Highlights
-
•
Consultation on the sustainability and monitoring of the European Code against Cancer (ECAC).
-
•
The ECAC needs to be continuously updated, optimized, and disseminated.
-
•
Cost-effective evidence-based population measures to be included.
-
•
Synergy with preventive messages for other non-communicable diseases.
-
•
Research agenda to complement update and maintenance.
Abbreviations: CSF, Cancer Society of Finland; DG SANTÉ, Directorate-General for Health and Food Safety; EC, European Commission; ECAC, European Code Against Cancer; ECL, Association of European Cancer Leagues; EU, European Union; IARC/WHO, International Agency for Research on Cancer/World Health Organisation; iPAAC, Innovative Partnership for Action Against Cancer; NCDs, non-communicable diseases; WP5, Work Package 5
Keywords: Prevention and control, Evidence-based medicine, Information dissemination
Abstract
Introduction
As part of the third European Commission’s Joint Action on Cancer (Innovative Partnership for Action Against Cancer, iPAAC), the International Agency for Research on Cancer (IARC) was commissioned to produce a report on recommendations to sustain and monitor future updates of the European Code Against Cancer (ECAC).
Materials and methods
A co-creational consultation process, including a virtual workshop, was carried out. More than 100 experts in cancer prevention, public health, communication and representatives of European authorities provided input on the scope of future editions of the ECAC, including updating the scientific evidence and its maintenance, and on strategies for its implementation and dissemination across Europe.
Results and discussion
Overwhelming support for the need of the ECAC and its continuous updating, optimization and wider dissemination was expressed by all the stakeholders. Eight recommendations and four research needs summarise the assessment and pave the way for the future of the ECAC.
1. Introduction
The European Code Against Cancer (ECAC) is a valuable instrument for cancer prevention education given that about 40 % of cancer cases can be prevented and cancer mortality can be reduced, through practices and actions targeted at the individual and population levels [1,2]. The ECAC recommendations summarize how to avoid or reduce exposures to carcinogens, to adopt healthy behaviours and to participate in national vaccination and screening programmes [3]. In addition, it has been used as a guide and framework to influence the formulation of European National Cancer Plans by stakeholders [4]. The International Agency for Research on Cancer (IARC/WHO) has been the coordinator of the 4th edition of the ECAC (Fig. 1). The Innovative Partnership for Action Against Cancer (iPAAC) is the third European Commission’s Joint Action on Cancer, in which Work Package 5 (WP5) focuses on cancer prevention. As part of WP5, IARC was commissioned to develop recommendations for the sustainability and monitoring of the ECAC, focusing particularly on the scope of a future 5th edition of the ECAC, including updating and maintaining the scientific evidence, and on strategies to further expand the dissemination of the ECAC across the European Union (EU).
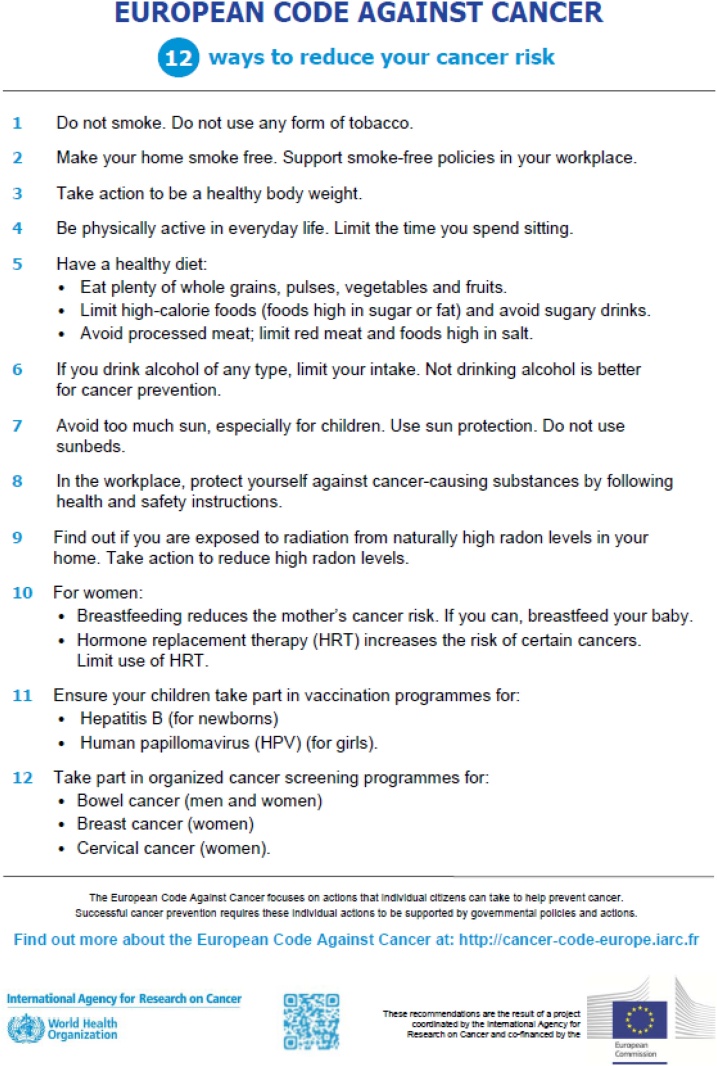
Fig. 1.
The 12 Recommendations of the 4th edition of the ECAC [3].
2. Materials and methods
A co-creational consultation process, including formal and informal meetings and online exchanges, with stakeholders from the iPAAC WP5, the Directorate-General for Health and Food Safety (DG SANTE) of the European Commission (EC) and the consortium Cancer Prevention Europe [5], was coordinated by IARC, the Association of European Cancer Leagues (ECL), and the iPAAC WP5 leader, the Cancer Society of Finland (CSF). A virtual workshop with more than 100 experts in cancer prevention, public health, dissemination and communication, as well as EU representatives, was organized in April 2020. Input on cancer prevention in the context of other non-communicable diseases (NCDs), the methods needed to update the ECAC and to modernize its dissemination, was gathered to develop the recommendations.
3. Results and discussion
3.1. Recommendations on the scope of the European Code Against Cancer
3.1.1. Broadening the scope to evidence-based individual- and population-level interventions and their implementation
Strong consensus among all stakeholders was reached to recommend adding cost-effective evidence-based prevention measures at population level (e.g. policy-oriented measures to provide healthy environments), to those already existing at individual level, to future editions of the ECAC (Table 1). A regular update of the scientific evidence on the causes of cancer remains pertinent to allow designing evidence-based prevention measures. Attention should be given to those population-level measures where the individual lifestyle measure has not, or not yet, succeeded in reducing the cancer burden (e.g. obesity) [6]. Since Europe-wide recommendations may be challenging to implement, a careful assessment of the local situation would be needed, allowing adjustment at the implementation and dissemination phases to reflect different national contexts and target groups. In addition, lessons learned from strategies that have proven to be ineffective would assist in highlighting what should not be implemented or should potentially be de-implemented.
Table 1.
List of Recommendations for the sustainability and monitoring of the European Code Against Cancer.
| Recommendations | |
|---|---|
| Recommendation #1 | The 5th edition of the ECAC should include cost-effective evidence-based cancer prevention measures at the individual and population levels (including advice regarding strategies proven to be ineffective, not implementable, and potentially to be de-implemented), alongside an updating of the evidence on the causes of cancer. |
| Recommendation #2 | Establish the appropriate framework for the 5th edition of the ECAC, including: (i) a mapping and prioritization plan, (ii) a formal process to assess the evidence, to translate it into action, and to evaluate the impact, (iii) a governance structure, including an implementation and dissemination plan, and (iv) intersectoral collaborations and partnerships. |
| Recommendation #3 | The 5th edition of the ECAC should follow a multidisciplinary approach to develop evidence-based cancer-specific recommendations in synergy with NCDs preventive messages, where applicable, allowing flexible use within unified NCDs- or cancer-targeted dissemination strategies, aligned with the social determinants of health, and with special attention to social inequalities. |
| Recommendation #4 | Enhance the visibility of the ECAC as the unifying tool in cancer prevention (i.e. cancer prevention toolbox for the EU), in alignment with the EU Europe’s Beating Cancer Plan and the Cancer Mission, while allowing adaption to the national context at the implementation and dissemination level. |
| Recommendation #5 | The 5th edition of the ECAC should be developed to address messages to different target groups (especially health professionals and policy-makers), by including several levels of information based on the same evidence base, while maintaining the general public as the primary target group and fully acknowledging that it is a heterogeneous group influenced by social, economic, and environmental determinants of health. |
| Recommendation #6 | The ECAC should be updated periodically, maintaining its high-quality process with a centralized governance of a permanent inter-institutional infrastructure. |
| Recommendation #7 | Develop a Dissemination Action Plan including: (i) a description of the recommended strategies to tailor messages to the different target audiences, including risk communication strategies, and (ii) the implementation of novel, attractive, and modern distribution formats, channels and methods to reach the general public, making the ECAC adaptable to the local context and social differences, with a special focus on increasing health literacy and trust. |
| Recommendation #8 | Engage in intersectoral partnerships to promote the ECAC. |
In order to successfully achieve this level of complexity in future editions of the ECAC, the following elements are recommended: (i) an appropriate framework created by the EC and EU Member States, including more guidance to implement the recommendations at the individual and population levels; (ii) a mapping and prioritization plan to identify relevant cancer prevention-related policies and best practices; (iii) a formal process to assess the evidence, including the appropriate sources of evidence and the breadth of expertise (e.g. behavioural and implementation science, NCDs and policy analysis); (iv) the corresponding communication strategies; (v) and intersectoral partnerships. A successful implementation of a future 5th edition of the ECAC with a broader policy dimension would need a clear implementation and dissemination plan to help policy-makers to set goals and monitor progress.
3.1.2. Using synergies between cancer-targeted and NCDs-related recommendations
Given that several cancer risk factors and preventive policy measures are common to other NCDs (e.g. high taxes on tobacco and alcohol, or food labelling regulations) [7], synergizing efforts to unify messages on NCD prevention was recommended. To show the joint impact and co-benefits of healthy behaviours and preventive measures, and not to confuse the general public, implementation and dissemination strategies should follow a NCD-oriented approach. However, the scientific evidence assessment should be carried out separately by disease, as cancer is a complex group of diseases that deserves its own recommendations. Maintaining a focus on cancer would be needed to draw attention to cancer-specific risk factors (e.g. ultraviolet radiation, human papillomavirus infection) and preventive interventions (e.g. screening). It was recommended using the ECAC as the unifying tool for cancer prevention in the EU, as a horizontal, integrated and multidisciplinary approach, hand-in-hand with other NCD scientific groups and stakeholders.
3.1.3. Tailoring the ECAC to different target groups and audiences
The 4th edition selected the individual as the direct target group of the messages of the ECAC; however, as reported by Ritchie et al., the awareness on cancer prevention in general and on the ECAC, in particular at the general public level, differs greatly across Europe, with the highest awareness where well-reputed local players have taken on the role of raising awareness [8]. In order to encourage the general public to adopt and sustain healthy lifestyles and make healthy choices, targeting individuals remains highly relevant for future editions of the ECAC; however, addressing recommendations to stakeholders, especially policy-makers and health professionals, is key given that the implementation of cost-effective population-level interventions goes beyond the direct responsibility of the individual. Therefore, a future ECAC should contain several levels of information aimed at different target groups, based on the same evidence base, while keeping simplicity, consistency, and the adequate total number of messages. Other important audiences should be reached as the recipients or mediators of multiple dissemination strategies (e.g. educators, cancer societies, patient groups). This would enable the recommendations to be further tailored to different needs (e.g. young people).
3.1.4. Update and maintenance
To facilitate updating, monitoring and follow-up of the ECAC the following mechanisms were recommended: (i) a centralized governance with scientific coordination by IARC/WHO in alliance with leading EU cancer prevention institutions; (ii) a high-quality “live” system that would allow frequent updating of rapidly evolving topics (i.e. through incremental updates between more comprehensive reviews of the evidence), while keeping other topics more static; (iii) a combination of the classical centralized approach for the evidence assessment, including multidisciplinary working groups of experts, cancer control and public health advisors with political influence and governmental health authorities; along with innovative approaches to stimulate citizens’ engagement (i.e. co-creation); (iv) a set of indicators for monitoring and evaluating the implementation of the recommendations; (v) the allocation of the resources needed; (vi) and investment in research (including implementation research) to allow the evidence to be continuously updated.
3.2. Recommendations on the dissemination of the European Code Against Cancer
Although the ECAC is often communicated as a fixed set of recommendations and an easy and practical language should be kept, some flexibility is required to adjust messages locally in order to promote the right messages, at the right moment, and to the right audiences. In order to improve the dissemination of the ECAC across the EU, a dissemination action plan was recommended, covering different target audiences and the corresponding strategies to tailor messages (e.g. to educators, families and children, primary health care providers, students of medicine and health sciences, or cancer survivors). Also, sharing and promoting best practices between countries should be enhanced. Involving experts in communication is crucial, as well as using novel, attractive and modern distribution formats, channels and methods (i.e. participatory action approaches). Investing in digital platforms and communication channels of wide reach (e.g. social media, user-friendly interactive apps, gamification), but also social and commercial marketing and advocacy, would enhance dissemination. Special emphasis was placed on how to ensure effective dissemination among vulnerable groups. Making the ECAC accessible to everyone, with the main goal of increasing health literacy and trust, and targeting misinformation, would consequently empower individuals to tackle and reduce social inequalities in cancer prevention and health promotion.
To broaden the scope of the ECAC to include policy-related recommendations, creating alliances with different stakeholders working in the same arena, such as the EC, the World Health Organization or the World Cancer Research Fund would be required early in the process. In addition, larger intersectoral partnerships with a Health in All Policies approach will be needed for a broader governmental involvement in dissemination [9]. In addition, communication partnerships with industry, education providers and the higher education establishment, the civil society and community organizations, philanthropic organizations or social media influencers should be promoted according to the respective ethical guidelines.
3.3. Research needs
An accompanying research agenda was proposed to support the sustainability and monitoring of the ECAC (Table 2), focused on implementation and dissemination research, etiological research, complemented with gathering, assessment, evaluation of impact and transfer of the knowledge.
Table 2.
List of Research needs for the sustainability and monitoring of the European Code Against Cancer.
| Research needs | |
|---|---|
| Research Need #1 | Research to successfully implement evidence-based primary and secondary prevention measures across Europe, and to evaluate novel preventive interventions and their implementation to optimize their impact on the health of individuals or different risk groups within populations. |
| Research Need #2 | Future editions of the ECAC should be accompanied by a systematic evaluation of the ECAC as a cohesive set of guidelines, in the framework of dissemination research, to ensure that the ECAC reaches the target population(s) and to measure the impact of its use. This evaluation should be performed at three levels: the (i) structural, (ii) functional, and (iii) scaling-up levels. |
| Research Need #3 | The creation and maintenance of a landmark European Evidence-based Cancer Prevention Centre, including an Evidence-based Prevention Portal and an e-Learning platform to: (i) promote rapid dissemination of best practices in cancer prevention, (ii) contribute to implementation research to optimize the implementation of known preventive strategies, (iii) identify unanswered questions that require research investment, and (iv) build capacity in cancer prevention for a variety of audiences. |
| Research Need #4 | Strengthening research into the causes of cancer with targeted European research programmes. |
To date, most research has focused on developing new interventions rather than on optimizing the delivery of existing successful ones by investigating major social, behavioural or economic barriers that impede effective implementation within the wide range of existing health systems (i.e. smoking as the most striking example, as it still causes half of all preventable cancer cases in Europe) [2,10]. Implementation research aims “to understand not only what is and isn’t working, but how and why implementation is going right or wrong, and testing approaches to improve it” [11]. In support of the EU Cancer Mission Board call for effective policy underpinned by excellent research [12], a network of prominent European scientific cancer organizations and centres has developed recommendations addressing implementation research in primary and secondary prevention (i.e. to enhance the effectiveness of prevention programmes that address well-known risk factors, to promote behavioural/nudging community-based intervention research, to evaluate currently applied early detection methods, or to optimize effectiveness and cost-effectiveness by novel strategies of risk-adapted screening) [9]. In addition, dissemination research aims to understand the best ways to spread knowledge and the associated evidence-based interventions to communities and practice settings [13]. Health education and behaviour change-promoting tools, such as the ECAC, would need a wide reach and proper dissemination to have an impact on public health, overcoming lack of health literacy at individual but also at structural level. Furthermore, the evaluation of the dissemination strategies would track the knowledge transfer, exchange and use, with the ultimate goal of enhancing the awareness, motivation, capability and opportunity of the target groups to adopt and adhere to behavioural change [14]. In line with this, to optimize the impact of the ECAC in influencing behavioural-related outcomes and to prevent regional variations in promotion and dissemination [8], research should be conducted to measure implementation and dissemination outcomes [15]: (i) at structural or decision-maker level by identifying barriers to supporting the ECAC in different countries; (ii) at functional level by defining, implementing and analysing standardized awareness metrics across the EU; and (iii) at scaling-up level by studying novel approaches to further spread the messages of the ECAC in order to increase individuals’ knowledge and self-efficacy, as well as reaching interest groups or mediators, such as health providers or educators.
Likewise, beating cancer requires a comprehensive approach to understand the link between the environment and health in general, allowing the ECAC recommendations to be revised from one edition to another, as scientific knowledge accumulates over time. Distinct geographical cancer patterns and over time suggest that among the approximately half of all cancer cases for which no cause has yet been identified, a large portion will turn out to be due to environmental and thereby modifiable risk factors, and hence also be preventable [2]. Moreover, changing human behaviour has proven to be a challenge. Therefore, promising multilevel strategies that integrate organisational, community and individual actions (the so called behavioural‐structural dichotomy) [16], need to be further studied to overcome methodological challenges related to its multivariate nature to accurately assess their effects.
Finally, the creation of a European scientific centre for evidence-based cancer prevention was suggested to make evidence on cancer prevention easily accessible for evidence-based decision-making. This Centre would offer a platform for researchers, policy-makers, programme implementers, health professionals, international organizations and cancer prevention advocates, to build upon the available evidence and research-tested materials, and foster interdisciplinary dialogue.
4. Conclusions
Overwhelming support of the need for the ECAC and its continuous updating, optimization, and wider dissemination was expressed by all the stakeholders and EU authorities involved in the consultation process. The overarching recommendation calls for including cost-effective evidence-based cancer prevention measures at individual and population levels in future ECAC editions, as well as developing cancer-specific recommendations in synergy with NCDs preventive messages. Addressing the ECAC to the most suitable target groups, integrating the ECAC into the professional health structures (i.e. using of the “teachable moment” by health professionals), or engaging with communities, citizens’ advocates and policy-makers early in the process, was recommended. Embracing technological innovations and modern ways of communication, while acknowledging socio-political and structural contexts and collaborating with committed actors across society could improve dissemination.
Finally, a clear governance structure for inclusion of implementation research in the policy agenda, and a monitoring and evaluation framework to measure the impact of the ECAC across the EU would be needed. Putting the above recommendations in practice is essential and timely, ensuring that the ECAC remains a key cancer prevention instrument contributing to the success of EC’s Europe’s Beating Cancer Plan [17].
Funding
This work was supported by the Innovative Partnership for Action Against Cancer (iPAAC) Joint Action. European Commission [Grant Agreement number: 801520 — iPAAC — HP-JA-2017].
CRediT authorship contribution statement
Carolina Espina and Joachim Schüz: conceptualized the manuscript. Carolina Espina wrote the manuscript draft. Joachim Schüz, Wendy Yared, David Ritchie, Satu Lipponen, Ahti Anttila and Kaarina Tamminiemi: reviewed the manuscript. The manuscript is a part of documentation of the iPAAC Joint Action in the field of cancer prevention. The cancer prevention report will be delivered to the European Commission in 2021.
Disclaimer
Where authors are identified as personnel of the International Agency for Research on Cancer/World Health Organization, the authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy or views of the International Agency for Research on Cancer /World Health Organization.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgements
The authors thank the experts involved in the co-creational consultation process, through the virtual workshop “Cancer Prevention & the European Code Against Cancer” hosted by the Association of European Cancer Leagues (ECL) and co-organised by the Cancer Society of Finland (CSF) and the International Agency for Research on Cancer (IARC/WHO) on 28-29 April 2020, and through the Cancer Prevention Europe consortium (https://cancerpreventioneurope.iarc.fr/).
References
- 1.Vineis P., Wild C. Global cancer patterns: causes and prevention. Lancet. 2014;383:549–557. doi: 10.1016/S0140-6736(13)62224-2. [DOI] [PubMed] [Google Scholar]
- 2.Schüz J. Primary prevention: a need for concerted action. Mol. Oncol. 2019;13:567–578. doi: 10.1002/1878-0261.12432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schüz J. European Code against Cancer 4th edition: 12 ways to reduce your cancer risk. Cancer Epidemiol. 2015;39:S1–10. doi: 10.1016/j.canep.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 4.Espina C. Cancer prevention policy in the EU: best practices are now well recognised; no reason for countries to lag behind. J. Cancer Policy. 2018;18:40–51. doi: 10.1016/j.jcpo.2018.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wild C. Cancer prevention Europe. Mol. Oncol. 2019;13(3):528–534. doi: 10.1002/1878-0261.12455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Friedenreich C.M., Ryder-Burbidge C., McNeil J. Physical activity, obesity and sedentary behavior in cancer etiology: epidemiologic evidence and biologic mechanisms. Mol. Oncol. 2020;(August) doi: 10.1002/1878-0261.12772. Epub ahead of print. PMID: 32741068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization . World Health Organization; Geneva: 2017. Best Buys and Other Recommended Interventions for the Prevention and Control of Noncommunicable Diseases. [Google Scholar]
- 8.Ritchie D. Evaluation of the impact of the European Code against Cancer on awareness and attitudes towards cancer prevention at the population and health promoters’ levels. Cancer Epidemiol. 2021;71(February Pt A) doi: 10.1016/j.canep.2021.101898. [DOI] [PubMed] [Google Scholar]
- 9.Leppo K, et al., editors (2013). Health in All Policies - Seizing opportunities, implementing policies. Available at: https://julkaisut.valtioneuvosto.fi/handle/10024/69920.
- 10.Berns A. Towards a cancer mission in Horizon Europe. Mol. Oncol. 2020;14:1589–1615. doi: 10.1002/1878-0261.12763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peters D.H. World Health Organization; 2013. Implementation Research in Health: A Practical Guide. Alliance for Health Policy and Systems Research.https://www.who.int/alliance-hpsr/resources/implementationresearchguide/en/ Available at: [Google Scholar]
- 12.Mission Board for Cancer . 2020. Conquering Cancer: Mission Possible. Report of the Mission Board for Cancer.https://ec.europa.eu/info/sites/info/files/research_and_innovation/funding/documents/ec_rtd_mission-board-report-cancer.pdf Available at: [Google Scholar]
- 13.NIH . 2020. Dissemination & Implementation (D&I) Research. United States National Institutes of Health.https://prevention.nih.gov/research-priorities/dissemination-implementation Available at: [Google Scholar]
- 14.Michie S. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement. Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Proctor E. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm. Policy Ment. Health. 2011;38:65–76. doi: 10.1007/s10488-010-0319-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Martin‐Moreno J.M. Behavioural and structural interventions in cancer prevention: towards the 2030 SDG horizon. Mol. Oncol. 2020;15(March 3):801–808. doi: 10.1002/1878-0261.12805. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Europe’s Beating Cancer Plan . 2020. European Commission.https://ec.europa.eu/info/law/better-regulation/have-your-say/initiatives/12154-Europe-s-Beating-Cancer-Plan [Accessed 07/01/2021] [Google Scholar]