Introduction
Catheter-associated urinary tract infection (CAUTI) remains a significant health care associated infection. The risk of acquiring bacteriuria is 3–7% while urinary catheters remain in place1 suggesting that research should focus on earlier urinary catheter removal. Urinary catheter utilization rates in the intensive care unit (ICU) are higher than rates in non-ICU areas, 61% compared to 20% respectively.2 A national initiative disseminated information and guidance on technical and socio-adaptive factors to prevent CAUTI. This initiative across 603 acute care hospitals led to a decline in both catheter utilization and CAUTI rates in non-ICU patients, yet no difference in rates was observed in ICU patients.3 Thus, interventions to decrease catheter utilization and CAUTI rates specifically in ICU patients are needed.
Research has demonstrated that bladder scanners (BS) using ultrasound (US) technology can reduce indwelling urinary catheter days in catheter removal protocols.3–4 However, research demonstrating accuracy of the BS as a bladder US device was primarily conducted in non-ICU patients4–10 with minimal research in ICU patients.11–12 Our previous pilot study in ICU patients demonstrated inaccuracies of BS when abdominal fluid (ascites) or morbid obesity were present.13 Traditional US devices allow for direct visualization of the bladder prior to bladder volume measurement. However, the lack of direct visualization with early model BSs to distinguish between bladder volume and other fluid collections (e.g. ascites, retroperitoneal hemorrhage) in the pelvis or lower abdomen was previously noted as a potential reason for inaccuracy of BS.14
One patient population commonly seen in the ICU with the potential for ascites are those who develop acute kidney injury (AKI). The incidence of AKI and need for renal replacement therapy occurs frequently in ICU patients undergoing cardiac surgery or extracorporeal membrane oxygenation, and patients with shock, sepsis, or severe traumatic injury.15–17 In oliguric AKI patients, urinary catheters are often kept in place to monitor changes in urine output as an indicator of kidney function recovery which can be complete, partial, or non-recovery.18 Criteria for appropriate indication for urinary catheters developed by a panel of experts included the indication for an indwelling urinary catheter for daily measurement of urine volume in patients with AKI. The criteria for appropriate indication for intermittent straight catheterization (ISC) was not included for AKI patients, and BS or US measurement was not identified as a non-catheter option.19 Exploration of interventions to reduce urinary catheter days in dialysis patients and patients with AKI is needed.
BS technology now provides actual imaging of the bladder and observation of abdominal fluid prior to scanning20 similar to traditional 2-dimensional (2-D) US technology. Research is needed to examine the diagnostic accuracy of these new BSs with imaging capability compared to US for bladder volume measurements in ICU patients and specifically in critically ill patients who develop AKI and need hemodialysis or have low urine output.
The purpose of this study was to examine the accuracy of BS and US bladder volume measurements in ICU patients on dialysis or unable to void 6 hours after urinary catheter removal and if accuracy was clinician dependent. The aims of this prospective correlational descriptive study were to 1) compare BS (Verathon Prime Plus®, Bothell, WA), 2-D US (Sono-Site II, FujiFilm, Bothell, WA), and urinary ISC bladder volumes (gold standard) in ICU patients with low urine output receiving dialysis or ICU patients unable to void; 2) compare the accuracy of measurements by different clinicians (physician and APRN for US; APRN and RN for BS); 3) determine frequency that BS and US measurements correctly identified clinical decision points indicating ISC needed or ISC not needed.
Materials and Methods
The study was conducted in 4 ICUs at a 1350 bed quaternary Level 1 Trauma academic medical center in the Midwest USA. The 4 ICUs included a 36-bed Surgical/Burn/Trauma ICU, 34-bed Medical ICU, 27-bed Cardiothoracic Thoracic ICU, and 20-bed Neurology/Neurosurgery ICU. Critical care faculty and fellows, APRNs, and bedside nurses were recruited for data collection. Didactic bladder US education and training of 3 fellows, 4 APRNs, and 9 bedside nurses was provided by the Director of Critical Care Ultrasound Training Program (EA) followed by hands-on practice on the US or BS device by the vendor’s clinical specialist. An additional attending with US expertise participated in data collection.
Devices
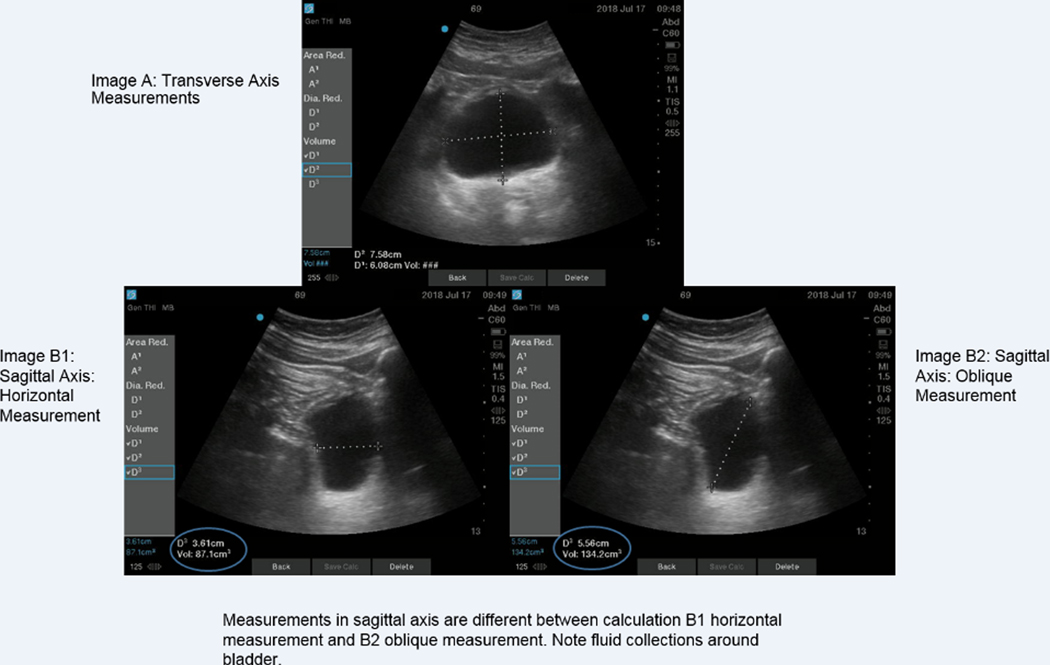
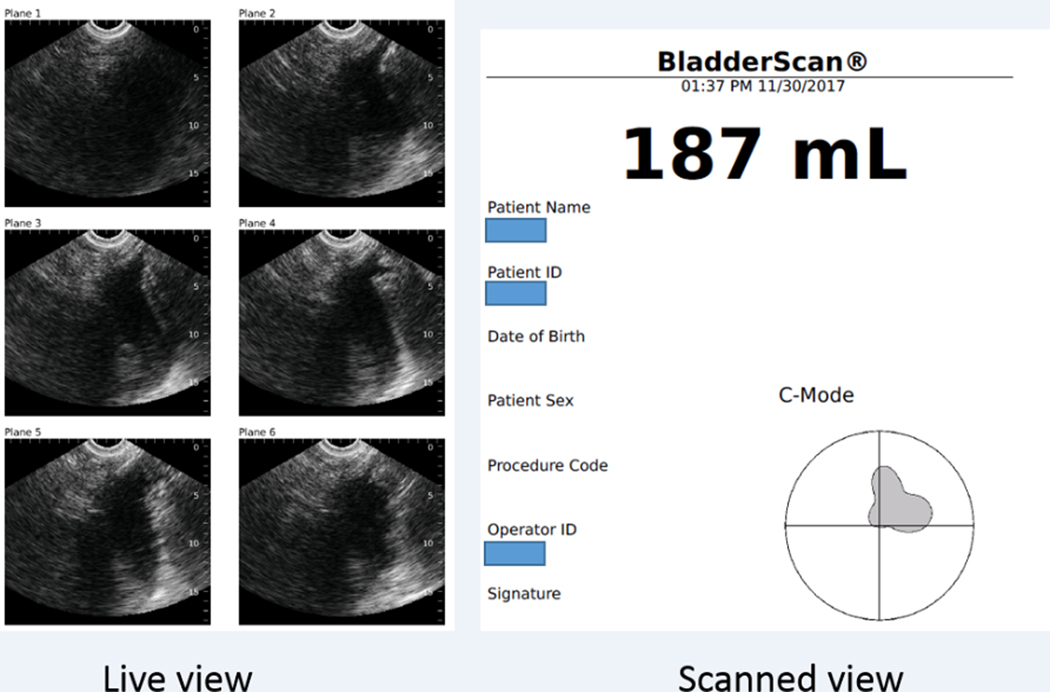
Bladder volume measurements were calculated using the SonoSite II US machine. For the first 29 patients, bladder volume was calculated with 3 measurements (vertical and horizontal measurement in the transverse axis of the bladder and a horizontal measurement in the sagittal axis). Upon review of the initial results comparing non-invasive measurements with ISC volume, US measurements using a horizontal measurement in the sagittal view were consistently lower than ISC volumes. Therefore, an oblique measurement in the sagittal bladder axis was also obtained for the remaining 44 patients21 (Figure 1). Thus, for 44 patients, 2 different bladder volume measurements with US were recorded, horizontal sagittal and oblique sagittal. The BS device, Verathon Prime Plus®, has live visual capability allowing the clinician to identify the bladder prior to volume measurement. However, it was not possible to refocus the device to only capture bladder measurement once it locked on ascites as part of the bladder (Figure 2).
Figure 1.
Horizontal and oblique measurement with sagittal axis view
Figure 2.
Verathon Prime Plus® Live scanning views and completed scanned view
Inter-rater Reliability:
Prior to data collection, each clinician underwent inter-rater reliability (IRR) testing with 35 pairs of measurements on 35 different patients without a urinary catheter. For the US, each clinician had at least 5 paired measurements with two US expert intensivists (EA and BW). Sample size for determining the IRR was estimated based on the width of the Wald confidence interval for IRR.22 The following inputs were used: 6 observations per patient, width of 0.1, desired intra-class correlation of 0.8, alpha of 0.05, and 80% power. IRR reflects the variation between the measurements taken by two or more independent parties, using the same tool measuring the same group of subjects. The intra-class correlation coefficient (ICC) based on a two-way random-effects model was used to assess interrater reliability.23 ICC guidelines for good/excellent correlation require values above 0.75. Each clinician achieved ≥.80 ICC with the 35 pairs of measurements prior to participating in data collection for the study.
Patients
Inclusion criteria included ICU patients receiving any form of renal dialysis with no indwelling urinary catheter or patients unable to void 6 hours post urinary catheter removal or 6 hours after admission. Patients were excluded if < 18 years of age or pregnant.
Data Collection
Following approval from the Human Research Protection Office, data were collected from December 2017 through July 2018, Monday-Friday. Upon consent, the research coordinator contacted the 4 research team members (MD, 2 APRNs, RN). For patients unable to void, immediate measurements were obtained. For dialysis patients, a time was scheduled. The research coordinator guided the sequence of measurements which varied daily and ensured clinicians were blinded to each other’s measurements. Each clinician documented the measured bladder volume and observation of abdominal fluid. After BS and US measurements, the bedside nurse performed an ISC and recorded a bladder volume. All measurements were completed ≤ 30 minutes.
Statistical Analysis
Analysis was conducted on aggregate de-identified data with the statistical package IBM SPSS version 25 (IBM Corporation, 1 New Orchard Road, Armonk, New York 10504–1722) by a statistician. Continuous variables were reported as a mean and standard deviation (SD). Categorical variables were reported as number and percentages. Bland-Altman analysis for repeated measures were conducted to evaluate the level of agreement between the following values: (1) US horizontal measurement and ISC, (2) BS and ISC, (3) US oblique measurements and ISC, (4) APRN US horizontal and MD US horizontal, (5) APRN oblique US and MD US oblique US, and (6) APRN BS and RN BS. Bland-Altman upper and lower limits of agreement with 95% confidence intervals and bias were calculated. Scatter plots of the differences between the aforementioned pairs of values against the average of the aforementioned pairs of values were generated.
To prevent patient discomfort, clinical decision points for ISC are important for ICU patients who cannot communicate the need to void. Three volumes for ISC decision points were analyzed: ≥ 300 ml and ≥ 550 ml indicating need for catheterization and < 150 ml for no catheterization. Comparison between clinicians and devices were conducted via chi square analysis with sample sizes of 5 or greater. Fisher’s Exact test was used when expected cell counts were less than 5. Catheterization decision points were based on the hospital’s current nurse driven protocol that uses ≥ 300 ml measurement with a BS as an indication for ISC and < 150 ml as no need for catheterization. The decision point of ≥ 550 ml was based on literature supporting approximately 500–600 ml as first sensation for fullness24 and volumes of 582±199 ml to 611±209 ml in a study that examined individual maximum bladder capacity.25
Results
Seventy five patients were consented; 73 completed the study with at least 3 of the device measurements obtained. The mean patient age was 56.9 years ± 16.1 with a BMI 33.1 ± 10.1, 67% (49) male with 77% (56) patients on dialysis and 23% unable to void. ISC volume was 171.7 ± 269.7 (range 0–1100 milliliters [ml]). Abdominal fluid was noted in 28% of measurements.
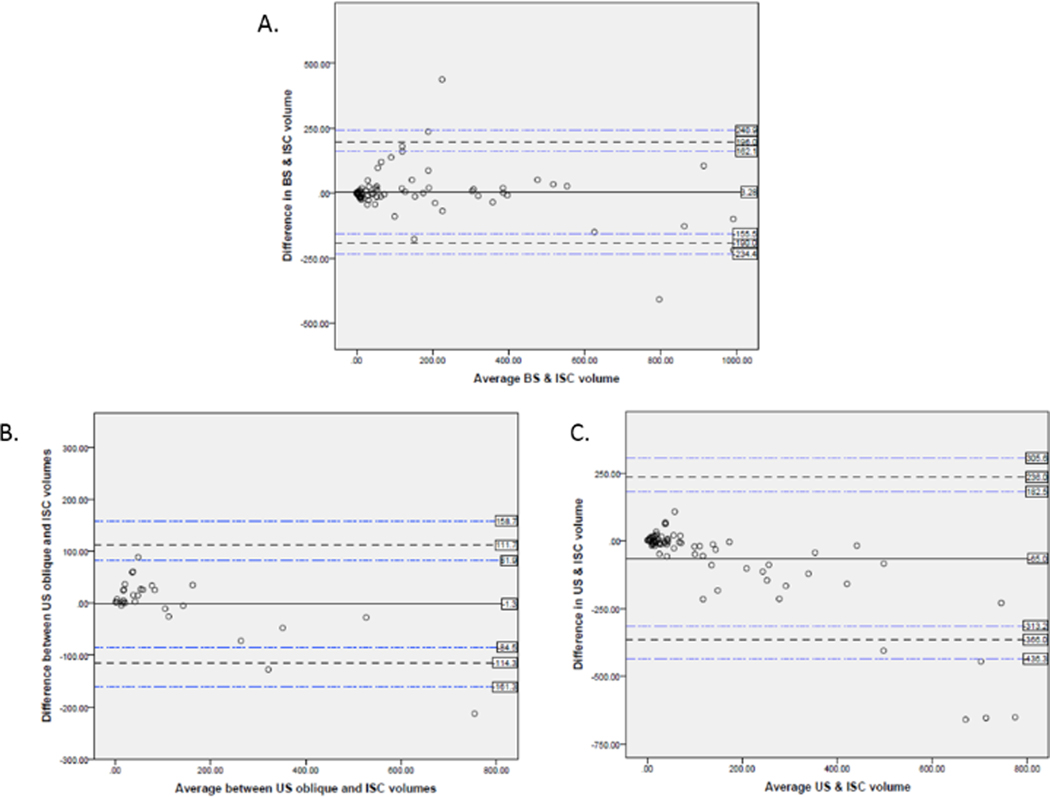
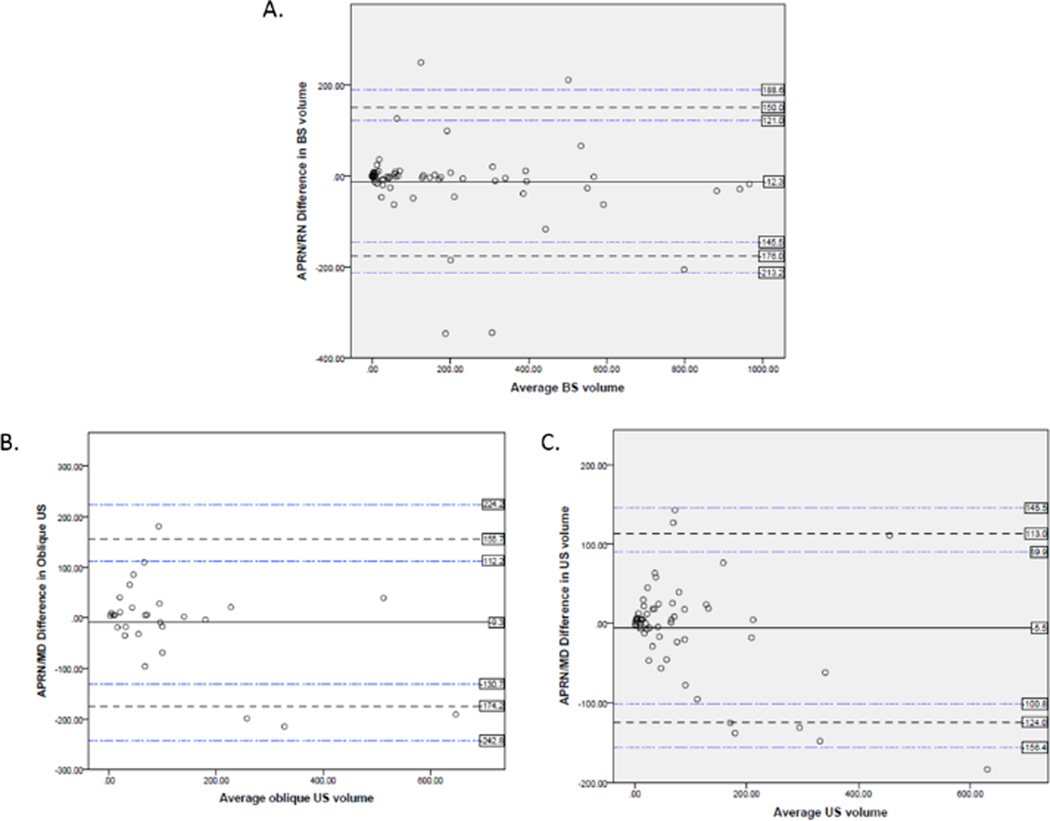
Bland Altman Plots (Figures 3–4) demonstrated outliers for all comparisons except APRN/MD US with oblique measurement in the sagittal axis. Bias was lowest for US oblique measurement in the sagittal axis and ISC volume at −1.3 ml while bias for BS and ISC volume was 3.3 ml (Table 1). The negative bias for US oblique and ISC volume was primarily due to volume measurements > 150 ml with a negative overall trend observed in the plots. Overall, larger differences were observed in the measurements at higher ISC volumes. APRN/MD US bias was lower, −5.5 in horizontal and −9.3 with oblique, than APRN/BS at −12.3. The APRN to other clinician measurements were negative in all comparisons indicating lower volumes measured with US than the comparison measurement.
Figure 3.
Bland Altman Plots of Device and Urine Volume Measurements: A. Bland Altman Plot of Bladder Scanner and Urine Volume Measurements, B. Bland Altman Plot of Ultrasound Oblique Measurement in Sagittal View and Urine Volume Measurements, C. Bland Altman Plot of Ultrasound Horizontal Measurement in Sagittal Axis Measurements and Urine Volume Measurements
Figure 4.
Bland Altman Plots of Clinician Comparisons: A. Bland Altman Plot of APRN and RN Bladder Scanner Measurements, B. Bland Altman Plot of APRN and Physician Ultrasound Oblique in Sagittal Axis Measurements, C. Bland Altman Plot of APRN and Physician Ultrasound Horizontal in Sagittal Axis Measurements
Table 1.
Bland Altman Results
| Device or Clinician Comparisons | Bias | Upper Limits of Agreement | Upper Confidence Intervals | Lower Limits of Agreement | Lower Confidence Intervals |
|---|---|---|---|---|---|
| US Horizontal measure in long view & ISC (n=73) | −65 | 236 | 182.5, 305.6 | −366 | −313.2, −436.3 |
| US Oblique measure in long view & ISC (n=44) | −1.3 | 111.7 | 81.9, 158.7 | −114.3 | −84.5, −161.3 |
| BS & ISC (n=73) | 3.3 | 196 | 162.1, 240.9 | −190 | −155.5, −234.4 |
| APRN/MD US & Average US (n=73) | −5.5 | 113 | 89.9, 145.5 | −124 | −100.8, −156.4 |
| APRN/MD US Oblique & Average US (n=44) | −9.3 | 155.7 | 112.2, 224.2 | −174.2 | −130.7, −242.8 |
| APRN/RN BS & Average BS (n=73) | −12.3 | 150 | 121, 188.6 | −176 | −145.5, −213.2 |
US=ultrasound; ISC=intermittent straight catheter urine volume, BS=bladder scanner; MD=physician;
APRN=Advanced Practice RN; RN=bedside RN
Clinical decision points (Table 2) using ≥ 300 ml ISC volume as criteria for catheterization (n=16) showed that BS measurements by both RN and APRN accurately identified need for bladder catheterization in 94–100% of measurements while US measurements were less accurate at identifying need for catheterization 50–80%. When ISC volumes were larger, ≥ 550 ml (n=6), BS accuracy for need to catheterize for RNs and APRNs was 83% −100% respectively, and again, US measurements indicating need to catheterize were less accurate, 0–100% depending on clinician and horizontal measurement. However, the number of measurements for ISC ≥ 550 ml was lower (n=6) compared to other clinical decision points. APRN BS and APRN US measurements were significantly different at ≥ 300 ml (p=.001) and ≥ 550 ml (p=.015). For the clinical decision point of < 150 ml (n=51) indicating no need for catheterization (n=51), BS measurements correctly identified 92–94% of patients would not need to be catheterized while US measurements were correct for 97–100% of measurements (Table 2). However, with the identification of ascites by at least one clinician and bladder volume < 150 ml (n=37), BS was accurate 86–89% of measurements while US was accurate 97–100% of measurements (p=.021).
Table 2.
Clinical Decision Points for Need or No Need for Catheterization
| Clinician and Device | Urine Catheter Volume ≥ 300 ml compared to device and clinician ≥ 300 ml | Urine Catheter Volume ≥ 550 ml compared to device and clinician ≥ 550 ml | Urine Catheter Volume < 150 ml compared to device and clinician < 150 ml | Urine Catheter Volume < 150 ml compared to device and clinician < 150 ml when abdominal fluid present |
|---|---|---|---|---|
| RN BS | 94% (n=16) | 100% (n=6) | 92% (n=51) | 86% (n=37)^ |
| APRN BS | 100% (n=15)* | 83% (n=6)+ | 94% (n=50) | 89% (n=36)# |
| APRN US | 50% (n=16)* | 0% (n=6)+ | 100% (n=51) | 100% (n=37)^# |
| MD US | 56% (n=9) | 33% (n=3) | 98% (n=44) | 97% (n=31) |
| APRN US oblique | 63% (n=8) | 33% (n=3) | 97% (n=33) | 100% (n=23) |
| MD US oblique | 80% (n=5) | 100% (n=1) | 96% (n=24) | 100% (n=16) |
RN=bedside RN; BS=bladder scanner; APRN=Advanced Practice; US=ultrasound; MD=physician; US oblique=oblique measurement in sagittal view
Significant differences where adequate sample size of at least 5 measures
APRN BS vs APRN US Urine Catheter Volume ≥ 300 ml: p=0.001
APRN BS vs APRN US: Urine Catheter Volume ≥ 550 ml p=0.015
RN BS vs APRN US: Urine Catheter Volume < 150 ml and ascites p=0.021
APRN BS vs APRN US: p=0.037
Discussion
This study identified several key findings. First, abdominal fluid collections contiguous with the bladder remain a confounder for BS bladder volume measurements leading to inaccurate volume estimates. However, BS visualization capability improved recognition of abdominal fluid collections. Second, APRN and MDs were equally accurate when using the US with the oblique measurement in the sagittal axis, while greater differences were seen with the use of horizontal measurements in the sagittal axis. Additionally, BS measurements compared to US had a higher percentage of correctly identified patients who needed catheterization at clinical decision point of ≥ 300 ml. For larger bladder volumes, physicians demonstrated slightly higher accuracy with clinician decision points than APRN measurements using US, although physicians conducted fewer measurements. Finally, the percentage of correct identification of patients who did not need catheterization because of bladder volumes < 150 ml was higher with US than BS in patients with abdominal fluid. We hypothesize that at lower bladder volumes, the confounding effect of abdominal fluid adjacent to the bladder is included in the bladder volume measurement which leads to inaccuracy with the BS.
To reduce indwelling urinary catheter days, a variety of interventions have been examined. Interventions include alternatives to indwelling urinary catheters such as condom catheters and ISC.26 Serial non-invasive measurement of bladder volume with a BS or US technology is recommended in urinary catheter protocols to verify urinary retention before catheterization.3–4 Despite recommendations for a BS, clinical implementation remains low in ICUs.27–30 This study adds important results regarding a potential reason for low use of BSs in ICU patients due to concerns with ascites. BS manufacturers advise against bladder volume measurements in patients with ascites.20 This contraindication is supported by the findings from this study. Patients with AKI often have ascites. With the increase in AKI observed in critically ill patients,31 accurate non-invasive measurements are needed to reduce urinary catheter days
Nurses are generally not taught US techniques for bladder volume measurements. After US education and IRR testing, APRNs in our study demonstrated similar US accuracy as MDs although slightly less accurate at higher volumes. Collaboration with physician US experts was instrumental in APRNs acquisition of US skills. Thus, APRNs can measure bladder volumes with US for patients in whom the BS is inaccurate due to abdominal fluid. However, additional research on nursing accuracy using US is limited. A simplified US technique measuring the largest transverse image of the bladder, either in transverse or sagittal probe position, was conducted to calculate bladder volume. The findings demonstrated feasibility and accuracy on surgical patients with bladder volumes > 600 ml.32 More research on use of this simplified US measurement technique is also needed. US skills are now required for newer BS technology which incorporate direct ultrasound visualization to identify the bladder. Therefore, education of nurses in US techniques should be provided to improve accuracy of both BS and US bladder volume measurements.
Accuracy of any non-invasive bladder volume measurement is ultimately relevant to determine need for catheterization, yet research with clinical decision points is minimal. In a pediatric ICU quality improvement study, the majority of BS volumes were similar to catheterization volumes. However, in two patients, BS volume was greater than calculated capacity volume while catheter volume was less (patients were catheterized without need). In 11 patients, BS volume was less than calculated capacity volume, but catheterization volume exceeded calculated capacity volume. In these 11 patients, they would not have been catheterized but likely would have benefited from a catheterization to prevent incontinence or risk of bladder rupture secondary to urinary retention.33 Findings in this pediatric population and our adult population demonstrate that devices used to measure bladder volumes need to be examined regarding the impact on clinical decision points.
Additionally, we found that MDs and APRNs were generally equally accurate with US using oblique measurement in the sagittal axis of the bladder. However, standardization of the best method of measuring bladder volumes with US is lacking and may vary amongst devices. Investigation of new devices are needed in various ICU patient populations to ensure accuracy across a range of bladder volumes and in the presence of ascites.
The results of this study provide guidance to creating a protocol that incorporates both BS and US devices in order to reduce catheter days in ICU patients. BS technology with direct visualization of the bladder can be used to exclude intra-abdominal fluid collections. If no abdominal fluid is visualized, BS bladder volume measurement should be the first step in measuring bladder volume in ICU patients. In our results, when ascites is not present, the BS performed better than US at bladder volumes > 300 ml. US measurements by either APRN or MD can be used to accurately measure bladder volumes for patients with observed ascites on the BS. Our results suggest that a bladder volume of > 300 ml is the most appropriate volume to set as a clinical decision point for urinary catheterization in ICU patients unable to communicate the need to void as accuracy diminished with volumes ≥ 550 ml as a clinical decision point. Research is needed to evaluate the implementation of a catheter removal protocol incorporating BS and US in patients with AKI and its impact on catheter utilization rates and CAUTI rates.
Limitations
This study had several limitations impacting generalizability including use of a convenience sample of clinicians, single US technology vendor, single BS technology vendor, and patients from a single hospital site. It is possible that other potential accuracy problems associated with BS or US technologies were not identified with the study sample. However, the diversity of the ICU populations across a large institution enrolled in our study likely mitigates this limitation to some degree. Additionally, the results are for two manufactured devices only, and we cannot account for the variance in accuracy across all BS and US devices. The addition of an oblique measurement in the sagittal view after data collection in the first 29 patients may have biased the accuracy of US results for the last 44 patients due to a re-education of data collections on the new process. Last, with a variety of RNs conducting urinary catheterization, it is possible that complete bladder emptying varied with the potential for the gold standard measurement to have variable accuracy.
Conclusions
US and new technology BS provided accurate measurements of bladder volume in ICU patients. When intra-abdominal fluid was present, US was more accurate than BS. Oblique measurements of the bladder in a sagittal axis was more accurate than horizontal measurements to assess bladder volume with US. Incorporating both devices with skilled clinicians (trained in US and BS technology) in a catheter removal protocol may reduce urinary catheter days and ultimately CAUTI rates in ICU patients with low urine output or on dialysis; however more research is needed.
Summary of Key Points.
Removal of indwelling urinary catheters depends on accurate non-invasive bladder volume measurements. Bladder scanners (BS) are commonly used in urinary catheter removal protocols; however, BS use is contraindicated in patients with ascites which is often observed in patients with acute kidney injury. Implications from study findings include:
Learning ultrasound (US) techniques to identify ascites will help nurses correctly visualize the bladder to obtain accurate bladder volume measurements.
US should be used if ascites is present and cannot be eliminated from bladder volume measurement with BS devices.
With current technology, both US and BS devices should be incorporated into urinary catheter removal protocols to prevent unnecessary bladder catheterization or patient discomfort from a distended bladder.
Urinary catheters can safely be removed in patients with oliguric acute kidney injury when accurate non-invasive bladder volume measurement are available with either US bladder visualization with BS or US.
Acknowledgments
The authors would like to acknowledge and thank all of the patients and families who agreed to study participation, bedside nurses who performed timely bladder catheterization of study participants, Gretel McKinley RN, MSN research coordinator, and clinicians who conducted BS or US measurements including RNs Stephanie Banaszynski, Emily Dodd, Charlotte Gibson, Meghan Hudock, Jayme Jones, and Mary Sauer; APRNs Paula Mantia and Ann Petlin; ICU Physician Fellows Jacob Basak, Amjad Musleh, and Jasmine Swaniker. Their assistance led to the successful completion of the study.
The study was conducted at Barnes-Jewish Hospital, St. Louis, MO
Financial Support: This study was supported by a grant from the Institute of Clinical and Translational and Sciences through the Barnes-Jewish Hospital Foundation. Verathon Medical, Inc. provided two bladder scanners for the study.
References
- 1.Lo E, Nicolle LE, Coffin SE, et al. : Strategies to prevent catheter-associated urinary tract infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014;35(5):464–479 [DOI] [PubMed] [Google Scholar]
- 2.Greene MT, Fakih MG, Fowler KE, et al. : Regional variation in urinary catheter use and catheter-associated urinary tract infection: Results from a National Collaborative. Infect Control Hosp Epidemiol. 2014;31(S3):S99–S106 [DOI] [PubMed] [Google Scholar]
- 3.Saint S, Greene T, Krein SL, et al. : A program to prevent catheter-associated urinary tract infection in acute care. New Engl J Med. 2016;374(22):2111–2119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosseland LA, Stubhaug A, Breivak H: Detecting postoperative urinary retention with an ultrasound scanner. ACTA Anaesthesiol Scand. 2002;46:279–282 [DOI] [PubMed] [Google Scholar]
- 5.Palese A, Buchini S, Deroma L, et al. : The effectiveness of ultrasound bladder scanner in reducing urinary tract infections: A meta-analysis. J Clin Nurs. 2010;19:2970–2979 [DOI] [PubMed] [Google Scholar]
- 6.Cutright J: The effect of the bladder scanner policy on the number of urinary catheters inserted. J Wound Ostomy Continence Nurs. 2011;38(1):71–76 [DOI] [PubMed] [Google Scholar]
- 7.Oman KS, Makic MBF, Fink R, et al. : Nurse-directed interventions to reduce catheter-associated urinary tract infections. Am J Inf Control. 2012;40:548–553 [DOI] [PubMed] [Google Scholar]
- 8.Durant DJ: Nurse-driven protocols and the prevention of catheter-associated urinary tract infections: A systematic review. Am J Inf Control. 2017;45:1331–1341 [DOI] [PubMed] [Google Scholar]
- 9.Kelley K, Johnson T, Burgess J, et al. : Effect of implementation of intermittent straight catheter protocol on rate of urinary tract infections in a trauma population. Am Surgeon. 2017;83:747–749 [PubMed] [Google Scholar]
- 10.Meddings J, Rogers MAM, Krein SL, et al. : Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infection: An integrative review. BMJ Qual Saf. 2014;23:277–289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sulzbach-Hoke LM, Schanne LC: Using a portable ultrasound bladder scanner in the cardiac care unit. Crit Care Nurs.1999;19(6):35–39 [PubMed] [Google Scholar]
- 12.Elpern EH, Killeen K, Ketchem A, et al. : Reducing use of indwelling urinary catheters and associated urinary tract infections. Am J Crit Care. 2009;18(6):535–542 [DOI] [PubMed] [Google Scholar]
- 13.Prentice DM, Sona C, Wessman BT et al. : Discrepancies in measuring bladder volumes with bedside ultrasound and bladder scanning in the intensive care unit: A pilot study. J Intensive Care Society. 2018;19(2):122–126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choe JH, Le JY, Lee KS: Accuracy and precision of a new portable ultrasound scanner, the BME-150A, in residual urine volume measurement: a comparison with the bladderscan BVI 3000. Int Urogynecol J. 2007;18:647–644 [DOI] [PubMed] [Google Scholar]
- 15.Skinner DL, Hardcastle TC, Rodseth RN, et al. : The incidence and outcomes of acute kidney injury amongst patients admitted to a level 1 trauma unit. Injury. 2014;45:259–264 [DOI] [PubMed] [Google Scholar]
- 16.Hu J, Chen R, Liu S, et al. : Global incidence and outcomes of adult patients with acute kidney injury after cardiac surgery: A systematic review and meta-analysis. J Cardiothorac Vasc Anesth. 2016;30(1):82–89 [DOI] [PubMed] [Google Scholar]
- 17.Tignanelli CJ, Wiktor AJ, Vatsaas CJ, et al. : Outcomes of acute kidney injury in patients with severe ARDS due to influenza A(H1N1). Am J Crit Care. 2018;27(1):67–73 [DOI] [PubMed] [Google Scholar]
- 18.Schneider AG, Bagshaw SM: Effects of renal replacement therapy on renal recovery after acute kidney injury. Nephron Clin Pract. 2014;127:35–41 [DOI] [PubMed] [Google Scholar]
- 19.Meddings J, Saint S, Fowler KE, et al. : The Ann Arbor criteria for appropriate urinary catheter use in hospitalized medical patients: Results obtained by using the RAND/UCLA appropriateness method. Ann Intern Med. 2015;162:S1–S34 [DOI] [PubMed] [Google Scholar]
- 20.Verathon Bladerscan Prime Plus Operations & Maintenance Manual. May 2019. Available at https://www.verathon.com/product-documentation/ accessed October 2019 [Google Scholar]
- 21.Bih LI, Ho CC, Tsai SJ, Lai YC, Chow W. Bladder shape impact on the accuracy of ultrasonic estimation of bladder volume. Archives of physical medicine and rehabilitation. 1998;79(12):1553–6 [DOI] [PubMed] [Google Scholar]
- 22.Zou GY: Sample size formulas for estimation intraclass correlation coefficients with precision and assurance. Statist Med. 2012;31:3972–3981 [DOI] [PubMed] [Google Scholar]
- 23.Koo TK, Li MY: A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research [published correction appears in J Chiropr Med. 2017;16(4):346]. J Chiropr Med. 2016;15(2):155–163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Janjua QM, Saeed S, Mahmud Q, et al. : Effect of gender and BMI on maximum urine holding capacity of the urinary bladder. Biomedica. 2017;33(2):128–130 [Google Scholar]
- 25.Brouwer TA, Rosier PFWM, Moons KGM, et al. : Postoperative bladder catheterization based on individual bladder capacity. Anesthesiology. 2015;122(1):46–54 [DOI] [PubMed] [Google Scholar]
- 26.Chenoweth C, Saint S: Preventing catheter-associated urinary tract infections in the intensive care unit. Crit Care Clin. 2013;29:19–32 [DOI] [PubMed] [Google Scholar]
- 27.Saint S, Kowalski CP, Kaufman SR, et al. : Preventing hospital-acquired urinary tract infection in the United States: A national study. Clin Infect Dis. 2008;46:243–250 [DOI] [PubMed] [Google Scholar]
- 28.Conway LJ, Pogorzelska M, Larson E, et al. : Adoption of policies to prevent catheter-associated urinary tract infections in United States intensive care unit. Am J Inf Control. 2012;40:705–710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krein SL, Fowler KE, Ratz D, et al. : Preventing device-associated infections in US hospitals: National surveys from 2005 to 2013. BMJ Qual Saf. 2015;24:385–392 [DOI] [PubMed] [Google Scholar]
- 30.Saint S, Greene MT, Kowalski CP, et al. : Preventing catheter-associated urinary tract infection in the United States. JAMA Intern Med. 2013;173(10):874–879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wald R, McArthur E, Adihikari NKJ, et al. : Changing incidence and outcomes following dialysis-requiring acute kidney injury among critically ill adults: A population-based cohort study. Am J Kidney Dis. 2015; 65(6):870–877 [DOI] [PubMed] [Google Scholar]
- 32.Daurat A, Choquet O, Bringuier S, et al. : Diagnosis of postoperative urinary retention using a simplified ultrasound bladder measurement. Anesth Analg. 2015;120(5):1033–1038 [DOI] [PubMed] [Google Scholar]
- 33.Wheeler J, O’Riordan MA, Allareddy V, et al. : Would the use of bedside bladder ultrasound decrease the necessity of invasive bladder catheterization in the pediatric intensive care unit? Clinical Pediatrics. 2015; 54(8):800–802 [DOI] [PubMed] [Google Scholar]