Abstract
Background:
The axillary nerve is at risk for iatrogenic injuries in surgical procedures involving the lateral aspect of the shoulder joint. To date and to our knowledge, there have been no studies that have compared the relevant distances in the common arm abduction positions used in these types of surgery as well as the relative risks of each position.
Purpose:
To evaluate the effect of arm abduction position on the distance from the acromion process to the axillary nerve in the common abducted arm positions.
Study Design:
Descriptive laboratory study.
Methods:
The shoulders of 10 fresh-frozen, full-body cadaveric specimens were used. A saber incision was made at the anterolateral edge of the acromion, and the anterior branch of the axillary nerve was identified. The distance between the anterolateral edge of the acromion process and the axillary nerve was measured 3 times in each of 4 positions: with the arm at the side as well as at 30°, 60°, and 90° of abduction. Then, the same procedure was performed from the midlateral and the posterolateral edges of the acromion process. The distances of the acromion process to the axillary nerve in the 4 positions were compared using 2-way analysis of variance.
Results:
The mean distances from the anterolateral edge of the acromion process to the anterior branch of the axillary nerve were 52.76 ± 4.64 mm with the arm at the side, 49.48 ± 4.77 mm at 30° of abduction, 46.00 ± 4.75 mm at 60° of abduction, and 42.88 ± 4.59 mm at 90° of abduction. There was a significant decrease in the distance from the anterolateral edge of the acromion process to the axillary nerve as the abduction angle of the arm increased from 0° to 60°, 0° to 90°, and 30° to 90° (P < .05).
Conclusion:
The distances from the acromion process to the axillary nerve were shorter in all abducted arm positions than with the arm at the side.
Clinical Relevance:
To avoid iatrogenic axillary nerve injuries, surgeons should be aware of the safe zone based on the shortest distance from the acromion process to the axillary nerve to ensure no accidental damage to this structure instead of using the mean distance of 5 cm.
Keywords: arm positions, axillary nerve, iatrogenic, surgery
The anterior branch of the axillary nerve winds along the neck of the humerus beneath the deltoid muscle and crosses perpendicularly to the deltoid fiber. This structure is at risk for iatrogenic injuries in surgical procedures involving the lateral aspect of the shoulder joint such as open or closed reduction; internal fixation of a proximal humeral fracture with a locking plate or intramedullary nail fixation by open, minimally invasive, or percutaneous techniques; percutaneous external fixation; or subdeltoid bursectomy for subdeltoid bursitis or double-row rotator cuff repair.5,7–9,12 In both open and minimally invasive procedures, common incisions are the anterolateral and midlateral incisions, which both use the acromion process as a reference. For the percutaneous technique, stab incisions for inserting screws are made at the antero-, mid-, and posterolateral aspects of the shoulder joint, depending on the plate and nail designs from various manufacturers. To avoid iatrogenic injuries of the anterior branch of the axillary nerve, the recommended safe zone for this area is 5 cm below the acromion process, as the average distance between the acromion process and the axillary nerve is 5 to 7 cm.1,3,4,6,11 However, even though this guide is well-known to surgeons, the incidence of iatrogenic axillary nerve injuries by making an anterolateral incision in the shoulder is 7.0% to 12.7%.7,10,11 This can occur because the distance may be affected by the arm abduction position during surgery. The anterior branch of the axillary nerve is located at the subdeltoid area, and the exact location of the nerve can vary with different arm abduction positions.
There is only 1 study that has evaluated the distances between the anterolateral edge of the acromion process and the axillary nerve in 2 arm positions: with the arm at the side and at 90° of abduction.6 That study found that the distance from the acromion process to the axillary nerve in the 90° abducted arm position was shorter than with the arm at the side.6 However, the results of these 2 positions are not applicable to all surgical procedures because some procedures are easier to perform in a 30° abducted arm position such as subdeltoid bursectomy or double-row rotator cuff repair.
To our knowledge, no previous studies have examined the distance between the acromion process and the anterior branch of the axillary nerve in various degrees of arm abduction, and we felt that this specific information would be very useful in helping to decrease the incidence of iatrogenic axillary nerve injuries. Therefore, the purpose of this study was to evaluate the effect of arm positioning on the distances from the antero-, mid-, and posterolateral edges of the acromion process to the axillary nerve in various arm abduction positions.
Methods
A total of 10 adult fresh-frozen full-body cadaveric specimens were used for the study: 5 male and 5 female specimens with a mean age at death of 63.5 ± 6.7 years. All cadaveric specimens were obtained from the anatomy department of our university. Specimens with obvious lesions of the shoulder and/or proximal humerus were excluded from the selection process. The mean height of the cadaveric specimens was 168.0 ± 7.2 cm, and the mean length of each arm, measured from the midlateral acromion process to the lateral epicondyle in the arm-at-the-side position, was 288.51 ± 6.90 mm. Each specimen was thawed at room temperature for 10 hours before being used, and the study was conducted with the specimens in the supine position with both arms at the sides.
Before the main study, a pilot study was performed to assess any differences in distances from the acromion process to the axillary nerve with the arms in the 4 study positions: with the arm at the side as well as at 30°, 60°, and 90° of abduction in both the beach-chair and the supine positions. There were no significant differences in the distance of each arm position between the beach-chair and supine positions, and thus, we decided to perform all measurements for the study with the specimens in the supine position. Overall, 3 distances were measured in each arm position: from the anterolateral edge, the midlateral edge, and the posterolateral edge of the acromion process to the axillary nerve (Figure 1). All procedures and measurements were performed using a standardized protocol by 1 experienced microneurovascular orthopaedic surgeon, who was not on the study team. Before making the incision, the upper arm length was measured from the midlateral acromion process to the lateral epicondyle. An 8 cm–long saber incision was made at the anterolateral edge of the acromion in a longitudinal direction, and the deltoid muscle was carefully dissected along the deltoid fiber. The anterior branch of the axillary nerve was then identified and looped with a vascular suture. The distance between the anterolateral edge of the acromion process and the anterior branch of the axillary nerve was measured 3 times with the arm at the side. Then, the arm was moved to 30°, 60°, and 90° of abduction, and the same measurements were performed. When measurements for an arm position were complete, before moving the arm to the next position, it was repositioned in the arm-at-the-side position. Each arm abduction position was standardized by a universal goniometer. After the completion of measurements, the deltoid muscle was repaired, and the skin was closed layer by layer. The same procedure was then performed with the incision made to expose the midlateral edge and then the posterolateral edge of the acromion process. All distances in the 4 arm positions were measured using a vernier caliper with a precision of 0.001 mm (Insize).
Figure 1.
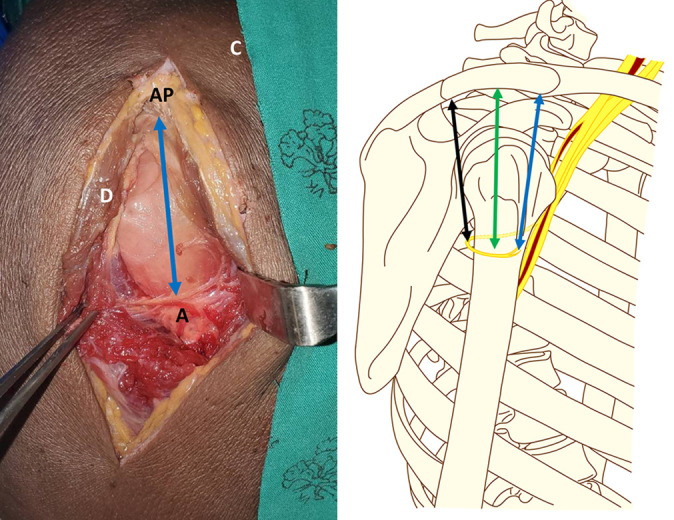
Measurement of the distances from the anterolateral edge (blue arrow), midlateral edge (green arrow), and posterolateral edge (black arrow) of the acromion process to the anterior branch of the axillary nerve. A, anterior branch of the axillary nerve; AP, acromion process; C, clavicle; D, deltoid muscle.
Each distance was measured by 1 orthopaedic surgeon (C.C.) 3 times, and the mean ± SD was calculated. Statistical analysis was performed with the R program and epicalc package (Version 3.4.3; R Foundation for Statistical Computing). Also, 2-way analysis of variance was used to determine the effect of the locations of the incision and the arm positions on the distance from the acromion process to the axillary nerve. P = .05 was considered significant.
Results
The mean distances from the acromion process to the axillary nerve are summarized in Table 1 and Figure 2, which show that there were no interaction effects between the location of the incision and the arm position (P = .994). Only the arm position affected the distance from the acromion process to the anterior branch of the axillary nerve, as all distances decreased in the arm abduction positions (P < .001).
Table 1.
Distance From the Acromion Process to the Anterior Branch of the Axillary Nerve in Each Arm Position
| Mean ± SD, mm | Minimum, mm | |
|---|---|---|
| Anterolateral edge | ||
| Arm at side | 52.76 ± 4.64 | 45.49 |
| 30° of abduction | 49.48 ± 4.77 | 42.75 |
| 60° of abduction | 46.00 ± 4.75 | 40.07 |
| 90° of abduction | 42.88 ± 4.59 | 36.87 |
| Midlateral edge | ||
| Arm at side | 52.20 ± 4.21 | 46.07 |
| 30° of abduction | 49.66 ± 4.54 | 43.37 |
| 60° of abduction | 46.39 ± 4.23 | 40.33 |
| 90° of abduction | 42.90 ± 4.11 | 37.00 |
| Posterolateral edge | ||
| Arm at side | 53.86 ± 4.77 | 45.40 |
| 30° of abduction | 50.83 ± 4.83 | 43.55 |
| 60° of abduction | 47.34 ± 4.23 | 40.51 |
| 90° of abduction | 43.28 ± 4.06 | 36.48 |
Figure 2.
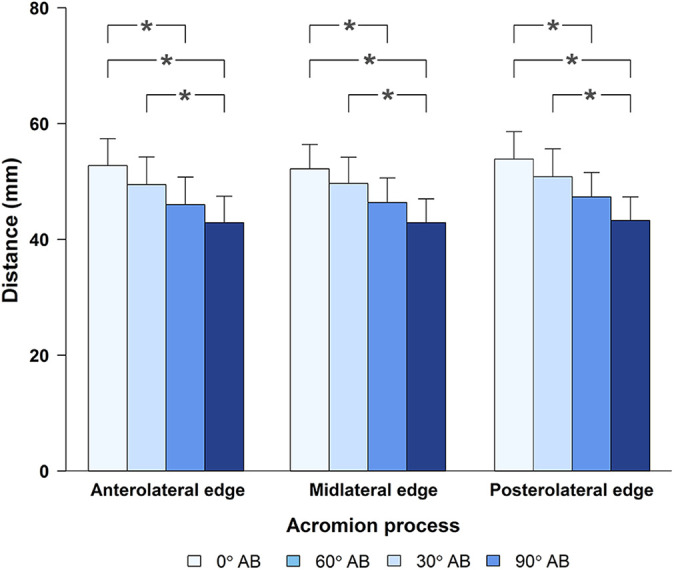
Distances from the antero-, mid-, and posterolateral edges of the acromion process to the anterior branch of the axillary nerve in each arm position. *P < .05. AB, abduction.
The distance significantly decreased from the antero-, mid-, and posterolateral edges of the acromion process to the axillary nerve as the abduction angle of the arm increased from 0° to 60°, from 0° to 90°, and from 30° to 90° (Figure 2).
Discussion
In our study, we found that in all 3 arm abduction positions—30°, 60°, and 90°—the distances from the antero-, mid-, and posterolateral edges of the acromion process to the axillary nerve were shorter than with the arm at the side. The shortest distance from the antero-, mid-, and posterolateral edges of the acromion process to the axillary nerve in all 4 arm positions was less than 5 cm.
In open and minimally invasive plate surgery involving proximal humeral fixation, there is a risk of iatrogenic injuries to the anterior branch of the axillary nerve with the anterolateral incision. The mean distance between the anterolateral edge of the acromion process and the axillary nerve was 52.76 ± 4.64 mm with the arm at the side, which was similar to the results of Abhinav et al,1 Vathana et al,11 and Gosavi et al.6 These distances were shorter as the arm abduction angle increased, for which the mean distances were 49.48 ± 4.77 mm at 30° of abduction, 46.00 ± 4.75 mm at 60° of abduction, and 42.88 ± 4.59 mm at 90° of abduction. The safe zone in this area has been accepted as 5 cm from the acromion process, but as our study shows, it cannot be ascertained that iatrogenic axillary nerve injuries will always be avoided using this value. Kongcharoensombat and Wattananon7 made a 5-cm saber incision from the anterolateral edge of the acromion process and found that the incidence of inadvertent iatrogenic injuries to the anterior branch of the axillary nerve was 12.7% (10/79 patients). The realistic safe zone within which an anterolateral incision can be made is the shortest distance from the anterolateral edge of the acromion process to the axillary nerve, which our study found to be 45.49 mm with the arm at the side, 42.75 mm at 30° of arm abduction, and 40.07 mm at 60° of arm abduction. Based on our findings, we suggest that the “magic” value for the safe zone should be changed from 5 cm below the acromion process to 4 cm below the acromion process.
For percutaneous fixation of a proximal humeral fracture by plating and nailing, the direction of screw fixation depends on the design of the plate, which in turn depends on the manufacturer. Yet, in all designs, there are 3 starting positions from which the fixation screw can be initiated: the anterolateral, midlateral, and posterolateral lines arising from the lateral aspect of the shoulder joint. There are 2 studies that have evaluated the risk of injuries to the iatrogenic anterior branch of the axillary nerve in percutaneous proximal humeral plate fixation using the PHILOS plate (Synthes), reporting that the screws in the third to fifth rows had a risk of axillary nerve injuries.5,9 The surgeon needs to consider the location of the incision and the arm position while making the incision, drilling the bone, and inserting the screws. If the incision is outside of the safe zone, the surgeon should minimize the possibility of iatrogenic axillary nerve injuries by carefully dissecting the deltoid muscle to identify and protect the nerve.
Arthroscopic surgery is often performed in the subdeltoid area, with the most common procedure being subdeltoid bursectomy in cases of subdeltoid bursitis and double-row rotator cuff repair. These procedures involve the chance of unintentionally injuring the anterior branch of the axillary nerve. Beals et al2 reported that the distance from the midpoint of the acromion process to the subdeltoid bursa was 4.0 ± 1.0 cm, which was close to the axillary nerve. The surgeon performing this procedure usually abducts the arm of the patient to increase the space of the subdeltoid area, which in turn decreases the distance between the axillary nerve and the acromion process, resulting in the risk of iatrogenic axillary nerve injuries. In this study, we evaluated the distances from the anterolateral, midlateral, and posterolateral edges of the acromion process to the axillary nerve in the 4 most common arm positions, and surgeons can reduce the likelihood of axillary nerve injuries by using the results from this study.
The results from this study may not only be used in orthopaedic surgery, but they can also assist in locating the safe zone for an intramuscular injection over the deltoid area. Normally, nurses and doctors use the landmark of 2 finger breadths below the acromion process, and our study confirms that this landmark is safe for intramuscular injections over the deltoid area in the arm-at-the-side and 30° of arm abduction positions.
This study had some limitations. First, in actual proximal humeral fractures, the distances from the acromion process to the axillary nerve may be different from the results of this study, as in real-life situations, displacement of the fracture fragment and the degree of soft tissue injury around the shoulder joint will affect these distances. Second, we had no way of knowing if there were preexisting conditions of the shoulder and/or proximal humerus in the cadaveric specimens, but any specimens with obvious lesions of the shoulder and proximal humerus were removed from the study. Third, in a study such as this, there is a risk that the anatomic relationship between the acromion process and the axillary nerve may be disturbed by dissection. We tried to decrease this possibility by having all dissections performed by 1 well-experienced microneurovascular orthopaedic surgeon.
Conclusion
The distances from the acromion process to the axillary nerve were affected by the position of the arm. The surgeon should keep in mind that in arm abduction positions, the axillary nerve is brought closer to the acromion process.
Acknowledgment
The authors sincerely thank Wirachai Samai, head of the Department of Pathology, and their assistants for arranging the supply of cadaveric specimens; Boonsin Trangtrakulwanich of the Department of Orthopedics and Nannapat Pruhetkaew of the Department of Epidemiology for providing statistical consulting and support; and Dave Patterson of the Office of International Affairs for his assistance in English editing.
Footnotes
Final revision submitted December 8, 2020; accepted January 12, 2021.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was waived for the present study (REC 63-056-11-1).
References
- 1. Abhinav G, Sivaraman B, Matthew N, Grahame JST. A contribution to the calculation of a safe deltoid split. Int J Shoulder Surg. 2008;2(3):52–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Beals TC, Harryman DT, 2nd, Lazarus MD. Useful boundaries of the subacromial bursa. Arthroscopy. 1998;14(5):465–470. [DOI] [PubMed] [Google Scholar]
- 3. Cetik O, Uslu M, Acar HI, Comert A, Tekdemir I, Cift H. Is there a safe area for the axillary nerve in the deltoid muscle? A cadaveric study. J Bone Joint Surg Am. 2006;88(11):2395–2399. [DOI] [PubMed] [Google Scholar]
- 4. Cheung S, Fitzpatrick M, Lee TQ. Effects of shoulder position on axillary nerve positions during the split lateral deltoid approach. J Shoulder Elbow Surg. 2009;18(5):748–755. [DOI] [PubMed] [Google Scholar]
- 5. Dang KH, Ornell SS, Reyes G, Hussey M, Dutta AK. A new risk to the axillary nerve during percutaneous proximal humeral plate fixation using the Synthes PHILOS aiming system. J Shoulder Elbow Surg. 2019;28(9):1795–1800. [DOI] [PubMed] [Google Scholar]
- 6. Gosavi SN, Jadhav SD, Zambre BR, Vatsalaswamy P. Location of axillary nerve in relation to acromion process of scapula: a cadaveric study. J Med Dent Sci. 2012;2(1):1–3. [Google Scholar]
- 7. Kongcharoensombat W, Wattananon P. Risk of axillary nerve injury in standard anterolateral approach of shoulder: cadaveric study. Malaysian Orthop J. 2018;12(3):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Perlmutter GS. Axillary nerve injury. Clin Orthop Relat Res. 1999;368:28–36. [PubMed] [Google Scholar]
- 9. Saran N, Bergeron SG, Benoit B, Reindl R, Harvey EJ, Berry GK. Risk of axillary nerve injury during percutaneous proximal humerus locking plate insertion using an external aiming guide. Injury. 2010;41(10):1037–1040. [DOI] [PubMed] [Google Scholar]
- 10. Ulucay C, Ozler T, Akman B. Treatment of acromioclavicular joint injuries in athletes and in young active patients. J Trauma Treat. 2016;5:1000344. [Google Scholar]
- 11. Vathana P, Chiarapattanakom P, Ratanalaka R, Vorasatit P. The relationship of the axillary nerve and the acromion. J Med Assoc Thai. 1998;81(12):953–957. [PubMed] [Google Scholar]
- 12. Westphal T, Woischnik S, Adolf D, Feistner H, Piatek S. Axillary nerve lesions after open reduction and internal fixation of proximal humeral fractures through an extended lateral deltoid-split approach: electrophysiological findings. J Shoulder Elbow Surg. 2017;26(3):464–471. [DOI] [PubMed] [Google Scholar]


