Abstract
Introduction and importance
Foreign body aspiration (FBA) is more frequently presented in children and considered a rare presentation in adults. One of the most common causes of FBA in adults are orthodontic appliances.
Case presentation
We present a case of a 70-year-old male with an accidently discovered fixed partial denture (bridge) in the right mainstem bronchus. The partial denture was removed successfully by flexible bronchoscopy.
Clinical discussion
FBA is an event that most frequently occurs with children, and rarely with adults having various risk factors and complications on patients.
Conclusion
This study aims to spotlight the danger of asymptomatic FBA and how retrieving sharp objects can be managed by flexible bronchoscopy thus leading to better management and increased awareness of such cases.
Keywords: Foreign body aspiration, Denture, Bronchoscopy, Chronic cough
Highlights
-
•
Foreign Body Aspiration (FBA) is very uncommon in adults.
-
•
Dental procedures and appliances are considered the second most common leading cause of FBA.
-
•
High level of physicians' susception is needed to identify FBA cases in adults is needed.
-
•
Flexible bronchoscopy has an important role in retrieving aspirated foreign bodies.
1. Introduction
Most FBA incidences occur in children [1]. It is a hazardous, life-threatening event, as foreign bodies of huge sizes can lead to deadly airway obstruction and is considered the leading cause of accidental home deaths in children aged less than six years old [2,3]. Moreover, FBA death rates in the united states range from 500 to 2000 yearly [4]. FBA is very uncommon in adults [[4], [5], [6]]. The most affected adult groups include mentally disabled and psychotic patients, prisoners, and alcoholics [7]. Asymptomatic aspiration of dentures in the trachea or bronchus is considered very rare to occur. Interestingly, dental procedures and appliances are considered the second most common leading cause of FBA [8]. For more effective prevention and better management of such cases in the future, we report an unusual case of a 70-year-old male with a denture accidently discovered on Computed Tomography (CT) scan requested for a wholly different medical condition. This case report has been reported in line with the SCARE Criteria [9].
2. Case presentation
A 70-year-old-male, a known case of Hypertension, Diabetes Miletus (DM), and asthma, presented at our clinic with typical asthma symptoms (shortness of the breath and a wheezy chest) and a history of fever, malaise, and loss of smell for a one-week duration after a close contact with positive COVID-19 family members. Polymerase Chain Reaction (PCR) tests for COVID-19 were ordered and turned out negative. Later on, a COVID-19 Antibodies (CoV-19 Abs) IgG Serum result was 53AU/ml (Reactive reference range ≥ 10 AU/ml). A Chest X-ray was ordered and showed diffuse bilateral patchy infiltrate (Fig. 1) suspected to be an infection. For the control of his asthma exacerbation, a Maintenance and Reliever Therapy (MART) composed of a combination of budesonide and formoterol fumarate dihydrate inhaler substituted his previous regimen (salbutamol inhaler) and based on the chest x-ray findings and the repeatedly negative PCR results, a CT scan was scheduled for further evaluation. The patient postponed his CT appointment, presented for follow-up 20 days later and had fully controlled asthma symptoms. The CT showed multiple areas of peripherally predominant ground-glass opacities with interlobar septal thickening and atelectatic bands seen in both lung fields more prominent in both upper lung lobes in addition to evidence of hyperdense foreign body seen in the right mainstem bronchus and bronchus intermedius with surrounding metallic artifact, measuring about 4.2 cm in length (Fig. 2). Retrospectively, a day before the delayed CT scan, the patient recalled that his denture was lost after he had gone through a syncopal attack that was thought to be due to hypoglycemia and the patient showed complete recovery within 1 min.
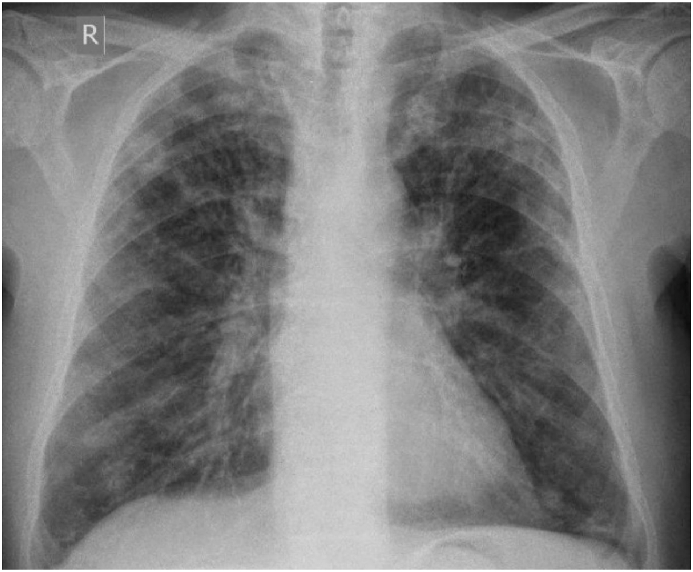
Fig. 1.
A Posterior Anterior (PA) chest X-ray showing a diffuse bilateral patchy infiltrate, more dominant peripherally.
Fig. 2.
(A) Coronal and (B) axial chest CT scan showing multiple areas of peripherally predominant ground glass opacities with interlobar septal thickening and atelectatic bands seen in both lung fields, findings are concerning for fibrotic lung changes more prominent in both upper lung lobes in addition to an evidence of hyperdense foreign body seen in the right main bronchus and bronchus intermedius with surrounding metallic artifact, measuring about 4.2 cm in length. (black arrow).
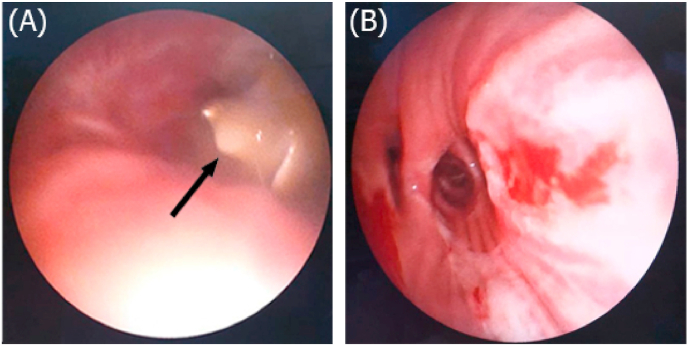
Based on the CT findings, the patient was urgently admitted for bronchoscopy. The procedure was performed under deep sedation in the operating room. Vocal cords were anesthetized with a local anesthetic. Using a Laryngeal Mask Airway (LMA), an appropriately sized flexible bronchoscope was inserted down. The partial denture was causing incomplete obstruction of the right main bronchus (Fig. 3. A). It was grasped through a metal dental post (screw) that was oriented medially using alligator forceps inserted through the flexible bronchoscope's working channel. To prevent slippage of the partial denture or dislodgment in the LMA, the scope and LMA were pulled all together after crossing the vocal cords. Re-inspection of the endobronchial tree revealed no mucosal injury (Fig. 3. B). This procedure confirmed the presence and the estimated measurement of the partial denture (Fig. 4). The patient was observed for a few hours after the procedure and was discharged afterward. The patient was followed up 25 days after discharge in the clinic, his x-ray was normal and showed no signs of complications.
Fig. 3.
(A) Pre-operative bronchoscopic view of the right main bronchus showing the aspirated denture (black arrow), (B) Post-operative bronchoscopic view of the right main bronchus.
Fig. 4.
A post-operative gross view of the aspirated denture with a size of 4.2cm in addition to the metal dental post that assessed its removal.
3. Discussion
FBA is considered a frequently encountered life-threatening event that occurs mainly in children [10,11]. Although it is frequently suspected in children with pulmonary symptoms, it is infrequent to occur in adults. Only 20% of FBA cases are patients above the age of 15 [10]. Aspirated foreign bodies can be classified into organic bodies like food, nuts or seeds aspirated due to incomplete chewing of substances, and inorganic bodies like nails or pins [12,13]. Dental prosthetics and procedures are considered the second most common leading cause of FBA after food; they represent up to 27.7% of this event's causes [14]. FBA can also occur in adults as a result of various risk factors such as advanced age, primary neurologic disorders (cerebrovascular accidents, alzheimer's, mental retardation, primary brain neoplasm, cerebral palsy, seizures, dementia, parkinson's disease), drugs, and alcohol consumption leading to the loss of consciousness and altered mental status. It can also take place without any notable risk factors [[15], [16], [17]]. Patients' symptoms of FBA differ based on the size and location of the foreign body, but the most common symptom in adults is a chronic cough. Less common symptoms may include chest pain, fever and hemoptysis [18,19]. In rare cases FBA can be asymptomatic as in our case [20].
Asthma medications may mask various FBA symptoms. Bronchodilators may reduce airway obstruction and corticosteroids decrease inflammation and irritation of airway mucosa. Moreover, Asthma or some respiratory infections symptoms may overlap with presenting FBA symptoms [21,22].
Most foreign bodies get aspirated into the right bronchi as in our case because it is broader, steeper, and more directly aligned with the trachea [23]. Acute presentation is infrequent [24]. Interestingly, some cases may take years to diagnose the presence of a foreign body in the bronchi [20]. Most patients do not remember aspiring foreign bodies thus, delaying their diagnosis [25]. Depending on the foreign body's effect on airflow, its characteristics, and the period after aspiration of the foreign body, it might lead to some serious manifestations and complications such as unresolving pneumonia, granulation tissue formation around the foreign body, lung abscesses, and inflammatory polyps [[26], [27], [28]]. Moreover, this can lead to the false diagnosis of various respiratory diseases [4]. Usually, FBA cannot be diagnosed clinically [29]. The diagnosis depends mainly on the visualization of the foreign body usually by chest radiograph or bronchoscopy. In some fewer cases, advanced imaging techniques can be used like Computed Tomography (CT) scanning, Magnetic Resonance Imaging (MRI) and fluoroscopy for the diagnosis [[30], [31], [32], [33], [34]]. In many cases as our case, foreign bodies are discovered accidently after ordering images for other medical conditions [35].
The proper intervention for FBA is to remove it once detected leading to rapid improvement of symptoms and preventing of any further damage from progressing [36]. Universally, rigid or flexible bronchoscopy are the most common techniques used in removing foreign bodies [37]. The first reported successful bronchoscopic elimination was by Gustav Killian in 1897 [38]. Rigid bronchoscopy is considered the first choice for foreign body retrieval as it provides broader view, allows airway ventilation, and requires less surgical experience [37,39]. Recently, flexible bronchoscopy has been more commonly used for FBA cases as it is operated under conscious sedation instead of general anesthesia thus, reducing procedure duration and its associated complications. In addition, flexible bronchoscopy reaches more distal branches of the bronchial tree and has less traumatic effects [40,41]. In our case, considering the age and co-morbidities of the patient, and the shape of the partial denture, flexible bronchoscopy was preferred. However, thoracotomy and bronchotomy may be required in 2% of FBA cases [42].
Protective orthodontic techniques have been suggested to prevent FBA, like securing loose orthodontic structures or devices in the mouth during different procedures and periodically checking and replacing any defected appliances [43]. In our case, there were no limitations or complications, the procedure went smoothly and the patient did not show any kind of complications.
4. Conclusion
In conclusion, foreign body aspiration can be a serious life-threatening situation that requires appropriate attention, when it comes to children or elderly patients using orthodontic appliances. Such events need a high level of physicians’ susception for patients presenting with various respiratory symptoms.
Source of funding
The author received no specific funding for this work.
Ethical approval
Ethical approval for case reports and case series are waived from any institutional review board approval according to the ongoing regulations of Yarmouk university.
Research consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Author contribution
Case report design and patient medical and surgical care: S.G and S·H.
Wrote the initial draft of the case report: S·H and F·H and M.A.
Critically, revised the manuscript: S.G and S·H.
All authors read and approved the content of the submitted case report.
Research registration
Name of the registry: N/A.
Unique Identifying number or registration ID: N/A.
Hyperlink to your specific registration (must be publicly accessible and will be checked): N/A.
Guarantor
Sahem Gharaibeh.
Declaration of competing interest
The authors report no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.102391.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Cramer N., Jabbour N., Tavarez M.M., Taylor R.S. StatPearls. Treasure Island (FL) StatPearls Publishing Copyright © 2021; 2021. Foreign body aspiration. StatPearls Publishing LLC. [PubMed] [Google Scholar]
- 2.Lifschultz B.D., Donoghue E.R. Deaths due to foreign body aspiration in children: the continuing hazard of toy balloons. J. Forensic Sci. 1996;41(2):247–251. [PubMed] [Google Scholar]
- 3.Brkic F., Umihanic S., Altumbabic H. Death as a consequence of foreign body aspiration in children. Med. Arch. 2018;72(3):220–223. doi: 10.5455/medarh.2018.72.220-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Limper A.H., Prakash U.B. Tracheobronchial foreign bodies in adults. Ann. Intern. Med. 1990;112(8):604–609. doi: 10.7326/0003-4819-112-8-604. [DOI] [PubMed] [Google Scholar]
- 5.Chen C.H., Lai C.L., Tsai T.T., Lee Y.C., Perng R.P. Foreign body aspiration into the lower airway in Chinese adults. Chest. 1997;112(1):129–133. doi: 10.1378/chest.112.1.129. [DOI] [PubMed] [Google Scholar]
- 6.Lan R.S. Non-asphyxiating tracheobronchial foreign bodies in adults. Eur. Respir. J. 1994;7(3):510–514. doi: 10.1183/09031936.94.07030510. [DOI] [PubMed] [Google Scholar]
- 7.Zitzmann N.U., Elsasser S., Fried R., Marinello C.P. Foreign body ingestion and aspiration. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999;88(6):657–660. doi: 10.1016/s1079-2104(99)70004-1. [DOI] [PubMed] [Google Scholar]
- 8.Doh R.M. Foreign body aspiration during dental treatment under general anesthesia: a case report. Journal of dental anesthesia and pain medicine. 2019;19(2):119–123. doi: 10.17245/jdapm.2019.19.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A. The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 10.Hilliard T., Sim R., Saunders M., Hewer S.L., Henderson J. Delayed diagnosis of foreign body aspiration in children. Emerg. Med. J. 2003;20(1):100. doi: 10.1136/emj.20.1.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rafanan A.L., Mehta A.C. Adult airway foreign body removal. What's new? Clin. Chest Med. 2001;22(2):319–330. doi: 10.1016/s0272-5231(05)70046-0. [DOI] [PubMed] [Google Scholar]
- 12.Choroomi S., Curotta J. Foreign body aspiration and language spoken at home: 10-year review. J. Laryngol. Otol. 2011;125(7):719–723. doi: 10.1017/S0022215111000727. [DOI] [PubMed] [Google Scholar]
- 13.Medidi S., Fountain A., Radwan M., Rumbak M. "Fishing in the trachea": a unique case of foreign body aspiration. Journal of bronchology & interventional pulmonology. 2012;19(2):168–170. doi: 10.1097/LBR.0b013e3182517cd0. [DOI] [PubMed] [Google Scholar]
- 14.Tamura N., Nakajima T., Matsumoto S., Ohyama T., Ohashi Y. Foreign bodies of dental origin in the air and food passages. Int. J. Oral Maxillofac. Surg. 1986;15(6):739–751. doi: 10.1016/s0300-9785(86)80116-8. [DOI] [PubMed] [Google Scholar]
- 15.Jaggi S., Kumar A., Garg K., Aggarwal D., Kundu R. Foreign body aspiration: an unusual presentation and outcome. J. Clin. Diagn. Res. : J. Clin. Diagn. Res. 2017;11(9):Od08–od09. doi: 10.7860/JCDR/2017/32020.10643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kullbom T.L., Adwers J. Unusual complication associated with severe maxillofacial trauma. Oral Surg. Oral Med. Oral Pathol. 1974;37(3):355–358. doi: 10.1016/0030-4220(74)90106-6. [DOI] [PubMed] [Google Scholar]
- 17.Hewlett J.C., Rickman O.B., Lentz R.J., Prakash U.B., Maldonado F. Foreign body aspiration in adult airways: therapeutic approach. J. Thorac. Dis. 2017;9(9):3398–3409. doi: 10.21037/jtd.2017.06.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 48-1983. A 14-year-old boy with recurrent hemoptysis and a right-lower-lobe infiltrate. The New England journal of medicine. 1983;309(22):1374-1381. [DOI] [PubMed]
- 19.Willett L.L., Barney J., Saylors G., Dransfield M. An unusual cause of chronic cough. Foreign body aspiration. J. Gen. Intern. Med. 2006;21(2):C1–C3. doi: 10.1111/j.1525-1497.2005.00224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salim M.U., Asghar A., Tareen I., Azhar M. Asymptomatic inhaled foreign body. A bullet in the lung for 2 years. Saudi Med. J. 2016;37(10):1136–1139. doi: 10.15537/smj.2016.10.16046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rai S., Kashyap M., Bakshi K. Foreign body aspiration masquerading as difficult asthma. 2007;24(1):25–27. [Google Scholar]
- 22.Pelaia G., Vatrella A., Busceti M.T. Molecular and cellular mechanisms underlying the therapeutic effects of budesonide in asthma. Pulm. Pharmacol. Therapeut. 2016;40:15–21. doi: 10.1016/j.pupt.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 23.Lin L., Lv L., Wang Y., Zha X., Tang F., Liu X. The clinical features of foreign body aspiration into the lower airway in geriatric patients. Clin. Interv. Aging. 2014;9:1613–1618. doi: 10.2147/CIA.S70924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bain A., Barthos A., Hoffstein V., Batt J. Foreign-body aspiration in the adult: presentation and management. Can. Respir. J. J. Can. Thorac. Soc. 2013;20(6):e98–99. doi: 10.1155/2013/754121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Samarei R. Survey of foreign body aspiration in airways and lungs. Global J. Health Sci. 2014;6(7 Spec No):130–135. doi: 10.5539/gjhs.v6n7p130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blazer S., Naveh Y., Friedman A. Foreign body in the airway. A review of 200 cases. Am. J. Dis. Child. 1980;134(1):68–71. doi: 10.1001/archpedi.1980.02130130050015. 1960. [DOI] [PubMed] [Google Scholar]
- 27.Hussain A. Neglected foreign body in the right bronchial tree. Int. Surg. 1976;61(6–7):366–367. [PubMed] [Google Scholar]
- 28.Yang Y.H., Zhang X.G., Zhang J.L., Zhang Y.B., Kou C.P. Risk factors for preoperative respiratory complications in children with tracheobronchial foreign bodies. J. Int. Med. Res. 2016;44(2):338–345. doi: 10.1177/0300060515602031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sink J.R., Kitsko D.J., Mehta D.K., Georg M.W., Simons J.P. Diagnosis of pediatric foreign body ingestion: clinical presentation, physical examination, and radiologic findings. Ann. Otol. Rhinol. Laryngol. 2016;125(4):342–350. doi: 10.1177/0003489415611128. [DOI] [PubMed] [Google Scholar]
- 30.Gibbons A.T., Casar Berazaluce A.M., Hanke R.E. Avoiding unnecessary bronchoscopy in children with suspected foreign body aspiration using computed tomography. J. Pediatr. Surg. 2020;55(1):176–181. doi: 10.1016/j.jpedsurg.2019.09.045. [DOI] [PubMed] [Google Scholar]
- 31.Laya B.F., Restrepo R., Lee E.Y. Practical imaging evaluation of foreign bodies in children: an update. Radiol. Clin. 2017;55(4):845–867. doi: 10.1016/j.rcl.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 32.Martinot A., Closset M., Marquette C.H. Indications for flexible versus rigid bronchoscopy in children with suspected foreign-body aspiration. Am. J. Respir. Crit. Care Med. 1997;155(5):1676–1679. doi: 10.1164/ajrccm.155.5.9154875. [DOI] [PubMed] [Google Scholar]
- 33.Sattar A., Ahmad I., Javed A.M., Anjum S. Diagnostic accuracy of chest x-ray in tracheobronchial foreign body aspiration in paediatric patients. J. Ayub Med. Coll. Abbottabad : JAMC (J. Assoc. Med. Can.) 2011;23(4):103–105. [PubMed] [Google Scholar]
- 34.Mu L.C., Sun D.Q., He P. Radiological diagnosis of aspirated foreign bodies in children: review of 343 cases. J. Laryngol. Otol. 1990;104(10):778–782. doi: 10.1017/s0022215100113891. [DOI] [PubMed] [Google Scholar]
- 35.Reddy R.Z., Carter Y.M., Hsia D.W. Successful removal of a chronic aspirated foreign body after twelve years. Case Reports in Pulmonology. 2018;2018 doi: 10.1155/2018/8241591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Senkaya I., Sağdiç K., Gebitekin C., Yilmaz M., Ozkan H., Cengiz M. Management of foreign body aspiration in infancy and childhood. A life-threatening problem. Turk. J. Pediatr. 1997;39(3):353–362. [PubMed] [Google Scholar]
- 37.Cohen S., Pine H., Drake A. Use of rigid and flexible bronchoscopy among pediatric otolaryngologists. Arch. Otolaryngol. Head Neck Surg. 2001;127(5):505–509. doi: 10.1001/archotol.127.5.505. [DOI] [PubMed] [Google Scholar]
- 38.Banerjee A., Rao K.S., Khanna S.K. Laryngo-tracheo-bronchial foreign bodies in children. J. Laryngol. Otol. 1988;102(11):1029–1032. doi: 10.1017/s0022215100107170. [DOI] [PubMed] [Google Scholar]
- 39.Golan-Tripto I., Mezan D.W., Tsaregorodtsev S. From rigid to flexible bronchoscopy: a tertiary center experience in removal of inhaled foreign bodies in children. Eur. J. Pediatr. 2021 May;180(5):1443–1450. doi: 10.1007/s00431-020-03914-y. [DOI] [PubMed] [Google Scholar]
- 40.Simpson G.T. Rigid vs. flexible bronchoscopy for foreign-body aspiration. N. Engl. J. Med. 1984;310(18):1190–1191. [PubMed] [Google Scholar]
- 41.Farrell P.T. Rigid bronchoscopy for foreign body removal: anaesthesia and ventilation. Paediatr. Anaesth. 2004;14(1):84–89. doi: 10.1046/j.1460-9592.2003.01194.x. [DOI] [PubMed] [Google Scholar]
- 42.Kiran S., Ahluwalia C., Chopra V., Eapen S. Bronchotomy for removal of foreign body bronchus in an infant. Indian J. Anaesth. 2014;58(6):772–773. doi: 10.4103/0019-5049.147156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Umesan U.K., Chua K.L., Balakrishnan P. Prevention and management of accidental foreign body ingestion and aspiration in orthodontic practice. Therapeut. Clin. Risk Manag. 2012;8:245–252. doi: 10.2147/TCRM.S30639. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.