Abstract
Laparoscopic sacrocolpopexy is one of the most difficult laparoscopic surgical techniques. In this study, we report on our efforts to safely perform this procedure, which consists of suturing a piece of mesh onto the anterior longitudinal ligament using a nonabsorbent suture during mesh fixation onto the prepromontorium layer, which can lead to massive bleeding if a mistake is made, by performing preoperative and intraoperative image evaluation. Preoperative contrast-enhanced computed tomography was performed. Images in DICOM format were acquired, and three-dimensional vessel reconstruction was performed. After performing a peritoneal incision in the presacral area, ultrasonography was performed using a probe inserted through a 12-mm trocar into the abdominal cavity to re-confirm the absence of vessels near the planned suturing area. After ultrasonography, an Ethibond® suture was inserted through the anterior longitudinal ligament. In our hospital, 126 patients underwent the procedure, and none had a serious hemorrhage or required blood transfusion, indicating the safety of this modified procedure without separation of a wide presacral area. We believe that these techniques can be performed safely with minimal incision. However, we did not examine the efficacy of these techniques in this paper. Further studies are needed to determine whether this approach is suitable.
Keywords: Computed tomography, laparoscopic sacrocolpopexy, ultrasonography
INTRODUCTION
Pelvic organ prolapse, which is becoming increasingly common due to the aging population, is a disorder that adversely affects the quality of life of women. The incidence of pelvic organ prolapse is high, one in four healthy women and 40% of women who have given birth will be affected by this disease in Japan.[1,2] The relative risk of undergoing surgery for this disorder is 11%.[3] Laparoscopic sacrocolpopexy (LSC) was first reported by Nezhat et al. in 1994.[4] Since the Food and Drug Administration issued an alert concerning vaginal mesh surgery has been issued in the US, it has become a well-used treatment option.[5] However, LSC remains a technically challenging laparoscopic surgery.
This difficult procedure involves suturing a piece of mesh to the anterior longitudinal ligament using a nonabsorbable suture into the prepromontorium layer. Large vessels are present in this area, and even a small error can lead to serious hemorrhage.[1,6,7] In addition, anatomical variations in the veins in this area require close attention. Albanesi et al. describe creating a three-dimensional (3D) model of the female pelvis using computed tomography (CT) and estimating the positional relationship between the blood vessels and the prepromontorium layer.[8] While these 3D models are useful for safe mesh fixation, they are merely theoretical and have yet to be analyzed in practice.
We report two measures that increase the safety of placing a nonabsorbable suture through the anterior longitudinal ligament after opening the entire presacral area, which is associated with a high risk of serious hemorrhage. First, preoperative contrast-enhanced CT is performed to identify anatomical variations in the arteries and veins based on reconstructed 3D images. Second, perioperative ultrasonography using a probe introduced through a trocar is performed to confirm the absence of vessels at the site before suturing. To the best of our knowledge, these two measures have not been previously reported.
SUBJECTS AND METHODS
The surgical indications for LSC were all pelvic organ prolapse injuries at DeLancey's level I,[9] predominantly in sexually active young individuals. LSC was performed for pelvic organ prolapse in patients with favorable performance status and no uncontrollable medical complications such as diabetes. This study was approved by the Ethics Committee of Kindai University (No. 26-090). All patients provided written informed consent prior to participating in this study.
Preoperative contrast-enhanced CT was performed using a contrast agent (600 mg I/kg bodyweight) administered over a 30 s period [Figure 1]. The first-phase scan started 12 s after visual confirmation of the arrival of the contrast agent at the monitoring site (from the liver to the horizontal portion of the duodenum) for simultaneous visualization of both arteries and veins. The second-phase scan began 80 s after the start of contrast agent administration. Images in DICOM format (slice thickness, 0.625 mm) were acquired, and 3D vessel reconstruction was performed using OsiriX® .
Figure 1.
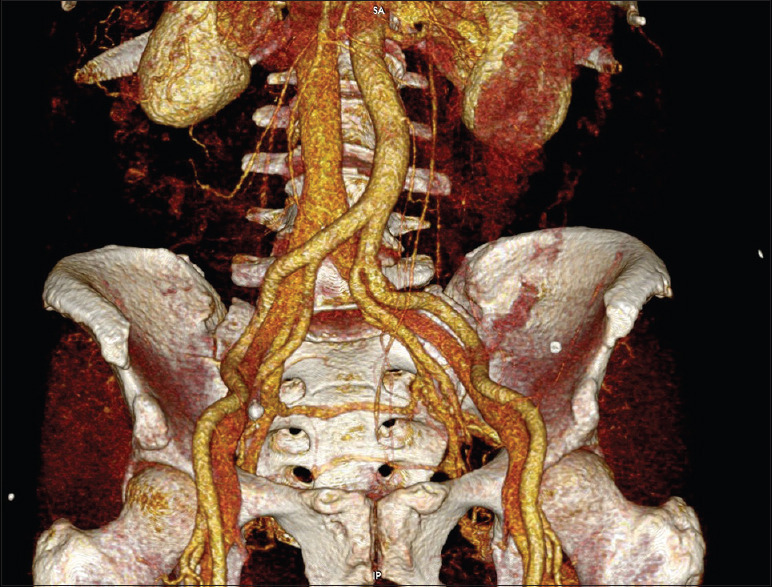
Preoperative contrast-enhanced computed tomography image. Anatomical vascular variations were examined after three-dimensional reconstruction
A closed approach was used to establish the pneumoperitoneum through the umbilicus, and a trocar with a camera was inserted to observe the inside of the abdominal cavity. A 12-mm trocar was inserted into the lower left abdomen, and 5-mm trocars were inserted in the center and the lower right abdomen. A Free Jaw clip® (Kyocera Medical, Osaka, Japan) was placed on an epiploic appendix along the sigmoid colon, and the intestines were lifted and placed on the upper left abdomen to establish the surgical view. After performing a peritoneal incision into the presacral area, ultrasonography was performed using an ARIETTAS70® (Hitachi Aloka, Tokyo, Japan) and a 7.5 MHz probe inserted through a 12-mm trocar into the abdominal cavity to re-confirm the absence of vessels near the planned suturing area [Figures2 and 3]. A drop-in probe with an L43K transducer was used. The terminal scale was 51 mm, and the width of the field of view was 26 mm. An Ethibond® (Johnson and Johnson Japan, Tokyo, Japan) suture (No. 0) was inserted through the anterior longitudinal ligament and left untied.
Figure 2.
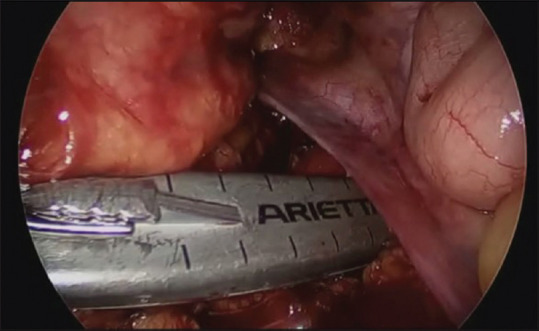
The absence of vessels at the suturing site was confirmed before suturing using an ultrasonography probe (drop-in probe) introduced through a trocar
Figure 3.
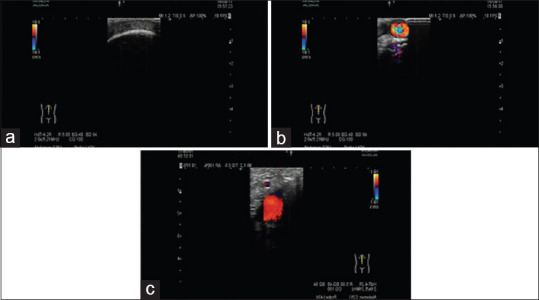
Ultrasound image confirming the absence of vessels in the presacral area. (a) Image at a position where there are no blood vessels and a thread can be applied (b) Image to the right of a, where the common iliac artery is visible (c) Image to the left of a, where the common iliac vein is visible
The retroperitoneum was cut on the medial side of the right uterosacral ligament, and a subtotal hysterectomy and bilateral adnexectomy were then performed.[10,11] The uterus was removed using a morcellator. The rectovaginal space was exposed, and a posterior colporrhaphy was performed using a V-Loc® (Medtronic Japan). The vesicovaginal space was separated, and a piece of mesh (Gynemesh® , Johnson and Johnson Japan) was inserted and placed on the anterior wall of the vagina. The mesh was sutured with seven stitches using Ethibond® sutures (No. 3-0) onto the vaginal wall and the cervix of the uterus, and was then lifted and stitched to the premade untied suture in the anterior longitudinal ligament. The peritoneum was fully closed using an absorbable suture to complete the surgery.
In general, patients were ambulatory and began to orally intake food on postoperative day 1, underwent urethral catheter removal on postoperative day 2, and were discharged on postoperative day 4.
RESULTS
In our hospital, 126 patients have undergone the procedure presented, and none of them had serious hemorrhage or required blood transfusion, indicating the safety of this modified procedure without separation of a wide presacral area. Nevertheless, the sacral vein, in addition to a branch of the abdominal aorta and both iliac veins, runs in the presacral area in some patients [Figure 4].
Figure 4.

Computed tomography image depicting the right internal iliac vein merging into the left common iliac vein
DISCUSSION
Suturing in the presacral area, which can contain anatomical variations in the vasculature, is one of the most difficult procedures in LSC because an injury to a vessel can cause serious hemorrhage.[1,6,7] Abnormally distributed blood vessels can require the separation of a wide presacral area necessary to confirm the path of the blood vessels. Sutton et al. reported that the separation of a wide presacral area increases the risk of hemorrhage from vascular plexuses.[6] Our technique can be performed with a minimal incision, without widening the prepromontorium layer, to check the vascularization.
Albanesi et al. describe creating a 3D model of the female pelvis using CT and estimating the positional relationship between the blood vessels and the prepromontorium layer.[8] Our paper does not discuss the distances and relationship between the anatomy. We think that the combination of CT and intraoperative ultrasonography of the vascular enables performing the procedure safely by ensuring that there are no vessels in the area to be sutured. However, although this technique seems to improve safety, to unequivocally determine its safety profile, a comparative study that includes alternative techniques is necessary, which would address the limiting factor of this study.
The modified procedure described in this study ensures the safety of this increasingly common procedure not just when performed by select experts but by any surgeon.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ganatra AM, Rozet F, Sanchez-Salas R, Barret E, Galiano M, Cathelineau X, et al. The current status of laparoscopic sacrocolpopexy: A review. Eur Urol. 2009;55:1089–103. doi: 10.1016/j.eururo.2009.01.048. [DOI] [PubMed] [Google Scholar]
- 2.Cosson M, Rajabally R, Bogaert E, Querleu D, Crépin G. Laparoscopic sacrocolpopexy, hysterectomy, and burch colposuspension: Feasibility and short-term complications of 77 procedures. JSLS. 2002;6:115–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89:501–6. doi: 10.1016/S0029-7844(97)00058-6. [DOI] [PubMed] [Google Scholar]
- 4.Nezhat CH, Nezhat F, Nezhat C. Laparoscopic sacral colpopexy for vaginal vault prolapse. Obstet Gynecol. 1994;84:885–8. [PubMed] [Google Scholar]
- 5.FDA Safety Communication: UPDATE on Serious Complications Associated with Transvaginal Placement of Surgical Mesh for Pelvic Organ Prolapse. 2011. [[Last accessed on 2019 Dec 30]]. Available from: http://wayback.archive-it.org/7993/20170722150848/https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm262435.htm . [DOI] [PubMed]
- 6.Sutton GP, Addison WA, Livengood CH 3rd, Hammond CB. Life-threatening hemorrhage complicating sacral colpopexy. Am J Obstet Gynecol. 1981;140:836–7. doi: 10.1016/0002-9378(81)90750-x. [DOI] [PubMed] [Google Scholar]
- 7.Cundiff GW, Harris RL, Coates KW, Bump RC. Clinical predictors of urinary incontinence in women 11. Am J Obstet Gynecol. 1997;177:262–7. doi: 10.1016/s0002-9378(97)70185-6. [DOI] [PubMed] [Google Scholar]
- 8.Albanesi G, Giannini A, Carbone M, Russo E, Mannella P, Ferrari V, et al. Computed-tomography image segmentation and 3D-reconstruction of the female pelvis for the preoperative planning of sacrocolpopexy: Preliminary data. Int Urogynecol J. 2019;30:725–31. doi: 10.1007/s00192-018-3706-3. [DOI] [PubMed] [Google Scholar]
- 9.DeLancey JO. Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol. 1992;166:1717–24. doi: 10.1016/0002-9378(92)91562-o. [DOI] [PubMed] [Google Scholar]
- 10.Ginath S, Garely AD, Condrea A, Vardy MD. Mesh erosion following abdominal sacral colpopexy in the absence and presence of the cervical stump. Int Urogynecol J. 2013;24:113–8. doi: 10.1007/s00192-012-1845-5. [DOI] [PubMed] [Google Scholar]
- 11.Tan-Kim J, Menefee SA, Luber KM, Nager CW, Lukacz ES. Prevalence and risk factors for mesh erosion after laparoscopic-assisted sacrocolpopexy. Int Urogynecol J. 2011;22:205–12. doi: 10.1007/s00192-010-1265-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


