Abstract
Background
Prior to the COVID-19 pandemic, the use of telemedicine to evaluate pediatric surgery patients was uncommon. Due in part to restrictions imposed to mitigate the spread of the virus, the use of telemedicine within pediatric surgery has significantly expanded.
Methods
Prior to the use of telemedicine within surgery divisions at our institution, pediatric surgeons were surveyed to determine their perspectives on the use of telemedicine. Following the expanded use of telemedicine in response to the COVID-19 pandemic, a follow up survey was distributed to determine the impact of telemedicine and the perceived benefits and barriers of continuing its use going forward.
Results
The pre-COVID survey was completed by 37 surgeons and the post-COVID survey by 36 surgeons and advanced practice providers across 10 pediatric surgical divisions. General surgeons were the most represented division for both the pre- (25%) and post-COVID (33.3%) survey. Less than 25% of providers reported use of telemedicine at any point in their career prior to COVID-19; but following the expanded use of telemedicine 95% of respondents reported interest in continuing its use. After expansion, 25% of respondents were concerned with the possibility of inaccurate diagnoses when using telemedicine compared to nearly 50% prior to expanded use.
Conclusion
Following the expanded use of telemedicine within pediatric surgery, there was a decrease in the concern for inaccurate diagnoses and a near uniform desire to continue its use. Going forward, it will be imperative for pediatric surgeons to take an active role in creating a process for implementing telemedicine that best fits their needs and the needs of their patients and patients’ families.
Keywords: Telemedicine, Telehealth, COVID-19, Pediatrics, Pediatric surgery
Introduction
An increase in access to reliable high-speed internet services combined with a growth in the number of communication platforms have made real-time, remote interaction possible for most Americans.1 , 2 Within the healthcare domain, these technologies have been leveraged by providers to reach a growing number of potential patients through the use of telemedicine. Across the United States, the use of telemedicine has been increasing for more than a decade.3 In 2016, it was estimated by the department of Health and Human Services (HHS) that more than 60% of healthcare institutions made use of some form of telehealth, which includes telemedicine and other platforms that support patient-to-provider communication.4 Amongst pediatric surgeons, the use of telemedicine remained rare prior to the COVID-19 pandemic, despite evidence that supports video visits as a safe and effective method for evaluating patients in the pre- and post-operative phases of care.5 The low adoption rates by surgeons have been attributed to factors such as a lack of compensation, unfamiliarity, and security concerns.4 However, these limitations have not been fully explored in the scientific literature.
At our institution, there was no consistent use of telemedicine in any surgical divisions prior to the COVID-19 pandemic. To curb the spread of the virus, restrictions were put in place in the early stages of the pandemic to limit physical contact between patients and providers in nonemergent settings. There was a rapid rollout of telemedicine across the institutional to replace in-person outpatient visits. The aim of this study was to assess the perspectives of surgical providers towards using telemedicine, defined for this study as either synchronous video encounters or synchronous audio only encounters, to evaluate and care for patients. Prior to the expanded use of telemedicine, a survey was distributed to surgeons with the goal of ascertaining their interest and perceived potential barriers for using telemedicine to care for pediatric surgical patients. Following the rapid expansion of telemedicine, a second survey was distributed to determine if the increased use of telemedicine impacted the perspectives of surgical providers at our institution.
Materials and Methods
An overview of telemedicine at our institution
The terms “telemedicine” and “telehealth” have been defined in my ways and may be used differently depending on the organization and the context. For all survey material and for this manuscript the term “telemedicine” refers to a synchronous encounter between a provider and a patient and can include video and audio or audio only (phone) appointments, unless otherwise specified.
At our institution, the decision to support telemedicine use within a specific division was made at the organizational level. Once approval was granted for use within a division, it was at the discretion of the individual providers to decide how to implement telemedicine into their practice. Prior to COVID-19, telemedicine parity laws had not been enacted in our state, leaving decisions regarding reimbursement for telemedicine services to the individual insurers.
All video appointments were carried out using software embedded within the electronic medical record, which can be accessed by computer or with a video capable phone. Before patients could complete a telemedicine appointment, they first provided authorization for remote access to the electronic medical record. During the video visit, patients and providers were connected remotely by the embedded application. The functionality of the software is limited to video and audio sharing, and there were no healthcare team members present with the family to assist with the appointment.
Pre-COVID-19 survey development
Before the COVID-19 pandemic, our group was in the process of assessing interest in telemedicine across the surgical divisions at our institution. As a part of that process, a survey was developed to determine the perspectives of surgical providers on the use of telemedicine within their practice. The aims of the survey were to determine the perceived barriers and potential benefits of using telemedicine to evaluate and care for pediatric surgery patients. Assessments of surgeon comfort using telemedicine and perceived cost used a 5-point Likert-type scale, and all other questions were presented at the categorical or ordinal level. Participants were given the opportunity to write clarification or other comments. Modifications to the survey were made following feedback from members of the Department of Pediatric Surgery, resulting in the final list of questions. The survey was reviewed by the local IRB and approved with a waiver of written consent. The complete survey has been included as Appendix A.
Pre-COVID-19 survey distribution
On March 27, 2020, an invitation to complete the pre-COVID survey was distributed by email to all pediatric surgeons at our institution. The following divisions were included: General Pediatric Surgery, Cardiothoracic Surgery, Colorectal Surgery, Dentistry, Gynecology, Neurosurgery, Otolaryngology, Orthopedic Surgery, Plastic Surgery, and Urology. Clinicians who chose to participate completed REDCap surveys online via a secure network.6 To reduce the potential for bias or misreporting, responses were anonymous.
Post-COVID-19 survey development
Following the implementation of telemedicine at our institution, we developed a survey for surgical providers to determine the impact of the increased use of telemedicine on their perceived barriers and interest in continuing the use of telemedicine beyond the restrictive period. The pre-COVID differed from the post-COVID survey due to the difference in the aims of the two surveys and to account for the difference in context regarding telemedicine use when the studies were distributed. The assessments of comfort using telemedicine and perceived cost used a 5-point Likert-type scale, and all other questions were presented at the categorical or ordinal level. Participants were given space at the end of the survey to write clarification or other comments. Modifications were made following feedback from the Department of Pediatric Surgery, resulting in the final list of questions. The survey was reviewed by the local IRB and approved for distribution with a waiver of written consent. The complete survey has been included as Appendix B.
Post-COVID-19 survey distribution
On July 1, 2020, an invitation to complete the post-COVID survey was distributed via email to all attending surgeons and advanced practice providers across all pediatric surgical specialties at our institution. The choice of how to utilize telemedicine was made at the level of the divisions. It came to our attention after the pre-COVID survey had been distributed that the divisions of gynecology, neurosurgery, otolaryngology, and urology had extended the use of telemedicine to advanced practice providers (APP) while others had limited the use of telemedicine to surgeons. To be inclusive of all providers who were responsible for evaluating surgical patients the decision was made to send the post-COVID survey to APPs as well as surgeons. Clinicians who chose to participate completed REDCap surveys online via a secure network. To reduce the potential for bias or misreporting, responses were anonymous.
Telemedicine use within pediatric surgery
To combat the spread of COVID-19 at our institution, a restriction on in-person contact was put in place on March 16, 2020. The restriction was eventually lifted on June 25, 2020. The medical record at our institution was queried to identify all outpatient clinic visits that were completed from January 1, 2020 to July 10, 2021. Telemedicine appointments were identified by using the following current procedural terminology (CPT) codes: 280097 (telehealth phone call new patient), 280098 (telehealth phone call follow up), 280095 (video visit new patient), and 280096 (video visit follow up).
Analysis
Descriptive statistics were generated and percentages and frequencies were calculated for categorical variables. Comparisons between the pre-COVID and post-COVID periods and between the use of video or phone telemedicine were made using chi square or Fisher exact tests as appropriate. Significance was determined at a P value of <0.05.
Results
Response rate and demographics
The pre-COVID survey was completed by 37 of 69 (54%) surgeons, and the post-COVID survey was completed by 36 of 83 (43%) providers (Table 1 ). Pediatric general surgery was the most represented division in both the pre- (25%) and post-COVID (33%) phases. Most providers reported having been in practice between 2-10 years (pre-51.3%, post-44.4%). In the pre-COVID group, 21.6% of surgeons reported previous experience with telemedicine, compared to only 5.6% of providers in the Post-COVID group. Before the COVID-19 pandemic, at least half of the time, providers scheduled in-person post-operative appointments for patients undergoing ambulatory (56.7%) or inpatient (64.8%) procedures.
Table 1.
Respondent characteristics.
| Pre-COVID (n = 37) |
Post-COVID (n = 36) |
|||
|---|---|---|---|---|
| N | % | N | % | |
| Respondent Title/Role | ||||
| Surgeon | 37 | 100 | 33 | 91.7 |
| Advanced Practice Provider | NA | NA | 3 | 8.3 |
| Other | NA | NA | 0 | 0 |
| Primary Specialty | ||||
| Pediatric General Surgery* | 10 | 27 | 14 | 42.4 |
| Pediatric Cardiothoracic Surgery | 0 | 0 | 1 | 2.8 |
| Pediatric Dentistry | 1 | 2.8 | 1 | 2.8 |
| Pediatric Gynecology | 2 | 5.6 | 2 | 5.6 |
| Pediatric Neurosurgery | 3 | 8.3 | 3 | 8.3 |
| Pediatric Otolaryngology | 7 | 19.4 | 5 | 13.9 |
| Pediatric Orthopedic Surgery | 7 | 19.4 | 4 | 11.1 |
| Pediatric Plastic Surgery | 1 | 2.8 | 3 | 8.3 |
| Pediatric Urology | 5 | 13.9 | 3 | 8.3 |
| Other | 0 | 0 | 0 | 0 |
| Years in Practice | ||||
| Less than 2 | 3 | 8.1 | 2 | 5.6 |
| 2-5 | 9 | 24.3 | 7 | 19.4 |
| 5-10 | 10 | 27 | 9 | 25 |
| 10-15 | 4 | 10.8 | 6 | 16.7 |
| 15-20 | 4 | 10.8 | 5 | 13.9 |
| More than 20 | 7 | 18.9 | 7 | 19.4 |
| Previous Experience with Telemedicine | ||||
| Yes | 8 | 21.6 | 2 | 5.6 |
| No | 29 | 78.4 | 34 | 94.4 |
| Approximately What Proportion of Your Ambulatory Surgery Patients Are Scheduled for a Post-Operative In-Person Appointment? | ||||
| None | 1 | 2.7 | NA | NA |
| Less than 10% | 7 | 18.9 | NA | NA |
| 10-25% | 3 | 8.1 | NA | NA |
| 25-50% | 5 | 13.5 | NA | NA |
| 50-75% | 9 | 24.3 | NA | NA |
| 75-100% | 2 | 5.4 | NA | NA |
| All patients | 10 | 27 | NA | NA |
| How Often Do Your Ambulatory Surgery Patients Require 2 or More Post-Operative Visits? | ||||
| None | 1 | 2.7 | NA | NA |
| Less than 10% | 13 | 35.1 | NA | NA |
| 10-25% | 7 | 18.9 | NA | NA |
| 25-50% | 8 | 21.6 | NA | NA |
| 50-75% | 3 | 8.1 | NA | NA |
| 75-100% | 4 | 10.8 | NA | NA |
| All patients | 1 | 2.7 | NA | NA |
| Approximately What Proportion of Your Inpatient Surgery Patients Are Scheduled for a Post-Operative In-Person Appointment? | ||||
| None | 1 | 2.7 | NA | NA |
| Less than 10% | 2 | 5.4 | NA | NA |
| 10-25% | 3 | 8.1 | NA | NA |
| 25-50% | 7 | 18.9 | NA | NA |
| 50-75% | 5 | 13.5 | NA | NA |
| 75-100% | 8 | 21.6 | NA | NA |
| All patients | 11 | 29.7 | NA | NA |
| How Often Do Your Inpatient Surgery Patients Require 2 or More Post-Operative Visits? | ||||
| None | 1 | 2.7 | NA | NA |
| Less than 10% | 7 | 18.9 | NA | NA |
| 10-25% | 4 | 10.8 | NA | NA |
| 25-50% | 13 | 35.1 | NA | NA |
| 50-75% | 2 | 5.4 | NA | NA |
| 75-100% | 8 | 21.6 | NA | NA |
| All patients | 2 | 5.4 | NA | NA |
Includes colorectal surgery.
The Impact of COVID-19 on telemedicine use within pediatric surgery
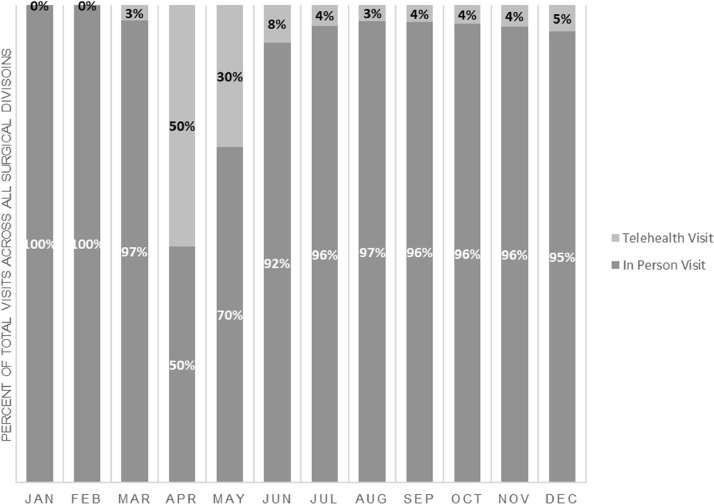
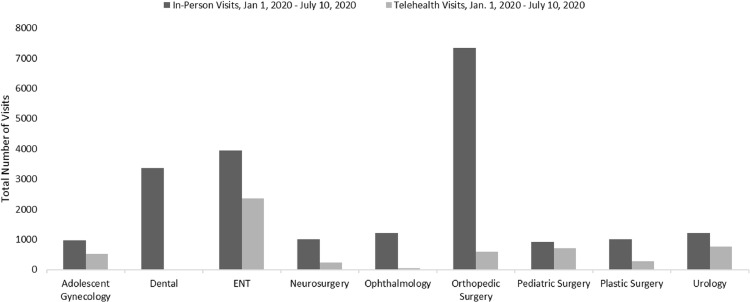
Prior to March 27, 2020, there was no use of telemedicine within the surgical divisions at our institution. During the restrictive period, surgical providers had reduced clinics and saw fewer patients each week as a result (Table 2 ). For 44.7% of providers, at least 75% of visits during the restrictive period were performed using telemedicine. In response to the restrictions put in place from March 16, 2020 to June 25, 2020, to combat the response of COVID-19, the use of telemedicine to complete outpatient clinic appointments increased dramatically compared to the use of telemedicine in 2019 (Fig. 1 ). Use by division varied widely during the restrictive period, with surgical dentistry completing zero appointments compared to more than 2000 for otolaryngology providers (Fig. 2 ). Following the removal of the restriction on in-person encounters, there was a sudden decrease in the use of telemedicine across most divisions (Fig. 1).
Table 2.
The impact of COVID-19 on telemedicine use within pediatric surgery.
| Provider responses before COVID-19 (N = 37) | |
|---|---|
| Frequency of clinic | N (%) |
| Less than weekly | 2 (5.4) |
| Weekly | 13 (35.1) |
| Twice weekly | 11 (29.7) |
| Three or more times per week | 11 (29.7) |
| What percentage of clinic visits are preoperative? (N = 37) | |
| Less than 10% | 9 (25) |
| 10-25% | 5 (13.9) |
| 25-50% | 15 (41.7) |
| 50-75% | 5 (13.9) |
| More than 75% | 2 (5.6) |
| What percentage of clinic visits are post-operative? | |
| Less than 10% | 11 (29.7) |
| 10-25% | 18 (48.7) |
| 25-50% | 5 (13.5) |
| 50-75% | 3 (8.1) |
| More than 75% | 0 (0) |
| Would You Choose to Add a Role for Telemedicine to Your Practice? | |
| Yes | 21 (56.8) |
| No | 5 (13.5) |
| I use telemedicine but WOULD expand use | 10 (27) |
| I use telemedicine but WOULD NOT expand use | 1 (2.7) |
| Provider Perspective After COVID-19 (N = 36) | |
| The following were decreased during the COVID-19 restrictive period | N(%) |
| The frequency of clinic | 23 (63.9) |
| The number of patients seen each week | 36 (100) |
| The percentage of new patient visits | 19 (52.8) |
| The percentage of post-op visits (N = 37) | 26 (74.3) |
| The percentage of visits resulting in surgery being recommended (N=37) | 21 (60) |
| During the restrictive period, what percentage of your clinic visits were telemedicine visits? | |
| None | 0 (0) |
| Less than 10% | 2 (5.3) |
| 10-25% | 5 (13.2) |
| 26-50% | 8 (21.1) |
| 51-75% | 5 (15.8) |
| 76-99% | 12 (34.2) |
| 100% | 4 (10.5) |
| Compared to before the restrictive period, do you feel more confident using telemedicine? | |
| Yes | 35 (97.2) |
| No | 0 (0) |
| Unchanged | 1 (2.8) |
| If given the option, would you offer telemedicine appointments for your patients going forward? | |
| Yes | 34 (94.4) |
| No | 2 (5.6) |
Fig. 1.
The impact of COVID-19 on the use of telemedicine across all pediatric surgery divisions. Restrictions on in-person contact aimed at combating the spread of COVID-19 were in effect from March 16, 2020 to June 25, 2020. In response, there was a rapid increase in the use of telemedicine amongst surgical providers in the early phase of the restrictive period. However, as restrictions lessened, the use of telemedicine by surgical providers decreased dramatically.
Fig. 2.
The use of telemedicine within pediatric surgery divisions during COVID-19. Prior to March 27, 2020, the use of telemedicine within surgery was rare at our institution. Within 4 months of the onset of COVID-19, nine surgical divisions were utilizing telemedicine services; however, use varied widely by specialty.
The perceived barriers for implementing telemedicine in pediatric surgery
The expanded use of telemedicine coincided with a lessening of provider concerns regarding patient and physician satisfaction and was associated with a marginally significant increase in provider confidence in the ability to obtain an accurate diagnosis through video (Table 3 ). Providers listed issues with compensation, staffing, and workflow as potential areas of concern in both the pre- and post-COVID periods. Of note, six of the eight respondents who choose “other” on the pre-COVID survey stated “the ability to do a physical exam.” Additional issues that were mentioned by respondents who selected “other” concerns included technology issues (five respondents) and confidentiality (two respondents).
Table 3.
The perceived barriers for implementing synchronous telemedicine appointments into pediatric surgery before and after COVID-19.
| What issues do you see with trying to use video appointments within your practice? |
|||
|---|---|---|---|
| Pre-COVID N (%) | Post-COVID N (%) | P | |
| None | 1 (2.7) | 3 (8.3) | 0.36 |
| Insurance (Compensation) | 25 (67.6) | 20 (55.6) | 0.29 |
| Staffing | 8 (21.6) | 8 (22.2) | 0.95 |
| Workflow Disruption | 21 (56.8) | 21 (58.3) | 0.89 |
| Cost | 3 (8.1) | 0 (0) | 0.24 |
| Patient Satisfaction | 16 (43.2) | 8 (22.2) | 0.06 |
| PCP Satisfaction | 7 (18.9) | 0 (0) | 0.01 |
| Surgeon Satisfaction | 18 (48.7) | 9 (25) | 0.04 |
| Inaccurate Diagnoses | 17 (46) | 9 (25) | 0.06 |
| Inability to Provide Appropriate Treatment | Not asked | 13 (36.1) | —- |
| Other | 8 (21.6) | 8 (22.2) | 0.95 |
The desire for ongoing use of telemedicine in pediatric surgery
Prior to COVID-19, 83.8% of surgeons were interested in adding telemedicine or expanding the role of telemedicine in their practice. Following its expanded use during COVID-19, 94.4% reported that they would prefer to continue offering telemedicine appointments (Table 2). There were no differences in respondents’ choice of video or phone telemedicine appointments for completing appointments for initial evaluation, postoperative follow-up after ambulatory surgery, or postoperative follow up after an inpatient stay (Table 5). However, when asked to rate their confidence level with completing various tasks, providers were more confident when using video to obtain information to make a common diagnosis, order the appropriate diagnostic study, prescribe the appropriate medication, and relay information to the patient in a way that is easy to understand (Table 4 )
Table 5.
Preferences on video or audio only telemedicine use based on appointment type (N = 36).*
| Which option would you choose for completing the initial evaluation of a patient for select operations/diagnoses under normal working conditions? | |||
|---|---|---|---|
| Video | Phone | Neither | |
| All Providers | 29 (80.6) | 3 (8.3) | 7 (19.4) |
| Which option would you choose for completing a post-operative follow up after ambulatory surgery under normal working | |||
|---|---|---|---|
| conditions? | |||
| Video | Phone | Neither | |
| All Providers | 28 (77.8) | 19 (52.8) | 2 (5.6) |
| Which option would you choose for completing a post-operative follow up after select operations accompanied by an inpatient stay under | |||
| normal working conditions? | |||
| Video | Phone | Neither | |
| All Providers | 30 (83.3) | 9 (25) | 4 (11.1) |
Respondents were able to choose multiple answer choices.
Table 4.
A comparison of the perceived differences between phone and video telemedicine appointments for evaluating pediatric surgery patients (N = 36).
| More than 25% of appointments required additional information outside of the visit to help make a clinical decision |
|||
|---|---|---|---|
| Phone N (%) | Video N (%) | P | |
| Yes | 15 (41.7) | 13 (36.1) | 0.56 |
| No | 21 (58.3) | 23 (63.9) | |
| During telemedicine appointments, I feel that I can confidently complete the following tasks at least most of the time | |||
|---|---|---|---|
| Phone N (%) | Video N (%) | ||
| Obtaining information to diagnose common conditions | 12 (33.3) | 30 (83.3) | <0.001 |
| Obtaining information to diagnose rare or complex conditions | 9 (25) | 16 (44.4) | 0.03 |
| Ordering the appropriate diagnostic study | 18 (50) | 31 (86.1) | <0.001 |
| Prescribing the appropriate medication/treatment | 12 (33.3) | 25 (69.4) | <0.001 |
| Relaying information to the patient in a way that is easy to understand | 19 (52.8) | 32 (88.9) | <0.001 |
| Responding to the patient's questions and concerns | 26 (72.2) | 34 (94.4) | 0.01 |
| Providing an experience for the patient that is as stress free as possible | 20 (55.6) | 33 (91.7) | 0.002 |
Discussion
Despite concerns regarding workflow disruptions and compensation, pediatric surgical providers perceive the benefits of telemedicine to outweigh the potential barriers, leading to overwhelming support for its continued use in the evaluation and management of patients. Following a period of expanded use, support for telemedicine grew from 84% to 95%, and there was a marginally significant decrease in the proportion of providers concerned with the ability to obtain an accurate diagnosis. The COVID-19 pandemic has provided the impetus to evaluate the resiliency and effectiveness of the healthcare delivery model in the United States, including the current options for patients seeking evaluation from a surgeon. Previous studies have demonstrated the safety and effectiveness of using telemedicine to evaluate surgical patients and to reduce the disparity in access to specialists that exists across the United States.7 , 8 Now more than ever, patients and providers are familiar with telemedicine and supportive of its use.9 Lessons learned during the COVID-19 pandemic can help guide future decisions regarding how best to incorporate telemedicine into a surgical practice.
The restrictions on in-person contact during COVID-19 required surgeons to adjust their approach to patient care and provided an opportunity for many to gain first-hand experience using telemedicine in a surgical practice. Following the expanded use of telemedicine, there were only two areas that were identified by more than 40% of respondents as potential issues – compensation and workflow disruption. In a 2016 report on telemedicine from the Department of Health and Human Services (HHS), it was speculated that the regional discrepancy in telemedicine use was due in part to insurers’ uneven compensation policies.4 Inconsistent reimbursement policies may affect organizational support, potentially limiting opportunities for surgeons seeking to offer telemedicine to their patients. In the years following the HHS report, the financial landscape has changed in favor of telemedicine. With the 2018 Bipartisan Budget Act, telemedicine became a supported option for patients covered under Medicare Advantage.10 Despite movement in a positive direction, inconsistencies amongst private insurers were common prior to COVID-19.11 In recognition of the importance of telemedicine use during the COVID-19 pandemic, federal legislation was passed to temporarily expand the previously established compensation practices to include a wider group of patients covered through government-supported insurance.12 In addition, it was stipulated that video appointments were to be reimbursed at the same rate as in-person appointments.13 , 14
The growth of telemedicine coincided with the adoption of policies that incentivized institutions to support telemedicine services, but many of these policies were temporary. The value of telemedicine is predicated in part upon it being a widely accessible technology, and continued use beyond the COVID-19 period will not be possible without organizational support. Ensuring availability beyond the pandemic will require the adoption of permanent legislation that includes both private and public insurers. To this end, research on the impact of telemedicine on patients and providers during the COVID-19 pandemic will be essential for maintaining the support needed to continue its use.
The long-term success of telemedicine within pediatric surgery will require acceptance from both patients and providers. There is strong evidence that patients are highly satisfied with telemedicine, and in some instances even prefer it to the traditional in-person encounter.15 The patient perspective is important, but without surgeon buy-in the potential impact is limited. In our study, nearly 60% of respondents in both the pre- and post-COVID groups reported workflow disruptions as a potential issue with trying to use video appointments within their surgical practice. At our institution, the decision to expand the use of telemedicine was made to provide surgical providers with an opportunity to continue caring for their patients during a period of hospital-wide restriction on in-person contact. Following the removal of the restriction on in-person contact, telemedicine use dropped precipitously across most divisions. Possible explanations for the abrupt decline include patient or provider preference as well as decisions that were made at the level of the organization or individual division. It is not possible to delineate further with the currently available data, but future studies should be designed to evaluate the impact of telemedicine across all levels of the hospital system.
There has been an explosion in the presence of technology within healthcare in recent decades, but most of these changes occurred slowly over time. For many surgical providers, the transition to telemedicine during the COVID-19 pandemic was abrupt, providing little time for adjustment. The dangers of not considering the long-term impact on providers when implementing new technology can be exemplified through studies examining the provider perspective on the electronic health record (EHR). Use of an EHR was strongly incentivized in 2009 with passage of the American Recovery and Reinvestment Act.16 Early support of the EHR was high amongst providers, but there were concerns about its impact on workflow, efficiency, and patient-provider communication.17 , 18 Now, the EHR is viewed as a major contributor to provider burnout and use of the EHR is inversely related to physician satisfaction.19, 20, 21 Like the EHR, telemedicine is a tool with the capability of improving the patient experience. However, unlike the EHR, there is no federal policy in place to either mandate or incentivize its long-term use. It is imperative for pediatric surgeons and other providers to take an active role in creating a process for implementing telemedicine that best fits their individual needs and the needs of their patients.
Our study included providers from ten different pediatric surgery divisions. Not surprisingly, there was a wide range of responses regarding the types of patient encounters that occur in each practice under normal working conditions. For surgical patients that require in-office procedures, such as those needing in-person treatment from an oral or orthopedic surgeon, the utility of telemedicine will be limited. Telemedicine is not a direct substitution for an in-person appointment with a surgeon. Given the currently available technology, telemedicine is also of limited value for ophthalmologists and other providers who require specialized equipment to complete most evaluations. For surgical patients who do not require an in-office procedure or the use of specialized equipment, video offers a high level of confidence to providers when completing most tasks. When compared to audio alone, video was viewed by providers as superior for developing a diagnosis and for communicating with the patient and their caregivers. The use of telemedicine is not without limitations, but remote evaluation by video is widely supported by pediatric surgeons and should be considered an option for evaluating and treating patients in both the pre- and post-operative phases of care.
This study is not without limitations. Our goal with the post-COVID-19 survey was to obtain a sample of responses across all the pediatric surgical divisions at our institution. This included more than 60 providers, many of whom were not directly involved with the research. The survey used was anonymous and the sample size relatively small, leading to the possibility that the results of this study are not generalizable to all institutions or pediatric surgical providers. The use of an anonymous survey that was devoid of most identifiers, including respondent age and sex prohibited attempts to match responses between the two cohorts, making it difficult to evaluate unexpected findings in the pre-and post-COVID survey. For instance, a higher percentage of respondents reported previous experience with telemedicine in the pre-COVID group than in the post-COVID group. Without the ability to match responses, it is not possible to determine if the unexpected difference in reported previous experience was the result of recall bias or the product of a small sample size. Future studies should examine the outcomes of patients evaluated using telemedicine and determine whether there were errors in diagnosis or changes in operative plans after in-person evaluation.
Conclusion
Following the expanded use of telemedicine with pediatric surgery, there was a decrease in the concern for inaccurate diagnoses and a near uniform desire to continue its use. Going forward, it will be imperative for pediatric surgeons to take an active role in creating a process for implementing telemedicine that best fits their individual needs and the needs of their patients and their patients’ families.
Acknowledgments
Acknowledgments
Thank you to Laura McLaughlin and Zach Gray for their help in obtaining and collating the data needed to evaluate the change in use of telemedicine within surgical divisions at our institution.
Disclosure
The authors have no financial relationships relevant to this article to disclose.
Conflicts of interest: The authors have no conflicts of interest relevant to this article to disclose.
Funding
The project described was supported by Award Number UL1TR002733 from the National Center for Advancing Translational Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Author Contributions
Study conception and design: GM, KJ, KD IH, PM. Acquisition of data: GM, CL, LN, KJ. Analysis and Interpretation of data: JC, GM, KJ, IH, KD, PM. Drafting of Manuscript: GM, PM, JC, IH. Critical Revision: All authors.
References
- 1.Perrin A.D. M. Americans' Internet Access: 2000-2015. Pew Res Center. 2020 https://www.pewresearch.org/internet/2015/06/26/americans-internet-access-2000-2015/ Published 2015. Accessed April 15. [Google Scholar]
- 2.Smith A. The Pew Research Center; 2014. American Americans and Technology Use. [Google Scholar]
- 3.Waller M, Stotler C. Telemedicine: a Primer. Curr Allergy Asthma Rep. 2018;18:54. doi: 10.1007/s11882-018-0808-4. [DOI] [PubMed] [Google Scholar]
- 4.Report to Congress: E-health and Telemedicine. In: Services USDoHaH, ed2016.
- 5.Asiri A, AlBishi S, AlMadani W, ElMetwally A, Househ M. The use of telemedicine in surgical care: a systematic review. Acta Informatica Medica. 2018;26:201–206. doi: 10.5455/aim.2018.26.201-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marcin JP, Ellis J, Mawis R, Nagrampa E, Nesbitt TS, Dimand RJ. Using telemedicine to provide pediatric subspecialty care to children with special health care needs in an underserved rural community. Pediatrics. 2004;113(1 Pt 1):1–6. doi: 10.1542/peds.113.1.1. [DOI] [PubMed] [Google Scholar]
- 8.Marcin JP, Shaikh U, Steinhorn RH. Addressing health disparities in rural communities using telehealth. Pediatr Research. 2016;79:169–176. doi: 10.1038/pr.2015.192. [DOI] [PubMed] [Google Scholar]
- 9.Hamilton EC, Saiyed F, Miller CC, 3rd, et al. The digital divide in adoption and use of mobile health technology among caregivers of pediatric surgery patients. J Pediatr Surg. 2018;53:1478–1493. doi: 10.1016/j.jpedsurg.2017.08.023. [DOI] [PubMed] [Google Scholar]
- 10.The use of telemedicine by physicians: still the exception rather than the rule. Health Affairs. 2018;37:1923–1930. doi: 10.1377/hlthaff.2018.05077. [DOI] [PubMed] [Google Scholar]
- 11.Lacktman NAJ, Levine S. 2019. 50-State Survey of Telehealth Commercial Payer Statutes. [Google Scholar]
- 12.Notification of enforcement discretion for telehealth remote communications during the COVID-19 Nationwide Public Health Emergency. In: (OCR) OfCR, ed2020.
- 13.Revisions to Payment Policies under the Medicare Physician Fee Schedule, Quality Payment Program and Other Revisions to Part B for CY 2020. Centers Medicare Medicaid Serv. 2020 https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Federal-Regulation-Notices-Items/CMS-1715-F Published 2019. Accessed April 15. [Google Scholar]
- 14.Contreras CM, Metzger GA, Beane JD, Dedhia PH, Ejaz A, Pawlik TM. Telemedicine: patient-provider clinical engagement during the COVID-19 pandemic and beyond. J Gastrointest Surg. 2020;24:1692–1697. doi: 10.1007/s11605-020-04623-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ramaswamy A, Yu M, Drangsholt S, et al. Patient satisfaction with telemedicine during the COVID-19 pandemic: retrospective cohort study. J Med Internet Res. 2020;22:e20786. doi: 10.2196/20786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Recovery and Reinvestment Act: making hospitals technologically advanced. GHA Today. 2009;53:8–9. [PubMed] [Google Scholar]
- 17.Cantiello J, Cortelyou-Ward KH. The American Recovery and Reinvestment Act: lessons learned from physicians who have gone electronic. Health Care Manag (Frederick) 2010;29:332–338. doi: 10.1097/HCM.0b013e3181fa04c8. [DOI] [PubMed] [Google Scholar]
- 18.Likourezos A, Chalfin DB, Murphy DG, Sommer B, Darcy K, Davidson SJ. Physician and nurse satisfaction with an Electronic Medical Record system. J Emerg Med. 2004;27:419–424. doi: 10.1016/j.jemermed.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 19.Shapiro DE, Duquette C, Abbott LM, Babineau T, Pearl A, Haidet P. Beyond burnout: a physician wellness hierarchy designed to prioritize interventions at the systems level. Am J Med. 2019;132:556–563. doi: 10.1016/j.amjmed.2018.11.028. [DOI] [PubMed] [Google Scholar]
- 20.Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc. 2016;91:836–848. doi: 10.1016/j.mayocp.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 21.Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J Am Med Inform Assoc. 2014;21(e1):e100–e106. doi: 10.1136/amiajnl-2013-001875. [DOI] [PMC free article] [PubMed] [Google Scholar]