Abstract
Background
Indigenous populations throughout the world experience poorer health outcomes than non-indigenous people. The reasons for the health disparities are complex and due in part to historical treatment of Indigenous groups through colonisation. Evidence-based interventions aimed at improving health in this population need to be culturally safe. However, the extent to which cultural adaptation strategies are incorporated into the design and implementation of nutrition interventions designed for Indigenous peoples is unknown. The aim of this scoping review was to explore the cultural adaptation strategies used in the delivery of nutrition interventions for Indigenous populations worldwide.
Methods
Five health and medical databases were searched to January 2020. Interventions that included a nutrition component aimed at improving health outcomes among Indigenous populations that described strategies to enhance cultural relevance were included. The level of each cultural adaptation was categorised as evidential, visual, linguistic, constituent involving and/or socio-cultural with further classification related to cultural sensitivity (surface or deep).
Results
Of the 1745 unique records screened, 98 articles describing 66 unique interventions met the inclusion criteria, and were included in the synthesis. The majority of articles reported on interventions conducted in the USA, Canada and Australia, were conducted in the previous 10 years (n = 36) and focused on type 2 diabetes prevention (n = 19) or management (n = 7). Of the 66 interventions, the majority included more than one strategy to culturally tailor the intervention, combining surface and deep level adaptation approaches (n = 51), however, less than half involved Indigenous constituents at a deep level (n = 31). Visual adaptation strategies were the most commonly reported (n = 57).
Conclusion
This paper is the first to characterise cultural adaptation strategies used in health interventions with a nutrition component for Indigenous peoples. While the majority used multiple cultural adaptation strategies, few focused on involving Indigenous constituents at a deep level. Future research should evaluate the effectiveness of cultural adaptation strategies for specific health outcomes. This could be used to inform co-design planning and implementation, ensuring more culturally appropriate methods are employed.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12939-021-01462-x.
Keywords: Aboriginal, Adult, Child, Co-design, Cultural safety, Community, Indigenous, First nations
Background
Indigenous peoples are recognised as being connected to a particular geographical region and having ancestral ties to the original land inhabitants prior to the development of modern states and borders [1, 2]. Indigenous peoples share unique cultural, societal, environmental, political and economic values that differ from the dominant society in which they live [1, 3]. Despite having strong ancestral connections to original land owners, Indigenous peoples have consistently faced marginalization and the denial of basic human rights and represent about one third of the world’s poorest communities [4]. The consequences of marginalisation and poverty include significantly poorer health outcomes [5] and reduced access to quality education and health services [2, 4, 6]. Persistent institutional racism further contributes to the health gap between Indigenous and non-indigneous people [7]. Clearly, action is required to address the health disparities faced by Indigenous peoples.
Improving diet quality has been shown to reduce the incidence of chronic diseases by up to 50% [8]. Therefore, effective nutrition interventions for combatting the gaps in health outcomes, particularly preventable chronic diseases, are needed for Indigenous peoples. While there is some evidence that nutrition interventions can improve diet-related health outcomes in Indigenous populations [9], a systematic review of 26 nutrition-related interventions among Australian Aboriginal and Torres Strait Islander people showed these gains to be short-term [10]. The authors concluded that lack of cultural adaptation limited the long-term effectiveness of interventions.
Indigenous peoples hold an holistic view of health incorporating community, environment, spiritual, emotional and physical wellbeing [11, 12]. This is in contrast to the typical western model of health care provision which is more individualistic and disease-centric [13]. A recent systematic scoping review of Indigenous primary healthcare service delivery models identified a preference for healthcare that was accessible, culturally appropriate, holistic and involved community participation [14]. While all interventions need to be tailored, this is particularly true for Indigenous peoples, acknowledging their unique cultural needs and healthcare preferences.
Ensuring cultural safety of evidence-based interventions to improve health is therefore an important approach [15, 16]. Curtis and colleagues propose a comprehensive definition for cultural safety that references the need for “healthcare organisations to influence healthcare to reduce bias and achieve equity” [17]. Cultural adaptation of an intervention involves careful consideration of the needs of the group for whom the intervention is being developed, as well as a meaningful collaboration during intervention design, development, implementation and evaluation [15, 18]. Frameworks to achieve cultural adaptation have been developed. Kreuter and colleagues [19] describe five categories of adaptation commonly used to make health interventions more culturally appropriate (evidential, visual, linguistic, constituent involving, and socio-cultural). Resincow et al. [20] further posits that cultural sensitivity in developing interventions consists of two dimensions: surface (gives the sense of culturally appropriate messages reflecting settings and experiences of the group, including: music, pictures, foods, clothing, locations, and people) or deep (involves cultural sensitivity and a comprehensive understanding of the ethnic group’s core cultural values, norms, and stressors affecting health behaviours).
The type and level of cultural adaptation strategies incorporated into the design and implementation of nutrition interventions for Indigenous peoples is unknown. According to Munn and colleagues [21], a scoping review is the type of review indicated when the aim is to identify key characteristics from an evidence base. This review therefore aims to examine the range of research undertaken on nutrition-related health interventions that are culturally adapted for Indigenous peoples focusing on the type and nature of adaptations made.
Methods
A scoping review was conducted systematically using a predefined protocol following the methodological framework of Arksey and O’Malley [22]. This approach included identifying the research question, selecting studies relevant to the research question, and charting the data - which includes summarising and reporting the results. This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews- Scoping reviews extension checklist [23].
Identifying the research question
This review aimed to identify and categorise the key characteristics of cultural tailoring in health interventions with a nutrition component designed for Indigenous populations. The system outlined by the United Nations was adopted to determine Indigenous populations from any nation worldwide [24], noting that terms vary by country and geographical region and that the right to identify as Indigenous is the right of the people themselves [25]. Interventions conducted in mixed populations (i.e. Indigenous and non-indigenous peoples) were excluded.
Lifestyle interventions with a nutrition component with the aim of improving health outcomes, that described deliberate strategies used to enhance cultural relevance were included. Nutrition components of interventions were defined as the manipulation of food or dietary intake directly (e.g. provision of food or nutritional supplement) or indirectly (e.g. nutrition education). The nutrition component could be the sole focus of the intervention or delivered in conjunction with other components such as physical activity.
The typology of Kreuter and colleagues [19] was used to categorise the cultural adaptation strategies (Table 1). Articles were included if they described at least one of the five strategies. To further explore the extent of cultural adaptations, the model for understanding cultural sensitivities of Resincow and colleagues was also applied to included studies [20]. Each strategy was classed as ‘surface’ or ‘deep’ according to this model [20] (Table 1).
Table 1.
Description of cultural adaptation strategies used to tailor nutrition health interventions for Indigenous peoples
| Strategy type | Strategy Descriptiona | Sensitivity Levelb |
|---|---|---|
| Peripheral |
Use of colours, imagery, fonts, pictures of the community, music, or declarative titles. Gives the appearance of cultural appropriateness by packaging them in ways likely to appeal to a group. These elements can create interest, establish credibility and set the tone for content in printed communications |
Surface |
| Evidential |
Use of data on a given health issue within the population/community. To enhance the perceived relevance of a health issue for a given group by presenting evidence of its impact on that group. Such statements seek to raise awareness, concern, and or perceived personal vulnerability to a health issue by showing that it affects the given group. |
Surface |
| Linguistic |
Use of dominant or traditional language. To make programs and materials more accessible. Must consider translations – should be culturally relevant, not direct translations. |
Surface (direct translation) Deep (full translations with culturally relevant statements) |
| Constituent Involving |
Drawing directly on the experience of members of the community. Can range from using stories of community members, through to formal community guidance, through to full ownership and directing of the project by the community. |
Surface (testimonials or stories) Deep (delivery of intervention by community members) |
| Sociocultural strategies |
Discusses health issues in the context of broader social and cultural values and characteristics. The cultural values, beliefs and behaviours of the group are recognised, reinforced and built upon to provide context and meaning to the health promotion activity. |
Deep |
Published peer-reviewed studies, of any design, were considered for inclusion. Articles were included if the health outcomes were reported or if the health outcomes were specified but not yet evaluated within the existing publication. Where health outcomes were not stated, a category of ‘no outcomes reported’ was used. The health outcomes of interest were reported in the description of each included study (Additional file 1). Where health outcome data was available, the specific changes were extracted (e.g. decreased weight, increased intake of vegetable serves).
Selection of studies relevant to the research question
A structured search of available peer-reviewed literature was conducted with support from an experienced health librarian. The following databases were searched from inception to January, 2020: Embase, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Central Register Medline, PsychInfo, and Scopus (restricted to non-Medline indexed articles). Terms searched can be seen in Additional file 2. A web application (Rayaan) was used to manage the review (Available at: https://rayyan.ai/) [26]. All included studies were hand searched for references not captured by the initial search strategy. Reference lists of identified systematic reviews were searched to check all relevant papers from those reviews were included. Title/abstract and full-text screening were coded independently in duplicate. Discrepancies were resolved through discussion.
Charting of data
Data from all included articles were extracted into a purposefully-developed spreadsheet by one researcher. A second researcher reviewed the coding on a subsample of articles (n = 24; ~ 25%) to ensure adequate and consistent application of the inclusion and exclusion criteria. Extracted data included: first author name and year of publication, intervention or program name, Indigenous population name (cited as reported in the article including any tribal affiliations) and location (including country), population of interest, level of intervention (individual (aimed at individual behaviour change), community (aimed at community behavioural or value change), or systems (aimed at environmental change (e.g. food systems)), a brief description of the intervention (including length, frequency and duration), theories of behaviour change used to underpin the intervention, a brief description of intervention outcomes (if reported), and whether or not formative research was undertaken in the same population or community (i.e. evidence for the intervention to improve health outcomes for the people involved). To achieve a yes for formative research, authors needed to refer to evidence (published or unpublished) to support the application of the intervention or program within the Indigenous population or specific community they were planning to work with. Involvement of the community in intervention design was extracted as ‘yes-minimal’ if community members were reported to have been consulted or asked to provide feedback, ‘yes-maximal’ if community-based participatory research was employed, and ‘no’ if there was no community involvement in design of the intervention or program. Categories of strategies used to culturally tailor the intervention were extracted as per Table 1 [19].
Where multiple articles clearly reported on the same intervention and focussed on health outcomes, they were grouped for data extraction. As per the convention of scoping reviews, extracted data was summarised numerically to provide an overview of study characteristic frequency.
Results
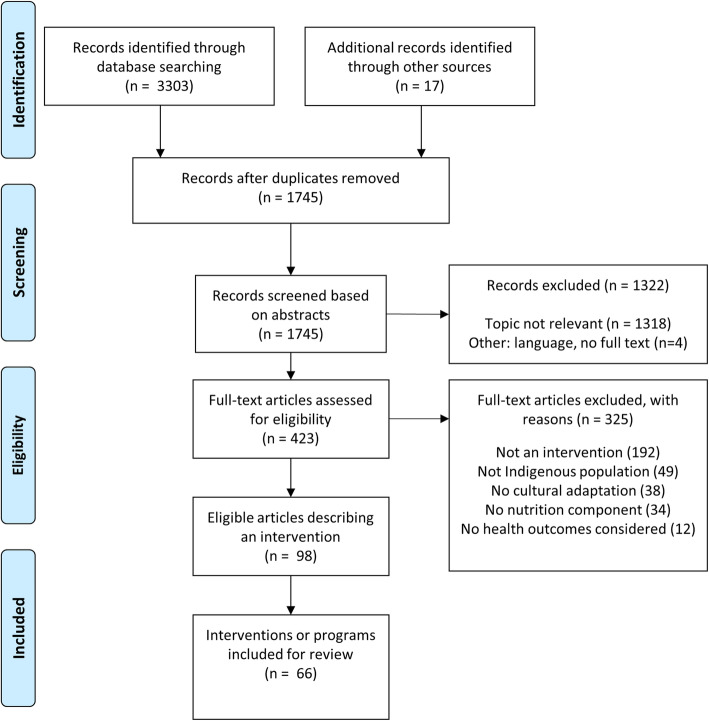
The database search resulted in 3303 records with an additional 17 articles identified through other sources (Fig. 1). There were 1745 Articles remaining once duplicates were removed. Of the 423 articles included in full text screening, 98 met the inclusion criteria. These 98 records described 66 unique interventions. The articles described 19 randomised controlled trials (RCTs), 3 Randomised Trials, 9 non-randomised trials and 35 pre-post studies.
Fig. 1.
Flow diagram for identification of culturally adapted health interventions for Indigenous peoples
Characteristics of included studies
Table 2 summarises the characteristics of included interventions (n = 66) [27–92]. Individual study characteristics are described in Additional file 2. Where an intervention has multiple articles, the first publication by date has been used throughout as the source reference.
Table 2.
Characteristics of the 66 included interventions
| Study Characteristic | n | (%) |
|---|---|---|
| Population (Country) | ||
| Native American / Native Alaskan / Native Hawaiian (USA) | 33 | 50.0 |
| Aboriginal and/or Torres Strait Islander People (Australia) | 14 | 21.2 |
| First Nations Peoples (Canada) | 11 | 16.8 |
| Maori (New Zealand) | 4 | 6.0 |
| Other Indigenous groups (inc. Palauan, Samoan, Fiji & Soloman Islanders, Guatemalan) | 4 | 6.0 |
| Year of Publication | ||
| < 1996 | 3 | 4.5 |
| 1996–2000 | 8 | 12.1 |
| 2001–2005 | 6 | 9.1 |
| 2006–2010 | 13 | 19.7 |
| 2011–2015 | 20 | 30.3 |
| 2016–2020 | 16 | 24.3 |
| Health Focus of Intervention | ||
| Diabetes prevention | 19 | 28.8 |
| Obesity prevention and treatment | 12 | 18.2 |
| Nutritional adequacy/Food security | 9 | 13.6 |
| Women and infant health | 8 | 12.1 |
| Diabetes management | 7 | 10.6 |
| Cardiovascular disease prevention | 6 | 9.1 |
| Chronic disease prevention (otherwise not already covered) | 5 | 7.6 |
| Type of primary Nutrition Intervention component | ||
| Nutrition education | 34 | 51.6 |
| Healthy food environment | 14 | 21.2 |
| Individual dietary intervention | 8 | 12.1 |
| Cooking classes | 4 | 6.0 |
| Other (eg. Cultural stories, home-visits, dental care) | 6 | 9.1 |
| Population | ||
| Adult | 29 | 43.9 |
| Child | 18 | 27.3 |
| Both | 19 | 28.8 |
| Intervention duration | ||
| < 3 months | 14 | 21.2 |
| 3–6 months | 15 | 22.7 |
| > 6–12 months | 15 | 22.7 |
| > 12–24 months | 11 | 16.7 |
| > 24 months | 10 | 15.2 |
| Not reported | 1 | 1.5 |
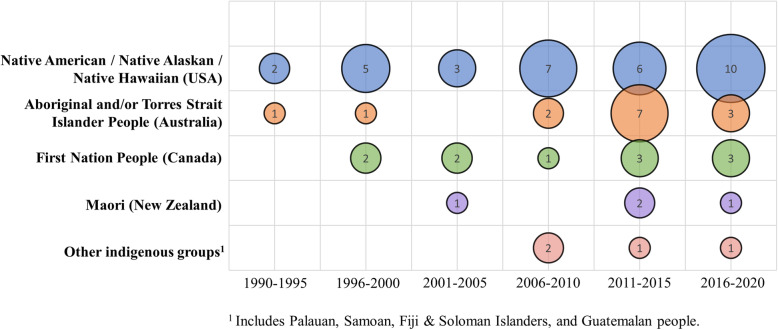
The majority of interventions were conducted in the USA among Native American (n = 27) [28, 32, 33, 37, 38, 42, 43, 46, 48, 50, 52, 56–58, 61–63, 65, 70, 72–74, 82, 83, 87, 89, 92], Alaskan (n = 4) [47, 64, 75, 93] & Hawaiian (n = 2) [54, 71] populations. Together with Australian Aboriginal and/or Torres Strait Islander (n = 14) [27, 29–31, 40, 44, 51, 68, 78, 80, 85, 86, 88, 91] and Canadian First Nations People (n = 11) [35, 36, 41, 45, 49, 55, 67, 69, 76, 84, 90] these three groups accounted for 85% of the literature included in this review. Figure 2 illustrates the interventions published by year and by Indigenous population and location.
Fig. 2.
Bubble chart of interventions by publication year and by Indigenous population and location (n = 66)
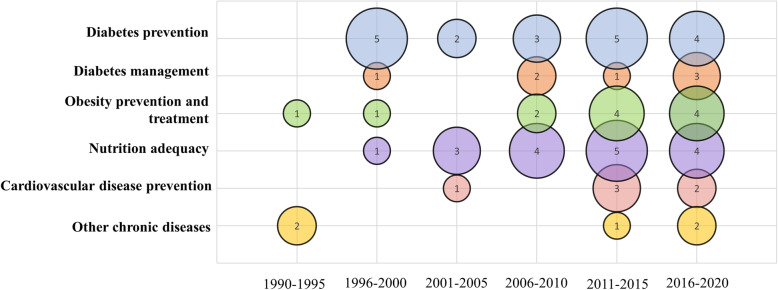
Most interventions were designed for adults (n = 29) [27, 28, 36, 39, 40, 42, 46, 51–54, 58, 60–63, 66, 71, 74–77, 80, 81, 83, 85–87, 91], with less than a third (n = 19) [29–31, 34, 35, 38, 44, 47, 48, 50, 59, 65, 68, 69, 73, 78, 79, 88, 90] designed for both adults and children. Most interventions aimed to change health outcomes for diabetes prevention (n = 19) [27, 28, 36, 38, 44, 55, 56, 60, 62, 67, 69, 70, 79, 81, 82, 88, 89, 92, 93], obesity prevention or treatment (n = 11) [32, 34, 42, 50, 57, 59, 65, 72, 80, 83, 90], and diabetes management (n = 7) [31, 33, 39, 48, 51, 58, 63, 68, 71, 86, 87, 91]. Figure 3 illustrates interventions published by Indigenous population and health focus.
Fig. 3.
Bubble chart of articles published by Indigenous population and location and helath focus (n = 66)
Intervention characteristics and cultural adaptation used in included studies
Table 3 summarises the intervention characteristics and cultural adaptation strategies employed (n = 66). Interventions that incorporated both individual and community level approaches were the most common (n = 32) [28, 29, 33, 34, 37, 41, 44, 47, 49, 50, 52–56, 58–63, 66–68, 70, 71, 74–76, 88, 92, 93]. Two studies each employed community only [43, 90], system only [35, 57] and individual plus system [39, 91] level interventions. Seven interventions aimed to influence all three levels [30–32, 45, 69, 81, 89]. Most interventions (n = 56) [28, 30–39, 41–50, 52–59, 61, 63–69, 77, 80, 81, 83–87, 90–92] cited formative research. Only one-third of interventions (n = 22) were informed by a combination of formative research at both the population and community level [31–33, 35, 37–39, 42, 44, 46, 49, 54, 64, 66, 69–74, 86, 90]. Of the 46 studies that referred to formative research and also reported outcomes, most reported positive intervention outcomes (n = 38; 83%) [28, 30–33, 36–39, 42, 43, 45, 47, 50, 53, 54, 56–58, 61, 63, 64, 66–73, 80, 84–86, 89–91, 93]. Nineteen interventions reported employing an underlying theory of behaviour change [28, 31–33, 36, 41, 42, 50, 55, 57, 65, 67, 70, 72, 73, 80, 90, 92, 93]. Of those that did, most employed multiple theories of behaviour change (n = 9) [31, 33, 36, 50, 55, 65, 90, 92, 93] social cognitive theory (n = 7) [28, 41, 42, 57, 72, 73, 80], or its predecessor of social learning theory (n = 3) [32, 67, 70].
Table 3.
Summary of Intervention chracteristics and cultural adaptation strategies (n = 66)
| Study Characteristic | n (%) | (%) |
|---|---|---|
| Level of Intervention | ||
| Individual only | 12 | 18.2 |
| Community only | 2 | 3.0 |
| System only | 2 | 3.0 |
| Individual + Community | 32 | 48.5 |
| Individual + System | 2 | 3.0 |
| Community + System | 9 | 13.6 |
| Individual + Community + System | 7 | 10.6 |
| Level of Community Input on design | ||
| None | 16 | 24.2 |
| Minimal | 21 | 31.8 |
| Maximal | 29 | 43.9 |
| Formative research cited | ||
| Population level | 28 | 42.4 |
| Community level | 6 | 9.1 |
| Both | 22 | 33.3 |
| None | 10 | 15.2 |
| Intervention based on Behavior change theory | ||
| None reported | 47 | 71.2 |
| Social cognitive theory | 7 | 10.6 |
| Social learning theory | 3 | 4.5 |
| Multiple therories | 9 | 13.6 |
| Number of cultural strategies employeda | ||
| 1 strategy | 1 | 1.5 |
| 2 strategies | 8 | 12.1 |
| 3 strategies | 23 | 34.8 |
| 4 strategies | 22 | 33.3 |
| 5 strategies | 12 | 18.2 |
| Cultural sensitivities employed by categoryb | ||
| Surface only | 12 | 19.7 |
| Deep only | 3 | 3.0 |
| Both surface and deep | 51 | 77.3 |
Almost all interventions employed more than one type of strategy to culturally tailor an intervention (n = 65). Twelve interventions employed all five cultural adaptation strategies [34, 38, 48, 51, 53, 63–65, 68–70, 76], 22 employed four strategies [36, 39, 42, 44, 46, 47, 49, 54–61, 67, 72–74, 81], 23 employed three strategies [28–30, 32, 33, 37, 40, 41, 43, 45, 50, 52, 62, 71, 78, 82, 83, 86–89, 93], eight employed two strategies [27, 31, 35, 79, 80, 85, 91, 92], and only one study employed a single strategy [90]. Most interventions employed a combination of surface and deep cultural sensitivity approaches (n = 51) [27–77], 12 used surface strategies only [78–89] and three studies [90–92] employed deep strategies only.
Cultural adaptation strategies used in each individual study are described in Additional file 3. Visual adaptation strategies were the most frequently used (n = 57) such as ensuring print materials had pictures of Indigenous peoples, native foods, or colours of cultural significance [28, 29, 32–34, 36–49, 51–76, 78, 79, 81–89]. The second most frequently used strategy was constituent involving (n = 51) which ranged from the surface level strategies of requesting participant feedback, incorporation of participant stories or engagement of local media and businesses (n = 20) [27, 33, 36, 39, 42, 44, 46, 47, 61, 63, 68, 78, 80–84, 86–88], through to the deep level strategies of training of respected community members to deliver an intervention (n = 31) [28–30, 32, 34, 37, 38, 41, 45, 48–51, 53, 55–60, 64, 65, 67, 69, 70, 72, 73, 90–92]. Socio-cultural strategies were also widely employed (n = 50) and included a range of activities such as incorporating traditional activities and ceremonies in the intervention, and ensuring childcare was available for participants [27–47, 49–66, 68–71, 73–76, 91, 92]. Linguistic strategies were employed in 41 of the interventions. Most of these were at the surface level [34, 40, 42–44, 48–50, 52, 54, 57, 59, 62, 63, 68, 70, 75, 79, 81–84, 86–89], such as incorporating single Indigenous words into intervention materials (e.g. name of the intervention), or by translating messages exactly from English into Indigenous languages. Deep linguistic strategies (n = 15) included providing all materials in Native languages and English, or by incorporating Native language and concepts into the intervention materials and activities [38, 39, 51, 53, 60, 64–67, 69, 71, 72, 74, 76, 93]. Evidential strategies were least commonly employed (n = 34) and included providing specific information about disease risk for Indigenous peoples in the community [30, 34–36, 38, 46–48, 51, 53–56, 58, 61, 63–65, 67–70, 72–76, 78, 80, 81, 84, 85, 89].
Discussion
This is the first scoping review, to our knowledge, to examine the extent and range of research undertaken to culturally adapt nutrition interventions for Indigenous peoples across the world. Despite there being no restriction on year of publication, the review found only 98 papers representing 66 studies that fit the inclusion criteria. The publication rate on this topic appears to be accelerating with more than half of the included studies (n = 36) published in the past decade. Most studies were conducted with first peoples in the USA, Australia and Canada, despite the fact that Indigenous peoples inhabit over 90 countries worldwide [94]. This may be partly due to the shared experience of European colonization in these countries, and subsequently the need to sensitively adapt health care to improve cultural appropriateness [25, 95, 96]. Interventions included in this review had a strong emphasis on the prevention and management of diabetes and obesity. This is consistent with the known prevalence of metabolic disease which occurs at higher rates in Indigenous compared with non-indigenous populations [97–99], and important given these conditions are responsible for much of the gap in life expectancy and burden of disease between Indigenous and non-indigenous peoples [100]. It is important to note that the representation of research in low- and middle-income countries was clearly absent, as was a focus on the double burden of malnutrition experienced in many Indigenous peoples from these nations [101, 102]. Further research in this area is urgently needed.
The review shows that there has been a concerted effort to culturally adapt the design and delivery of nutrition interventions for Indigenous populations particularly in more contemporary research. The primary intervention strategy in over half of the studies was nutrition education, compared to less than one quarter of interventions aiming to improve the food environment. This tends to be consistent with nutrition interventions around the world despite the fact that nutrition knowledge, or lack of it, is usually not the underlying cause of health problems. This is particularly important to consider in Indigenous populations where social, economic and environmental inequalities pose significant challenges to health, rather than a lack of nutrition education [103, 104]. The United Nations Sustainable Development Goals [105] encompass aims relevant to improving Indigenous health including ending poverty and reducing inequalities. Interventions aiming to improve nutrition-related health in Indigenous populations need to incorporate strategies beyond nutrition education to address the social determinants of health at a community level [105, 106]. Less than a third of the included studies reported basing their intervention on a stated behaviour change theory. This phase of intervention design needs to be considered given the findings of a systematic review of the use of behaviour change theories in nutrition interventions by Rigby and colleagues [107]. That review showed interventions based on behaviour change theories were more effective at achieving health outcomes [107]. The Rigby review also found social cognitive theory/social learning theory to be the most commonly applied theories in designing nutrition interventions, consistent with the findings in our review. This reinforces the dominance of nutrition education as a key component of interventions. The use of models that focus more on environmental change maybe more appropriate in designing interventions for indigenous populations.
While the majority of interventions were applied across multiple levels, this review found that only half of the interventions incorporated a community level approach. This is despite the definition of health for Indigenous peoples consistently adopting a holistic view incorporating social concepts that are expressed and applied in the community [94]. In a review of three environmental intervention case studies addressing chronic disease prevention interventions in American Indians, Gittelsohn and Rowan concluded that strategies were more successful when multiple intervention levels including environmental approaches with a particular emphasis placed on partnering with local stakeholders to positively influence healthy behaviours were implemented [108].
Importantly, this review identified that the majority of interventions employed multiple cultural adaptation strategies as classified according to Kreuter and colleagues’ categories [19]. Most commonly this involved adopting peripheral and evidential strategies at a level that Resincow would classify as surface, which is consistent with interventions predominantly taking a nutrition education approach. Of interest was that deep linguistic approaches were least commonly utilised. A deep linguistic approach would involve making texts culturally relevant rather than simply a direct translation. Health education resources are often non-specific and lack cultural sensitivities for specific populations [109]. Further, direct language translations may lack cultural nuances putting cultural safety at risk. Health education resources need to be community-owned and incorporate cultural sensitivities to improve utiliastion and acceptance.
The majority of interventions involved key stakeholders at a surface level, and less than half involved constituents on a deep level. The review highlights that cultural adaptation of interventions to date has commonly involved engaging with Indigenous community stakeholders to elicit key understandings and experiences, for example, in conducting formative research. However, it was less common for interventions to be owned, delivered and/or directed by the community themselves. Similar findings to this review have also been reported in a recent scoping review evaluating community engagement in the design and implementation of chronic disease-based interventions for Indigenous populations [110]. In that review, Wali and colleagues reported that despite the agreed need to engage with Indigenous communities to support intervention engagement, few meaningfully consulted the community through all levels of intervention design and delivery [110]. Several authors have similarly argued that adopting participatory design approaches involving Indigenous communities as co-designers and decision-makers from the outset of intervention development is critical to achieve meaningful and lasting change [111–113].
A strength of this review was the application of an organisational system for categorising cultural adaption by a Kreuter and colleagues [19] which allowed for consistent and clear description of approaches currently used in nutrition interventions for Indigenous populations around the world. The additional application of Resnicow and colleagues [20] sensitivity levels to these categories has provided another analysis and categorisation of how interventions to date have been culturally adapted. This has highlighted areas for improvement in nutrition and health intervention research, particularly related to the need for deeper approaches that go beyond consultation, such as co-design. However, we note that while the classification systems by Kreuter and colleagues [19] and Resincow and colleagues [20] are published, they are by no means recognised as a combined validated tool to measure cultural adaptability. Constructing and validating a tool to guide cultural adaptation would be useful for the design of culturally safe interventions for Indigenous populations. Further, the classification schemes used are open to subjectivity in their interpretation and may therefore be influenced by the researcher during data extraction.
The review had other limitations. Given the significant differences between the cultures of Indigenous populations worldwide and the variety of health outcomes included, an evaluation of intervention effectiveness was not within the scope of this review. Determining intervention effectiveness by Indigenous population and health outcome is an important next step. Future evaluations of intervention effectiveness should consider the level of cultural adaptations made so as to better understand potential mechanisms for intervention success. Despite the rigourous search and screening methods, given the numerous terms used to describe Indigenous populations worldwide it is possible the search strategy was not able to capture all relevant studies. Further, Indigenous health research is often published in grey literature and subsequently may not have been identified for inclusion. While this review comprehensively investigated cultural adaptation strategies used, it did not evaluate the cultural safety of these interventions. Future research should consider the cultural safety of health interventions.
Conclusion
This review is an initial step in overcoming the many barriers to developing and implementing culturally safe interventions. The results of this review provide evidence of what has previously been done and highlights priority areas for further research. This scoping review found that there is growing literature reporting complex and diverse approaches to cultural adaptation of nutrition interventions for Indigenous populations across the world. Interventions commonly use a mix of approaches for cultural adaptation, however few are adopting approaches that involve constituents at deeper levels where interventions can be owned, delivered and/or directed by the community themselves. The review highlights the need to move beyond traditional nutrition education techniques focused on behaviour change, to strengthen cultural adaptation approaches that involve Indigenous people at the community level as co-designers and decision makers in all phases of the intervention. Further research is now needed to explore the effectiveness of the types and levels of cultural adaptations used on various health outcomes to determine the most effective strategies for culturally safe nutrition interventions. This is especially relevant given the need to improve health equity for Indigenous populations and the increasing number of interventions being conducted in this population group.
Supplementary Information
Additional file 1. Detailed summary of intervention characteristics
Additional file 2. Search strategy terms with example MeSH subject headings used in Medline and Scopus databases
Additional file 3. Detailed summary of cultural adaptation strategies, formative research and theories of behaviour change used
Acknowledgements
The authors thank Tailane Scapin for her support in editing the references and final manuscript.
Abbreviations
- CINAHL
Cumulative Index to Nursing and Allied Health Literature
- RCTs
Randomized Controlled Trials
- USA
United States of America
Authors’ contributions
LV, KB and LW conceptulaised the hypothesis and design of the study. KB supported the bibliographic search. LV, KB, MS, AR, HA, RL and LW participated in the collection, analysis and interpretation of data from identified articles. LV, KB, MS & LW have written the manuscript and all authors made important contributions to different drafts. All authors approve the final manuscript and its submission to this journal.
Funding
This scoping review was supported as part of a larger project by the Children’s Hospital Foundation’s Woolworths Nutrition-Related Health Services Research Grant. The funder had no role in the study design, analysis and interpretation of data; in the communication of these results; and in the decision to submit the article for publication.
Availability of data and materials
All available data is included in the publication.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.United Nations . Indigenous peoples at the UN. 2021. [Google Scholar]
- 2.United Nations. United Nations Department of Economic and Social Affairs: State of the world's indigenous peoples. In: Division for Senior Policy and Development. II ed. New York: United Nations; 2013. p. 200. https://www.un.org/esa/socdev/unpfii/documents/SOWIP/en/SOWIP_web.pdf.
- 3.World Health Organization . Indigenous populations. 2021. [Google Scholar]
- 4.United Nations . Indigenous peoples and the MDGs. 2015. [Google Scholar]
- 5.Anderson I, Robson B, Connolly M, Al-Yaman F, Bjertness E, King A, Tynan M, Madden R, Bang A, Coimbra CEA, et al. Indigenous and tribal peoples' health (the lancet–Lowitja Institute global collaboration): a population study. Lancet. 2016;388(10040):131–157. doi: 10.1016/S0140-6736(16)00345-7. [DOI] [PubMed] [Google Scholar]
- 6.Mitrou F, Cooke M, Lawrence D, Povah D, Mobilia E, Guimond E, Zubrick SR. Gaps in indigenous disadvantage not closing: a census cohort study of social determinants of health in Australia, Canada, and New Zealand from 1981–2006. BMC Public Health. 2014;14(1):201. doi: 10.1186/1471-2458-14-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bourke CJ, Marrie H, Marrie A. Transforming institutional racism at an Australian hospital. Aust Health Rev. 2019;43(6):611–618. doi: 10.1071/AH18062. [DOI] [PubMed] [Google Scholar]
- 8.Willett WC, Koplan JP, Nugent R, Dusenbury C, Puska P, FGaziano TA. Prevention of chronic disease by means of diet and lifestyle changes. Disease control priorities in developing countries. New York: Oxford University Press; 2006. [Google Scholar]
- 9.Browne J, Lock M, Walker T, Egan M, Backholer K. Effects of food policy actions on indigenous peoples’ nutrition-related outcomes: a systematic review. BMJ Glob Health. 2020;5(8):e002442. doi: 10.1136/bmjgh-2020-002442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gwynn J, Sim K, Searle T, Senior A, Lee A, Brimblecombe J. Effect of nutrition interventions on diet-related and health outcomes of Aboriginal and Torres Strait islander Australians: a systematic review. BMJ Open. 2019;9(4):e025291. doi: 10.1136/bmjopen-2018-025291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stephens C, Nettleton C, Porter J, Willis R, Clark S. Indigenous peoples' health--why are they behind everyone, everywhere? Lancet. 2005;366(9479):10–13. doi: 10.1016/S0140-6736(05)66801-8. [DOI] [PubMed] [Google Scholar]
- 12.Mark GT, Lyons AC. Maori healers' views on wellbeing: the importance of mind, body, spirit, family and land. Soc Sci Med. 2010;70(11):1756–1764. doi: 10.1016/j.socscimed.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 13.Wade DT, Halligan PW. Do biomedical models of illness make for good healthcare systems? BMJ. 2004;329(7479):1398–1401. doi: 10.1136/bmj.329.7479.1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harfield SG, Davy C, McArthur A, Munn Z, Brown A, Brown N. Characteristics of indigenous primary health care service delivery models: a systematic scoping review. Glob Health. 2018;14(1):12. doi: 10.1186/s12992-018-0332-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Castro FG, Barrera M, Jr, Holleran Steiker LK. Issues and challenges in the design of culturally adapted evidence-based interventions. Annu Rev Clin Psychol. 2010;6(1):213–239. doi: 10.1146/annurev-clinpsy-033109-132032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Movsisyan A, Arnold L, Evans R, Hallingberg B, Moore G, O’Cathain A, Pfadenhauer LM, Segrott J, Rehfuess E. Adapting evidence-informed complex population health interventions for new contexts: a systematic review of guidance. Implement Sci. 2019;14(1):105. doi: 10.1186/s13012-019-0956-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Curtis E, Jones R, Tipene-Leach D, Walker C, Loring B, Paine S-J, Reid P. Why cultural safety rather than cultural competency is required to achieve health equity: a literature review and recommended definition. Int J Equity Health. 2019;18(1):174. doi: 10.1186/s12939-019-1082-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marsiglia FF, Booth JM. Cultural adaptation of interventions in real practice settings. Res Soc Work Pract. 2015;25(4):423–432. doi: 10.1177/1049731514535989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav. 2003;30(2):133–146. doi: 10.1177/1090198102251021. [DOI] [PubMed] [Google Scholar]
- 20.Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn Dis. 1999;9(1):10–21. [PubMed] [Google Scholar]
- 21.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 23.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 24.United Nations . United Nations Permanent Forum on Indigenous Issues. Indigenous People Indigenous Voice Fact Sheet. 2008. [Google Scholar]
- 25.United Nations . State of the World's indigenous peoples: implementing the United Nations declaration on the rights of indigenous peoples. New York: Department of Economic and Social Affairs; 2019. [Google Scholar]
- 26.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abbott PA, Davison JE, Moore LF, Rubinstein R. Effective nutrition education for Aboriginal Australians: lessons from a diabetes cooking course. J Nutr Educ Behav. 2012;44(1):55–59. doi: 10.1016/j.jneb.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 28.Allen P, Thompson JL, Herman CJ, Qualls C, Helitzer DL, Whyte AN, et al. Impact of periodic follow-up testing among urban American Indian women with impaired fasting glucose. Prev Chronic Dis. 2008;5(3):A76. [PMC free article] [PubMed] [Google Scholar]
- 29.Balmer L, Foster V. Preliminary evaluation of the effects of a nutrition awareness project on the Ngaanyatjarra Pitjantjatjara Yankunytjatjara communities of Central Australia. Collegian. 1997;4(2):26–32. doi: 10.1016/S1322-7696(08)60218-8. [DOI] [PubMed] [Google Scholar]
- 30.Bertilone C, McEvoy S. Success in closing the gap: Favourable neonatal outcomes in a metropolitan aboriginal maternity group practice program. MJA. 2015;203(6):262.e1–262.e7. doi: 10.5694/mja14.01754. [DOI] [PubMed] [Google Scholar]
- 31.Brimblecombe J, Ferguson M, Liberato SC, Ball K, Moodie ML, Magnus A, et al. Stores healthy options project in remote indigenous communities (SHOP@RIC): a protocol of a randomised trial promoting healthy food and beverage purchases through price discounts and in-store nutrition education. BMC Public Health. 2013;13:744. doi: 10.1186/1471-2458-13-744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Caballero B, Davis S, Davis CE, Ethelbah B, Evans M, Lohman T, Stephenson L, Story M, White J. Pathways: a school-based program for the primary prevention of obesity in American Indian children. J Nutr Biochem. 1998;9(9):535–543. doi: 10.1016/S0955-2863(98)00049-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chambers RA, Rosenstock S, Neault N, Kenney A, Richards J, Begay K, Blackwater T, Laluk O, Duggan C, Reid R, Barlow A. A home-visiting diabetes prevention and management program for American Indian youth. Diabetes Educ. 2015;41(6):729–747. doi: 10.1177/0145721715608953. [DOI] [PubMed] [Google Scholar]
- 34.Collier AF, Daiss S, Temengil E, Russell SC, Miller JC, Renguul FM. Developing an obesity intervention in Micronesia: from needs assessment to planning. Eval Program Plann. 2018;69:33–42. doi: 10.1016/j.evalprogplan.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 35.Counil É, Gauthier MJ, Blouin V, Grey M, Angiyou E, Kauki T, et al. Translational research to reduce trans-fat intakes in Northern Québec (Nunavik) Inuit communities: A success story? Int J Circumpolar Health. 2012;71(1):18833. doi: 10.3402/ijch.v71i0.18833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Daniel M, Green LW, Marion SA, Gamble D, Herbert CP, Hertzman C, Sheps SB. Effectiveness of community-directed diabetes prevention and control in a rural Aboriginal population in British Columbia, Canada. Soc Sci Med. 1999;48(6):815–832. doi: 10.1016/S0277-9536(98)00403-1. [DOI] [PubMed] [Google Scholar]
- 37.Davis S, Gomez Y, Lambert L, Skipper B. Primary prevention of obesity in American Indian children. In: Williams CK, Kimm SYS, editors. Prevention and Treatment of Childhood Obesity. New York: New York Academy of Sciences; 1993. pp. 167–180. [DOI] [PubMed] [Google Scholar]
- 38.DeBruyn L, Fullerton L, Satterfield D, Frank M. Integrating culture and history to promote health and help prevent type 2 diabetes in American Indian/Alaska native communities: traditional foods have become a way to talk about health. Prev Chronic Dis. 2020;17:1–14. doi: 10.5888/pcd17.190213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.DePue JD, Rosen RK, Seiden A, Bereolos N, Chima ML, Goldstein MG, et al. Implementation of a culturally tailored diabetes intervention with community health workers in American Samoa. Diabetes Educ. 2013;39(6):761–771. doi: 10.1177/0145721713504630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Foley W, Spurr S, Lenoy L, De Jong M, Fichera R. Cooking skills are important competencies for promoting healthy eating in an urban indigenous health service. Nutr Diet. 2011;68(4):291–296. doi: 10.1111/j.1747-0080.2011.01551.x. [DOI] [Google Scholar]
- 41.Gates A, Hanning RM, Gates M, Tsuji LJS. The food and nutrient intakes of first nations youth living in northern Ontario, Canada: evaluation of a harvest sharing program. J Hunger Environ Nutr. 2016;11(4):491–508. doi: 10.1080/19320248.2016.1157552. [DOI] [Google Scholar]
- 42.Gittelsohn J, Kim EM, He S, Pardilla M. A food store-based environmental intervention is associated with reduced BMI and improved psychosocial factors and food-related behaviors on the Navajo nation. J Nutr. 2013;143(9):1494–1500. doi: 10.3945/jn.112.165266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Govula C, Kattelman K, Ren C. Culturally appropriate nutrition lessons increased fruit and vegetable consumption in American Indian children. Top Clin Nutr. 2007;22(3):239–245. doi: 10.1097/01.TIN.0000285378.01218.67. [DOI] [Google Scholar]
- 44.Gracey M, Bridge E, Martin D, Jones T, Spargo R, M. o et al. An Aboriginal-driven program to prevent, control and manage nutrition-related "lifestyle" diseases including diabetes. Asia Pac J Clin Nutr. 2006;15(2):178–188. [PubMed] [Google Scholar]
- 45.Hanbazaza MA, Triador L, Ball GDC, Farmer A, Maximova KA, et al. The impact of school gardening on cree children's knowledge and attitudes toward vegetables and fruit. Can J Diet Pract Res. 2015;76(3):133–139. doi: 10.3148/cjdpr-2015-007. [DOI] [PubMed] [Google Scholar]
- 46.Jernigan VBB, Williams M, Wetherill M, Taniguchi T, Jacob T, Cannady T, Grammar M, Standridge J, Fox J, Wiley AD, Tingle JA, Riley M, Spiegel J, Love C, Noonan C, Weedn A, Salvatore AL. Using community-based participatory research to develop healthy retail strategies in native American-owned convenience stores: the THRIVE study. Prev Med Rep. 2018;11:148–153. doi: 10.1016/j.pmedr.2018.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Karanja N, Lutz T, Ritenbaugh C, Maupome G, Jones J, Becker T, Aickin M. The TOTS community intervention to prevent overweight in American Indian toddlers beginning at birth: a feasibility and efficacy study. J Community Health. 2010;35(6):667–675. doi: 10.1007/s10900-010-9270-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kattelmann KK, Conti K, Ren C. The medicine wheel nutrition intervention: a diabetes education study with the Cheyenne River Sioux tribe. J Acad Nutr Diet. 2009;109(9):1532–1539. doi: 10.1016/j.jada.2009.06.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kenny TA, MacLean J, Gale P, Keats S, Chan HM, Wesche SD. Linking health and the environment through education—a traditional food program in Inuvik, Western Canadian Arctic. J Hunger Environ Nutr. 2018;13(3):429–432. doi: 10.1080/19320248.2017.1420330. [DOI] [Google Scholar]
- 50.LaRowe TL, Wubben DP, Cronin KA, Vannatter SM, Adams A, K. r Development of a culturally appropriate, home-based nutrition and physical activity curriculum for Wisconsin American Indian families. Prev Chronic Dis. 2007;4(4):A109–A10A. [PMC free article] [PubMed] [Google Scholar]
- 51.Lee AJ, Bailey AP, Yarmirr D, O'Dea K, Mathews JD. Survival tucker: improved diet and health indicators in an Aboriginal community. Aust J Public Health. 1994;18(3):277–285. doi: 10.1111/j.1753-6405.1994.tb00245.x. [DOI] [PubMed] [Google Scholar]
- 52.Lee ET, Jobe JB, Yeh J, Ali T, Rhoades ER, Knehans AW, Willis DJ, Johnson MR, Zhang Y, Poolaw B, Rogers B. A cardiovascular risk reduction program for American Indians with metabolic syndrome: the balance study. J Prim Prev. 2012;33(4):187–196. doi: 10.1007/s10935-012-0273-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Leenen I, Givaudan M, Pick S, Venguer T, Vera J, Poortinga YH. Effectiveness of a Mexican health education program in a poverty-stricken rural area of Guatemala. J Cross-Cult Psychol. 2008;39(2):198–214. doi: 10.1177/0022022107312588. [DOI] [Google Scholar]
- 54.Leslie JH. Uli'eo Koa program: incorporating a traditional Hawaiian dietary component. Pac Health Dialog. 2001;8(2):401–406. [PubMed] [Google Scholar]
- 55.Macaulay AC, Paradis G, Potvin L, Cross EJ, Saad-Haddad C, McComber A, Desrosiers S, Kirby R, Montour LT, Lamping DL, Leduc N, Rivard M. The Kahnawake schools diabetes prevention project: intervention, evaluation, and baseline results of a diabetes primary prevention program with a native community in Canada. Prev Med. 1997;26(6):779–790. doi: 10.1006/pmed.1997.0241. [DOI] [PubMed] [Google Scholar]
- 56.Marlow E, Melkus GD, Bosma AM. Professional development. STOP diabetes! An educational model for native American adolescents in the prevention of diabetes. Diabetes Educ. 1998;24(4):441–448. doi: 10.1177/014572179802400403. [DOI] [PubMed] [Google Scholar]
- 57.Mattingly JA, Andresen PA. NAP SACC: Implementation of an obesity prevention intervention in an American Indian head start program. J Community Health Nurs. 2016;33(3):145–153. doi: 10.1080/07370016.2016.1191871. [DOI] [PubMed] [Google Scholar]
- 58.Mendenhall TJ, Berge JM, Harper P, GreenCrow B, LittleWalker N, WhiteEagle S, BrownOwl S. The family education diabetes series (FEDS): community-based participatory research with a midwestern American Indian community. Nurs Inq. 2010;17(4):359–372. doi: 10.1111/j.1440-1800.2010.00508.x. [DOI] [PubMed] [Google Scholar]
- 59.Mercer C, Riini D, Hamerton H, Morrison L, McPherson B. Evaluating a healthy eating, healthy action program in small Mãori communities in Aotearoa. N Z Aust J Prim Health. 2013;19(1):74–80. doi: 10.1071/PY11096. [DOI] [PubMed] [Google Scholar]
- 60.Murphy E, McAuley KA, Bell D, McLay RT, Chisholm A, Hurley R, Story G, Mann JI, Thomson R, Williams SM. A new approach to design and implement a lifestyle intervention programme to prevent type 2 diabetes in New Zealand Maori. Asia Pac J Clin Nutr. 2003;12(4):419–422. [PubMed] [Google Scholar]
- 61.Murphy S, Wilson C. Breastfeeding promotion: a rational and achievable target for a type 2 diabetes prevention intervention in native American communities. J Hum Lact. 2008;24(2):193–198. doi: 10.1177/0890334408317434. [DOI] [PubMed] [Google Scholar]
- 62.Narayan KMV, Hoskin M, Kozak D, Kriska AM, Hanson RL, Pettitt DJ, et al. Randomized clinical trial of lifestyle interventions in Pima Indians: a pilot study. Diabet Med. 1998;15(1):66–72. doi: 10.1002/(SICI)1096-9136(199801)15:1<66::AID-DIA515>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 63.Nelson RG, Pankratz VS, Ghahate DM, Bobelu J, Faber T, Shah VO. Home-based kidney care, patient activation, and risk factors for CKD progression in zuni indians a randomized, controlled clinical trial. CJASN. 2018;13(12):1801–1809. doi: 10.2215/CJN.06910618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nu J, Bersamin A. Collaborating with Alaska native communities to design a cultural food intervention to address nutrition transition. Prog Community Health Partnersh. 2017;11(1):71–80. doi: 10.1353/cpr.2017.0009. [DOI] [PubMed] [Google Scholar]
- 65.Redmond LC, Jock B, Gadhoke P, Chiu DT, Christiansen K, Pardilla M, Swartz J, Platero H, Caulfield LE, Gittelsohn J. OPREVENT (obesity prevention and evaluation of InterVention effectiveness in NaTive north Americans): design of a multilevel, multicomponent obesity intervention for native American adults and households. Curr Dev Nutr. 2019;3(Suppl 2):81–93. doi: 10.1093/cdn/nzz009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rolleston AK, Doughty R, Poppe K. Integration of kaupapa Māori concepts in health research: a way forward for Māori cardiovascular health? J Prim Health Care. 2016;8(1):60–66. doi: 10.1071/HC15034. [DOI] [PubMed] [Google Scholar]
- 67.Ronsley R, Lee AS, Kuzeljevic B, Panagiotopoulos C. Healthy buddies™ reduces body mass index z-score and waist circumference in Aboriginal children living in remote coastal communities. J Sch Health. 2013;83(9):605–613. doi: 10.1111/josh.12072. [DOI] [PubMed] [Google Scholar]
- 68.Rowley KG, Daniel M, Skinner K, Skinner M, White GA, O'Dea K. Effectiveness of a community-directed 'healthy lifestyle' program in a remote Australian Aboriginal community. Aust N Z J Publ Health. 2000;24(2):136–144. doi: 10.1111/j.1467-842X.2000.tb00133.x. [DOI] [PubMed] [Google Scholar]
- 69.Saksvig BI, Gittelsohn J, Harris SB, Hanley AJG, Valente TW, Zinman B. A pilot school-based healthy eating and physical activity intervention improves diet, food knowledge, and self-efficacy for native Canadian children. J Nutr. 2005;135(10):2392–2398. doi: 10.1093/jn/135.10.2392. [DOI] [PubMed] [Google Scholar]
- 70.Sauder KA, Dabelea D, Bailey-Callahan R, Kanott Lambert S, Powell J, James R, Percy C, Jenks BF, Testaverde L, Thomas JM, Barber R, Smiley J, Hockett CW, Zhong VW, Letourneau L, Moore K, Delamater AM, Mayer-Davis E. Targeting risk factors for type 2 diabetes in American Indian youth: the tribal turning point pilot study. Pediatr Obes. 2018;13(5):321–329. doi: 10.1111/ijpo.12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shintani TT, Hughes CK, Beckham S, O'Connor HK. Obesity and cardiovascular risk intervention through the ad libitum feeding of traditional Hawaiian diet. Am J Clin Nutr. 1991;53(6 Suppl):1647s–1651s. doi: 10.1093/ajcn/53.6.1647S. [DOI] [PubMed] [Google Scholar]
- 72.Story M, Hannan PJ, Fulkerson JA, Rock BH, Smyth M, Arcan C, et al. Bright start: description and main outcomes from a group-randomized obesity prevention trial in American Indian children. Obesity. 2021;20(11):2241–2249. doi: 10.1038/oby.2012.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Vastine A, Gittelsohn J, Ethelbah B, Anliker J, Caballero B. Formative research and stakeholder participation in intervention development. Am J Health Behav. 2005;29(1):57–69. doi: 10.5993/AJHB.29.1.5. [DOI] [PubMed] [Google Scholar]
- 74.Walters KL, LaMarr J, Levy RL, Pearson C, Maresca T, Mohammed SA, et al. Project həli?dx(w)/healthy hearts across generations: development and evaluation design of a tribally based cardiovascular disease prevention intervention for American Indian families. J Prim Prev. 2012;33(4):197–207. doi: 10.1007/s10935-012-0274-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Witmer JM, Hensel MR, Holck PS, Ammerman AS, Will JC. Heart disease prevention for Alaska native women: a review of pilot study findings. J Women's Health. 2004;13(5):569–578. doi: 10.1089/1540999041280981. [DOI] [PubMed] [Google Scholar]
- 76.Ziabakhsh S, Pederson A, Prodan-Bhalla N, Middagh D, Jinkerson-Brass S. Women-centered and culturally responsive heart health promotion among indigenous women in Canada. Health Promot Pract. 2016;17(6):814–826. doi: 10.1177/1524839916633238. [DOI] [PubMed] [Google Scholar]
- 77.Jiang L, Johnson A, Pratte K, Beals J, Bullock A, Manson SM. Long-term outcomes of lifestyle intervention to prevent diabetes in American Indian and Alaska native communities: the special diabetes program for Indians diabetes prevention program. Diabetes Care. 2018;41(7):1462–1470. doi: 10.2337/dc17-2685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Blinkhorn F, Wallace J, Smith L, Blinkhorn AS. Developing leaflets to give dental health advice to Aboriginal families with young children. Int Dent J. 2014;64(4):195–199. doi: 10.1111/idj.12108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Brooking LA, Williams SM, Mann JI. Effects of macronutrient composition of the diet on body fat in indigenous people at high risk of type 2 diabetes. Diabetes Res Clin Pract. 2012;96(1):40–46. doi: 10.1016/j.diabres.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 80.Canuto KJ, McDermott RA, Cargo M, Esterman AJ. Study protocol: a pragmatic randomised controlled trial of a 12-week physical activity and nutritional education program for overweight Aboriginal and Torres Strait Islander women. BMC Public Health. 2011;11:655. doi: 10.1186/1471-2458-11-655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Coppell KJ, Tipene-Leach DC, Pahau HLR, Williams SM, Abel S, Iles M, Hindmarsh JH, Mann JI. Two-year results from a community-wide diabetes prevention intervention in a high risk indigenous community: the Ngati and healthy project. Diabetes Res Clin Pract. 2009;85(2):220–227. doi: 10.1016/j.diabres.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 82.Gachupin FC, Joe JR. American Indian youth: a residential camp program for wellness. Health Dispar Res Pract. 2017;10(4):11. [Google Scholar]
- 83.Hemmingson K, Lucchesi R, Droke E, Kattelmann KK. Tailoring a web-based weight maintenance intervention for Northern Plains American Indian public university students. Health Educ J. 2016;75(5):528–539. doi: 10.1177/0017896915607909. [DOI] [Google Scholar]
- 84.Lawrence HP, Romanetz M, Rutherford L, Cappel L, Binguis D, Rogers JB. Effects of a community-based prenatal nutrition program on the oral health of Aboriginal preschool children in northern Ontario. Probe. 2004;38(4):172–188. [Google Scholar]
- 85.Merrick J, Chong A, Parker E, Roberts-Thomson K, Misan G, Spencer J, Broughton J, Lawrence H, Jamieson L. Reducing disease burden and health inequalities arising from chronic disease among indigenous children: an early childhood caries intervention. BMC Public Health. 2012;12(1):323. doi: 10.1186/1471-2458-12-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Quinn E, O'Hara BJ, Ahmed N, Winch S, McGill B, Banovic D, et al. Enhancing the get healthy information and coaching service for Aboriginal adults: evaluation of the process and impact of the program. Int J Equity Health. 2017;16(1):168–178. doi: 10.1186/s12939-017-0641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Robertson C, Kattelmann K, Ren C. Control of type 2 diabetes mellitus using interactive internet-based support on a Northern Plains Indian reservation: a pilot study. Top Clin Nutr. 2007;22(2):185–193. doi: 10.1097/01.TIN.0000270137.00099.91. [DOI] [Google Scholar]
- 88.Seear KH, Atkinson DN, Lelievre MP, Henderson-Yates LM, Marley JV. Piloting a culturally appropriate, localised diabetes prevention program for young Aboriginal people in a remote town. Aust J Prim Health. 2019;25(5):495–500. doi: 10.1071/PY19024. [DOI] [PubMed] [Google Scholar]
- 89.Teufel NI, Ritenbaugh CK. Development of a primary prevention program: insight gained in the Zuni diabetes prevention program. Clin Pediatr. 1998;37(2):131–141. doi: 10.1177/000992289803700211. [DOI] [PubMed] [Google Scholar]
- 90.Anand SS, Davis AD, Ahmed R, Jacobs R, Xie C, Hill A, et al. A family-based intervention to promote healthy lifestyles in an Aboriginal community in Canada. Can J Public Health. 2007;98(6):447–452. doi: 10.1007/BF03405436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Battersby MW, Kit JA, Prideaux C, Harvey PW, Collins JP, Mills PD. Implementing the flinders model of self-management support with Aboriginal people who have diabetes: findings from a pilot study. Aust J Prim Health. 2008;14(1):66–74. doi: 10.1071/PY08009. [DOI] [Google Scholar]
- 92.Brown B, Noonan C, Harris KJ, Parker M, Gaskill S, Ricci C, Cobbs G, Gress S. Developing and piloting the journey to native youth health program in Northern Plains Indian communities. Diabetes Educ. 2013;39(1):109–118. doi: 10.1177/0145721712465343. [DOI] [PubMed] [Google Scholar]
- 93.Jiang L, Manson SM, Beals J, Henderson WG, Huang H, Acton KJ, Roubideaux Y, the Special Diabetes Program for Indians Diabetes Prevention Demonstration Project Translating the diabetes prevention program into American Indian and Alaska native communities: results from the special diabetes program for Indians diabetes prevention demonstration project. Diabetes Care. 2013;36(7):2027–2034. doi: 10.2337/dc12-1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.United Nations . Department of Economic and Social Affairs. New York: United Nations Publications; 2009. Statistical division. State of the World's indigenous peoples. [Google Scholar]
- 95.Paradies Y. Colonisation, racism and indigenous health. J Popul Res. 2016;33(1):83–96. doi: 10.1007/s12546-016-9159-y. [DOI] [Google Scholar]
- 96.Pulver LJ, Haswell M, Ring I, Waldon J, Clark W, Whetung V, et al. Indigenous health: Australia, Canada, Aotearoa, New Zealand and the United States: laying claim to a future that embraces health for us all. Geneva: World Health Organization; 2010. [Google Scholar]
- 97.Randall DA, Lujic S, Havard A, Eades SJ, Jorm L. Multimorbidity among Aboriginal people in New South Wales contributes significantly to their higher mortality. Med J Aust. 2018;209(1):19–23. doi: 10.5694/mja17.00878. [DOI] [PubMed] [Google Scholar]
- 98.Schumacher C, Ferucci ED, Lanier AP, Slattery ML, Schraer CD, Raymer TW, Dillard D, Murtaugh MA, Tom-Orme L. Metabolic syndrome: prevalence among American Indian and Alaska native people living in the southwestern United States and in Alaska. Metab Syndr Relat Disord. 2008;6(4):267–273. doi: 10.1089/met.2008.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hutchinson RN, Shin S. Systematic review of health disparities for cardiovascular diseases and associated factors among American Indian and Alaska native populations. PLoS One. 2014;9(1):e80973. doi: 10.1371/journal.pone.0080973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Titmuss A, Davis EA, Brown A, Maple-Brown LJ. Emerging diabetes and metabolic conditions among Aboriginal and Torres Strait Islander young people. Med J Aust. 2019;210(3):111–3.e1. doi: 10.5694/mja2.13002. [DOI] [PubMed] [Google Scholar]
- 101.Ramirez-Zea M, Kroker-Lobos MF, Close-Fernandez R, Kanter R. The double burden of malnutrition in indigenous and nonindigenous Guatemalan populations. Am J Clin Nutr. 2014;100:1644s–1651s. doi: 10.3945/ajcn.114.083857. [DOI] [PubMed] [Google Scholar]
- 102.Wong CY, Zalilah MS, Chua EY, Norhasmah S, Chin YS, Siti Nur’Asyura A. Double-burden of malnutrition among the indigenous peoples (orang Asli) of peninsular Malaysia. BMC Public Health. 2015;15(1):680. doi: 10.1186/s12889-015-2058-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hudson S. Healthy stores, healthy communities: the impact of outback stores on remote indigenous Australians. St Leonards: Centre for Independent Studies; 2010.
- 104.Kagie R, Lin S-YN, Hussain MA, Thompson SC. A pragmatic review to assist planning and practice in delivering nutrition education to indigenous youth. Nutrients. 2019;11(3):510. doi: 10.3390/nu11030510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.United Nations. Transforming our world: the 2030 Agenda for sustainable development. In: Division for Sustainable Development Goals. New York: United Nations; 2015. https://sustainabledevelopment.un.org/content/documents/21252030%20Agenda%20for%20Sustainable%20Development%20web.pdf.
- 106.Di A. Indigenous health: a worldwide focus. Lancet. 2016;388(10040):104. doi: 10.1016/S0140-6736(16)31020-0. [DOI] [PubMed] [Google Scholar]
- 107.Rigby RR, Mitchell LJ, Hamilton K, Williams LT. The use of behavior change theories in dietetics practice in primary health care: a systematic review of randomized controlled trials. J Acad Nutr Diet. 2020;120(7):1172–1197. doi: 10.1016/j.jand.2020.03.019. [DOI] [PubMed] [Google Scholar]
- 108.Gittelsohn J, Rowan M. Preventing diabetes and obesity in American Indian communities: the potential of environmental interventions. Am J Clin Nutr. 2011;93(5):1179S–1183S. doi: 10.3945/ajcn.110.003509. [DOI] [PubMed] [Google Scholar]
- 109.Davis PC, Jr, Rankin LL. Guidelines for making existing health education programs more culturally appropriate. Am J Health Educ. 2006;37(4):250–252. doi: 10.1080/19325037.2006.10598912. [DOI] [Google Scholar]
- 110.Wali S, Superina S, Mashford-Pringle A, Ross H, Cafazzo JA. What do you mean by engagement? – evaluating the use of community engagement in the design and implementation of chronic disease-based interventions for indigenous populations – scoping review. Int J Equity Health. 2021;20(1):8. doi: 10.1186/s12939-020-01346-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Cyril S, Smith BJ, Possamai-Inesedy A, Renzaho AMN. Exploring the role of community engagement in improving the health of disadvantaged populations: a systematic review. Glob Health Action. 2015;8(1):29842. doi: 10.3402/gha.v8.29842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Harding T, Oetzel J. Implementation effectiveness of health interventions for indigenous communities: a systematic review. Implement Sci. 2019;14(1):76. doi: 10.1186/s13012-019-0920-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Schembri L, Curran J, Collins L, Pelinovskaia M, Bell H, Richardson C, Palermo C. The effect of nutrition education on nutrition-related health outcomes of Aboriginal and Torres Strait islander people: a systematic review. Aust N Z J Public Health. 2016;40(S1):S42–SS7. doi: 10.1111/1753-6405.12392. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Detailed summary of intervention characteristics
Additional file 2. Search strategy terms with example MeSH subject headings used in Medline and Scopus databases
Additional file 3. Detailed summary of cultural adaptation strategies, formative research and theories of behaviour change used
Data Availability Statement
All available data is included in the publication.