To the Editor:
To decrease the spread of coronavirus disease 2019 (COVID-19), 32 states initiated stay-at-home orders (“lockdowns”) by March 31, 2020.1 Influenza places a substantial burden on the United States, with up to 45 million symptomatic infections and 61,000 deaths per year,2 and an estimated total annual economic burden of $122 billion (2020 dollars).3 Influenza, like coronaviruses, is transmitted through respiratory droplets or direct contact. Interventions to prevent COVID-19 infection should decrease influenza infection. There is anecdotal evidence that COVID-19 restrictions have decreased influenza cases in the United States.4 We compared influenza rates in the United States during COVID-19 lockdowns with influenza rates in previous years.
We used data from 2015 to 2020 (through week 20) from the Centers for Disease Control and Prevention, which receives influenza weekly test results from approximately 100 public health centers and 300 clinical laboratories located through all 50 states, Puerto Rico, Guam, and the District of Columbia.5 As an analysis of a public dataset, this research is exempt from review under the Protection of Human Subjects Act 945 CFR 46.102(f)). Weekly reports were grouped into influenza seasons from week 40 of a given year through week 39 of the following year. The 2019–2020 season contained 33 weekly reports; 24 weeks (week 40 of 2019–week 11 of 2020) were prelockdown and 9 weeks (weeks 12–20 of 2020) were postlockdown.
Postlockdown cases were predicted by applying the linear regression model to the number of influenza cases from weeks 12 to 20 of the 4 years pre-COVID-19. These were compared with the reported cases from week 12 to 20 in the influenza year 2019–2020 with the Wilcoxon signed rank test. All of the statistics were completed using R version 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria).
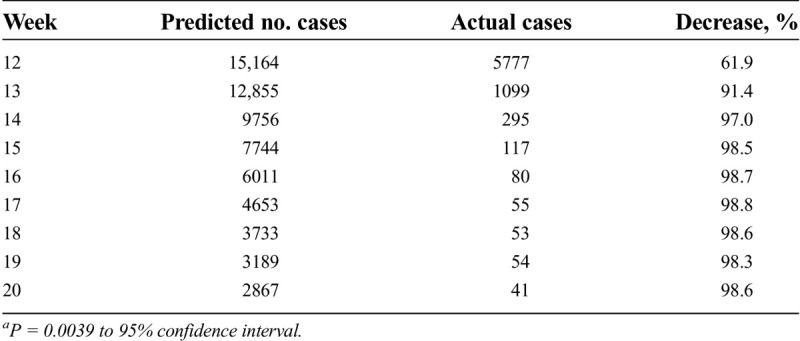
The linear regression model had a good fit (adjusted R2 0.975). Influenza rates were substantially decreased during the COVID-19 lockdown period compared with previous years (reduced by 61.9%, 91.5%, 96%, and 98% or more during weeks 12, 13, 14, and 15–20, respectively; P = 0.0039) (Table).
Table.
Comparison of predicted 2019–2020 influenza infections to actual infections, weeks 12–20a
During the COVID-19-related lockdown period, seasonal influenza activity was lower during weeks 12 to 20 of the 2019–2020 influenza season than predicted based on the previous 4 years in the United States. The limitations of this comparison include potential changes in public careseeking behaviors or physician testing patterns during the COVID-19 lockdowns. This may be more pronounced in older adults, as they are at increased risk from COVID-19; we did not evaluate age-specific influenza infections.
Restrictive public health interventions to decrease the spread of COVID-19 appear to have a substantial, significant impact on influenza virus as well. Regions facing particularly high-burden influenza seasons may consider implementing some or all of these interventions to rapidly reduce influenza infections.
Robert P. Lennon, MD, JD
Erin L. Miller, BS
Huamei Dong, PhD
David Rabago, MD
Aleksandra E. Zgierska, MD, PhD
Departments of Family and Community Medicine and Public Health Sciences Penn State Health Milton S. Hershey Medical Center Hershey, Pennsylvania
Contributor Information
Robert P. Lennon, Email: rlennon@pennstatehealth.psu.edu.
Erin L. Miller, Email: emiller22@pennstatehealth.psu.edu.
Huamei Dong, Email: hdong@pennstatehealth.psu.edu.
David Rabago, Email: drabago@pennstatehealth.psu.edu.
Aleksandra E. Zgierska, Email: azgierska@pennstatehealth.psu.edu.
References
- 1.Higham A. US lockdown: when did the US go into lockdown? https://www.express.co.uk/news/world/1270061/US-lockdown-When-did-the-US-go-into-lockdown. Published April 16, 2020. Accessed July 22, 2020.
- 2.Centers for Disease Control and Prevention . Disease burden of influenza [Internet]. https://www.cdc.gov/flu/about/burden/index.html. Published June 1, 2020. Accessed September 15, 2020.
- 3.Molinari N-AM Ortega-Sanchez IR Messonnier ML, et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine 2007;25:5086–5096. [DOI] [PubMed] [Google Scholar]
- 4.Jones N. How coronavirus lockdowns stopped flu in its tracks. Nature 2020;10.1038/d41586-020-01538-8. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention . National, regional, and state level outpatient illness and viral surveillance. https://gis.cdc.gov/grasp/fluview/fluportaldashboard.html. Published June 1, 2020. Accessed July 22, 2020.


