Abstract
Background:
The influence of patient sex on clinical outcomes after arthroscopic anterior shoulder stabilization is unclear.
Purpose:
To investigate sex-based differences in clinical outcomes after arthroscopic anterior shoulder stabilization.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A retrospective study was conducted among 76 patients who underwent arthroscopic anterior shoulder stabilization from February 2010 to December 2017. The patients were grouped by sex. The recurrence rate of instability was compared, as were pre- and postoperative pain scores, functional outcome scores, and active range of motion (ROM). Postoperative magnetic resonance imaging (MRI) was also performed for structural assessment of the glenohumeral joint.
Results:
No significant difference was found in the recurrence rate between female and male patients (13.3% vs 14.8%; P ≥ .999; risk ratio, 1.107 [95% CI, 0.266-4.597]). Compared with male patients, female patients had a significantly lower preoperative Constant score (94.4 ± 6.4 vs 85.4 ± 11.1; P = .002), forward flexion (173.8° ± 10.7° vs 154.0° ± 33.8°; P = .011), abduction (171.0° ± 18.4° vs 142.7° ± 39.9°; P = .001), and external rotation (76.6° ± 21.6° vs 67.7° ± 20.4°; P = .037). Postoperatively, female patients had a significantly lower Simple Shoulder Test score compared with men (8.8 ± 1.9 vs 10.3 ± 1.6; P = .005). The mean changes from pre- to postoperative Rowe score (43.6 ± 21.4 vs 31.5 ± 19.8; P = .044), Constant score (9.9 ± 8.9 vs 0.8 ± 8.1; P = .002), forward flexion (24.0 ± 36.2 vs 4.2 ± 10.9; P = .013), abduction (36.0 ± 38.3 vs 7.6 ± 18.4; P < .001), and external rotation (19.7 ± 21.3 vs 6.7 ± 26.2; P = .023) in female patients were significantly higher than those in the men. There were no sex-based differences on any MRI parameter measured.
Conclusion:
Female patients had a similar recurrence rate as that of male patients after arthroscopic anterior shoulder stabilization. Most postoperative clinical outcome measures showed no significant difference between the sexes. Despite worse preoperative values, more significant improvements in postoperative shoulder function and active ROM were seen in women.
Keywords: anterior shoulder instability, sex, arthroscopic shoulder stabilization, clinical outcome, recurrence
Shoulder instability has a relatively low incidence, varying between 23.12 and 23.91 per 100,000 person-years.23 Anterior shoulder instability is the most common type, with a prevalence of 1.7% in the general population.4,16 Men are at a particularly high risk of anterior shoulder instability, about 3 times that of women.16 In previously reported cohort studies, the ratio of enrolled male to female patients is high, around 3.8% to 5.6%.14,22,25 Consequently, male patients compose the majority of participants in existing studies, while female patients are underrepresented.
Given the paucity of female patients, although sex-based anatomic differences in shoulder instability are fairly investigated to some degree, studies regarding sex-related research of arthroscopic shoulder stabilization are few.9 To our knowledge, the only prior cohort study involving the sex-based postoperative outcome differences was conducted by Kaipel et al15; these authors studied 36 patients (24 men, 12 women) undergoing arthroscopic shoulder stabilization and found that postoperative Constant score and shoulder stability were significantly lower in female patients.
It is generally reported that male sex predicts a significantly higher risk of recurrent instability after nonsurgical management of traumatic primary anterior shoulder dislocation.23,39 However, sex-based differences in recurrence rates after stabilization surgery have been controversial. Porcellini et al29 found that recurrence rates for male and female patients were 10.1% and 2.8%, respectively (P = .02). Based on the pooled data from 5 previously published studies, Randelli et al30 reported an overall recurrence rate of 15.0% (96/642) in men compared with 8.7% (20/230) in women (P = .02). However, women have also been found to have a higher risk of recurrence.21 Bradley et al5 found that female athletes were significantly more likely to undergo revision surgery after arthroscopic posterior shoulder capsulolabral repair (P = .001; OR = 4.47). Another study reported no difference in recurrence rates between the sexes.30
The purpose of this study was to investigate sex-based differences in clinical outcomes of patients who underwent arthroscopic anterior shoulder stabilization. It was hypothesized that the clinical outcomes of female patients after arthroscopic anterior shoulder stabilization would be similar to those of male patients.
Methods
Study Design
This study was approved by the health sciences institutional review board of our hospital, and informed consent was obtained from all participants. Patients who underwent arthroscopic shoulder stabilization between February 2010 and December 2017 were retrospectively included. The study inclusion criteria were patients who were diagnosed with anterior glenohumeral instability, underwent arthroscopic Bankart repair alone or Bankart repair with remplissage, had a Bankart or ALPSA (anterior labroligamentous periosteal sleeve avulsion) lesion under arthroscopy, and had a minimum of 2 years of follow-up data.
The exclusion criteria were patients who had posterior shoulder instability or multidirectional instability, were diagnosed with a rotator cuff tear or frozen shoulder, underwent a Latarjet procedure or an open surgery, had bilateral surgery or previous surgery on either the ipsilateral or contralateral shoulder, and were diagnosed with a glenoid bone defect larger than 25% or superior labral anterior posterior (SLAP) lesion under arthroscopy.
Surgical Technique
The procedure of arthroscopic shoulder stabilization was performed by a senior surgeon (S.C.) with an assistant according to previously established methods.27,42 All patients were under general anesthesia in the lateral decubitus position during the surgery. A diagnostic arthroscopy for Bankart lesion, ALPSA lesion, Hill-Sachs lesion, SLAP lesion, glenoid bone defect, rotator cuff tear, and other concomitant injuries through a standard posterior portal was performed. The dynamic examination of the affected arm was performed to confirm the diagnosis. Bankart lesions and ALPSA lesions were repaired by fixing the capsulolabral tissues to the glenoid rim with 2 to 5 anchors (2.9-mm Lupine; Mitek). Whether the Hill-Sachs lesion engaged with the anterior glenoid rim was examined based on a previous study.8 Engaging Hill-Sachs lesions or Hill-Sachs lesions with a tendency to be engaged were treated with an additional remplissage procedure by implanting 1 or 2 suture anchors (4.5-mm Biocorkscrew; Arthrex). When the glenoid bone defect was less than 25% in size, no bone graft was needed.
Postoperative Rehabilitation
All patients underwent a standardized rehabilitation plan. A sling was worn on the operated arm, which was kept in 15° of abduction within 6 weeks postoperatively. Passive shoulder flexion and external rotation at 90° of abduction were initiated after 6 weeks postoperatively. Wall slides, internal rotation stretching, stretching training of abduction-external rotation at 90° of abduction, and isometric strengthening exercises were carried out after 3 months. About 6 months after surgery, the patient was evaluated by the surgeon before being allowed to return to previous activities.
Outcome Evaluations
Preoperative information and intraoperative findings were obtained from the medical records and confirmed with the patients during postoperative follow-up. Recurrence was defined as at least 1 episode of postoperative shoulder dislocation or subluxation. Preoperative evaluations included the visual analog scale (VAS) score for pain; Rowe score;32 Constant score;10 and active range of motion (ROM), including forward flexion, abduction, external rotation at 90° of abduction, and internal rotation. In addition to preoperative functional scores and ROM, postoperative evaluations were supplemented with the American Shoulder and Elbow Surgeons (ASES) score,20 Simple Shoulder Test (SST) score,3 Oxford Shoulder Instability Score (OSIS),12 Single Assessment Numeric Evaluation (SANE) score,40 and recurrence rate.
Magnetic Resonance Imaging Assessment
Magnetic resonance imaging (MRI) assessments were completed by a surgeon (M.C.) and an experienced radiologist (Y.X.), both of whom were blinded to the patient grouping. The operated shoulder was assessed postoperatively using a 3.0-T machine (Magnetom Verio; Siemens) equipped with an 8-channel shoulder coil. The sequences mainly included T1, T2, proton density, fat suppression, and water excitation. The cartilage was evaluated using axial 3-dimensional proton-density sequences with fat suppression and water excitation.13 According to the method of Yoo et al,43 the parameters measured on axial images were anterior labrum glenoid height index (LGHI) and anterior labral slope, while inferior LGHI and inferior labral slope were measured on coronal images. Cartilage thickness on the humeral head side and the glenoid side were measured from 3 consecutive axial planes around the largest diameter of the humeral head: anterior, middle, and posterior.
Statistical Analysis
The sample-size estimation was performed before patient involvement. The recurrence rate was selected as the endpoint. The recurrence rate of male and female patients was respectively based on the reports of van der Linde et al37 and Balg and Boileau.2 The α level was set at .05, the statistical power was 0.8, and the distribution ratio was 4 between reported epidemiological studies16,28 and enrollment in the previous cohort studies.7,11,16,17 The calculation indicated that at least 36 male patients and 9 female patients were needed to detect a significant difference.
Continuous variables, presented as mean ± SD, were analyzed with a Mann-Whiney U test, and categorical variables, presented as n (%), were compared using Pearson chi-square tests and continuity correction in the chi-square test. The risk ratio of recurrence was calculated. SPSS Statistics 26 (IBM) and STATA 16.0 (StataCorp) software were used to conduct statistical analyses. P <.05 was considered statistically significant.
Results
A total of 108 patients met the inclusion criteria, and 76 (70.4%) patients were available for the final follow-up. Of these, 61 patients were male and 15 patients were female. The mean follow-up time of the 76 patients was 64.9 ± 29.3 months (range, 29-123 months).
Patient Characteristics and Intraoperative Findings
Patient characteristics are reported in Table 1. The 2 groups did not differ significantly in characteristics, except for less contact sports participation in women (13.3% vs 63.9%; P = .001). No postoperative complications were reported. No significant differences were found between the 2 groups in terms of operative technique and intraoperative findings (Table 2).
Table 1.
Patient Characteristicsa
| Female (n = 15) | Male (n = 61) | P Value | |
|---|---|---|---|
| Age at surgery, y | 28.9 ± 9.1 | 25.9 ± 6.3 | .257 |
| Age at initial instability, y | 22.7 ± 6.9 | 21.2 ± 4.7 | .508 |
| Follow-up time, mo | 54.6 ± 19.5 | 67.4 ± 30.8 | .190 |
| Preoperative dislocations | 7.0 ± 3.5 | 6.6 ± 3.6 | .565 |
| Duration of symptoms, mo | 77.0 ± 86.6 | 57.8 ± 55.5 | .760 |
| Dominant arm affected | 10 (66.7) | 34 (55.7) | .442 |
| Cause of initial shoulder instability | .091 | ||
| Sports | 6 (40.0) | 39 (63.9) | |
| Nonsports | 9 (60.0) | 22 (36.1) | |
| Contact sports | 2 (13.3) | 39 (63.9) | .001 |
aData are presented as mean ± SD or n (%).
Table 2.
Intraoperative Findingsa
| Female (n = 15) | Male (n = 61) | P Value | |
|---|---|---|---|
| Repair technique | .387 | ||
| Bankart repair alone | 9 (60.0) | 29 (47.5) | |
| Bankart repair with remplissage | 6 (40.0) | 32 (52.5) | |
| Bankart lesion | 7 (46.7) | 35 (57.4) | .455 |
| ALPSA lesion | 8 (53.3) | 26 (42.6) | .455 |
| Hill-Sachs lesion | 10 (66.7) | 45 (73.8) | .581 |
| Glenoid bone defect <25% | 1 (6.7) | 11 (18.0) | .492 |
aData are presented as n (%). ALPSA, anterior labroligamentous periosteal sleeve avulsion.
Results of Outcome Evaluations
The pre- and postoperative shoulder function scores and active ROMs are shown in Table 3. Compared with male patients, female patients had a significantly lower preoperative Constant score (94.4 ± 6.4 vs 85.4 ± 11.1; P = .002), forward flexion (173.8° ± 10.7° vs 154.0° ± 33.8°; P = .011), abduction (171.0° ± 18.4° vs 142.7° ± 39.9°; P = .001), and external rotation (76.6° ± 21.6° vs 67.7° ± 20.4°; P = .037). Postoperatively, female patients had a significantly lower SST score compared with men (8.8 ± 1.9 vs 10.3 ± 1.6; P = .005), but the difference was less than the minimal clinically important difference (MCID) for the SST score after shoulder arthroplasty (2.4 points).34 The recurrence rate was not significantly different between female and male patients (13.3% vs 14.8%; P ≥ .999; risk ratio, 1.107 [95% CI, 0.266-4.597]). All patients were able to resume activities of daily living postoperatively.
Table 3.
Clinical Outcomesa
| Preoperative | Postoperative | |||||
|---|---|---|---|---|---|---|
| Female (n = 15) | Male (n = 61) | P Value | Female (n = 15) | Male (n = 61) | P Value | |
| VAS pain score | 2.7 ± 3.5 | 1.1 ± 2.2 | .065 | 1.1 ± 1.9 | 0.8 ± 1.5 | .452 |
| Functional scores | ||||||
| Rowe | 41.8 ± 28.3 | 56.8 ± 16.1 | .136 | 85.4 ± 17.9 | 88.3 ± 14.2 | .967 |
| Constant | 85.4 ± 11.1 | 94.4 ± 6.4 | .002 | 95.3 ± 5.0 | 95.2 ± 5.9 | .994 |
| ASES | — | — | — | 89.8 ± 13.7 | 92.6 ± 10.4 | .319 |
| SST | — | — | — | 8.8 ± 1.9 | 10.3 ± 1.6 | .005 |
| OSIS | — | — | — | 38.6 ± 8.0 | 39.1 ± 8.0 | .862 |
| SANE | — | — | — | 84.5 ± 14.6 | 85.6 ± 13.5 | .774 |
| Active ROM, deg | ||||||
| Forward flexion | 154.0 ± 33.8 | 173.8 ± 10.7 | .011 | 178.0 ± 7.7 | 177.8 ± 9.5 | .988 |
| Abduction | 142.7 ± 39.9 | 171.0 ± 18.4 | .001 | 178.7 ± 5.2 | 178.3 ± 8.7 | .824 |
| External rotation | 67.7 ± 20.4 | 76.6 ± 21.6 | .037 | 87.3 ± 5.9 | 82.9 ± 11.2 | .121 |
| Internal rotation, vertebra | T10 ± 5 | T8 ± 3 | .128 | T8 ± 3 | T9 ± 3 | .434 |
| Recurrence | — | — | — | 2 (13.3) | 9 (14.8) | ≥.999 |
| Resumed activities of daily living | — | — | — | 15 (100) | 61 (100) | — |
aData are presented as mean ± SD or n (%). Bolded P values indicate statistically significant difference between sexes. Dashes indicate that the data was not collected in the study. ASES, American Shoulder and Elbow Surgeons; OSIS, Oxford Shoulder Instability Score; ROM, range of motion; SANE, Single Assessment Numeric Evaluation; SST, Simple Shoulder Test; T, thoracic; VAS, visual analog scale.
The pre- to postoperative changes in outcomes are shown in Table 4. Both groups had significant postoperative improvements in VAS, Rowe, and Constant scores as well as active ROM, with the exception of internal rotation in the male patients. The mean changes in outcomes were all higher in women compared with men (Figure 1). The improvement in female patients was significantly greater than in male patients regarding the Rowe score (43.6 ± 21.4 vs 31.5 ± 19.8; P = .044), the Constant score (9.9 ± 8.9 vs 0.8 ± 8.1; P = .002), forward flexion (24.0 ± 36.2 vs 4.2 ± 10.9; P = .013), abduction (36.0 ± 38.3 vs 7.6 ± 18.4; P < .001), and external rotation (19.7 ± 21.3 vs 6.7 ± 26.2; P = .023). For the Rowe score, this difference in improvement (12.1 points) between the sexes was greater than the reported MCID of 9.7 points.26 The MCID for the Constant score has not been evaluated for arthroscopic shoulder stabilization but has been reported as 8 points for reverse shoulder arthroplasty.36 The difference in improvement of Constant score between the sexes was 9.1 points in the current study.
Table 4.
Mean Changes From Preoperative to Postoperative Evaluationa
| Female (n = 15) | Male (n = 61) | P Value | |
|---|---|---|---|
| VAS painb | –1.6 ± 3.5 | –0.3 ± 2.4 | .309 |
| Rowe | 43.6 ± 21.4 | 31.5 ± 19.8 | .044 |
| Constant | 9.9 ± 8.9 | 0.8 ± 8.1 | .002 |
| Forward flexion | 24.0 ± 36.2 | 4.2 ± 10.9 | .013 |
| Abduction | 36.0 ± 38.3 | 7.6 ± 18.4 | <.001 |
| External rotation | 19.7 ± 21.3 | 6.7 ± 26.2 | .023 |
| Internal rotationb | –1T ± 6 | 0T ± 4 | .426 |
aData are presented as mean ± SD. Bolded P values indicate statistically significant difference between sexes. VAS, visual analog scale.
bA negative difference indicated improvement after surgery in these evaluations.
Figure 1.
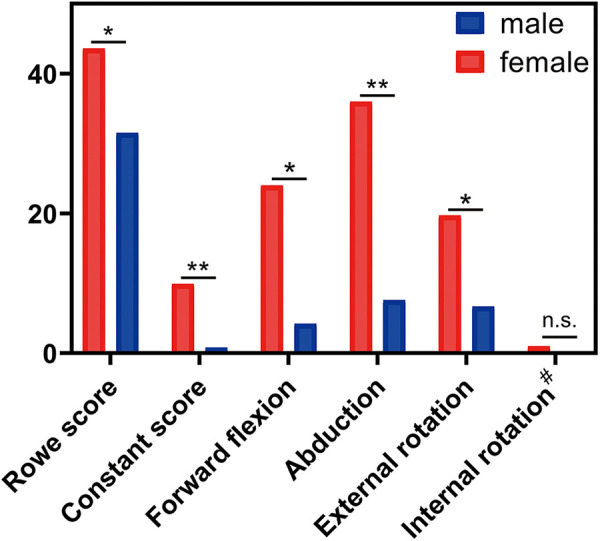
Mean pre- to postoperative changes in outcomes between the sexes. *P < .05; **P < .01; n.s., not significant. #Absolute values were used in place of negative numbers.
Results of MRI Assessment
Of the 76 study patients, 48 (63.2%; 11 women and 37 men) were willing to undergo a postoperative MRI. Results indicated that there were no statistically significant differences between the sexes on any of the MRI parameters measured (Table 5).
Table 5.
MRI Assessmentsa
| Female (n = 11) | Male (n = 37) | P Value | |
|---|---|---|---|
| Labrum | |||
| Anterior LGHI | 3.2 ± 0.6 | 3.2 ± 0.7 | .755 |
| Inferior LGHI | 2.7 ± 0.6 | 2.7 ± 0.6 | .893 |
| Anterior labral slope, deg | 27.6 ± 3.8 | 26.5 ± 2.8 | .137 |
| Inferior labral slope, deg | 25.2 ± 1.7 | 26.1 ± 2.6 | .220 |
| Cartilage | |||
| Thickness (humeral head side), mm | |||
| Anterior | 1.4 ± 0.2 | 1.4 ± 0.1 | .719 |
| Middle | 1.3 ± 0.1 | 1.3 ± 0.2 | .628 |
| Posterior | 1.4 ± 0.1 | 1.4 ± 0.2 | .793 |
| Thickness (glenoid side), mm | |||
| Anterior | 1.3 ± 0.2 | 1.4 ± 0.1 | .067 |
| Middle | 1.3 ± 0.1 | 1.3 ± 0.2 | .966 |
| Posterior | 1.3 ± 0.1 | 1.4 ± 0.2 | .192 |
aData are presented as mean ± SD. LGHI, labrum glenoid height index; MRI, magnetic resonance imaging.
Discussion
To our knowledge, this was the first study that compared pre- and postoperative shoulder function and active ROM between 2 sexes to evaluate sex-based differences in clinical outcomes of arthroscopic anterior shoulder stabilization. This study serially evaluated the clinical outcomes after arthroscopic anterior shoulder stabilization and analyzed the sex-based differences in them. The most important finding was that most clinical outcomes of women were no worse than those of men and that women had even greater improvements in shoulder function scores and active ROM.
Three factors—physiological, psychological, and social—may be related to the present findings. In terms of physiological factors, the reported anatomic difference between male and female glenohumeral joints lies in the glenoid anatomy and humeral head size but not in joint laxity and glenohumeral relationships.19,33,38 The glenoid of women is smaller, taller, and thinner than that of men. The oval-shaped glenoid makes women more prone to shoulder instability, especially multidirectional shoulder instability.9,41 Based on the MRI assessments in this study, there was no difference in the labrum and cartilage thickness between the sexes. It was suggested that structural similarities might not affect the clinical outcomes, including the recurrence rate of women.
In terms of psychological factors, women might be more sensitive to pain and apprehensiveness about the disease. In this study, postoperative SST scores of the female patients were significantly lower than those of the male patients, although other postoperative functional scores and active ROM of the female patients were similar to or higher than those of the male patients. This might be because the SST score consists of 12 yes or no questions about whether the patient can perform activities of daily living, which are supposed to be answered by the patients. Lacking testing data with sufficient measurement properties, this score mainly focuses on the subjective feelings of the patients.1 However, the subjective satisfaction of female patients with shoulder instability or other shoulder diseases has been reported to be insufficient compared with male patients. Largacha et al18 conducted a study reporting 2674 patients having 1 of the 16 most prevalent shoulder diagnoses. The results showed that sex had a differential effect on the self-assessments, in which female patients tended to identify greater deficits in comfort and the SST score than male patients. A deficit in comfort was also found in female patients undergoing rotator cuff decompression or rotator cuff repair. Razmjou et al31 found that female candidates for rotator cuff—related surgeries reported more frustration and depression because of the shoulder as well as more anxiety about the effect of their shoulder’s condition on their occupation.
Notably, the preoperative Constant score of women was lower than that of men in this study. According to the literature, certain shoulder functional scores can be biased by sex, such as the Constant score. Brinker et al6 investigated 120 healthy collegiate or recreational athletes and found that men had significantly higher Constant scores than women, primarily because of the strength subscale. In contrast, the pre-1994 ASES score and OSIS had mostly negligible variance attributable to sex.6 Therefore, it was suggested that examiners should adopt the Constant score with caution when evaluating patients of different sexes, as women might be underestimated because of their inferior physical strength. Furthermore, the present results gave a hint that the change in Constant score from preoperatively to postoperatively, rather than absolute value, might be more precise for analyzing the difference in therapeutic efficacy of arthroscopic stabilization between sexes.
In terms of social factors, women’s activity intensity is lower than that of men in both daily life and sports, regardless of professional athletes. For preferred sports, women are less likely to engage in contact sports than men. Meanwhile, men are larger, so involvement in contact sports results in higher forces to the shoulder. As in this study, the contact sports participation rate of women was significantly lower than that of men (P = .001). Low postoperative activity intensity and rare participation in contact sports result in a lower risk of recurrence.24,35
Based on this study, advice for future sex-related investigation regarding shoulder function after arthroscopic stabilization can be offered. First and foremost, the shoulder functional scores that are less affected by sex, such as the Rowe score, ASES score, and OSIS, are recommended to reduce bias. Besides, more attention should be paid to the postoperative recovery of shoulder function and active ROM in male patients, as they might not get the desired improvements in shoulder function and active ROM compared with female patients. Last but not least, physiological, psychological, and social factors should all be taken into consideration when counseling patients before and after surgery to ensure suitable treatment and rehabilitation based on the sex difference in clinical outcomes.
There were some limitations in the current study. First, biases and inaccuracies associated with retrospective studies could not be avoided. Second, like other shoulder instability cohort studies, the rate of female patients enrolled was lower than that reported in epidemiology studies. As a result, the number of female patients was relatively small. Further study with a larger sample size for female patients in the general population is needed. Third, the lack of preoperative ASES score, SST score, OSIS, and SANE score made a more detailed comparison of pre- and postoperative shoulder function impossible.
Conclusion
Women have similar recurrence rates to men after anterior shoulder stabilization. Most postoperative clinical outcome measures showed no significant difference. Despite worse preoperative values, women showed significantly greater improvements in postoperative shoulder function and active ROM compared with men.
Footnotes
Final revision submitted November 19, 2020; accepted December 21, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: Funding for this study was received from the National Key R&D Program of China (2016YFC1100300), the National Natural Science Foundation of China (Nos. 81572108, 81772339, 8181101445, 81811530750, 81811530389, and 81972129), the Key Clinical Medicine Center of Shanghai (2017ZZ01006), the Sanming Project of Medicine in Shenzhen (SZSM201612078), the Shanghai Rising-Star Project (18QB1400500), and the Introduction Project of Clinical Medicine Expert Team for Suzhou (SZYJTD201714), Development Project of Shanghai Peak Disciplines-Integrative Medicine (20180101), and Shanghai Committee of Science and Technology (19441901600 and 19441902000). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Huashan Hospital, affiliated with Fudan University Institutional Review Board (HIRB No. 2019-410).
References
- 1. Angst F, Schwyzer HK, Aeschlimann A, Simmen BR, Goldhahn J. Measures of adult shoulder function: Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH) and its short version (QuickDASH), Shoulder Pain and Disability Index (SPADI), American Shoulder and Elbow Surgeons (ASES) Society standardized shoulder assessment form, Constant (Murley) Score (CS), Simple Shoulder Test (SST), Oxford Shoulder Score (OSS), Shoulder Disability Questionnaire (SDQ), and Western Ontario Shoulder Instability Index (WOSI). Arthritis Care Res (Hoboken). 2011;63(suppl 11):S174–S188. [DOI] [PubMed] [Google Scholar]
- 2. Balg F, Boileau P. The Instability Severity Index Score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007;89(11):1470–1477. [DOI] [PubMed] [Google Scholar]
- 3. Beaton DE, Richards RR. Measuring function of the shoulder. A cross-sectional comparison of five questionnaires. J Bone Joint Surg Am. 1996;78(6):882–890. [DOI] [PubMed] [Google Scholar]
- 4. Bernhardson AS, Murphy CP, Aman ZS, LaPrade RF, Provencher MT. A prospective analysis of patients with anterior versus posterior shoulder instability: a matched cohort examination and surgical outcome analysis of 200 patients. Am J Sports Med. 2019;47(3):682–687. [DOI] [PubMed] [Google Scholar]
- 5. Bradley JP, Arner JW, Jayakumar S, Vyas D. Risk factors and outcomes of revision arthroscopic posterior shoulder capsulolabral repair. Am J Sports Med. 2018;46(10):2457–2465. [DOI] [PubMed] [Google Scholar]
- 6. Brinker MR, Cuomo JS, Popham GJ, O’Connor DP, Barrack RL. An examination of bias in shoulder scoring instruments among healthy collegiate and recreational athletes. J Shoulder Elbow Surg. 2002;11(5):463–469. [DOI] [PubMed] [Google Scholar]
- 7. Brophy RH, Hettrich CM, Ortiz S, Wolf BR. Patients undergoing shoulder stabilization surgery have elevated shoulder activity compared with sex- and age-matched healthy controls. Sports Health. 2016;9(1):59–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16(7):677–694. [DOI] [PubMed] [Google Scholar]
- 9. Carter CW, Ireland ML, Johnson AE, et al. Sex-based differences in common sports injuries. J Am Acad Orthop Surg. 2018;26(13):447–454. [DOI] [PubMed] [Google Scholar]
- 10. Constant CR, Gerber C, Emery RJ, et al. A review of the Constant score: modifications and guidelines for its use. J Shoulder Elbow Surg. 2008;17(2):355–361. [DOI] [PubMed] [Google Scholar]
- 11. Cronin KJ, Wolf BR, Magnuson JA, et al. The prevalence and clinical implications of comorbid back pain in shoulder instability: a Multicenter Orthopaedic Outcomes Network (MOON) shoulder instability cohort study. Orthop J Sports Med. 2020;8(2):2325967119894738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dawson J, Rogers K, Fitzpatrick R, Carr A. The Oxford shoulder score revisited. Arch Orthop Trauma Surg. 2009;129(1):119–123. [DOI] [PubMed] [Google Scholar]
- 13. Hauger O, Dumont E, Chateil JF, Moinard M, Diard F. Water excitation as an alternative to fat saturation in MR imaging: preliminary results in musculoskeletal imaging. Radiology. 2002;224(3):657–663. [DOI] [PubMed] [Google Scholar]
- 14. Jakobsen BW, Johannsen HV, Suder P, Sojbjerg JO. Primary repair versus conservative treatment of first-time traumatic anterior dislocation of the shoulder: a randomized study with 10-year follow-up. Arthroscopy. 2007;23(2):118–123. [DOI] [PubMed] [Google Scholar]
- 15. Kaipel M, Reichetseder J, Schuetzenberger S, Hertz H, Majewski M. Sex-related outcome differences after arthroscopic shoulder stabilization. Orthopedics. 2010;33(3). [DOI] [PubMed] [Google Scholar]
- 16. Kraeutler MJ, McCarty EC, Belk JW, et al. Descriptive epidemiology of the MOON shoulder instability cohort. Am J Sports Med. 2018;46(5):1064–1069. [DOI] [PubMed] [Google Scholar]
- 17. Lansdown DA, Cvetanovich GL, Zhang AL, et al. Risk factors for intra-articular bone and cartilage lesions in patients undergoing surgical treatment for posterior instability. Am J Sports Med. 2020;48(5):1207–1212. [DOI] [PubMed] [Google Scholar]
- 18. Largacha M, Parsons IM IV, Campbell B, et al. Deficits in shoulder function and general health associated with sixteen common shoulder diagnoses: a study of 2674 patients. J Shoulder Elbow Surg. 2006;15(1):30–39. [DOI] [PubMed] [Google Scholar]
- 19. Merrill A, Guzman K, Miller SL. Gender differences in glenoid anatomy: an anatomic study. Surg Radiol Anat. 2009;31(3):183–189. [DOI] [PubMed] [Google Scholar]
- 20. Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11(6):587–594. [DOI] [PubMed] [Google Scholar]
- 21. Moore TK, Hurley ET, Rowe DN, et al. Outcomes following arthroscopic Bankart repair in female patients. J Shoulder Elbow Surg. 2020;29(7):1332–1336. [DOI] [PubMed] [Google Scholar]
- 22. Nakagawa S, Iuchi R, Mae T, Mizuno N, Take Y. Clinical outcome of arthroscopic Bankart repair combined with simultaneous capsular repair. Am J Sports Med. 2017;45(6):1289–1296. [DOI] [PubMed] [Google Scholar]
- 23. Olds M, Ellis R, Donaldson K, Parmar P, Kersten P. Risk factors which predispose first-time traumatic anterior shoulder dislocations to recurrent instability in adults: a systematic review and meta-analysis. Br J Sports Med. 2015;49(14):913–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Olds MK, Ellis R, Parmar P, Kersten P. Who will redislocate his/her shoulder? Predicting recurrent instability following a first traumatic anterior shoulder dislocation. BMJ Open Sport Exerc Med. 2019;5(1):e000447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ozturk BY, Maak TG, Fabricant P, et al. Return to sports after arthroscopic anterior stabilization in patients aged younger than 25 years. Arthroscopy. 2013;29(12):1922–1931. [DOI] [PubMed] [Google Scholar]
- 26. Park I, Oh MJ, Shin SJ. Minimal clinically important differences and correlating factors for the Rowe score and the American Shoulder and Elbow Surgeons score after arthroscopic stabilization surgery for anterior shoulder instability. Arthoscopy. 2019;35(1):54–59. [DOI] [PubMed] [Google Scholar]
- 27. Park MJ, Tjoumakaris FP, Garcia G, Patel A, Kelly JD IV. Arthroscopic remplissage with Bankart repair for the treatment of glenohumeral instability with Hill-Sachs defects. Arthroscopy. 2011;27(9):1187–1194. [DOI] [PubMed] [Google Scholar]
- 28. Patzkowski JC, Dickens JF, Cameron KL, et al. Pathoanatomy of shoulder instability in collegiate female athletes. Am J Sports Med. 2019;47(8):1909–1914. [DOI] [PubMed] [Google Scholar]
- 29. Porcellini G, Campi F, Pegreffi F, Castagna A, Paladini P. Predisposing factors for recurrent shoulder dislocation after arthroscopic treatment. J Bone Joint Surg Am. 2009;91(11):2537–2542. [DOI] [PubMed] [Google Scholar]
- 30. Randelli P, Ragone V, Carminati S, Cabitza P. Risk factors for recurrence after Bankart repair a systematic review. Knee Surg Sports Traumatol Arthrosc. 2012;20(11):2129–2138. [DOI] [PubMed] [Google Scholar]
- 31. Razmjou H, Holtby R, Myhr T. Gender differences in quality of life and extent of rotator cuff pathology. Arthroscopy. 2006;22(1):57–62. [DOI] [PubMed] [Google Scholar]
- 32. Rowe CR, Zarins B. Recurrent transient subluxation of the shoulder. J Bone Joint Surg Am. 1981;63(6):863–872. [PubMed] [Google Scholar]
- 33. Tackett JJ, Ablove RH. Magnetic resonance imaging study of glenohumeral relationships between genders. J Shoulder Elbow Surg. 2011;20(8):1335–1339. [DOI] [PubMed] [Google Scholar]
- 34. Tashjian RZ, Hung M, Keener JD, et al. Determining the minimal clinically important difference for the American Shoulder and Elbow Surgeons score, Simple Shoulder Test, and visual analog scale (VAS) measuring pain after shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26(1):144–148. [DOI] [PubMed] [Google Scholar]
- 35. Torrance E, Clarke CJ, Monga P, Funk L, Walton MJ. Recurrence after arthroscopic labral repair for traumatic anterior instability in adolescent rugby and contact athletes. Am J Sports Med. 2018;46(12):2969–2974. [DOI] [PubMed] [Google Scholar]
- 36. Torrens C, Guirro P, Santana F. The minimal clinically important difference for function and strength in patients undergoing reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25(2):262–268. [DOI] [PubMed] [Google Scholar]
- 37. van der Linde JA, van Kampen DA, Terwee CB, et al. Long-term results after arthroscopic shoulder stabilization using suture anchors: an 8- to 10-year follow-up. Am J Sports Med. 2011;39(11):2396–2403. [DOI] [PubMed] [Google Scholar]
- 38. Voycheck CA, Rainis EJ, McMahon PJ, Weiss JA, Debski RE. Effects of region and sex on the mechanical properties of the glenohumeral capsule during uniaxial extension. J Appl Physiol (1985). 2010;108(6):1711–1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wasserstein DN, Sheth U, Colbenson K, et al. The true recurrence rate and factors predicting recurrent instability after nonsurgical management of traumatic primary anterior shoulder dislocation: a systematic review. Arthroscopy. 2016;32(12):2616–2625. [DOI] [PubMed] [Google Scholar]
- 40. Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med. 1999;27(2):214–221. [DOI] [PubMed] [Google Scholar]
- 41. Wolf JM, Cannada L, Van Heest AE, O’Connor MI, Ladd AL. Male and female differences in musculoskeletal disease. J Am Acad Orthop Surg. 2015;23(6):339–347. [DOI] [PubMed] [Google Scholar]
- 42. Xiao H, Chen S, Chen J, Hua Y, Li Y. Arthroscopy combined with modified remplissage procedure for treating recurrent traumatic anterior shoulder instability with Hill-Sachs lesion. Chin J Sports Med. 2012;31(5):379–385. [Google Scholar]
- 43. Yoo JC, Lee YS, Tae SK, et al. Magnetic resonance imaging appearance of a repaired capsulolabral complex after arthroscopic Bankart repair. Am J Sports Med. 2008;36(12):2310–2316. [DOI] [PubMed] [Google Scholar]


