Abstract
Background:
Maintaining essential HIV services has being a Global challenge during the COVID-19 crises. Myanmar has 54 million inhabitants. Neighbor of China, Thailand, India and Bangladesh it was impacted by COVID-19, but came up with a comprehensive and effective response, following WHO recommendations. The HIV Prevalence is 0.58% and it is concentrated among key population. A HIV Contingency Plan was developed to face this challenge.
Methodology:
The programme-based cross-sectional descriptive study with analysis of routinely collected data from MoHS data system, between 2019 and 2020 was conducted, comparing first six months of 2019 and 2020.
Results:
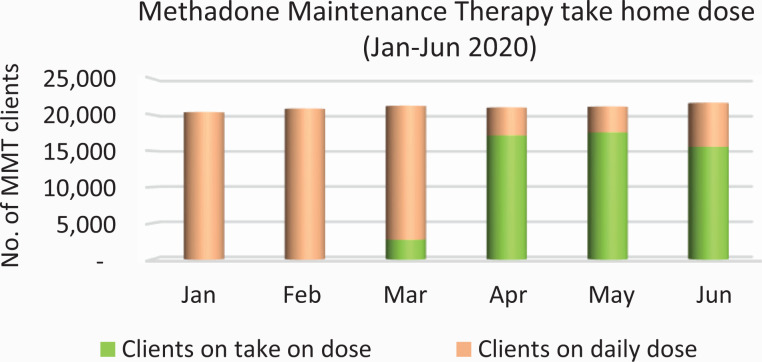
HIV outreach activities and HIV testing were slightly affected after detection of first COVID-19 case, till mid May 2020. After that, outreach activities resumed. Introduction of HIV self-testing was initiated. 72% of more than 21,000 PWID on MMT were receiving take home dose up to 14 days and 60% of ART patients were receiving 6 months ARV dispensing.
Conclusion:
Essential HIV services were maintained.
Keywords: Myanmar, COVID-19, HIV, contingence plan
What do we already know about this topic?
The maintenance of essential services for HIV during the COVID-19 Pandemic was a big global challenge and disruption of services was the rule, not the exception.
How does your research contribute to the field?
With the design and implementation of a specific HIV Contingence Plan we found a way to maintain essential services and use innovation as an additional tool
What are your research’s implications toward theory, practice, or policy?
The main impact can be in practice and policies for low- and middle-income countries, since we still have a long way to go to halt the COVID-19 Pandemic, and that successful outcomes can be used for any other emergently circumstances.
Introduction
Myanmar is a country in the South East Asian Region with 54 million inhabitants and an HIV Prevalence of 0.58%.1 The HIV epidemic in Myanmar is concentrated and affects mostly Key Populations (People Who Inject Drugs, Transgender People, Men Who Have Sex with Men, Sex Workers and Prisoners in that order) and their sexual partners.2
Despite the long standing challenge of HIV in the country, Myanmar is also known for a robust response to HIV supported by the Government and like-minded donors, including the Global Fund to Fight AIDS, Tuberculosis and Malaria (GFATM), US Presidential Emergency Plan Fund for AIDS Relief (PEPFAR), Access to Health, and the Japan Fund for Poverty Reduction through the Asian Development Bank (ADB). From the low- and middle-income countries in the region, Myanmar is one of a few that pays for more than 80% of the Antiretroviral (ARV) drugs freely provided in the country, plus 100% of all the methadone dispensed through the methadone maintenance treatment (MMT) program reaching more than 21,000 people from the Government’s budget.3
Based on the programme aggregate data at the end of 2019, approximately 85% of the estimated people living with HIV (PLHIV) in the country knew their status for HIV; among them 91% were on Antiretroviral Therapy (ART) and 94% of those on ART were virally suppressed.4 As noted in the UNAIDS Global Report, the country has now one of the best performances in the Asia and the Pacific region for the 90-90-90 global targets.5
The reports on a cluster of mysterious of COVID-19 cases in a neighboring country of Myanmar, and more precisely in Wuhan, capital of Hubei, China, became public in the end of 2019 and drove WHO to use International Health Regulations and declare a Public Health Emergency of International Concern on 30 January 2020.6
Myanmar detected its first two COVID-19 cases on 23 March 2020. Since early January of the same year, the Government of Myanmar introduced a series of public health control measures. These early efforts were aimed at increasing public awareness, introducing infection control, reducing the potential burden on the health care system and mitigating economic and social disruption. By that time, it was clear that this virus was affecting the entire world (already declared a Pandemic on March 11).7 It also became clear that it could seriously impact on the population of Myanmar. In response, the Ministry of Health and Sports developed contingency plans to reduce the impact on other essential health services, including a specific Contingency Plan was developed for HIV, to ensure maintaining essential services for the People Living with and Most Affected by HIV during this pandemic.
This paper reports on the Contingency Plan for HIV and its implementation in the first few months as an example on how low- and middle-income countries can work to provide essential services to People Living with HIV and Key Populations.
The Contingency Plan for HIV8 was designed in March and launched in April 2020. It was an initiative of the National AIDS Program (NAP) with support and participation from many stakeholders. A Rapid Response Team (RRT) for COVID-19 and HIV was also established to serve as a platform for coordination, monitoring and tracking of implementation of the HIV contingency plan. WHO, UNAIDS, US CDC and other technical partners, non-governmental organizations and representatives of the communities provided essential support to the development and follow-up of Contingency Plan and the Rapid Response Team. Funding support was provided for Covid-19 and HIV through the GFATM and, to a lesser extent, other multi and bilateral donors.
The three main objectives were:
To reduce the risk of contracting COVID-19 among PLHIV, Key Populations and other vulnerable populations.
To ensure the uninterrupted treatment for PLHIV and Methadone Maintenance Therapy (MMT) clients.
To minimize the exposure to COVID-19 of health service providers, including peer workers and community health volunteers.
The Plan was comprehensive and focused on the following strategies:
Community awareness
Prevention and Harm Reduction
Infection Control and disinfection measures
Antiretroviral Therapy (ART)
ART Patient Management
Community Involvement
Work Arrangements
For Community awareness, the Plan focused on social media and online communication which is popular in Myanmar and, in particular, Facebook) as well as classical printed materials to disseminate correct information about prevention of COVID-19; potential interaction of COVID-19 and HIV; and other information needed related to service-provision during the COVID-19 crises for HIV prevention, care & support as well as Opioid substitution therapy.
In prevention of HIV and Harm Reduction, the Plan highlighted the rationale of reducing outreach and drop-in center physical contacts and, at the same time, granting the continued provision of condoms and needles/syringes at fixed locations where they would be accessible and with a wide dissemination of information. A very important part of the Harm Reduction strategy was the provision of take-home doses of MMT, until then not widely applied in Myanmar. Before the COVID-19 crises, the MMT take-home doses was for the maximum of 7 days and achieved around 20-25% of the clients, and after the Contingence Plan implementation, it was extended to 14 days and achieved 70% of the clients.
The core intention of the infection control and disinfection measures was to ensure the safety and mitigate the risk of the health professionals dedicated to HIV prevention and continuum of care, including outreach workers, peers and volunteers. The Plan foresaw, early on, that one of the main potential challenges of the Pandemic would be the vulnerability of health professionals at large and, as a consequence, the disruption of essential services for PLHIV and Key Populations. Capacity building in infection prevention, the important provision of Personal Protective Equipment (PPE), the decrease in number of daily patients in services (by the changes on the dispensing cycles of ARV and MMT as examples) were some of the approaches adopted in the HIV Contingency Plan during the COVID-19 Pandemic. Another important strategy suggested in the Plan was the constant disinfection of the premises to make sure that no risk of transmission of COVID-19 was left on surfaces.
For People Living with HIV, ART is crucial in emergency circumstances. The first important action was mitigating the potential supply chain disruption to guarantee uninterrupted supply of ARV medicines and other commodities; preponing international shipping; expanding the storage capacity of warehouses; and the flow of the medicines to support the decisions on long-term take-home doses or multi-month dispensing (MMD) of ART. An important strategic shift was provided by the Care and Treatment Technical Working Group in changing the Guidelines for a dispensing to six months of ART for all the stable patients. Furthermore, the directions changed for new patients that got prescriptions initially for one month and after the first return visit were also included in the six months policy. It was clearly recommended not to change the regimens of stable patients, even for more updated ones (like changing from Efavirenz to Dolutegravir), to avoid any disruption if the patient did not adapt to new regimens. Priority was given for pregnant females, children and people who live far away from health services (like in remote rural areas), as an extra caution in case there was any problem on ARV provision. TB Preventive Therapy was also taken in account to make sure that the patients will access to the whole cycle without any disruption. Finally, it was suggested that investments were needed to renovate and adapt facilities to make feasible the stock of a greater quantity of medicines in their spaces.
The Plan also emphasized the importance of sharing information with PLHIV on how to manage availability of larger quantities of ARVs in their own homes. Another important topic was to guarantee that all patients were well informed about services that were opened and the closest to their homes while services were informed about patients that could request their support in this exceptional circumstance. Specifically, for the treatment of serious intercurrences or for the treatment of serious opportunist infections, patients were oriented where to go in case of lockdown or restrictions of circulation. Regarding Viral Load, considering the high demand from laboratory technicians and machines during the COVID-19 crises, it was necessary to define a prioritization of testing starting by Early Infant Diagnosis (EID) and considering focus on priority cases for Viral Load testing.
Another crucial aspect of the Plan was community involvement, including engaging community Networks, National and International NGOs from the beginning of the crises, considering their important role in the National Response to HIV. The main expected goal was to maintain essential work going (including core prevention activities conducted by them in “normal” times) as well as engaging them in the prevention of COVID-19 for PLHIV and Key Populations, disseminating correct and understandable information, doing peer support and helping their communities to keep safe access to needed services. Aspects like people who are under ARV or broader treatment in neighboring countries and were returning to Myanmar and their linkage to national care services were also part of this important aspect of the Contingency Plan.
The final topic consigned in the Plan was related to working arrangement aspects that are essential under the exceptional circumstances. The HIV-related workforce was re-organized by their schedule so as not to overwhelm the health facilities; the organization of a back-up workforce in case personnel and volunteers got infected by COVID-19 and were secluded from their workplace; the intense reduction of physical meetings, trainings or workshops; the expansion of online communication tools and strategy to guarantee participation; the extension of this approach to peer educators and community volunteers and the natural necessary postponement of activities that were not critical.
Methodology
The programme-based cross-sectional descriptive study with analysis of routinely collected data between 2019 and 2020 was conducted. Routine programme aggregate data of National AIDS Programme was reviewed comparing first six months of 2019 and 2020 and monthly trend of 2020. Situation updates from states/regions and communities at bi-weekly meeting of the Rapid Response Team (RRT) for COVID-19 and HIV were also included.
Results
The first results of the implementation of the HIV Contingency Plan were reviewed after four months of implementation during the first wave of COVID-19 in Myanmar which began in March 2020. Mitigation of impact on HIV service delivery efforts across the country were scaled-up under the leadership of the National AIDS Program (NAP) and the support from various stakeholders. State and regional NAP teams, donor and technical agencies, implementing partners and community networks worked closely to ensure uninterrupted essential HIV service delivery as much as possible.
HIV Prevention Services
The results of the same period in 2019 and 2020, January to June, were compared and analyzed to visualize the impact of COVID-19 on HIV prevention efforts. Based on Figures 1, 2 and 3, prevention outreach activities for sexual transmission were slightly affected and reduced after detection of first COVID-19 case till mid May 2020 while harm reduction activities were maintained the same momentum at the pre-COVID-19 period partly due to the fact that the States and Regions with predominantly harm reduction services were least affected by COVID-19. In addition, starting from mid-May, individual outreach activities by peers and community workers resumed for HIV prevention services and health education session were planned and conducted by limiting number of clients with less than 5 persons or one to one session. Outreach through online contacts is being designed to avoid face to face exposure considering confidentiality and the need for monitoring activities.
Figure 1.
Free needle and syringe distribution compared between 2019 and 2020 for the same period.
Figure 2.
Free condom distribution compared between 2019 and 2020 for the same period.
Figure 3.
HIV testing among key populations compared between 2019 and 2020 for the same period.
Information on HIV testing was provided by peers through information sharing through social media & hotline services. Counselling for HIV testing is provided via messenger, Viber or phone. The process to introduce HIV self-testing was also initiated and test-kit validation was performed by the National Reference Laboratory and this initiative was accelerated in order to promote accessibility to HIV Testing Services (HTS) services during COVID-19.
Drug Dependency Treatment and Research Unit (DDTRU) managed to provide take home Methadone doses for the clients. At the end of June 2020, 72% of clients were receiving take home doses with the majority getting 7 days and some up to 14 days (Figure 4).
Figure 4.
Number of MMT clients received take home doses from Jan to Jun 2020.
Continuum of HIV treatment
For the purpose of ensuring uninterrupted treatment especially for those who could face difficulty in accessing HIV services during COVID-19 restrictions, 6-month ARV dispensing was provided to PLHIV at ART facilities (both public and NGOs) across the country, including for inmates released from prison in April as part of an Amnesty for 25,000 inmates. Around 60% of PLHIV on ART were receiving 6-month ARV supplies as of June 2020. PLHIV on ART (nearly 800 patients) were able to refill ARV supply at nearest public ART facility since they could not visit their original ART site (public sector or NGO clinics) for follow up because of movement restriction. Community Networks (PLHIV and key population groups) worked together with the NAP and local health authorities to disseminate the update information on service accessibility and to facilitate ARV refill in case of quarantine measures or lockdowns.
Six hundred (600) Myanmar patients from near the India border seeking ART at MSF-Moreh (India) were accepted as transfer-in patients to be able to continue the treatment in ART sites nearest to their residence as the patients cannot cross the border during COVID-19. National PLHIV Network (Myanmar Positive Group) in collaboration with local peer groups, assisted to trace the patients to get enrolled into care. For ART patients from Myanmar and currently working in Thailand, ARV dispensing services were arranged at 2 cross-borders point: Myawaddy-Maesot and Tachileik-Mesai in collaboration with Thailand MoPH, Department of Immigration and NGOs working in the border area. In addition to that, HIV testing services were provided for returning migrant workers at border crossing points and HIV positive confirmed cases from this entry point were able to initiate ART within one week at ART facilities near to their residence.
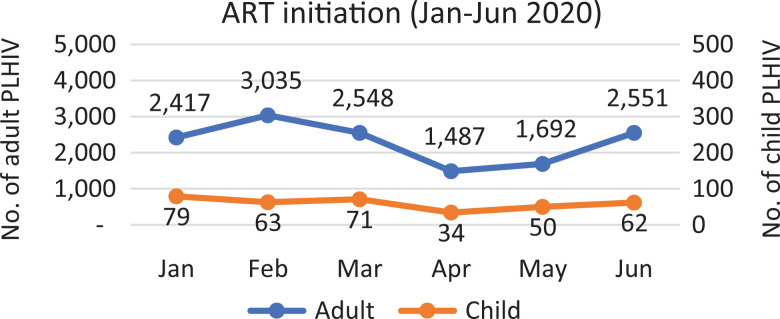
ART enrolment for new HIV positive clients continued. In April and May, ART initiation decreased to around 40% and increased back in June again (Figure 5). April has a long holiday due to Myanmar New Year Festival and it is the usual time that some of the services usually decrease.
Figure 5.
ART initiation from Jan to Jun 2020.
For routine viral load monitoring, it decreased due to delay of reagent shipment arrival and movement restriction of public transportation around April. After the arrival of reagents in May, viral load testing was able to resume. Yet the laboratories had to accommodate for COVID-19 testing in priority in terms of the health work force as well as the lab machines.
Infection Prevention and Control measures
 An Infection Prevention and Control (IPC) guidance for HIV service facilities and health care workers was developed and put in practice introducing critical IPC measures accordingly in-service delivery sites. The guidance included for decongesting patient load by scheduling appointments and patient triage, health care provider safety by segregation of the workforce, adapting clinic settings, PPE and disinfection procedure for clinics. COVID-19 preventive measures are displayed at HIV service facilities together with hand hygiene facilities. HIV service facilities were renovated for necessary environmental and distancing measures and physical distancing arrangement according to the IPC guidance. Commodities for IPC measures including infrared thermometers, hand-sanitizers, disinfectant solutions and PPE were provided to HIV service facilities with support from Global Fund COVID-19 Response Mechanism (C19RM) funding.
An Infection Prevention and Control (IPC) guidance for HIV service facilities and health care workers was developed and put in practice introducing critical IPC measures accordingly in-service delivery sites. The guidance included for decongesting patient load by scheduling appointments and patient triage, health care provider safety by segregation of the workforce, adapting clinic settings, PPE and disinfection procedure for clinics. COVID-19 preventive measures are displayed at HIV service facilities together with hand hygiene facilities. HIV service facilities were renovated for necessary environmental and distancing measures and physical distancing arrangement according to the IPC guidance. Commodities for IPC measures including infrared thermometers, hand-sanitizers, disinfectant solutions and PPE were provided to HIV service facilities with support from Global Fund COVID-19 Response Mechanism (C19RM) funding.
Monitoring of Implementation of Contingency Plan for HIV
The NAP organized weekly virtual meetings with their state and regional teams for situation updates and troubleshooting for field level implementation. Drug Dependency Treatment and Research Unit also organized regularly with the Drug Treatment Centers across the country. This RRT team for coordination and tracking implementation has been convening regular virtual meeting, inviting relevant NAP teams from State/Regional alternatively to facilitate necessary coordination and linkages, identify issues and solutions, and monitor overall progress to move forward based on update situations of COVID-19 in the country.
Discussion
During emergency crises, like the one we are facing with COVID-19, National Responses to HIV need to find ways to maintain, in priority, essential services provided for people living with HIV as well as for key populations. Myanmar, led by the NAP, but working jointly with support from the UN, bilateral, National and International NGOs with a strong focus and mobilization of the community, found alternative ways to keep the provision of ART, prevention and drug treatment services (including for PWID - whom are still the driving force of the epidemic in Myanmar) running. The participatory way of constructing a Contingency Plan that involved various key dimensions to not disrupt the National Response (Community awareness; Prevention and Harm Reduction; Infection Control and disinfection measures; Antiretroviral Therapy (ART); ART Patient management; Community Involvement and Administration) was a very important first step in the direction of securing that the continuity of key services were provided.
Countries that do not produce medicines, such as ARVs, methadone and do not produce all their need in essential protective equipment, condoms, needle and syringes, and other key products face challenges in the area of procurement and supply chain that are an important step to guarantee that the technical decisions – such as MMD of medicines – can be accomplished. That was made possible with the support of UNOPS as procurer for the Government of Myanmar of resources dedicated to ARVs, MMT, other medicines, medical supplies and equipment. An internal logistic improvement to face the crises added to the expansion of the deposits in some of the health units, were also critical to make this all feasible.
However, the success of this overall intervention would be almost impossible without the clear commitment of the communities most concerned by HIV and civil society in the design, implementation and continuous evaluation with bi-weekly meetings of the RRT.
Conclusion
Developing a clear and participatory Contingency Plan to face the HIV epidemic during the COVID-19 Pandemic was an important decision for Myanmar to ensure that essential services provided to PLHIV and key populations were not immobilized. Considering that Myanmar is a lower-middle income country (LMIC), strategic thinking and community involvement were crucial to make this Plan work and preserve lives plus maintain standards of health care at large (such as drug dependence treatment) and prevention activities ongoing.
The challenges and uncertainty will continue until we find a global solution for the COVID-19 Pandemic. Nevertheless, we will need to consider long-term changes in the HIV response given the ups and downs of this pandemic. As we wait for signs of the health and socio-economic recovery at some point, we must continue to explore ways to live with COVID-19 and its consequences over the next year and possibly beyond that. The commitment to not disrupt HIV-related services and mitigate to the maximum the impact of this emergency has been a positive and constructive response despite the difficult circumstances of 2020.
Acknowledgments
This paper was produced as a result of the contribution of many institutions and their people, that worked from the beginning in the strategic thinking, implementation, monitoring and evaluation. First, we would like to acknowledge the political direction of the Minister of Health and Sports, Dr Myint Htwe, who from the beginning highlighted the importance of the maintenance of essential health services regardless the importance of COVID-19. Colleagues from National and International NGOs are being essential in all phases of the work so far. They are represented in the authorship by the leader of the NGO of People Living with HIV in Myanmar (Myanmar Positive Group), Khin Mar Win. To Dr Stephan Jost, WHO Representative in Myanmar, who enabled the environment creating conditions to his HIV Team to work with given priority. To the US CDC colleagues based in Myanmar, particularly Dr Ei Ei Khin who was crucial in the weekly meetings for monitoring progress of the HIV Contingence Plan. To the colleagues from UNOPS and Save the Children for their great contribution to maintain the needed supply.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Fabio Mesquita  https://orcid.org/0000-0002-8297-0224
https://orcid.org/0000-0002-8297-0224
References
- 1. Myanmar National Strategic Plan on HIV and AIDS – (2021 – 2025), data from the AEM-Spectrum HIV estimates from April 2019. Ministry of Health and Sports, National AIDS Program, Myanmar; 2020.
- 2. National AIDS Program. 2016 HIV Estimates & Projections (National & Sub-National Levels). Myanmar, March 2018.
- 3. International AIDS Society. AIDS 2020. Oral presentation of Dr Htun Nyunt Oo, Manager of the National AIDS Program; June/July 2020.
- 4. Programme data 2019, National AIDS Programme. Myanmar, 2019. [Google Scholar]
- 5. UNAIDS Global Report 2020. Accessed January 11, 2021. https://www.unaids.org/sites/default/files/media_asset/2020_global-aids-report_en.pdf
- 6. WHO Declaration of COVID-19 as a Public Health Emergency, at. Switzerland: January 30, 2020. Accessed January 11, 2021. https://www.who.int/dg/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov). [Google Scholar]
- 7. WHO Declaration of COVID-19 as a Pandemic, at. Switzerland: March 11, 2020. Accessed January 11, 2021. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. [Google Scholar]
- 8. The Contingency Plan for HIV prevention, treatment and care in response of COVID-19. hNationsal AIDS Program Myanmar, April 2020. [Google Scholar]