Abstract
Background:
Duration and number of power outages have increased over time, partly fueled by climate change, putting users of electricity-dependent durable medical equipment (hereafter, “durable medical equipment”) at particular risk of adverse health outcomes. Given health disparities in the United States, we assessed trends in durable medical equipment rental prevalence and individual- and area-level sociodemographic inequalities.
Methods:
Using Kaiser Permanente South California (KPSC) electronic health record data, we identified durable medical equipment renters. We calculated annual prevalence of equipment rental and fit hierarchical generalized linear models with ZIP code random intercepts, stratified by rental of breast pumps or other equipment.
Results:
243,559 KPSC members rented durable medical equipment between 2008–2018. Rental prevalence increased over time across age, sex, racial–ethnic, and Medicaid categories, most by >100%. In adjusted analyses, Medicaid use was associated with increased prevalence and 108 (95% CI: 99, 117) additional days of equipment rental during the study period. ZIP code-level sociodemographics were associated with increased prevalence of equipment rentals, for example, a one standard-deviation increase in percent unemployed and < high school diploma (prevalence ratio [PR] = 1.1, 95% CI: 1.1, 1.1; and PR = 1.1, 95% CI: 1.1, 1.2, respectively). Increased Supplemental Nutrition Assistance Program usage was associated with decreased breast pump rentals (PR = 0.83, 95% CI: 0.78, 0.88).
Conclusions:
We observed some socioeconomic disparities among a growing electricity-dependent population. Our findings are consistent with the hypothesis that reliable electricity access is increasingly required to meet the health needs of medically disadvantaged groups.
Keywords: Durable Medical Equipment, Electronic Health Records, Socioeconomic Factors, Vulnerable Populations, Medicaid
INTRODUCTION
Major power outages increased 10-fold between 1984–2012 and the average U.S. household experienced 470 minutes without power in 2017.1,2 Major events, like winter storms, hurricanes, heatwaves, and wildfires, projected to intensify with climate change,3 accounted for virtually the entire increase. In addition to severe weather, power outages can be a result of Public Safety Power Shutoffs (PSPS), utility-conducted power shutoffs during times of heightened wildfire risks. In October 2019, over 2 million electric customer accounts in California lost power due to PSPS events.4 Beyond lights and appliances, these shutoffs cut power to electricity-dependent durable medical equipment (hereafter, “durable medical equipment”). Durable medical equipment encompasses at-home medical devices such as oxygen delivery systems, infusion pumps, ventilators, and dialysis machines. Today, at least 2.5 million people in the United States rely on durable medical equipment.5 During outages, these individuals may face life-threatening situations.6–8 Few studies, however, have characterized the durable medical equipment population by age, sex, race–ethnicity, type of durable medical equipment, or socioeconomic status (SES) despite their vulnerability during power outages due to reliance on electricity to manage their health.9
The U.S. Department of Health and Human Service (HHS) emPOWER map reported a nationwide prevalence of 45.84 durable medical equipment users per 1,000 Medicare beneficiaries in April 2020.5 Individuals of all ages and disability statuses, however, use durable medical equipment. After the 2011 Japanese tsunami, where blackout durations averaged 8 days, 75% of pediatric patients admitted to a local hospital were electricity-dependent.10 During the 2003 New York City Blackout, Montefiore Medical Center received 26 adults and 11 children respiratory care device users.11 While those reliant on respiratory durable medical equipment are the most vulnerable and well-characterized, other types of durable medical equipment users may face significant stress and disruption to activities of daily living during a power outage, even if their device provides back-up battery power. Profiles of these other groups, including users of electric wheelchairs, beds, and breast pumps do not exist. Breast pump users are an unstudied and unique group of generally healthy women of childbearing age that may require hospital-grade electric breast pumps to express breast milk for premature or sick infants.
Households dependent on electricity for medical devices require more than food, water, and supplies during power outages. Unfortunately, a minority of durable medical equipment users have specific disaster plans, and preparedness may decline as physical disability increases.12 One study reported only 25% of durable medical equipment users had an alternative power supply.13 Disparities may also exist in power outage duration. In Florida, power outages lasted longer in rural areas and in communities with higher percentages of Hispanic, unemployed, and disabled populations.14 These inequalities in provision of energy services threaten energy justice, which includes as a tenet provision of reliable energy services as a basic social good.15 Further, in addition to possible unequal allocation of energy services, racial–ethnic and socioeconomic disparities in health outcomes that may require durable medical equipment –e.g., chronic obstructive pulmonary disease and cardiovascular disease–persist in the U.S.16,17 In New York, 57% of poorer respondents, those with an annual household income <$50,000, reported a household member using durable medical equipment, compared to 36% overall.18
Here, we use electronic health record (EHR) data from a large healthcare system in California from 2008–2018 to provide sociodemographic profiles of individuals relying on durable medical equipment. We also assess potential disparities in durable medical equipment use and sociodemographic factors that may increase vulnerability of durable medical equipment users to power outages. Such data are required to adequately serve the medically-vulnerable and advance energy justice goals in support of health19 as power outage frequency and duration increases.
METHODS
We conducted an observational cohort study among members of Kaiser Permanente Southern California (KPSC), an integrated healthcare organization that serves >4.7 million individuals in Southern California. The integrated healthcare model means patients enroll as KPSC members, pay monthly premiums, and their health plan, the hospitals, and medical groups are integrated with the assistance of the EHR. Physicians receive salaries rather than fee-for-service payments. KPSC patients represent the underlying population in the region, except for slight under-representation of individuals living in the highest and lowest SES communities.20 KPSC EHRs store member health information including demographics, encounters, procedures, and equipment rentals. Clinicians place orders for durable medical equipment through HealthConnect, a secure communication network. The durable medical equipment office handles rentals by connecting with the appropriate contract provider depending on requested equipment. The KPSC and Columbia University Institutional Review Boards approved this study.
Sample
The study population included KPSC members of all ages between 2008–2018, among whom we identified individuals who rented durable medical equipment each year (eFigure 1). We focused on durable medical equipment rentals alone, and not purchases, because EHR data provides start and stop rental dates and because renters are likely a more vulnerable, lower SES population. We identified members renting durable medical equipment using Centers for Medicare & Medicaid Services Healthcare Common Procedure Coding System codes (eTable 1). Durable medical equipment categories included Bilevel Positive Airway Pressure (BiPAP) machines, oxygen equipment, ventilators, enteral feeding machines, infusion pumps, suction pumps, hospital beds, wheelchairs, and breast pumps.21 KPSC EHR data included member sex, age, race–ethnicity, insurance type, annual ZIP code of residence, and durable medical equipment rental type. Clinicians usually record member sex in the EHR based on member self-report and sex likely matched natal sex for the majority of members, although it may represent gender identity for a sub-population.22 We refer to this variable as sex. We categorized insurance as Medicaid, Medicare, dual-Medicaid/Medicare, and other- or self-pay based, with Medicaid use as a surrogate for low SES.23 We calculated each member’s total durable medical equipment rental duration and whether they rented two or more categories of durable medical equipment in a single year between 2008–2018.
SES measures
We downloaded Zip Code Tabulation Area (ZCTA) level sociodemographic variables from the 2010 US census and the 2006–2010 American Community Survey,24 mapped ZCTAs to US Postal ZIP codes, and linked data based on member ZIP code. We created percentages of the following variables by ZIP code: < high school education, living below the federal poverty threshold, Supplemental Nutrition Assistance Program (SNAP) use, linguistically isolated, unemployed, renting, rural, ≥ 65 years, and racial–ethnic categories (non-Hispanic Asian, Black, and White, and Hispanic). We also included median household income. We standardized all sociodemographic variables by dividing them by their standard deviation, except for race–ethnicity, which we scaled so beta coefficients corresponded to a 10% change in racial–ethnic group makeup.
Statistical analysis
We calculated annual prevalence of durable medical equipment rentals between 2008–2018 as the count of KPSC members who rented durable medical equipment divided by the number of active KPSC members, each year. We estimated durable medical equipment rentals per 1,000 persons overall and by sex, age category (0–17, 18–64, ≥65), race–ethnicity (non-Hispanic Asian, Black, White, other, and Hispanic), and Medicaid status. We calculated annual prevalence of breast pump rentals among women aged 15–49. For analyses, we generated two groups: durable medical equipment renters and the subset who rented electric breast pumps, which we refer to as durable medical equipment renters and breast pump renters to reflect varied durable medical equipment use patterns.
We evaluated the association between ZIP code-level characteristics of KPSC members and census sociodemographics and annual prevalence of durable medical equipment rentals, stratified by durable medical equipment and breast pumps rentals. To do so, we fit generalized linear models using a Poisson distribution for the outcome (count of members renting durable medical equipment per ZIP code) with a log-link, random intercept for ZIP code, and log(total KPSC population) per ZIP code as the offset, except for breast pump models, which used log(KPSC women aged 15–49). We evaluated the association between the ZIP code-level sociodemographic variables in 13 separate models (12 for breast pump models because age ≥65 was not included) due to high correlation between variables (eFigure 2). Models were adjusted for year and ZIP code-level KPSC member population characteristics: mean age, percent Medicaid users, percent Hispanic and non-Hispanic Black members, and percent female members (non-breast pump models only).
In an individual-level analysis, we used a model with an identity link function and Gaussian distribution, with a random intercept for ZIP code to assess the association between individual- and area-level factors and cumulative duration of durable medical equipment use between 2008–2018. Again, we ran 13 separate models. All models included member age, sex, race–ethnicity, and Medicaid use, and ZIP code-level median household income. We also used hierarchical logistic regression to evaluate associations between individual- and ZIP code-level variables and rental of two or more categories of durable medical equipment in the same year.
After running models evaluating ZIP code-level predictors of annual prevalence of durable medical equipment rental and duration separately, we used LASSO (Least Absolute Shrinkage and Selection Operator) to select a subset of predictors when including all variables in the same model (eMethods).25 LASSO helps select the most important predictors when exposure variables are correlated.
In two sensitivity analyses, we (1) inspected model residuals for spatial autocorrelation visually and using Moran’s I; and (2) calculated the distance between each ZIP code centroid and the nearest KPSC facility and included this variable in the model. We performed analyses using R Statistical Software version 3.5.1 (R Core Team [2018] https://www.R-project.org/). Analytic code is available on GitHub at https://github.com/joanacasey/dme_kpsc.
RESULTS
Between 2008–2018, 243,559 KPSC members rented electricity-dependent durable medical equipment. Electric breast pumps comprised 40% of these rentals, and other types of durable medical equipment 60% (Table 1). All breast pump renters were females aged 15–49 years, the majority were of Hispanic ethnicity, and nearly 20% used Medicaid as insurance. Other durable medical equipment renters consisted of equal numbers of men and women and the majority were aged ≥65 years and of non-Hispanic White race–ethnicity; only ~10% used Medicaid as insurance (likely due to the older average age). Less than 1% of breast-pump users rented another type of durable medical equipment while >25% of those that rented other durable medical equipment rented two or more categories of durable medical equipment (e.g., a hospital bed and oxygen equipment) during the study period.
Table 1:
Characteristics of 243,559 renters of electric durable medical equipment at Kaiser Permanente Southern California, 2008–2018
| Characteristic | Renters of durable medical equipmenta | Renters of breast pumpsb |
|---|---|---|
| Overall, n (%) | 147,295 (100) | 96,534 (100) |
| Age, years, n (%) | ||
| 0–17 | 4,295 (2.9) | 0 (0) |
| 18–64 | 64,690 (44) | 96,534 (100) |
| 65+ | 78,310 (53) | 0 (0) |
| Sex, n (%) | ||
| Female | 77,034 (523) | 96,534 (100) |
| Male | 70,261 (48) | 0 |
| Race/ethnicity, n (%) | ||
| Non-Hispanic | ||
| Asian | 10,159 (6.9) | 15,187 (16) |
| Black | 18,528 (13) | 7,491 (7.8) |
| White | 8,2415 (56) | 22,414 (23) |
| Otherc | 2,141 (1.5) | 1,276 (1.3) |
| Hispanic | 3,4052 (23) | 50,166 (52) |
| Insurance type, n (%) | ||
| Medicaid | 15,504 (11) | 17,727 (18) |
| Medicare | 107,742 (73) | 190 (0.2) |
| Dual-eligibled | 9,547 (6.5) | 190 (0.2) |
| Private/self-pay/unknown | 33,596 (23) | 77,807 (81) |
| Rental of 2+ durable medical equipment categories during at least one year, n (%) | 38,981 (26.5) | 162 (0.2) |
| Distance to nearest KPSC facility (km), median (IQR) | 3.3 (2.0, 5.4) | 3.1 (1.9, 4.6) |
| Duration of durable medical equipment rental, 2008–2018 (days), median (IQR) | 303 (173, 431) | 206 (106, 297) |
Includes all non-breast pump durable medical equipment rental types: Bilevel Positive Airway Pressure (BiPAP) machines, enteral feeding machines, hospital beds, infusion pumps, oxygen equipment, suction pumps, ventilators, and wheelchairs
270 KPSC members rented a breast pump and other durable medical equipment during the study period and appear in both columns.
Includes other, missing or unknown, or multiple races/ethnicities.
Eligible for both Medicaid and Medicare
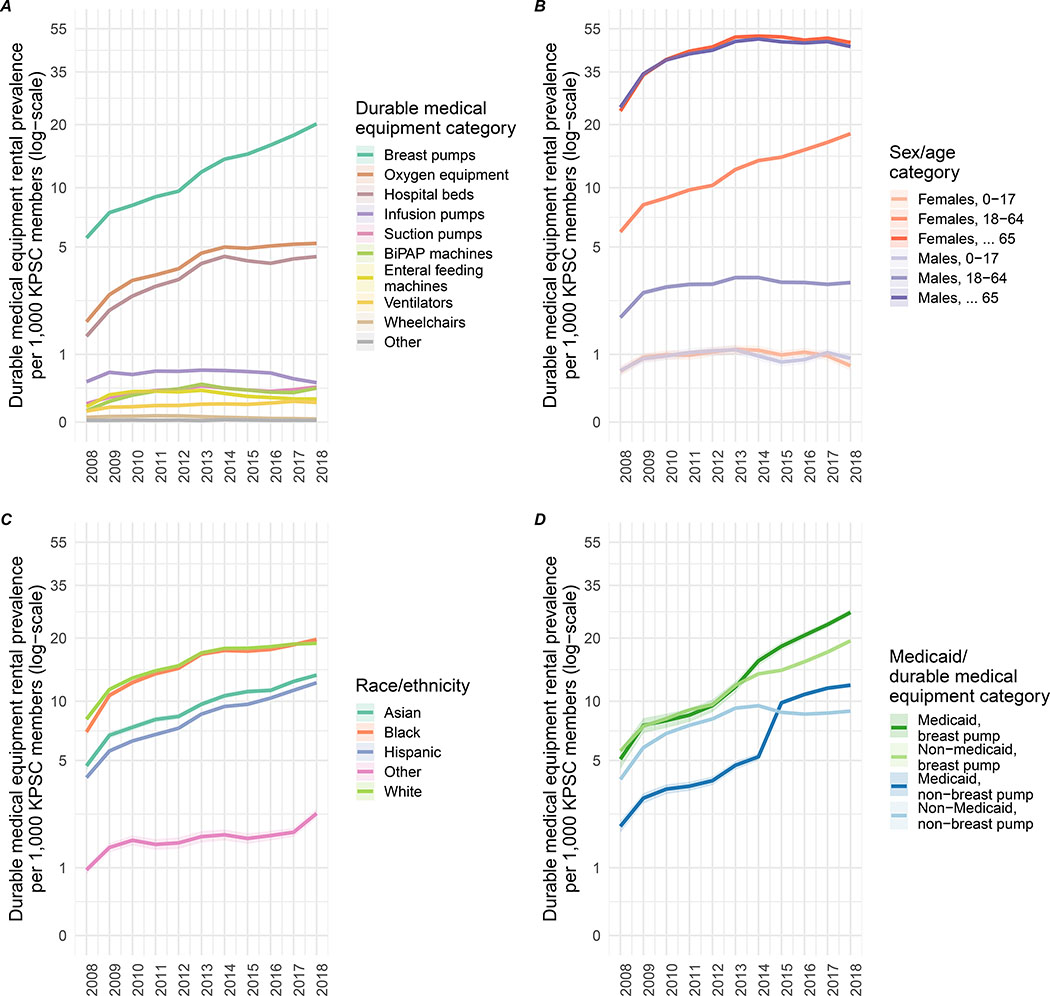
During the 11-year period, annual prevalence of durable medical equipment rentals generally increased. For example, the annual prevalence of oxygen equipment rentals grew from 1.79 (95% CI: 1.75, 1.84) per 1,000 persons in 2008 to 5.22 (95% CI: 5.16, 5.29) per 1,000 persons in 2018, while the annual prevalence of breast pump rentals increased from 5.59 (95% CI: 5.43, 5.74) to 20.16 (95% CI: 19.90, 20.42) per 1,000 persons (Figure 1, eTables 2–3). Those aged ≥65 had the highest prevalence of rentals; 46.8 (95% CI: 46.2, 47.3) per 1,000 persons in 2018. Overall, the annual prevalence of durable medical equipment rental was highest among non-Hispanic Black and non-Hispanic White members, but prevalence among all racial–ethnic groups increased over the study period.
Figure 1: Annual prevalence of electricity-dependent durable medical equipment rental per 1,000 Kaiser Permanente Southern California members, 2008–2018.
A) Durable medical equipment category; B) Sex and age category; C) Race/ethnicity; D) Medicaid status.
Notes. BiPAP, Bilevel Positive Airway Pressure.
We observed a sharp increase in durable medical equipment rental among Medicaid recipients, particularly after 2012 (Figure 1). Between 2012–2015, an additional 8,992 KPSC members aged 18–64 years used Medicaid as insurance and the annual prevalence of durable medical equipment rental in this group increased by 124% (eFigure 3). The annual prevalence of renting two or more durable medical equipment categories increased by 300% between 2008 and 2018; annual prevalence plateaued ~2 per 1,000 persons in 2014 (eFigure 4). Spatially, durable medical equipment rental among the KPSC population has increased across the KPSC catchment area over time, with higher prevalence of rentals clustered in Los Angeles and San Diego for breast pumps, distributed more evenly across the study region for other durable medical equipment types, and more confined to urban areas for those using Medicaid (eFigures 5–6).
KPSC member characteristics were associated with annual prevalence of durable medical equipment rental at the ZIP code-level in adjusted models (Table 2, eFigure 7). A 10-year increase in mean ZIP-code level KPSC member age was associated with an increased prevalence ratio (PR) for durable medical equipment rental but a reduced PR for breast pump rental. For durable medical equipment rental, a 10% increase in ZIP code-level KPSC non-Hispanic White race–ethnicity was associated with a 10% increase in PR. While for breast pump rental, KPSC non-Hispanic Black race–ethnicity was most strongly associated with an increased PR and KPSC non-Hispanic White race–ethnicity was associated with a decreased PR. For both types of durable medical equipment, a 10% increase in the ZIP code-level KPSC member population using Medicaid was associated with increased annual prevalence of durable medical equipment rental.
Table 2:
ZIP code-level prevalence ratio for electric durable medical equipment rentals by Kaiser Permanente Southern California member sociodemographics, 2008–2018
| Durable medical equipmenta | Breast pump | |
|---|---|---|
| Variable | PR (95% CI)b | PR (95% CI)c |
| KPSC member characteristicsd | ||
| Age | 1.8 (1.7, 1.9) | 0.84 (0.75, 0.93) |
| Sex | 1.1 (1.0, 1.2) | Not estimated |
| Race/ethnicity | ||
| Non-Hispanic | ||
| Asian | 1.0 (1.0, 1.0) | 1.0 (1.0, 1.1) |
| Black | 1.0 (1.0, 1.0) | 1.1 (1.1, 1.2) |
| White | 1.1 (1.1, 1.1) | 0.76 (0.71, 0.82) |
| Other | 1.0 (1.0, 1.0) | 1.0 (1.0, 1.0) |
| Hispanic | 0.96 (0.94, 0.98) | 1.0 (1.0, 1.0) |
| Medicaid | 1.2 (1.2, 1.3) | 1.2 (1.1, 1.3) |
Notes. KPSC, Kaiser Permanente Southern California; PR, prevalence ratio
Includes all non-breast pump durable medical equipment rental types: Bilevel Positive Airway Pressure (BiPAP) machines, enteral feeding machines, hospital beds, infusion pumps, oxygen equipment, suction pumps, ventilators, and wheelchairs.
Generalized hierarchical Poisson model with a random intercept for ZIP code, adjusted for year, ZIP code-level median household income, and descriptors of the ZIP code-level KPSC member population: mean age, percent Medicaid users, percent Hispanic members, percent non-Hispanic Black members, and percent female members.
Generalized hierarchical Poisson model with a random intercept for ZIP code, adjusted for year ZIP code-level median household income, and descriptors of the ZIP code-level KPSC member population: mean age, percent Medicaid users, percent Hispanic members and percent non-Hispanic Black members.
PR per 10-year increase in ZIP code-level average KPSC membership age or 10% increase in other KPSC member population characteristics.
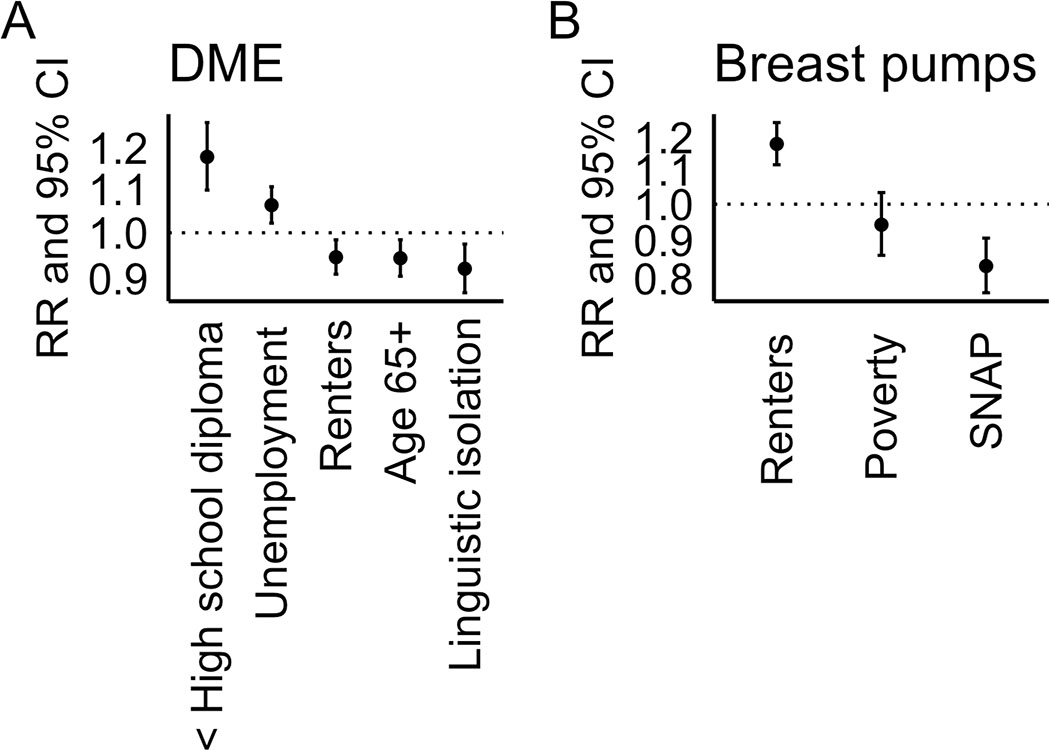
ZIP code-level factors were associated with annual prevalence of both durable medical equipment and breast pump rentals. Our LASSO model suggested that for durable medical equipment rental, a one standard-deviation increase in percent unemployed and < high school diploma (PR = 1.1, 95% CI: 1.1, 1.1; and PR = 1.1, 95% CI: 1.1, 1.2, respectively), while higher linguistic isolation and proportion of individuals ≥65 years were associated with reduced prevalence of rentals (Figure 2A). For breast pumps, increased percent renters and lower percent SNAP users were associated with increased prevalence of rentals (PR = 1.1, 95% CI: 1.1, 1.2 and PR = 0.83, 95% CI: 0.78, 0.88, respectively, Figure 2B). Models where each ZIP code-level sociodemographic factor was entered separately generally agreed with the LASSO results (eFigures 8–9, eTable 6).
Figure 2: ZIP code-level prevalence ratio for durable medical equipment and breast pump rentals at Kaiser Permanente Southern California, 2008–2018 by ZIP code-level socioeconomic factors.
A) durable medical equipment (DME); B) Breast pumps.
All SES variables were modeled jointly, and a subset of important predictors selected using LASSO (see eMethods). Models were adjusted for year and descriptors of the ZIP code-level KPSC member population: mean age, percent Medicaid users, percent Hispanic members, percent non-Hispanic Black members, and percent female members (DME models only).
a Includes all non-breast pump durable medical equipment rental types: Bilevel Positive Airway Pressure (BiPAP) machines, enteral feeding machines, hospital beds, infusion pumps, oxygen equipment, suction pumps, ventilators, and wheelchairs.
ZIP code-level racial–ethnic composition was also associated with annual prevalence of durable medical equipment rentals (eTable 6). For example, a 10% increase in Black or Hispanic race–ethnicity was associated with increased prevalence of durable medical equipment rentals (PR = 1.19, 95% CI: 1.12, 1.26), but not breast-pump rentals (PR = 0.94, 95% CI: 0.85, 1.04). Only Asian race–ethnicity was associated with an increase in breast-pump rentals (PR = 1.16, 95% CI: 1.12, 1.20).
On average, KPSC members rented breast pumps for 206 days during the 11-year study period and other durable medical equipment for 303 days. In adjusted models, Medicaid as insurance was associated with 108 (95% confidence interval [CI]: 99, 117) additional days of durable medical equipment rental and 6 (95% CI: 4, 9) additional days of breast-pump rental between 2008–2018 (Table 3, eFigure 10). Being a dual Medicaid/Medicare beneficiary was associated with even longer rental duration, 125 days (95% CI: 114, 136) for durable medical equipment and 39 days (95% CI: 15, 64) for breast pumps. Non-Hispanic White and Black members rented durable medical equipment longer than other race–ethnicities. Generally, individual-level factors were not associated with breast pump rental duration.
Table 3:
Change in cumulative duration of durable medical equipment rental in days by Kaiser Permanente Southern California member characteristics, 2008–2018
| Category | ||
|---|---|---|
| Durable medical equipmenta | Breast pump | |
| Variable | β (95% CI)b | β (95% CI)c |
| Age (per additional year) | 11 (9, 12) | 9 (8, 11) |
| Female sex | 31 (25, 36) | N/A |
| Medicaid | 108 (99, 117) | 6 (4, 9) |
| Dual-eligible for Medicaid and Medicare | 125 (114, 136) | 39 (15, 64) |
| Race/ethnicity | ||
| Non-Hispanic | ||
| Asian | −60 (−72, −49) | −1 (−4, 2) |
| Black | 12 (2, 22) | −4 (−8, 0) |
| White | REF | REF |
| Other | −78 (−101, −55) | 0 (−8, 8) |
| Hispanic | −56 (−64, −49) | −2 (−4, 1) |
Includes all non-breast pump durable medical equipment rental types: Bilevel Positive Airway Pressure (BiPAP) machines, enteral feeding machines, hospital beds, infusion pumps, oxygen equipment, suction pumps, ventilators, and wheelchairs.
Generalized hierarchical linear model with a random intercept for ZIP code. Adjusted for KPSC member age, sex, race/ethnicity, Medicaid status, and ZIP code-level median household income.
Generalized hierarchical linear model with a random intercept for ZIP code. Adjusted for KPSC member age, race/ethnicity, Medicaid status, and ZIP code-level median household income.
ZIP code-level factors were not predictive of cumulative durable medical equipment rental duration (eFigures 11–12). The LASSO model only retained ZIP code-level unemployment as a relevant predictor of durable medical equipment rental duration (β = 31 days, 95% CI: 26, 36 per 4.6% increase in unemployment); no variables were retained in the breast pump model.
In a secondary analysis, we found that the PR of renting two or more durable medical equipment categories increased with age (PR = 1.38, 95% CI: 1.36, 1.39 per 10-year increase), male sex (PR = 0.84, 95% CI: 0.82, 0.86 for females), Medicaid use (PR = 1.30, 95% CI: 1.24, 1.35), and Non-Hispanic Asian (PR = 1.37, 95% CI: 1.30, 1.44), Black (PR = 1.22, 95% CI: 1.17, 1.28), and Hispanic (PR = 1.34, 95% CI: 1.29, 1.38) race–ethnicity (eTable 7). The LASSO model only retained ZIP code-level % with less than high school education as predictive of renting two or more durable medical equipment categories (PR = 1.04, 95% CI: 1.02, 1.07).
Visual inspection of model residuals and Moran’s I both indicated our models appropriately accounted for spatial autocorrelation (eFigure 13). Including distance to the nearest KPSC healthcare facility in models changed effect estimates by <1% (data not shown).
DISCUSSION
Between 2008–2018 in a large, integrated healthcare system in California, we found increases in annual prevalence of durable medical equipment rental across age, sex, race–ethnicity, and Medicaid categories. The increased annual prevalence was particularly dramatic between 2012–2015 for members using Medicaid, and Medicaid use was associated with increased durable medical equipment rentals and durations in adjusted analyses. We also found that while lower ZIP code-level educational attainment and unemployment were associated with increased annual prevalence of durable medical equipment rental, linguistic isolation was associated with decreased prevalence, potentially indicating unmet need. Likewise, increased ZIP code-level use of SNAP was associated with lower prevalence of breast pump rentals. Increased ZIP code-level non-Hispanic race–ethnicity was associated with decreased prevalence of rentals, possibly reflecting purchase, rather than rental of durable medical equipment. Our results are consistent with increased demand for at-home medical care in an aging population, Medicaid expansion to cover durable medical equipment, and potential disparities in durable medical equipment provision.
The Affordable Care Act (ACA) expanded Medicaid eligibility to most low-income adults in an effort to address systemic health inequalities in the U.S. The Medicaid population has greater morbidity in general23 and the ACA increased at-home durable medical equipment use, recognizing the preference of Americans with functional needs to remain in communities and including provisions to support individuals at home.26 Many states, including California, elected to also cover durable medical equipment as an optional service under Medicaid. From December 2012–2014, California’s Medicaid enrollment increased by 60%, from 7.6 million to 12 million individuals.27 Our data reflect this surge as the KPSC Medicaid population aged 18–64 increased by 67% between 2012–2014. These members gained access to durable medical equipment; prevalence increased by >100% during the same time period. We also observed rapid increases in electric breast pump rental that mirrored the 7.5% annual growth in the worldwide breast pump market from 2012–2018.28 We note, however, that durable medical equipment use in our sample was increasing prior to the ACA expansion including for the non-Medicaid population (Figure 1). Our data are limited such that we lack geographic variation in the ACA rollout. As such, we are unable to robustly estimate the impact of the ACA expansion on durable medical equipment use. However, this is an important topic for future research.
We observed the highest annual prevalence of durable medical equipment rental among KPSC members aged ≥65 years. However, despite higher average KPSC member age being associated with increased durable medical equipment rentals, higher ZIP code-level percentages of adults aged ≥65 overall were associated with reduced prevalence, consistent with scholarship finding <50% of chronically disabled elderly individuals have received Medicare-reimbursed durable medical equipment.29 While some studies suggest that after disasters, older adults, particularly those living with chronic conditions that require durable medical equipment, face elevated risk of adverse health outcomes,30 a recent review found little evidence of such increased risk.31
Despite persistent racial–ethnic and socioeconomic health disparities in the U.S. that could make certain sub-populations require more durable medical equipment,17 we know of no studies that have characterized individual or area-level sociodemographics in the population of durable medical equipment renters. We found Medicaid use associated with higher prevalence and longer duration of durable medical equipment rental, consistent with a higher prevalence of chronic conditions among the Medicaid population32 and greater durable medical equipment needs among children on Medicaid/Children’s Health Insurance Program (CHIP) compared to those on private insurance.33 From a clinical standpoint, the increased prevalence of durable medical equipment rental among low SES KPSC members likely represent met need but also makes this group vulnerable during power outages. After Hurricane Sandy and subsequent outages, hospitals reported dramatic increases in emergency department patients seeking care for respiratory device failure.30,34 Low SES individuals may be particularly vulnerable because standby generators cost $2,000–5,000, limiting access to backup power for medical devices during outages.
Other measures of SES, ZIP code-level unemployment and lower educational attainment, were related to increased prevalence of durable medical equipment rentals in the KPSC population. ZIP code-level unemployment was associated with longer duration durable medical equipment rental, suggesting a bidirectional relationship where unemployed individuals require and rent more durable medical equipment. Conversely, we observed decreased prevalence of durable medical equipment rentals in ZIP codes with higher levels of SNAP use and linguistic isolation, potentially reflecting less access to medically important devices. We found a 17% reduction in the prevalence of breast pump rental associated with a standard deviation increase in ZIP code-level SNAP use. This relationship could also reflect the known lower breastfeeding rates among lower SES women in the US.35 With respect to linguistic isolation, previous studies have reported lower levels of healthcare access and preventive (e.g., flu shot) and psychiatric care services when comparing Spanish-speaking to English-speaking Hispanics.36,37 Further, linguistic isolation may inhibit disaster preparedness due to lack of bilingual emergency messages or financial resources to prepare.38 A 2016 survey of 887 New Yorkers found 58% prepared for a disaster, and those that took the survey in Spanish had the lowest preparedness (29%).18
Regarding racial–ethnic differences, we found higher percentages of non-Hispanic White KPSC members associated with higher ZIP code-level annual prevalence of durable medical equipment rentals, and no difference in prevalence by other racial–ethnic groups. For breast pump rental, we observed the opposite, lower annual prevalence of rental in ZIP codes with a higher percentage of non-Hispanic White KPSC members. This may reflect purchase of electric breast pumps by these groups rather than reduced use. Above and beyond the KPSC population composition, ZIP code-level Hispanic and Black race–ethnicity were associated with increased annual prevalence of durable medical equipment rental. Prior studies indicate lower disaster preparedness among lower income, Black, and Hispanic individuals;19 Cox et al. found that low-income older Black participants in the Health and Retirement Study were the least prepared of all groups surveyed.39 This, coupled with Black and Hispanic respondents reporting the greatest concerns about health during power outages18 suggests that racial–ethnic and socioeconomic differences in annual prevalence of durable medical equipment rental may translate into worse health outcomes during future power outages.
Electric utilities often encourage durable medical equipment users to register for priority in terms of evacuation, sheltering, power restoration, or early alerts of planned outages. Southern California Edison, which serves a large segment of the KPSC population, provides power outage alerts and offers additional electricity to durable medical equipment users at a lower baseline rate, but leaves healthcare providers to develop disaster plans. Utility and public health registries, however, may go unused. Only 40% of electricity-dependent households in New York surveyed in 2016 had registered to receive early notification of outages from utilities.18 In New Orleans, 611 Medicare beneficiaries were identified as relying on at-home respiratory durable medical equipment but only 15 (2.5%) had enrolled in the city’s special medical need registry.40
An alternative power supply, such as a gas or diesel generator, can help individuals shelter in-place during an outage, but can cause carbon monoxide poisoning,8,18 be difficult to operate and refuel (especially for those with mobility impairments), and require substantial capital inputs. Clean energy technologies–battery storage, ideally paired with onsite solar generation–can provide reliable backup power without harmful emissions, fuel supply concerns, or operating difficulties, but also come with high upfront costs (a battery may cost >$6,500). Such costs can exacerbate existing disparities in backup power access. One study found non-Hispanic White respondents 2.5x as likely to own a generator as other racial–ethnic groups.41 Lower SES individuals suffer from energy insecurity.42,43 In California, 36% of low-income households surveyed reported cutting back on buying food to pay utility bills.44 These disparities in energy access and backup power further highlight the vulnerability of low SES individuals, who in our study had higher prevalence of rented durable medical equipment than higher SES individuals.
Two prior data points provide estimates of durable medical equipment use in California. Commercial outpatient claims from large employers found a prevalence of at-home ventilator or oxygen concentrator use of 1.02 (95% CI: 0.97, 1.07) per 1,000 covered lives in Los Angeles in 2012 45, this compares to 3.80 (95%: 3.74, 3.86) per 1,000 KPSC members in 2012. Second, the HHS emPOWER map reported an average prevalence of durable medical equipment use among KPSC ZIP codes as 33.1 per 1,000 Medicare beneficiaries in the fall of 2019 (earliest date for which we have data), similar to the KPSC prevalence of 43.3 per 1,000 persons among adults aged ≥65 in 2018 (eFigure 14). emPOWER can assist in identifying Medicare durable medical equipment user locations in disaster-scenarios,40 but lacks information on non-Medicare beneficiaries who accounted for 27% of durable medical equipment renters and nearly 100% of breast pump renters at KPSC. emPOWER does not track breast pump rentals.
This study had limitations. We evaluated only durable medical equipment rentals, not total durable medical equipment use, which would include purchased equipment. Further, we could not assess unmet need among KPSC members, those that could have benefited from durable medical equipment rentals but did not obtain them. The majority of SES variables were measured at the ZIP code-level, rather than individual-level, precluding us from answering questions related to, for example, individual-level unemployment and durable medical equipment rental.
Because irregular power supply makes durable medical equipment users vulnerable to medical emergencies, future work should focus on evaluating their healthcare needs and outcomes.
Our present analysis identified increased annual prevalence and longer duration of durable medical equipment rental among Medicaid recipients as well as area-level sociodemographic factors associated with increased annual prevalence of durable medical equipment rental. These findings suggest that energy access is increasingly critical in meeting the health needs of medically disadvantaged groups. Annual prevalence of durable medical equipment rental also increased rapidly between 2008–2018 across all groups, including previously uncharacterized breast pump users. Descriptive studies such as ours can help identify trends and potentially vulnerable sub-groups of durable medical equipment renters, information useful for healthcare providers and disaster preparedness officials.
Supplementary Material
Acknowledgments:
We thank KPSC members for their contribution to this study through use of their electronic health record data.
Sources of funding: This study was funded, in part, by the Robert Wood Johnson Foundation and an R00ES027023 award to JAC from the National Institutes of Environmental Health Sciences.
Footnotes
Conflicts of interest: Marriele Mango and Seth Mullendore are employees of Clean Energy Group.
Data availability: Due to patient confidentiality, the data used in this study are not publicly available. R code is available on GitHub at https://github.com/joanacasey/dme_kpsc.
REFERENCES
- 1.U.S. Energy Information Administration. Average U.S. electricity customer interruptions totaled nearly 8 hours in 2017. https://www.eia.gov/todayinenergy/detail.php?id=37652 Accessed 4 June 2019.
- 2.Kenward A, Raja U. Blackout: Extreme weather, climate change, and power outages. In: Central C, ed. Princeton, NJ, 2014. [Google Scholar]
- 3.Auffhammer M, Baylis P, Hausman CH. Climate change is projected to have severe impacts on the frequency and intensity of peak electricity demand across the United States. Proc Natl Acad Sci U S A 2017;114(8):1886–1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.California Public Utilities Commission. Public Report on the Late 2019 Public Safety Power Shutoff Events. https://www.cpuc.ca.gov/uploadedFiles/CPUCWebsite/Content/News_Room/NewsUpdates/2020/SED%20Public%20Report%20On%20The%20Late%202019%20PSPS%20Events.pdf Accessed 25 Sept 2020.
- 5.United States Department of Health and Human Services (US DHHS). HHS emPOWER Map 3.0. https://empowermap.hhs.gov/ Accessed 05 June 2019.
- 6.Rubin GJ, Rogers MB. Behavioural and psychological responses of the public during a major power outage: A literature review. Int J Disaster Risk Reduct 2019:101226. [Google Scholar]
- 7.Greenwald PW, Rutherford AF, Green RA, Giglio J. Emergency department visits for home medical device failure during the 2003 North America blackout. Acad Emerg Med 2004;11(7):786–9. [DOI] [PubMed] [Google Scholar]
- 8.Geehr EC, Salluzzo R, Bosco S, Braaten J, Wahl T, Wallenkampf V. Emergency health impact of a severe storm. Am J Emerg Med 1989;7(6):598–604. [DOI] [PubMed] [Google Scholar]
- 9.U.S. Department of Homeland Security and the Federal Emergency Management Agency. Power Outage Incident Annex to the Response and Recovery Federal Interagency Operational Plans: Managing the Cascading Impacts from a Long-Term Power Outage. https://www.fema.gov/media-library-data/1512398599047-7565406438d0820111177a9a2d4ee3c6/POIA_Final_7-2017v2_(Compliant_pda)_508.pdf Accessed 21 Apr 2020.
- 10.Nakayama T, Tanaka S, Uematsu M, Kikuchi A, Hino-Fukuyo N, Morimoto T, Sakamoto O, Tsuchiya S, Kure S. Effect of a blackout in pediatric patients with home medical devices during the 2011 Eastern Japan earthquake. Brain Dev 2014;36(2):143–7. [DOI] [PubMed] [Google Scholar]
- 11.Prezant DJ, Clair J, Belyaev S, Alleyne D, Banauch GI, Davitt M, Vandervoorts K, Kelly KJ, Currie B, Kalkut G. Effects of the August 2003 blackout on the New York City healthcare delivery system: a lesson for disaster preparedness. Crit Care Med 2005;33(1 Suppl):S96–101. [DOI] [PubMed] [Google Scholar]
- 12.Al-Rousan TM, Rubenstein LM, Wallace RB. Preparedness for natural disasters among older US adults: a nationwide survey. Am J Public Health 2014;104(3):506–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.University of Michigan Institute for Healthcare Policy & Innovation. After the storm: The health impacts of weather and climate-related disasters on older adults in the U.S. https://ihpi.umich.edu/news/ihpi-briefs/disasters Accessed 15 May 2020.
- 14.Mitsova D, Esnard A-M, Sapat A, Lai BS. Socioeconomic vulnerability and electric power restoration timelines in Florida: the case of Hurricane Irma. Natural Hazards 2018;94(2):689–709. [Google Scholar]
- 15.Sovacool BK, Jones BR, Sidortsov RV. Energy Security, Equality and Justice. Abingdon, Oxon: Routledge, 2014. [Google Scholar]
- 16.Adler NE, Rehkopf DH. U.S. disparities in health: descriptions, causes, and mechanisms. Annu Rev Public Health 2008;29:235–52. [DOI] [PubMed] [Google Scholar]
- 17.Singh GK, Daus GP, Allender M, Ramey CT, Martin EK, Perry C, Reyes AAL, Vedamuthu IP. Social Determinants of Health in the United States: Addressing Major Health Inequality Trends for the Nation, 1935–2016. Int J MCH AIDS 2017;6(2):139–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dominianni C, Ahmed M, Johnson S, Blum M, Ito K, Lane K. Power outage preparedness and concern among vulnerable New York City residents. J Urban Health 2018;95(5):716–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hernandez D Sacrifice along the energy continuum: A call for energy justice. Environ Justice 2015;8(4):151–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Koebnick C, Langer-Gould AM, Gould MK, Chao CR, Iyer RL, Smith N, Chen W, Jacobsen SJ. Sociodemographic characteristics of members of a large, integrated health care system: comparison with US Census Bureau data. Perm J 2012;16(3):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.United States Department of Health and Human Services (US DHHS). Executive Summary: Shaping Decisions to Protect Health in an Emergency. 2019.
- 22.Quinn VP, Nash R, Hunkeler E, Contreras R, Cromwell L, Becerra-Culqui TA, Getahun D, Giammattei S, Lash TL, Millman A, Robinson B, Roblin D, Silverberg MJ, Slovis J, Tangpricha V, Tolsma D, Valentine C, Ward K, Winter S, Goodman M. Cohort profile: Study of Transition, Outcomes and Gender (STRONG) to assess health status of transgender people. BMJ Open 2017;7(12):e018121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Casey JA, Pollak J, Glymour MM, Mayeda ER, Hirsch AG, Schwartz BS. Measures of SES for electronic health record-based research. Am J Prev Med 2018;54(3):430–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Manson S, Schroeder J, Riper DV, Ruggles S. IPUMS National Historical Geographic Information System: Version 13.0 [Database]. 10.18128/D050.V12.0 Accessed 10 Oct 2019. [DOI]
- 25.Tibshirani R Regression shrinkage and selection via the lasso: a retrospective. J R Stat Soc Series B Stat Methodol 2011;73(3):273–282. [Google Scholar]
- 26.Jan S, Lurie N. Disaster resilience and people with functional needs. N Engl J Med 2012;367(24):2272–3. [DOI] [PubMed] [Google Scholar]
- 27.Department of Health Care Services (DHCS) Research and Analytic Studies Division (RASD). Medi-Cal’s Historic Period of Growth: A 24-Month Examination of How the Program has Changed since December 2012. https://www.dhcs.ca.gov/dataandstats/statistics/Documents/Historic-Growth-Brief.pdf Accessed 22 Apr 2020.
- 28.Research and Markets Offers. 2013. Report on the International Breast Pumps Market - Industry Analysis, Size, Share, Growth, Trends and Forecast to 2018, Business Insights: Essentials. https://www.researchandmarkets.com/research/txjdmk/breast_pumps Accessed 22 Apr 2020.
- 29.Iwashyna TJ, Christie JD. Low use of durable medical equipment by chronically disabled elderly. J Pain Symptom Manage 2007;33(3):324–30. [DOI] [PubMed] [Google Scholar]
- 30.Gotanda H, Fogel J, Husk G, Levine JM, Peterson M, Baumlin K, Habboushe J. Hurricane Sandy: Impact on emergency department and hospital utilization by older adults in Lower Manhattan, New York (USA). Prehosp Disaster Med 2015;30(5):496–502. [DOI] [PubMed] [Google Scholar]
- 31.Bell SA, Horowitz J, Iwashyna TJ. Health Outcomes After Disaster for Older Adults With Chronic Disease: A Systematic Review. The Gerontologist 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Machlin S, D W. Healthcare expenses for chronic conditions among non-elderly adults: variations by insurance coverage, 2005–06 (average annual estimates). Statistical brief no. 243. http://meps.ahrq.gov/mepsweb/data_files/publications/st243/stat243.pdf Accessed 8 May 2020. [Google Scholar]
- 33.Musumeci M, Poindexter D. Medicaid Restructuring and Children with Special Health Care Needs. https://collections.nlm.nih.gov/master/borndig/101717011/Issue-Brief-Medicaid-Restructuring-and-Children-with-Special-Health-Care-Needs.pdf Accessed 8 May 2020.
- 34.Greenstein J, Chacko J, Ardolic B, Berwald N. Impact of Hurricane Sandy on the Staten Island University Hospital Emergency Department. Prehosp Disaster Med 2016;31(3):335–9. [DOI] [PubMed] [Google Scholar]
- 35.Singh GK, Kogan MD, Dee DL. Nativity/immigrant status, race—ethnicity, and socioeconomic determinants of breastfeeding initiation and duration in the United States, 2003. Pediatrics 2007;119 Suppl 1:S38–46. [DOI] [PubMed] [Google Scholar]
- 36.DuBard CA, Gizlice Z. Language spoken and differences in health status, access to care, and receipt of preventive services among US Hispanics. Am J Public Health 2008;98(11):2021–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim G, Aguado Loi CX, Chiriboga DA, Jang Y, Parmelee P, Allen RS. Limited English proficiency as a barrier to mental health service use: A study of Latino and Asian immigrants with psychiatric disorders. Journal of Psychiatric Research 2011;45(1):104–110. [DOI] [PubMed] [Google Scholar]
- 38.Mendez M, Flores-Haro G, Zucker L. The (in)visible victims of disaster: Understanding the vulnerability of undocumented Latino/a and indigenous immigrants. Geoforum 2020;116:50–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cox K, Kim B. Race and income disparities in disaster preparedness in old age. J Gerontol Soc Work 2018;61(7):719–734. [DOI] [PubMed] [Google Scholar]
- 40.DeSalvo K, Lurie N, Finne K, Worrall C, Bogdanov A, Dinkler A, Babcock S, Kelman J. Using Medicare data to identify individuals who are electricity dependent to improve disaster preparedness and response. Am J Public Health 2014;104(7):1160–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chakalian PM, Kurtz LC, Hondula DM. After the lights go out: Household resilience to electrical grid failure following Hurricane Irma. Nat Hazards Rev 2019;20(4):05019001. [Google Scholar]
- 42.Hernandez D Understanding ‘energy insecurity’ and why it matters to health. Soc Sci Med 2016;167:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Energy Information Agency. One in three U.S. households faced challenges in paying energy bills in 2015. https://www.eia.gov/consumption/residential/reports/2015/energybills/ Accessed 21 Sept 2020.
- 44.Sandoval G, Toney M. Living without power:vHealth impacts of utility shutoffs in California http://www.turn.org/wp-content/uploads/2018/05/2018_TURN_Shut-Off-Report_FINAL.pdf Accessed 1 June 2020.
- 45.Molinari NA, Chen B, Krishna N, Morris T. Who’s at risk when the power goes out? The at-home electricity-dependent population in the United States, 2012. J Public Health Manag Pract 2017;23(2):152–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.