Abstract
Background:
Children in rural communities often lack access to subspecialty medical care. Telemedicine has the potential to improve access to these services but its effectiveness has not been rigorously evaluated for paediatric patients with endocrine conditions besides diabetes.
Introduction:
The purpose of this study was to assess the association between telemedicine and visit attendance among patients who received care from paediatric endocrinologists at an academic medical centre in northern California between 2009–2017.
Methods:
We abstracted demographic data, encounter information and medical diagnoses from the electronic health record for patients ≤18 years of age who attended at least one in-person or telemedicine encounter with a paediatric endocrinologist during the study period. We used a mixed effects logistic regression model – adjusted for age, diagnosis and distance from subspecialty care – to explore the association between telemedicine and visit attendance.
Results:
A total of 40,941 encounters from 5083 unique patients were included in the analysis. Patients who scheduled telemedicine visits were predominantly publicly insured (97%) and lived a mean distance of 161 miles from the children’s hospital. Telemedicine was associated with a significantly higher odds of visit attendance (odds ratio 2.55, 95% confidence interval 2.15–3.02, p < 0.001) compared to in-person care.
Conclusions:
This study demonstrates that telemedicine is associated with higher odds of visit attendance for paediatric endocrinology patients and supports the conclusion that use of telemedicine may improve access to subspecialty care for rural and publicly insured paediatric populations.
Keywords: Telemedicine, telehealth, remote consultation, paediatrics, endocrinology, diabetes
Introduction
Paediatric subspecialists are unevenly distributed across the USA, creating disproportionately low access to speciality care among rural and low-income populations.1-3 Lack of local access may be a driving factor for the high non-attendance rates observed for subspeciality appointments among paediatric patients, particularly those with public insurance.4,5 Telemedicine has been identified as a potential solution to low access to care6 through its ability to mitigate the access barriers most commonly cited by families, including transportation, missed work time and need for child care.5 However, recent research demonstrates low rates of telehealth use among publicly insured paediatric populations,7 making it difficult to assess the impact of this alternate care modality.
In 2009, UC Davis Children’s Hospital (UCDCH) in Sacramento, California initiated clinic-to-clinic telemedicine consultation programmes for paediatric endocrinology services in partnership with clinics that offer primary care services in underserved areas of California. Many of these clinics are Federally Qualified Health Centers (FQHCs), which receive federal funding to provide primary care to underserved communities. These clinics were located in 17 counties throughout the state. During telemedicine consultations, patients and their family members would present in person to the local primary care clinic. Upon arrival, the staff at that clinic would measure vital signs and the primary care physician would perform a physical examination. A real-time, audio-visual telemedicine connection would then be established between the primary care clinic and the UC Davis paediatric endocrinology provider. This subspecialist would interact with the patient, his/her family members and the primary care provider to obtain relevant history details as well as the patient’s vital sign results and physical examination findings. At the conclusion of the visit, the subspecialist would make recommendations for appropriate workup and management of the diagnosed condition (s), and the primary care provider would place the necessary orders as well as arrange for a follow-up visit at the recommended interval. For these telemedicine encounters, the primary care clinic would bill insurance and the subspecialist’s time would be reimbursed by the primary care clinic at a contracted rate.
Paediatric endocrinologists, who manage complex conditions including diabetes, thyroid disease and disorders of growth and puberty, are in high demand for consultations and are rare in rural areas.8,9 A previous study by Anderson et al. demonstrated improved completion rates for endocrinology consultations among adult patients at an FQHC after implementation of an e-consultation telehealth platform.10 However, the impact of telemedicine on visit attendance rates for endocrinology care has not yet been studied in a paediatric population except among smaller samples of patients with diabetes mellitus.11-13 The purpose of this retrospective study was to compare visit attendance rates for telemedicine and in-person encounters among children receiving subspeciality endocrinology care at UCDCH during the years 2009–2017. We hypothesized that telemedicine would be associated with improved odds of visit attendance for scheduled endocrinology encounters during the study period.
Methods
We defined our study population as all patients aged ≤18 years who attended at least one scheduled visit with a UC Davis paediatric endocrinologist between 1 January 2009–31 July 2017. Visits could be in-person or via telemedicine. In-person visits took place at UCDCH in Sacramento, California. Telemedicine visits took place at any of the 25 primary care clinics with which our medical centre was contracted to provide paediatric endocrinology care via telemedicine during the study period. Because reimbursement for telemedicine encounters was covered via contract with the originating sites, payer restrictions for coverage of telemedicine did not impact on which patients could receive telemedicine care within our study population. However, telemedicine care was restricted to patients who received primary care at the clinics with active telemedicine contracts during the study period.
For patients included in our study population, we abstracted demographic data from the UC Davis electronic health record (EHR) including date of birth, sex, address and insurance status. Insurance status was then categorised as private or public, with the public category also including a small number of patients who were uninsured or self-pay. We used geocoded addresses and a proprietary geolocation application programming interface to estimate each patient’s travel distance from UCDCH based on geographic coordinates.14 To characterise whether scheduled encounters were attended, we also abstracted encounter-level data for all paediatric endocrinology encounters that were scheduled for patients in our study population during the study period. This data included the encounter type (in-person or telemedicine), date, attendance status and primary associated diagnosis. Because an attended visit was required for a patient to be included in the study population, for the encounter-level analysis we only included encounters subsequent to the patient’s first attended visit, to avoid selection bias. For encounters that were not attended, no primary diagnosis was coded by a physician. To address this, we imputed the primary diagnosis that was associated with the patient’s closest attended visit. Diagnoses were initially categorised based on the International Classification of Pediatric Endocrine Diagnoses (ICPED), and categories were then adjusted slightly (making diabetes mellitus a separate group; combining disorders of the reproductive tract, puberty and sex development into a single category; and combining short and tall stature) to create the following categories: (a) diabetes mellitus, (b) growth disorders, (c) reproductive disorders, (d) thyroid disorders, (e) obesity, (f) pituitary disorders, (g) calcium and bone disorders and (h) other. Common diagnoses included in the ‘other’ category were hypoglycaemia, disorders of salt and water regulation, adrenal disorders and other syndromes with endocrine features.
To evaluate the association between telemedicine and visit attendance, we fitted an encounter-level mixed effects logistic regression model for visit attendance with type of visit (telemedicine or in-person), age, primary diagnosis, distance to UCDCH, insurance type and year of visit as predictors. These covariates were selected a priori. Because there was a linear relationship between year and visit attendance, we included year as a continuous variable. In addition to these fixed effects, we specified random intercepts for individual patients, to account for correlations among scheduled encounters from the same patient. We performed a robustness analysis by fitting the same model with variables for patient-level mean and the encounter-level deviation for telemedicine use in place of the variable for encounter type; this method permits evaluating whether the between-patient and within-patient effects of telemedicine are similar, as is assumed in the model that only includes the telemedicine indicator.15,16 All analyses were completed using Stata statistical software version 16.1.17 This study was approved by the UC Davis Institutional Review Board.
Results
A total of 5083 unique patients with 40,941 encounters met the inclusion criteria. Table 1 shows the demographic and health characteristics of the sample. At the time of the first encounter 36.6% of included patients were adolescents (ages 13–17 years), 36.6% were school-aged (ages 7–12 years), 20.7% were preschool-aged (ages 1–6 years), and 6.2% were infants less than one year of age. Approximately half of patients were female (52.9%). Most patients were publicly insured (64.0%) and lived 30 miles or fewer from the children’s hospital (53.2%). The median number of scheduled visits with a paediatric endocrinologist during the study period was four (interquartile range (IQR): 2–10), although 18.9% scheduled only one visit, suggesting an initial consultation without need for ongoing endocrinology care.
Table 1.
Study population
| All patients n (%) | Patients with >1 in-person visita |
Patients with >1 telemedicine visita |
|
|---|---|---|---|
| Age at first encounter | |||
| Infant (<1 year) | 316 (6.2) | 304 (6.3) | 15 (5.1) |
| Preschool-aged (1–6 years) | 1050 (20.7) | 991 (20.4) | 72 (24.7) |
| School-aged (7–12 years) | 1859 (36.6) | 1785 (36.8) | 107 (36.6) |
| Adolescent (13–18 years) | 1858 (36.6) | 1777 (36.6) | 98 (33.6) |
| Sex | |||
| Male | 2396 (47.1) | 2298 (47.3) | 132 (45.2) |
| Female | 2687 (52.9) | 2559 (52.7) | 160 (54.8) |
| Insurance | |||
| Private | 1828 (36.0) | 1824 (37.6) | 9 (3.1) |
| Public | 3255 (64.0) | 3033 (62.5) | 283 (96.9) |
| Distance to specialist | |||
| 30 miles or fewer | 2704 (53.2) | 2703 (55.6) | 2 (0.7) |
| 31–60 miles | 1008 (19.8) | 1006 (20.7) | 2 (0.7) |
| 61–100 miles | 540 (10.6) | 509 (10.5) | 43 (14.7) |
| >100 miles | 831 (16.4) | 639 (13.2) | 245 (83.9) |
| Mean (SD) | 53.9 (62.8) | 48.8 (57.9) | 160.9 (63.8) |
| Number of visits scheduled | |||
| 1 | 962 (18.9) | 898 (18.4) | 69 (23.6) |
| >1 | 4121 (81.1) | 3964 (81.6) | 223 (76.4) |
| Median (IQR) | 4 (2,10) | 4 (2,11) | 3 (2,6) |
| Total | 5,083 | 4,857 | 292 |
IQR: interquartile range; SD: standard deviation.
Patients who scheduled both a telemedicine and an in-person visit (n=66) are represented in all three columns.
Demographic characteristics differed between patients who had telemedicine appointments and those who did not. Specifically, patients who scheduled a telemedicine visit were more likely to have public insurance (96.9% vs 62.5%) and live significantly farther from the subspeciality medical centre, at a mean distance of 160.9 miles (standard deviation (SD) = 63.9 miles) compared to 48.8 miles (SD = 57.9 miles) for the in-person cohort.
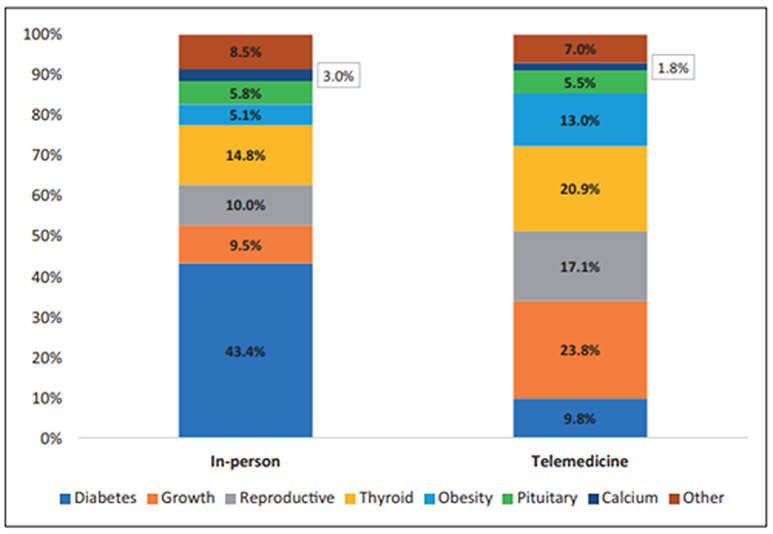
Figure 1 shows the primary diagnoses associated with scheduled in-person and telemedicine encounters. Diabetes mellitus was the most common diagnosis for in-person encounters, accounting for 43.4% of in-person visits. The next most common diagnoses associated with in-person visits were thyroid disorders (14.8%), reproductive disorders (10.0%) and growth disorders (9.5%). Growth disorders, thyroid disorders and reproductive disorders were the most common reasons for telemedicine visits, accounting for 23.8%, 20.9% and 17.1% of visits, respectively.
Figure 1.
Primary diagnoses associated with scheduled in-person and telemedicine encounters.
Table 2 shows the adjusted odds ratios and 95% confidence intervals (CIs) resulting from our mixed effects logistic regression model with patient identity (ID) specified as a random intercept. Telemedicine encounters demonstrated significantly higher odds of attendance compared to in-person encounters (odds ratio (OR) = 2.55, 95% CI = 2.15–3.02, p < 0.001) after adjusting for year of encounter, distance to subspecialist, patient age at time of encounter, insurance type and primary diagnosis. Encounters had lower odds of visit attendance if the patient had nonprivate insurance, or if the patient lived at a distance of 61–100 miles (OR = 0.88, 95% CI = 0.81–0.95, p = 0.002) or >100 miles (OR = 0.86, 95% CI = 0.80–93, p < 0.001) from the UCDCH in Sacramento. We also found that visit attendance was inversely associated with patient age, with infants demonstrating highest attendance rates followed by preschool-aged children (OR = 0.75, 95% CI = 0.64–0.89, p < 0.001) and school-aged children (OR = 0.75, 95% CI = 0.63–0.86, p < 0.001) and then adolescents (OR = 0.62, 95% CI = 0.53–0.72, p < 0.001). Finally, visits with a primary diagnosis of obesity demonstrated lower adjusted odds of attendance compared to a reference diagnostic category of diabetes (OR = 0.82, 95% CI = 0.74–0.90, p < 0.001). Comparison of within-cluster and between-cluster estimates of telemedicine effects in the sensitivity analysis revealed no substantial differences, supporting the specification of the model in our primary analysis.
Table 2.
Adjusted odds of visit attendance from mixed effects logistic regression model.a
| Adjusted odds ratio | 95% CI | p-Value | |
|---|---|---|---|
| Encounter type | |||
| In-person (ref) | – | – | – |
| Telemedicine | 2.55 | 2.15–3.02 | <0.001 |
| Year of encounter | 1.00 | 1.00–1.01 | 0.333 |
| Distance to specialist | |||
| 30 miles or fewer (ref) | – | – | – |
| 31–60 miles | 0.97 | 0.91–1.04 | 0.370 |
| 61–100 miles | 0.88 | 0.81–0.95 | 0.002 |
| >100 miles | 0.86 | 0.80–0.93 | <0.001 |
| Age at encounter | |||
| Infant (<1 year) (ref) | – | – | – |
| Preschool-aged (1–6 years) | 0.75 | 0.64—0.89 | 0.001 |
| School-aged (7–12 years) | 0.74 | 0.63–0.86 | <0.001 |
| Adolescent (13–18 years) | 0.62 | 0.53–0.72 | <0.001 |
| Insurance | |||
| Private (ref) | – | – | – |
| Public | 0.85 | 0.80–0.89 | <0.001 |
| Primary diagnosis | |||
| Diabetes (ref) | – | – | – |
| Growth | 1.00 | 0.92–1.09 | 0.958 |
| Reproductive | 0.95 | 0.88–1.03 | 0.253 |
| ThyroidObesity | 1.010.82 | 0.94–1.09 | 0.722 |
| 0.74–0.90 | <0.001 | ||
| Pituitary | 1.00 | 0.90–1.11 | 0.985 |
| Calcium and bone | 0.97 | 0.84–1.11 | 0.646 |
| Other | 0.99 | 0.90–1.08 | 0.771 |
CI: confidence interval.
Analysis restricted to scheduled encounters following a patient’s first attended encounter.
Discussion
The patients served by our paediatric endocrinology clinic-to-clinic telemedicine programme between 2009–2017 were predominantly publicly insured and lived at a mean distance of 160.9 miles from our academic children’s hospital. Based on published literature, these factors are associated with low visit attendance rates for subspeciality appointments. However, our analysis reveals that telemedicine encounters during the study period were more likely to be attended than in-person encounters after adjustment for age, diagnosis and distance from specialist. This suggests that use of telemedicine as a care modality reduced existing access barriers for these high-risk patients.
It is important to note that the distribution of diagnoses seen by telemedicine and in-person were different. Diabetes mellitus made up 43% of in-person encounters but only 9.8% of telemedicine encounters, and telemedicine encounters were more likely to address growth disorders, reproductive disorders, thyroid disorders and obesity. The low prevalence of telemedicine encounters for diabetes is because only a few telemedicine sites had the capability to download data from patients’ home glucose meters – an essential aspect of outpatient diabetes management. The higher rates of growth, reproductive and thyroid disorders and obesity among telemedicine encounters are likely because these diagnoses are relatively straightforward and well-suited to remote management. It may also be that local primary care providers felt more comfortable managing these common diagnoses in consultation with a remote specialist, whereas for disorders of the pituitary, the adrenal gland or calcium metabolism they preferred to refer patients for in-person endocrine care.
Our findings overall support previous studies which have found that telemedicine is associated with higher rates of visit attendance for subspeciality care. A similar study conducted by the authors which examined paediatric tele-neurology consultations found that telemedicine visits were associated with significantly higher odds of attendance compared to in-person visits,18 and a recent publication out of Australia demonstrated improved attendance for immunology visits conducted via telemedicine versus in-person.19 In addition, multiple studies of telemedicine for diabetes care in the paediatric population have demonstrated higher visit frequency and better adherence to recommended quarterly encounters with use of telemedicine.11-13,20-23 To our knowledge, this study is the first to explore visit attendance rates via telemedicine for a paediatric endocrinology population that includes non-diabetes diagnoses.
In addition to demonstrating higher odds of attendance for telemedicine encounters, our regression model confirms the findings of prior studies that older age and greater distance from subspecialists are associated with lower visit attendance among paediatric patients.4,5 Our mixed effects model also revealed that obesity was the only diagnostic category with significantly lower adjusted odds of visit attendance compared to diabetes. This finding is not surprising because, unlike the other diagnostic categories, obesity is frequently managed by primary care providers and typically does not require any subspecialty prescription medications, making it more likely that patients would cancel or reschedule a higher proportion of their scheduled visits for this diagnosis.
Our analysis has several limitations. Most notably, patients were not randomly assigned to telemedicine, and therefore our telemedicine and in-person cohorts differed demographically and clinically. We adjusted for measured differences between these cohorts via our statistical analysis, but there may have been unmeasured confounders that could have influenced both a patient’s likelihood to schedule a telemedicine visit as well as the likelihood of visit attendance. However, based on published literature we would expect our population served by telemedicine to demonstrate lower rates of visit attendance, and for any unmeasured confounders to therefore bias toward a lower odds of attendance for telemedicine encounters. Thus, the fact that telemedicine was associated with higher visit attendance in our analysis is an important and significant finding.
In addition, we only included patients who attended at least one visit with a paediatric endocrinologist. Therefore, we did not capture the group of patients who were referred for care but never scheduled or attended a visit, and we do not know if the odds of attendance for initial endocrinology scheduled visits might be different between the two care modalities. Finally, this study only included telemedicine visits that were conducted using real-time video conferencing between local primary care clinics and our children’s hospital. As such, our findings may not be applicable to other forms of telemedicine such as asynchronous e-consultations or direct patient-to-provider video visits, which are increasingly common since the onset of the coronavirus disease 2019 (COVID-19) pandemic.
This study contributes to the body of literature supporting telemedicine as a means to improve access to subspeciality care for rural and publicly insured paediatric populations. Particularly since the onset of the COVID-19 pandemic, the use of clinic-to-clinic as well as home-to-clinic and asynchronous telehealth encounters has risen dramatically, and further research of this type – retrospective analyses utilising rigorous methodology – will be essential as we evaluate how well these services are working to sustain the health of patients in their local environments and which factors may influence their sustainability and ongoing use.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This project was supported by the National Center for Advancing Translational Sciences, National Institutes of Health (NIH), through grant number UL1 TR001860 and linked award TL1 TR001861. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
References
- 1.Mayer ML. Disparities in geographic access to pediatric subspecialty care. Matern Child Health J 2008; 12: 624–632. [DOI] [PubMed] [Google Scholar]
- 2.Mayer ML. Are we there yet? Distance to care and relative supply among pediatric medical subspecialties. Pediatrics 2006; 118: 2313–2321. [DOI] [PubMed] [Google Scholar]
- 3.Mayer ML, Beil HA and von Allmen D. Distance to care and relative supply among pediatric surgical subspecialties. J Pediatr Surg 2009; 44: 483–495. [DOI] [PubMed] [Google Scholar]
- 4.Bohnhoff JC, Taormina JM, Ferrante L, et al. Unscheduled referrals and unattended appointments after pediatric subspecialty referral. Pediatrics 2019; 144. [DOI] [PubMed] [Google Scholar]
- 5.Zuckerman KE, Perrin JM, Hobrecker K, et al. Barriers to specialty care and specialty referral completion in the community health center setting. J Pediatr 2013; 162: 409–414.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Utidjian L and Abramson E. Pediatric telehealth: Opportunities and challenges. Pediatr Clin North Am 2016; 63: 367–378. [DOI] [PubMed] [Google Scholar]
- 7.Ray KN, Mehrotra A, Yabes JG, et al. Telemedicine and outpatient subspecialty visits among pediatric Medicaid beneficiaries. Acad Pediatr 2020; 20: 642–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lu H, Holt JB, Cheng YJ, et al. Population-based geographic access to endocrinologists in the United States, 2012. BMC Health Serv Res 2015; 15: 541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee JM, Davis MM, Menon RK, et al. Geographic distribution of childhood diabetes and obesity relative to the supply of pediatric endocrinologists in the United States. J Pediatr 2008; 152: 331–336. [DOI] [PubMed] [Google Scholar]
- 10.Anderson D, Porto A, Koppel J, et al. Impact of endocrinology econsults on access to endocrinology care for Medicaid patients. Telemed J E Health. Epub ahead of print 5 February 2020. [DOI] [PubMed] [Google Scholar]
- 11.Crossen SS, Marcin JP, Qi L, et al. Home visits for children and adolescents with uncontrolled type 1 diabetes. Diabetes Technol Ther 2020; 22: 34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reid MW, Krishnan S, Berget C, et al. CoYoT1 clinic: Home telemedicine increases young adult engagement in diabetes care. Diabetes Technol Ther 2018; 20: 370–379. [DOI] [PubMed] [Google Scholar]
- 13.Wood CL, Clements SA, McFann K, et al. Use of telemedicine to improve adherence to American Diabetes Association standards in pediatric type 1 diabetes. Diabetes Technol Ther 2016; 18: 7–14. [DOI] [PubMed] [Google Scholar]
- 14.Weber S and Peclat M. A simple command to calculate travel distance and travel time. Stata J 2017; 17: 962–971. [Google Scholar]
- 15.Neuhaus JM. Assessing change with longitudinal and clustered binary data. Annu Rev Public Health 2001; 22: 115–128. [DOI] [PubMed] [Google Scholar]
- 16.Neuhaus JM and Kalbfleisch JD. Between-and within-cluster covariate effects in the analysis of clustered data. Biometrics 1998: 638–645. [PubMed] [Google Scholar]
- 17.StataCorp. Stata Statistical Software: Release 16. College Station, TX: StataCorp LLC, 2019. [Google Scholar]
- 18.Dayal P, Chang CH, Benko WS, et al. Appointment completion in pediatric neurology telemedicine clinics serving underserved patients. Neurol Clin Pract 2019; 9: 314–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Snoswell CL and Comans TA. Does the choice between a telehealth and an in-person appointment change patient attendance? Telemed J E Health. Epub ahead of print 19 August 2020. [DOI] [PubMed] [Google Scholar]
- 20.Bashshur RL, Shannon GW, Krupinski EA, et al. National telemedicine initiatives: Essential to healthcare reform. Telemed J E Health 2009; 15: 600–610. [DOI] [PubMed] [Google Scholar]
- 21.Malasanos T and Ramnitz MS. Diabetes clinic at a distance: Telemedicine bridges the gap. Diabetes Spectr 2013; 26: 226–231. [Google Scholar]
- 22.Malasanos TH, Burlingame JB, Youngblade L, et al. Improved access to subspecialist diabetes care by telemedicine: Cost savings and care measures in the first two years of the FITE diabetes project. J Telemed Telecare 2005; 11: 74–76. [DOI] [PubMed] [Google Scholar]
- 23.Smith AC, Batch J, Lang E, et al. The use of online health techniques to assist with the delivery of specialist paediatric diabetes services in Queensland. J Telemed Telecare 2003; 9: 54–57. [DOI] [PubMed] [Google Scholar]