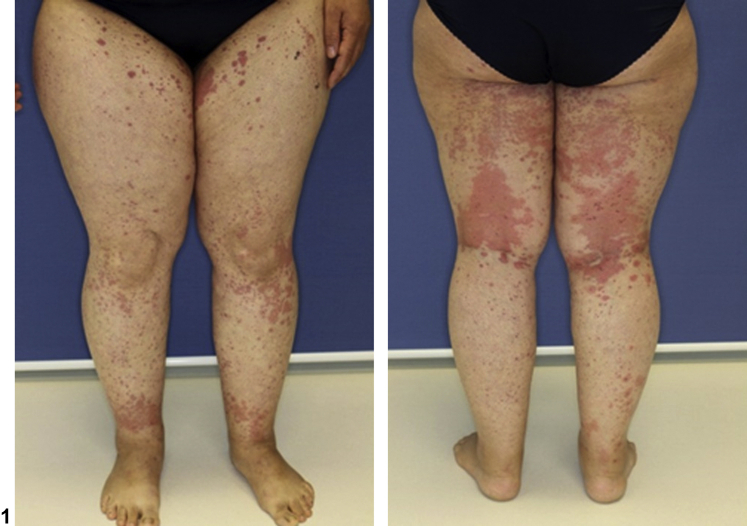
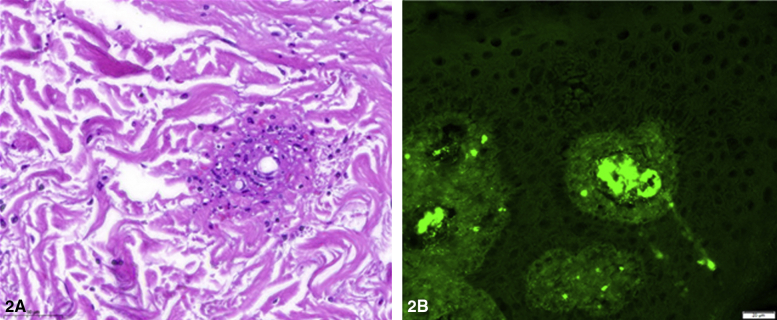
A 42-year-old woman presented with hemorrhagic macules and papules, especially affecting the lower extremity (Fig 1). Two weeks prior to presentation, she had cough, diarrhea, malaise, and limb pain. Infection with COVID-19 was confirmed through polymerase chain reaction. The rash began as a pruritic eruption on her right tibia, progressing to the current presentation over 2 days. C-reactive protein level was found to be increased (60.4 mg/L; normal level, ≤5.0 mg/L). The measurement of kidney function and blood count revealed no anomalies. Two skin biopsies were taken: one for histologic examination and the other for direct immunofluorescence (Fig 2).
Fig 1.
Fig 2.
Question 1: What is the most likely diagnosis?
-
A.
Schamberg disease
-
B.
COVID-associated vasculopathy
-
C.
Skin-limited IgA vasculitis
-
D.
Thrombocytopenic purpura
-
E.
Rocky Mountain spotted fever
Answers:
-
A.
Schamberg disease–Incorrect. Although the distribution of Schamberg disease is often symmetrical on the lower extremities as in the present case, this condition does not account for the severe fibrinoid necrosis of the vessel walls as identified in the histology.
-
B.
COVID-associated vasculopathy–Incorrect. Vasculopathy is defined by thickening of the intima due to the deposition of immunoglobulins, complement components, and fibrinogen without inflammatory lymphocyte infiltration. In the present case, fibrinoid necrosis and leukocytoclasia were present.
-
C.
Skin-limited IgA vasculitis–Correct. The patient showed a typical manifestation of leukocytoclastic vasculitis, which often occurs parainfectious. The fibrinoid necrosis of the vessel walls, nuclear dust from neutrophil fragmentation, and extravasation of red blood cells in addition to direct immunofluorescence staining with IgA are common characteristics of IgA vasculitis.
-
D.
Thrombocytopenic purpura–Incorrect. Laboratory findings showed no sign of thrombocytopenia.
-
E.
Rocky Mountain spotted fever–Incorrect. Although hemorrhagic rash is one of the common symptoms of Rocky Mountain spotted fever, our patient had no history of potential tick exposure and was not in an endemic area.
Question 2: Which is not a possible complication of IgA vasculitis?
-
A.
Arthritis
-
B.
Abdominal pain
-
C.
Hepatitis
-
D.
IgA nephropathy
-
E.
Orchitis
Answers:
-
A.
Arthritis–Incorrect. In 74% of the cases, patients with IgA vasculitis may develop joint swelling and pain accompanied by functional limitation. Most frequently, large joints such as knees, hips, and ankles are affected. Arthritis can precede the onset of purpura in 5%-25% of the cases.
-
B.
Abdominal pain–Incorrect. Gastrointestinal manifestations occur in 50%-80% of the cases.1 Typically, colicky abdominal pain and vomiting can be present. In severe cases, gastrointestinal bleeding can occur.
-
C.
Hepatitis–Correct. Hepatitis is not a common complication of IgA vasculitis. Pancreatobiliary involvements such as pancreatitis are possible complications of IgA vasculitis. It should be mentioned that leukocytoclastic or cryoglobulinemic vasculitis are associated with hepatitis.
-
D.
IgA nephropathy–Incorrect. Approximately 30%-50% of the patients show abnormal urinalysis such as proteinuria and hematuria.1 A recent study of 186 children with IgA vasculitis identified girls, patients aged >10 years, and an increased C-reactive protein level as potential risk factors for IgA nephropathy.2
-
E.
Orchitis–Incorrect. IgA vasculitis can involve the male genitalia and induce inflammatory complications such as orchitis and epididymitis. It is important to be aware that the symptoms can mimic testicular torsion.
Question 3: In a glucocorticosteroid skin-limited refractory case, what would be the most reasonable therapy?
-
A.
Ibuprofen
-
B.
Heparin
-
C.
Adalimumab
-
D.
Dapsone
-
E.
Cyclophosphamide
Answers:
-
A.
Ibuprofen–Incorrect. Although ibuprofen has anti-inflammatory effects, it is not sufficient to treat vasculitis. Additionally, the potential adverse renal effects should be considered.
-
B.
Heparin–Incorrect. A study with 228 children investigated heparin in IgA vasculitis and suggested a reduced risk of persistent kidney disease.3 However, the therapy is not justified due to the risk of severe side effects.
-
C.
Adalimumab–Incorrect. Several studies have investigated the effect of adalimumab in a variety of vasculitis forms with mixed results. Regarding IgA vasculitis, there are case reports that presented an IgA vasculitis that was triggered by adalimumab.4 Considering these reports, adalimumab is not recommended in IgA vasculitis.
-
D.
Dapsone–Correct. A recently published review on IgA vasculitis observed that dapsone was effective in refractory IgA vasculitis.5 In our case, dapsone induced a stable remission of IgA vasculitis after a relapse under the glucocorticosteroid therapy.
-
E.
Cyclophosphamide–Incorrect. There is evidence that other immunosuppressants are more effective than cyclophosphamide. Although cyclophosphamide is a potential therapeutic option, side effects must be considered. Other treatments should be preferred, especially in the case of skin-limited IgA vasculitis.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Du L., Wang P., Liu C., Li S., Yue S., Yang Y. Multisystemic manifestations of IgA vasculitis. Clin Rheumatol. 2021;40(1):43–52. doi: 10.1007/s10067-020-05166-5. [DOI] [PubMed] [Google Scholar]
- 2.Demircioğlu Kiliç B., Kasap Demir B. Determination of risk factors in children diagnosed with Henoch-Schönlein purpura. Arch Rheumatol. 2018;33(4):395–401. doi: 10.5606/ArchRheumatol.2018.6562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hahn D., Hodson E.M., Willis N.S., Craig J.C. Interventions for preventing and treating kidney disease in Henoch-Schönlein. purpura (HSP). Cochrane Database Syst Rev. 2015;(8):CD005128. doi: 10.1002/14651858.CD005128.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wei S.S., Sinniah R. Adalimumab (TNF α inhibitor) therapy exacerbates IgA glomerulonephritis acute renal injury and induces lupus autoantibodies in a psoriasis patient. Case Rep Nephrol. 2013;2013:812781. doi: 10.1155/2013/812781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee K.H., Hong S.H., Jun J. Treatment of refractory IgA vasculitis with dapsone: a systematic review. Clin Exp Pediatr. 2020;63(5):158–163. doi: 10.3345/kjp.2019.00514. [DOI] [PMC free article] [PubMed] [Google Scholar]