Abstract
Background
Delirium in older hospital inpatients appears to be associated with various adverse outcomes. The limitations of previous research on this association have included small sample sizes, short follow-up periods and lack of consideration of important confounders or modifiers, such as severity of illness, comorbidity and dementia. The objective of this study was to determine the prognostic significance of delirium, with or without dementia, for cognitive and functional status during the 12 months after hospital admission, independent of premorbid function, comorbidity, severity of illness and other potentially confounding variables.
Methods
Patients 65 years of age and older who were admitted from the emergency department to the medical services were screened for delirium during their first week in hospital. Two cohorts were enrolled: patients with prevalent or incident delirium and patients without delirium, but similar in age and cognitive impairment. The patients were followed up at 2, 6 and 12 months after hospital admission. Analyses were conducted for 4 patient groups: 56 with delirium, 53 with dementia, 164 with both conditions and 42 with neither. Baseline measures included delirium (Confusion Assessment Method), dementia (Informant Questionnaire on Cognitive Decline in the Elderly), physical function (Barthel Index [BI] and premorbid instrumental activities of daily living, IADL), the Mini-Mental State Examination (MMSE), comorbidity, and physiologic and clinical severity of illness. Outcome variables measured at follow-up were the MMSE, Barthel Index, IADL and admission to a long-term care facility.
Results
After adjustment for covariates, the mean differences in MMSE scores at follow-up between patients with and without delirium were –4.99 (95% confidence interval [CI] –7.17 to –2.81) for patients with dementia and –3.36 (95% CI –6.15 to –0.58) for those without dementia. At 12 months, the adjusted mean differences in the BI were –16.45 (95% CI –27.42 to –5.50) and –13.89 (95% CI –28.39 to 0.61) for patients with and without dementia respectively. Patients with both delirium and dementia were more likely to be admitted to long-term care than those with neither condition (adjusted odds ratio 3.18, 95% CI 1.19 to 8.49). Dementia but not delirium predicted worse IADL scores at follow-up. Unadjusted analyses yielded similar results.
Interpretation
For older patients with and without dementia, delirium is an independent predictor of sustained poor cognitive and functional status during the year after a medical admission to hospital.
Delirium (acute confusional state) is a mental disorder characterized by acute onset, altered level of consciousness, fluctuating course and disturbances in orientation, memory, thought and behaviour.1 It occurs in up to 51% of older patients who have been admitted to hospital2 and is related to several adverse outcomes, including longer mean length of hospital stay, poor functional status, need for institutional care and death.3
Five controlled studies have investigated the effects of delirium in older hospital inpatients on cognitive and functional status after discharge from hospital.4,5,6,7,8 The limitations of these studies have included small sample sizes, short follow-up periods (only 2 studies followed patients for more than 3 months after discharge4,8) and limited number of outcomes studied. Important confounding variables such as severity of illness and comorbidity were not always controlled; not all studies measured dementia, a risk factor for delirium;9 and the joint effects of delirium and dementia on functional status outcomes were not considered. Finally, the baseline for assessment of function differed: in some studies, a premorbid baseline was used (assessed during a specified period before hospital admission), whereas in others baseline function was as assessed during the admission. The choice of baseline is important because delirium can affect function during hospital stay, whereas dementia may affect premorbid function.
We studied the prognosis of delirium among older medical inpatients and found that delirium is a marker for death during the year after the hospital stay, particularly among patients without dementia.10 In this paper, we examine the prognostic significance of delirium, with and without dementia, for cognitive and functional status up to 12 months after admission to hospital.
Methods
Study subjects were enrolled at a 400-bed, university-affiliated, primary acute care hospital in Montreal during the period February 1997 to January 1999. The study design was a prospective, observational study of 2 cohorts: the delirium cohort, in whom prevalent or incident delirium was detected during the first week of the hospital stay, and a cohort in whom delirium was not detected. Each cohort was further subdivided into those with and without dementia. The study was conducted at the same time as a randomized trial of the detection and treatment of delirium (unpublished data), and a subgroup of the delirium cohort also participated in that trial.
Patients 65 years of age and older who were admitted from the emergency department to the medical services were eligible for the studies. We excluded patients with a primary diagnosis of stroke, those admitted to the oncology unit, those admitted to the intensive care unit or cardiac monitoring unit unless they were transferred to a medical ward within 48 hours of admission, and those who did not speak English or French. At admission and during the first week of the hospital stay, a research nurse screened eligible patients for delirium using the Short Portable Mental Status Questionnaire (SPMSQ)11 and a review of the nursing notes. She also administered the Confusion Assessment Method (CAM)12 for those whose initial SPMSQ score was 3 or more, whose SPMSQ score at repeat screening increased by at least 1 point from the first assessment, or whose nursing notes indicated symptoms of delirium. Members of the cohort without delirium were selected from patients screened for delirium but free of this condition. To balance the distributions of age and prior cognitive impairment among patients with and without delirium, a stratified sampling method, based on the patient's age and initial SPMSQ score, was used. Thus, patients without delirium were selected from those 70 years of age and over, and only a subsample of patients with SPMSQ scores of less than 3 were included. Patients with an SPMSQ score of 4 or less gave informed consent to participate in the study; those with a score of 5 or more assented to participation and a relative provided written consent. The study was approved by the hospital's Research Ethics Committee.
A research assistant, blinded to study group, assessed the patients at enrolment and at 2, 6 and 12 months after admission; the research assistant also interviewed a family member. The 2-month follow-up took place in hospital for patients who had not been discharged or, for those who had been discharged, at home 8 weeks after discharge. The mean time from enrolment to the 2-month follow-up was 58 (standard deviation 20) days and was similar in the 4 study groups. In most cases the 6- and 12-month follow-ups were conducted at home.
Delirium was diagnosed by means of the CAM,12 a structured instrument validated against the clinical judgement of a psychiatrist, which assesses 10 symptoms of delirium specified in the revised 3rd edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R) (similar to the DSM-IV criteria) specifically acute onset, fluctuating course, inattention, disorganized thinking, altered level of consciousness, disorientation, memory impairment, perceptual disturbances, psychomotor activity and sleep–wake disturbance. We have previously reported that a nurse-administered CAM, validated against a consensus diagnosis, has sensitivity of 89% and specificity of 100%.13 Prevalent delirium was diagnosed if the patient met the criteria for delirium at admission and incident delirium if the criteria were met during the week after admission.
The presence of dementia was assessed on the basis of the 16-item Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE), an instrument with high internal consistency and test–retest reliability.14,15,16 In validation studies against clinical diagnosis, in which dementia was defined by a score of 3.38 or more, the sensitivity varied between 75% and 91% and the specificity between 65% and 82%.14,15 A French version tested in Quebec, in which dementia was defined by a score of 3.6 or more, had sensitivity of 75% and specificity of 95%.17 We used a cut-off value of 3.5 in defining dementia, midway between the cut-off values used previously.
Three measures of illness burden and severity were used. Comorbidity at admission was assessed by chart review with the Charlson Comorbidity Index (CCI), higher scores indicating greater comorbidity.18 Acute physiologic severity of illness was assessed with the Acute Physiology Score (APS), which is derived from the Acute Physiology and Chronic Health Evaluation (APACHE) II scale and was coded (on the basis of chart review) according to laboratory and clinical measures taken on or just before the date of enrolment; the APS score ranges from 0 (no impairment) to 44 (severe impairment).19 Clinical severity of illness was assessed by the research nurse at enrolment; the score ranges from 1 (minimal) to 9 (most severe).20,21 Finally, demographic variables (age, sex, marital status and living arrangement) and enrolment in the treatment arm of the randomized trial were recorded in study baseline forms.
The Mini-Mental State Examination (MMSE),22 a widely used instrument with established reliability and validity,23 was rated by the research assistant at enrolment and follow-up. The MMSE score ranges from 0 to 30, lower scores indicating greater cognitive impairment.
The Barthel Index (BI), which measures activities of daily living,24 was rated by the research assistant at enrolment and at follow-up, usually during a home visit. The BI score was based on observation, when possible; otherwise it was based on judgement. At 6 months, for example, the proportion of subjects whose BI scores were based on observation ranged from 1% for bathing to 87% for ambulation. We used the modified scoring suggested by Shah and associates;5 25 and inter-rater reliability (Pearson's r) was 0.99.26
The Instrumental Activities of Daily Living (IADL) questionnaire from the Older American Resources and Services project,27 administered to an informant, was used to assess function; the scores for this scale range from 0 (completely dependent) to 16 (completely independent). At baseline, the IADL scale was rated for the premorbid period (i.e., before the current illness but not more than 1 month before hospital admission).8 - -
Admission to a long-term care facility was determined by the research assistant during each follow-up contact and was defined as residence in a nursing home or long-term care hospital at 12 month follow-up or at the last follow-up before death or withdrawal from the study, among patients not resident in such a facility at enrolment.
We created a 4-category variable (delirium alone, dementia alone, both and neither) to study the individual and combined effects of delirium and dementia on the outcome variables. Pairwise comparisons of the 4 categories were used to make inferences about the effects of delirium and dementia on the various outcomes.
We analyzed changes over time in MMSE, BI and IADL scores using general linear models for longitudinal data with an autoregressive error structure.29 MMSE and BI scores were potentially available for all 4 time points, whereas IADL scores were potentially available only at enrolment and the 6- and 12-month follow-ups, because many patients were still hospitalized at 2 months. For each outcome we first fitted a model that included an interaction between subject group and time. If this interaction was statistically significant (i.e., there was a differential rate of change in the outcome in the 4 study groups), we fitted a separate linear regression model at each time point. Covariates in these analyses were age, sex, marital status, education, patient's living arrangement, comorbidity (measured by CCI), physiologic severity (measured by APS) and clinical severity. A treatment group covariate was added to the multivariate regression models to adjust for the possible effect of the intervention on any of the outcomes. This variable was not a statistically or clinically significant predictor of any of the outcomes and hence was not included in the final analyses. Our primary analyses used all available data; we also conducted secondary analyses with data for patients who had completed all potential assessments of each measure. In our primary analyses of the MMSE and BI scores, we did not control for the baseline level of each score, because these measures, determined in hospital, could be affected by the presence of delirium. We also did not control for premorbid IADL, as this measure is known to be affected by the presence of dementia, an independent variable in the study.23 However, we conducted secondary analyses in which we adjusted for the premorbid IADL score.
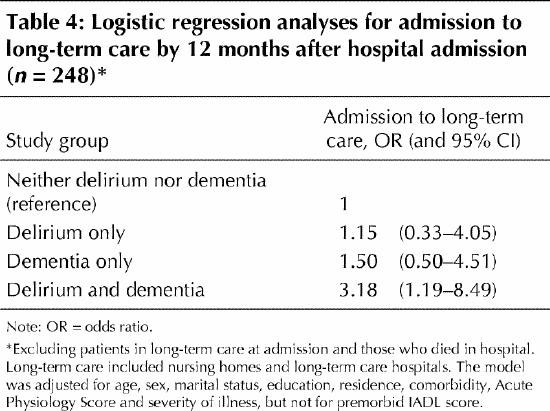
After excluding patients who had been in a long-term care facility at baseline and who died before hospital discharge, we used multiple logistic regression analysis to investigate the effect of the 4-category delirium–dementia variable on admission to long-term care, adjusting for the same set of covariates as for the analyses of the other outcomes.
Statistical tests were deemed significant if the 2-sided p value was less than 0.05.
Results
During the study enrolment period, a total of 4085 patients were admitted to medical services, of which 1552 (38%) were screened for delirium. The reasons for exclusion were admission to oncology (452), admission to the intensive care or coronary care unit (377), transfer to long-term care (332), language barrier (301), stroke (289), not sampled or missed (181), refused screening (164), previously enrolled in the study (127), transferred or discharged (113), communication problem (105), residence outside geographic area (69), death (20) and other (3). Of the 1552 patients screened, 243 with a diagnosis of delirium and 118 without delirium were enrolled in the study. Of these, we excluded 23 patients with delirium and 23 without delirium because data on dementia status or education (or both) were missing (because of failure to interview an informant), which left 220 patients with delirium and 95 patients without delirium in the study sample. By 12 months, 93 patients with and 14 without delirium had died, and 7 patients with and 7 without delirium had withdrawn from the study or could not be contacted. Among the 220 patients with delirium, 30 (14%) had incident delirium and 190 (86%) had prevalent delirium.
At enrolment, there were significant differences between the 4 patient groups with respect to age, sex, living arrangement and all measures of function and severity of illness (Table 1). Figs. 1-3 show changes over time in unadjusted MMSE, BI and IADL scores, respectively, determined from all available data; Table 2 presents the results of pairwise comparisons for the 4 patient groups. Similar results were obtained when data from subjects with complete data at all time points were graphed (not shown). Results of the regression analyses, which were adjusted for covariates, are displayed in Table 3.
Table 1
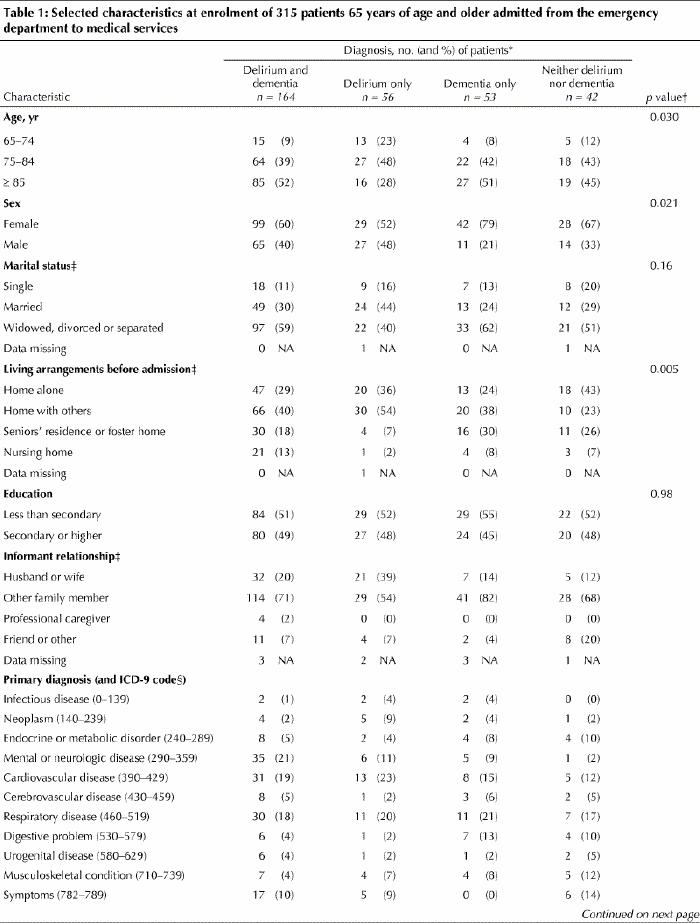
Table 1 continued
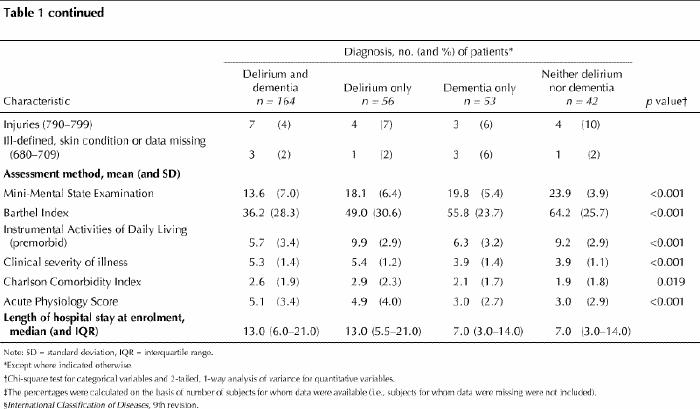
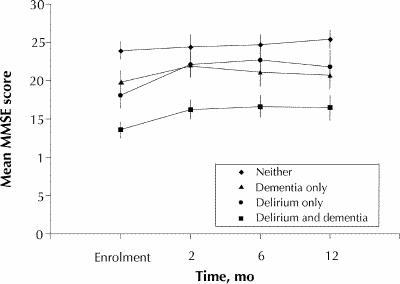
Fig. 1: Mean score (and 95% confidence interval [CI]) for the Mini-Mental State Examination (MMSE) at enrolment and follow-up, according to delirium and dementia status at enrolment. The p values for 2-sided t-tests of pairwise differences in means are presented in Table 2.
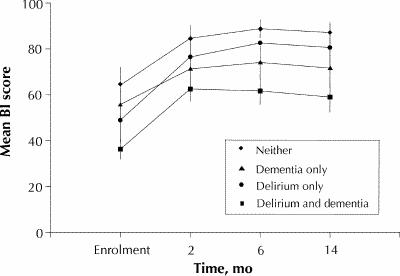
Fig. 2: Mean score (and 95% CI) for Barthel Index at enrolment and follow-up, according to delirium and dementia status at enrolment. The p values for 2-sided t-tests of pairwise differences in means are presented in Table 2.
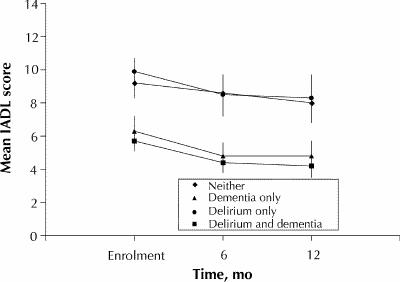
Fig. 3: Mean score (and 95% CI) for Instrumental Activities of Daily Living (IADL) at enrolment and follow-up, according to delirium and dementia status at enrolment. The p values for 2-sided t-tests of pairwise differences in means are presented in Table 2.
Table 2
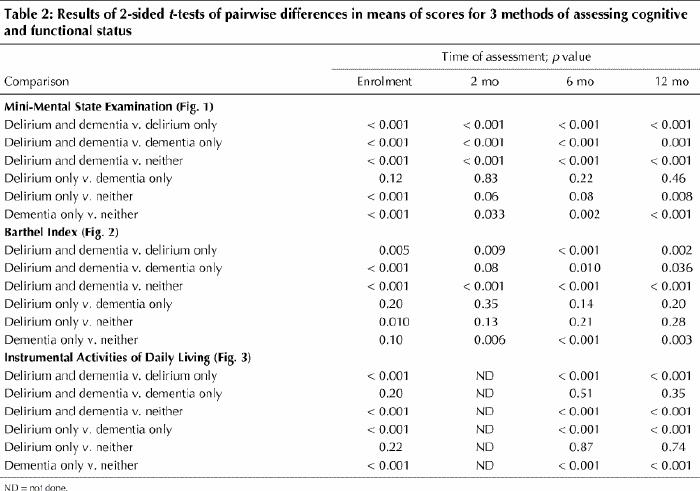
Table 3
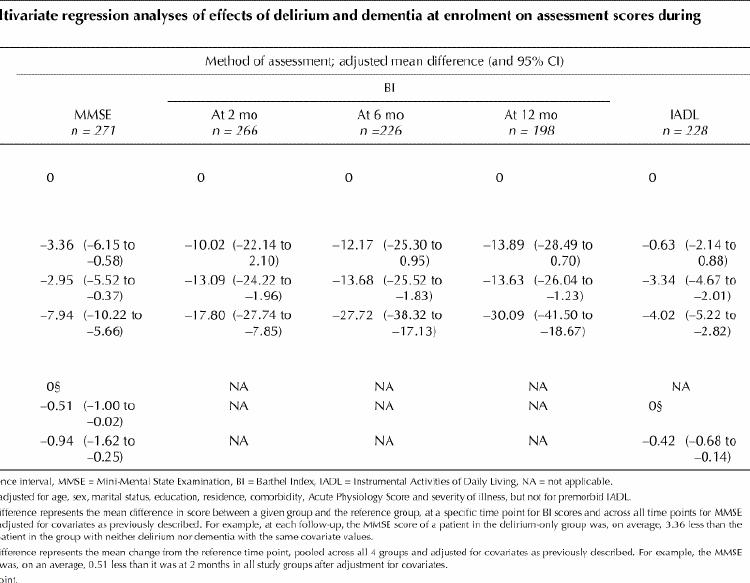
Over time, patients with both delirium and dementia had the worst MMSE scores and those with neither condition had the best scores (Fig. 1). At enrolment, patients with delirium only had worse MMSE scores than those with dementia only, but patients with delirium only showed more improvement at follow-up than those with dementia only (Fig. 1). After adjustment for covariates, all 4 study groups showed small but statistically significant declines in MMSE scores from 2 to 6 and 12 months (Table 3). For example, after adjustment for covariates, the mean MMSE scores for all study groups at 6 and 12 months changed by –0.51 (95% confidence interval [CI] –1.00 to –0.02) and –0.94 (95% CI –1.62 to –0.25) relative to the scores at 2 months. There were no significant interactions between study group and time, which indicates that there were no differential changes among the 4 groups between 2 and 12 months. Finally, the effect of delirium on MMSE scores at follow-up was statistically significant among patients with and without dementia: the adjusted mean difference in MMSE scores between patients with and without delirium was –4.99 (95% CI –7.17 to –2.81) among patients with dementia and –3.36 (95% CI –6.15 to –0.58) among those without dementia.
Descriptive results suggest changes over time in the BI score similar to those for the MMSE. At all 3 follow-up times, patients with dementia, with or without delirium, had significantly lower BI scores than those with neither delirium nor dementia (Fig. 2). Separate linear models are presented for the BI score at each of the 3 follow-up times, because of statistically significant interactions between study group and time (Table 3). After adjustment for covariates, all 4 study groups showed small but statistically significant declines in mean BI scores from 2 to 6 and 12 months. Finally, the effect of delirium on BI scores at follow-up, although similar in magnitude among patients with and without dementia, was statistically significant only in the former group: at 12 months, the adjusted mean difference in BI scores between patients with and without delirium was –16.45 (95% CI –27.42 to –5.50) among patients with dementia and –13.89 (95% CI –28.39 to 0.61) among those without dementia.
Over time, the IADL scores declined steadily in all groups; furthermore, the scores for the 2 groups with dementia were consistently about 4 points lower than those for the 2 groups without dementia (Fig. 3). After adjustment for covariates, all 4 study groups showed small but statistically significant declines in IADL scores between 6 and 12 months (Table 3). The regression model also confirmed the significant effect of dementia but not delirium on IADL scores at follow-up (6 and 12 months).
Significant covariates not shown in Table 3 that predicted worse MMSE, BI and IADL scores at follow-up included residence in a long-term care facility at baseline (affecting MMSE, BI and IADL), lower education (MMSE), older age (MMSE) and greater clinical severity (BI at 2 months only).
Among 248 patients at risk of admission to long-term care (after exclusion of 29 patients residing in a nursing home at enrolment and 38 patients who died before discharge) the numbers of each group admitted to long-term care by 12 months were as follows: 7 (19%) of 37 patients with neither condition, 7 (16%) of 44 patients with delirium alone, 12 (26%) of 46 with dementia alone and 47 (39%) of 121 with both conditions. There was no significant effect of delirium among patients with or without dementia. This was true even after adjustment for covariates; the odds ratio for admission to long-term care by 12 months, in a comparison of patients with and without delirium, was 2.12 (95% CI 0.91 to 4.95) among patients with dementia and 1.15 (95% CI 0.33 to 4.05) among those without dementia. However, both adjusted and unadjusted analyses showed that, in comparison with patients with neither delirium not dementia, the increase in the odds of admission to long-term care was statistically significant among patients with both conditions but not among patients with either delirium or dementia alone (Table 4). The only significant covariate in this model was residence in a seniors' residence or foster home, which was associated with increased odds of admission to long-term care (data not shown).
Table 4
The inclusion of premorbid IADL scores in the regression models described above (not shown) had the expected result of reducing the effect of dementia, with or without delirium, on the study outcomes. However, the effect of delirium on these outcomes was unchanged.
All of the analyses reported above included all data available at each time and were repeated for the patients for whom we had complete follow-up data; the parameter estimates of the regression models remained similar to those obtained in the earlier analyses.
Interpretation
Our results indicate that, among survivors, both delirium and dementia in older medical inpatients are associated with significantly worse physical and cognitive status during the 12 months after admission, after adjustment for comorbidity, severity of illness and other relevant covariates. Of the 2 conditions, dementia predicted these outcomes more consistently. However, among patients with and without dementia, delirium predicted worse MMSE and BI scores at both 6 and 12 months after admission. Delirium also increased the odds of admission to long-term care among patients with dementia. The inclusion of baseline IADL scores in the regression models reduced the effect of dementia on the outcomes, as expected, but did not reduce the effect of delirium. Thus, our results indicate that delirium was not associated with a differential rate of functional decline but with higher levels of disability and cognitive impairment that were sustained during the 12-month follow-up period.
Five controlled studies have investigated the effects of delirium on postdischarge cognitive and functional status. In a study of medical inpatients 70 years of age and older, admitted from the community and excluding cases of cancer and severe dementia, patients with prevalent or incident delirium were followed for up to 2 years.4 Although at 6-month follow-up there was little difference between patients with and without delirium with respect to cognitive and physical function, delirium was a significant predictor of a composite outcome measure - being both alive and independent at 2-year follow-up - after adjustment for initial severity of illness and comorbidity. In a subsample of patients with high baseline cognitive performance, those with delirium had greater subsequent cognitive decline than those without delirium. In a study of patients with incident delirium (20% of whom had previous cognitive impairment) and patients without any form of delirium, after adjustment for premorbid level of function, delirium but not dementia predicted worse functional status at 3 month follow-up.5 Delirium in a mixed medical and surgical population was not associated with differential change in basic activities of daily living status from 2 weeks before admission to 90 days after discharge.6 Another study reported that delirium was a significant predictor of functional decline, both at hospital discharge and 3 months after discharge, after adjustment for covariates, including premorbid IADL, severity of illness and dementia.7 Dementia was defined as cognitive impairment in the absence of acute onset or fluctuations, but it is unclear how this measure was applied to patients with both dementia and delirium. Most recently, hospital inpatients with delirium were reported to be at increased risk of experiencing dementia over the following 3 years.8
Our results confirm and extend those of previous research showing an association between delirium and subsequent level of independence in basic activities of daily living4,5,7,31 and of cognitive function,4 demonstrating that these effects persist up to 12 months after diagnosis. Moreover, we found that delirium was associated with poor cognitive and functional status outcomes among patients with and without dementia.
Our study had 4 strengths. It incorporated 2 important methodologic improvements over previous studies, a larger sample size and longer follow-up periods, and it controlled for 2 important confounding variables, a comorbidity index and a measure of dementia.
Our study had 3 potential limitations. First, our original sample-size calculations (which did not account for the extra information available from repeated measurements) indicated that about 55 subjects were required in each of the 2 cohorts (with and without delirium) to detect a clinically meaningful difference of 3 points in the MMSE and that 90 subjects were required in each cohort to detect a clinically meaningful difference of 10% in the BI scores (with 80% power and 2-sided type I error of 5%). For this paper, we thought it important to stratify the 2 cohorts (with and without delirium) into patients with and without dementia. Thus, on the basis of our original calculations, we had a sufficient sample size to detect a clinically meaningful difference between any 2 groups on the MMSE score. However, we may not have had a sufficient sample size to detect differences between some groups on the BI score. A second limitation is that our instrument for identifying dementia, the IQCODE, may yield variable results for patients with delirium. The IQCODE asks informants to rate behavioural change that took place from over 5 years previously until immediately before the illness that led to hospital admission; informants may have confused the acute behavioural changes of delirium with the longer-term changes associated with dementia. Finally, we found that delirium was associated with one functional measure, the BI, but not with another, the IADL. There are 2 possible reasons for this finding. First, the rating method for the BI may be more sensitive to change than that used for the IADL.25 Second, the BI was rated on the basis of observations and the judgement of the research assistant, an experienced nurse, whereas the IADL was rated on the basis of proxy reports, which may differ systematically from reports made by patients themselves or by observers.31
There are 3 possible explanations for the negative long-term outcomes associated with delirium. First, some symptoms of delirium (e.g., inattention) may persist long after resolution of the delirium episode (perhaps related to chronic physical illness or delayed neurophysiologic homeostasis) and result in cognitive and functional impairment. Second, irreversible neuronal dysfunction or selective neuronal death, consequent to the episode of delirium, may account for the new cognitive and functional deficits. Third (and the most intriguing possibility), delirium in this population may represent a chronic disorder. Delirium is reportedly a risk factor for dementia;8 both delirium and dementia have been attributed to reduced cerebral metabolism, deficits in cholinergic transmission, inflammation or disturbances in neuronal systems that regulate response to stress.32 Delirium, the persistent cognitive and functional impairment reported in this study, and dementia may be the result of a common underlying illness.
In conclusion, we have found that delirium is an important prognostic marker for functional and cognitive status for at least 12 months after admission among patients with and without dementia. In particular, delirium in patients with dementia increases the likelihood of transfer to a long-term care institution. Thus, prevention of delirium through established protocols has the potential to improve the long-term outcomes of hospital admission among older patients.33 Detection of delirium may also be useful for identifying patients who may benefit from additional services in hospital and after discharge.
Footnotes
This article has been peer reviewed.
Acknowledgements: This research was supported by grants from the Medical Research Council of Canada (MA14709), the Fonds de la Recherche en Santé du Québec (980892) and St. Mary's Hospital Center (SMH9627).
Competing interests: None declared.
Correspondence to: Dr. Jane McCusker, Department of Clinical Epidemiology and Community Studies, St. Mary's Hospital, 3830 ave. Lacombe, suite 2508, Montreal QC H3T 1M5; 514 734-2652; jane.mccusker@mcgill.ca
References
- 1.Lipowski Z. Delirium in geriatric patients. In: Delirium: acute confusional states. New York: Oxford University Press; 1990. p. 413-41.
- 2.Levkoff S, Cleary P, Liptzin B, Evans D. Epidemiology of delirium: an overview of research issues and findings. Int Psychogeriatr 1991;3(2):149-67. [DOI] [PubMed]
- 3.Cole M, Primeau F. Prognosis of delirium in elderly hospital patients. CMAJ 1993;149:41-6. [PMC free article] [PubMed]
- 4.Francis J, Kapoor WN. Prognosis after hospital discharge of older medical patients with delirium. J Am Geriatr Soc 1992;40:601-6. [DOI] [PubMed]
- 5.Murray AM, Levkoff SE, Wetle TT, Beckett L, Cleary PD, Schor JD, et al. Acute delirium and functional decline in the hospitalized elderly patient. J Gerontol 1993;48(5):M181-6. [DOI] [PubMed]
- 6.Pompei P, Foreman M, Rudberg MA, Inouye SK, Braund V, Cassel CK. Delirium in hospitalized older persons: outcomes and predictors. J Am Geriatr Soc 1994;42:809-15. [DOI] [PubMed]
- 7.Inouye S, Rushing J, Foreman M, Palmer R, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med 1998;13:234-42. [DOI] [PMC free article] [PubMed]
- 8.Rockwood K, Cosway S, Carver D, Jarrett P, Stadnyk K, Fisk J. The risk of dementia and death after delirium. Age Ageing 1999;28:551-6. [DOI] [PubMed]
- 9.Élie L, Cole M, Primeau F, Bellavance F. Delirium risk factors in elderly hospitalized patients. J Gen Intern Med 1998;13:204-12. [DOI] [PMC free article] [PubMed]
- 10.McCusker J, Cole M, Abrahamowicz M, Primeau F, Belzile É. Delirium predicts 12-month mortality. Arch Intern Med 2000. [DOI] [PubMed]
- 11.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 1975;23(10):433-41. [DOI] [PubMed]
- 12.Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990;113:941-8. [DOI] [PubMed]
- 13.Zou Y, Cole MG, Primeau FJ, McCusker J, Bellavance F, Laplante J. Detection and diagnosis of delirium in the elderly: Psychiatrist diagnosis, confusion assessment method or consensus diagnosis? Int Psychogeriatr 1998;10(3):303-8. [DOI] [PubMed]
- 14.Jorm A. A short form of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): development and cross-validation. Psychol Med 1994;24:145-53. [DOI] [PubMed]
- 15.Jorm AF, Broe AG, Creasey H, Sulway MR, Dent O, Fairley MJ, et al. Further data on the validity of the informant questionnaire on cognitive decline in the elderly (IQCODE). Int J Geriatr Psychiatry 1996;11:131-9.
- 16.Jorm A, Christensen H, Henderson A, Jacomb PA, Korten A, Mackinnon A. Informant ratings of cognitive decline of elderly people: relationship to longitudinal change on cognitive tests. Age Ageing 1996;25:125-9. [PubMed]
- 17.Law S, Wolfson C. Validation of a French version of an informant-based questionnaire as a screening test for Alzhemeir's disease. Br J Psychiatr 1995; 167:541-4. [DOI] [PubMed]
- 18.Charlson M, Pompei P, Ales K, MacKenzie R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40(5):373-83. [DOI] [PubMed]
- 19.Knaus W, Draper E, Wagner D, Zimmerman J. APACHE II: a severity of disease classification system. Crit Care Med 1985;13(10):818-29. [PubMed]
- 20.Charlson M, Sax F, MacKenzie R, Fields S, Braham R, Douglas R. Assessing illness severity: Does clinical judgment work? J Chronic Dis 1986;39(6):439-52. [DOI] [PubMed]
- 21.Inouye S, Viscoli C, Horwitz R, Hurst L, Tinetti M. A predictive model for delirium in hospitalized elderly medical patients based on admission characteristics. Ann Intern Med 1993;119(6):474-81. [DOI] [PubMed]
- 22.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189-98. [DOI] [PubMed]
- 23.Tombaugh TN, McIntyre NJ. The Mini-Mental State Examination: a comprehensive review. J Am Geriatr Soc 1992;40(9):922-35. [DOI] [PubMed]
- 24.Mahoney FI, Barthel DW. Functional evaluation: the Barthel Index. Md State Med J 1965;14(2):61-5. [PubMed]
- 25.Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel index for stroke rehabilitation. J Clin Epidemiol 1989;42(8):703-9. [DOI] [PubMed]
- 26.Shinar D, Gross C, Brohstein K, Licata-Gehr EE, Eden DT, Cabrera AR, et al. Reliability of the Activities of Daily Living Scale and its use in telephone interview. Arch Phys Med Rehabil 1987;68(10):723-8. [PubMed]
- 27.Fillenbaum G. Multidimensional functional assessment: the OARS methodology — a manual. 2nd ed. Durham (NC): Duke University, Center for the Study of Aging and Human Development; 1978.
- 28.McCusker J, Bellavance F, Cardin S, Belzile É. Validity of an activities of daily living questionnaire among older patients in the emergency department. J Clin Epidemiol 1999;52(11):1023-30. [DOI] [PubMed]
- 29.Jenrich R, Schluchter M. Unbalanced repeated-measures models with structured covariance matrices. Biometrics 1986;42:805-20. [PubMed]
- 30.O'Keeffe S, Lavan J. The prognostic significance of delirium in older hospital patients. J Am Geriatr Soc 1997;45:174-8. [DOI] [PubMed]
- 31.Magaziner J, Zimmerman S, Gruber-Baldini A, Hebel J, Fox K. Proxy reporting in five areas of functional status: comparison with self-reports and observations of performance. Am J Epidemiol 1997;146(5):418-28. [DOI] [PubMed]
- 32.Eikelenboom P, Hoogendijk WJ. Do delirium and Alzheimer's dementia share specific pathogenetic mechanisms? Dement Geriatr Cogn Disord 1999; 10:319-24. [DOI] [PubMed]
- 33.Inouye S, Bogardus S, Charpentier P, Leo-Summers L, Acampora D, Holford TR, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med 1999;340(9):669-720. [DOI] [PubMed]


