it may be able to provide a better measure of disease activity (by identifying people who were not diagnosed by PCR or who may have had asymptomatic or subclinical infection).[8] Thus, serological testing provides a surrogate measure of herd immunity in a population. Malegaon has very high population density with poorly ventilated building, structures, common toilet facility which makes it very difficult to maintain social distancing. Interestingly, there has been decline in positivity from 12% to 3–5% in April to June 2020. It was unlikely that social distancing could account for this decline. Knowledge about the true extent of infection is critical for an effective public health response to COVID-19. As per World Health Organization (WHO), cross-sectional surveys, the most appropriate after the peak transmission is established,[9] that's why this study was conducted with primary objective to study the seroprevalence of anti-SARS-CoV-2 IgG antibodies and its determinants in hotspot area after first wave of COVID-19 pandemic.
Methods
Study design and study setup: The community-based cross sectional study was conducted in total 98 closed containment zones demarcated by Municipal Corporation, Malegaon. The study was conducted from 25 July to 20 Aug 2020. Approval of the Shri Bhausaheb Hire Government Medical College, (SBHGMC, Dhule) Institutional Ethics committee (IEC) was obtained prior to commencement of the study. Written informed consent was obtained prior to data collection, Data collection tools were prepared with the help of WHO community-based serosurvey for anti-SARS-CoV-2 IgG antibody detection in community.[9]
Sampling design and sample size: A multistage sampling design was used (flowchart in [Figure 1]), sampling unit was household, and sampling frame was available with Medical officer of Health (MOH), MMC, Malegaon. A sample size of 360 was calculated using EPI INFO software,[10] considering the prevalence of 12% (positivity of COVID-19 cases in Malegaon is 12%, considering this as minimum prevalence), with 5% margin of error, 95% confidence interval, and design effect of 2 (as multistage sampling). In this study, 10% non-responders (NR) had been considered. Therefore, the total calculated sample size was 330 + 30 (10% NR), that is, 360 individuals.
Figure 1.
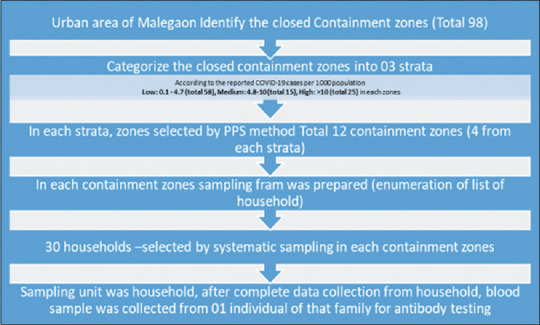
Flowchart of sampling design
Survey procedure: After obtaining informed consent, data were collected on sociodemographic information, COVID-19 swab test, history of clinical symptoms, quarantine, isolation, contacts with COVID-19 positive patients, and death in the family.
Laboratory procedure: After data collection, under all aseptic precaution 3 ml blood sample were collected in plain tubes in the community by train lab technicians, all personal protective measures were taken before blood collection. The labelling of unique codes on the tubes were done prior to blood collection. The field staffs were trained to administer the questionnaires used in the study and how to systematically select the sampling unit, that is, household in field. The various field activities were monitored by PI, Co-PI, it greatly motivated the field team and helped to assure quality of data collection. Blood samples were stored and transported in vaccine carrier. Blood test were performed by trained lab technicians at General hospital, Malegaon by anti-SARS-CoV-2 IgG ELISA kit with sensitivity 93% and specificity of 100% authorized by NIV, ICMR, Pune.[11,12] In the present study, overcrowding was assessed based on number of family members and number of rooms as well as ventilation was assessed by number of windows present in homes.
Statistical analysis: We expressed seroprevalence and infection fatality rate (IFR) in terms of percentages, 95% confidence interval (CI) was calculated for the Seroprevalence. Chi-square test was used to test the association. For studying epidemiological correlates we used odds ratio as a measure of association, 95% CI was also calculated for odds ratio. P value < 0.05 was taken as statistically significant.
Results
Clinical and demographic data of 1,653 individuals were collected from 338 households. The response rate was 100% in 9 clusters, except in the 3 cluster, the response rate were 80%, 77%, and 74%, respectively. Total 338 blood samples were collected, anti-SARS-CoV-2 IgG antibody testing were performed on 336 blood samples (2 samples were hemolysed).
About 32% of individuals were from 26 to 35 age group. Majority of study participants about 70% (236) of study subjects belonged to Muslim community, followed by 22% (75) Hindus. 34% (114) were educated up to secondary and higher secondary level (9th-12th) followed by 29% (98), 25% (84%), and 7% (22) were graduate/postgraduate, middle class (up to 5th to 8th) and illiterate, respectively. There were 38% (127) homemaker/not working and 17% (57) were government/non-government servants. Remaining 21% (72), 19% (62), and 5% (17) were businessmen, loom workers/laborer, and students, respectively. Most of the study participants were reported overcrowding 62% (209) and no adequate ventilation 61% (204) in their homes. Majority of the study subjects, 86% (290) and 97.7% (328) had no history of SARI/ILI and contact with COVID-19 patients or suspects, respectively (Table 1, shows the general charachteristics of study participants).
Table 1.
General characteristics of study participants (n=336)
| Characteristics | Categories | Frequency (%) |
|---|---|---|
| Age (in years) | 15-25 | 64 (19) |
| 26-35 | 107 (32) | |
| 36-45 | 84 (25) | |
| 46-60 | 69 (20) | |
| 61-70 | 12 (4) | |
| Gender | Male | 175 (52) |
| Female | 161 (48) | |
| Religion | Muslim | 236 (70) |
| Hindu | 75 (22) | |
| Buddhist/Cristian | 25 (8) | |
| Education | Illiterate | 22 (7) |
| Primary (1-4th std.) | 18 (5) | |
| Middle (5th-8th std.) | 84 (25) | |
| Secondary and Higher secondary (9th - 12th std.) | 114 (34) | |
| Graduate and above | 98 (29) | |
| Occupation | Homemaker/not working | 127 (38) |
| Student | 17 (5) | |
| Loom worker | 43 (13) | |
| Labourer | 19 (6) | |
| Business | 48 (14) | |
| Service | 57 (17) | |
| Others* | 25 (7) | |
| Toilet facility | Separate toilet | 296 (88) |
| Common public toilet | 40 (12) | |
| Overcrowding | Present | 209 (62) |
| Absent | 127 (38) | |
| Ventilation | Present | 132 (39) |
| Absent | 204 (61) | |
| History of SARI/ILI | Yes | 46 (14) |
| No/Don’t know | 290 (86) | |
| Contact with COVID-19 case/suspects | Yes | 8 (2.3) |
| No/Don’t know | 328 (97.7) |
Discussion
In the present study, the seroprevalence of antibodies to SARS-CoV-2 in urban area of Malegaon was estimated to be 40% (95% CI 35–45). Our results indicate that the number of infections was much greater than number of reported cases; most likely because of asymptomatic and mild infections which went undetected. As per the seroprevalence and using statistical model, we can predict that total 230,616 peoples were infected because of COVID-19 in urban area of Malegaon till the end of July 2020. As per Indian Council of Medical Research (ICMR), in hotspot area of Ahmedabad, Mumbai, and Agra were reported 49%, 37%, and 23% Seroprevalence, respectively.[12,13] Even in Maharashtra, the serosurvey was conducted in Beed, Jalgaon, Parbhani, Nanded, Ahmednagar and Sangli, which showed the seroprevalence of anti-SARS-CoV-2 IgG antibody were less than 5% in all sites while as per JV Dixit et al., the seroprevalence was 11.81 from corporation area of Aurangabad.[14,15] The difference in seroprevalence may be because of the difference in the study design, demographic profile of study population, and the situation of COVID-19 pandemic in each site. In the present study, two (2) deaths were reported in which one death reported because of COVID-19, so the IFR was 0.7%, similar IFR were reported from Mumbai (0.05–0.12), Delhi (0.07). Globally, from different studies estimated the IFR in the range of 0.5–0.10.[16,17,18]
Another important objective of our study was to investigate the determinants of the infection of SARS-CoV-2. We found that religious background, occupation, overcrowding, poor ventilation significantly associated with higher seroprevalence of anti-SARS-CoV-2 IgG antibody. Highest proportion (45%) of anti-SARS-CoV-2 IgG antibody was in the age group 46–60 years followed by 44% in 36–45 years. This may be because of the fact that persons of age group 25–59 years lead more active life and kept themselves in outdoor activities, and exposing them to symptomatic or asymptomatic COVID-19 cases. The odds of seroconversion did not significantly change with age (Table 2, shows the seroprevalence according to general charachteristics of study subjects). The proportion of seroconversion was 45% among females as compared to 35% in males, the similar finding reported in Greater Mumbai (NITI Ayog-BMC-TIFR study), they found that seroprevalence was marginally higher in women (59%) as compared to men (53%).[13] Herd immunity is a stage of an epidemic of any infectious disease in which some members of the community develop immunity for that particular disease because of previously infected or recovered or either through vaccination. Various studies suggested that to develop herd immunity for COVID-19, minimum 55–70% of the total population were previously infected to develop herd immunity.[19] On the other side, the impact of presence of antibodies among the people assume that they will be protected from the second wave of infection and there may be possibility that they will ignore the public health measures for the prevention of SARS-CoV-2 infection.[20]
Table 2.
seroprevalence according to characteristics of study subjects
| Characteristics | Categories | Seroconversion Positive/Total (Percentage) | OR (95%CI) |
|---|---|---|---|
| Age (in years) | 15-25 | 27/64 (42%) | 0.97 (0.28-3.41) |
| 26-35 | 35/107 (33%) | 1.46 (0.43-4.96) | |
| 36-45 | 37/84 (44%) | 0.90 (.26-.3.0) | |
| 46-60 | 31/69 (45%) | 0.87 (0.26-3.0) | |
| 61-70 | 5/12 (42%) | 1 | |
| Gender | Female | 62/161 (45%) | 1 |
| Male | 73/175 (35) | 1.51 (0.97-2.34) | |
| Religion | Hindu | 6/75 (8%) | 1 |
| Muslim | 125/236 (53%) | 12 (5.4-30.9)** | |
| Buddhist and others | 4/22 (18%) | (0.65-10 | |
| Education | Illiterate | 6/22 (27%) | 1.31 (0.30-5.6) |
| Primary (1-4th std.) | 4/18 (22%) | 1 | |
| Middle (5th - 8th std.) | 45/84 (54%) | 4 (1.2-13.0)** | |
| Secondary and Higher secondary (9th-12th std.) | 49/114 (43%) | 2.6 (0.81-8.5)** | |
| Graduate and above | 31/98 (32%) | 1.6 (0.49-5.3) | |
| Occupation | Homemaker/not working | 62/127 (49%) | 3.57 (1.73-7.39)** |
| Student | 5/17 (29%) | 1.5 (0.46-5.30) | |
| Loom worker/labourer | 34/62 (55%) | 4.5 (2-10)** | |
| Business/other | 22/73 (30%) | 1.61 (0.71-3.6) | |
| Service | 12/57 (21%) | 1 | |
| Overcrowding | Present | 101/209 (48%) | 2.5 (1.5-4.2)** |
| Absent | 34/127 (27%) | 1 | |
| Family size (number of members in family) | 1-2 | 6/36 (17%) | 1 |
| 3-4 | 39/143 (27%) | 1.8 (0.7-4.8) | |
| 5-8 | 78/134 (58%) | 6.9 (2.7-17.7)** | |
| >8 | 12/23 (52%) | 5.4 (1.6-18)** | |
| Ventilation | Present | 37/132 (28%) | 1 |
| Absent | 98/204 (48%) | 2.3 (1.4-3.7)** | |
| History of SARI/ILI | Present | 26/46 (56) | 2.1 (1.1-4.0)** |
| Absent | 109/290 (38%) | 1 | |
| History of contact with Covid-19 patients or suspects | Present | 5/8 (62%) | 2.5 (0.59-10.8) |
| Absent | 130/328 (40%) | 1 |
Our study is first to investigate seroprevalence of anti-SARS-CoV-2 IgG Antibody and its socioeconomic determinants in a hotspot area in India. Our study was very cost-effective (approximate cost was below 1 lakh) as compared to other studies conducted for seroprevalence. However, our study has few limitations. In this study, below 15 years population were not included for the detection of seroprevalence. The completion of objectives in this proposal was to uncover a) the true prevalence of COVID-19 in population, b) estimate the level of herd immunity required for decline/stabilization of COVID-19 spread. The cross-sectional nature of the design does not allow for cause–effect relationships to be made.
Finally, we note that the antibody testing detects a large number of asymptomatic cases or previously infected cases which would have been missed by clinical history. Thus, the number of undiagnosed cases was found significantly higher even with rigorous implementation of lockdown. The seroprevalence significantly varies in different religious groups, based on occupation and was found higher in people living in overcrowded and poorly ventilated conditions. Further studies are needed to determine seroprevalence and its determinant to predict the course of the disease and to inform the strategies and planning to prevent the spread of infection.
Financial support and sponsorship
Director, Public Health, Government of Maharashtra, India.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We must pay our sincere thanks to respected Dr. Archana Patil, Director, Public Health Department, Pune, Dr. Pradip Awate, State Surveillance officer, IDSP, Maharashtra, Mr. Suraj Mandhare, District Collector Nashik, Dr. Pankaj Ashiya, Commissioner, Municipal Corporation, Bhiwandi, Mr. Dhananjay Nikam, Adidtional Collector, Malegaon, Mr. Trambak Kasar, Commissioner Municipal Corporation Malegaon, Dr. Pralhad Gutte, Medical Superintendent, General Hospital, Malegaon, Dr. Alka Bhavsar and all Medical officers of all Urban Health Post's, Dr. MAH Azar (SMO, WHO), Dr. Sayyad Minhaj, all field investigators (intern doctors) from Mohammadia Tibbia Unani Medical College, Malegaon, Lab technicians, all nursing staff and ASHA workers for their strongly determined support and immense help for completion of this survey.
References
- 1.World health organization (WHO) Corona virus disease (COVID-19) situation report-135. Geneva: WHO; 2020. [Google Scholar]
- 2.Ministry of health and family welfare (MOHFW) Government of India (GOI). Corona virus disease (COVID-19) situation report dated 03/06.2020. New Delhi: Ministry of health and family welfare (MOHFW); 2020. [Google Scholar]
- 3.Municipal Corporation of Malegaon (MCM) COVID 19 daily reporting data. MOH, MCM, Malegaon. 2020/03/2020 [Google Scholar]
- 4.Indian council of Medical research (ICMR) Strategy for COVID-19 testing in India. ICMR, Department of Health research, Delhi, India. 09 April 2020 [Google Scholar]
- 5.Sutton D, Fuchs K, D’Alton M, Goffman D. Universal Screening for SARS-CoV-2 in women admitted for delivery. N Engl J Med. 2020;382:2163–4. doi: 10.1056/NEJMc2009316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oran DP, Topol EJ. Prevalence of Asymptomatic SARS-CoV-2 Infection. Ann Inter Med. 2020;173:362–7. doi: 10.7326/M20-3012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Campbell KH, Tornatore JM, Lawrence KE, Illuzzi JL, Sussman LS, Lipkind HS, et al. Prevalence of SARS-CoV-2 among patients admitted for childbirth in Southern Connecticut. JAMA. 2020;323:2520–2. doi: 10.1001/jama.2020.8904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Indian council of Medical research (ICMR) ICMR advises States to conduct sero-survey to measure Coronavirus exposure in the population using IgG ELISA Test. ICMR, Department of Health research, Delhi, India. Press release, 30 May 2020 [Google Scholar]
- 9.WHO. Population-based age-stratified seroepidemiological investigation protocol for coronavirus 2019 (COVID-19) infection. WHO. 26 May 2020 [Google Scholar]
- 10.EPI. Open sourse epidemiologic statistics for public health. Version 3.01 [Google Scholar]
- 11.National Institute of Virology (NIV), Indian council of Medical research (ICMR). Performance evaluation report of ELISA kit for covid-19. NIV/DVG/ER/E-06 dated 01 July 2020. Department of Health research, Pune: National Institute of Virology (NIV); 2020. [Google Scholar]
- 12.Kumar A. Ahmedabad tops COVID prevalence with 49% in hotspots, Mumbai second with 36%. Times Now. India/ article/exclusive. 2020 July 21. cited 2020 Oct 04. Available from: https://www.timesnownews.com/india/article/exclusive-ahmedabad-tops-covid-prevalence-with-49-inhotspots-mumbai-second-with/625353 .
- 13.Banaji M. What Do the Delhi and Mumbai Sero-Survey Results Tell Us About COVID-19 in India? The Wire (Internet) Government/Health/Science. 2020 July 31. cited 2020 Oct 04. Available from: https://thewire.in/health/delhimumbai-covid-19-coronavirus-seroprevalence-surveyresults .
- 14.Barnagarwala T. Higher share in slums exposed to virus than in societies: Mumbai sero survey. Indian Express (Internet) 2020. Jul 29, cited 2020 Oct 04. Available from: https://indianexpress.com/article/cities/mumbai/higher-sharein-slums-exposed-to-virus-than-in-societies-mumbai-serosurvey-6527865/
- 15.Dixit J.V, Iravane J, Andurkar SP, Gandal U, Padalkar N. Mujib Sayyed Seroprevalence of COVID-19 in Aurangabad district. Int J Creative Res. 2020;8:3675–83. [Google Scholar]
- 16.Perez-Saez FJ, Lauer SA, Kaiser L, Regard S, Delaporte E, Guessous I, et al. Serology-informed estimates of SARSCoV- 2 infection fatality risk in Geneva, Switzerland. Lancet Infect Dis. 2020;S1473-3099(20):30584–3. doi: 10.1016/S1473-3099(20)30584-3. doi: 10.1016/S1473-3099 (20) 30584-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stringhini S, Wisniak A, Piumatti G, Azman AS, Lauer SA, Baysson H, et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): A population-based study. Lancet. 2020;396:313–9. doi: 10.1016/S0140-6736(20)31304-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The infection fatality rate of COVID-19 in Stockholm – Technical report. Available from: https://www.folkhalsomyndigheten.se/contentassets/53c0dc391be54f5d959ead9131edb771/infection-fatality-rate-covid-19-stockholm-technical-report.pdf .
- 19.Amitabh Sinha. Are we approaching the stage of herd immunity? Indian Express (Internet) Explained. 2020. Jul 27, cited 2020 Oct 04. Available from: https://indianexpress.com/article/explained/serological-surveyantibodies-herd-immunity-covid-19-6522183/
- 20.WHO. “Immunity Passports” in the context of COVID-19. Available from: WHO/2019-nCoV/Sci_Brief/Immunity_passport/2020. 2020 April 24 .


