Abstract
Background
COVID-19 pandemic has a great impact on the disruption of maternal health-care services. Family planning is one component of maternal health-care service that needs attention during this devastating time. Compromise on family planning services and the preventive strategies of COVID-19 might increase the burden of unintended pregnancy, but there is limited evidence that shows the magnitude of unintended pregnancy during the COVID-19 pandemic. Therefore, the objective of this study was to assess unintended pregnancy during the COVID-19 pandemic and its associated factors among women attending antenatal care in northwest Ethiopia.
Methods
This study was an institutional-based cross-sectional study, including 424 women attending antenatal care from November 12/2020 to December 12/2020. The study participants were selected using a systematic random sampling technique. A pretested questionnaire was used. Binary logistic regression (bivariable and multivariable) was employed. The adjusted odds ratio with a 95% confidence interval was used to declare statistically significant variables based on p<0.05 in the multivariable logistic regression model.
Results
The magnitude of unintended pregnancy during the COVID-19 pandemic among women attending antenatal care was found to be 47.17% (42.2–52.2%). Women did not expose to community education (AOR=2.2; 95% CI1.1–4), women with no bad obstetric history (AOR=2.3; 95% CI1.3–4.1), a woman was not the primary decision maker for family planning service (AOR=2.9; 95% CI 1.5–5.7), no complication during index pregnancy (AOR=5.4; 95% CI 2.2–13) and women with no health-care provider support (AOR=2.4, 95% CI1.4–3.9) were significantly associated with unintended pregnancy.
Conclusions
The magnitude of unintended pregnancy was found to be high. Community education about maternal health services including family planning, improving women’s decision-making power for maternal health-care services, giving emphasis on pregnancy-related complications with health-care provider support, and pregnant women with bad obstetric history were suggested to reduce the problem.
Keywords: unintended pregnancy, Gondar, Ethiopia
Background
Routine health-care services reduced due to the introduction of the coronavirus (COVID-19) pandemic. COVID-19 pandemic can lead to limited health-care services especially on sexual and reproductive healthcare (SRH) aspects, such as screening of sexually transmitted infections and contraception utilization. Diminishing in SRH access due to the introduction of COVID-19 is one predisposing factor for unintended pregnancy either directly or indirectly.1 Currently there is a research question that needs to be covered timely whether the magnitude of unintended pregnancy exacerbated or not due to the introduction of COVID-19? The disease coronavirus (COVID-19) is an international health emergency. Major disruption to health-care services due to the condition of the diseases will last even for long period.2 The COVID-19 directly affects the utilization of SRH by the principles of isolation, physical distancing, Restrictions, and stay at home then family planning provision will be diminished and unintended pregnancy might be increased. COVID-19 indirectly associated with increased time dedicated to sexual intercourse among couples this, in turn, predisposes to unintended pregnancy. Parallel to that, restrictions and lockdowns are hindering the utilization contraceptive services and supplies. These could predispose to millions of unsafe abortions and death of the women.
Unintended pregnancy is a basic concept that is used to understand the demand and unmet need for contraception.3 For saying pregnancy is unintended if it is either mistimed or unwanted. Unwanted pregnancy occurs when no more children or no child is desired. Whereas mistimed pregnancy is described as when the pregnancy occurs earlier to the desired time but needed later.4 In general, unintended pregnancy is a pregnancy that occurred without consideration of whether or not contraception was being used but the pregnancy was not wanted at the time conception occurred.5,6 It is a public health issue globally, and it is one of the major reproductive and sexual health problem which ends with a higher risk of mortality and morbidity among reproductive age groups of women.7 There is evidence that shows at the global level 80 million women experienced unintended pregnancy each year. In Ethiopia, around one-third of women have experiences of unintended pregnancy even before the occurrence of COVID-19.8 Contraceptive accesses during the era of COVID-19 were limited due to programmatic shifting to the prevention and control of COVID-19.9 In addition, the prevention and control strategies for COVID-19 indirectly increase the risk of sexual violence.10,11 This in turn one factor for the increase in the magnitude of unintended pregnancy.12
Despite the aforementioned challenges, there is limited evidence that shows the magnitude of unintended pregnancy and its associated factors among pregnant women. Therefore the objective of this study was to assess the magnitude and associated factors of unintended pregnancy among pregnant women attending antenatal care in Gondar city northwest Ethiopia.
Methods
Study Design, Area and Period
An institution-based cross-sectional study was conducted among pregnant women attending antenatal care in Gondar city from 12th of November to 12th of December 2020. Gondar city is located 760 km away from Addis Ababa, the capital city of Ethiopia. Currently, there are eight public health facilities in Gondar city and from all those public health facilities approximately 2000 pregnant women had got ANC services from the report of the preceding month.
Sample Size Determination
The sample size of this study was obtained by using the formula for a single population proportion. n=  estimated Proportion of women who had experienced unintended pregnancy during COVID-19 pandemic was 50%, a level of significance 95%, a margin of error 5%, and non-response rate 10%. Where n= Initial sample size
estimated Proportion of women who had experienced unintended pregnancy during COVID-19 pandemic was 50%, a level of significance 95%, a margin of error 5%, and non-response rate 10%. Where n= Initial sample size
Z= 1.96, the corresponding Z-score for the 95% CI P= Proportion= 50%
W= Margin of error= 5%= 0.05 n=
 = 384
= 384
Taking non-response rate 10% the final sample size required for our study was 424.
Sampling Technique
All public health facilities in Gondar city were taken in a study setting. The sample size was allocated proportionally to the eight public health facilities in the city based on the number of pregnant women that visited each health facility during the preceding month before data collection. Then, the study participants were selected through a systematic random sampling technique. The K interval/fraction was calculated by K = N/n = where N=total number of pregnant women attending antenatal care per month from a single public health facility in Gondar city and n=the required sample should be taken per health facility. Then to start the interview, we had used the lottery method from the 1st pregnant woman attending antenatal care to the value of k antenatal care attendee per a given health facility. Then the interview started from the one selected pregnant woman antenatal care attendee and continued by recruiting every k value pregnant woman antenatal care attendee based on their sequence of exit after check-up, up to the required 424 participants. All pregnant women who attained antenatal care included in the study and pregnant women who are not voluntary to give full information were excluded from the study.
Data Collection Tools and Procedures
Data were collected for variable related unintended pregnancy and a pre-tested face-to-face interview took place. A minimum of one-meter distance was kept between interviewers and interviewees. The questionnaire was first prepared in English and translated to Amharic, and then back to English for the sake of consistency consisting of four sections. Three BSc midwives were distributing the questionnaire and collect data. Two BSc midwives with similar work experience were assigned to supervise the data collection process and monitored data collectors.
Data Processing and Analysis
The data were coded, entered into EPI-info version 7, cleaned, and exported to SPSS software version 20 for statistical analysis. Descriptive statistics, bivariate and multivariate logistic regressions were performed to identify factors associated with the dependent variable. The Odds ratio with a 95% confidence interval was computed to determine the level of significance.
Results
Socio-Demographic Characteristics of the Study Participants
A total of 424 women participated in the study. The majority of the respondents were between ages of 20–34 years and 309 (72.9%) of them were Orthodox and 384 (90.6%) were married. All study participants were Amhara in Ethnicity with 274 (64.6%) of them from rural residence and 239 (56.4%) had no formal education. Their median monthly income was 2400 EB with (IQ R of 1900–3286EB) Table 1.
Table 1.
Socio-Demographic Characteristics of Study Participants Northwest Ethiopia; 2020 (n=424)
| Characteristics | Frequency | Percentage |
|---|---|---|
| Age of woman in year | ||
| 15–19 | 22 | 5.2 |
| 20–34 | 262 | 61.8 |
| 35–49 | 140 | 33 |
| Religion | ||
| Orthodox | 309 | 72.9 |
| Muslim | 98 | 23.1 |
| Others* | 17 | 4 |
| Residency | ||
| Rural | 274 | 64.6 |
| Urban | 150 | 35.4 |
| Marital status | ||
| Married | 384 | 9.6 |
| Others** | 40 | 9.4 |
| Educationalstatus of woman | ||
| Has no formal education | 239 | 56.4 |
| Grade 1–8 | 49 | 11.6 |
| Grade 9and above | 136 | 32.1 |
| Occupational Status of women | ||
| Farmer | 129 | 30.4 |
| Housewife | 21 | 5 |
| Private employee | 81 | 19.1 |
| Government employee | 158 | 37.3 |
| Others*** | 35 | 8.2 |
Notes: Others*=Catholic and protestant; Other**=Single, divorced, widowed; Other***=Student, daily laborer.
Prevalence of Unintended Pregnancy
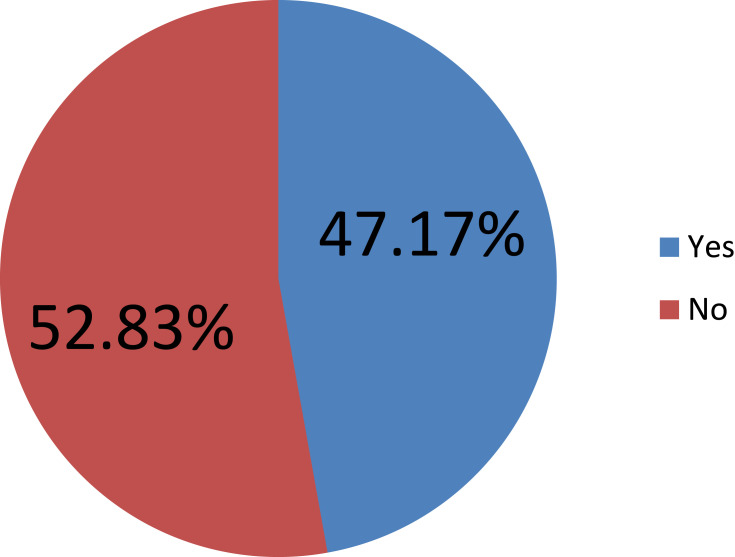
The magnitude of unintended pregnancy during the COVID-19 pandemic among women attending antenatal care was found to be 47.17% (95% CI 42.2–52.2%) Figure 1.
Figure 1.
Magnitude of unintended pregnancy during COVID-19 pandemic among women attending antenatal care.
Factors Associated with Unintended Pregnancy During COVID-19 Among Women Attending Antenatal Care
In multivariable analysis, five variables exposure to community education, decision-maker for attending family planning services, Bad obstetric history, pregnancy-related complications during index pregnancy, and health-care provider support were continued to be significant with unintended pregnancy.
Women who did not expose to community education 2.2 times more likely unintended pregnancies (AOR=2.2; 95% CI 1.1–4) as compared to those exposed to maternal and child health-related community education. Women without bad obstetric history 2.3 times more likely unintended pregnancy (AOR= 2.3; 95% CI 1.3–4.1) as compared to women with bad obstetric history. Women were not the primary decision-maker for family planning services 2.9 times more likely unintended pregnancy (AOR=2.9, 95% CI 1.5–5.7) as compared to those women were the primary decision-maker, women who did not develop index pregnancy-related complication 5.4 times more likely unintended pregnancy (AOR=5.4,95% CI 2.2–213) as compared to those who develop a pregnancy-related complication, respondents without health-care provider support 2.4 times more likely unintended pregnancy (AOR=2.4; 95% CI 1.4–3.9) as compared to those with health-care provider support Table 2.
Table 2.
Bivariable and Multivariable Logistic Regression Analysis of Factors Associated with Unintended Pregnancy Among Women Attending Antenatal Care
| Variables | Unintended Pregnancy | COR 95% CI | AOR 95% CI | |
|---|---|---|---|---|
| Yes | No | |||
| Age | NA | |||
| 15–19 | 11 | 11 | 1 | |
| 20–34 | 117 | 145 | 1.3(0.8–1.9)* | |
| 35–49 | 72 | 68 | 1.1(0.4–2.6)** | |
| Residency | NA | |||
| Rural | 135 | 139 | 1 | |
| Urban | 65 | 85 | 0.7(0.5–1.1)*** | |
| Education of women | NA | |||
| No formal education | 89 | 150 | 1 | |
| Grade 1–8 | 28 | 21 | 1.1(0.6–2.2) | |
| Grade 9 and above | 83 | 53 | 2.6(1.7–4.1)*** | |
| Exposure to community education | ||||
| Yes | 23 | 201 | 1 | 1 |
| No | 49 | 151 | 2.8(1.6–4.8)*** | 2.2(1.1–4)** |
| Decision maker for family planning service | ||||
| Primarily by women | 16 | 208 | 1 | 1 |
| Other than by woman | 49 | 151 | 4.2(2.3–7.7)*** | 2.9(1.5–5.7)*** |
| Bad obstetric history | ||||
| Yes | 28 | 196 | 1 | 1 |
| No | 51 | 149 | 2.3(1.4–3.9)*** | 2.3(1.3–4.1)** |
| Pregnancy related complication | ||||
| Yes | 7 | 217 | 1 | 1 |
| No | 33 | 167 | 6.1(2.6–14.1)*** | 5.4(2.2–13)*** |
| Health care provider support | ||||
| Yes | 58 | 166 | 1 | 1 |
| No | 80 | 119 | 1.9(1.2—2.9)*** | 2.4(1.4–3.9)** |
Notes: NA=not have association to outcome variable 1: reference category,*=0.05<p<0.2, **=0.001<p<0.05, ***=p<0.001.
Abbreviations: COR, crude odds ratio; AOR, adjusted odds ratio; CI, confidence interval.
Discussion
Currently, great attention shifting to the outbreak management of COVID-19 might affect the quality of maternal and neonatal health-care services especially family planning services. Stay at home and other preventive strategies of COVID-19 can exacerbate the magnitude of unintended pregnancy.
This study finds that the magnitude of unintended pregnancy is 47.17%.
Respondents without exposure for community education 2.2 times more likely unintended pregnancy as compared to women with community education about maternal health services. The possible explanation could be women who have no exposure to community education cannot understand the formal communication with health-care providers at the time of family planning services and even the family planning failure rate might increase due to miss use of the contraceptive that they had given by the health-care providers.
Women with no bad obstetric history 2.3 times more likely the pregnancy was unintended as compared to women with bad obstetric history. The possible explanation could be due to health-seeking behavior among women with bad obstetric history make the pregnancy planned and wanted to save their life. Previous history of bad obstetric history the determinative for the subsequent pregnancy whether it is planned or unplanned.
Respondents who were not the primary decision maker for family planning use 2.9 times more likely the pregnancy is unintended. This finding is supported by a study done in Cambodia.13 The possible explanation could be women who cannot decide on maternal health service especially for family planning mostly exposed to upland and unwanted pregnancy. This type of pregnancy mostly associated with less to attend the full elements of the maternity continuum of care.14
Respondents who did not develop pregnancy-related complications before index pregnancy 5.4 times the pregnancy was unintended as compared to those in normal state. This might be due to negligence among respondents for the subsequent pregnancy. Once the pregnancy experience is normal women might not conscious of family planning and unintended pregnancy might increase.
Women with a lack of health-care provider support are 2.4 times unintended pregnancy as compared to respondents with health-care provider support at the time of visiting a health facility for family planning services. The possible explanation might be due to women satisfied by health-care provider the probability to use family planning increase and unintended pregnancy can be prevented. To the reverse, if the health-care provider approach was not good she might refuse the use of family planning services and unintended pregnancy might increase.
Conclusions
The magnitude of unintended pregnancy was found to be high. Community education about maternal health services including family planning, improving women’s decision-making power for maternal health-care services, giving emphasis to pregnancy-related complications with health-care provider support, and pregnant women with bad obstetric history were suggested to reduce the problem.
Acknowledgments
First, I would like acknowledge University of Gondar College of Medicine and Health Sciences for the provision of ethical clearance.
Likewise, I am indebted to study participants for their permission and cooperation to participate in this study. In the same way I would like to acknowledge data collectors and supervisors.
Funding Statement
The funder had no role in the design of the study and collection, analysis and interpretation of data and in writing the manuscript.
Data Sharing Statement
The data set used and analyzed during the current study is available from the corresponding author on the reasonable request.
Ethics Approval and Consent to Participate
Ethical clearance was obtained from the Institutional Review Board (IRB) of the University of Gondar. A formal letter of approval was taken from Gondar city health office. The purpose, risk, and benefits of the study were explained in detail. We told as participation was on a voluntary basis, and they can withdraw at any time if there is any inconvenience at the time of the interview, and written informed consent was obtained from every study participant before data collection and for those less than 18 years old written informed consent was taken from their parents/guardians. And it was approved by the ethical review committee on behalf of IRB of the University of Gondar. The author would like to confirm that this study was conducted in accordance with the declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors have declared that they have no competing of interests.
References
- 1.Mmeje OO, Coleman JS, Chang T. Unintended consequences of the COVID-19 pandemic on the sexual and reproductive health of youth. J Adolesc Health. 2020;67(3):326–327. doi: 10.1016/j.jadohealth.2020.06.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ferreira-Filho ES, de Melo NR, Sorpreso ICE, et al. Contraception and reproductive planning during the COVID-19 pandemic. Expert Rev Clin Pharmacol. 2020;13(6):615–622. doi: 10.1080/17512433.2020.1782738 [DOI] [PubMed] [Google Scholar]
- 3.Moges Y, Worku SA, Niguse A, Kelkay B. Factors associated with the unplanned pregnancy at Suhul General Hospital, Northern Ethiopia, 2018. J Pregnancy. 2020;2020:2020. doi: 10.1155/2020/2926097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bekele H, Dheressa M, Mengistie B, Sintayehu Y, Fekadu G. Unintended pregnancy and associated factors among pregnant women attending antenatal care at Bako Tibe District Public Health Facility, Oromia Region, Ethiopia. J Pregnancy. 2020;2020:2020. doi: 10.1155/2020/3179193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yenealem F, Niberet G. Prevalence and associated factors of unintended pregnancy among pregnant woman in Gondar Town, North West Ethiopia, 2014. BMC Res Notes. 2019;12(1):161. doi: 10.1186/s13104-019-4203-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mosher W, Jones J, Abma J. Nonuse of contraception among women at risk of unintended pregnancy in the United States. Contraception. 2015;92(2):170–176. doi: 10.1016/j.contraception.2015.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kassahun EA, Zeleke LB, Dessie AA, et al. Factors associated with unintended pregnancy among women attending antenatal care in Maichew Town, Northern Ethiopia, 2017. BMC Res Notes. 2019;12(1):381. doi: 10.1186/s13104-019-4419-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gebremariam Weldearegawi G, Berhe Tekola K, Fseha Teklehaymanot B. Magnitude and associated factors of unintended pregnancy among pregnant women at Saesie Tsaeda Emba Woreda Eastern Zone of Tigray, North Ethiopia, 2018. J Pregnancy. 2019;2019:2019. doi: 10.1155/2019/1694808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aly J, Haeger KO, Christy AY, Johnson AM. Contraception Access During the COVID-19 Pandemic. Springer; 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xue J, Chen J, Chen C, Hu R, Zhu T. The hidden pandemic of family violence during COVID-19: unsupervised learning of tweets. J Med Internet Res. 2020;22(11):e24361. doi: 10.2196/24361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gosangi B, Park H, Thomas R, et al. Exacerbation of physical intimate partner violence during COVID-19 lockdown. Radiology. 2020;298(1):202866. doi: 10.1148/radiol.2020202866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boserup B, McKenney M, Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. Am J Emerg Med. 2020;38(12):2753–2755. doi: 10.1016/j.ajem.2020.04.077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sakuma S, Yasuoka J, Phongluxa K, Jimba M, Oh J. Determinants of continuum of care for maternal, newborn, and child health services in rural Khammouane, Lao PDR. PLoS One. 2019;14(4):e0215635. doi: 10.1371/journal.pone.0215635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yeji F, Shibanuma A, Oduro A, et al. Continuum of care in a maternal, newborn and child health program in Ghana: low completion rate and multiple obstacle factors. PLoS One. 2015;10(12):e0142849. doi: 10.1371/journal.pone.0142849 [DOI] [PMC free article] [PubMed] [Google Scholar]