Abstract
Resurfacing arthroplasty of the hip has had a difficult last decade.
Fracture of the femoral neck has been a known complication of resurfaced hip replacement; however, fracture of the metal peg within the femoral component has only been reported twice. We encountered and treated a patient with a unique type of metal failure.
A 45 year old lady had advanced arthritis of her left hip secondary to rheumatoid disease.
In 2006, an ASR resurfacing arthroplasty was performed and excellent function of the hip was achieved. After 9 years, she experienced an acute pain in the hip without trauma.
Serial radiographs before & after the onset of symptoms did not reveal any significant abnormality. MRI scan did not suggest any adverse features too. No evidence emerged in favour of adverse reactions to metal debris (ARMD). Decision to revise the hip was taken with suspicion of an occult fracture.
At surgery, the stem of the femoral component was found fractured at its junction with the dome, the dome being still well fixed with the femoral neck. The acetabular component was well fixed. Till date she is very satisfied with the revised hip.
Fracture of the femoral peg at its junction to the dome is a complication of hip resurfacing that has not been previously reported in the literature. On the retrieved specimen, instead of ‘beach lines’ indicative of failure of the material over a prolonged period, we observed only a notched area of bending on the medial side of the implant. This is indicative of an acute event.
We wish to make surgeons aware of this particular complication when investigating a similar Case presentation. There is unlikely any standard investigation that diagnoses the fractured implant accurately.
Keywords: Fracture, Sudden onset hip pain, Hip resurfacing
1. Introduction
Resurfacing arthroplasty of the hip has had a long and tumulus journey in the last decade. In the previous decade this was considered to be a superior form of hip arthroplasty for the younger patient. It preserves the anatomy & biomechanics of the hip better.3,6 It provides more longevity, less risk of dislocation and preserves more bone stock.3 Complications were seen related to early learning curve e.g. inaccurate positioning of implants leading to femoral notching & subsequent fracture; edge loading leading to loosening; AVN of femoral head etc.3, 4, 5,8, 9, 10,12 The most significant complication emerged to be related to adverse reactions to metal debris (ARMD).7,11 The effects of this has been path changing in the field of hip arthroplasty with our understanding of metal on metal (MoM) bearings.
Fracture of the preserved femoral neck has been a known complication of resurfaced hip replacement; however, fracture of the metal peg within the femoral component has only been reported twice1,2 with two different implants but both were visible on plain radiograph. We report a Case of metal peg dissociation from the metal head which was not visible on plain radiograph, CT and MRI.
2. Case description
A 45-year old lady was diagnosed to have advanced arthritis of her left hip secondary to rheumatoid disease in 2006. An ASR resurfacing arthroplasty was performed in the same year using a modified Hardinge approach. A 48 mm size cup with 43 mm femoral head size were used. Recovery was uneventful and excellent function of the hip was achieved. Rheumatoid arthritis was confirmed from histology of intraoperative synovial tissue samples. She continued to function normally without any adverse symptoms from the operated hip for 9 years. In the meantime, she was recalled following the MHRA MoM regulations in 2012. She was asymptomatic. She had Cobalt & Chromium ion levels checked which were within normal limits.
On a particular day in 2015 she experienced an acute pain in the hip as she was walking. The pain was unremitting & affected her mobility, requiring her to use a walking stick. The pain was in her left groin & anterior thigh. She felt the left leg to be shorter. Serial radiographs before & after the onset of symptoms did not reveal any significant abnormality. She had a presumed slight superior ‘notching’ from the very first post op radiographs that did not alter with time. We performed a MRI scan, which did not suggest any adverse features. Metal ion levels were rechecked – Cr level was marginally above normal, with a Co level within normal limit. A decision was made by the senior surgeon to revise the resurfaced hip suspecting an acute injury, most likely a fractured neck femur within the femoral component(Fig. 1).
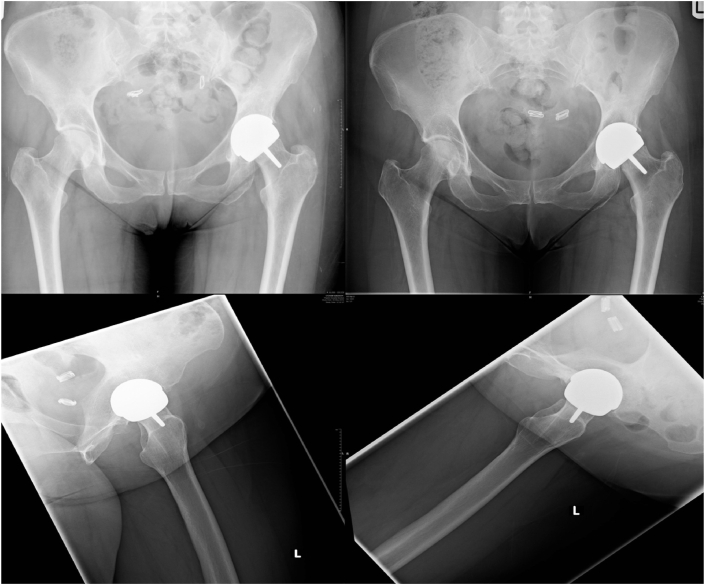
Fig. 1.
Top left and Bottom left- AP and lateral x-ray of the pelvis and left lateral hip one year after surgery
Top right and Bottom right- AP and lateral x-ray of the pelvis and left hip at the time of patient becoming symptomatic.
The revision surgery was performed 4 months following the onset of her symptoms. A posterolateral approach was used. Operative findings were – 200 mls clean fluid, small necrotic tissue, bone atrophy under the femoral component, soft bone, poor abductors & a broken peg. The stem of the femoral component was fractured at its junction with the dome, the dome being still well fixed with the femoral neck (Fig. 2). The acetabular component was well fixed; it was explanted & revised with a 54 mm uncemented cup using supplementary bone autograft. The femoral neck was cut & a primary uncemented stem was used. A 36mm ceramic femoral head with highly crosslinked polyethylene liner were used as bearings. She made a good recovery post operatively. At 5 years follow-up, she is very satisfied with the revised hip, which has functioned well without any complications.
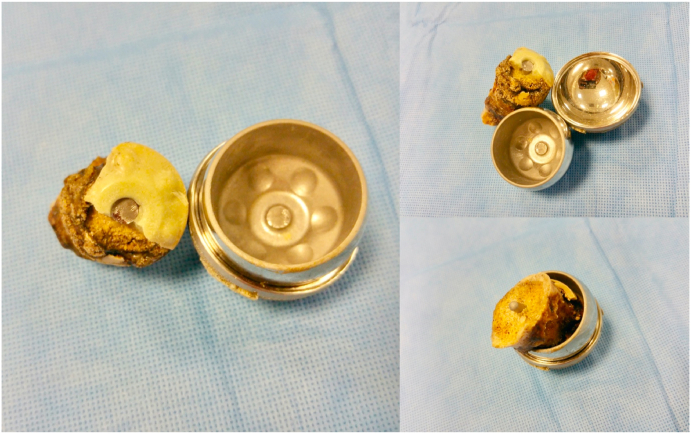
Fig. 2.
Retrieved implants showing fracture of the femoral stem with the stem well fixed within the femoral neck.
3. Conclusion
Fracture of the femoral peg at its junction to the dome is a complication of hip resurfacing that has not been previously reported in the literature, to our knowledge. There are two previous reports of fractures of the femoral peg that was visible in plain radiographs. In our case we had a diagnostic dilemma until the hip was explored intraoperatively. Imaging modalities failed to diagnose this particular implant failure. Interestingly, the hip functioned perfectly well for 9 years before failing as an acute event without trauma. The onset of symptoms was the only clue to prompt us to offer a revision surgery.
Examination of the removed specimens revealed an absence of ‘beach lines’ those are indicative of failure of the material over a prolonged period.2 Instead we observed only a notched area of bending on the medial side of the implant. This is indicative of an acute event.
The previous two fractured resurfacing implants belonged to different companies – Cormet (Corin Medical Ltd, UK) in 2006 and ReCap (Biomet, USA) in 2011. The ASR resurfacing implant was withdrawn in 2010 due to well-established complications. However, this is the first time that this implant had this particular complication.
It was noted from immediate post-operative radiographs that there was a slight notching of the implant at the lateral femoral neck. If this had indeed increased abnormal stress through the implant, the expectation was a fatigue failure within 6–16 weeks.2,7,8 This did not happen for 9 years. On the other hand, the implant did fail without significant trauma, and likely as an acute event. Although not conclusive of the exact mechanism of failure, there are several possibilities for the cause of failure of the implant. It is likely to be multifactorial. There is little doubt that a trivial trauma has caused the implant to fracture and became symptomatic with pain. Our hypothesis is: There could have been bone resorption at the bone – cement interface, causing loosening and progression to the cement – implant interface too. Repeated microtrauma would have aided the loosening. This may have led to the dome slowly becoming loosened while the peg staying well fixed. The supposed trivial trauma is likely to have caused enough shearing force going across the joint leading to its failure.
Our purpose of this report is to make surgeons aware of this possibility when investigating a similar case presentation. As we did, we would recommend standard investigation protocols to diagnose a more common complication for a resurfaced hip replacement e.g. AVN of the femoral neck with or without fracture, metallosis related complications etc. The decision to explore the hip need to be based on the severity of the patient's symptoms by a senior surgeon experienced in managing similar patients with MoM hips. This is particularly important as there is unlikely to be any investigation that diagnoses the fractured implant accurately. We do acknowledge that the possibility of this is small, and in a similar occurrence, it is more likely to show radiological abnormality at the outset.
Contributor Information
Hemanta Das, Email: d.hemanta@gmail.com.
Tahawwar Minhas, Email: minhas@lineone.net.
Rohit Rambani, Email: rohit@rambani.com.
References
- 1.Bowman N.K., Bucher T.A., Bassily A.A. Fracture of the stem of the femoral component after resurfacing arthroplasty of the hip. JBJS (Br) 2006;88-B:1652–1653. doi: 10.1302/0301-620X.88B12.18299. [DOI] [PubMed] [Google Scholar]
- 2.Bhutta M.A., Shah V.B. Fracture of the femoral alignment stem of a hip resurfacing arthroplasty A Case report. Acta Orthop Belg. 2011;77:128–131. [PubMed] [Google Scholar]
- 3.Shimmin A.J., Bare J., Back D.L. Complications associated with hip resurfacing arthroplasty. Orthop Clin N Am. 2005;36:187–193. doi: 10.1016/j.ocl.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 4.Back D.L., Dalziel R., Young D., Shimmin A. Early results of primary Birmingham hip resurfacings: an independent prospective study of the first 230 hips. J Bone Joint Surg[Br] 2005;87-B:324–329. doi: 10.1302/0301-620x.87b3.15556. [DOI] [PubMed] [Google Scholar]
- 5.Cossey A.J., Back D.L., Shimmin A., Young D., Spriggins A.J. The nonoperative management of periprosthetic fractures associated with the Birmingham hip resurfacing procedure. J Arthroplasty. 2005;20:358–361. doi: 10.1016/j.arth.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 6.Ritter M.A., Lutgring J.D., Berend M.E., Pierson J.L. Failure mechanisms of total hip resurfacing. Clin Orthop Relat Res. 2006;453:110–114. doi: 10.1097/01.blo.0000238849.23744.8e. [DOI] [PubMed] [Google Scholar]
- 7.Long J.P., Bartel D.L. Surgical variables affect the mechanics of a hip resurfacing system. Clin Orthop Relat Res. 2006;453:115–122. doi: 10.1097/01.blo.0000238873.09390.6f. [DOI] [PubMed] [Google Scholar]
- 8.Marker D.R., Seyler T.M., Jinnah R.H. Femoral neck fractures after metal-on-metal total hip resurfacing : a prospective cohort study. J Arthroplasty. 2007;22(7 Suppl 3):66–71. doi: 10.1016/j.arth.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 9.Steffen R., O'Rourke K., Gill H.S., Murray D.W. The anterolateral approach leads to less disruption of the femoral head-neck blood supply than the posterior approach during hip resurfacing. JBJS. 2007;89-B:1293–1298. doi: 10.1302/0301-620X.89B10.18974. [DOI] [PubMed] [Google Scholar]
- 10.Vail T.P., Glisson R.R., Dominguez D.E. Position of hip resurfacing component affects strain and resistance to fracture in the femoral neck. J Bone Joint Surg Am. 2008 Sep;90(9):1951–1960. doi: 10.2106/JBJS.F.00788. [DOI] [PubMed] [Google Scholar]
- 11.Langton D.J., Joyce T.J., Jameson S.S. Adverse reaction to metal debris following hip resurfacing: the influence of component type, orientation and volumetric wear. JBJS(Br) 2011 Feb;93(2) doi: 10.1302/0301-620X.93B2.25099. [DOI] [PubMed] [Google Scholar]
- 12.Morlock M.M., Bishop N., Zustin J. Modes of implant failure after hip resurfacing: morphological and wear analysis of 267 retrieval specimens. J Bone Joint Surg Am. 2008 Aug;90(Suppl 3):89–95. doi: 10.2106/JBJS.H.00621. [DOI] [PubMed] [Google Scholar]