Abstract
Background
In low-and middle-income countries, it is challenging to provide basic health-care services even before the COVID-19 pandemic outbreak. The purpose of this study was to evaluate the early indirect impact of COVID-19 on the utilization of reproductive, maternal, and newborn health services at government health facilities in South West Ethiopia, and its consequences.
Methods
A comparative cross-sectional study was employed. The collected data were entered into Microsoft excel 2010 and then exported to SPSS 25 and R3.5.0 software for analysis. Independent sample t-test and two-sample test of proportion were computed, and the results were presented in text, tables, and graphs. P-value <0.05 was considered statistically significant.
Results
This study showed that there was a significant reduction in mean utilization of antenatal care (943.25 visits vs 694.75 visits), health facility birth (808.75 births vs 619 births), family planning (4744.5 visits vs 3991.25 visits), and newborn immunization (739.5 given vs 528.5 given) between March–June 2019 and March–June 2020. However, there were significant increases in proportion of teenage pregnancy (7.5% vs 13.1%), teenage abortion care user (21.3% vs 28.5%), institutional stillbirth (14% vs 21.8%) and neonatal death (33.1% vs 46.2%) during the same period.
Conclusion and Recommendation
This study showed that utilization of reproductive, maternal, and newborn health-care services was affected by the pandemic with deterioration of maternal and perinatal outcomes. An increase in the proportion of teenage pregnancy who seeks abortion care and the rising cesarean section rate with no improvement in perinatal outcome is a great concern that needs further investigation. Further research is also needed to explore the main reason for an increase in teenage pregnancy, abortion care users, stillbirth, and neonatal death during COVID-19.
Keywords: COVID-19, impact, utilization, outcome, maternal and child health, Ethiopia
Introduction
The World Health Organization (WHO) declared coronavirus diseases-2019 (COVID-19) as a global pandemic on March 11, 2020. On June 30, 2020, more than ten million confirmed cases and more than five hundred thousand deaths, making a fatality rate of 4.95% but in Africa, only 297,290 cases and 6010 deaths were reported, respectively, making a case fatality rate of 2.02%.1
The COVID-19 pandemic had brought unpredicted changes to the daily well-being of people across the globe.2 Many countries had tried to limit the disease transmission through the local or national lockdown. However, health-care institutions were not adequately prepared enough to respond to the pandemic, and this might affect the delivery of basic health-care services including maternal, reproductive, and newborn health-care services especially in countries with a scarce resource.3,4
The WHO has developed an updated guideline to support the country’s preparedness and responses to the COVID-19 pandemic to limit its impact. Giving priority and continuing the basic health-care services is highly recommended along with prevention and control of the COVID-19 pandemic.5 Maternal and child health care and immunization are among the highly recommended health services.6 However, these services are being decreased due to COVID-19 pandemic response in resource-limited countries, and the quality of health-care service delivery has become compromised with an increased risk of deaths, but a reduction of better achievement gained in the past two decades.7
The impact of the pandemic might be more significant during the early response and preparedness measures in low resource countries. Unavailability, inaccessibility, or unaffordability of high quality and timely basic health-care services including maternal and child health care is more common even before the outbreak of the COVID-19 pandemic. Nowadays, travel restrictions inadequate supply of personal protective equipment’s, poor infection control practice redirected manpower might negatively affect the overall health-care delivery system and women’s health in particular.8
A modeling study has predicted that the use of maternal and reproductive health and immunization coverage has been significantly decreased with an increase in additional mortality and morbidity. In this study, a 10% decrease in the coverage of maternal and neonatal health care could result in 28,000 and 168,000 additional maternal and neonatal deaths, respectively.9 Additionally, a similar reduction in utilization of family planning services would result in more than 48 million additional women with the unmet need for modern contraceptives and 15 million women with additional unintended pregnancy.10
Evidence from the Ebola virus outbreak in West Africa in 2014 had shown that the indirect effect of the epidemic on the health-care service delivery system was more pronounced than the diseases itself.11 Maternal and newborn health services were reduced because of an interrupted health-care delivery system and delay of getting treatment due to fear of acquiring the virus from the health institutions.12 Antenatal care, health facility birth, postnatal care, and family planning utilization was significantly decreased by 22%, 8%, 13%, and 6%, respectively, which all contributing to an estimated 3, 600 maternal deaths while the stillbirth and neonatal deaths were slightly more than maternal death (about 4000) which was directly caused by the Ebola virus in the country.13
Findings from this study will be important for all stakeholders at all levels of health-care systems in providing necessary information which might be used to develop a new strategy towards the alleviation of the negative impact of COVID-19 on utilization of reproductive, maternal, and newborn health service, and its consequences. To the best of the investigators’ knowledge, there is no published study investigating the indirect impact of COVID-19 on the use of maternal and reproductive health-care services and newborn immunizations in our study setting. To fill this gap in the scientific literature and respond to the limited evidence, this study was designed to evaluate the early indirect impact of COVID-19 on the utilization and outcomes of reproductive, maternal, and newborn health-care services in governmental health facilities of Bench Sheko, Sheka, Keffa, and West Omo zone, southern Ethiopia.
Methods and Materials
Study Design
A comparative cross-sectional study was employed. A four-month period from March–June 2019 (before COVID-19) was used as a baseline comparator to assess the utilization and outcome of reproductive, maternal, and newborn health-care services. These data were compared with an equivalent four-month period of March–June 2020 (during COVID-19) to evaluate any significant change in utilization and outcome.
Study Area and Period
This study was conducted in governmental health facilities of Bench Sheko, Sheka, Keffa, and West Omo zones in southern Ethiopia. These zones are found in the southern nations, nationalities, and peoples region (SNNPR) of Ethiopia. The study area was selected because the authors observed a decrease in client flow during site selection for clinical practice.
Bench Sheko zone has a total population of 609, 588 within two administrative towns and six rural districts (woredas). It has 21 health centers and one teaching hospital. There is a laboratory and treatment center for COVID-19 in this zone which serves the surrounding zones too. Sheka zone has four rural districts (woredas) and one administrative town. It has one general hospital and 13 health centers. Keffa zone has a total population of more than two million within 10 rural districts (woredas) and one administrative town. It has 44 health centers and one general hospital while the west Omo zone has six rural districts and one administrative town. It has 11 health centers and one primary hospital. Each hospital and health center provides basic health-care services, including maternal and reproductive health-care services, maternal and reproductive health-care services, and newborn immunizations during the COVID-19 pandemic. The data were collected from July 1st–August 1st, 2020.
Study Population
All reproductive age women who received reproductive and maternal health-care services, and/or who visit health facilities for their newborn health-care services at the selected governmental health facilities of Bench Sheko, Sheka, Keffa, and West Omo zone from March–June 2019 and March–June 2020.
Sample Size and Sampling Procedure
All women who visited the selected governmental health facilities for reproductive, maternal, and newborn health-care services during the selected timeline (March-June) in both years were included in the study. The list of all hospitals and health centers was taken from the respective zonal health office and all four hospitals were included in this study as there is only one hospital in each zone while more than one-third of health centers were selected by simple random sampling in each zone. Accordingly, eight and fifteen health centers were selected in Bench Sheko and Keffa zone, respectively, and four health centers were taken from Sheka and West Omo zone. Thirty-one health centers and four hospitals were included in the study.
Study Variables and Operational Definitions
The primary outcome variables were maternal and reproductive health-care service utilization like antenatal care (ANC), health facility birth and postnatal care (PNC), family planning, and newborn immunizations while the secondary outcome variables were teenage pregnancy, teenage abortion, maternal outcomes like cesarean section, maternal complication requiring intensive care unit (ICU) admission and perinatal outcomes like stillbirth, neonatal intensive care unit admission (NICU) and neonatal death.
Antenatal care service utilization was defined as at least one antenatal care visit used by pregnant women at the health center or hospital during their last pregnancy. Health facility birth was defined as mothers used governmental health facilities (hospital or health center) for giving birth while postnatal care service utilization was defined as any visit to a hospital or health center during the postpartum period. Accordingly, if women received the service as per the above definition they were considered as utilized; if they were not received, they were considered as not utilized.
Data Collection and Quality Assurance
The data collection tool (checklist) was extracted from the Ethiopian demographic and health survey, 2016 (EDHS, 2016). The data were collected by reviewing hospital and health centers’ records for each service component. Reproductive health-care service data were collected from family planning and abortion care clinic while maternal and newborn health service data were collected from the antenatal care clinic, labor/delivery room, maternal and neonatal intensive care units, and immunization room. Data collectors were nurses or midwives working in each health facility. Data quality was assured by giving one-day training for data collectors about the purpose of the study, close supervision during data collection, making double entry, and independent analysis.
Data Analysis Procedure
The collected data were entered into Microsoft excel 2010 for ease of cleaning and then exported to SPSS 25 version and R 3.5.0 software for analysis. The reproductive, maternal, and newborn service utilization variables were categorized into six groups: ANC (four indicators), health facility birth (one indicator), postnatal care (one indicator), family planning visit (two indicators), abortion care (one indicator) and newborn immunization (two indicators). An independent t-test was used to evaluate whether there were statistically significant differences in mean utilizations of maternal, reproductive, and newborn health services between March-June 2019 (before COVID-19) and March-June, 2020 (during COVID-19). An independent t-test was used when the variable has continuous or discrete data value with an assumption of normal distribution. Test of normality was checked by histogram. Two sample tests of proportion were also computed for indicators within the main variable to evaluate whether there were statistically significant differences in proportion considering the indicator variables as dichotomous variables. The null hypothesis was that there was no difference in outcome measure from March-June 2019 compared to March-June 2020. When a statistically significant difference was identified, the null hypothesis was rejected. Statistical significance was declared at p-value <0.05.
Results
Reproductive, Maternal, and Newborn Health Services Utilization
This study showed that the overall ANC, health facility birth, PNC, family planning visit, and newborn immunization service utilization were decreased by 27.4%, 23.5%, 29.1%, 15.9%, and 28.5%, respectively, from March-June 2019 to March-June 2020. However, even though not significant abortions care service utilization was increased by 8.5% during the same period. There was a statistically significant reduction in mean utilization of all services except abortion care (Table 1).
Table 1.
Change in Utilization of Reproductive, Maternal and Newborn Health Services During COVID-19 at Governmental Health Facilities of Bench Sheko, Sheka, Keffa and West Omo Zone, Southern Ethiopia, 2020
| Services | March–June 2019 | March–June 2020 | Change | p-value |
|---|---|---|---|---|
| Utilization(Mean ±SD) | Utilization(Mean ±SD) | |||
| Antenatal care visits | 943.25±22.79 visits | 694.75 ±52.24 visits | −258.5 | 0.000 |
| Health facility birth | 808.75±23.11 births | 619 ±58.12 births | −189.75 | 0.001 |
| Postnatal care visits | 435.5 ±20.69 visits | 308.75 ±25.76 visits | −126.75 | 0.001 |
| Family planning visits | 4744.5 ±189.01 visits | 3991.25 ±442.82 visits | −753.25 | 0.020 |
| Abortion care visits | 204 ±20.92 visits | 221.25±17.55 visits | 17.25 | 0.253 |
| Newborn immunization | 739.5±10.66 given | 528.5±38.78 given | −211 | 0.000 |
Abbreviation: SD, standard deviation.
In this study, the service utilization reduction varies across zones. Overall, the service utilization was reduced by 48.2%, 35.6%, 26.4%, and 11.9% in Bench Sheko, Keffa, Sheka, and West Omo zones, respectively. It was shown that Bench Sheko and Keffa zones were most affected followed by Sheka and West Omo zone. Comparing the service utilization reduction by a health facility, hospitals contributed to a greater reduction than health centers. The overall health center services were reduced by more than one-third while the hospital services were reduced by more than 50%.
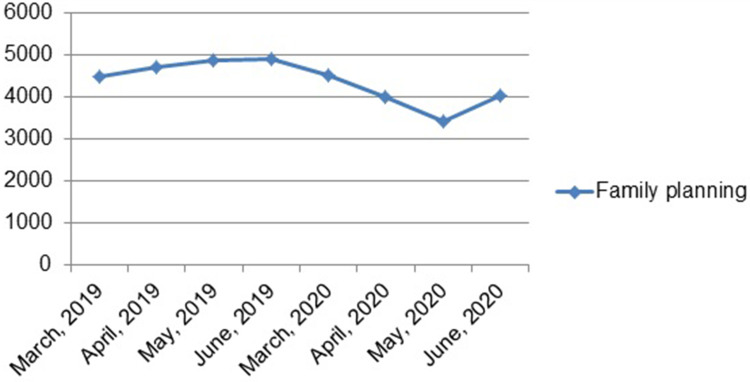
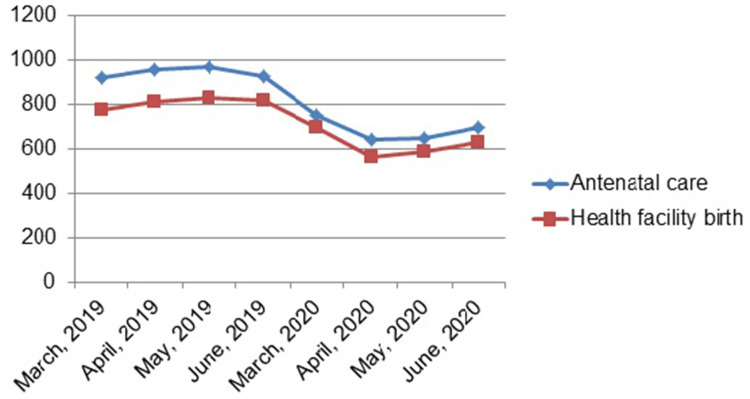
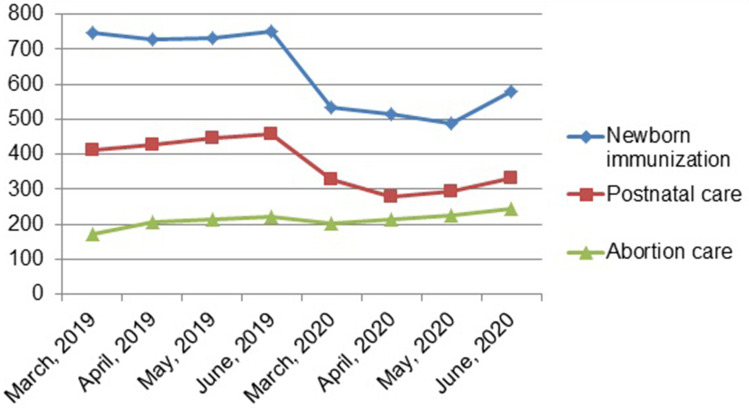
In this study, it was observed that the trend across the months showed a reduction in all services, early from March to May 2020 except abortion care service. There was a sharp rise in family planning by the end of May 2020 (Figure 1). But there was a steady increment in ANC and health facility births (Figure 2), and PNC and abortion care (Figure 3) by the end of May 2020.
Figure 1.
Trends in family planning utilization in equivalent four month periods before and during COVID-19 pandemic at governmental health facilities in South West Ethiopia, 2020.
Figure 2.
Trends in utilization of antenatal care and health facility birth services in equivalent four month periods before and during COVID-19 pandemic at governmental health facilities in South West Ethiopia, 2020.
Figure 3.
Trends in utilization of newborn immunization, postnatal care and abortion care services in equivalent four month periods before and during COVID-19 pandemic at governmental health facilities in South West Ethiopia, 2020.
Proportion of Antenatal Care and Abortion Care Services
The proportion of new clients using antenatal care services significantly decreased during the COVID-19 pandemic. It was decreased by 2.4% (95% CI: −0.466 to −0.001; p=0.037). However, there was a significant increment in the proportion of revisiting clients for antenatal care. Even though not significant, there was also an increment in the proportion of fourth visit antenatal care. The proportion of teenage pregnancy was significantly increased from 7.5% to 13.1% during the same period. It was increased by 5.6% (95% CI: 0.040–0.071; p=0.000). The proportion of teenagers using abortion care services also significantly increased from 21.3% to 28.5% (p=0.001) during the COVID-19 pandemic (Table 2).
Table 2.
Two Sample Test of Proportion for Reproductive, Maternal, and Newborn Health Service Utilization and Outcomes at Governmental Health Facilities in South West Ethiopia, 2020
| Variables | March to June 2019 | March to June 2020 | Change | P-value | ||
|---|---|---|---|---|---|---|
| Total | Proportion | Total | Proportion | |||
| Antenatal care related indicators (n=total clients) | n=3773 | n=2739 | ||||
| New visit client | 1139 | 0.302 | 761 | 0.278 | −0.024 | 0.005 |
| Revisiting clients | 2634 | 0.698 | 1978 | 0.722 | 0.024 | 0.728 |
| Fourth visit clients | 716 | 0.189 | 523 | 0.191 | 0.002 | 0.699 |
| Teenage client | 285 | 0.075 | 359 | 0.131 | 0.056 | 0.000 |
| Family planning visit (n= total family planning clients) | n=18,978 | n=15,965 | ||||
| New clients | 8615 | 0.453 | 7037 | 0.441 | −0.012 | 0.014 |
| Revisiting clients | 10,363 | 0.546 | 8928 | 0.559 | −0.013 | 0.014 |
| Contraceptives (n=total users) | n=18,522 | n=12,337 | ||||
| Emergency pills | 543 | 0.029 | 826 | 0.066 | 0.037 | 0.000 |
| Combined oral contraceptives | 2472 | 0.133 | 2208 | 0.178 | 0.045 | 0.000 |
| Injectable | 11,835 | 0.638 | 7588 | 0.615 | −0.023 | 0.000 |
| Implant | 3006 | 0.162 | 1253 | 0.101 | −0.061 | 0.000 |
| Intrauterine contraceptive device | 666 | 0.035 | 262 | 0.021 | −0.014 | 0.000 |
| Abortion care (n=total user) | n=816 | n=885 | ||||
| Teenage abortion | 174 | 0.213 | 253 | 0.286 | 0.073 | 0.001 |
| Maternal & perinatal outcomes (n=total birth) | n=3235 | n=2476 | ||||
| Cesarean section | 303 | 0.094 | 340 | 0.137 | 0.043 | 0.000 |
| Still birth | 453 | 0.140 | 541 | 0.218 | 0.078 | 0.000 |
| Neonatal intensive care admition | 1563 | 0.483 | 1383 | 0.558 | 0.075 | 0.000 |
| Neonatal death* | 1040 | 0.374 | 1079 | 0.557 | 0.183 | 0.000 |
| Maternal complications requiring ICU admission | 801 | 0.247 | 726 | 0.293 | 0.046 | 0.001 |
| Newborn Immunization (n=total newborn vaccinated) | n=2958 | n=2114 | ||||
| Pentavalent 1 | 915 | 0.309 | 584 | 0.276 | 0.033 | 0.011 |
| Mease l | 658 | 0.222 | 405 | 0.191 | 0.031 | 0.008 |
Note: *Denominator was total number of live births.
Abbreviation: ICU, intensive care unit.
Proportion of Family Planning Service Utilization
The proportion of new clients for family planning service significantly decreased during COVID-19, and it was decreased by 1.2% (95% CI: −0.024 to −0.003; p=0.014). Comparing by methods injectable contraceptive has been the most frequently used method, both before and during COVID-19 pandemic. Even though it has been the most frequently used method, there was a significant reduction in the proportion of clients using injectable contraceptives from 63.8% to 61.5% (p=0.000). The proportion of clients using an implant and intrauterine contraceptive device were also significantly decreased from 16.2% to 10.1% and 3.5% to 2.1%, respectively, during the same periods (p=0.000). In contrast, the proportion of clients using combined oral contraceptive pills and emergency oral contraceptive pills significantly increase from 13.3% to 17.8% and 2.9% to 6.6%, respectively, during the same periods (p=0.000).
Proportion of Maternal and Perinatal Outcomes
There was a significant increase in the proportion of maternal complications requiring intensive care unit (ICU) admission from 24.7% to 29.3% (p=0.001) from March-June 2019 to March-June 2020. During the same period, there was a significant increase in the proportion of institutional neonatal deaths, cesarean section, stillbirths, neonatal intensive care unit (NICU) admission from 33.1% to 46.2%, 9.3% to 13.7%, 14% to 21.8%, and 48.3% to 55.8%, respectively (p=0.000) (Table 2).
Discussion
This study aimed to compare the utilization of reproductive, maternal, and newborn health services and its outcome before and during the COVID-19 pandemic. The impact of an epidemic on the delivery of basic health-care services is not recovered early as the effects are not the direct effect of the epidemic, but an indication of an indirect consequence of the epidemic on the health-care delivery system due to redirected resources and attention to the pandemic itself.6,14,15
In this study, almost all of the services were significantly decreased in the first four months during the COVID-19 pandemic. This finding was in line with previous studies which have reported the early impacts of the COVID-19 pandemic on basic health-care services.10,16–20 This could be explained by women may face problems in trying to access maternal and child health services during their scheduled follow-up visit or they may intentionally miss their visit due to fear of contracting the virus or fear of forced quarantine.21 However, the decrease could be compounded by pre-existing challenges like poor quality of service and poor road conditions and infrastructures.18 This study showed that the service reduction varies across zones. Bench Sheko and Keffa zones were most affected followed by the Sheka zone while the reduction was not significant in the West Omo zone. This could be due to the stay-at-home order issued by the government likely contributed to the disparities in health service utilization as the restriction of movement varies depending on the number of COVID-19 reported cases in the area. In this study, the service reduction was more significant among hospitals than health centers. This might be due to hospitals were being used as diagnostic and treatment centers which might directly or indirectly affect the service delivery or it might be due to higher service delivery in hospitals before the COVID-19 outbreak.
The trends across the services started to fall early from March 2020 when the daily COVID-19 reported cases in Ethiopia were low and only from the center (Addis Ababa). The possible explanation for the early fall of services could be due to the effect of media propaganda (which might have stopped women from using health-care services) about the diseases which make the public fear of disease transmission, whereas the eventual rise could be due to an increased awareness of women about the nature of the disease (route of transmission and its prevention method) which might help them to decrease fear and rumors related to the disease and to visit a health facility.
This study showed that the proportion of new antenatal care visits has significantly decreased during the COVID-19 pandemic. This result was supported by the study finding from northeast Ethiopia, which showed that a significant number of pregnant women has lost or unable to start their antenatal care visit during the COVID-19 pandemic.22 This might be due to restricted movement forwarded as an ongoing COVID-19 pandemic response during the national state of emergency and transportation difficulty as a result may cause delay in reaching health facility or seeking health care.17,21 However, the proportion of fourth ANC visits was almost similar before and during the COVID-19 pandemic. This might be due to women who receive more antenatal care may develop positive healthcare-seeking behavior even in challenging conditions.
In this study, health facility birth and PNC was significantly decreased with an increase in the proportion of women who had a complication at admission during COVID-19. This finding was supported by the study finding done in Nepal which reported a significant reduction in institutional delivery and PNC but an increase in maternal complication during COVID-19.16 This could be explained by women may come to health facility for delivery or PNC if they faced complications unless they would give birth at home during the pandemic.
In this study the proportion of modern contraceptive methods like injectable, implant and intra uterine contraceptive device (IUCD) had significantly decreased, but an increase in uptake of oral contraceptive pills during COVID-19 pandemic. This result was supported by the study finding in South Africa which reported a decline in use of injectable contraceptive methods and increase in use of oral contraceptive pills.23 This might be due to women might dread acquiring a COVID-19 infection while they receive these methods from health-care professionals and they may choose to take oral contraceptive pills as it needs no/less contact with other people.24 Other possible explanation could be their previous myth or misconception about long-term family planning methods.25
In this study, the proportion of teenagers who get pregnant and use abortion care services significantly increased during the COVID-19 pandemic. This finding was supported by the study finding in Kenya, which showed that 59% of pregnancies among teenagers were unintended and 45% of pregnancies end up with severe abortion complications during the COVID-19 pandemic.26 This might be explained by adolescent girls who stayed at home because of closure of school were more prone to sexual abuse including rape even by their parents and their fewer access to family planning services.27 An increase in awareness of reproductive-age women about safe abortion services from time to time may be another possible explanation.
This study showed that the proportion of cesarean section rate was significantly increased during the COVID-19 pandemic which was higher than the standards set by WHO.28 This might be an indication of decreased quality of care in general and/or decreased intrapartum fetal heart rate monitoring during labor in particular, but the reason for an increased cesarean section rate needs further investigation.
Maternal and perinatal mortality can be reduced if pregnant women can access maternal care as set by WHO.29 The proportion of institutional stillbirth was significantly increased in this study. This might be due to the delay of pregnant women with complication to visit a health facility early when they recognized reduced fetal movement or reduced basic obstetric care secondary to staff shortage during COVID-19.30
This study showed that the proportion of neonatal intensive care unit admission and neonatal deaths had significantly increased during the COVID-19 pandemic. This might be an indication of inadequate intrapartum care and/or immediate newborn care practices like kangaroo mother care (KMC) during COVID-19.
This study has its own strength and limitations. As strength, it compared the indirect impact of the COVID-19 pandemic on the utilization and outcome of maternal, reproductive, and newborn health services by taking data from multicenter and at a different level of care (health centers, primary hospital and teaching referral hospital) before and during COVID-19 pandemic. Some of the limitations of this study include the following. First, it was not an observational study so that we are unable to explore the main reason for the decrease in maternal, reproductive, and newborn health services. Second, this study was conducted during the early COVID-19 pandemic period in the country when the reported cases were low as compared with other countries. We anticipate that the service utilization could be further affected as the outbreak continuous so that the result may not be generalizable to other countries and could be interpreted in context. However, this result might be used as an insight how the pandemic indirectly affect the health-care delivery system.
Conclusion and Recommendation
This study showed that utilization of maternal, reproductive, and newborn health-care services was affected by the pandemic with deterioration of the adverse maternal, perinatal outcomes. An increase in the proportion of teenage pregnancy along with abortion care users and the rising cesarean section rate with no improvement in perinatal outcome is a great concern that needs further investigation. Further research is also needed to explore the main reason for an increase in teenage pregnancy, abortion care users, stillbirth, and neonatal death during COVID-19.
Acknowledgment
We would like to thank Mizan-Tepi University research ethical review committee for their approval to do this research. Our special thanks go to each zone and health facility’s administrative body in southwest Ethiopia for their permission for data collection. Finally, we would like to acknowledge our data collectors.
Funding Statement
Any funds or benefits are not received by the authors from industry or elsewhere to undergo this study.
Abbreviations
ANC, antenatal care; COC, combined oral contraceptives; EDHS, Ethiopian Demographic Health Survey; ICU, intensive care unit; IUCD, intra-uterine contraceptive device; NICU, neonatal intensive care unit; PNC, postnatal care; SD, standard deviation; SNNRP, Southern Nation Nationality and Peoples Regions; WHO, World Health Organization.
Data Sharing Statement
The row data used to analyze this study are available from the corresponding author.
Ethical Consideration
Ethical clearance was obtained from Mizan-Tepi University College of medicine and health science, department of nursing. An official letter of cooperation was taken from each health facility to the respective unit. Data sources were free of identification and the data were used for study purposes only. The client informed consent was not needed as the data source was secondary data and this study was conducted in accordance with the Helsinki declaration.
Author Contributions
All authors made a significant contribution to the work during the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article and have agreed on the journal to which the article has been submitted.
Disclosure
The authors report no conflict of interest in this work.
References
- 1.World Health Organization. Coronavirus disease (COVID-19) situation report – 162. World Health Organization; 2020. Available from: https://www.who.int/docs/default. [Google Scholar]
- 2.Cheval S, Mihai Adamescu C, Georgiadis T, et al. Observed and potential impacts of the COVID-19 pandemic on the environment. Int J Environ Res Public Health. 2020;17(11):4140. doi: 10.3390/ijerph17114140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bonardi J-P, Gallea Q, Kalanoski D, et al. Fast and local: how did lockdown policies affect the spread and severity of the covid-19. Covid Econ. 2020;23:325–351. [Google Scholar]
- 4.Trevisanuto D, Weiner G, Lakshminrusimha S. et al. Management of mothers and neonates in low resources setting during covid-19 pandemia. J Matern Fetal Neonatal Med;2020. 1–12. doi: 10.1080/14767058.2020.1784873 [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. COVID-19: operational guidance for maintaining essential health services during an outbreak: interim guidance, 25 March 2020. World Health Organization; 2020. Available from: https://apps.who.int/iris/bitstream/handle/10665/331561. Accessed April30, 2021. [Google Scholar]
- 6.World Health Organization. Maintaining essential health services: operational guidance for the COVID-19 context: interim guidance, 1 June 2020. WHO; 2020. Available from: https://www.who.int/publications/i/item/covid-19-operational-guidance-for-maintaining-essential-health-services-during-an-outbreak. Accessed May1, 2021. [Google Scholar]
- 7.Graham WJ, Afolabi B, Benova L, et al. Protecting hard-won gains for mothers and newborns in low-income and middle-income countries in the face of COVID-19: call for a service safety net. BMJ Glob Health. 2020;5(6):e002754. doi: 10.1136/bmjgh-2020-002754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stein D, Ward K, Cantelmo C. Estimating the potential impact of COVID-19 on mothers and newborns in low- and middle-income countries. Health Policy Plus. 2020. [Google Scholar]
- 9.Roberton T, Carter ED, Chou VB, et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8(7):e901–e08. doi: 10.1016/S2214-109X(20)30229-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riley T, Sully E, Ahmed Z, et al. Estimates of the potential impact of the COVID-19 pandemic on sexual and reproductive health in low- and middle-income countries. Int Perspect Sex Reprod Health. 2020;46:73–76. doi: 10.1363/46e9020 [DOI] [PubMed] [Google Scholar]
- 11.Elston JW, Cartwright C, Ndumbi P, et al. The health impact of the 2014–15 Ebola outbreak. Public Health. 2017;143:60–70. doi: 10.1016/j.puhe.2016.10.020 [DOI] [PubMed] [Google Scholar]
- 12.Elston J, Moosa A, Moses F, et al. Impact of the Ebola outbreak on health systems and population health in Sierra Leone. J Public Health (Bangkok). 2016;38(4):673–678. doi: 10.1093/pubmed/fdv158 [DOI] [PubMed] [Google Scholar]
- 13.Sochas L, Channon AA, Nam S. Counting indirect crisis-related deaths in the context of a low-resilience health system: the case of maternal and neonatal health during the Ebola epidemic in Sierra Leone. Health Policy Plan. 2017;32(suppl_3):iii32–iii39. doi: 10.1093/heapol/czx108 [DOI] [PubMed] [Google Scholar]
- 14.Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Educational UN. Taking action to end domestic violence during COVID-19 pandemics; 2020. Available from: https://en.unesco.org/news/taking-action-end-domestic-violence-during-pandemics. Accessed May1, 2021.
- 16.Ashish K, Gurung R, Kinney MV, et al. Effect of the COVID-19 pandemic response on intrapartum care, stillbirth, and neonatal mortality outcomes in Nepal: a prospective observational study. Lancet Glob Health. 2020;8(10):e1273–e81. doi: 10.1016/S2214-109X(20)30345-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goyal M, Singh P, Singh K, et al. The effect of the COVID‐19 pandemic on maternal health due to delay in seeking health care: experience from a tertiary center. Int J Gynaecol Obstet. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roberton T, Carter ED, Chou VB, et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8(7):e901–e908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saso A, Skirrow H, Kampmann B. Impact of COVID-19 on immunization services for maternal and infant vaccines: results of a survey conducted by imprint—the immunising pregnant women and infants network. Vaccines. 2020;8(3):556. doi: 10.3390/vaccines8030556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wanyana D, Wong R, Hakizimana D. Rapid assessment on the utilization of maternal and child health services during COVID-19 in Rwanda. Public Health Action. 2021;11(1):12–21. doi: 10.5588/pha.20.0057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pant S, Koirala S, Subedi M. Access to maternal health services during COVID-19. Europasian J Med Sci. 2020;2(2):48–52. doi: 10.46405/ejms.v2i2.110 [DOI] [Google Scholar]
- 22.Tadesse E. Antenatal care service utilization of pregnant women attending antenatal care in public hospitals during the COVID-19 pandemic period. Int J Womens Health. 2020;12:1181–1188. doi: 10.2147/IJWH.S287534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adelekan T, Mihretu B, Mapanga W, et al. Early effects of the COVID-19 pandemic on family planning utilisation and termination of pregnancy services in Gauteng, South Africa: March–April 2020. Wits J Clin Med. 2020;2(2):145–152. doi: 10.18772/26180197.2020.v2n2a7 [DOI] [Google Scholar]
- 24.Mickler AK, Carrasco MA, Raney L, et al. Applications of the high impact practices in family planning during COVID-19. Sex Reprod Health Matters. 2021;29(1):1881210. doi: 10.1080/26410397.2021.1881210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Endriyas M, Eshete A, Mekonnen E, et al. Where we should focus? Myths and misconceptions of long acting contraceptives in Southern Nations, Nationalities and People’s Region, Ethiopia: qualitative study. BMC Pregnancy Childbirth. 2018;18(1):1–6. doi: 10.1186/s12884-018-1731-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.International. P. COVID-19: lockdown linked to high number of unintended teen pregnancy in Kenya 2020; 2020. Available from: https://plan-international.org/news/2020-06-25-covid-19-lockdown-linked-high-number-unintended-teen-pregnancies-kenya. Accessed May1, 2021.
- 27.Evans ML, Lindauer M, Farrell ME. A pandemic within a pandemic—intimate partner violence during Covid-19. N Engl J Med. 2020;383(24):2302–2304. doi: 10.1056/NEJMp2024046 [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. WHO statement on caesarean section rates. Geneva: World Health Organization; 2015. Available from: https://apps.who.int/iris/bitstream/handle/10665/161442/WHO_RHR_15.02_eng.pdf?sequence=1. Accessed May1, 2021. [Google Scholar]
- 29.World Health Organization. Pregnant women must be able to access the right care at the right time, says WHO; 2020. Available from: https://www.who.int/en/news-room/detail/07-11-2016-pregnant-women-must-be-able-to-access-the-right-care-at-the-right-time-says-who. Accessed May1, 2021.
- 30.Khalil A, Von Dadelszen P, Draycott T, et al. Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA. 2020;324(7):705–706. doi: 10.1001/jama.2020.12746 [DOI] [PMC free article] [PubMed] [Google Scholar]