Abstract
Background
The World Health Organization (WHO) recommends that people of all ages take regular and adequate physical activity. If unable to meet the recommendations due to health conditions, international guidance advises being as physically active as possible. Evidence from community interventions of physical activity indicate that people living with medical conditions are sometimes excluded from participation in studies. In this review, we considered the effects of activity‐promoting interventions on physical activity and well‐being in studies, as well as any adverse events experienced by participants living with inherited or acquired neuromuscular diseases (NMDs).
Objectives
To assess the effects of interventions designed to promote physical activity in people with NMD compared with no intervention or alternative interventions.
Search methods
On 30 April 2020, we searched Cochrane Neuromuscular Specialised Register, CENTRAL, Embase, MEDLINE, and ClinicalTrials.Gov. WHO ICTRP was not accessible at the time.
Selection criteria
We considered randomised or quasi‐randomised trials, including cross‐over trials, of interventions designed to promote physical activity in people with NMD compared to no intervention or alternative interventions. We specifically included studies that reported physical activity as an outcome measure. Our main focus was studies in which promoting physical activity was a stated aim but we also included studies in which physical activity was assessed as a secondary or exploratory outcome.
Data collection and analysis
We used standard Cochrane procedures.
Main results
The review included 13 studies (795 randomised participants from 12 studies; number of participants unclear in one study) of different interventions to promote physical activity. Most studies randomised a minority of invited participants. No study involved children or adolescents and nine studies reported minimal entry criteria for walking. Participants had one of nine inherited or acquired NMDs.
Types of intervention included structured physical activity support, exercise support (as a specific form of physical activity), and behaviour change support that included physical activity or exercise. Only one included study clearly reported that the aim of intervention was to increase physical activity. Other studies reported or planned to analyse the effects of intervention on physical activity as a secondary or exploratory outcome measure. Six studies did not report results for physical activity outcomes, or the data were not usable. We judged 10 of the 13 included studies at high or unclear risk of bias from incomplete physical activity outcome reporting.
We did not perform a meta‐analysis for any comparison because of differences in interventions and in usual care. We also found considerable variation in how studies reported physical activity as an outcome measure. The studies that reported physical activity measurement did not always clearly report intention‐to‐treat (ITT) analysis or whether final assessments occurred during or after intervention. Based on prespecified measures, we included three comparisons in our summary of findings.
A physical activity programme (weight‐bearing) compared to no physical activity programme
One study involved adults with diabetic peripheral neuropathy (DPN) and reported weekly duration of walking during and at the end of a one‐year intervention using a StepWatch ankle accelerometer. Based on the point estimate and low‐certainty evidence, intervention may have led to an important increase in physical activity per week; however, the 95% confidence interval (CI) included the possibility of no difference or an effect in either direction at three months (mean difference (MD) 34 minutes per week, 95% CI –92.19 to 160.19; 69 participants), six months (MD 68 minutes per week, 95% CI –55.35 to 191.35; 74 participants), and 12 months (MD 49 minutes per week, 95% CI –75.73 to 173.73; 70 participants). Study‐reported effect estimates for foot lesions and full‐thickness ulcers also included the possibility of no difference, a higher, or lower risk with intervention.
A sensor‐based, interactive exercise programme compared to no sensor‐based, interactive exercise programme
One study involved adults with DPN and reported duration of walking over 48 hours at the end of four weeks' intervention using a t‐shirt embedded PAMSys sensor. It was not possible to draw conclusions about the effectiveness of the intervention from the very low‐certainty evidence (MD –0.64 hours per 48 hours, 95% CI –2.42 to 1.13; 25 participants). We were also unable to draw conclusions about impact on the Physical Component Score (PCS) for quality of life (MD 0.24 points, 95% CI –5.98 to 6.46; 35 participants; very low‐certainty evidence), although intervention may have made little or no difference to the Mental Component Score (MCS) for quality of life (MD 5.10 points, 95% CI –0.58 to 10.78; 35 participants; low‐certainty evidence).
A functional exercise programme compared to a stretching exercise programme
One study involved adults with spinal and bulbar muscular atrophy and reported a daily physical activity count at the end of 12 weeks' intervention using an Actical accelerometer. It was not possible to draw conclusions about the effectiveness of either intervention (requiring compliance) due to low‐certainty evidence and unconfirmed measurement units (MD –8701, 95% CI –38,293.30 to 20,891.30; 43 participants). Functional exercise may have made little or no difference to quality of life compared to stretching (PCS: MD –1.10 points, 95% CI –5.22 to 3.02; MCS: MD –1.10 points, 95% CI –6.79 to 4.59; 49 participants; low‐certainty evidence).
Although studies reported adverse events incompletely, we found no evidence of supported activity increasing the risk of serious adverse events.
Authors' conclusions
We found a lack of evidence relating to children, adolescents, and non‐ambulant people of any age. Many people living with NMD did not meet randomised controlled trial eligibility criteria. There was variation in the components of supported activity intervention and usual care, such as physical therapy provision. We identified variation among studies in how physical activity was monitored, analysed, and reported. We remain uncertain of the effectiveness of promotional intervention for physical activity and its impact on quality of life and adverse events. More information is needed on the ITT population, as well as more complete reporting of outcomes. While there may be no single objective measure of physical activity, the study of qualitative and dichotomous change in self‐reported overall physical activity might offer a pragmatic approach to capturing important change at an individual and population level.
Keywords: Humans; Bias; Exercise; Health Promotion; Health Promotion/methods; Muscle Stretching Exercises; Neuromuscular Diseases; Neuromuscular Diseases/rehabilitation; Outcome Assessment, Health Care; Quality of Life; Randomized Controlled Trials as Topic; Resistance Training; Resistance Training/statistics & numerical data; Time Factors; Walking; Walking/statistics & numerical data
Plain language summary
What interventions promote physical activity in people living with neuromuscular disease?
Review question
We looked at the evidence on ways to increase physical activity in people with neuromuscular disease. We only included studies that measured physical activity as an outcome. We collected and analysed all relevant studies to answer this question.
Background
Physical activity includes any type of everyday activity, such as work, travel, or exercise. Based on well‐known health benefits, international guidance recommends that everyone does enough regular physical activity. This guidance is relevant to people with health conditions, including neuromuscular diseases, which affect the way that muscles and nerves work. However, many people with neuromuscular disease live with disability and face barriers to being more physically active. Research studies also sometimes exclude people who have health conditions.
Study characteristics
This review included 13 studies (795 participants from 12 studies; the number of participants was unclear in one study). The studies mostly involved adults who were able to walk, although our review question included people of any age who were able to move around with or without assistance. Only one study intervention had a stated aim to increase physical activity. The main focus of most studies was to assess the effects of physical activity interventions on other aspects of health, fitness, and well‐being. Interventions involved supported exercise or other types of physical activity, advice about being more active, or talking therapies that included changing everyday activity behaviour. Physical therapists and other health and fitness professionals provided the support for most interventions.
Results and certainty of the evidence
The evidence related to adults with nine different types of neuromuscular disease. All 13 studies planned to measure physical activity but the results from six studies were not reported or usable. We found important differences in the interventions and in the usual care provided in different places. We also found differences in how studies measured and reported outcomes. Missing information on physical activity may have affected the results. In terms of time spent physically active, we are uncertain whether any intervention promoted physical activity in people with neuromuscular disease. We are also uncertain about the impact of physical activity interventions on quality of life and any harms. However, we found no evidence that physical activity intervention increased serious harms. Our uncertainty in the evidence is due to limitations in study design and because the results were imprecise or did not directly address our review question.
The evidence is current to 30 April 2020.
Summary of findings
Summary of findings 1. A physical activity programme (weight‐bearing) compared to no physical activity programme in people living with NMD.
| Physical activity programme compared to no physical activity programme | ||||||
|
Patient or population: people with NMD Setting: primary care, endocrinology, or podiatry practices in central Missouri, USA Intervention: physical activity programme (weight‐bearing) Comparison: no physical activity programme | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with no physical activity programme | Risk with physical activity programme | |||||
|
Time spent walking (minutes per week, activity monitor)
assessed with: final scores, during intervention Follow‐up: 3 months |
The mean time spent walking was 526 minutes per week | MD 34 minutes more (92.19 fewer to 160.19 more) | — | 69 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Time spent walking (minutes per week, activity monitor)
assessed with: final scores, during intervention Follow‐up: 6 months |
The mean time spent walking was 511 minutes per week | MD 68 minutes more (55.35 fewer to 191.35 more) | — | 74 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Time spent walking (minutes per week, activity monitor)
assessed with: final scores, unclear if during or after intervention Follow‐up: 12 months |
The mean time spent walking was 500 minutes per week | MD 49 minutes more (75.73 fewer to 173.73 more) | — | 70 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
| Quality of life | — | — | — | — | — | Outcome not measured. |
| Adverse events/serious adverse events | — | — | — | — | — | No comparative data between groups available for all types of adverse event. However, the study reported rate ratios specifically for foot lesions and ulcers in participants with diabetic peripheral neuropathy. Over 12 months, the reported rate ratio for all types of foot lesions (ignoring multiple lesions/episode) was 1.24 (95% CI 0.70 to 2.19; 1 study, 70 participants). Based on the point estimate, intervention may have led to higher rate of foot lesions; however, the 95% CI included the possibility of no difference or an effect in either direction. Over 12 months, the reported rate ratio for all full‐thickness foot ulcers (ignoring multiple lesions/episode) was 0.96 (95% CI 0.38 to 2.42; 1 study, 70 participants). Based on the point estimate, intervention may have led to a lower rate of full‐thickness foot ulcers; however, the 95% CI included the possibility of no difference or an effect in either direction. |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; NMD: neuromuscular disease; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| See interactive version of this table: gdt.gradepro.org/presentations/#/isof/isof_question_revman_web_422109324271426071. | ||||||
aDowngraded once for study limitations associated with an unclear risk of bias in random sequence generation. bDowngraded once for imprecision associated with a wide CI.
Summary of findings 2. A sensor‐based, interactive exercise programme compared to no sensor‐based, interactive exercise programme in people living with NMD.
| Sensor‐based, interactive exercise programme compared to no sensor‐based, interactive exercise programme | ||||||
|
Patient or population: people with NMD Setting: USA and Qatar Intervention: sensor‐based exercise programme Comparison: no sensor‐based exercise programme | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with no exercise programme | Risk with exercise programme | |||||
|
Time spent walking (hours per 48 hours, activity monitor) assessed with: final scores, after intervention Follow‐up: 4 weeks |
The mean time spent walking was 4.12 hours | MD 0.64 hours fewer (2.42 fewer to 1.13 more) | — | 25 (1 RCT) | ⊕⊝⊝⊝ Verylowa,b | — |
|
Quality of life (SF‐12 PCS) assessed with: final scores, after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 4 weeks |
The mean quality of life (SF‐12 PCS) was 40.12 points | MD 0.24 points higher (5.98 lower to 6.46 higher) | — | 35 (1 RCT) | ⊕⊝⊝⊝ Verylowa,b | — |
|
Quality of life (SF‐12 MCS) assessed with: final scores, after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 4 weeks |
The mean quality of life (SF‐12 MCS) was 47.3 points | MD 5.1 points higher (0.58 lower to 10.78 higher) | — | 35 (1 RCT) | ⊕⊕⊝⊝ Lowa,c | — |
| Adverse events/serious adverse events | — | — | — | — | — | No comparative data available between groups for any type of adverse event. |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MCS: Mental Component Score; MD: mean difference; NMD: neuromuscular disease; PCS: Physical Component Score; RCT: randomised controlled trial; SF‐12: 12‐item Short Form Health Survey. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| See interactive version of this table: gdt.gradepro.org/presentations/#/isof/isof_question_revman_web_422110856458804259. | ||||||
aDowngraded once for study limitations associated with a high risk of selective reporting and attrition bias. bDowngraded twice for imprecision associated with a very wide CI. cDowngraded once for imprecision associated with a wide CI.
Summary of findings 3. A functional programme compared to a stretching programme in people living with NMD.
| Functional programme compared to stretching programme | ||||||
|
Patient or population: people with NMD Setting: Bethesda, Maryland, USA Intervention: functional exercise programme Comparison: stretching exercise programme | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with stretching programme | Risk with functional programme | |||||
|
Physical activity (unspecified count per day, activity monitor) assessed with: final scores, during intervention Follow‐up: 12 weeks |
The mean physical activity (unspecified counts per day, activity monitor) was 70,498 counts | MD 8701 counts lower (38,293.3 lower to 20,891.3 higher) | — | 43 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Quality of life (SF‐36 PCS) assessed with: final scores, unclear if during or after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 12 weeks |
The mean quality of life (SF‐36 PCS) was 34.1 points | MD 1.1 points lower (5.22 lower to 3.02 higher) | — | 49 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Quality of life (SF‐36 MCS) assessed with: final scores, unclear if during or after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 12 weeks |
The mean quality of life (SF‐36 MCS) was 54.4 points | MD 1.1 points lower (6.79 lower to 4.59 higher) | — | 49 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
| Adverse events/serious adverse events | — | — | — | — | — | No usable adverse event data available. |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MCS: Mental Component Score; MD: mean difference; NMD: neuromuscular disease; PCS: Physical Component Score; RCT: randomised controlled trial; SF‐36: 36‐item Short Form Health Survey. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| See interactive version of this table: gdt.gradepro.org/presentations/#/isof/isof_question_revman_web_422114406971747153. | ||||||
aDowngraded once for study limitations associated with a high risk of attrition bias. bDowngraded once for imprecision associated with a wide CI.
Background
Description of the condition
People with neuromuscular disease (NMD) are part of a clinically heterogeneous population with inherited or acquired disorders of muscle, peripheral nerve, neuromuscular junction, or anterior horn cell of the spinal cord (Fowler 2002; Öksüz 2011). Diagnosis is based on genetic testing where possible, biopsy, and established clinical criteria. In most types of primary NMD (e.g. Duchenne muscular dystrophy), prevalence rates are estimated to vary between 1 and 10 per 100,000 population. The estimated prevalence is higher for Charcot‐Marie‐Tooth (CMT) disease and postpolio syndrome (PPS), at over 10 per 100,000 (Deenen 2015). More than one in four people are estimated to have diabetic peripheral neuropathy (DPN) as a secondary complication of type 2 diabetes (Lu 2020). The number of people affected by DPN may rise further with an increasing global prevalence of type 2 diabetes that is, in part, attributed to less physically active lifestyles (Saeedi 2019).
NMD manifests with different patterns of disease activity and progression, sometimes requiring therapeutic intervention, assistive technology, and aids to support movement. Muscle weakness and limitations in activities of daily life are common features but everyday activity, and quality of life, may also be impacted by other factors, such as foot lesions, difficulties with balance, pain, and fatigue. Secondary disuse weakness and cardiovascular deconditioning may develop over time, which increases the risk of further chronic health problems and complications (Aitkens 2005; Apabhai 2011; Dal Bello‐Haas 2013; Fowler 2002; Jimenez‐Moreno 2017; Kilmer 2005; McDonald 2002; Öksüz 2011; Phillips 2009; Ramdharry 2017; Voet 2013; White 2004; WHO 2020a). According to the World Health Organization (WHO), physical inactivity is one of the main risk factors for non‐communicable diseases mortality (WHO 2020b).
Description of the intervention
WHO recommends regular and adequate physical activity, which is based on a minimum duration, intensity, frequency, and type of physical activity in different age groups. For people unable to meet the recommendations due to health conditions, WHO advises being as physically active as possible (WHO 2020a). In muscle‐wasting conditions, recommendations for exercise include more specific information on precautions and progression, as well as guidance on duration, intensity, frequency, and type of exercise (MDUK 2014).
This review includes any intervention that aims to promote physical activity in adults or children with NMD. We used the WHO definition of physical activity as "any bodily movement produced by skeletal muscles that requires energy expenditure" – including all movement during leisure time, while working, and travelling (WHO 2020a; WHO 2020b). As previously highlighted by the American College of Sports Medicine (ACSM), 'physical activity' and 'exercise' are sometimes used interchangeably, but the latter is a specific form of physical activity that consists of "planned, structured, and repetitive bodily movement done to improve or maintain one or more components of physical fitness" (ACSM 2010).
Exercise is often the form of physical activity studied in NMD. However, there are other potential types of lifestyle intervention (as per the WHO definition, such as monitoring, advice, and support) that may also help to promote physical activity (Foster 2005; Foster 2013; Richards 2013a; Richards 2013b). At a population level, a multi‐component approach is often taken, involving policy and environmental changes, as well as behavioural and informational interventions (Baker 2015). In this review, we considered the promotion of physical activity to include any strategy or approach that contributes to people with NMD becoming more physically active.
How the intervention might work
In studies of apparently healthy populations, short‐ to medium‐term improvements in self‐reported physical activity outcomes and cardiorespiratory fitness follow physical activity interventions compared with no intervention, attention control (e.g. general health check of an equivalent duration), minimal intervention, or a combination of these (Foster 2005). There is also some evidence in favour of particular modes of intervention delivery, such as use of technologies with support from a trained professional (Foster 2013). However, this evidence excludes people with known medical conditions, and findings after community‐level interventions have been inconsistent (Baker 2015; Foster 2005; Foster 2013). For apparently healthy populations (within which as many as one in two people with diabetes mellitus globally are thought to be undiagnosed (Saeedi 2019)), increasing and maintaining regular physical activity is likely to be beneficial in terms of reducing all‐cause mortality risk, as well as for the primary and secondary prevention of noncommunicable diseases, such as diabetes mellitus, cardiovascular disease, colon and breast cancer, osteoporosis, and depression, as well as risk factors such as hypertension and obesity. At a mechanistic level, routine physical activity has been associated with enhanced mental well‐being, reduced blood pressure, and improvement in glucose control and other biomarkers for inflammation and cardiovascular disease risk (Warburton 2006). These effects might reduce the need for pharmacological or other treatment, the associated costs, and possible adverse effects. While the risk of chronic conditions will increase with age, the benefits of physical activity have been shown across the lifespan, with recommended 'doses' adjusted for children, adults, and older adults, as well as for those already living with chronic conditions and disability (Warburton 2006; Warburton 2017; WHO 2020a).
The effect of interventions to promote physical activity may be different in people with certain medical conditions, such as NMD, compared with those living without such conditions. Ambulatory status may also vary but the potential to be more physically active applies to non‐ambulant as well as ambulant people with NMD. Several studies have highlighted that people with particular types of NMD are less physically active than apparently healthy controls without a diagnosed NMD, and have higher perceived barriers to becoming physically active (Aitkens 2005; Apabhai 2011; Heutinck 2017; McCrory 1998; Phillips 2009; Ramdharry 2017). This could suggest differences in the effect of physical activity in terms of biological mechanism or facilitation at an individual or community level. People with different types of NMD may also respond differently to physical activity interventions because of the clinical heterogeneity of their conditions (Voet 2013) (with variable disease pattern, severity, and progression), as well as differences in the timing of disease onset in relation to developmental and ageing processes (e.g. childhood versus adult onset of NMD). Furthermore, people with NMD who are non‐ambulant may be at a greater risk from waking behaviours with low energy expenditure in sitting, reclining, or lying (referred to as sedentary behaviour) than those who are ambulant; this could have an impact on health outcomes that is independent of recommended doses of everyday physical activity. As such, sedentary behaviour could confound the effect of increased physical activity in terms of the risk for all‐cause mortality and chronic disease. However, there is evidence to suggest that physical activity can attenuate, if not negate, risks associated with prolonged sitting (Ekelund 2016).
The type and dose of physical activity can affect health benefits and complications, which in turn may shape everyday physical activity behaviour. Peak performance measures are often a primary outcome in studies involving physical activity although it may be unclear whether the intervention has actually changed everyday physical activity as an outcome. In terms of potential adverse effects of physical activity, there is currently limited evidence to assess the risk in NMD. Increasing physical activity may not always be appropriate for all people with NMD. The overworking of muscles affected by NMD could increase the risk of muscle damage and impairment. For example, overexertion can lead to myalgia (muscle pain), myoglobinuria (muscle protein in the urine, associated with muscle breakdown), weakness, and fatigue in people with muscle disease (MDUK 2014). For some, there may also be particular concerns about weight‐bearing activity, for example, in relation to managing falls risk or foot lesions in DPN. Focusing on exercise intervention as a specific form of physical activity, one systematic review of studies in NMD found no evidence of serious adverse events (Stefanetti 2020). Another systematic review in people with muscle disease highlighted that adverse event data from five included randomised controlled trials (RCT) was incomplete (Voet 2013). Six years later, an update of that review found low‐ to very low‐certainty evidence relating to adverse events (Voet 2019). There was no RCT evidence for exercise intervention in one systematic review involving people with McArdle disease (Quinlivan 2011). In peripheral neuropathy, one systematic review (including three RCTs) found one incidence of lower limb pain with exercise intervention, which was attributed to the aggravation of arthritis (White 2004). Although one systematic review of RCTs in amyotrophic lateral sclerosis (ALS) found no reported adverse effects due to exercise, fatigue and rapid deterioration resulting in death were reasons given for participants dropping out from one of the two included studies (Dal Bello‐Haas 2013).
Why it is important to do this review
The purpose of this review was to better understand the effects of different approaches for people living with NMD to become more physically active as part of a management strategy for health and well‐being.
Objectives
To assess the effects of interventions designed to promote physical activity in people with NMD compared with no intervention or alternative interventions.
Methods
Criteria for considering studies for this review
Types of studies
We included parallel RCTs involving people with any type of NMD. We included randomised cross‐over studies that matched our inclusion criteria. In cross‐over studies, participants each undergo more than one intervention. This study design is considered suitable for assessing "a temporary effect in the treatment of stable, chronic conditions" (Higgins 2020), and so may be suitable in some but not all types of NMD (i.e. not those where progression is expected to lead to a clinically important decline within the timescale of the study).
We planned to include quasi‐RCTs, defined as trials that allocated participants to groups using methods such as alternation, use of a case record number, or date of attendance. We referred to other types of evidence in the 'Discussion' only.
We included studies reported as full text and those published as abstract only. We also sought unpublished data for inclusion. There were no language restrictions.
Types of participants
We accepted studies that included adults, children, or both, with NMD. We considered studies in which NMDs had been diagnosed by any established criteria, and studies that did not describe diagnostic criteria or predated genetic diagnosis. As part of the spectrum of NMD, we included genetic or acquired peripheral nerve disorders, muscle diseases, neuromuscular junction, and motor neuron disorders. We excluded mechanical nerve compression conditions, such as carpal tunnel syndrome. We reported comorbidities where this information was available.
If studies included a subset of participants with NMD, we planned to contact the investigators or study sponsors to gather any relevant subgroup data not reported. If they were unable or unwilling to provide subgroup data, we would not have included these studies in the meta‐analysis. As a protocol deviation, we limited eligible study populations with a subset of participants with NMD to those study populations with neurological disorders, including a subset of participants with NMD. See Differences between protocol and review.
Types of interventions
We included studies of any practical (e.g. exercise or environmental adaptation), informational, or motivational intervention that was designed to promote physical activity, compared with no intervention, or another intervention designed to promote physical activity (Foster 2005). This included studies of any mode of delivery, dose, duration, or intensity, in a community setting. We included co‐interventions if they were provided to each group equally. For the purposes of this review, very brief interventions that might promote physical activity, such as general health checks, were included as interventions although these have also been defined as an attention control comparison elsewhere (Foster 2005). We reported details of supervisory support provided as part of an intervention, and we reported any concurrent treatment and care where this information was provided. We would have performed subgroup analyses to explore differences in the delivery of interventions if sufficient data had been available.
Potential interventions included one or a combination of the following (Foster 2005; Foster 2013; Richards 2013a; Richards 2013b):
one‐to‐one advice or support;
group advice or support;
telephone advice or support;
Internet‐based, mobile apps, or telehealth (remote) advice or support;
written advice or support;
self‐directed or unsupervised participation in a prescribed physical activity programme;
supervised physical activity in the home;
supervised physical activity in a facility;
monitoring device (e.g. accelerometer or pedometer);
other intervention designed to promote physical activity.
Types of outcome measures
Participation in physical activity was the main focus of this review and measurement of physical activity was an inclusion criterion for the review. However, the authors acknowledge that increases in physical activity may also lead to changes in quality of life and adverse events, which we explored as a secondary focus. We reported details of outcome measure assessment where this information was provided.
Primary outcomes
Physical activity: measured by self‐report or objectively, using monitoring devices (e.g. accelerometer or pedometer).
In accordance with the WHO definition of physical activity, primary outcomes related to everyday activity and included: overall physical activity, measured by self‐report using standardised questionnaires (e.g. the WHO Global Physical Activity Questionnaire, which collects information on activity at work or doing household chores, recreational activities, and travel to and from places); total time spent in physical activity, measured by self‐report or objectively (minutes/week); estimated total energy expenditure, measured by self‐report or objectively (calories or joules/week); step count, measured objectively (steps/week) (Foster 2005; Foster 2013; Richards 2013a; Richards 2013b).
We planned to prioritise the inclusion of physical activity outcomes in the following order: overall physical activity > total time spent in physical activity > estimated total energy expenditure > step count. We would have performed subgroup analysis to explore differences in physical activity measured subjectively and objectively if sufficient data had been available.
Secondary outcomes
Quality of life: measured by self‐report using standardised questionnaire scales (e.g. 36‐item Short Form Health Survey (SF‐36)).
-
Adverse events:
increase in pain: measured by self‐report;
any other, emergent and intervention‐related;
leading to discontinuation from study.
-
Serious adverse events:
hospitalisation;
all‐cause death.
As a protocol deviation, we included available data on serious adverse events a defined by one included study as 'serious adverse events'; see Differences between protocol and review.
To avoid potential selection bias, we planned to only analyse final values where studies did not report change scores. If either final or change scores were reported incompletely (e.g. without a measure of variability), we prioritised the reporting of those results reported most completely. As a protocol deviation we also prioritised the reporting of unadjusted final scores over adjusted change scores from one study; see Differences between protocol and review and Characteristics of included studies table. If we had sufficient data for meta‐analysis, we planned to make comparisons at the following time points:
less than six weeks from baseline;
six weeks to less than six months from baseline;
six to 12 months from baseline;
over 12 months from baseline.
We did not exclude study data available at multiple time points. If an included study reported multiple measures for the same outcome domain, we included the data for each of these measures. We planned to base the minimal important difference (MID) for outcomes on established values in the literature where possible. Where MIDs were unavailable, we reported this in the interpretation of the outcomes in the 'Results' and 'Discussion'.
Search methods for identification of studies
Electronic searches
On 30 April 2020, the Cochrane Neuromuscular Information Specialist searched the following databases:
Cochrane Neuromuscular Specialised Register via the Cochrane Register of Studies (CRS‐Web; Appendix 1);
Cochrane Central Register of Controlled Trials (CENTRAL) via CRS‐Web (Appendix 2);
MEDLINE (1946 to 30 April 2020; Appendix 3);
Embase (1974 to 2020 Week 17; Appendix 4);
US National Institutes for Health Clinical Trials Registry, ClinicalTrials.Gov (Appendix 5);
The WHO International Clinical Trials Registry Portal (ICTRP; apps.who.int/trialsearch/) was not accessible at the search date; however, most of its content is indexed in CENTRAL. We searched all databases from their inception, and we imposed no restriction on language of publication.
Searching other resources
We searched review articles for additional references but not the reference lists of included studies; see Differences between protocol and review. We also searched for errata or retractions of included studies.
Data collection and analysis
Selection of studies
One review author (KJ) imported all results of the search into Covidence software for dual screening (Covidence). Two review authors (KJ and FH) independently screened titles and abstracts of all potential studies identified by the search for inclusion and coded them as 'retrieve' (eligible or potentially eligible/unclear) or 'do not retrieve'. During selection of studies, the review author team clarified eligibility of particular conditions not specified in the search strategies and in accordance with the scope of Cochrane Neuromuscular. Review authors also clarified the exclusion of studies, including exercise‐based studies, that did not explicitly refer to physical activity measurement or promotion. As an extension to the protocol, one review author (KJ) noted eligibility rationale for all judgements on potentially eligible records initially identified in Covidence, and both review authors (FH and KJ) performed a second screen of these records (see Differences between protocol and review). This additional round of screening narrowed down the potentially eligible records. We retrieved the full‐text study reports/publications, and two review authors (KJ and JN) independently screened the full text and identified studies for inclusion. We identified and recorded reasons for exclusion of the ineligible studies. We resolved any disagreement through discussion and consulted a third review author (GR) to confirm eligibility of a study population. The Information Specialist for Cochrane Neuromuscular (FS) identified and excluded duplicates and we collated multiple reports of the same study so that each study rather than each report was the unit of interest in the review. We recorded the selection process in sufficient detail to complete a PRISMA flow diagram (Moher 2009), Characteristics of included studies table, and Characteristics of excluded studies table.
Data extraction and management
We used a data extraction form for study characteristics and outcome data that had been piloted on at least one study in the review. We planned to apply the TIDieR Checklist (Template for intervention Description and Replication; The EQUATOR Network), but focused on completion of the Checklist by included studies. We considered other intervention‐reporting guidance (including the CERT framework (Consensus on Exercise Reporting Template; Slade 2016) and MARS (Mobile App Rating Scale; Stoyanov 2015)) as part of our discussion of the evidence. At least one review author (KJ and FH, JN, JM, or GR) extracted the following study characteristics from included studies: study design and setting, characteristics of participants, eligibility criteria, intervention details, outcomes assessed, source(s) of study funding, and any conflicts of interest among investigators.
Two review authors (KJ and FH, JN, JM, or GR) extracted outcome data from included studies and one review author (KJ) transferred data into Review Manager 5 and RevMan Web (Review Manager 2020; RevMan Web 2020). If a review author had been involved in a potential included study, another uninvolved review author completed data extraction instead. As a protocol deviation, the first author (KJ) contributed to data extraction for one study despite involvement due to constraints on co‐author availability (see Differences between protocol and review). We noted in the Characteristics of included studies table if outcome data were not reported in a usable way. We resolved any disagreements by discussion. We planned for a third review author to check the outcome data entries and spot‐check study characteristics for accuracy against the trial report. As a protocol deviation, the first author (KJ) completed these checks (see Differences between protocol and review).
If full text reports had required translation, the translator would have extracted data directly using a data extraction form, or authors would have extracted data from the translation provided. Where possible, a review author would have checked numerical data in the translation against the study report.
Assessment of risk of bias in included studies
Two review authors (KJ and JN, FH, JM, or GR) independently assessed risk of bias for each outcome using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved any disagreements by discussion. If a review author had involvement in any potential included studies, we planned for a third review author to complete the assessment instead. As a protocol deviation, one review author involved in an included study (KJ) contributed to its risk of bias assessment (see Differences between protocol and review). We assessed the risk of bias according to the following domains:
random sequence generation;
allocation concealment;
blinding of participants and personnel;
blinding of outcome assessment;
incomplete outcome data;
selective outcome reporting;
other bias.
We graded each potential source of bias as high, low, or unclear risk and provided a quote from the study report together with a justification for our judgement in the risk of bias table. We summarised the risk of bias judgements across different studies for each of the domains listed; we planned to consider all outcomes separately as some domains may have different risks of bias for different outcomes but we presented assessments at the study level with reference to outcomes of specific relevance to the review. If information on risk of bias had related to unpublished data or correspondence with a trialist, we would have noted this in the risk of bias table.
When considering treatment effects, we considered the risk of bias for the evidence that contributed to that outcome.
Assessment of bias in conducting the systematic review
We conducted the review according to the published protocol (Jones 2020), and reported any deviations from it in the Differences between protocol and review section.
Measures of treatment effect
The main effect of interest in this review was the effect of assignment to the intervention rather than adherence, which is a different review question. Therefore, we planned to limit our meta‐analysis to the intention‐to‐treat (ITT) population if we had sufficient data.
Dichotomous data
We analysed dichotomous data as risk ratios (RR) with 95% confidence intervals (CIs). If we had found rare events (zero in either arm or less than 1%), we would have used the Peto odds ratio (Peto OR) with 95% CIs. To assess absolute risk where there were zero events in the control arm, we would have calculated the risk difference (RD) with 95% CIs in Review Manager 5 (Review Manager 2020).
Continuous data
We presented continuous data as mean difference (MD) with 95% CIs. Where studies reported a mean with standard error or 95% CI, we calculated the standard deviation (SD) using Review Manager 5 (Review Manager 2020). If we had undertaken meta‐analysis, we would have considered using the standardised mean difference (SMD) with 95% CIs for results across studies with outcomes that were conceptually the same but measured in different ways (including physical activity questionnaires and health‐related quality of life questionnaires). Where necessary, we would have combined final values and change scores in the same analysis if reporting the MD but not when reporting the SMD. We would have entered data presented as a scale with a consistent direction of effect.
We planned to undertake meta‐analyses only where this was meaningful (i.e. if the interventions, participants, and underlying clinical question were similar enough for pooling to make sense).
Unit of analysis issues
Multiple arm studies
Where a study reported results for multiple arms, we planned to only include arms eligible for this review (although we would list additional arms in the Characteristics of included studies table). If two comparisons (e.g. intervention A versus intervention C and intervention B versus intervention C) had been included in the same meta‐analysis, we intended to avoid double‐counting by combining groups to create a single pair‐wise comparison (Higgins 2020). However, this approach was not found to be helpful on application (e.g. comparison of exercise versus advice versus usual care). If meta‐analysis had been appropriate, an alternative approach could have been to split the control group between multiple arms. Where the review included more than one comparison that could not be included in the same analysis, we reported the results for each comparison separately.
Cross‐over studies
As there may be carry‐over in the effect of physical activity promotion and a period effect in some neuromuscular conditions, we planned to only include first‐period data from cross‐over studies.
Cluster‐randomised controlled trials
We did not expect or find any eligible studies that were cluster‐RCTs; if we had found any cluster‐RCTs, we would have discussed these narratively in the review.
Within‐patient trial designs
We did not expect or find any eligible studies that used within‐patient trial designs (e.g. an uncontrolled before‐and‐after design as distinct from a cross‐over design); if we had found any, we would have considered these narratively in the review.
Dealing with missing data
We emailed investigators from two included studies to try to verify key study characteristics and obtain relevant missing numerical outcome data where possible (e.g. if a study was available as an abstract only).
Assessment of heterogeneity
If we had undertaken meta‐analysis, we would have used the I² statistic to measure heterogeneity among the studies in each analysis. We planned to use the rough guide to interpretation as outlined in Chapter 11 of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2020), as follows:
0% to 40%: might not be important;
30% to 60%: may represent moderate heterogeneity;
50% to 90%: may represent substantial heterogeneity;
75% to 100%: considerable heterogeneity.
We would have also considered the following factors: the overlap of CIs in forest plots, whereby poor overlap is expected to indicate heterogeneity; the Chi² test included in forest plots, for which a large result relative to the degrees of freedom is expected to indicate heterogeneity; a low P value for heterogeneity (less than 0.10) in forest plots.
If we identified substantial unexplained heterogeneity, we would have reported it and explored possible causes narratively and by prespecified subgroup analysis.
Assessment of reporting biases
We note that small‐study effects can bias results even in the absence of heterogeneity. If we had been able to pool more than 10 studies, we would have created and examined a funnel plot to explore possible small‐study biases, as detailed in the Cochrane Handbook for Systematic Reviews of Interventions (Page 2021).
Data synthesis
If we had undertaken meta‐analysis, we would have used the Mantel‐Haenszel (M‐H) method to meta‐analyse dichotomous data, and the inverse variance method to meta‐analyse continuous data. We planned to use a random‐effects model in Review Manager 5 and RevMan Web (Review Manager 2020; RevMan Web 2020), on the assumption that different studies were estimating different, yet related, intervention effects (Deeks 2020).
Subgroup analysis and investigation of heterogeneity
If we had sufficient data, we planned to carry out the following subgroup analyses to investigate clinically plausible differences in the intervention effect (Deeks 2020):
in different types of NMD, including muscle disease, peripheral nerve disorders, neuromuscular junction disorders, and motor neuron disorders (analysis 1);
adults (aged 18 years or older) versus children (aged less than 18 years) versus mixed adults and children (analysis 2);
ambulatory (independent walking and occasional use of an assistive device) versus non‐ambulatory (habitual use of an assistive device or wheelchair) versus mixed ambulatory and non‐ambulatory (analysis 3);
regular supervisory support (operational definition: at least two scheduled sessions with identified personnel to plan and progress activity) versus no regular supervisory support (analysis 4);
subjectively measured physical activity versus objectively measured physical activity (analysis 5).
On reviewing the evidence, we removed one prespecified subgroup analysis for comparing general health visits with other interventions designed to promote physical activity because we would have considered this as a main comparison (see Differences between protocol and review). If meta‐analysis had been undertaken, we would have had sufficient subgroup information available for subgroup analysis 1 only. We did not attempt to meta‐analyse different physical activity outcome measures as a single domain.
We planned to use the following primary outcomes in subgroup analyses.
Overall physical activity, measured by self‐report using standardised questionnaires (e.g. Global Physical Activity Questionnaire).
Total time spent in physical activity, measured by self‐report or objectively (minutes/week).
Estimated total energy expenditure, measured by self‐report or objectively (calories or joules/week).
Step count, measured objectively (steps/week).
For subgroup analyses 1 to 4, we prioritised the inclusion of physical activity outcomes using the order above. For subgroup analysis 5, we planned to only include comparable measures of physical activity (total time; total energy expenditure).
We would have used the formal test for subgroup differences in Review Manager 5 or RevMan Web (Review Manager 2020; RevMan Web 2020). Overlap of CIs and a high I² statistic would indicate a difference between subgroups, and suggest there could be differential effects of interventions to promote physical activity in different types of NMD.
Sensitivity analysis
We initially planned to carry out the following sensitivity analyses to investigate the robustness of findings to the decisions made in obtaining them (Deeks 2020). If sufficient data had been available for meta‐analysis of the primary outcome, we would have repeated the analysis:
excluding unpublished studies (if there were any);
excluding studies that did not describe diagnostic criteria for NMDs;
excluding studies at high risk of bias for missing data;
excluding the data from cross‐over studies;
using a fixed‐effect model.
If we had sufficient data for meta‐analysis, a sensitivity analysis for adjusted and unadjusted results may also have been helpful.
Reaching conclusions
We based our conclusions only on findings from the quantitative or narrative synthesis of included studies for this review. We avoided making recommendations for practice and, in our implications for research, suggested priorities for future research and outlined remaining uncertainties in the area.
Summary of findings and assessment of the certainty of the evidence
We created summary of findings tables using GRADEpro GDT software (GRADEpro GDT), and intended to present the following outcomes.
Physical activity: overall physical activity measured by self‐report, using standardised questionnaires (e.g. Global Physical Activity Questionnaire) at less than six weeks from baseline.
Physical activity: overall physical activity measured by self‐report using standardised questionnaires (e.g. Global Physical Activity Questionnaire) at six weeks to less than six months from baseline.
Physical activity: total time spent in physical activity measured by self‐reported minutes/week at less than six weeks from baseline.
Physical activity: total time spent in physical activity measured by self‐reported minutes/week at six weeks to less than six months from baseline.
Quality of life: measured by self‐report using standardised questionnaire scales (e.g. SF‐36) at less than six weeks from baseline.
Quality of life: measured by self‐report using standardised questionnaire scales (e.g. SF‐36) at six weeks to less than six months from baseline.
Adverse events leading to discontinuation from study.
We presented results for three of the eight main comparisons in this review, using one summary of findings table for each comparison. In the absence of any usable evidence on overall physical activity, we did not include this in the summary of findings. The three main comparisons in people living with NMD included: a physical activity programme compared to no physical activity programme; a sensor‐based, interactive exercise programme compared to no sensor‐based, interactive exercise programme; and a functional exercise programme compared to a stretching exercise programme. We created additional tables for four other comparisons that did not report the prespecified physical activity outcomes for summary of findings tables. These comparisons included: an aerobic exercise programme compared to no aerobic exercise programme; an aerobic exercise programme compared to cognitive behavioural therapy (CBT); CBT compared to no CBT; CBT with or without an exercise programme compared no CBT and no exercise programme. We did not create a summary of findings table for another comparison of a weight‐bearing exercise programme with a non‐weight‐bearing exercise programme because this comparison included no summary of findings table outcomes. Physical activity parameters were the primary outcome of interest for assessing the effect of interventions to promote physical activity. As a protocol deviation, we included any measure of total time spent in physical activity (i.e. using an activity monitor or self‐reported measure; see Differences between protocol and review). In addition, we included well‐being and safety aspects, which could influence intervention uptake and adherence across a spectrum of NMDs. We planned to prioritise standardised, self‐reported outcome measurement and time points that would include both very brief interventions and short‐ to medium‐length programmes of physical activity promotion. Although prioritising outcomes can assist decision‐makers, as a protocol deviation, we reported outcomes at multiple time points to also include longer term follow‐up. We included multiple time points for outcomes (as per the studies) in the absence of a single, appropriate standard for outcome reporting in people with different types of NMD (see Differences between protocol and review). We also reported mental and physical component summary scores for quality of life (as per the studies) to help capture the impact of physical and communication‐based approaches to physical activity promotion. Two review authors (KJ and JN, FH, or GR) used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias) to independently assess the certainty of the body of evidence (studies that contributed data for the prespecified outcomes). We used methods and recommendations described in Chapters 11 and 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2011a; Schünemann 2011b).
For assessing imprecision consistently in continuous outcomes, we considered the CI width for the intervention effect in relation to a cut‐off of ± 0.5 SD of the control group risk. We resolved any disagreements in GRADE judgements by discussion. If a review author had involvement in any included studies, we planned for a third person to complete the assessment instead. As a protocol deviation, the first review author (KJ) was involved in an included study and contributed to its assessment (see Differences between protocol and review). We considered outcomes to have high‐certainty evidence if the five GRADE factors were not present to any serious degree, but downgraded the certainty to moderate, low, or very low according to review author interpretation. We downgraded evidence once if a GRADE consideration was serious and twice if very serious. We justified all decisions to downgrade the certainty of the evidence using footnotes and made comments to aid readers' understanding of the review where necessary. If we had undertaken meta‐analysis, we planned to use a median control group risk across studies but also report the second highest and second lowest control group risks as representative rates for assumed risk per row of the table (i.e. low‐, moderate‐, and high‐risk populations) where there was potentially important variation. We would have provided a source or rationale and corresponding time duration for the control group risk, indicating the types of participants in which this might apply. In the absence of meta‐analyses, we included narratively synthesised evidence within the summary of findings tables.
Results
Description of studies
We identified RCTs (including cross‐over trials) that explicitly aimed to promote physical activity in people living with NMD. We also identified studies in which physical activity was measured as an outcome, irrespective of the aim of the study. This approach facilitated the consideration of evidence in which 'promotion' could be evaluated as both an intentional and consequential action, although our main focus was the ITT population. We broadly identified three strata of interventions compared with each other or with usual care: structured physical activity support; structured exercise support (as a specific form of physical activity); and structured behaviour change support, including physical activity or exercise. These interventions focused on assessing benefits and harms within the included study population.
Results of the search
The Information Specialist for Cochrane Neuromuscular (FS) ran the search strategies for this review as published in the protocol and reported in Appendix 1; Appendix 2; Appendix 3; Appendix 4; and Appendix 5. The results of this search, performed on 30 April 2020, were as follows: 23,362 records identified through searching databases and 17,123 records screened following deduplication. See flow diagram in Figure 1.
1.
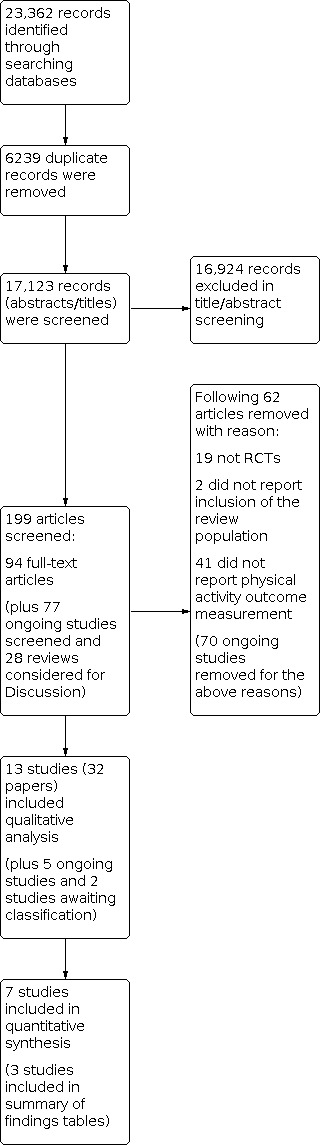
Flow diagram. RCT: randomised controlled trial.
Among 28 narrative and systematic reviews of potential relevance, we checked for physical activity outcome reporting in six other Cochrane Reviews (Bartels 2019; Dal Bello‐Haas 2013; Koopman 2015; Mehrholz 2015; Quinlivan 2011; Voet 2019). We identified no additional RCTs from the Cochrane Reviews for consideration in this review. However, we discussed the findings of this review within the context of evidence from other published reviews (see Discussion). We also evaluated the available trial information for 77 potentially relevant ongoing studies. We found five records for ongoing studies and two records for completed studies awaiting classification (see Characteristics of ongoing studies and Characteristics of studies awaiting classification tables). We did not seek unpublished data from ongoing studies or those awaiting classification but we plan to do so as part of the updating process of this review. We found additional published information from one of the studies awaiting classification (see Discussion). In total, we found 94 conference abstracts or full‐text reports, of which 13 studies (32 papers) met the inclusion criteria. We included seven studies in the quantitative analysis (three of which we included in summary of findings tables and four of which we summarised as additional tables). See Characteristics of included studies and Figure 1. None of the included studies (written in English) required translation.
Included studies
We included 13 studies (795 randomised participants from 12 studies; the number of participants eligible for the review in Elsworth 2011 was unclear). Elsworth 2011 reported inclusion of 26 participants with NMDs and 10 with other conditions including cerebral palsy, traumatic brain injury, and transverse myelitis. On contacting study investigators for more information, we understood 'other' diagnoses included two people with mitochondrial cytopathy, one with CMT disease, and one with polymyostasis. We were unable to ascertain participants' allocated intervention and decided not to seek additional outcome data for quantitative analysis.
The remaining 12 included studies compared interventions in people with a particular NMD (Andersen 2015; Andersen 2017; Grewal 2015; Koopman 2016; Lemaster 2008; Mueller 2013; Okkersen 2018; Shrader 2015; Van Groenestijn 2019; Voet 2014; Wallace 2019; White 2016). Participants had inherited or acquired NMDs including ALS, CMT disease type 1A, DPN, facioscapulohumeral muscular dystrophy (FSHD), inclusion body myositis (IBM), PPS, myotonic dystrophy type 1 (DM1), spinal and bulbar muscular atrophy (SBMA), and stable inflammatory immune‐mediated neuropathy (IN). Three studies involved participants whose NMD (DPN) was secondary to diabetes (Grewal 2015; Lemaster 2008; Mueller 2013). Four studies reported major comorbidities in some participants that may have prevented their participation in other studies (Andersen 2017; Lemaster 2008; Mueller 2013; Okkersen 2018) (see Characteristics of included studies table). Twelve studies excluded children and adolescents and one study did not specify eligibility by age, although participants were aged over 60 years on average. Nine studies included only ambulant participants and the other four studies did not specify baseline ambulatory status of participants but included ambulatory outcome measures.
One of the 13 included studies reported the aim of intervention being to increase physical activity (Lemaster 2008). Two included studies reported the effects of intervention on physical activity as a primary outcome measure (Lemaster 2008; Mueller 2013). All other included studies reported the effects of intervention on physical activity as either a secondary or exploratory outcome measure. Eight studies reported registration with clinical trial registers, of which four were partly or entirely conducted in the Netherlands (Koopman 2016; Okkersen 2018; Van Groenestijn 2019; Voet 2014), one in the USA (Mueller 2013), and four were partly or entirely conducted in the UK (Elsworth 2011; Okkersen 2018; Wallace 2019; White 2016). Five studies published a protocol; of these, four were set partly or entirely in the Netherlands (Koopman 2016; Okkersen 2018; Van Groenestijn 2019; Voet 2014), and two were set partly or entirely in the UK (Okkersen 2018; White 2016). One study published a description of interventions using the template for intervention and replication (TIDieR) checklist and guide by the EQUATOR Network (The EQUATOR Network) (Okkersen 2018).
Across 11 full reports of studies of people with NMD (excluding Elsworth 2011 and White 2016), 737 randomised participants were included of 2777 people invited or assessed for eligibility (less than 27%). As noted previously, relatively few studies reported everyday physical activity as a primary outcome. Other primary outcomes reported included measures of self‐reported fatigue and quality of life, and performance measures for postural stability, fitness, and functional ability. Aside from reimbursement for travel expenses and gym membership in several studies, one included study paid an additional cash incentive for study participation (Mueller 2013). This financial incentive could contribute to the effectiveness of physical activity‐promoting intervention but its analysis as a possible effect modifier is beyond the scope of this review.
How randomised controlled trial interventions relate to aspects of physical activity promotion
Elsworth 2011 compared the effects on physical activity of a 12‐week exercise programme with a Physical Activity Support System versus no exercise programme and no Physical Activity Support System in adults with neurological conditions including NMD. A stated aim of this parallel RCT was to assess the feasibility and safety of the activity‐supported intervention. Physical activity was one of the primary outcome measures, although not used in a power calculation to determine the study sample size.
Recruitment: the study took place in the UK with potential participants recruited through local neurological services and the Dementias and Neurodegenerative Diseases Research Network (DeNDRoN). Of 103 people assessed for eligibility, 99 were randomised into the study (96%). Two people became unwell, one could not be contacted, and another declined to participate after further discussion.
Baseline characteristics and comparability: these data were not available for the subpopulation of participants with NMD. Overall baseline characteristics appeared similar between groups, in accordance with reporting by study authors.
Physical activity outcome measurement: 'experienced physical activity' was reported using the Physical Activity Scale for the Elderly (PASE; ranging from 0 to 400+ with higher scores indicating a better outcome). Physical activity was also measured using a Step Activity Monitor (SAM) for eight days. Change scores in the composite PASE rating and daily steps (count) were reported over 12 weeks between assessments at baseline and at the end of intervention, with measurements reported to be completed after assessment visits. Final scores were also reported after 12 weeks and 24 weeks (three months' follow‐up). No results were reported for the subgroup of participants with NMDs.
Three studies involved adults with DPN (Grewal 2015; Lemaster 2008; Mueller 2013). Grewal 2015 compared the effects on physical activity of a four‐week sensor‐based, interactive exercise programme with no sensor‐based, interactive exercise programme in adults living with DPN. A stated aim of this parallel RCT was to assess the effects of intervention on physical activity. However, physical activity was neither a primary outcome nor used in a power calculation to determine the study sample size.
Recruitment: the study took place in the USA (Arizona) and Qatar, with potential participants recruited through outpatient clinics. Of 54 people assessed for eligibility, 39 were randomised into the study (72%). Eight people (15%) met exclusion criteria and seven people (13%) declined to participate.
Baseline characteristics and comparability: 19 people were randomised to the intervention group (42% male, ethnicity not reported) and 20 to the control group, of whom 16 supplied baseline characteristics (50% male, ethnicity not reported). The mean age of the intervention group was 62.6 years (SD 7.98) and 64.9 years (SD 8.50) in the control group. Baseline characteristics appeared similar between groups, in accordance with reporting by study authors.
Physical activity outcome measurement: a PAMSys activity sensor was positioned in the chest pocket of a custom‐made t‐shirt that was worn for 48 hours. Time spent walking (hours per 48 hours) and daily steps (count, activity monitor) were reported as final scores after four weeks, with the assessment assumed to be after the intervention.
Lemaster 2008 compared the effects on physical activity of a 12‐month physical activity programme (weight‐bearing) with no physical activity programme in adults living with DPN. A stated aim of this parallel RCT was to 'encourage participants to gradually increase total daily weight‐bearing steps'. Physical activity was the primary outcome measure and also used in a power calculation to determine the study sample size.
Recruitment: the study took place in the USA (Missouri) with recruitment through primary care, endocrinology, or podiatry practices of participants aged 50 years and over who received diabetes or foot care. Of 260 people invited to participate, only 79 were randomised into the study (30%). One hundred and five people (40%) declined to participate or could not be contacted; it is understood that 44 people (17%) did not meet inclusion criteria and 50 people (19%) met exclusion criteria.
Baseline characteristics and comparability: 41 people were randomised to the intervention group (53% male and 92% white ethnicity) and 38 to the control group (47% male and 93% white ethnicity). The mean age of the intervention group was 66.6 years (SD 10.4) and 64.8 years (SD 9.4) in the control group. Baseline characteristics appeared to be similar between groups, in accordance with reporting by study authors.
Physical activity outcome measurement: participants wore a StepWatch accelerometer on the ankle for 14 days. Time spent walking (minutes per week), daily steps (count) and steps taken in 30‐minute bouts (count) were reported as final scores after three months, six months, and 12 months. Assessment was during intervention at three months and six months, but it was unclear if the final assessment was during or after the intervention.
Mueller 2013 compared the effects on physical activity of a 12‐week weight‐bearing exercise programme with a non‐weight‐bearing exercise programme in people living with DPN. A stated aim of this parallel RCT was to assess the effects of intervention on physical activity, which was one of the primary outcome measures and also used in a power calculation to determine the study sample size.
Recruitment: the study took place in the USA with potential participants recruited through a database of previous participants, the Washington University School of Medicine Research Participant Registry, cable television commercials, a newspaper story, and recruitment posters displayed in a Diabetes Treatment Center and on area commuter trains. Of 265 people invited to participate, only 29 were randomised into the study (11%). Ninety people (34%) did not have diabetes or neuropathy, 84 people (32%) declined to participate, could not be contacted, had a time conflict or lack of interest; 43 people (16%) were excluded due to other illnesses, orthopaedic issues, or inability to exercise; and 19 people (7%) did not meet inclusion criteria.
Baseline characteristics and comparability: 15 people were randomised to the weight‐bearing group (67% male, ethnicity not reported) and 14 to the non‐weight‐bearing group (50% male, ethnicity not reported). The mean age of the weight‐bearing group was 65.2 years (SD 12.8) and 63.9 years (SD 12.5) in the non‐weight‐bearing group. We noted the difference in proportion of males, but baseline characteristics appeared to be broadly similar between groups, in accordance with reporting by study authors.
Physical activity outcome measurement: participants wore a StepWatch accelerometer on the ankle for 14 days with data used from a seven‐day period in which at least eight hours of activity were recorded and at least one weekend day. Daily steps (count) were reported as final scores after 16 weeks with the assessment completed after intervention.
Three studies involved adults with FSHD (Andersen 2015; Andersen 2017; Voet 2014). Andersen 2015 compared the effects on physical activity of a 12‐week exercise programme with a protein supplement versus an exercise programme with a placebo supplement versus neither intervention in adults with FSHD type 1. This parallel RCT did not state that it aimed specifically to promote or assess the effects of intervention on physical activity. Included as a secondary outcome measure, physical activity was not used in a power calculation to determine the study sample size.
Recruitment: the study took place in Denmark with potential participants recruited through the Copenhagen Neuromuscular Center and from the Rehabilitation Centre for Neuromuscular Diseases in Denmark. Of 140 people assessed for eligibility, only 41 were randomised into the study (29%). Fifty people (36%) did not respond on contact, 40 people (29%) met exclusion criteria, and nine people declined to participate (6%).
Baseline characteristics and comparability: 18 participants were randomised to a protein supplement and training group of whom 13 were included in baseline characteristics (62% male, ethnicity not reported), 13 to a placebo supplement and training group (54% male, ethnicity not reported) and 10 to no intervention, of whom nine had included baseline data (56% male, ethnicity not reported). The mean age of the protein‐supplemented training group was 42.6 years (range 24 to 55), 45.7 years (range 22 to 63) in the placebo‐supplemented training group and 51.3 years (range 24 to 65) in the no intervention group. Baseline fitness and walking speed were reported to be lower in the non‐intervention group than the training groups but demographics appeared similar between groups.
Physical activity outcome measurement: participants wore a SenseWear Pro3 accelerometer for three days before and after 16 weeks of intervention. Physical activity was measured as daily steps (1000 counts) and daily energy expenditure (1000 kilocalories (kcal)). A Bouchard diary was also used to estimate daily energy expenditure (1000 kcal). Final scores were reported after the intervention but the results were not usable because the mean data were only reported with ranges.
Andersen 2017 compared the effects on physical activity of eight weeks of high‐intensity interval training (HIT) with no HIT in adults with FSHD type 1. This parallel RCT stated that it aimed specifically to promote or assess the effects of intervention on physical activity. In fact, the study investigators specified that participants could not change their activity during the study, although this was not an exclusion criterion. Included as a secondary outcome measure, physical activity was not used in a power calculation to determine the study sample size.
Recruitment: the study took place in Denmark with potential participants recruited through the Copenhagen Neuromuscular Center. Of 97 people assessed for eligibility, only 13 were randomised into the study (13%). Forty‐three people (44%) met exclusion criteria, 25 people (26%) declined to participate, and 16 people (16%) did not respond on contact.
Baseline characteristics and comparability: six participants were randomised to a supervised HIT group (67% male, ethnicity not reported) and seven to a usual care group of whom six were included in baseline characteristics (83% male, ethnicity not reported). The mean age of the HIT group was 53 years (SD 15) and 46 years (SD 9) in the usual care group. Baseline self‐reported physical activity (Metabolic Equivalent of Task (MET) hours/week) was lower in the training group than usual care, but characteristics appeared broadly similar between groups, in accordance with reporting by study authors.
Physical activity outcome measurement: an Omron Walking Style Pro pedometer was worn for four to seven days at baseline (before exercise intervention) and prior to the follow‐up assessment at eight weeks. Physical activity was also reported using the International Physical Activity Questionnaire (IPAQ). However, narrative results were reported only for physical activity measured as steps/day.
Voet 2014 compared the effects on physical activity of a 16‐week aerobic exercise programme versus CBT versus neither intervention in adults with FSHD. This parallel RCT did not state that it aimed to promote or assess the effects of intervention on physical activity. Included as a secondary outcome measure, physical activity was not used in a power calculation to determine the study sample size.
Recruitment: the study took place at nine healthcare institutions in the Netherlands. People with FSHD were invited to participate if they had participated in any previous study at the centre, were registered in a Dutch neuromuscular database, or participated in a patient support organisation. Of 337 people invited to participate, only 57 were randomised into the study (17%). One hundred and ninety‐nine people declined to participate (59%), 84 people did not respond on contact (25%), and 37 people either met exclusion criteria or did not meet inclusion criteria (11%).
Baseline characteristics and comparability: 20 people were randomised to aerobic exercise training (60% male, ethnicity not reported), 13 to CBT (62% male, ethnicity not reported), and 24 to usual care (71% male, ethnicity not reported). The median age of the exercise group was 59 years (range 21 to 68), 49 years (range 24 to 69) in the CBT group and 52 years (range 20 to 79) in the usual care group. Baseline characteristics appeared to be similar between groups, in accordance with reporting by study authors.
Physical activity outcome measurement: 'experienced physical activity' was reported using the physical activity subscale of the Checklist Individual Strength (CIS‐Activity), which includes three questions about activity over the previous two weeks and scores each question on a seven‐point Likert scale (higher scores indicate a poorer outcome). An actometer (model unreported) was also worn on the ankle for 12 days and nights and registered data analysed across this period. The CIS‐Activity subscale ratings and body accelerations per five‐minute period (count) were reported as change scores over 16 weeks with assessments completed before and after intervention but these were not usable because participants originally in the usual care group were later amalgamated with other intervention groups.
Van Groenestijn 2019 planned to compare the effects on physical activity of a 16‐week aerobic exercise programme with no aerobic exercise programme in adults with ALS. A secondary aim of this parallel RCT was to assess the effects of intervention on activity limitations. Study investigators planned to measure physical activity but the outcome was removed because participants did not complete the questionnaire.
Recruitment: the study took place in the Netherlands with consecutive participants screened at five rehabilitation centres or rehabilitation departments of academic hospitals. Of 325 people assessed for eligibility, only 57 were randomised into the study (18%). One hundred and seventy‐six people (54%) did not meet eligibility criteria, 77 people (24%) declined to participate, and 15 people (5%) enrolled in a CBT trial.
Baseline characteristics and comparability: 27 people (67% male, ethnicity not reported) were randomised to aerobic exercise therapy and 30 to usual care (73% male, ethnicity not reported). The mean age of the exercise group was 60.9 years (SD 10.0) and 59.9 years (SD 10.7) in the usual care group. Baseline characteristics appeared to be similar between groups, which is consistent with reporting by study authors although they undertook a propensity‐matched analysis for baseline inequalities.
Physical activity outcome measurement: study investigators applied the LASA Physical Activity Questionnaire (LAPAQ) to estimate METs per day. As a protocol deviation, no results were reported.
Koopman 2016 compared the effects on physical activity of a four‐month aerobic exercise programme versus CBT versus neither intervention in adults living with PPS. A stated aim of this parallel RCT was to assess the effects of intervention on improving activities. However, physical activity was neither a primary outcome nor used in a power calculation to determine the study sample size.
Recruitment: the study took place in the Netherlands with potential participants recruited through seven hospitals and rehabilitation centres. Of 490 people invited to participate, only 68 were randomised into the study (14%). Two hundred people (41%) declined to participate, 129 people (26%) did not respond on contact, and 93 people (19%) did not meet inclusion criteria.
Baseline characteristics and comparability: 23 people were randomised to the exercise therapy group, of whom 22 were included in baseline characteristics (41% male and 87% white ethnicity), 23 to CBT (43% male and 96% white ethnicity), and 22 to usual care (50% male and 82% white ethnicity). The mean age of the exercise group was 56.9 years (SD 8.9), 60.1 years (SD 8.2) in the CBT group, and 60.1 years (SD 8.2) in the usual care group. Baseline characteristics appeared to be similar between groups, in accordance with reporting by study authors.
Physical activity outcome measurement: participants wore a StepWatch activity monitor for seven days. Daily steps (count) were reported as final scores after four, seven, and 10 months, with all assessments completed after intervention.
Okkersen 2018 compared the effects on physical activity of 10 months of CBT with or without an exercise programme versus no CBT and no exercise programme in adults with DM1. A stated aim of this parallel RCT was to assess the effects of intervention on health status. However, physical activity was neither a primary outcome nor used in a power calculation to determine the study sample size.
Recruitment: the multi‐centre study took place in France, Germany, the Netherlands, and the UK. Potential participants were recruited through DM1 registries, from clinics via their treating neurologists, or independent volunteering through patient organisations. Of 344 people assessed for eligibility, 255 were randomised into the study (74%). Eighty‐nine people (26%) were ineligible because they either met exclusion criteria or did not meet inclusion criteria.
Baseline characteristics and comparability: 128 people were randomised to CBT (55% male, ethnicity not reported) and 127 to standard care (53% male, ethnicity not reported). The mean age of the CBT group was 44.8 years (SD 11.7) and 46.4 years (SD 1.3) in the standard care group. Baseline characteristics appeared to be similar between groups, in accordance with reporting by study authors.
Physical activity outcome measurement: a GENEActiv tri‐axial accelerometer was worn on the ankle for seven to 14 consecutive days. Data were only analysed for days with at least 23 hours of registered activity over at least seven days. The first and last days of recorded activity were excluded 'to avoid confounding factors related to distribution or delivery procedures'. Physical activity, interpreted as mean magnitude of ankle acceleration over 24 hours and over five hours of highest and lowest activity, was reported as final scores after five, 10, and 16 months. The first assessment was completed during intervention and the final assessment postintervention, but it was unclear whether the assessment at 10 months was completed during or after the intervention.
Shrader 2015 compared the effects on physical activity of a 12‐week functional exercise programme with a stretching exercise programme in adults with SBMA. This parallel RCT did not state that it aimed specifically to promote or assess the effects of intervention on physical activity. Included as a secondary outcome measure, physical activity was not used in a power calculation to determine the study sample size.
Recruitment: the study took place in Maryland, USA. The method of recruiting participants was not reported. Of 61 people assessed for eligibility, 54 people were randomised into the study (89%) and seven people met exclusion criteria.
Baseline characteristics and comparability: 27 people were randomised to a functional exercise group of whom 24 were included in baseline characteristics (sex and ethnicity not reported), and 27 to a stretching exercise group of whom 26 had included baseline data (sex and ethnicity not reported). The mean age of the functional exercise group was 53.8 years (SD 10.0) and 56.5 years (SD 8.1) in the stretching exercise group. Baseline characteristics appeared similar between groups, in accordance with reporting by study authors.
Physical activity outcome measurement: an Actical accelerometer was worn for the first and last 10 days of the trial. Data were weighted by the number of days recorded and only included if there were at least six days of registered activity. Total physical activity was reported as an unspecified count per day. Final scores were reported after 12 weeks, with the assessment completed during intervention.
Wallace 2019 compared the effects on physical activity of a 16‐week aerobic exercise training programme versus regular telephone contact that included review of activity in adults with CMT type 1A and IBM. A stated aim of this cross‐over RCT was to explore the secondary physical and non‐physical effects of exercise intervention. Included as a secondary outcome measure, physical activity was not used in a power calculation to determine the study sample size.
Recruitment: the study took place in the UK with potential participants recruited through clinics and research databases of the National Hospital for Neurology and Neurosurgery, plus national clinics of colleagues from the British Myology Society for people with IBM. Of 404 people assessed for eligibility, only 45 people (28 with CMT and 17 with IBM) were randomised into the study (11%). One hundred and fifty‐six people (39%) did not meet inclusion criteria, 71 people (18%) declined to participate, and 132 people (33%) were excluded for other reasons.
Baseline characteristics and comparability: 23 participants (with CMT and IBM) were randomised to an aerobic exercise training group during the first period of the cross‐over study, of whom 21 participants were included in baseline characteristics (67% male, ethnicity not reported). Twenty‐two participants were randomised to a control group during the first period, of whom 20 were included in the baseline data (65% male, ethnicity not reported). The mean age of the exercise group was 46.3 years (95% CI 37.2 to 55.4) in participants with CMT and 65.4 years (95% CI 59.1 to 71.8) in participants with IBM; in the control group, the mean age was 45.3 years (95% CI 35.9 to 54.6) in participants with CMT and 57.1 years (95% CI 50.4 to 63.9) in those with IBM. Baseline characteristics appeared similar between groups of participants with the same condition although exercising participants with IBM were slightly older than those who did not exercise. The study authors noted that, as a measure of fitness, peak oxygen uptake (VO2peak) did not fully return to baseline after an eight‐week washout period among participants with CMT.
Physical activity outcome measurement: the study used a SenseWear activity monitor to measure physical activity over seven days. Physical activity duration over 3 METs (minutes) was reported as a final score following 12 weeks of training, after the intervention. The timing of physical activity review differed between groups because of the cross‐over design of the study. The IPAQ was also used before and after intervention but with sitting time (minutes) reported as an outcome rather than physical activity. Participants' first period data over 12 weeks (before cross‐over) were not available separately.
White 2016 compared the effects on physical activity of a home exercise programme with written advice about physical activity in adults with IN. Based on the study protocol, a stated aim of this parallel RCT was to assess the effects of the intervention on activity limitation. Included as a secondary outcome measure, physical activity was not used in a power calculation to determine the study sample size.
Recruitment: the study protocol set out to recruit people attending selected specialist peripheral nerve clinics in the South East and West Midlands of England and people with IN who accessed the Guillain‐Barré syndrome and Associated Inflammatory Neuropathy (GAIN) charity website or newsletter. Fifty‐eight people were randomised into the study. No further recruitment information was available at the time of preparing this review.
Baseline characteristics and comparability: these data were not available.
Physical activity outcome measurement: the seven‐question IPAQ‐short was a prespecified outcome for measuring physical activity after 12 weeks' intervention and 12 months after intervention but no results were available.
See Characteristics of included studies table for a list of all outcome measures and further information.
Excluded studies
We excluded 62 conference abstracts or full‐text reports because the studies were not RCTs, they involved a different study population, or they did not report physical activity outcome measurement (see Characteristics of excluded studies table). We translated one excluded conference abstract from Spanish (Cejudo‐Ramos 2000). We also excluded a full report in Chinese without translation as it was identifiable as a review (Zhang 2005).
Risk of bias in included studies
We completed risk of bias assessments based on full reports, with the exception of one study published only as an abstract (White 2016). We judged nine of the 13 studies to have a high risk of bias in at least one domain. Incomplete physical activity outcome reporting was one of the main reasons for this high risk of bias judgement. Two studies had at least two domains with an unclear risk of bias assessment, and two studies had a low risk of bias in all domains. See Characteristics of included studies table and, for a risk of bias summary, Figure 2.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Most studies were at low risk of bias associated with random sequence generation. We judged two studies to have an unclear risk of bias because randomisation was reported by postcode or type of clinical site (Andersen 2017; Lemaster 2008).
In terms of allocation concealment, four studies had an unclear risk of bias (Andersen 2015; Andersen 2017; Shrader 2015; White 2016); the other studies were at low risk of bias.
Blinding
We judged that it was not applicable to blind participants and personnel involved in supporting any study intervention for promoting physical activity and so we considered this at low risk of bias throughout. However, the blinding of outcome assessors was feasible. We judged most studies to have a low risk of bias associated with the blinding of outcome assessors. We found that two studies had an unclear risk of detection bias (Grewal 2015; Okkersen 2018), and we found one study to have a high risk of detection bias because the study was reported to be unblinded (Andersen 2017).
Incomplete outcome data
We judged nine of 13 studies to have a high risk of bias associated with incomplete physical activity outcome data because of large proportions of missing data or unexplained missing data (Andersen 2015; Andersen 2017; Grewal 2015; Koopman 2016; Okkersen 2018; Shrader 2015; Van Groenestijn 2019; Voet 2014; Wallace 2019). One study had an unclear risk of attrition bias (White 2016), and the other studies were at low risk of attrition bias.
Selective reporting
We judged seven studies at low risk of selective reporting. We found three studies had an unclear risk of selective reporting (Andersen 2017; Wallace 2019; White 2016). Three studies were at high risk of selective reporting because available results were reported incompletely (Grewal 2015; Koopman 2016; Van Groenestijn 2019). In terms of selective non‐reporting, two studies had prespecified outcome measures (including the EuroQol (EQ‐5D) and LAPAQ) that were not reported in the results (Koopman 2016; Van Groenestijn 2019). Another study prespecified activities of daily living assessment but, as a protocol deviation, the study investigators reported they had forgotten to delete this outcome domain from the list; we did not judge this to be reporting bias (Okkersen 2018).
Other potential sources of bias
We judged one study at unclear risk of other potential sources of bias because the study was published as an abstract only (White 2016). We did not identify any of the other 12 studies to have other potential sources of bias.
Effects of interventions
See: Table 1; Table 2; Table 3
Interventions with physical activity as a primary outcome
A physical activity programme (weight‐bearing) compared to no physical activity programme in people living with NMD
One RCT involving people with DPN contributed data for this comparison (Lemaster 2008).
At six months, 18 participants (45%) in the physical activity programme and 13 participants (35%) in the control group adhered to more than half of the study protocol elements. At 12 months, only seven participants (18%) in the physical activity programme and nine participants (24%) in the control group adhered to more than half of the study protocol elements. The study reported ITT analysis of randomised participants, irrespective of adherence, but did not specify the assumptions made for ITT analysis.
Time spent walking (minutes per week, activity monitor)
After three months (during intervention): the MD was 34 min per week (95% CI –92.19 to 160.19; 1 study, 69 participants; low‐certainty evidence; Analysis 1.1) in favour of the physical activity programme but the CIs included the possibility of an effect favouring either the physical activity programme or no physical activity programme (Table 1).
1.1. Analysis.

Comparison 1: A physical activity (PA) programme (weight‐bearing) compared no PA programme in people living with NMD, Outcome 1: Time spent walking (minutes per week, activity monitor)
After six months (during intervention): the MD was 68 min per week (95% CI –55.35 to 191.35; 1 study, 74 participants; low‐certainty evidence; Analysis 1.1) in favour of the physical activity programme but the CI included the possibility of an effect favouring either the physical activity programme or no physical activity programme (Table 1).
After 12 months (unclear if during or after intervention): the MD was 49 min per week (95% CI –75.73 to 173.73; 1 study, 70 participants; low‐certainty evidence; Analysis 1.1) in favour of the physical activity programme but the CI included the possibility of an effect favouring either the physical activity programme or no physical activity programme (Table 1).
We downgraded the certainty of the evidence once for study limitations associated with an unclear risk of bias in random sequence generation, and once for imprecision associated with a wide CI. We did not identify an MID from the literature although WHO guidance emphasises at least meeting recommended levels of physical activity (WHO 2020a; WHO 2020b). On the premise that any increase in physical activity is considered important, the intervention may have led to an important increase in physical activity.
Daily steps (count, activity monitor)
After three months (during intervention): the MD was 178 steps per day (95% CI –459.81 to 815.81; 1 study, 69 participants; Analysis 1.2) in favour of the physical activity programme but the CI included the possibility of an effect favouring either the physical activity programme or no physical activity programme.
1.2. Analysis.

Comparison 1: A physical activity (PA) programme (weight‐bearing) compared no PA programme in people living with NMD, Outcome 2: Daily steps (count, activity monitor)
After six months (during intervention): the MD was 408 steps per day (95% CI –243.40 to 1059.40; 1 study, 74 participants; Analysis 1.2) in favour of the physical activity programme but the CI included the possibility of an effect favouring either the physical activity programme or no physical activity programme.
After 12 months (unclear if during or after intervention): the MD was 262 steps per day (95% CI –407.40 to 931.40; 1 study, 70 participants; Analysis 1.2) in favour of the physical activity programme but the CI included the possibility of an effect favouring either the physical activity programme or no physical activity programme.
Steps taken in 30‐minute bouts (count, activity monitor)
After three months (during intervention): the MD was 50 steps in 30‐minute bouts (95% CI –27.66 to 127.66; 1 study, 69 participants; Analysis 1.3) in favour of the physical activity programme but the CIs included the possibility of an effect favouring either the physical activity programme or no physical activity programme.
1.3. Analysis.

Comparison 1: A physical activity (PA) programme (weight‐bearing) compared no PA programme in people living with NMD, Outcome 3: Steps taken in 30‐minute bouts (count, activity monitor)
After six months (during intervention): the MD was 83 steps in 30‐minute bouts (95% CI –20.95 to 186.95; 1 study, 74 participants; Analysis 1.3) in favour of the physical activity programme but the CIs included the possibility of an effect favouring either the physical activity programme or no physical activity programme.
After 12 months (unclear if during or after intervention): the MD was 33 steps in 30‐minute bouts (95% CI –69.56 to 135.56; 1 study, 70 participants; Analysis 1.3) in favour of the physical activity programme but the CIs included the possibility of an effect favouring either the physical activity programme or no physical activity programme.
Quality of life
The study did not report quality of life.
Adverse events
There were no comparative data between groups for any type of adverse event. However, we narratively reported rate ratios calculated in the study specifically for foot lesions and ulcers (see Comments in Table 1).
Over 12 months, the reported rate ratio for all types of foot lesions (ignoring multiple lesions/episode) was 1.24 (95% CI 0.70 to 2.19; 1 study, 70 participants) in favour of no physical activity programme but the CI included the possibility of an effect favouring either the physical activity programme or no physical activity programme.
Over 12 months, the reported rate ratio for all full‐thickness foot ulcers (ignoring multiple lesions/episode) was 0.96 (95% CI 0.38 to 2.42; 1 study, 70 participants) in favour of the physical activity programme but the CI included the possibility of an effect favouring either the physical activity programme or no physical activity programme.
These study‐reported data on foot lesions and full‐thickness ulcers were limited by imprecision.
Serious adverse events
There were no data on the number of participants with serious adverse events.
A weight‐bearing exercise programme compared to a non‐weight‐bearing exercise programme in people living with NMD
One RCT involving people with DPN contributed data for this comparison (Mueller 2013). We did not create a summary of findings table for this comparison because none of the study outcomes matched prespecified outcome measurement for inclusion.
The mean proportion of participants attending all exercise sessions in the weight‐bearing programme was 83.4% (SD 11), compared with 83.3% (SD 10.8) in the non‐weight‐bearing programme. The study reported ITT analysis of randomised participants but did not specify assumptions made for ITT analysis.
Daily steps (count, activity monitor)
After 16 weeks (after intervention): the MD was –485 steps per day (95% CI –1773.66 to 803.66; 1 study, 29 participants; Analysis 2.1) in favour of the non‐weight‐bearing exercise programme but the CI included the possibility of an effect favouring either the non‐weight‐bearing exercise programme or the weight‐bearing exercise programme.
2.1. Analysis.

Comparison 2: A weight‐bearing (WB) exercise programme compared to a non‐WB exercise programme in people living with NMD, Outcome 1: Daily steps (count, activity monitor)
Quality of life
The study did not report quality of life.
Adverse events
There were no comparative data available between groups for any type of adverse event. We calculated RRs specifically for foot lesions and ulcers in the absence of study‐reported rate ratios, and reported these narratively.
Participants with foot lesions after 16 weeks: the RR was 1.31 (95% CI 0.54 to 3.17; 1 study, 29 participants) in favour of the non‐weight‐bearing exercise programme but the CI included the possibility of an effect favouring either the non‐weight‐bearing exercise programme or the weight‐bearing exercise programme.
Participants with foot ulcers after 16 weeks: the RR was 0.50 (95% CI 0.05 to 4.90; 1 study, 29 participants) in favour of the weight‐bearing exercise programme but the CI included the possibility of an effect favouring either the weight‐bearing exercise programme or the non‐weight‐bearing exercise programme.
Serious adverse events
There were no data on the number of participants with serious adverse events.
Interventions with physical activity as a secondary or exploratory outcome
A sensor‐based, interactive exercise programme compared to no sensor‐based, interactive exercise programme in people living with NMD
One RCT involving people with DPN contributed data for this comparison (Grewal 2015).
The study did not report on participants' adherence. Physical activity was reported for a subgroup of participants without further details, and those with active foot ulcers, among other contraindications, were excluded from the study analysis (see Characteristics of included studies table). Other outcomes were reported using per‐protocol analysis.
Time spent walking (hours per 48 hours, activity monitor)
After four weeks (interpreted to be after intervention): the MD was –0.64 hours per 48 hours (95% CI –2.42 to 1.13; 1 study, 25 participants; very low‐certainty evidence; Analysis 3.1) in favour of no exercise programme but the CI included the possibility of an effect favouring either the exercise programme or no exercise programme (Table 2). We downgraded the certainty of the evidence once for study limitations associated with a high risk of selective reporting and attrition bias, and twice for imprecision associated with a very wide CI.
3.1. Analysis.

Comparison 3: A sensor‐based, interactive exercise programme compared to no sensor‐based, interactive exercise programme in people living with NMD, Outcome 1: Time spent walking (hours per 48 hours, activity monitor)
Daily steps (count, activity monitor)
After four weeks (interpreted to be after intervention): the MD was 1788 steps per day (95% CI –3440.55 to 7016.55; 1 study, 25 participants; Analysis 3.2) in favour of the exercise programme but the CI included the possibility of an effect favouring either the exercise programme or no exercise programme.
3.2. Analysis.

Comparison 3: A sensor‐based, interactive exercise programme compared to no sensor‐based, interactive exercise programme in people living with NMD, Outcome 2: Daily steps (count, activity monitor)
Quality of life (12‐item Short Form Health Survey, Physical Component Score, questionnaire)
After four weeks (interpreted to be after intervention): the MD was 0.24 points (95% CI –5.98 to 6.46; 1 study, 35 participants; very low‐certainty evidence; Analysis 3.3) in favour of the exercise programme but the CI included the possibility of an effect favouring either the exercise programme or no exercise programme (Table 2). We downgraded the certainty of the evidence once for study limitations associated with a high risk of selective reporting and attrition bias, and twice for imprecision associated with a very wide CI.
3.3. Analysis.

Comparison 3: A sensor‐based, interactive exercise programme compared to no sensor‐based, interactive exercise programme in people living with NMD, Outcome 3: Quality of life (Physical Component Score, questionnaire)
Quality of life (12‐item Short Form Health Survey, Mental Component Score, questionnaire)
After four weeks (interpreted to be after intervention): the MD was 5.10 points (95% CI –0.58 to 10.78; 1 study, 35 participants; low‐certainty evidence; Analysis 3.4) in favour of the exercise programme but the CI included the possibility of an effect favouring either the exercise programme or no exercise programme (Table 2). We downgraded the certainty of the evidence once for study limitations associated with a high risk of selective reporting and attrition bias, and once for imprecision associated with a wide CI.
3.4. Analysis.

Comparison 3: A sensor‐based, interactive exercise programme compared to no sensor‐based, interactive exercise programme in people living with NMD, Outcome 4: Quality of life (Mental Component Score, questionnaire)
We did not identify an anchor‐ or distribution‐based MID for the SF‐12 quality of life questionnaire in people with DPN or NMD. Based on the effect estimates and low‐certainty evidence, we found that the sensor‐based interactive exercise programme may have made little or no difference to the Mental Component Score (MCS) and Physical Component Score (PCS) for quality of life.
Adverse events
There were no comparative data available between groups for any type of adverse event.
Serious adverse events
The study did not report serious adverse events.
An aerobic exercise programme compared to no aerobic exercise programme in people living with NMD
Two RCTs involving people with PPS or ALS contributed data for this comparison but we did not meta‐analyse them because they measured outcomes in different ways (Koopman 2016; Van Groenestijn 2019). We did not include physical activity outcomes in a summary of findings table because they did not match prespecified outcome measurements (Table 4).
1. An aerobic exercise programme compared to no aerobic exercise programme in people living with NMD.
| Aerobic exercise programme compared to no aerobic exercise programme | ||||||
|
Patient or population: people with NMD Setting: the Netherlands Intervention: aerobic exercise programme Comparison: no aerobic exercise programme | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with no aerobic exercise programme | Risk with aerobic exercise programme | |||||
| Time spent physically active | — | — | — | — | — | Outcome not measured. |
|
Quality of life (SF‐36 PCS)
assessed with: final scores, recorded after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 4 months |
The mean quality of life (SF‐36 PCS) was 33.6 points | MD 1.8 points higher (2.9 lower to 6.5 higher) | — | 37 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Quality of life (SF‐36 MCS)
assessed with: final scores, recorded after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 4 months |
The mean quality of life (SF‐36 MCS) was 52.5 points | MD 0.1 points lower (6.86 lower to 6.66 higher) | — | 37 (1 RCT) | ⊕⊝⊝⊝ Verylowa,c | — |
|
Disease‐specific quality of life (ALSAQ‐40, questionnaire; lower = better quality of life) assessed with: slope over time, after intervention Follow‐up: 6 months |
The mean disease‐specific quality of life (ALSAQ‐40; lower = better quality of life) was 2.48 points monthly | MD 1.06 points monthly lower (2.55 lower to 0.43 higher) | — | 57 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Quality of life (SF‐36 PCS; higher = better quality of life) assessed with: slope over time, after intervention Follow‐up: 6 months |
The mean quality of life (SF‐36 PCS, questionnaire; higher = better quality of life) was –0.5 points monthly | MD 0.51 points monthly lower (1.36 lower to 0.34 higher) | — | 57 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Quality of life (SF‐36 MCS; higher = better quality of life) assessed with: slope over time, after intervention Follow‐up: 6 months |
The mean quality of life (SF‐36 MCS; higher = better QoL) was –0.09 points monthly | MD 0.23 points monthly higher (0.64 lower to 1.1 higher) | — | 57 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Quality of life (SF‐36 PCS) assessed with: final scores, after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 7 months |
The mean quality of life (SF‐36 PCS, questionnaire) was 33.2 points | MD 1.1 points higher (3.74 lower to 5.94 higher) | — | 36 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Quality of life (SF‐36 MCS) assessed with: final scores, after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 7 months |
The mean quality of life (SF‐36 MCS) was 51.7 points | MD 1.9 points lower (8.74 lower to 4.94 higher) | — | 36 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Quality of life (SF‐36 PCS) assessed with: final scores, after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 10 months |
The mean quality of life (SF‐36 PCS) was 34.5 points | MD 1.3 points higher (3.71 lower to 6.31 higher) | — | 34 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Quality of life (SF‐36 MCS) assessed with: final scores, after intervention (higher = better quality of life) Follow‐up: 10 months |
The mean quality of life (SF‐36 MCS) was 52.4 points | MD 4.4 points lower (12.18 lower to 3.38 higher) | — | 34 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
| Adverse events/serious adverse events | — | — | — | — | — | No comparative data available between groups for any type of adverse event. |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ALSAQ‐40: Amyotrophic Lateral Sclerosis Assessment Questionnaire; CI: confidence interval; MCS: Mental Component Score; MD: mean difference; NMD: neuromuscular disease; PCS: Physical Component Score; QoL: quality of life; RCT: randomised controlled trial; SF‐36: 36‐item Short Form Health Survey. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| See interactive version of this table: gdt.gradepro.org/presentations/#/isof/isof_question_revman_web_422111384441723949. | ||||||
aDowngraded once for study limitations associated with a high risk of attrition and selection bias. bDowngraded once for imprecision associated with a wide CI. cDowngraded twice for imprecision associated with a very wide CI.
Koopman 2016 reported using ITT analysis with no imputation of missing data, under the assumption that data were missing at random. In the absence of measurement of outcome data from all randomised participants, the analysis could be described as an available‐case analysis. The amount of missing data varied across different time points and outcome measures. The study reported that additional per‐protocol analyses of a subset of participants who completed more than 47 of 63 (75%) exercise sessions showed similar effect estimates as ITT analysis. In the ITT population, the median number of exercise sessions completed was 57 (range 8 to 63).
Van Groenestijn 2019 reported ITT analysis of randomised participants, irrespective of whether they received the allocated intervention and completed follow‐up assessment. The assumptions made for ITT analysis were not specified. For outcomes at six months, including the ALS Assessment Questionnaire (ALSAQ‐40), the study reported additional per‐protocol analyses for a subset of participants who completed more than 75% of exercise sessions and attended the follow‐up assessment. The study reported that quality of life results favoured the exercise programme over usual care. Of the 18 participants who started the exercise programme, 11 (61%) attended at least 75% of the sessions, although one person died before follow‐up, for reasons considered unrelated to the exercise programme. The reasons reported for non‐attendance at exercise sessions included psychosocial problems, clavicular fracture due to a fall, time constraints, perceived lack of benefit, holiday, and an unrelated medical procedure.
Daily steps (count, activity monitor)
In Koopman 2016 after four months (after intervention): the MD was –197 steps per day (95% CI –2332.21 to 1938.21; 1 study, 36 participants; Analysis 4.1) in favour of no exercise programme but the CIs included the possibility of an effect favouring either the exercise programme or no exercise programme.
4.1. Analysis.

Comparison 4: An aerobic exercise programme compared to no aerobic exercise programme in people living with NMD, Outcome 1: Daily steps (count, activity monitor)
After seven months (three months after intervention): the MD was –118 steps per day (95% CI –2010.18 to 1774.18; 1 study, 34 participants; Analysis 4.1) in favour of no exercise programme but the CIs included the possibility of an effect favouring either the exercise programme or no exercise programme.
After 10 months (six months after intervention): the MD was 205 steps per day (95% CI –1618.68 to 2028.68; 1 study, 32 participants; Analysis 4.1) in favour of the exercise programme but the CIs included the possibility of an effect favouring either the exercise programme or no exercise programme.
Disease‐specific quality of life (ALS Assessment Questionnaire)
In Van Groenestijn 2019 (slope over time, up to six months after intervention): the MD was –1.06 points monthly (95% CI –2.55 to 0.43; 1 study, 57 participants; low‐certainty evidence; Analysis 4.2) in favour of the exercise programme but the CIs included the possibility of an effect favouring either the exercise programme or no exercise programme (Table 4). We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition and selection bias, and once for imprecision associated with a wide CI.
4.2. Analysis.

Comparison 4: An aerobic exercise programme compared to no aerobic exercise programme in people living with NMD, Outcome 2: Disease‐specific quality of life (ALSAQ‐40, questionnaire)
Quality of life (36‐item Short Form Health Survey, Physical Component Score, questionnaire)
In Van Groenestijn 2019 (slope over time, up to six months after intervention): the MD was –0.51 points monthly (95% CI –1.36 to 0.34; 1 study, 57 participants; low‐certainty evidence; Analysis 4.3) in favour of no exercise programme but the CIs included the possibility of an effect favouring either the exercise programme or no exercise programme (Table 4). We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition and selection bias, and once for imprecision associated with a wide CI.
4.3. Analysis.

Comparison 4: An aerobic exercise programme compared to no aerobic exercise programme in people living with NMD, Outcome 3: Quality of life (SF‐36 Physical Component Score, questionnaire)
Quality of life (36‐item Short Form Health Survey, Mental Component Score. questionnaire)
In Van Groenestijn 2019 (slope over time, up to six months after intervention): the MD was 0.23 points monthly (95% CI –0.64 to 1.10; 1 study, 57 participants; low‐certainty evidence; Analysis 4.4) in favour of the exercise programme but the CIs included the possibility of an effect favouring either the exercise programme or no exercise programme (Table 4). We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition and selection bias, and once for imprecision associated with a wide CI.
4.4. Analysis.

Comparison 4: An aerobic exercise programme compared to no aerobic exercise programme in people living with NMD, Outcome 4: Quality of life (SF‐36 Mental Component Score, questionnaire)
Quality of life (36‐item Short Form Health Survey, Physical Component Score, questionnaire)
In Koopman 2016 after four months (recorded after intervention): the MD was 1.80 points (95% CI –2.90 to 6.50; 1 study, 37 participants; low‐certainty evidence; Analysis 4.5) in favour of the exercise programme but the CI included the possibility of an effect favouring either the exercise programme or no exercise programme (Table 4).
4.5. Analysis.

Comparison 4: An aerobic exercise programme compared to no aerobic exercise programme in people living with NMD, Outcome 5: Quality of life (SF‐36 Physical Component Score, questionnaire)
After seven months (three months after intervention): the MD was 1.10 points (95% CI –3.74 to 5.94; 1 study, 36 participants; low‐certainty evidence; Analysis 4.5) in favour of the exercise programme but the CI included the possibility of an effect favouring either the exercise programme or no exercise programme (Table 4).
After 10 months (six months after intervention): the MD was 1.30 points (95% CI –3.71 to 6.31; 1 study, 34 participants; low‐certainty evidence; Analysis 4.5) in favour of the exercise programme but the CI included the possibility of an effect favouring either the exercise programme or no exercise programme (Table 4).
We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition and selection bias, and once for imprecision associated with a wide CI.
Quality of life (36‐item Short Form Health Survey, Mental Component Score, questionnaire)
In Koopman 2016 after four months (recorded after intervention): the MD was –0.10 points (95% CI –6.86 to 6.66; 1 study, 37 participants; very low‐certainty evidence; Analysis 4.6) in favour of no exercise programme but the CIs included the possibility of an effect favouring either the exercise programme or no exercise programme (Table 4). We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition and selection bias, and twice for imprecision associated with a very wide CI.
4.6. Analysis.

Comparison 4: An aerobic exercise programme compared to no aerobic exercise programme in people living with NMD, Outcome 6: Quality of life (SF‐36 Mental Component Score, questionnaire)
After seven months (three months after intervention): the MD was –1.90 points (95% CI –8.74 to 4.94; 1 study, 36 participants; low‐certainty evidence; Analysis 4.6) in favour of no exercise programme but the CI included the possibility of an effect favouring either the exercise programme or no exercise programme (Table 4). We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition and selection bias, and once for imprecision associated with a wide CI.
After 10 months (six months after intervention): the MD was –4.40 points (95% CI –12.18 to 3.38; 1 study, 34 participants; low‐certainty evidence; Analysis 4.6) in favour of no exercise programme but the CI included the possibility of an effect favouring either the exercise programme or no exercise programme (Table 4). We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition and selection bias, and once for imprecision associated with a wide CI.
Adverse events
Koopman 2016 and Van Groenestijn 2019 reported results for the training group but there were no comparative data available between groups for any type of adverse event.
Serious adverse events
There were no comparative data available between groups.
An aerobic exercise programme compared to CBT in people living with NMD
One RCT involving people with PPS contributed data for this comparison (Koopman 2016). We did not include physical activity outcomes in a summary of findings table because they did not match prespecified outcome measurements (Table 5).
2. An aerobic exercise programme compared to CBT in people living with NMD.
| Aerobic exercise programme compared to CBT | ||||||
|
Patient or population: people with NMD Setting: the Netherlands Intervention: aerobic exercise programme Comparison: CBT | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with CBT | Risk with aerobic exercise programme | |||||
| Time spent physically active | — | — | — | — | — | Outcome not measured. |
|
Quality of life (SF‐36 PCS) assessed with: final scores, recorded after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 4 months |
The mean quality of life (SF‐36 PCS) was 34.9 points | MD 0.5 points higher (4.19 lower to 5.19 higher) | — | 40 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b | — |
|
Quality of life (SF‐36 MCS) assessed with: final scores, recorded after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 4 months |
The mean quality of life (SF‐36 MCS) was 52.4 points | MD 1.2 points higher (3.9 lower to 6.3 higher) | — | 40 (1 RCT) | ⊕⊕⊝⊝ Lowa,c | — |
|
Quality of life (SF‐36 PCS) assessed with: final scores, after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 7 months |
The mean quality of life (SF‐36 PCS) was 36 points | MD 1.7 points lower (6.58 lower to 3.18 higher) | — | 37 (1 RCT) | ⊕⊕⊝⊝ Lowa,c | — |
|
Quality of life (SF‐36 MCS) assessed with: final scores, after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 7 months |
The mean quality of life (SF‐36 MCS) was 49.8 points | MD 3.2 points higher (3.03 lower to 9.43 higher) | — | 37 (1 RCT) | ⊕⊕⊝⊝ Lowa,c | — |
|
Quality of life (SF‐36 PCS) assessed with: final scores, after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 10 months |
The mean quality of life (SF‐36 PCS) was 36.1 points | MD 0.3 points lower (4.88 lower to 4.28 higher) | — | 38 (1 RCT) | ⊕⊝⊝⊝ Very lowa,b | — |
|
Quality of life (SF‐36 MCS) assessed with: final scores, after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 10 months |
The mean quality of life (SF‐36 MCS) was 48 points | MD 1.3 points higher (6.34 lower to 8.94 higher) | — | 38 (1 RCT) | ⊕⊕⊝⊝ Lowa,c | — |
| Adverse events/serious adverse events | — | — | — | — | — | No comparative data available between groups for any type of adverse event. |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CBT: cognitive behavioural therapy; CI: confidence interval; MCS: Mental Component Score; MD: mean difference; NMD: neuromuscular disease; PCS: Physical Component Score; RCT: randomised controlled trial; SF‐36: 36‐item Short Form Health Survey. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| See interactive version of this table: gdt.gradepro.org/presentations/#/isof/isof_question_revman_web_422112777684393547. | ||||||
aDowngraded once for study limitations associated with a high risk of attrition and selection bias. bDowngraded twice for imprecision associated with a very wide CI. cDowngraded once for imprecision associated with a wide CI.
Koopman 2016 reported using ITT analysis with no imputation of missing data, under the assumption that data were missing at random. In the ITT population, the median number of CBT sessions was seven (range zero to 12). According to the study protocol, the total number of sessions could vary from 12 to 16 depending on the modules taken. The median proportion of exercise sessions completed was 90% (range 13% to 100%).
Daily steps (count, activity monitor)
In Koopman 2016 after four months (after intervention): the MD was 449 steps per day (95% CI –1317.15 to 2215.15; 1 study, 36 participants; Analysis 5.1) in favour of the exercise programme but the CI included the possibility of an effect favouring either CBT or the exercise programme.
5.1. Analysis.

Comparison 5: An aerobic exercise training programme compared to cognitive behavioural therapy (CBT) in people living with NMD, Outcome 1: Daily steps (count, activity monitor)
After seven months (three months after intervention): the MD was –11 steps per day (95% CI –1852.50 to 1830.50; 1 study, 35 participants; Analysis 5.1) in favour of CBT but the CI included the possibility of an effect favouring either CBT or the exercise programme.
After 10 months (six months after intervention): the MD was 137 steps per day (95% CI –1604.76 to 1878.76; 1 study, 35 participants; Analysis 5.1) in favour of the exercise programme but the CIs included the possibility of an effect favouring either CBT or the exercise programme.
Quality of life (36‐item Short Form Health Survey, Physical Component Score, questionnaire)
In Koopman 2016 after four months (recorded after intervention): the MD was 0.50 points (95% CI –4.19 to 5.19; 1 study, 40 participants; very low‐certainty evidence; Analysis 5.2) in favour of the exercise programme but the CIs included the possibility of an effect favouring either CBT or the exercise programme (Table 5). We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition and selection bias, and twice for imprecision associated with a very wide CI.
5.2. Analysis.

Comparison 5: An aerobic exercise training programme compared to cognitive behavioural therapy (CBT) in people living with NMD, Outcome 2: Quality of life (SF‐36 Physical Component Score, questionnaire)
After seven months (three months after intervention): the MD was –1.70 points (95% CI –6.58 to 3.18; 1 study, 37 participants; low‐certainty evidence; Analysis 5.2) in favour of CBT but the CIs included the possibility of an effect favouring either CBT or the exercise programme (Table 5). We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition and selection bias, and once for imprecision associated with a wide CI.
After 10 months (six months after intervention): the MD was –0.30 points (95% CI –4.88 to 4.28; 1 study, 38 participants; very low‐certainty evidence; Analysis 5.2) in favour of CBT but the CIs included the possibility of an effect favouring either CBT or the exercise programme (Table 5). We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition and selection bias, and twice for imprecision associated with a very wide CI.
Quality of life (36‐item Short Form Health Survey, Mental Component Score, questionnaire)
In Koopman 2016 after four months (recorded after intervention): the MD was 1.20 points (95% CI –3.90 to 6.30; 1 study, 40 participants; low‐certainty evidence; Analysis 5.3) in favour of CBT but the CIs included the possibility of an effect favouring either CBT or the exercise programme (Table 5).
5.3. Analysis.

Comparison 5: An aerobic exercise training programme compared to cognitive behavioural therapy (CBT) in people living with NMD, Outcome 3: Quality of life (SF‐36 Mental Component Score, questionnaire)
After seven months (three months after intervention): the MD was 3.20 points (95% CI –3.03 to 9.43; 1 study, 37 participants; low‐certainty evidence; Analysis 5.3) in favour of CBT but the CIs included the possibility of an effect favouring either CBT or the exercise programme (Table 5).
After 10 months (six months after intervention): the MD was 1.30 points (95% CI –6.34 to 8.94; 1 study, 38 participants; low‐certainty evidence; Analysis 5.3) in favour of CBT but the CIs included the possibility of an effect favouring either CBT or the exercise programme (Table 5).
We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition and selection bias, and once for imprecision associated with a wide CI.
Adverse events
Koopman 2016 reported results for the training group but there were no comparative data available between groups for any type of adverse event.
Serious adverse events
There were no comparative data on serious adverse events available between groups.
CBT compared to no CBT in people living with NMD
One RCT involving people with PPS contributed data for this comparison (Koopman 2016). We did not include physical activity outcomes in a summary of findings table because they did not match prespecified outcome measurements (Table 6).
3. CBT compared to no CBT in people living with NMD.
| CBT compared to no CBT | ||||||
|
Patient or population: people with NMD Setting: the Netherlands Intervention: CBT Comparison: no CBT | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with no CBT | Risk with CBT | |||||
| Time spent physically active | — | — | — | — | — | Outcome not measured. |
|
Quality of life (SF‐36 PCS) assessed with: final scores, after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 4 months |
The mean quality of life (SF‐36 PCS) was 33.6 points | MD 1.3 points higher (2.96 lower to 5.56 higher) | — | 41 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Quality of life (SF‐36 MCS) assessed with: final scores, after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 4 months |
The mean quality of life (SF‐36 MCS) was 52.5 points | MD 1.1 points higher (5.18 lower to 7.38 higher) | — | 41 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Quality of life (SF‐36 PCS) assessed with: final scores, after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 7 months |
The mean quality of life (SF‐36 PCS) was 33.2 points | MD 2.8 points higher (2.07 lower to 7.67 higher) | — | 41 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Quality of life (SF‐36 MCS) assessed with: final scores, after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 7 months |
The mean quality of life (SF‐36 MCS) was 51.7 points | MD 1.3 points higher (4.42 lower to 7.02 higher) | — | 41 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Quality of life (SF‐36 PCS) assessed with: final scores, after intervention (higher = better quality of life) Scale: 0–100 Follow‐up: 10 months |
The mean quality of life (SF‐36 PCS) was 34.5 points | MD 1.6 points higher (3.22 lower to 6.42 higher) | — | 40 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Quality of life (SF‐36 MCS) assessed with: final scores, after intervention(higher = better quality of life) Scale: 0–100 Follow‐up: 10 months |
The mean quality of life (SF‐36 MCS) was 52.4 points | MD 3.1 points lower (9.53 lower to 3.33 higher) | — | 40 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
| Adverse events/serious adverse events | — | — | — | — | — | No comparative data available between groups for any type of adverse event. |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MCS: Mental Component Score; MD: mean difference: NMD: neuromuscular disease; PCS: Physical Component Score; RCT: randomised controlled trial; SF‐36: 36‐item Short Form Health Survey. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| See interactive version of this table: gdt.gradepro.org/presentations/#/isof/isof_question_revman_web_422113426106228546. | ||||||
aDowngraded once for study limitations associated with a high risk of attrition and selection bias. bDowngraded once for imprecision associated with a wide CI.
Koopman 2016 reported using ITT analysis with no imputation of missing data, under the assumption that data were missing at random. In the ITT population, the median number of CBT sessions was seven (range zero to 12) although between 12 and 16 sessions were prespecified in the study protocol.
Daily steps (count, activity monitor)
In Koopman 2016 after four months (after intervention): the MD was –646 steps per day (95% CI –2683.25 to 1391.25; 1 study, 36 participants; Analysis 6.1) in favour of CBT but the CIs included the possibility of an effect favouring either CBT or the exercise programme.
6.1. Analysis.

Comparison 6: Cognitive behavioural therapy (CBT) compared to no CBT in people living with NMD, Outcome 1: Daily steps (count, activity monitor)
After seven months (three months after intervention): the MD was –107 steps per day (95% CI –1773.16 to 1559.16; 1 study, 39 participants, Analysis 6.1) in favour of CBT but the CI included the possibility of an effect favouring either CBT or the exercise programme.
After 10 months (six months after intervention): the MD was 68 steps per day (95% CI –1672.87 to 1808.87; 1 study, 33 participants; Analysis 6.1) in favour of the exercise programme but the CI included the possibility of an effect favouring either CBT or the exercise programme.
Quality of life (36‐item Short Form Health Survey, Physical Component Score, questionnaire)
In Koopman 2016 after four months (recorded after intervention): the MD was 1.30 points (95% CI –2.96 to 5.56; 1 study, 41 participants; low‐certainty evidence; Analysis 6.2) in favour of CBT but the CI included the possibility of an effect favouring either CBT or no CBT (Table 6).
6.2. Analysis.

Comparison 6: Cognitive behavioural therapy (CBT) compared to no CBT in people living with NMD, Outcome 2: Quality of life (SF‐36 Physical Component Score, questionnaire)
After seven months (three months after intervention): the MD was 2.80 points (95% CI –2.07 to 7.67; 1 study, 41 participants; low‐certainty evidence; Analysis 6.2) in favour of CBT but the CIs included the possibility of an effect favouring either CBT or no CBT (Table 6).
After 10 months (six months after intervention): the MD was 1.60 points (95% CI –3.22 to 6.42; 1 study, 40 participants; low‐certainty evidence; Analysis 6.2) in favour of CBT but the CIs included the possibility of an effect favouring either CBT or no CBT (Table 6).
We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition and selection bias, and once for imprecision associated with a wide CI.
Quality of life (36‐item Short Form Health Survey, Mental Component Score, questionnaire)
In Koopman 2016 after four months (recorded after intervention): the MD was 1.10 points (95% CI –5.18 to 7.38; 1 study, 41 participants; low‐certainty evidence; Analysis 6.3) in favour of CBT but the CIs included the possibility of an effect favouring either CBT or the exercise programme (Table 6).
6.3. Analysis.

Comparison 6: Cognitive behavioural therapy (CBT) compared to no CBT in people living with NMD, Outcome 3: Quality of life (SF‐36 Mental Component Score, questionnaire)
After seven months (three months after intervention): the MD was 1.30 points (95% CI –4.42 to 7.02; 1 study, 41 participants; low‐certainty evidence; Analysis 6.3) in favour of CBT but the CIs included the possibility of an effect favouring either CBT or the exercise programme (Table 6).
After 10 months (six months after intervention): the MD was –3.10 points (95% CI –9.53 to 3.33; 1 study, 40 participants; low‐certainty evidence; Analysis 6.3) in favour of CBT but the CIs included the possibility of an effect favouring either CBT or the exercise programme (Table 6).
We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition and selection bias, and once for imprecision associated with a wide CI.
Adverse events
Koopman 2016 reported results for the CBT group but there were no comparative data available between groups for any type of adverse event.
Serious adverse events
The study did not report serious adverse events.
CBT with or without an exercise programme compared to no CBT and no exercise programme in people living with NMD
One study involving people with DM1 contributed data for this comparison (Okkersen 2018). We did not include physical activity outcomes in a summary of findings table because they did not match prespecified outcome measurements (Table 7).
4. CBT with or without an exercise programme compared to no CBT and no exercise programme in people living with NMD.
| CBT with or without an exercise programme compared to no CBT and no exercise programme | ||||||
|
Patient or population: people with NMD Setting: Paris (France), Munich (Germany), Nijmegen (the Netherlands), and Newcastle (UK) Intervention: CBT with or without an exercise programme Comparison: no CBT and no exercise programme | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with no CBT and no exercise programme | Risk with CBT with or without an exercise programme | |||||
| Time spent physically active | — | — | — | — | — | Outcome not measured. |
|
NMD‐specific quality of life (INQoL) assessed with: final scores, during intervention (lower = better quality of life) Scale: 0–100 Follow‐up: 5 months |
The mean NMD‐specific quality of life (INQOL – quality of life domain, questionnaire) was 70.26 points | MD 1.05 points lower (10.44 lower to 8.34 higher) | — | 218 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
NMD‐specific quality of life (INQoL) assessed with: final scores, unclear if during or after intervention (lower = better quality of life) Scale: 0–100 Follow‐up: 10 months |
The mean NMD‐specific quality of life (INQoL) was 68.5 points | MD 1.67 points higher (7.64 lower to 10.98 higher) | — | 222 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
NMD‐specific quality of life (INQoL) assessed with: final scores, after intervention (lower = better quality of life) Scale: 0–100 Follow‐up: 16 months |
The mean NMD‐specific quality of life (INQoL) was 69.32 points | MD 2.71 points higher (7.07 lower to 12.49 higher) | — | 208 (1 RCT) | ⊕⊕⊝⊝ Lowa,b | — |
|
Adverse events Follow‐up: up to 14 days after the final study visit (16 months after baseline) |
496 per 1000 | 506 per 1000 (397 to 650) | RR 1.02 (0.80 to 1.31) | 255 (1 RCT) | ⊕⊝⊝⊝ Very lowb,c | — |
|
Serious adverse events Follow‐up: up to 14 days after the final study visit (16 months after baseline) |
118 per 1000 | 71 per 1000 (32 to 155) | RR 0.60 (0.27 to 1.31) | 255 (1 RCT) | ⊕⊝⊝⊝ Very lowb,c | — |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CBT: cognitive behavioural therapy; CI: confidence interval; INQoL: Individualized Neuromuscular Quality of Life; MD: mean difference; NMD: neuromuscular disease; RCT: randomised controlled trial; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| See interactive version of this table: gdt.gradepro.org/presentations/#/isof/isof_question_revman_web_422113914345496441. | ||||||
aDowngraded once for study limitations associated with a high risk of attrition bias. bDowngraded once for indirectness because graded exercise therapy was not offered as part of intervention at all sites (variation in the intervention across different settings). cDowngraded twice for imprecision associated with a very wide CI.
The study reported ITT analysis for the primary outcome analysis only (DM1‐Active‐c score). Other outcomes were reported using available‐case analysis. The mean number of CBT sessions completed was 10.7 (SD 3.3) of a maximum of 14 sessions. The mean number of face‐to‐face CBT sessions completed was 6.3 (SD 4.0). An activity module was indicated in all participants receiving CBT and provided to 112 people (94%). Forty‐two participants were referred to the optional exercise programme, of whom nine were non‐compliant due to lack of motivation or because they did not satisfy an aerobic exercise criterion. In total, 33/128 participants (26%) received the optional exercise programme, with two further withdrawals during the programme (one person was lost to follow‐up and the other stopped due to a malignancy).
Physical activity (interpreted as mean magnitude of ankle acceleration over 24 hours, activity monitor with Euclidian Norm Minus One metric)
After five months (during intervention): the MD was 2.08 unknown units (95% CI –1.00 to 5.16; 1 study, 154 participants; Analysis 7.1) in favour of CBT with/without an exercise programme but the CIs included the possibility of an effect favouring either CBT with/without an exercise programme or no CBT and no exercise programme.
7.1. Analysis.

Comparison 7: Cognitive behavioural therapy (CBT) with/without an exercise programme compared to no CBT and no exercise programme in people living with NMD, Outcome 1: Physical activity (unclear units – interpreted as mean magnitude of ankle acceleration over 24 hours, activity monitor with Euclidian Norm Minus One metric)
After 10 months (unclear if during or after intervention): the MD was 1.90 unknown units (95% CI –0.97 to 4.77; 1 study, 164 participants; Analysis 7.1) in favour of CBT with/without an exercise programme but the CIs included the possibility of an effect favouring either CBT with/without an exercise programme or no CBT and no exercise programme.
After 16 months (six months after intervention): the MD was 1.26 unknown units (95% CI –2.09 to 4.61; 1 study, 139 participants; Analysis 7.1) in favour of CBT with/without an exercise programme but the CIs included the possibility of an effect favouring either CBT with/without an exercise programme or no CBT and no exercise programme.
Physical activity (interpreted as mean magnitude of ankle acceleration over five hours of highest activity, activity monitor with Euclidian Norm Minus One metric)
After five months (during intervention): the MD was 7.15 unknown units (95% CI –1.72 to 16.02; 1 study, 154 participants; Analysis 7.2) in favour of CBT with/without an exercise programme but the CIs included the possibility of an effect favouring either CBT with/without an exercise programme or no CBT and no exercise programme.
7.2. Analysis.

Comparison 7: Cognitive behavioural therapy (CBT) with/without an exercise programme compared to no CBT and no exercise programme in people living with NMD, Outcome 2: Physical activity (unclear units – interpreted as mean magnitude of ankle acceleration over 5 hours of highest activity, activity monitor with Euclidian Norm Minus One metric)
After 10 months (unclear if during or after intervention): the MD was 6.39 unknown units (95% CI –2.01 to 14.79; 1 study, 164 participants; Analysis 7.2) in favour of CBT with/without an exercise programme but the CIs included the possibility of an effect favouring either CBT with/without an exercise programme or no CBT and no exercise programme.
After 16 months (six months after intervention): the MD was 3.21 unknown units (95% CI –6.34 to 12.76; 1 study, 139 participants; Analysis 7.2) in favour of CBT with/without an exercise programme but the CIs included the possibility of an effect favouring either CBT with/without an exercise programme or no CBT and no exercise programme.
Physical activity (interpreted as average magnitude of ankle acceleration over five hours of lowest activity, activity monitor with Euclidian Norm Minus One metric)
After five months (during intervention): the MD was –0.02 unknown units (95% CI –0.36 to 0.32; 1 study, 154 participants; Analysis 7.3) in favour of no CBT and no exercise programme but the CIs included the possibility of an effect favouring either CBT with/without an exercise programme or no CBT and no exercise programme.
7.3. Analysis.

Comparison 7: Cognitive behavioural therapy (CBT) with/without an exercise programme compared to no CBT and no exercise programme in people living with NMD, Outcome 3: Physical activity (unclear units – interpreted as mean magnitude of ankle acceleration over 5 hours of lowest activity, activity monitor with Euclidian Norm Minus One metric)
After 10 months (unclear if during or after intervention): the MD was 0.08 unknown units (95% CI –0.14 to 0.30; 1 study, 164 participants; Analysis 7.3) in favour of CBT with/without an exercise programme but the CIs included the possibility of an effect favouring either CBT with/without an exercise programme or no CBT and no exercise programme.
After 16 months (six months after intervention): the MD was 0.07 unknown units (95% CI –0.15 to 0.29; 1 study, 139 participants; Analysis 7.3) in favour of CBT with/without an exercise programme but the CIs included the possibility of an effect favouring either CBT with/without an exercise programme or no CBT and no exercise programme.
NMD‐specific quality of life (Individualized Neuromuscular Quality of life, INQoL)
After five months (during intervention): the MD was –1.05 points (95% CI –10.44 to 8.34; 1 study, 218 participants; low‐certainty evidence; Analysis 7.4) in favour of CBT with/without an exercise programme but the CIs included the possibility of an effect favouring either CBT with/without an exercise programme or no CBT and no exercise programme (Table 7).
7.4. Analysis.

Comparison 7: Cognitive behavioural therapy (CBT) with/without an exercise programme compared to no CBT and no exercise programme in people living with NMD, Outcome 4: NMD‐specific quality of life (INQoL)
After 10 months (unclear if during or after intervention): the MD was 1.67 points (95% CI –7.64 to 10.98; 1 study, 222 participants; low‐certainty evidence; Analysis 7.4) in favour of no CBT and no exercise programme but the CIs included the possibility of an effect favouring either CBT with/without an exercise programme or no CBT and no exercise programme (Table 7).
After 16 months (six months after intervention): the MD was 2.71 points (95% CI –7.07 to 12.49; 1 study, 208 participants; low‐certainty evidence; Analysis 7.4) in favour of no CBT and no exercise programme but the CIs included the possibility of an effect favouring either CBT with/without an exercise programme or no CBT and no exercise programme (Table 7).
We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition bias, and once for indirectness because graded exercise therapy was not offered as part of intervention at all sites (variation in the intervention across different sites).
Adverse events
Up to 14 days after the final assessment at 16 months: the RR was 1.02 (95% CI 0.80 to 1.31; 1 study, 255 participants; very low‐certainty evidence; Analysis 7.5) in favour of no CBT and no exercise programme but the CIs included the possibility of an effect favouring either CBT with/without an exercise programme or no CBT and no exercise programme (Table 7). We downgraded the certainty of the evidence once for indirectness because graded exercise therapy was not offered as part of intervention at all sites (variation in the intervention across different sites), and twice for imprecision associated with a very wide CI.
7.5. Analysis.

Comparison 7: Cognitive behavioural therapy (CBT) with/without an exercise programme compared to no CBT and no exercise programme in people living with NMD, Outcome 5: Adverse events
Serious adverse events
Up to 14 days after the final assessment at 16 months: the RR was 0.60 (95% CI 0.27 to 1.31; 1 study, 255 participants; very low‐certainty evidence; Analysis 7.6) in favour of CBT with/without an exercise programme but the CIs included the possibility of an effect favouring either CBT with/without an exercise programme or no CBT and no exercise programme (Table 7). We downgraded the certainty of the evidence once for indirectness because graded exercise therapy was not offered as part of intervention at all sites (variation in the intervention across different sites), and twice for imprecision associated with a very wide CI.
7.6. Analysis.

Comparison 7: Cognitive behavioural therapy (CBT) with/without an exercise programme compared to no CBT and no exercise programme in people living with NMD, Outcome 6: Serious adverse events
A functional exercise programme compared to a stretching exercise programme in people living with NMD
One RCT involving people with SBMA contributed data for this comparison (Shrader 2015). We included physical activity outcomes in a summary of findings table although the unit of measurement was unconfirmed. It is anticipated that the Actical accelerometer measured the physical activity count as a time‐based outcome.
If participants did not meet a minimal level of compliance, they would have been excluded from the study analysis (see Characteristics of included studies table). However, overall intervention compliance was reported as 88.8% with only one dropout due to non‐compliance (from the functional exercise programme). ITT analysis was not reported. The amount of missing data varied across different time outcome measures, suggesting available‐case analysis.
Physical activity (unspecified count per day, activity monitor)
After 12 weeks (during intervention): the MD was –8701 unconfirmed units (95% CI –38,293.30 to 20,891.30; 1 study, 43 participants; low‐certainty evidence; Analysis 8.1) in favour of the stretching exercise programme but the CIs included the possibility of an effect favouring either the stretching or functional exercise programme (Table 3). We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition and selection bias, and once for imprecision associated with a wide CI.
8.1. Analysis.

Comparison 8: A functional exercise programme compared to a stretching exercise programme in people living with NMD, Outcome 1: Physical activity (unspecified count per day, activity monitor)
Quality of life (36‐item Short Form Health Survey, Physical Component Score, questionnaire)
After 12 weeks (unclear if during or after intervention): the MD was –1.10 points (95% CI –5.22 to 3.02; 1 study, 49 participants; low‐certainty evidence; Analysis 8.2) in favour of the stretching exercise programme but the CIs included the possibility of an effect favouring either the stretching or functional exercise programme (Table 3). We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition and selection bias, and once for imprecision associated with a wide CI.
8.2. Analysis.

Comparison 8: A functional exercise programme compared to a stretching exercise programme in people living with NMD, Outcome 2: Quality of life (SF‐36 Physical Component Score, questionnaire)
Quality of life (36‐item Short Form Health Survey, Mental Component Score, questionnaire)
After 12 weeks (unclear if during or after intervention): the MD was –1.10 points (95% CI –6.79 to 4.59; 1 study, 49 participants; low‐certainty evidence; Analysis 8.3) in favour of the stretching exercise programme but the CIs included the possibility of an effect favouring either the stretching or functional exercise programme (Table 3). We downgraded the certainty of the evidence once for study limitations associated with a high risk of attrition and selection bias, and once for imprecision associated with a wide CI.
8.3. Analysis.

Comparison 8: A functional exercise programme compared to a stretching exercise programme in people living with NMD, Outcome 3: Quality of life (SF‐36 Mental Component Score, questionnaire)
In the literature, we identified small (0.2 SD; 2.21), moderate (0.5 SD; 5.53) and large (0.8 SD; 8.85) distribution‐based MIDs that corresponded to the overall SF‐36 quality of life in people with NMDs before and after exercise intervention (Stefanetti 2020). However, we did not find an MID for the MD between interventions. Based on the effect estimates and low‐certainty evidence, we found that the functional exercise programme may have made little or no difference to PCS and MCS for quality of life when compared to the stretching exercise programme.
Quality of life (36‐item Short Form Health Survey, Vitality Component Score, questionnaire)
After 12 weeks (unclear if during or after intervention): the MD was –1.90 points (95% CI –13.14 to 9.34; 1 study, 49 participants; Analysis 8.4) in favour of the stretching exercise programme but the CIs included the possibility of an effect favouring either the stretching or functional exercise programme. We did not include this outcome in the summary of findings table as Vitality is one of eight Component Scores in the SF‐36 questionnaire.
8.4. Analysis.

Comparison 8: A functional exercise programme compared to a stretching exercise programme in people living with NMD, Outcome 4: Quality of life (SF‐36 Vitality Component Score, questionnaire)
Adverse events
The study did not report usable adverse event data.
Serious adverse events
The study did not report serious adverse event data.
We sought additional unpublished data relating to published outcome measures in three included RCTs, in accordance with the review protocol. In one study, we sought unpublished data on a subpopulation of 26 participants with motor neuron disease and other NMDs (Elsworth 2011). However, it was difficult to ascertain intervention allocation and so we did not analyse these data quantitatively. For Wallace 2019, we sought the first‐period data from the cross‐over trial but these were not available for the relevant published outcomes at the time of review development because the data had been analysed across both periods only. We did not analyse the combined first‐ and second‐period data quantitatively in this review, as per the protocol. We sought additional information in relation to one other study that had not been published as a full report, but it was not available at the time of preparing this review (White 2016).
Discussion
Summary of main results
Our review included 13 studies (795 randomised adults from 12 studies; number of participants unclear in one study). We did not perform meta‐analysis for any comparison because of differences in interventions and usual care. We also found considerable variation in how studies reported physical activity as an outcome measure. Six of the 13 included studies did not report results for physical activity outcomes, or the data were not usable in this review. The studies that reported physical activity measurement did not always clearly report ITT analysis or whether final assessments occurred during or after the completion of intervention. Based on prespecified measures, we included three comparisons in our summary of findings tables.
Two distinct studies of adults with DPN reported time spent physically active as time spent walking. One comparison of a physical activity programme (weight‐bearing) with no physical activity programme reported weekly duration of walking during and at the end of a one‐year intervention using a StepWatch ankle accelerometer. Based on the point estimate, intervention may have led to an important increase in physical activity per week; however, the 95% CI included the possibility of no difference or an effect in either direction at three months, six months, and 12 months. We assessed the evidence at low certainty. Another comparison of a brief, sensor‐based interactive exercise programme with no sensor‐based, interactive exercise programme reported duration of walking over 48 hours at the end of four weeks intervention using a t‐shirt embedded sensor. It was not possible to draw conclusions about the effectiveness of intervention based on the very low‐certainty evidence. It is unclear what minimal level of physical movement constituted objectively measured physical activity using an ankle and t‐shirt‐embedded accelerometer in these comparisons. Though an SMD could be calculated, we did not undertake such meta‐analysis for time spent physically active due to the variation between studies and low likelihood that statistical combination of these results would improve precision in a clinically meaningful way.
One study of adults with SBMA reported time spent physically active as a daily physical activity count. The comparison of a functional exercise programme with a stretching exercise programme involved measuring physical activity counts using an Actical accelerometer at the end of 12 weeks' intervention. It was not possible to draw conclusions about the effectiveness of the intervention (requiring compliance) from the low‐certainty evidence and unconfirmed measurement units.
The two exercise studies with prespecified measures of physical activity also reported on participants' quality of life. In one study, we found low‐certainty evidence that the sensor‐based interactive exercise programme may have made little or no difference to the MCS for quality of life when compared to no sensor‐based interactive exercise programme. However, we were unable to draw conclusions about the impact of intervention on the PCS for quality of life based on very low‐certainty evidence. In another study, we found that the functional exercise programme may have made little or no difference to the MCS or PCS for quality of life when compared to the stretching exercise programme, based on low‐certainty evidence. It is unclear whether the recording or recall period, or both, was during or after the intervention for final assessment of quality of life.
Although studies reported adverse events incompletely, we found no evidence of supported activity increasing the risk of serious adverse events or adverse events leading to study discontinuation. For the comparison of a physical activity programme (weight‐bearing) with no physical activity programme, one study specifically reported effect estimates for foot lesions and full‐thickness ulcers; this evidence included the possibility of no difference or a higher or lower risk with intervention.
Overall completeness and applicability of evidence
According to the WHO, physical inactivity is one of the main risk factors for noncommunicable disease mortality (WHO 2020b). For apparently healthy populations, increasing and maintaining regular physical activity is understood to be beneficial in terms of reducing all‐cause mortality risk, as well as for the primary and secondary prevention of chronic diseases, such as cardiovascular disease, diabetes mellitus, colon and breast cancer, osteoporosis, and depression, and risk factors such as hypertension and obesity. At a mechanistic level, routine physical activity has been associated with enhanced mental well‐being, reduced blood pressure, and improvement in glucose control and other biomarkers for inflammation and cardiovascular disease risk (Warburton 2006). By reducing the risk of type 2 diabetes, fewer people would be expected to develop peripheral neuropathy as a secondary complication, emphasising the need for effective prevention strategies.
Observational studies have shown that people with particular types of NMD are less physically active than apparently healthy controls, and have higher perceived barriers to becoming physically active (Aitkens 2005; Apabhai 2011; Heutinck 2017; McCrory 1998; Phillips 2009; Ramdharry 2017). This evidence further emphasises the need for effective strategies for physical activity participation in people living with NMD, in addition to prevention of secondary chronic diseases and complications.
In addressing the review question, we found fundamental evidence gaps for physical activity promotion among people living with NMD. Most included studies randomised only a minority of invited participants, which might suggest a broad recruitment strategy or strict inclusion criteria. However, the effectiveness of physical activity promotion could be affected by the initial study promotion and skewed by a low recruitment rate. Included studies involved people with nine of several hundred recognised types of NMD associated with varying severities of disease, disability, and impact on life expectancy. We also found some differences in the classification of NMDs. For example, one included study reported motor neuron disease separately from NMD, and other studies in the wider literature excluded DPN, unlike in this review. Four studies reported major comorbidities in some participants, which may have precluded their participation in other clinical trials. The restriction of this review to studies of people with NMD or neurological disorders including NMD, meant that we had a less heterogeneous review population than the general population but excluded evidence from other potentially relevant community interventions. Other Cochrane Reviews have aimed to address broader public health interventions for promoting physical activity but may not include people living with medical conditions such as NMD. Only one study in this review involved participants with different types of neurological disorders of whom a subgroup had NMD. We did not attempt to analyse the few data (unpublished) from this subgroup. If sufficient data had been available, the absence of stratification by condition may still have limited the usability or applicability of the evidence. All other included studies compared interventions in people with a specific NMD. The evidence related to adults in studies conducted over 2011 to 2019, largely facilitated through specialist healthcare settings in Western Europe. Twelve studies excluded children and adolescents and one study did not specify eligibility by age, although participants were aged over 60 years on average. The absence of evidence in children and adolescents, as well as in non‐ambulant people of any age, perhaps reflects a more general lack of clinical trials in these populations (Joseph 2015).
Also fundamental to the review question, we have shown how little research to date has addressed the effectiveness of promotional strategies for physical activity in people with NMD, as distinct from assessing the effects of exercise and compliance. As such, we have detailed promotional aspects of included RCTs in the study tables and main results of this review. We found that all included interventions and comparators related to the clinical care of people living with NMD. However, usual care varied across different conditions and clinical settings, for example, in national recommendations for physical therapy. We also found differences in study eligibility criteria in relation to baseline measures of physical activity. While all the studies intended to measure physical activity as an outcome, only one study clearly reported the aim of intervention being to promote physical activity. The main focus of 12 studies was to determine the effects of intervention on other aspects of health, fitness, and well‐being, such as fatigue, peak exercise capacity, or quality of life. We decided against meta‐analysis of any comparison, in part due to the different combinations of physical activity support and differences in usual care depending on the condition and setting.
We found that the studies reviewed tended to report physical activity as a secondary or exploratory outcome. We also found considerable variation in the way that physical activity was reported as an outcome measure. In the review, we applied a hierarchy of physical activity outcome measures for data extraction as per the protocol. We decided not to prioritise a specific time point because of the potential significance of different time points for different study populations, interventions, and comparators. Where specified, we also found variation in the timing of outcome measurement during or after intervention. We prioritised the reporting of measures of physical activity duration so that results could include participants irrespective of ambulatory status. However, nine studies included only ambulant participants and the other four studies did not specify baseline ambulatory status of participants but included ambulatory outcome measures. The number of daily steps taken was the most commonly reported measure of physical activity in included studies. This perhaps demonstrates the challenge of identifying a single primary outcome measure for physical activity across the spectrum of disability expected in NMD, including people who may use upper extremity physical activity to mobilise with assistive devices and wheelchairs.
In this review, we limited physical activity outcomes to self‐reported and objectively measured everyday physical activity as per the protocol. Assessment of the effects of interventions on performance measures such as timed walking distance and exercise capacity are addressed in other Cochrane Reviews. However, we still found considerable variation in the reporting of objectively measured physical activity outcomes and a lack of self‐reported physical activity outcomes. We did not attempt to meta‐analyse these measures as an overarching physical activity domain. Typically, studies each reported a single measure of physical activity, although accelerometers can collect data on multiple parameters (e.g. step count, energy expenditure, and duration of different intensities of physical activity). As a result, the chance of finding a statistically significant change may increase and there could be a risk of selective reporting if the chosen parameter is not prespecified in a protocol. To minimise the risk of selective reporting in the review process, we avoided prioritisation of shorter‐length follow‐up for outcomes reported at multiple time points. As highlighted above, we reported multiple time points for outcomes (as per the studies) in the absence of a single, appropriate standard for outcome reporting in people with different types of NMD. We also reported mental and physical component summary scores for quality of life (as per the studies) to help capture the impact of physical and communication‐based approaches to physical activity promotion. In our interpretation of the evidence, we did not identify or apply any anchor‐based MIDs for quality of life outcomes in people with NMD. We considered statistical, distribution‐based MIDs for overall quality of life before and after exercise interventions but these did not provide a MID for the MD between interventions (Stefanetti 2020). We also did not find any established MID for adverse events or physical activity outcomes within the review population. Most included studies reported adverse events incompletely and we found some differences in study exclusion criteria that may have affected the data for adverse events and other outcomes. For example, two studies monitored foot ulcers in participants with DPN (Lemaster 2008; Mueller 2013), whereas another study excluded people with active foot ulcers (Grewal 2015). In terms of time spent physically active, WHO guidance emphasises at least meeting recommended amounts of physical activity (WHO 2020a; WHO 2020b). As such, we interpreted the evidence on the premise that any increase in time spent physically active is considered important. More emphasis on qualitative and dichotomous change in self‐reported overall physical activity of people with NMD in future interventional studies might offer a pragmatic approach to capturing the multiple dimensions of physical activity participation as well as important change at an individual and population level.
Quality of the evidence
We assessed most included studies at high risk of bias due to incomplete outcome data. Missing data on physical activity outcomes was a particular concern. Studies highlighted technical problems with data retrieval from activity monitors and incomplete questionnaires. Although several studies reported an ITT analysis, the assumptions with this approach were not reported fully, which made it unclear how missing data were handled.
We are uncertain about whether the interventions promoted physical activity in people with NMD in terms of time spent physically active. We are also uncertain whether there was a benefit or harm of any intervention over another intervention or over usual care in terms of quality of life and adverse events. We assessed the certainty of the evidence as low to very low due to study limitations and because the results were imprecise or the comparison did not directly address the review question.
Potential biases in the review process
We conducted a thorough search for published RCTs and sought additional unpublished data in accordance with the review protocol. However, it is possible that further interventions for physical activity promotion may have been identified through searching other databases, such as CINAHL and AMED. Based on the completed search, we anticipate that we could have missed studies if the abstract did not explicitly state an aim to promote physical activity or omitted physical activity outcomes. Several studies reported pain or fatigue outcomes but we did not report these as adverse events unless studies reported them in this way despite our narrative reporting of foot lesions. In addition, we did not consider qualitative evidence in this review. However, one included study undertook interviews during and after intervention with a subset of participants (Wallace 2019). Another included study surveyed participants after intervention to understand better their perspective on the value of the exercise programme and their current exercise and skin‐monitoring habits (Mueller 2013).
Review authorship did not include people living with NMD although all review authors have clinical research experience of working with people who have neuromuscular conditions. Four review authors (JN, GG, KJ, and GR) had varying levels of involvement as personnel in one of two included RCTs in this review (Okkersen 2018; Wallace 2019), which might potentially bias the review process. Two review authors with study involvement (KJ and JN) contributed to the initial screening of full reports for inclusion, following the eligibility criteria previously published in the review protocol. We tried to minimise further potential biases in the review process through dual independent data extraction and dual independent risk of bias assessment by review authors not involved in the studies where possible. Due to logistical constraints, the first review author (KJ) contributed to data extraction and risk of bias assessment for one study, despite involvement. In addition, the first review author (KJ) and another review author (JN, FH, or GR) not involved in any included studies undertook GRADE assessments.
Agreements and disagreements with other studies or reviews
Physical activity interventions have been widely investigated at a community level and in subpopulations living with certain health conditions. However, we found limited reporting on physical activity promotion in RCTs of people with NMD. Other types of non‐randomised trial design may be more pragmatic for longer‐term follow up of outcomes such as all‐cause mortality risk and the primary and secondary prevention of other chronic diseases.
Through the review process, we identified some challenges in defining and communicating 'promotion' as potentially distinct from 'increasing', 'supporting', or 'encouraging' physical activity alone. We observed that our search results appeared to focus more on 'exercise' over 'physical activity' and 'compliance' or 'adherence' over the acceptability of intervention to participants. Although we did not search for qualitative evidence in this review, we identified qualitative methods such as the evaluation of motivational interviewing that might help to better understand the influence on physical activity promotion of communication between study participants and those involved in study delivery and usual care (NCT03515356).
In 2005, one Cochrane Review focussed on a population that was sedentary but "free from pre‐existing medical condition or with no more than 10% of subjects with pre‐existing medical conditions that may limit participation in physical activity" (Foster 2005). Given these exclusions, the evidence is less directly applicable to people living with NMD and a broader group of people with chronic conditions, who may benefit from physical activity intervention. The review included no evidence for objectively measured physical activity. The review authors meta‐analysed 19 studies of self‐reported physical activity, measured as a continuous variable in a variety of ways (e.g. weekly energy expended, scoring on the PASE, and total hours of physical activity per week). These outcome measures might be considered too different to meta‐analyse, highlighting a lack of consistency in the way that physical activity is measured, reported, and analysed as an outcome. However, the authors found a short‐ to medium‐term positive effect of physical activity interventions in terms of an SMD in self‐reported physical activity. The review authors also meta‐analysed 10 studies of self‐reported physical activity measured as a dichotomous outcome; this evidence indicated moderate statistical heterogeneity. Combined with marked variation in the components of interventions and in the personnel supporting them, we found that it remains difficult to apply conclusions from a broader population that involves more participants. As noted by the review authors, translation of the evidence into practice is further complicated by a potential difference in the motivation of people who participate in research studies compared with those who do not.
Also published in 2005, another Cochrane Review examined physical activity interventions by setting (home or centre‐based) (Ashworth 2005). Focusing on an older adult population with certain medical conditions or risk factors, the review authors decided not to meta‐analyse the available evidence due to the heterogeneity of the studies. The primary outcome for this review was functional ability but secondary outcomes included measures of long‐term maintenance of physical activity. We also chose not to meta‐analyse physical activity outcomes on the basis of heterogeneity between studies.
In 2013, several Cochrane Reviews investigated different methods of delivery for promoting physical activity, including face‐to‐face, web‐based, and remote interventions in apparently healthy study populations. When comparing face‐to‐face interventions with placebo or minimal intervention, review authors meta‐analysed self‐reported physical activity as a dichotomous and continuous outcome (Richards 2013a). The review authors cautioned that limited conclusions could be drawn about the effectiveness of components of interventions due to clinical and statistical heterogeneity despite some evidence in favour of face‐to‐face interventions. Similarly, caution was also advised when review authors compared remote and web 2.0 interventions with a placebo or minimal intervention for physical activity promotion although there was some evidence in favour of the use of technologies with support from a trained professional (Foster 2013). When face‐to‐face interventions were compared with remote and web 2.0 interventions for promoting physical activity, only one study met eligibility criteria and measured cardiorespiratory fitness, but included no measure of physical activity (Richards 2013b).
As we found in this review, most studies in other Cochrane Reviews of interventions for promoting physical activity have focused on adults. However, in 2013, one Cochrane Review assessed the effects of school‐based programmes for promoting physical activity and fitness in children and adolescents (Dobbins 2015). Review authors reported physical activity outcomes as dichotomous and continuous measures. As in this review, the duration of physical activity was a primary outcome either measured objectively or by self‐report. The proportion of participants engaging in moderate‐to‐vigorous physical activity was another primary outcome, again measured objectively or by self‐report. Also similar to this review, the authors decided not to meta‐analyse the available physical activity outcomes on the basis of variations in populations, interventions, and outcomes. The review authors emphasised caution in the interpretation of generally small effects supported by low‐certainty evidence.
A later Cochrane Review investigated community‐wide, multi‐component interventions for physical activity promotion (Baker 2015). Eligible study populations "must have been free living and not part of any institutionalised community, such as those who were mentally ill, the frail or bedridden elderly population, or those incarcerated in prison." Dichotomous and continuous measures of combined physical activity outcomes were reported narratively. The review authors reported that they did not conduct a meta‐analysis due to the heterogeneity in the populations and study designs. They assessed certainty of the evidence for combined physical activity outcomes as ranging from high to low. More recently, one Cochrane Review of workplace populations compared a pedometer intervention with minimal intervention and concluded that exercise can have a positive effect but authors did not perform meta‐analysis because of very high statistical heterogeneity (Freak‐Poli 2020). For comparisons with minimal and alternative physical activity interventions, the authors judged the certainty of the evidence for combined physical activity outcomes to be very low.
Several Cochrane Reviews have assessed the effects of exercise as a form of physical activity in people living with specific types of NMD. Among these reviews, two included the secondary outcome measurement of physical activity, although no data were available at that time (Bartels 2019; Quinlivan 2011). Quality of life appears to be more commonly reported than physical activity outcomes in reviews of RCTs that have involved physical activity. The reason for this might be that quality of life assessment has more standardised methods, such as the SF‐36. Quality of life is also used to determine quality‐adjusted life years, which can inform economic evaluations in healthcare decision‐making (along with measures of disability for determining disability‐adjusted life years). Use of published checklists and guidance has been proposed elsewhere to standardise assessment and reporting (Jimenez‐Moreno 2017; Slade 2016; Stoyanov 2015; The EQUATOR Network). In this review, quality of life was measured using disease‐specific and general population questionnaires. Uncertainty about whether the timing of the assessment period was during or after intervention complicated interpretation of changes in quality of life. For example, the recall period might be one week or four weeks, which could relate to the intervention period, the period when intervention stopped, or both. One review of psychosocial interventions designed to improve the quality of life and well‐being of people living with NMD found that most included studies reported a short‐term benefit of intervention but advised caution in the interpretation of the evidence because of widespread study limitations (Walklet 2016). For adverse event reporting, we found that studies in this review sometimes monitored the intervention arm only. However, in Okkersen 2018, we found very low‐certainty evidence that the intervention might reduce the risk of serious adverse events when compared with no intervention, which could carry implications for further research. It is unclear whether this finding, if confirmed, relates to closer monitoring alone or specific components of the intervention. Nevertheless, a reduction in all‐cause serious adverse events with intervention would be consistent with general population studies that support increased physical activity for reducing all‐cause mortality risk and the primary or secondary prevention of chronic diseases (Warburton 2006). In our review, one study undertook qualitative interviews of a subset of participants who identified that study personnel had helped to facilitate greater participation, but financial cost was a barrier to some people continuing exercise beyond the study (Wallace 2019). Another study surveyed participants after intervention and found that less than half of respondents continued to exercise three to seven days per week after approximately 15 months, despite the majority reporting that the exercise programme had been beneficial to them (Mueller 2013).
We excluded many studies involving physical activity that did not report physical activity outcomes. Of particular note, we excluded one study that reported social activity engagement but not physical activity (Veenhuizen 2019). One study awaiting classification assessed the effects of peer support on physical activity among adults with DPN (ChiCTR‐IPR‐15006127). Another study awaiting classification focused on physical activity among people who have muscular dystrophy and use wheelchairs (NCT00866112). In contrast, the studies in the current review focused on adults who were able to walk at study entry. However, Nary 2011 identified recruitment challenges due to strict eligibility criteria and a rare disease population, which may also be relevant to studies with low uptake in this review. While included studies largely focused on supported exercise, physical activity, and CBT, the ongoing studies we identified (mostly in DPN) investigate the use of insoles, aids, and devices, as well as supported exercise, and physical activity.
Authors' conclusions
Implications for practice.
Physical inactivity is associated with an increased risk of many major noncommunicable diseases in the general population. However, we remain unclear about the effectiveness of physical activity‐promoting intervention specifically in people with neuromuscular disease (NMD). This review also highlights important variation in usual care, such as physical therapy provision, for people living with NMD. Most studies reported adverse events incompletely. However, we found no evidence of supported activity increasing the risk of serious adverse events or adverse events leading to study discontinuation.
Implications for research.
The findings from our review and other reviews highlight particular challenges in addressing potentially conflicting intentions of inclusiveness and of minimising heterogeneity in the evaluation of interventions designed to promote physical activity; the inevitable question being 'whose' physical activity is being promoted? While larger randomised controlled trials (RCTs) might be one approach to tackling these challenges, our findings also raise questions about the way physical activity is measured, reported, and analysed, irrespective of sample size. The inclusion of people with NMD in broader public health interventions could potentially support more inclusive trials. However, there is also a further question of whether or not interventions that 'promote' physical activity are synonymous with interventions that motivate individual choice to participate in physical activity, and whether this matters to study participants and non‐participants. For example, some people living with NMD may find they do not have an option to be more active outside of a research setting if they do not have access to physical, psychological, social, or financial support. In terms of non‐health‐related incentives for participating in research, one included study paid a cash incentive for participation and several studies reported payment of travel expenses and gym membership. This financial cost might need to be weighed up against potential costs associated with the treatment of chronic diseases and complications attributed in part to physical inactivity. However, it is unclear to what extent intervention affected financial as opposed to physical, psychological, or social barriers to participants' physical activity and well‐being. Qualitative research could help to further explore these potential barriers to physical activity within participants who complete research interventions and those non‐participants lost at recruitment or during intervention.
Across different study populations, we anticipate that further technological changes in the way everyday physical activity is monitored through devices could play an increasing role in future studies of interventions for promoting physical activity. In this review, we found a lack of evidence relating to children, adolescents, and non‐ambulant people of any age. While there may be no single objective measure of physical activity, the study of qualitative and dichotomous change in self‐reported overall physical activity might offer a pragmatic approach to capturing important changes at an individual and population level. For evaluating promotional strategies, more complete reporting of outcomes is needed, including analysis of the intention‐to‐treat effect. Assessment of the potential for reducing all‐cause mortality risk, complications associated with NMD, and the primary and secondary prevention of other chronic diseases could also help us to better understand the value of interventions that promote physical activity in people living with NMD.
What's new
| Date | Event | Description |
|---|---|---|
| 15 July 2021 | Amended | Corrected typographical error in Sources of support |
History
Protocol first published: Issue 3, 2020 Review first published: Issue 5, 2021
| Date | Event | Description |
|---|---|---|
| 18 June 2021 | Amended | Edits to affiliation, Acknowledgements, and Sources of support |
Acknowledgements
The Cochrane Neuromuscular Information Specialists, Angela Gunn and Farhad Shokraneh, developed the search strategy in consultation with review authors, and ran the search.
Cochrane Neuromuscular and a panel of peer reviewers that included Dr Nicoline Voet, Radboud University Medical Centre, The Netherlands, and Associate Professor Shree Pandya, University of Rochester, USA provided peer review. The Cochrane Mental Health and Neuroscience Network Associate Editor, Dr Nuala Livingstone provided screening.
The 'Methods' section of this review was based on a template developed by Cochrane Neuromuscular from an original created by the Cochrane Airways Group.
This project was supported by the National Institute for Health Research (NIHR), via Cochrane Infrastructure funding to Cochrane Neuromuscular. The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service, or the Department of Health. Cochrane Neuromuscular is also supported by the Queen Square Centre for Neuromuscular Disease.
The UK NIHR Biomedical Research Centre (BRC) for Ageing and Age‐related Disease is a partnership between Newcastle Hospitals NHS Foundation Trust and Newcastle University, funded by the NIHR. JN, GG and DMT are supported by the NIHR Newcastle BRC. The NIHR University College London Hospitals BRC is a partnership between University College London Hospitals NHS Foundation Trust and University College London, funded by the NIHR. GR is supported by the NIHR University College London Hospitals BRC. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Appendices
Appendix 1. Cochrane Neuromuscular Specialised Register (CRSWeb) search strategy
1 MESH DESCRIPTOR Neuromuscular Diseases AND INREGISTER 46
2 MESH DESCRIPTOR Muscular Atrophy AND INREGISTER 57
3 MESH DESCRIPTOR Muscular Dystrophies EXPLODE ALL AND INREGISTER 188
4 MESH DESCRIPTOR Myositis AND INREGISTER 19
5 MESH DESCRIPTOR Myotonia AND INREGISTER 8
6 (myastheni* or (lambert and eaton and syndrome*)):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 168
7 MESH DESCRIPTOR Peripheral Nervous System Diseases AND INREGISTER 264
8 MESH DESCRIPTOR Polyneuropathies EXPLODE ALL AND INREGISTER 221
9 MESH DESCRIPTOR Peripheral Nerves AND INREGISTER 64
10 MESH DESCRIPTOR Neuritis AND INREGISTER 26
11 MESH DESCRIPTOR Neuromuscular Junction Diseases AND INREGISTER 0
12 MESH DESCRIPTOR Motor Neuron Disease EXPLODE ALL AND INREGISTER 334
13 MeSH DESCRIPTOR Motor Neuron Disease Explode All AND INREGISTER 334
14 "motor neuron disease*" or "motor neurone disease*" AND INREGISTER 155
15 "motoneuron disease*" or "motoneurone disease*" AND INREGISTER 4
16 "motorneuron disease*" or "motorneurone disease*" AND INREGISTER 2
17 "charcot disease" AND INREGISTER 1
18 "amyotrophic lateral sclerosis" AND INREGISTER 565
19 als:ti or als:ab or mnd:ti or mnd:ab AND INREGISTER 526
20 MESH DESCRIPTOR Glycogen Storage Disease Type V AND INREGISTER 14
21 (McArdle* or "Glycogen Storage Disease Type V" or "Glycogen Storage Disease Type 5" or GSDV or "muscle phosphorylase" deficiency or myophosphorylase):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 30
22 MESH DESCRIPTOR Glycogen Phosphorylase, Muscle Form AND INREGISTER 1
23 ("Glycogen Phosphorylase" NEAR3 "Muscle Form"):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 1
24 MESH DESCRIPTOR Muscular Diseases EXPLODE ALL AND INREGISTER 765
25 ("muscle disease*" or "muscle disorder*" or "muscular disease*" or "muscular disorder*" or "neuromuscular disease*" or "neuromuscular disorder*" or myopath* or dystroph* or myotoni* or myositis):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 839
26 (myopathy or "muscle fibre" or "muscle fiber"):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 130
27 ("muscular dystroph*" or "muscular atrophy" or myositis or myotonia):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 559
28 ("peripheral neuropath*" or polyneuropath* or "peripheral nerve*"):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 1314
29 (neuritis or polyradiculopathy or polyradiculoneuropathy or polyradiculoneuritis or polyneuritis):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 222
30 ("neuromuscular junction" NEAR3 (disease or diseases or disorder or disorders)):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 3
31 MESH DESCRIPTOR paraproteinemias AND INREGISTER 9
32 MESH DESCRIPTOR alcoholism AND INREGISTER 7
33 MESH DESCRIPTOR Paraneoplastic Syndromes AND INREGISTER 1
34 MESH DESCRIPTOR Paraneoplastic Syndromes, Nervous System AND INREGISTER 0
35 MESH DESCRIPTOR Pain EXPLODE ALL AND INREGISTER 1125
36 (pain or painful or chemically or toxicity):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 2820
37 #31 OR #32 OR #33 OR #34 OR #35 OR #36 AND INREGISTER 2869
38 MESH DESCRIPTOR Peripheral Nervous System Diseases AND INREGISTER 264
39 (neuropath*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 2190
40 #38 OR #39 AND INREGISTER 2230
41 #37 AND #40 AND INREGISTER 1158
42 (demyelin*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 187
43 (Inflammatory NEAR2 (polyradiculoneuropath* or polyneuropath* or mononeuropath*)):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 141
44 #42 AND #43 AND INREGISTER 134
45 MESH DESCRIPTOR Polyradiculoneuropathy AND INREGISTER 54
46 (polyradiculoneuritis or (guillain NEAR2 barre)):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 136
47 MESH DESCRIPTOR Polyradiculoneuropathy, Chronic Inflammatory Demyelinating AND INREGISTER 32
48 ("chronic inflammatory demyelinating polyradiculoneuropathy"):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 77
49 (multifocal NEAR neuropath*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 28
50 (paraprot* NEAR neuropath*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 7
51 MESH DESCRIPTOR POEMS Syndrome AND INREGISTER 2
52 (poems NEAR2 syndrome):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 2
53 MESH DESCRIPTOR Amyloid Neuropathies EXPLODE ALL AND INREGISTER 10
54 (amyloid NEAR neuropath*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 18
55 MESH DESCRIPTOR Hereditary Sensory and Motor Neuropathy AND INREGISTER 8
56 MESH DESCRIPTOR Hereditary Sensory and Autonomic Neuropathies AND INREGISTER 2
57 (hereditary NEAR neuropath*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 63
58 (toxic NEAR neuropath*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 13
59 (("drug induced" or "chemically induced") NEAR neuropath*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 10
60 (alcohol* NEAR neuropath*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 10
61 (borrelia*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 47
62 (herpes NEAR zoster):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 374
63 (diabetic NEAR neuropath*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 1144
64 (vasculiti* NEAR neuropath*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 0
65 (Brachial NEAR neuritis):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 21
66 (neuralgic NEAR amyotroph*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 0
67 (radiation NEAR plexopath*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 4
68 MESH DESCRIPTOR Brachial Plexus Neuropathies EXPLODE ALL AND INREGISTER 28
69 ("cervical spondylotic radiculopath*"):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 7
70 (lumbosacral near radiculopath*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 15
71 (Bell* NEAR pals*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 136
72 MESH DESCRIPTOR Facial Paralysis AND INREGISTER 54
73 #72 AND pals*:AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 33
74 ("cranial nerve*" NEAR pals*):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 3
75 (trigeminal NEAR neuralgia):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 118
76 MESH DESCRIPTOR Peripheral Nervous System Neoplasms AND INREGISTER 2
77 MESH DESCRIPTOR Peripheral Nervous System Neoplasms EXPLODE ALL AND INREGISTER 13
78 MESH DESCRIPTOR Neuralgia AND INREGISTER 287
79 #78 and (herpes or herpetic):AB,EH,EMT,KW,KY,MH,TI AND INREGISTER 81
80 MESH DESCRIPTOR Neuritis AND INREGISTER 26
81 MESH DESCRIPTOR Brachial Plexus AND INREGISTER 22
82 #80 AND #81 AND INREGISTER 0
83 MESH DESCRIPTOR Peripheral Nervous System Diseases WITH QUALIFIER RH AND INREGISTER 1
84 #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #41 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 OR #50 OR #51 OR #52 OR #53 OR #54 OR #55 OR #56 OR #57 OR #58 OR #59 OR #60 OR #61 OR #62 OR #63 OR #64 OR #65 OR #66 OR #67 OR #68 OR #69 OR #70 OR #71 OR #73 OR #74 OR #75 OR #76 OR #77 OR #79 OR #82 OR #83 AND INREGISTER 5251
85 "circuit based exercise" AND INREGISTER 0
86 MESH DESCRIPTOR exercise therapy EXPLODE ALL AND INREGISTER 209
87 MESH DESCRIPTOR Physical Education and Training AND INREGISTER 3
88 MESH DESCRIPTOR Sports AND INREGISTER 2
89 MESH DESCRIPTOR exercise AND INREGISTER 84
90 (aerobic NEAR3 exercise) or (aerobic NEAR3 training) or aerobics AND INREGISTER 81
91 "ambulatory care" or "behaviour therapy" or "behavior therapy" AND INREGISTER 96
92 "circuit training" or "cognitive therapy" or cycling or dance or dancing AND INREGISTER 122
93 "endurance exercise* or endurance training" or "exercise therapy" or "exercise training" or "exercise program*" AND INREGISTER 276
94 physical* NEAR5 (fit* or train* or activ* or endur* or exertion) AND INREGISTER 191
95 "activity tracking" or pedometer or pedometry or accelerometer or accelerometry AND INREGISTER 9
96 "muscle exercise" or "excessive training" AND INREGISTER 22
97 "fitness training" or "functional activity" or "physical education" AND INREGISTER 22
98 gait or "health training" or "health promotion" or "activities of daily living" or "patient education" AND INREGISTER 313
99 jog or jogging or running or kinesiotherapy or lifestyle or "life style" AND INREGISTER 92
100 MESH DESCRIPTOR Physical Therapy Modalities EXPLODE ALL AND INREGISTER 496
101 "physical therapy" or physiotherapy or "physical train*" AND INREGISTER 361
102 "resistive exercise" or "resistive training" or rowing or swim or swimming AND INREGISTER 9
103 "strength training" or "resistive exercise raining" or "weight training" AND INREGISTER 33
104 "training program" or "training programme" or treadmill or bicycle or yoga AND INREGISTER 124
105 MESH DESCRIPTOR Health Education AND INREGISTER 7
106 MESH DESCRIPTOR Primary Prevention AND INREGISTER 3
107 MESH DESCRIPTOR Health Promotion AND INREGISTER 2
108 MESH DESCRIPTOR Cognitive Behavioral Therapy AND INREGISTER 0
109 MESH DESCRIPTOR Primary Health Care AND INREGISTER 21
110 MESH DESCRIPTOR Workplace AND INREGISTER 1
111 promot* NEAR3 (health or activity or exercise) AND INREGISTER 14
112 educat* NEAR3 (health or activity or exercise) AND INREGISTER 49
113 rehabilitation AND INREGISTER 800
114 therapy NEAR2 (pool or aqua or aquatic or equine of riding) AND INREGISTER 2
115 therapies NEAR2 (pool or aqua or aquatic or equine of riding) AND INREGISTER 1
116 hydrotherapy or horseback or "wheelchair sport*" or "video gam*" AND INREGISTER 9
117 #85 OR #86 OR #87 OR #88 OR #89 OR #90 OR #91 OR #92 OR #93 OR #94 OR #95 OR #96 OR #97 OR #98 OR #99 OR #100 OR #101 OR #102 OR #103 OR #104 OR #105 OR #106 OR #107 OR #108 OR #109 OR #110 OR #111 OR #112 OR #113 OR #114 OR #115 OR #116 AND INREGISTER 1609
118 #117 AND #84 AND INREGISTER 991
119 ("carpal tunnel" or fibromyalgia or sciatica or "low back pain" or "chronic fatigue syndrome"):ti AND INREGISTER 969
120 "respiratory muscle" or "pelvic floor" AND INREGISTER 62
121 #118 NOT (#119 OR #120) AND INREGISTER 825
Appendix 2. CENTRAL (CRSWeb) search strategy
1 MESH DESCRIPTOR Neuromuscular Diseases OR MESH DESCRIPTOR Muscular Atrophy OR MESH DESCRIPTOR Muscular Dystrophies EXPLODE ALL OR MESH DESCRIPTOR Myositis OR MESH DESCRIPTOR Myotonia OR MESH DESCRIPTOR Peripheral Nervous System Diseases OR MESH DESCRIPTOR Polyneuropathies EXPLODE ALL OR MESH DESCRIPTOR Peripheral Nerves OR MESH DESCRIPTOR Neuritis OR MESH DESCRIPTOR Neuromuscular Junction Diseases OR MESH DESCRIPTOR Motor Neuron Disease EXPLODE ALL OR MESH DESCRIPTOR Motor Neuron Disease Explode All OR MESH DESCRIPTOR Glycogen Storage Disease Type V OR MESH DESCRIPTOR Glycogen Phosphorylase, Muscle Form OR MESH DESCRIPTOR Muscular Diseases EXPLODE ALL OR MESH DESCRIPTOR Amyloid Neuropathies EXPLODE ALL OR MESH DESCRIPTOR Brachial Plexus Neuropathies EXPLODE ALL OR MESH DESCRIPTOR Hereditary Sensory and Autonomic Neuropathies OR MESH DESCRIPTOR Hereditary Sensory and Motor Neuropathy OR MESH DESCRIPTOR Peripheral Nervous System Diseases WITH QUALIFIER RH OR MESH DESCRIPTOR Peripheral Nervous System Neoplasms OR MESH DESCRIPTOR Peripheral Nervous System Neoplasms EXPLODE ALL OR MESH DESCRIPTOR POEMS Syndrome OR MESH DESCRIPTOR Polyradiculoneuropathy OR MESH DESCRIPTOR Polyradiculoneuropathy, Chronic Inflammatory Demyelinating OR (myastheni* OR (lambert AND eaton AND syndrome*) OR McArdle* OR "Glycogen Storage Disease Type V" OR "Glycogen Storage Disease Type 5" OR GSDV OR "muscle phosphorylase" deficiency OR myophosphorylase OR ("Glycogen Phosphorylase" NEAR3 "Muscle Form") OR "muscle disease*" OR "muscle disorder*" OR "muscular disease*" OR "muscular disorder*" OR "neuromuscular disease*" OR "neuromuscular disorder*" OR myopath* OR dystroph* OR myotoni* OR myositis OR myopathy OR "muscle fibre" OR "muscle fiber" OR "muscular dystroph*" OR "muscular atrophy" OR myositis OR myotonia OR "peripheral neuropath*" OR polyneuropath* OR "peripheral nerve*" OR neuritis OR polyradiculopathy OR polyradiculoneuropathy OR polyradiculoneuritis OR polyneuritis OR ("neuromuscular junction" NEAR3 (disease OR diseases OR disorder OR disorders)) OR "cervical spondylotic radiculopath*" OR "chronic inflammatory demyelinating polyradiculoneuropathy" OR ("cranial nerve*" NEAR pals*) OR (("drug induced" OR "chemically induced") NEAR neuropath*) OR (alcohol* NEAR neuropath*) OR (amyloid NEAR neuropath*) OR (Bell* NEAR pals*) OR borrelia* OR (Brachial NEAR neuritis) OR (diabetic NEAR neuropath*) OR (hereditary NEAR neuropath*) OR (herpes NEAR zoster) OR (lumbosacral NEAR radiculopath*) OR (multifocal NEAR neuropath*) OR (neuralgic NEAR amyotroph*) OR (paraprot* NEAR neuropath*) OR (poems NEAR2 syndrome) OR polyradiculoneuritis OR (guillain NEAR2 barre) OR (radiation NEAR plexopath*) OR (toxic NEAR neuropath*) OR (trigeminal NEAR neuralgia) OR (vasculiti* NEAR neuropath*)):AB,EH,EMT,KW,KY,MH,TI OR (Als OR mnd):TI,AB OR "motor neuron disease*" OR "motor neurone disease*" OR "motoneuron disease*" OR "motoneurone disease*" OR "motorneuron disease*" OR "motorneurone disease*" OR "charcot disease" OR "amyotrophic lateral sclerosis" OR ((MESH DESCRIPTOR Paraproteinemias OR MESH DESCRIPTOR Alcoholism OR MESH DESCRIPTOR Paraneoplastic Syndromes OR MESH DESCRIPTOR Paraneoplastic Syndromes, Nervous System OR MESH DESCRIPTOR Pain EXPLODE ALL OR (pain OR painful OR chemically OR toxicity):AB,EH,EMT,KW,KY,MH,TI) AND (MESH DESCRIPTOR Peripheral Nervous System Diseases OR (neuropath*):AB,EH,EMT,KW,KY,MH,TI)) OR (demyelin* AND (Inflammatory NEAR2 (polyradiculoneuropath* OR polyneuropath* OR mononeuropath*))):AB,EH,EMT,KW,KY,MH,TI OR (MESH DESCRIPTOR Facial Paralysis AND pals*:AB,EH,EMT,KW,KY,MH,TI) OR (MESH DESCRIPTOR Neuralgia AND (herpes OR herpetic):AB,EH,EMT,KW,KY,MH,TI) OR (MESH DESCRIPTOR Neuritis AND MESH DESCRIPTOR Brachial Plexus) AND CENTRAL:TARGET 32228
2 MESH DESCRIPTOR Cognitive Behavioral Therapy OR MESH DESCRIPTOR Exercise OR MESH DESCRIPTOR Exercise Therapy EXPLODE ALL OR MESH DESCRIPTOR Health Education OR MESH DESCRIPTOR Health Promotion OR MESH DESCRIPTOR Physical Education and Training OR MESH DESCRIPTOR Physical Therapy Modalities EXPLODE ALL OR MESH DESCRIPTOR Primary Health Care OR MESH DESCRIPTOR Primary Prevention OR MESH DESCRIPTOR Sports OR MESH DESCRIPTOR Workplace OR "activity tracking" OR pedometer OR pedometry OR accelerometer OR accelerometry OR "ambulatory care" OR "behaviour therapy" OR "behavior therapy" OR "circuit based exercise" OR "circuit training" OR "cognitive therapy" OR cycling OR dance OR dancing OR "endurance exercise* OR endurance training" OR "exercise therapy" OR "exercise training" OR "exercise program*" OR "fitness training" OR "functional activity" OR "physical education" OR "muscle exercise" OR "excessive training" OR "physical therapy" OR physiotherapy OR "physical train*" OR "resistive exercise" OR "resistive training" OR rowing OR swim OR swimming OR "strength training" OR "resistive exercise raining" OR "weight training" OR "training program" OR "training programme" OR treadmill OR bicycle OR yoga OR (aerobic NEAR3 exercise) OR (aerobic NEAR3 training) OR aerobics OR (educat* NEAR3 (health OR activity OR exercise)) OR gait OR "health training" OR "health promotion" OR "activities of daily living" OR "patient education" OR hydrotherapy OR horseback OR "wheelchair sport*" OR "video gam*" OR jog OR jogging OR running OR kinesiotherapy OR lifestyle OR "life style" OR (physical* NEAR5 (fit* OR train* OR activ* OR endur* OR exertion)) OR (promot* NEAR3 (health OR activity OR exercise)) OR rehabilitation OR (therapies NEAR2 (pool OR aqua OR aquatic OR equine of riding)) OR (therapy NEAR2 (pool OR aqua OR aquatic OR equine of riding)) AND CENTRAL:TARGET 225767
3 #1 AND #2 7014
4 ("carpal tunnel" OR fibromyalgia OR sciatica OR "low back pain" OR "chronic fatigue syndrome"):ti OR "respiratory muscle" OR "pelvic floor" AND CENTRAL:TARGET 14762
5 #3 NOT #4 6177
6 #5 AND INREGISTER 802
7 #5 NOT #6 5375
Appendix 3. MEDLINE (OvidSP) search strategy
Database: Ovid MEDLINE(R) ALL <1946 to 30 April 2020>
Search strategy:
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 randomized controlled trial.pt. (504792)
2 controlled clinical trial.pt. (93651)
3 randomi#ed.ti,ab. (615430)
4 placebo.ab. (207195)
5 randomly.ab. (331945)
6 trial.ab. (502924)
7 groups.ab. (2038293)
8 or/1‐7 (2971635)
9 exp animals/ not humans.sh. (4694664)
10 8 not 9 (2531365)
11 Neuromuscular Diseases/ (10149)
12 Muscular Atrophy/ (10829)
13 exp Muscular Dystrophies/ (26419)
14 Myositis/ (8184)
15 Myotonia/ (1177)
16 (myastheni* or (lambert and eaton and syndrome*)).mp. (20038)
17 Peripheral Nervous System Diseases/ (22702)
18 exp Polyneuropathies/ (27288)
19 Peripheral Nerves/ (23002)
20 Neuritis/ (4977)
21 Neuromuscular Junction Diseases/ (200)
22 exp Motor Neuron Disease/ (27414)
23 (moto*1 neuron*1 disease*1 or moto?neuron*1 disease*1).mp. (9034)
24 (amyotrophic lateral sclerosis or charcot disease).tw. (22574)
25 Glycogen Storage Disease Type V/ (632)
26 (McArdle* or Glycogen Storage Disease Type V or Glycogen Storage Disease Type 5 or GSDV or muscle phosphorylase deficiency or myophosphorylase).mp. (1033)
27 Glycogen Phosphorylase, Muscle Form/ (321)
28 (Glycogen Phosphorylase adj3 Muscle Form).tw. (4)
29 exp Muscular Diseases/ (171957)
30 (muscle disease* or muscle disorder* or muscular disease* or muscular disorder* or neuromuscular disease* or neuromuscular disorder* or myopath* or dystroph* or myotoni* or myositis).mp. (136178)
31 (myopathy or muscle fibre or muscle fiber).mp. (33556)
32 (muscular dystroph* or muscular atrophy or myositis or myotonia).mp. (64549)
33 (peripheral neuropath* or polyneuropath* or peripheral nerve*).tw. (69233)
34 (neuritis or polyradiculopathy or polyradiculoneuropathy or polyradiculoneuritis or polyneuritis).mp. (26456)
35 (neuromuscular junction adj3 (disease*1 or disorder*1)).tw. (410)
36 paraproteinemias/ or alcoholism/ or Paraneoplastic Syndromes/ or exp pain/ or (pain or painful or chemically or toxicity).tw. (1307565)
37 peripheral Nervous System Diseases/ or neuropath*.mp. (154225)
38 36 and 37 (39964)
39 demyelin*.mp. (36526)
40 (Inflammatory adj2 (polyradiculoneuropath* or polyneuropath* or mononeuropath*)).mp. (3532)
41 39 and 40 (3353)
42 Polyradiculoneuritis.mp. or Polyradiculoneuropathy/ (4092)
43 (guillain and barre).mp. (10138)
44 Polyradiculoneuropathy, Chronic Inflammatory Demyelinating/ or chronic inflammatory demyelinating polyradiculoneuropathy.mp. (1838)
45 (multifocal and neuropath*).mp. (1816)
46 (paraprot* adj neuropath*).mp. (108)
47 POEMS syndrome/ (938)
48 (poems adj syndrome).mp. (1221)
49 amyloid neuropathies/ (576)
50 (amyloid adj neuropath*).mp. (2027)
51 "Hereditary Sensory and Motor Neuropathy"/ (1163)
52 "hereditary sensory and autonomic neuropathies"/ (775)
53 (heredit* and neuropath*).mp. (7413)
54 (toxic adj neuropath*).mp. (298)
55 ((drug induced or chemically induced) and neuropath*).mp. (9395)
56 (alcohol* adj neuropath*).mp. (229)
57 borrelia*.mp. (12705)
58 (herpes adj zoster).mp. (14790)
59 (diabetic adj neuropath*).mp. (17447)
60 (vasculiti* and neuropath*).mp. (1760)
61 (Brachial adj neuritis).mp. (173)
62 (neuralgic and amyotroph*).mp. (483)
63 (radiation and plexopath*).mp. (229)
64 Brachial Plexus Neuritis/ (1491)
65 cervical spondylotic radiculopath*.mp. (138)
66 (lumbosacral adj radiculopath*).mp. (356)
67 (Bell* adj pals*).mp. (2774)
68 facial paralysis/ and pals*.mp. (4447)
69 (cranial nerve* adj pals*).mp. (3112)
70 (trigeminal adj neuralgia).mp. (8400)
71 peripheral nervous system neoplasms/ (4462)
72 neuralgia/ and (herpes or herpetic).mp. (1017)
73 neuritis/ and brachial plexus/ (141)
74 peripheral nervous system diseases/rh (186)
75 or/11‐35,38,41‐74 (513168)
76 Circuit‐Based Exercise/ (58)
77 exp Exercise Therapy/ (49861)
78 exp "Physical education and training"/ (13407)
79 exp Sports/ (180732)
80 exp Exercise/ (192034)
81 ((aerobic adj3 exercise) or (aerobic adj3 training) or aerobics).mp. (14256)
82 (ambulatory care or behavio?r therapy).mp. (99044)
83 (circuit training or cognitive therapy cycling or dance or dancing).mp. (6954)
84 (endurance exercise* or endurance training or exercise therapy or exercise training or exercise program).mp. (64440)
85 (physical* adj5 (fit* or train* or activ* or endur* or exertion*)).tw. (141554)
86 (activity tracking or pedometer or pedometry or accelerometer or accelerometry).tw. (14465)
87 (muscle exercise or excessive training).mp. (766)
88 (physical exertion or fitness training or functional activity or physical education or physical fitness or physical endur*).mp. (126679)
89 (gait or health training or health promotion or activities of daily living or patient education).mp. (318970)
90 (jog or jogging or running or kinesiotherapy or lifestyle or life style or physical activit*).mp. (284783)
91 Physical Therapy Modalities/ or (physical therapy or physiotherapy or physical train*).mp. (67603)
92 (resistive exercise or resistive training or rowing or swim or swimming).mp. (44119)
93 ((strength or resistive exercise or weight) adj training).mp. (6077)
94 (training program or treadmill or bicycle or yoga).mp. (68056)
95 health education/ (60160)
96 patient education/ (84573)
97 primary prevention/ (18279)
98 health promotion/ (72894)
99 cognitive therapy/ (24969)
100 primary health care/ (76491)
101 workplace/ (22502)
102 ((promot* or educat*) adj3 (health or activity or exercise)).tw. (157191)
103 rehabilitation.tw. (154202)
104 ((pool or aqua or aquatic or equine or riding) adj2 therap*3).mp. (618)
105 (hydrotherapy or horseback or wheelchair sport*1 or video gam*3).mp. (10413)
106 or/76‐105 (1412604)
107 10 and 75 and 106 (7834)
108 (respiratory muscle or pelvic floor or incontinence).mp. (68726)
109 108 or (carpal tunnel or fibromyalgia or sciatica or low back pain).ti. (98416)
110 107 not 109 (7055)
111 110 and medline.st. (6683)
112 limit 111 to yr="2010 ‐Current" (3892)
113 remove duplicates from 112 (3882)
114 111 not 112 (2791)
115 remove duplicates from 114 (2786)
116 113 or 115 (6668)
117 (review or systematic review or case reports).pt. (4634725)
118 116 not 117 (5760)
Appendix 4. Embase (OvidSP) search strategy
Database: Embase <1974 to 2020 week 17>
Search strategy:
‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
1 crossover‐procedure.sh. (62872)
2 double‐blind procedure.sh. (171663)
3 single‐blind procedure.sh. (38649)
4 randomized controlled trial.sh. (599898)
5 (random* or crossover* or cross over* or placebo* or (doubl* adj blind*) or allocat*).tw,ot. (1765548)
6 trial.ti. (297054)
7 controlled clinical trial/ (464070)
8 or/1‐7 (2090900)
9 exp animal/ or exp invertebrate/ or animal.hw. or non human/ or nonhuman/ (27263094)
10 human/ or human cell/ or human tissue/ or normal human/ (20877879)
11 9 not 10 (6455633)
12 8 not 11 (1858927)
13 limit 12 to (conference abstracts or embase) (1564768)
14 neuromuscular disease/ (16043)
15 muscle atrophy/ (31485)
16 exp muscular dystrophy/ (43051)
17 myositis/ (15001)
18 inclusion body myositis/ (2520)
19 myotonia/ (2453)
20 (myastheni* or (lambert and eaton and syndrome*)).mp. (27248)
21 peripheral neuropathy/ (44795)
22 exp polyneuropathy/ (39303)
23 peripheral nerve/ (20908)
24 neuritis/ (4695)
25 neuromuscular junction disorder/ (956)
26 exp motor neuron disease/ (45371)
27 (moto*1 neuron*1 disease*1 or moto?neuron*1 disease*1).mp. (14232)
28 (amyotrophic lateral sclerosis or charcot disease).tw. (30589)
29 glycogen storage disease/ or glycogen storage disease type 5/ (3727)
30 (McArdle* or Glycogen Storage Disease Type V or Glycogen Storage Disease Type 5 or GSDV or muscle phosphorylase deficiency or myophosphorylase).mp. (1472)
31 glycogen phosphorylase/ (3120)
32 (Glycogen Phosphorylase adj3 Muscle Form).tw. (4)
33 exp muscle disease/ (498688)
34 (muscle disease* or muscle disorder* or muscular disease* or muscular disorder* or neuromuscular disease* or neuromuscular disorder* or myopath* or dystroph* or myotoni* or myositis).mp. (175977)
35 (myopathy or muscle fibre or muscle fiber).mp. (116579)
36 (muscular dystroph* or muscular atrophy or myositis or myotonia).mp. (76821)
37 (peripheral neuropath* or polyneuropath* or peripheral nerve*).tw. (95733)
38 (neuritis or polyradiculopathy or polyradiculoneuropathy or polyradiculoneuritis or polyneuritis).mp. (26098)
39 (neuromuscular junction adj3 (disease*1 or disorder*1)).tw. (748)
40 paraproteinemia/ or alcoholism/ or paraneoplastic syndrome/ or exp pain/ or (pain or painful or chemically or toxicity).tw. (2255833)
41 peripheral neuropathy/ or neuropath*.mp. (312303)
42 40 and 41 (101652)
43 demyelin*.mp. (60198)
44 (Inflammatory adj (polyradiculoneuropath* or polyneuropath* or mononeuropath*)).mp. (457)
45 43 and 44 (229)
46 polyradiculoneuropathy/ (2895)
47 neuritis/ (4695)
48 polyradiculoneuritis.tw. (640)
49 (guillain and barre).mp. (17862)
50 chronic inflammatory demyelinating polyradiculoneuropathy.mp. (1472)
51 (multifocal and neuropath*).mp. (3965)
52 (paraprot* adj neuropath*).mp. (180)
53 POEMS syndrome/ (1286)
54 (poems adj syndrome).mp. (1829)
55 amyloid neuropathy/ (1372)
56 (amyloid adj (neuropath* or polyneuropath)).mp. (1630)
57 hereditary motor sensory neuropathy/ (10647)
58 (heredit* and neuropath*).mp. (19823)
59 (toxic adj neuropath*).mp. (469)
60 ((drug induced or chemically induced) and neuropath*).mp. (5158)
61 (alcohol* adj neuropath*).mp. (217)
62 borrelia.mp. (16601)
63 (herpes adj zoster).mp. (26541)
64 (diabetic adj neuropath*).mp. (26373)
65 (vasculiti* and neuropath*).mp. (4938)
66 (brachial adj neuritis).mp. (243)
67 (neuralgic and amyotroph*).mp. (695)
68 (radiation and plexopath*).mp. (440)
69 brachial plexus neuropathy/ (1706)
70 cervical spondylotic radiculopath*.mp. (199)
71 (lumbosacral adj radiculopath*).mp. (538)
72 (Bell* adj pals*).mp. (4265)
73 facial paralysis/ and pals*.mp. (4149)
74 (cranial nerve* adj pals*).mp. (4551)
75 (trigeminal adj neuralgia).mp. (7477)
76 peripheral nerve tumor/ (1743)
77 neuralgia/ and (herpes or herpetic).mp. (791)
78 peripheral neuropathy/rh (123)
79 or/14‐39,42,45‐78 (896582)
80 exp kinesiotherapy/ (76475)
81 physical education/ (11060)
82 exp sport/ (161091)
83 exp exercise/ (333546)
84 ((aerobic adj3 exercise) or (aerobic adj3 training) or aerobics).mp. (25995)
85 (ambulatory care or behavio?r therapy).mp. (88972)
86 (circuit training or cycling or dance or dancing or walking).mp. (209644)
87 (endurance exercise* or endurance training or exercise therapy or exercise training or exercise program*).mp. (54642)
88 (physical* adj5 (fit* or train* or activ* or endur* or exertion*)).tw. (190692)
89 ((activity adj2 tracking) or pedometer or pedometry or accelerometer or accelerometry).tw. (18973)
90 ((muscle or excess*) adj2 (exercise or training)).mp. (28918)
91 (physical exertion or fitness training or functional activity or physical education or physical fitness or physical endur*).mp. (48548)
92 (gait or health training or health promotion or activities of daily living or patient education).mp. (355105)
93 (jog or jogging or running or kinesiotherapy or lifestyle or life style or physical activit*).mp. (480283)
94 (physical therapy or physiotherapy or physical train*).mp. (110611)
95 (resistive exercise or resistive training or rowing or swim or swimming).mp. (54879)
96 ((strength or resistive exercise or weight) adj2 training).mp. (9411)
97 (training program or treadmill or bicycle or yoga).mp. (109678)
98 health education/ (94133)
99 patient education/ (112003)
100 primary prevention/ (39957)
101 health promotion/ (96112)
102 cognitive therapy/ (43307)
103 primary health care/ (65137)
104 workplace/ (41051)
105 (patient education or primary prevention or workplace or cognitive therapy).tw. (101364)
106 ((promot* or educat*) adj3 (health or activity or exercise)).tw. (186506)
107 rehabilitation.tw. (216812)
108 ((pool or aqua or equine or riding) adj2 therap*3).mp. (433)
109 (hydrotherapy or horseback or wheelchair sport*1 or video gam*3).mp. (11896)
110 or/80‐109 (1988271)
111 13 and 79 and 110 (8931)
112 (respiratory muscle or pelvic floor or incontinence).mp. (123105)
113 112 or (carpal tunnel or fibromyalgia or sciatica or low back pain).ti. (160320)
114 111 not 113 (7955)
115 limit 114 to yr="2010 ‐Current" (5100)
116 remove duplicates from 115 (5058)
117 114 not 116 (2897)
118 remove duplicates from 117 (2870)
119 116 or 118 (7928)
Appendix 5. ClinicalTrials.Gov search strategy
Advanced search
Study type: interventional studies (clinical trials)
Search 1
Condition or disease: Amyotroph* OR Borrelia OR Charcot OR Dystroph* OR "Glycogen Storage Disease Type 5" OR "Glycogen Storage Disease Type V" OR Guillain OR Herpes Zoster OR Lambert OR Motor Neuron OR Muscle Disease* OR Muscle Disorder* OR Muscular Atrophy
Intervention/treatment: Acceleromet* OR Activ* OR Aerobic* OR Ambulatory OR Aqua* OR Behavior* OR Behaviour* OR Bicycle OR Cognitive OR Cycling OR Living OR Danc* OR Education OR Equine OR Exercis* OR Fitness OR Gait OR Health Promotion OR Horseback OR Hydrotherapy OR Jog*
819 Studies
Search 2
Condition or disease: Amyotroph* OR Borrelia OR Charcot OR Dystroph* OR "Glycogen Storage Disease Type 5" OR "Glycogen Storage Disease Type V" OR Guillain OR Herpes Zoster OR Lambert OR Motor Neuron OR Muscle Disease* OR Muscle Disorder* OR Muscular Atrophy
Intervention/treatment: Kinesiotherapy OR Life Style OR Lifestyle OR Pedomet* OR Physical* OR Physiotherap* OR Pool OR Primary Health Care OR Primary Prevention OR Rehabilitation OR Riding OR Rowing OR Running OR Sport* OR Swim* OR Train* OR Treadmill OR Video Game* OR Yoga
369 Studies
Search 3
Condition or disease: Muscular Disease* OR Muscular Disorder* OR Myastheni* OR Myopath* OR Myositis OR Myotoni* OR Neuralgia OR Neuritis OR Neuromuscular OR Neuropath* OR Palsy OR POEMS OR Polyneuritis OR Polyneuropath* OR Polyradiculo* OR Plexopath* OR Radiculopath*
Intervention/treatment: Acceleromet* OR Activ* OR Aerobic* OR Ambulatory OR Aqua* OR Behavior* OR Behaviour* OR Bicycle OR Cognitive OR Cycling OR Living OR Danc* OR Education OR Equine OR Exercis* OR Fitness OR Gait OR Health Promotion OR Horseback OR Hydrotherapy OR Jog*
1497 Studies
Search 4
Condition or disease: Muscular Disease* OR Muscular Disorder* OR Myastheni* OR Myopath* OR Myositis OR Myotoni* OR Neuralgia OR Neuritis OR Neuromuscular OR Neuropath* OR Palsy OR POEMS OR Polyneuritis OR Polyneuropath* OR Polyradiculo* OR Plexopath* OR Radiculopath*
Intervention/treatment: Kinesiotherapy OR Life Style OR Lifestyle OR Pedomet* OR Physical* OR Physiotherap* OR Pool OR Primary Health Care OR Primary Prevention OR Rehabilitation OR Riding OR Rowing OR Running OR Sport* OR Swim* OR Train* OR Treadmill OR Video Game* OR Yoga
789 Studies
Data and analyses
Comparison 1. A physical activity (PA) programme (weight‐bearing) compared no PA programme in people living with NMD.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Time spent walking (minutes per week, activity monitor) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1.1 3 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1.2 6 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1.3 12 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.2 Daily steps (count, activity monitor) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.2.1 3 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.2.2 6 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.2.3 12 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.3 Steps taken in 30‐minute bouts (count, activity monitor) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.3.1 3 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.3.2 6 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.3.3 12 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 2. A weight‐bearing (WB) exercise programme compared to a non‐WB exercise programme in people living with NMD.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Daily steps (count, activity monitor) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 3. A sensor‐based, interactive exercise programme compared to no sensor‐based, interactive exercise programme in people living with NMD.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Time spent walking (hours per 48 hours, activity monitor) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.2 Daily steps (count, activity monitor) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.3 Quality of life (Physical Component Score, questionnaire) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.4 Quality of life (Mental Component Score, questionnaire) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 4. An aerobic exercise programme compared to no aerobic exercise programme in people living with NMD.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Daily steps (count, activity monitor) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.1 4 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.2 7 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1.3 10 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.2 Disease‐specific quality of life (ALSAQ‐40, questionnaire) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.3 Quality of life (SF‐36 Physical Component Score, questionnaire) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.4 Quality of life (SF‐36 Mental Component Score, questionnaire) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.5 Quality of life (SF‐36 Physical Component Score, questionnaire) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.5.1 4 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.5.2 7 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.5.3 10 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.6 Quality of life (SF‐36 Mental Component Score, questionnaire) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.6.1 4 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.6.2 7 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.6.3 10 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 5. An aerobic exercise training programme compared to cognitive behavioural therapy (CBT) in people living with NMD.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Daily steps (count, activity monitor) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1.1 4 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1.2 7 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1.3 10 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.2 Quality of life (SF‐36 Physical Component Score, questionnaire) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.2.1 4 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.2.2 7 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.2.3 10 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.3 Quality of life (SF‐36 Mental Component Score, questionnaire) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.3.1 4 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.3.2 7 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.3.3 10 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 6. Cognitive behavioural therapy (CBT) compared to no CBT in people living with NMD.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Daily steps (count, activity monitor) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1.1 4 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1.2 7 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1.3 10 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.2 Quality of life (SF‐36 Physical Component Score, questionnaire) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.2.1 4 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.2.2 7 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.2.3 10 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.3 Quality of life (SF‐36 Mental Component Score, questionnaire) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.3.1 4 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.3.2 7 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.3.3 10 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Comparison 7. Cognitive behavioural therapy (CBT) with/without an exercise programme compared to no CBT and no exercise programme in people living with NMD.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Physical activity (unclear units – interpreted as mean magnitude of ankle acceleration over 24 hours, activity monitor with Euclidian Norm Minus One metric) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.1.1 5 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.1.2 10 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.1.3 16 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.2 Physical activity (unclear units – interpreted as mean magnitude of ankle acceleration over 5 hours of highest activity, activity monitor with Euclidian Norm Minus One metric) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.2.1 5 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.2.2 10 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.2.3 16 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.3 Physical activity (unclear units – interpreted as mean magnitude of ankle acceleration over 5 hours of lowest activity, activity monitor with Euclidian Norm Minus One metric) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.3.1 5 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.3.2 10 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.3.3 16 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.4 NMD‐specific quality of life (INQoL) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.4.1 5 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.4.2 10 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.4.3 16 months | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.5 Adverse events | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 7.6 Serious adverse events | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Comparison 8. A functional exercise programme compared to a stretching exercise programme in people living with NMD.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Physical activity (unspecified count per day, activity monitor) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.2 Quality of life (SF‐36 Physical Component Score, questionnaire) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.3 Quality of life (SF‐36 Mental Component Score, questionnaire) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.4 Quality of life (SF‐36 Vitality Component Score, questionnaire) | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Andersen 2015.
| Study characteristics | ||
| Methods |
Aim To investigate the effect of regular aerobic training and postexercise protein carbohydrate supplementation in people with FSHD. Design Parallel RCT Unit of allocation By individuals Ethical approval needed/obtained for study Yes (approved by the Ethics Committee of Copenhagen) Study dates 21 March 2012 to 28 October 2013 |
|
| Participants |
ITT population: Population description Adults with genetically verified FSHD type 1 Age Not reported for total randomised population Sex Not reported for total randomised population Setting Denmark Inclusion criteria Diagnosis of FSHD type 1 Exclusion criteria Regular cardio exercise (> 2 hours/week); pregnancy or breastfeeding; inability to cycle; disabilities other than FSHD that could confound the interpretation of the results Method of recruitment of participants From the Copenhagen Neuromuscular Center and the Rehabilitation Centre for Neuromuscular Diseases in Denmark Informed consent obtained Yes Total number randomised 41 Clusters Not applicable See Description of studies for more information on study participants in the context of physical activity promotion. |
|
| Interventions | For 12 weeks
Description of support provided: participants exercising were supervised by telephone and received a variable number of contacts according to different support needs. The report did not detail who provided supervisory support for the exercise intervention or any standard care provided to the 'no intervention' and other group. However, over half the participants also received ≥ 1 medication. |
|
| Outcomes |
Primary
Secondary
Outcomes in bold of interest to this review. See Description of studies for more information on physical activity outcome measurement in the context of physical activity promotion. |
|
| Notes | Final scores reported but outcome data were not reported in a usable way (mean and range values or no numerical results reported). Although 'safety and harm' was reported in the results, there was no prespecified or analysed adverse event outcome measurement. Sources of funding The Aase and Einar Danielsens Foundation, Augustinus Foundation, AP Moeller Foundation, and The Danish Rheumatism Association Foundation. Conflicts of interest No study‐related conflicts of interest in relation to the review question. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "we randomized patients to 3 groups." |
| Allocation concealment (selection bias) | Unclear risk | Study appendix appeared to refer to blinding not allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "All investigators and participants were kept blinded to the treatment assignment, until the last participant had finished the trial and all data were analyzed" (study appendix). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All investigators and participants were kept blinded to the treatment assignment, until the last participant had finished the trial and all data were analyzed" (study appendix). |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Physical activity outcomes were only reported for a subset of participants analysed (protein group, n = 9/13, placebo group, n = 10/13; no intervention group, n = 9/9). Quality of life was incompletely reported as an outcome. |
| Selective reporting (reporting bias) | Low risk | None identified. |
| Other bias | Low risk | None identified. |
Andersen 2017.
| Study characteristics | ||
| Methods |
Aim To determine whether HIT is safe and effective in FSHD type 1. Design Parallel RCT Unit of allocation By individuals Ethical approval needed/obtained for study Yes (study approved by the Ethics Committee of Copenhagen) Study dates August 2014 to September 2015 |
|
| Participants |
ITT population: Population description Adults with genetically verified FSHD type 1. Comorbidities included osteoporosis, depression, atrial fibrillation, hypertension, and psoriasis. Age Not reported for total randomised population Sex 67% male (randomised to a supervised HIT group); not reported for total randomised to a usual care group Setting Denmark Inclusion criteria Aged 18–70 years and genetically verified FSHD type 1 Exclusion criteria Inability to cycle; regular cardio exercise (1 hour/week), or factors that potentially could confound the results (pregnancy, breastfeeding, disabilities other than FSHD type 1, participation in other studies) Method of recruitment of participants Through the Copenhagen Neuromuscular Center Informed consent obtained Yes Total number randomised 13 Clusters Not applicable See Description of studies for more information on study participants in the context of physical activity promotion. |
|
| Interventions | For 8 weeks
Description of support provided: all HIT sessions were supervised, although it was unclear who by, or whether training was delivered individually or as a group. The report did not describe usual care but participants were not allowed to change either their diet or activity levels during the study. |
|
| Outcomes |
Primary
Secondary
Outcomes in bold of interest to this review. See Description of studies for more information on physical activity outcome measurement in the context of physical activity promotion. |
|
| Notes | Change scores reported but no numerical data for daily activity levels (outcome data were not reported in a usable way). Although the safety of intervention was reported, adverse events were not prespecified or analysed as an outcome measure. Sources of funding Aase and Einar Danielsens Foundation, Augustinus Foundation, and AP Moeller Foundation provided financial support. Conflicts of interest No study‐related conflicts of interest in relation to the review question. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomisation was performed by postcode which the authors acknowledge could potentially introduce bias, i.e., those living closer to the capital city, Copenhagen, may have better employment, finances, mobility, motivation, etc." |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Unblinded." Comment: we judged the risk of bias as low due to the nature of intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "Unblinded." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Physical activity data reported incompletely. |
| Selective reporting (reporting bias) | Unclear risk | As above, physical activity data incompletely reported without explanation; the methods reported that descriptive data were expressed as mean and SD and effect sizes with 95% CI; baseline demographics were reported as mean and SD and some outcomes included a 95% CI but there were no quantitative data reported for the physical activity outcome measure. |
| Other bias | Low risk | None identified. |
Elsworth 2011.
| Study characteristics | ||
| Methods |
Aim To examine the feasibility and safety of supporting community exercise for people with long‐term neurological conditions using a physical activity support system. Design Parallel RCT Unit of allocation By individuals Ethical approval needed/obtained for study Yes (study approved by Oxfordshire and Birmingham Ethics Committees) Study dates Recruitment between October 2007 and December 2008 |
|
| Participants |
ITT population: Population description People with a confirmed diagnosis of a long‐term neurological condition including multiple sclerosis, NMDs, Parkinson's disease and cerebral palsy Age Not reported for subgroup with NMD Sex Not reported for subgroup with NMD Setting UK Inclusion criteria Aged ≥ 18 years; able to engage with training in an exercise facility or gym; able to walk 10 m using an aid or assistance; able to participate for the duration of the study Exclusion criteria Unable to meet the study criteria; any contraindications to exercise; unwilling to participate in the programme Method of recruitment of participants Recruitment occurred through local neurological services and the Dementias and Neurodegenerative Diseases Research Network (DeNDRoN) Informed consent obtained Yes Total number randomised 99 (of whom 26 had motor neuron disease or other NMD) Clusters Not applicable See Description of studies for more information on study participants in the context of physical activity promotion. |
|
| Interventions | For 12 weeks
Description of support provided: community gym‐based exercise was facilitated through 'Inclusive Fitness Initiative' gyms that provided "a physically accessible fitness facility, equipment designed and tested for use by people with disabilities, and fitness staff with expertise in exercise prescription." Following an initial exercise induction with a physical therapist, intervention was self‐directed by participants and supported by a fitness professional with additional support from the physical therapist as needed. A Physical Activity Support System was also used, in which the physical therapist shared information and current guidance on exercise, as well as practical advice and support for both the participant and fitness professional. Study investigators reported that associated travel and gym costs were covered by the study. Standard care was not detailed fully. However, the control group receiving standard care were made aware of the opportunity to participate in the exercise intervention after completion of the RCT. |
|
| Outcomes |
Primary
Other
Outcomes in bold of interest to this review. See Description of studies for more information on physical activity outcome measurement in the context of physical activity promotion. |
|
| Notes | Change scores reported and postexercise final scores for the overall study population only. Additional unpublished data were sought for participants with motor neuron disease (n = 7) and 19 participants with other unspecified NMDs. However, few data were applicable to the review population and their allocation to intervention or usual care was unclear from coded data (outcome data were not available in a usable way). Sources of funding The research initiative for implementation of the National Service Framework Long‐term Neurological Conditions Department of Health, Thames Valley Primary Care Trust, National Institute for Health Research, Parkinson's UK, University of Birmingham. Conflicts of interest No study‐related conflicts of interest in relation to the review question. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was achieved by computer generated random block sizes of 2 and 4 by Birmingham Primary Care Clinical Trials and Research Unit and stratified by Barthel ADL Index score (≤15 and ≥16) and condition." |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation and block size was concealed from the assessor and study coordinator. Study physiotherapists were informed of patient allocation using email by the trials unit statistician following baseline assessments, and subsequently revealed group allocation to each participant." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Participants and the study physiotherapists were not blinded to group allocation" but review authors judged a low risk of bias due to the nature of intervention." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "the assessor was blinded to treatment assignment for the duration of the study. Only the study statisticians and the data monitoring committee saw unblinded data, but none had contact with study participants." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | None identified. |
| Selective reporting (reporting bias) | Low risk | None identified. |
| Other bias | Low risk | None identified. |
Grewal 2015.
| Study characteristics | ||
| Methods |
Aim To investigate the effect of sensor‐based interactive balance training on postural stability and daily physical activity in older adults with DPN. Design Parallel RCT Unit of allocation By individuals Ethical approval needed/obtained for study Unclear Study dates Not reported |
|
| Participants |
ITT population: Population description Adults with DPN Age Not reported for total randomised population Sex 42% male (randomised population) Setting USA and Qatar Inclusion criteria Ability to walk independently for 20 m; medically diagnosed type 2 diabetes with DPN. Peripheral neuropathy was confirmed using the criteria explained in the American Diabetes Association statement and the insensitivity to 10 g Semmes‐Weinstein monofilament. Additionally, the vibration perception threshold score was recorded to quantify the level of neuropathy with a cut‐off of 25 V as an indicator of neuropathy at recommended plantar foot sites Exclusion criteria Diagnosed with cognitive, vestibular, or central neurological dysfunction; musculoskeletal abnormality; active foot ulcers; Charcot's joints; or a history of balance disorder unrelated to DPN Method of recruitment of participants Outpatient clinics in Tucson, Arizona, USA, and Doha, Qatar Informed consent obtained Yes Total number randomised 39 Clusters Not applicable See Description of studies for more information on study participants in the context of physical activity promotion. |
|
| Interventions | For 4 weeks
Description of support provided: delivered at an outpatient clinic, the exercise intervention used a virtual reality interface with real‐time joint feedback. A qualified research member of staff was present at all exercise sessions. The control group received standard care but did not attend clinic or participate in any exercise during the study. |
|
| Outcomes |
Primary
Other
Follow‐up outcomes after 4 weeks included in results Outcomes in bold of interest to this review. See Description of studies for more information on physical activity outcome measurement in the context of physical activity promotion. |
|
| Notes | Final scores reported. Mean change scores also reported but with no measure of variability. Adverse events were not prespecified as an outcome measure but reported in the results for balance training. Source of funding Supported in part by the Qatar National Research Foundation (NPRP‐4‐1025‐3‐276). Conflicts of interest No study‐related conflicts of interest in relation to the review question. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was done using a computer‐generated list." |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation was concealed from the staff using opaque envelopes." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Study described as "single‐blinded;" low risk of bias due to the nature of intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Study described as "single‐blinded," but it was unclear who was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | For the overall study, 4/20 participants (20%) dropped out and were not included in analysis. As detailed in the methods, only a subset of participants (25/39) underwent physical activity monitoring. |
| Selective reporting (reporting bias) | High risk | Physical activity monitoring reported incompletely and there was no explanation of how this subset was identified or numbers who dropped out from physical activity monitoring. |
| Other bias | Low risk | None identified. |
Koopman 2016.
| Study characteristics | ||
| Methods |
Aim To study the efficacy of exercise therapy and CBT on reducing fatigue and improving activities and health‐related quality of life in people with PPS. Design Parallel RCT Unit of allocation By individuals Ethical approval needed/obtained for study Yes (study protocol approved by the Medical Ethics Committee of the Academic Medical Centre in Amsterdam) Study dates Enrolment from June 2009 to September 2012 |
|
| Participants |
ITT population: Population description Adults with PPS Age Not reported for total randomised population Sex Not reported for total randomised population Setting The Netherlands Inclusion criteria Diagnosis of PPS according to the criteria of the March of Dimes, which includes a gradual or sudden onset of progressive and persistent muscle weakness or abnormal muscle fatigability after a period of stable neurological function; severe perceived fatigue (CIS‐Fatigue ≥ 35); aged 18–75 years; life‐expectancy > 1 year, i.e. absence of life‐threatening comorbidity; walking ability at least indoors with or without a walking aid; ability to cycle on an ergometer against a load of ≥ 25 W Exclusion criteria Use of psychotropic drugs or other psychiatric treatment; clinical depression (BDI‐Primary Care > 6); disabling comorbidity interfering with the intervention programmes or influencing outcome parameters (including cardiopulmonary disease, epileptic seizures, poorly regulated diabetes mellitus); respiratory insufficiency (FVC < 50% predicted or carbon dioxide retention) or assisted ventilation; cognitive impairment; insufficient proficiency in the Dutch language; pregnancy Method of recruitment of participants From 7 hospitals and rehabilitation centres in the Netherlands Informed consent obtained Yes Total number randomised 68 Clusters Not applicable See Description of studies for more information on study participants in the context of physical activity promotion. |
|
| Interventions | For 4 months
Description of support provided: the participants in the exercise group undertook a combination of home‐based training and group exercise supervised by physical therapists trained in the study protocol. CBT, delivered by certified therapists, involved individually tailored provision of standard modules relating to fatigue, including deregulation of physical activity. Both intervention groups and the third group received usual care, such as physical therapy, support for the use of assistive devices and orthoses, and medication. The study did not limit participants' everyday physical activity in any group. |
|
| Outcomes |
Primary
Secondary
Exploratory
Other
Follow‐up outcomes after 4, 7, and 10 months included in results Outcomes in bold of interest to this review. See Description of studies for more information on physical activity outcome measurement in the context of physical activity promotion. |
|
| Notes | Final scores reported (after intervention) Sources of funding Prinses Beatrix SpierFonds (The Dutch Public Fund for Neuromuscular Disorders), ZonMw (the Netherlands Organisation for Health Research and Development, ID: ZonMw 89000003), het Revalidatiefonds/Revalidatie Nederland/de Nederlandse Vereniging van Revalidatieartsen (the Netherlands Society of Physical and Rehabilitation Medicine). Conflicts of interest No study‐related conflicts of interest in relation to the review question. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomization scheme was computer generated, and random blocks of sequences were created with variable block sizes of 3 and 6." |
| Allocation concealment (selection bias) | Low risk | Quote: "An independent investigator performed the randomization. The investigator responsible for the inclusion and the 2 experimenters who performed the outcome assessments were blinded to the group allocation." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | We judged at low risk of bias due to the nature of intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "single‐blinded… The investigator responsible for the inclusion and the 2 experimenters who performed the outcome assessments were blinded to the group allocation." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | ITT analysis was reported with no imputation for missing data under the assumption that data were missing at random. There was a large proportion of missing data from 2 arms of the study – the difference between ITT and per‐protocol analysis was 9/23 participants (39%) in the exercise intervention arm and 8/23 participants (in the CBT arm (35%), whereas all participants in the ITT analysis for the usual care arm were included in the per‐protocol analysis. Adverse event data were also only reported for the exercise arm of the study. |
| Selective reporting (reporting bias) | High risk | The availability of data on adverse events was not specified for each arm of the study. (In terms of selective non‐reporting, other outcomes including quality of life using the EQ‐5D were reported in the protocol but not in the full paper or supplement.) |
| Other bias | Low risk | None identified. |
Lemaster 2008.
| Study characteristics | ||
| Methods |
Aim To determine the effect of a lower extremity exercise and walking intervention programme on weight‐bearing activity and foot ulcer incidence in people with DPN and to encourage participants to gradually increase total daily weight‐bearing steps. Design Parallel RCT Unit of allocation By individuals Ethical approval needed/obtained for study Yes (study approved by the University of Missouri–Columbia Health Sciences and University of Washington institutional review boards and by the research and development committees at the Harry S Truman Memorial Veterans' Hospital in Columbia, Missouri, and the VA Puget Sound Health Care System in Seattle, Washington) Study dates Not reported |
|
| Participants |
ITT population: Population description Adults with DPN. Comorbidities included cardiovascular disease, joint pain in lower limbs, cancer, and respiratory disease (chronic bronchitis or asthma) Age Mean age 66.6 years (SD 10.4) in the intervention group and 64.8 years (SD 9.4) in the control group (randomised population) Sex 53% male (randomised population) Setting Primary care, endocrinology or podiatry practices in central Missouri, USA Inclusion criteria Inactive (did not engage in moderate‐intensity activity more than twice per week for more than 20 minutes per session); diagnosed type 1 or 2 diabetes mellitus; absent sensation to 5.07 Semmes‐Weinstein monofilament sensation ≥ 1 point at any of 10 sites on each foot, and had loss of vibratory sensation measured using a biothesiometer (unable to sense < 25 V at the hallux) Exclusion criteria No telephone access; had medical conditions that might contraindicate exercise Method of recruitment of participants People aged ≥ 50 years who received diabetes or foot care at primary care, endocrinology, or podiatry practices in central Missouri were invited to join the study Informed consent obtained Yes Total number randomised 79 Clusters Not applicable See Description of studies for more information on study participants in the context of physical activity promotion. |
|
| Interventions | For 12 months
Description of support provided: in the 1st part of the physical activity programme (months 1–3), individuals undertook progressive balance and strengthening exercises at home, and 8 supervised sessions with a physical therapist. The therapist and study nurse then supported participants to undertake an individually tailored walking programme, gradually increasing activity by adding ≥ 100 steps every 2 weeks. Participants monitored their activity with a pedometer and activity log. In the 2nd part of the programme (months 4–12), investigators used motivational techniques to promote physical activity via telephone calls and workshops. The study nurse undertook training in motivational interviewing techniques and called the participants every 2 weeks for ≥ 10 minutes to prompt participants to follow their walking plan and assist them in solving related barriers. The control group did not undertake a supported exercise and walking programme or receive motivational telephone contact. However, the control group participants received the same number of therapist visits for foot examination, and all participants received usual medical care. All participants were taught foot‐related self‐care and referred at enrolment to orthotists or podiatrists for therapeutic footwear; participants were encouraged to wear the footwear during physical activity. The study defined protocol adherence as attendance at > 50% of physical therapy sessions and at 3‐, 6‐, and 12‐month study visits, as well as participation in ≥ 50% of the weekly telephone calls. |
|
| Outcomes |
Primary
Other
Follow‐up outcomes after 3, 6, and 12 months included in results Outcomes in bold of interest to this review. See Description of studies for more information on physical activity outcome measurement in the context of physical activity promotion. |
|
| Notes | Final scores reported (after intervention). Adverse events were not prespecified as an outcome measure but reported on for the intervention group. Sources of funding The Robert Wood Johnson Foundation Generalist Physician Faculty Scholars Program. Supported with resources and the use of facilities at the University of Missouri Health Care System, the Harry S Truman Memorial Veterans' Hospital, and the VA Puget Sound Health Care System. Conflicts of interest No study‐related conflicts of interest in relation to the review question. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Because treatment strategies for early foot lesions could differ among types of clinical sites, randomization was by type of clinical site (specifically, university affiliated family medicine, university affiliated endocrinology, VA‐affiliated foot clinic, local family medicine and internal medicine practices not affiliated with the university, and out‐of county unaffiliated family medicine and internal medicine practices). Study groups were balanced within each type of site by using randomization blocks of various sizes." |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation to study groups was concealed by opaque envelopes, which were opened by the study nurse at the randomization visit." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Low risk of bias due to the nature of intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Research staff engaged in collecting physical measurements or questionnaire data from participants or tracking other outcomes (ie, foot lesions) were blinded to participants' study group identity (intervention vs. control). These staff did not take part in intervention activities." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analyses compared the intervention and control groups, regardless of their level of protocol adherence and study participation (Intervention group data: 37/41 at 3 months; 38/41 at 6 months; 35/41 at 12 months; control group data: 32/38 at 3 months; 36/38 at 6 months; 35/38 at 12 months). |
| Selective reporting (reporting bias) | Low risk | None identified. |
| Other bias | Low risk | None identified. |
Mueller 2013.
| Study characteristics | ||
| Methods |
Aim To determine the effect of a weight‐bearing exercise programme compared with a non‐weight‐bearing exercise programme on the primary outcome measures of the 6MWT and daily step counts (steps per day). Design Parallel RCT Unit of allocation By individuals Ethical approval needed/obtained for study Approved by the institutional review board Study dates Recruitment began in 2009 and terminated in 2011 |
|
| Participants |
ITT population: Population description People with DPN. Comorbidities included cardiac procedures/conditions, hypertension, history of cancer, and history of foot ulcers Age Mean age 65.2 years (SD 12.8) in the weight‐bearing group and 63.9 years (SD 12.5) in the non‐weight‐bearing group (randomised population) Sex 67% male randomised to the weight‐bearing group and 50% male randomised to the non‐weight‐bearing group Setting University‐based physical therapy research clinic, USA Inclusion criteria Type 2 diabetes mellitus and peripheral neuropathy (inability to sense the 5.07 Semmes‐Weinstein monofilament on ≥ 1 spot on the plantar foot and inability to sense vibration at the plantar great toe from a biothesiometer at < 25 V); have step count 2000–9000 steps per day; currently exercising < 3 times per week, < 20 minutes per session; have approval of their primary physician to participate in the study Exclusion criteria Weighed > 136 kg (scanner weight limit used in a different portion of study); had a severe foot deformity that would require custom therapeutic footwear; had a comorbidity; or took a medication that would interfere with ability to exercise according to the current American Diabetes Association guidelines Method of recruitment of participants From a database of previous participants, the Washington University School of Medicine Research Participant Registry, cable television commercials, a newspaper story, and recruitment posters displayed in a Diabetes Treatment Center and on area commuter trains Informed consent obtained Yes Total number randomised 29 Clusters Not applicable See Description of studies for more information on study participants in the context of physical activity promotion. |
|
| Interventions | For 12 weeks
Description of support provided: each intervention involved group exercise (1–4 participants) supervised by a physical therapist and assistant. Participants wore their own footwear but were supported to find alternative footwear if their own did not meet certain criteria. In the weight‐bearing exercise group, participants were instructed to increase their centre‐based step count every 2 weeks by 24% on the 3 days that they participated in the exercise programme, resulting in a mean increase in their daily step count by 10% during that 2‐week period. In the non‐weight‐bearing exercise group, baseline activity monitoring informed the participants' initial duration of cycling on a static bicycle. No other co‐intervention was reported except that participants examined their feet and footwear with the physical therapist as part of each exercise session. In addition to travel reimbursement, participants received a cash incentive for completing the final assessment. |
|
| Outcomes |
Primary
Secondary
Follow‐up outcomes after 16 weeks included in results Outcomes in bold of interest to this review. See Description of studies for more information on physical activity outcome measurement in the context of physical activity promotion. |
|
| Notes | Final scores (after intervention) reported. Skin lesions on the lower leg were monitored to document the safety of the interventions; adverse events were not prespecified as an outcome measure but analysed in the results. Sources of funding The National Institutes of Health (grant nos. NCMRR R21 HD058938, T32 HD007434‐17 NSMRC R24HD650837, NIH UL1 RR024992), Diabetes Research Training Center (grant number 5 P60 DK20579), and scholarships from the Foundation for Physical Therapy. Conflicts of interest No study‐related conflicts of interest in relation to the review question. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants were randomized into 2 groups (WB, NWB) using a prearranged schedule generated by the statistician (M.JS.) using a computer program." |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation was concealed to all except the research coordinator who entered subjects into the study." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Low risk of bias due to the nature of intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All outcome measures were collected and analyzed by a tester blinded to group assignment, except for the posttreatment 6MWD, which was conducted by a physical therapist who also provided some treatment." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | None identified. |
| Selective reporting (reporting bias) | Low risk | None identified. |
| Other bias | Low risk | None identified. |
Okkersen 2018.
| Study characteristics | ||
| Methods |
Aim To determine whether CBT optionally combined with graded exercise compared with standard care alone improved the health status of people with DM1. Design Parallel RCT Unit of allocation By individuals. Family members were allocated to the same intervention but there was no adjustment for clustering because outcomes were measured at the level of the participant Ethical approval needed/obtained for study Study approved by the institutional review boards at each of the 4 clinical sites Study dates Assignment to intervention from April 2014 to 29 May 2015 |
|
| Participants |
ITT population: Population description Adults with a confirmed genetic diagnosis of DM1. Comorbidities included cardiac conditions and presence of pacemaker or ICD and regular use of assistive ventilator device Age Mean age 44.8 years (SD 11.7) in the CBT group and 46.4 years (SD 11.3) in the standard care group (randomised population) Sex 55% male randomised to CBT and 53% male randomised to standard care Setting Multi‐centre trial in Paris (France), Munich (Germany), Nijmegen (the Netherlands), and Newcastle (UK) Inclusion criteria Confirmed genetic diagnosis of DM1; aged ≥ 18 years; severely fatigued (measured using CIS‐Fatigue score ≥ 35); able to walk independently (walking aids permitted); able to undergo trial interventions Additional inclusion criteria for carers of participants included: ability to give informed consent; ability to complete study questionnaires; ability to attend CBT sessions with participants Exclusion criteria Neurological or orthopaedic comorbidity interfering with the interventions or possibly influencing outcomes; use of psychotropic drugs (except modafinil, methylphenidate, and antidepressants where the dosing regimen was stable for ≥ 12 months prior to screening). If the doses of modafinil or methylphenidate increased during the 10 months of intervention or non‐intervention, then the person was excluded; severe depression at screening based on clinical judgement; participation in another clinical trial of an investigational medicinal product or other interventional study considered to influence outcomes being evaluated in the Observational Prolonged Trial in Myotonic Dystrophy Type 1 (OPTIMISTIC) concurrently or within 30 days prior to screening for entry into study; unable to complete study questionnaires Method of recruitment of participants By invitation via DM1 registries, from clinics via their treating neurologists, or independently through study awareness by patient organisations Informed consent obtained Yes Total number randomised 255 Clusters Immediate family members were allocated as a cluster to avoid treatment contamination. See Description of studies for more information on study participants in the context of physical activity promotion. |
|
| Interventions | For 10 months
Description of support provided: the study planned for ≥ 5 face‐to‐face sessions of CBT but also allowed for additional modes of delivery including telephone and video calls, and email contact. The intervention involved individually tailored provision of standard modules relating to fatigue, including activity regulation and graded activity. An optional graded exercise intervention, involving mainly aerobic activities and supported by physical therapists familiar with DM1 was discussed with participants at 2 study sites; this exercise intervention was only commenced if participants increased their physical activity levels during the graded activity module. However, 2 other study sites did not offer the exercise module because regular physiotherapy was part of the national standards of care. Therapists trained and experienced in CBT delivered the CBT and, where indicated, a physical therapist led the delivery of the graded exercise module. Participants in both groups received the local standard care, including medication, regular follow‐up by a multi‐disciplinary team, and physiotherapy. |
|
| Outcomes |
Primary
Secondary
Follow‐up after 5, 10, and 16 months Outcomes in bold of interest to this review. See Description of studies for more information on physical activity outcome measurement in the context of physical activity promotion. |
|
| Notes | Unadjusted final scores reported at all time points (after intervention). Change scores also reported from baseline to 10 months, which were (quote) "adjusted for baseline value, muscular impairment rating scale, site, caregiver involvement, and age." Source of funding The European Union Seventh Framework Program, under grant agreement number 305697 (the Observational Prolonged Trial In Myotonic dystrophy type 1 to Improve Quality of Life Standards, a Target Identification Collaboration (OPTIMISTIC) project). Conflicts of interest No study‐related conflicts of interest in relation to the review question (note: 2 review authors were involved in this study). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was done via the central Tayside Randomisation web‐based system (TRuST) developed by the Tayside Clinical Trials Unit (University of Dundee, Dundee, UK)." |
| Allocation concealment (selection bias) | Low risk | Randomisation via a central, web‐based system. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Low risk of bias due to the nature of intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "single‐blind." "Only outcome adjudicators were masked to treatment allocation; they were also instructed to refrain from interactions with the patient that could disclose treatment allocation. During therapy, patients were discouraged from disclosing their treatment allocation to outcome adjudicators." Comment: however, the study appendix highlights a protocol deviation that at 1 of the sites it was not possible to blind outcome assessors. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | There were missing data for physical activity outcomes (31% from CBT group and 40% from standard care group). Also, there were missing data for the quality of life outcome (12% from CBT group and 17% from standard care group). |
| Selective reporting (reporting bias) | Low risk | None identified. |
| Other bias | Low risk | None identified. |
Shrader 2015.
| Study characteristics | ||
| Methods |
Aim To determine the safety and efficacy of a home‐based functional exercise programme in SBMA. Design Parallel RCT Unit of allocation By individual Ethical approval needed/obtained for study Not reported Study dates July 2011 to January 2014 |
|
| Participants |
ITT population: Population description Adults with SBMA Age Not reported for total randomised population Sex Not reported for total randomised population Setting Bethesda, MD, USA Inclusion criteria Male; aged > 18 years; genetically confirmed SBMA; an AMAT5 score of 14–41 Exclusion criteria (in supplementary information) Medical condition which would preclude exercise such as COPD, congestive heart failure, and cardiac arrhythmias; presence of an additional comorbid condition such as stroke, myopathy, or radiculopathy which also resulted in weakness; beginning a separate exercise programme involving ≥ 2 weekly sessions of 20 minutes of exercise each within 2 months of start of trial Method of recruitment of participants Not reported Informed consent obtained Not reported Total number randomised 54 Clusters Not applicable See Description of studies for more information on study participants in the context of physical activity promotion. |
|
| Interventions | For 12 weeks
Description of support provided: the exercise programmes were designed by physical therapists familiar with SBMA and taught by physical therapy staff. It was unclear whether exercise was supervised, or completed individually or as a group. All participants had regular telephone or video calls to ensure compliance and intervention fidelity. There were no other co‐interventions reported. Minimum intervention compliance for inclusion in the study was defined as (quote) "80% of the telephone contact forms and other communications and 85% of the assigned exercise sessions." |
|
| Outcomes |
Primary
Secondary
Follow‐up outcomes after 12 weeks included in results Outcomes in bold of interest to this review. See Description of studies for more information on physical activity outcome measurement in the context of physical activity promotion. |
|
| Notes | Final scores reported (after intervention). Mean change scores also reported but with no measure of variability. Adverse event data were not presented in a usable format (adverse events reported by > 10% of participants in either group) Source of funding Intramural research funds from the National Institute of Neurological Disorders and Stroke. Conflicts of interest No study‐related conflicts of interest in relation to the review question. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Subjects were randomly assigned to either an intervention group that performed a functional exercise program or a control group that performed a stretching program." |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "[Participants] were taught by unblinded physical therapy staff;" low risk of bias due to the nature of intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "evaluator‐blinded." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Although dropouts were clearly reported for the primary outcome, there were missing data for 4 additional participants (17%) in the functional exercise group and 3 additional participants (12%) in the control group without explanation. Adverse events were also reported incompletely. |
| Selective reporting (reporting bias) | Low risk | None identified. |
| Other bias | Low risk | None identified. |
Van Groenestijn 2019.
| Study characteristics | ||
| Methods |
Aim To determine the effectiveness of aerobic exercise therapy plus usual care compared with usual care alone on disease‐specific and generic health‐related quality of life in ambulatory people with early‐stage ALS. Design Parallel RCT Unit of allocation By individuals Ethical approval needed/obtained for study Yes (study protocol was approved by the Medical Ethics Committee of the University Medical Center Utrecht) Study dates Screening from 26 February 2010 to 1 January 2015 |
|
| Participants |
ITT population: Population description Ambulatory adults with ALS Age Mean age 60.9 years (SD 10.0) in the exercise group and 59.9 years (SD 10.7) in the usual care group (randomised population) Sex 67% male randomised to aerobic exercise therapy and 73% male randomised to usual care Setting Multi‐centre, the Netherlands. Home‐based and centre‐based intervention Inclusion criteria Aged 18–80 years; FVC ≥ 80%; possible, laboratory‐supported probable, probable, or definite ALS according to the revised version of the El Escorial criteria; diagnostic phase completed; life expectancy > 1 year; ability to walk with or without walking aid (≥ 10 minutes); ability to cycle on a cycle ergometer (≥ 15 minutes) Exclusion criteria People who already exercised (≥ 2 hours a week) because the treatment effect was expected to be minimal; severe cognitive impairment (whether or not related to ALS, preventing completion of the aerobic exercise therapy), disabling comorbidity, and psychiatric disorder, all assessed using the Cumulative Illness Rating Scale; insufficient proficiency in the Dutch language. Method of recruitment of participants Consecutive patients were screened at 5 rehabilitation centres or rehabilitation departments of academic hospitals in the Netherlands Informed consent obtained Yes Total number randomised 57 Clusters Not applicable See Description of studies for more information on study participants in the context of physical activity promotion. |
|
| Interventions | For 16 weeks
Description of support provided: participants in the exercise group undertook a combination of home‐based training and individually supervised training by a specially trained physical therapist at a rehabilitation unit. Both the exercise and control group participants received usual care, which consisted of neuropalliative, secondary care provided by a multi‐disciplinary team. Most participants (73%) received concomitant treatment with riluzole. The study did not limit participants' everyday physical activity in either group. |
|
| Outcomes |
Primary
Secondary
Follow‐up outcomes after 6 months included in results Outcomes in bold of interest to this review. See Description of studies for more information on physical activity outcome measurement in the context of physical activity promotion. |
|
| Notes | Slope scores reported for monthly changes per outcome. Protocol deviation:physical activity in MET per day (estimated with the LASA Physical Activity Questionnaire) was a prespecified outcome measure that was subsequently removed because "patients failed to complete it adequately." Study investigators also removed the ÅR test at follow‐up because of a diminished feasibility of the ÅR test. Sources of funding The Netherlands Organization for Health Research and Development (ZonMw) and the Prinses Beatrix Spierfonds. Conflicts of interest No study‐related conflicts of interest in relation to the review question. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was performed centrally by an investigator (JHV) not involved in testing or treatment… according to the minimization method." |
| Allocation concealment (selection bias) | Low risk | Randomisation was performed centrally by an investigator not involved in testing or treatment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Patients and intervention physiotherapists could not be masked to group allocation because the intervention involved attendance at appointments and home exercises, but allocation was masked from data entry researchers and from the trial statistician (RPAvE) until the database had been closed." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "assessor‐blinded… The assessors who performed the outcome assessments were blinded to the group allocation." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | There were missing data for adverse events in the usual care arm. |
| Selective reporting (reporting bias) | High risk | The availability of adverse event data was not specified for each arm of the study. (In terms of selective non‐reporting (quote) "Deviations from the original protocol were removal of the LAPAQ questionnaire, because patients failed to complete it adequately." In addition, on review of the study protocol, a CBT group plus usual care was not reported in the results). |
| Other bias | Low risk | None identified. |
Voet 2014.
| Study characteristics | ||
| Methods |
Aim To investigate the effect of aerobic exercise training and CBT on chronic fatigue in people with FSHD. Design Parallel RCT Unit of allocation By individuals Ethical approval needed/obtained for study Yes (study protocol was approved by the regional medical ethics committee and by each institution's local committee) Study dates Enrolment from January 2009 to February 2012 |
|
| Participants |
ITT population: Population description Adults with FSHD Age Median age 59 years (range 21–68) in the exercise group, 49 years (range 24–69) in the CBT group, and 52 years (range 20–79) in the usual care group (randomised population) Sex 60% male randomised to aerobic exercise training; 62% male randomised to CBT; and 71% male randomised to usual care Setting At 9 healthcare institutions, the Netherlands Inclusion criteria Diagnosis of FSHD type 1 had to be confirmed by DNA testing; aged ≥ 18 years; severe fatigue (CIS‐Fatigue ≥ 35); able to walk independently (ankle‐foot orthoses and canes accepted); able to exercise on a bicycle ergometer; able to complete either type of intervention Exclusion criteria Cognitive impairment; insufficient mastery of the Dutch language; neurological or orthopaedic comorbidity interfering with the interventions or possibly influencing outcomes; pregnancy; use of psychotropic drugs (except simple sleeping medication); severe cardiopulmonary disease (chest pain, arrhythmia, pacemaker, cardiac surgery, severe exertional dyspnoea, emphysema); epileptic seizures; poorly regulated diabetes mellitus or hypertension; clinical depression, as diagnosed with the BDI‐Primary Care Method of recruitment of participants All adults with FSHD who participated in any previous study at the centre, who were registered in a Dutch neuromuscular database, or who participated in a patient support organisation were invited. Informed consent obtained Yes Total number randomised 57 Clusters Not applicable See Description of studies for more information on study participants in the context of physical activity promotion. |
|
| Interventions | For 16 weeks
Description of support provided: the participants in the exercise group undertook home‐based training and exercise individually supervised by a physical therapist. Similarly to Van Groenestijn 2019, CBT was delivered by a cognitive behavioural therapist and involved individually tailored provision of standard modules relating to fatigue, including deregulation of physical activity. Both intervention groups and a third group of participants received usual care. Occasional physiotherapy was permitted and the study did not limit participants' everyday physical activity in any group. |
|
| Outcomes |
Primary
Secondary
Outcomes in bold of interest to this review. See Description of studies for more information on physical activity outcome measurement in the context of physical activity promotion. |
|
| Notes | Final scores reported as median and range (outcome data were not reported in a usable way). Estimated mean change and 95% CI were also reported but included intervention following a 2nd randomisation of participants in the usual care group to aerobic exercise or CBT. Due to the amalgamation of participants from the usual care group into the intervention arms, we decided not to use these data. Sources of funding Prinses Beatrix SpierFonds (The Dutch Public Fund for Neuromuscular Disorders), the Netherlands Organisation for Health Research and Development (ID: ZonMW 89000003), and the FSHD Global Research Foundation. Conflicts of interest No study‐related conflicts of interest in relation to the review question. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "An independent research assistant allocated each participant to 16 weeks of AET [aerobic exercise training], CBT, or UC [usual care] using a computer‐generated randomization block list. The block sizes varied randomly in order to prevent predictability of the allocation process." |
| Allocation concealment (selection bias) | Low risk | Quote: "computer‐generated randomization block list." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Low risk of bias due to the nature of intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "assessor‐blinded… All measurements were performed at the Radboud University Medical Center by 2 blinded physical therapists." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | There were incomplete outcome data for physical activity without explanation (20% missing data for actometry in aerobic exercise training group). Also, adverse events were reported incompletely for the usual care group. |
| Selective reporting (reporting bias) | Low risk | None identified. |
| Other bias | Low risk | None identified. |
Wallace 2019.
| Study characteristics | ||
| Methods |
Aim There were 3 stated aims of this study 1. calculate the effect of training on aerobic capacity; 2. ascertain whether supported aerobic training in community leisure facilities is feasible, safe, and acceptable; 3. explore secondary physical and non‐physical effects of exercise in people with CMT and IBM. Design Cross‐over RCT Unit of allocation By individual Ethical approval needed/obtained for study Yes (this study achieved National Health Service National Research Ethics Service ethical approval) Study dates Recruitment took place over a 26‐month period before 2017 |
|
| Participants |
ITT population: Population description Adults with CMT type 1A and IBM Age Not reported for total randomised population Sex Not reported for total randomised population Setting Exercise intervention was based at a local community gym, UK Inclusion criteria Clinical and genetic diagnosis of CMT type 1A, or a clinical diagnosis of IBM, supported by histological confirmation as per the established Griggs criteria (only Griggs‐definite IBM cases were included); aged 18–80 years; able to walk for 30 m with or without a walking aid or orthotic devices; able to safely mount and dismount an exercise bike unaided or with minimal assistance; signed informed participant consent Exclusion criteria Presence of other significant neurological disorders or major comorbidities; limb surgery during the 6 months prior to screening (or planned before final assessment); failure to pass the screening assessment for exercise testing; aged > 80 years or < 18 years; concurrent involvement in another intervention trial; people already participating in moderate‐to‐vigorous aerobic exercise > 3 times per week; women of childbearing age if they were pregnant or planning to become pregnant during the study Method of recruitment of participants Potential participants were recruited from clinics and research databases of the National Hospital for Neurology and Neurosurgery, London, UK, plus national clinics of colleagues from the British Myology Society for people with IBM Informed consent obtained Yes Total number randomised CMT group: 28; IBM group: 17; total: 45 Clusters Not applicable See Description of studies for more information on study participants in the context of physical activity promotion. |
|
| Interventions | For 12 weeks
Description of support provided: the exercise intervention was facilitated at community gyms and supported by professionally qualified fitness instructors. They received a training manual and joined an initial exercise induction with the participant and a research physical therapist. Training was completed individually with scheduled supervisory support from the fitness instructor, a midway visit from the physical therapist, and 2‐weekly telephone contacts from the physical therapist. Quote: "Extra calls or visits were made where either the participant or the fitness instructor identified a need for more support." Participants in the control group were asked to maintain prestudy levels of physical activity. They received monthly telephone contact from the research physiotherapist, which included review of their general activity. Both the exercise and control groups also recorded their exercise and activity in a diary. No other co‐interventions were reported. |
|
| Outcomes |
Primary
Secondary
Outcomes in bold of interest to this review. See Description of studies for more information on physical activity outcome measurement in the context of physical activity promotion. |
|
| Notes | Overall final scores (combined 1st and 2nd period after intervention) reported, but outcome data were not reported in a usable way, as per the protocol (1st period after intervention only). Adverse events were not reported as such, although safety monitoring included serum creatine kinase levels and self‐reported energy, mood and fatigue using the VAS in diaries. Additional unpublished data for accelerometry and quality of life measures were sought for the 1st period of the cross‐over study but these were not available at the time of review development. Unpublished 1st period data were not sought for the IPAQ because the published outcome measure from this questionnaire related to sitting time only. Source(s) of study funding NIHR Research for Patient Benefit Award PB‐PG‐0711‐25151 (Chief Investigator: GMR) Conflicts of interest No study‐related conflicts of interest in relation to the review question (note: 2 review authors were involved in this study). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A block randomization method was used to allocate participants to groups. Block sizes of 4 were used based on random numbers generated in MATLAB (Mathworks, Cambridge, UK). The random block sequences were stored on a password‐protected spreadsheet." |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation to the groups was input and spreadsheets held by an unblinded member of staff who were not involved in screening, recruitment, assessment, or training of the participants. This ensured allocation was concealed after enrolment and consent." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Low risk of bias due to the nature of intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "single‐blinded… Blinding of assessors." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Physical activity data were not reported immediately before and after each period of the cross‐over study. Quote: "Missing data postintervention were imputed using a missing at random assumption." Comment: however it is unclear what proportion of missing data in each of the arm study related to the first period of the trial. |
| Selective reporting (reporting bias) | Unclear risk | The methods reported use of the IPAQ but did not specify sitting time as the outcome, although results from the questionnaire were only reported for sitting time. In terms of the timing of activity monitoring, this was reported as post‐training and elsewhere as at the end of the trial but participants completed training at different stages of the cross‐over study. |
| Other bias | Low risk | None identified. |
White 2016.
| Study characteristics | ||
| Methods |
Principal research question (in protocol) Is a tailored home exercise programme more effective in reducing disability (activity limitation) than advice about exercise and usual care in people with IN? Design Parallel RCT Unit of allocation By individual Ethical approval needed/obtained for study Yes (study was reviewed and approved by the London City & East NRES committee) Study dates Not reported |
|
| Participants |
ITT population: Population description (in protocol or abstract) Adults with IN Age Not reported Sex Not reported Setting Home‐based exercise intervention, UK Inclusion criteria (in protocol) Adults with stable motor neuropathy, with or without sensory neuropathy, as a result of GBS, CIDP or PDN diagnosed using established criteria (and where PDN was defined as the combination of demyelinating neuropathy, serum antibodies to myelin‐associated glycoprotein, and an immunoglobulin M monoclonal gammopathy with no evidence of haematological malignancy); able to walk 10 m, with or without walking aids; ≥ 1 year since onset if they have GBS; no change in self‐reported disability, immunotherapy, or medication for neuropathic pain in the previous 6 months (excepting medication dose of azathioprine, which must not have changed for 12 months). Patients receiving regular IVIg or plasma exchange were assessed at same time points after treatment to avoid fluctuations due to time since last treatment. Minor alterations to IVIg therapy in the lead‐up to the project were allowed. ≤ 10% change in mean weekly dose allowed in the 3 months prior to trial entry, and a change of ≤ 20% in previous 6 months. If patients had received greater changes, they were able to take part but must have waited until they met these criteria; participants should not have received physiotherapy in the 6 months prior to entering the study. Once in the trial, patients could receive additional physiotherapy for other unrelated musculoskeletal problems if necessary, but where possible this should have been postponed, at least until after the 12‐week intervention phase; able to understand spoken or written (or both) English and to communicate responses to questionnaires Exclusion criteria (in protocol) People scoring 0 on the ONLS or 1 on the upper limb scale alone (as this would reflect sensory symptoms not affecting function); any other unstable medical conditions that 1. affected activity limitation, 2. prevented them from exercising, or 3. would have made it unsafe to exercise; pregnancy; adults unable to consent for themselves Method of recruitment of participants (in protocol) From 2 main sources: patients attending selected specialist peripheral nerve clinics in the South East and West Midlands of England and people with IN who accessed the Guillain‐Barré syndrome and Associated Inflammatory Neuropathy (GAIN) charity website or newsletter Informed consent obtained Not reported in abstract Total number randomised 58 Clusters Not reported in abstract See Description of studies for more information on study participants in the context of physical activity promotion. |
|
| Interventions | For 12 weeks
Description of support provided: information not available. The study protocol planned for home exercise to be prescribed by a study physical therapist. Following demonstration and practice, the participants in the exercise group were to continue the programme individually with ≥ 3 scheduled telephone contacts from the physical therapist. In addition, participants would be asked to record an exercise diary. In the control group, participants were to receive written guidance, information, and advice on exercise and activity but no contact with the study physical therapist. Both groups would receive standard care, including "pharmacological, physical or other therapy interventions," although participants would be asked to avoid additional physiotherapy specifically for IN. |
|
| Outcomes |
Outcomes in bold of interest to this review. See Description of studies for more information on physical activity outcome measurement in the context of physical activity promotion. |
|
| Notes | Unpublished outcome data were sought but not available at the time of review development. The study protocol specified the following outcome measures: Primary outcome at baseline, after 12 weeks, and at 12 months' follow‐up Activity limitation assessed using the Rasch Overall Disability Scale Secondary outcomes at baseline, after 12 weeks, and at 12 months' follow‐up
For evaluating cost‐effectiveness: CSRI and the EQ‐5D at baseline and 12‐month follow‐up Qualitative assessment on a subset of participants Sources of funding GBS/CIDP International also known as GAIN charity (Guillain‐Barré and Associated Inflammatory Neuropathies, UK support group, ref: GBS2011/8). Additional funding support was received from London South CLRN contingency funds. Conflicts of interest No study‐related conflicts of interest in relation to the review question. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomised." |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to judge from abstract. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Low risk of bias due to the nature of intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "observer blind." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to judge from abstract. |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to judge from abstract. |
| Other bias | Unclear risk | Insufficient information to judge from abstract. |
2MWT: 2‐Minute Walk Test; 5STS: 5‐times‐sit‐to‐stand test; 6MWT: 6‐Minute‐Walk Test; ALCOS: Algemene Competentieschaal; ALS: amyotrophic lateral sclerosis; ALSAQ‐40: Amyotrophic Lateral Sclerosis Assessment Questionnaire; ALSFRS‐R: ALS Functional Rating Scale; AMAT: Adult Myopathy Assessment Tool; BDI: Beck Depression Inventory; BMI: body mass index; CBT: cognitive behavioural therapy; CI: confidence interval; CIDP: chronic inflammatory demyelinating polyradiculoneuropathy; CIS: Checklist Individual Strength; CISS: Coping Inventory for Stressful Situations; CMT: Charcot‐Marie‐Tooth disease type 1A; COPD: chronic obstructive pulmonary disease; DM1: myotonic dystrophy type 1; CSRI: Client Services Receipt Inventory; DPN: diabetic peripheral neuropathy; EARS: Exercise Adherence Rating Scale; EQ‐5D: EuroQol; FSHD: facioscapulohumeral muscular dystrophy; FVC: forced vital capacity; GBS: Guillain‐Barré syndrome; HADS: Hospital Anxiety and Depression Scale; HIT: high‐intensity interval training; IBM: inclusion body myositis; IBMFRS: Inclusion Body Myositis Functional Rating Scale; ICD: implantable cardioverter‐defibrillator; IN: stable inflammatory immune‐mediated neuropathy; IPAQ: International Physical Activity Questionnaire; IPQ: Illness Perceptions Questionnaire; ITT: intention to treat; IVIg: intravenous immunoglobulin; MET: metabolic equivalent task; n: number; NHP: Nottingham Health Profile; NMD: neuromuscular disease; ONLS: Overall Neuropathy Limitations Scale; PDN: paraproteinaemic demyelinating neuropathy; PPS: postpolio syndrome; QMA: Quantitative Muscle Assessment; RCT: randomised controlled trial; RFSS: Rasch‐modified Fatigue Severity Scale; SBMA: spinal and bulbar muscular atrophy; SD: standard deviation; SEE: Self‐Efficacy for Exercise; SF‐12: 12‐item Short Form Survey; SF‐36: 36‐item Short Form Survey; SIP: Sickness Impact Profile; SNIP: sniff nasal inspiratory pressure; STS: sit‐to‐stand; TUG: Timed‐Up‐and‐Go; VAS; Visual Analogue Scale; VO2max: maximal oxygen uptake; VO2peak: peak oxygen uptake; Wmax: maximal workload.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adams 2019 | Physical activity not reported as an outcome measure as per the review protocol. |
| Ahlstrom 2006 | Not an RCT. |
| Alemdaroglu 2015 | Physical activity not reported as an outcome measure as per the review protocol. |
| Andrews 2018 | Physical activity not reported as an outcome measure as per the review protocol. |
| Armon 2008 | Commentary only. |
| Bauer 2017 | Physical activity not reported as an outcome measure as per the review protocol. |
| Bauer 2018 | Physical activity not reported as an outcome measure as per the review protocol. |
| Bogdanovic 2015 | Physical activity not reported as an outcome measure as per the review protocol. |
| Buch 2015 | Physical activity not reported as an outcome measure as per the review protocol. |
| Cazares Miranda 2017 | Physical activity not reported as an outcome measure as per the review protocol. |
| Cejudo 2000 | Physical activity not reported as an outcome measure as per the review protocol. |
| Cejudo‐Ramos 2000 | Physical activity not reported as an outcome measure as per the review protocol. |
| Chetlin 2004a | Physical activity not reported as an outcome measure as per the review protocol. |
| Chetlin 2004b | Physical activity not reported as an outcome measure as per the review protocol. |
| Connolly 2015 | Physical activity not reported as an outcome measure as per the review protocol. |
| Drory 2001a | Physical activity not reported as an outcome measure as per the review protocol. |
| Drory 2001b | Physical activity not reported as an outcome measure as per the review protocol. |
| Evans 1984 | Not an RCT. |
| Favejee 2015 | Not an RCT. |
| Flannery 2014 | Physical activity not reported as an outcome measure as per the review protocol. |
| Gagnon 2018 | Commentary only. |
| Ghavami 2018 | Physical activity not reported as an outcome measure as per the review protocol. |
| Henke 2012 | No reporting of participants with neuromuscular disease. |
| Katz 2004 | Commentary only. |
| Khan 2011 | Physical activity not reported as an outcome measure as per the review protocol. |
| Kierkegaard 2011 | Physical activity not reported as an outcome measure as per the review protocol. |
| Kierkegaard 2012 | Not an RCT. |
| Kitano 2018 | Not an RCT. |
| Kleckner 2016 | Physical activity not reported as an outcome measure as per the review protocol. |
| Kluding 2017 | Protocol only for a RCT. Activity monitoring is reported as part of intervention but physical activity is not specified as an outcome measure. |
| Landon‐Cardinal 2018 | Not an RCT. |
| Landon‐Cardinal 2019 | Not an RCT. |
| Lehmann 1994 | Not an RCT. |
| Longstreth 1998 | Not an RCT. |
| Lustenhouwer 2019 | Protocol for a RCT. No physical activity outcome measure reported as per the review protocol. |
| Mishra 2012 | Not an RCT. |
| Monini 2017 | Physical activity not reported as an outcome measure as per the review protocol. |
| Mori 2016 | Physical activity not reported as an outcome measure as per the review protocol. |
| Mori 2017 | Physical activity not reported as an outcome measure as per the review protocol. |
| Mosforth 1958 | Not an RCT. |
| Oksuz 2011 | Physical activity not reported as an outcome measure as per the review protocol. |
| Otterman 2011 | Not an RCT. |
| Ozalevli 2004 | No reporting of participants with neuromuscular disease. |
| Phillips 2009 | Not an RCT. |
| Phillips 2012 | Physical activity not reported as an outcome measure as per the review protocol. |
| Ramdharry 2012 | Not an RCT. |
| Rideau 1995 | Physical activity not reported as an outcome measure as per the review protocol. |
| Schenone 2010 | Physical activity not reported as an outcome measure as per the review protocol. |
| Schenone 2015 | Physical activity not reported as an outcome measure as per the review protocol. |
| Schonsteiner 2015 | Physical activity not reported as an outcome measure as per the review protocol. |
| Scott 1981 | Physical activity not reported as an outcome measure as per the review protocol. |
| Sendhilkumar 2013 | Physical activity not reported as an outcome measure as per the review protocol. |
| Spencer 2016 | Physical activity not reported as an outcome measure as per the review protocol. |
| Terpstra Lindeman 1992 | Physical activity not reported as an outcome measure as per the review protocol. |
| Tomas 2011 | Physical activity not reported as an outcome measure as per the review protocol. |
| Van Puymbroeck 2016 | Not an RCT. |
| Veenhuizen 2015 | Physical activity not reported as an outcome measure as per the review protocol although different types of social activity engagement reported as an outcome measure. |
| Veenhuizen 2019 | Physical activity not reported as an outcome measure as per the review protocol although different types of social activity engagement reported as an outcome measure. |
| Wiesinger 1998 | Extension following on from an RCT and physical activity not reported as an outcome measure as per the review protocol. |
| Zhang 2005 | Not an RCT. |
| Zilliox 2018 | Physical activity not reported as an outcome measure as per the review protocol. |
| Zilliox 2019 | Physical activity not reported as an outcome measure as per the review protocol. |
RCT: randomised controlled trial.
Characteristics of studies awaiting classification [ordered by study ID]
ChiCTR‐IPR‐15006127.
| Methods | Randomised, parallel intervention |
| Participants | Adults with DPN |
| Interventions | Peer support and health education compared with health education only |
| Outcomes |
Primary Physical activity Exercise self‐efficacy Secondary Depression Social support Glycated haemoglobin |
| Notes | Estimated study completion date: August 2015 Registry record accessed on 5 May 2021 |
NCT00866112.
| Methods | RCT |
| Participants | Adults who use wheelchairs including those living with muscular dystrophy |
| Interventions | Intervention group: physical activity consisting of educational session, goal setting, and self‐monitoring of daily engagement in physical activity Minimal contact control group: self‐guided education manual about adopting physical activity and self‐monitor daily engagement in physical activity |
| Outcomes |
Primary
Secondary
|
| Notes | Actual study completion date: June 2012 Registry record accessed on 5 May 2021 Associated publication considered in the Discussion (Nary 2011). |
DPN: diabetic peripheral neuropathy; RCT: randomised controlled trial.
Characteristics of ongoing studies [ordered by study ID]
ACTRN12617000543381.
| Study name | Do different shoe insole surfaces affect balance and walking in adults with diabetes and foot nerve damage? |
| Methods | RCT |
| Participants | Adults with diabetic peripheral neuropathy |
| Interventions | Textured insoles compared with smooth, control insoles |
| Outcomes |
Primary
Secondary
|
| Starting date | November 2017 |
| Contact information | Principal Investigator: Dr Anna Hatton, School of Health and Rehabilitation Sciences Therapies Building (84A), The University of Queensland, St Lucia, Brisbane, QLD 4072, Australia Telephone: +61733654590 Email: a.hatton1@uq.edu.au |
| Notes | Anticipated last data collection: September 2020 Registry record accessed on 5 May 2021 |
NCT02089880.
| Study name | Comparing functional outcomes in individuals using micro‐processor controlled orthosis versus stance control orthosis |
| Methods | Cross‐over RCT |
| Participants | Adults with lower extremity functional impairment due to neurological or neuromuscular disease, orthopaedic disease, or trauma |
| Interventions | Training with a micro‐processor controlled orthosis compared to training with a stance control orthosis |
| Outcomes |
Primary
Secondary
Other
|
| Starting date | February 2014 |
| Contact information | Arun Jayaraman, Research Scientist, Shirley Ryan AbilityLab, USA |
| Notes | Estimated study completion date: December 2021 Registry record accessed on 5 May 2021 |
NCT02790931.
| Study name | Effects of foot muscle strengthening in daily activity in diabetic neuropathic patients |
| Methods | RCT |
| Participants | Adults with diabetic polyneuropathy |
| Interventions | Control group: recommended foot care by international consensus with no exercises Intervention group: 12‐week physical therapy exercises, twice a week, under the supervision of a physiotherapist, and twice a week being remotely supervised by a software at home |
| Outcomes |
Primary
Secondary
|
| Starting date | August 2016 |
| Contact information | Principal Investigator: Isabel CN Sacco, Associate Professor at São Paulo University |
| Notes | Study completion date: December 2020 Registry record accessed on 5 May 2021 |
NCT03515356.
| Study name | Exercise to reduce chemotherapy‐induced peripheral neuropathy |
| Methods | RCT |
| Participants | Adults living with chemotherapy‐induced peripheral neuropathy |
| Interventions | Intervention: motivational enhancement therapy and home‐based aerobic walking intervention Control: a physical activity education pamphlet only |
| Outcomes |
Primary
Secondary
Other
|
| Starting date | June 2018 |
| Contact information | Principal Investigators: Grace Kanzawa‐Lee and Ellen M Lavoie Smith, University of Michigan School of Nursing |
| Notes | Actual study completion date: June 2019 Registry record accessed on 5 May 2021 |
NCT03531788.
| Study name | Use of dynamic arm supports to promote activities of daily living in individuals with DMD |
| Methods | RCT |
| Participants | Boys and men aged ≥ 14 years who are non‐ambulant, wheelchair users with DMD |
| Interventions | Intervention: actively assisted mechanical arm support (electric powered to balance arm; the Armon Ayura dynamic arm support) Control: passive mechanical arm support (elastic bands to balance arm; JAECO WREX) |
| Outcomes |
Primary
Secondary
|
| Starting date | August 2018 |
| Contact information | Not reported |
| Notes | Study completion date: December 2020 Registry record accessed on 5 May 2021 |
6MWT: 6‐Minute Walk Test; DMD: Duchenne muscular dystrophy; EORTC QLQ‐C30: European Organisation of Research and Treatment of Cancer Quality of Life Questionnaire; EORTC QLQ‐CIPN20: European Organisation of Research and Treatment of Cancer Quality of Life Questionnaire Chemotherapy‐Induced Peripheral Neuropathy Scale; GPS: Global Positioning System; MITI: Motivational Interviewing Treatment Integrity Code; RCT: randomised controlled trial; WHOQOL‐BREF: World Health Organization Quality of Life, brief form.
Differences between protocol and review
We considered studies potentially eligible for inclusion if they involved a subset of participants with NMD. During screening, we limited eligible study populations with a subset of participants with NMD to those study populations with neurological disorders, including a subset of participants with NMD. Our rationale for making this protocol deviation was that inclusion of an analysable subgroup with NMD was less likely to be reported in the study title or abstract for a population not focused on people with neurological disorders. Due to the large volume of search results, we found that our search needed to be more targeted for both relevancy and logistical feasibility.
In addition to hospitalisation and all‐cause death, we included available data on serious adverse events as defined by one study as 'serious adverse events'.
We prioritised the reporting of final scores over change scores reported in one study because the change scores were adjusted and not available for all time points in the study.
We planned to search reference lists of included studies but did not do so because of the limited specificity in study eligibility criteria based on titles alone.
We undertook a second round of screening of titles and abstracts after discussion of the first round results between the review authors screening records in Covidence.
We revised the allocation of review tasks to named review authors in line with review author availability during the COVID‐19 pandemic.
Study characteristics were extracted by more than one author (KJ) to assist dual, independent risk of bias assessments.
The first author (KJ) contributed to data extraction and assessment from one study (Wallace 2019) despite involvement, due to constraints on co‐author availability during the COVID‐19 pandemic. This study was not included in the quantitative analysis.
Data were entered into RevMan Web (RevMan Web 2020), as well as Review Manager 5 software (Review Manager 2020).
We planned to consider all outcomes separately for risk of bias assessment as some domains may have different risks of bias for different outcomes, but we presented assessments at the study level with reference to outcomes of specific relevance to the review.
We removed one prespecified subgroup analysis for comparing general health visits with other interventions designed to promote physical activity because we would have considered this as a main comparison.
In the summary of findings tables, we included any measure of total time spent in physical activity (i.e. using an activity monitor or self‐reported measure).
In the summary of findings tables, we decided to include multiple time points for outcomes in the absence of a single, appropriate length of follow‐up in people with different types of NMD.
In the summary of findings tables, we decided to include adverse events and any serious adverse events instead of adverse events leading to study discontinuation because of the limited adverse event data available.
Contributions of authors
KJ drafted the protocol and JB, GG, FH, DGJ, JM, JN, GR, and DMT contributed to the development of the protocol.
All contributed to review planning, resolved unforeseen issues, and oversaw review completion.
KJ, FH, and JN screened studies for inclusion.
KJ, FH, JN, JM, and GR completed data extraction, risk of bias assessment, and GRADE assessment
KJ drafted the review and JB, GG, FH, DGJ, JM, JN, GR, and DMT contributed to author discussions and development of the review.
DMT provided executive direction.
GR and KJ oversaw contact with study investigators and responses to peer review.
All review authors agreed on the final text.
Sources of support
Internal sources
Not applicable, UK
External sources
-
NIHR Newcastle Biomedical Research Centre, UK
Support for Jane Newman, Grainne Gorman
-
Wellcome Centre for Mitochondrial Research (203105/Z/16/Z), Newcastle University Centre for Ageing and Vitality (supported by the Biotechnology and Biological Sciences Research Council and Medical Research Council [G016354/1]), UK NIHR Biomedical Research Centre for Ageing and Age‐Related Disease award to the Newcastle upon Tyne Hospitals National Health Service (NHS) Foundation Trust, and the UK NHS Specialist Commissioners, which funds the Rare Mitochondrial Disorders of Adults and Children Diagnostic Service in Newcastle upon Tyne, UK
Support for Douglass Turnbull
-
NIHR University College London Hospitals Biomedical Research Centre, UK
Support for Gita Ramdharry
Declarations of interest
KJ: employed as a Research Physiotherapist during 2015 to 2016 for one of the included studies (Wallace 2019). She is currently the NIHR Network Support Fellow for the Cochrane Acute and Emergency Care Network, and previously for the Cochrane Mental Health and Neuroscience Network (2019 to 2021).
FH: none. She is a podiatrist and member of the Australian Podiatry Association.
JN: none. She was involved in Okkersen 2018. This study was funded by the European Union Seventh Framework Program, under grant agreement number 305697 (the Observational Prolonged Trial In Myotonic dystrophy type 1 to Improve quality of life Standards, a Target Identification Collaboration (OPTIMISTIC) project).
JM: none.
JB: receives research funding from NIH (National Institute of Neurological Diseases and Stroke and National Center for Advancing Translational Sciences, Inherited Neuropathies Consortium, Rare Disease Clinical Research Network #2U54NS065712), Charcot‐Marie Tooth Association of Australia, Charcot‐Marie Tooth Association (USA), Diabetes Australia, Multiple Sclerosis Research Australia, Sydney Southeast Asia Centre, New Zealand Neuromuscular Research Foundation Trust, Elizabeth Lottie May Rosenthal Bone Bequest and Perpetual Limited. Consultancies: Acceleron Pharma (September 2016). He is a registered podiatrist working at The Children's Hospital at Westmead, Australia.
DGJ: none.
GG: none.
DMT: our work was supported by The Wellcome Trust Centre for Mitochondrial Research (906919), the Newcastle University Centre for Brain Ageing and Vitality supported by Biotechnology and Biological Sciences Research Council, Engineering and Physical Sciences Research Council, Economic and Social Research Council, and Medical Research Council as part of the cross‐council Lifelong Health and Wellbeing Initiative (G0700718). Consultancies: Imel Therapeutics and Nanna Therapeutics. Scientific Advisory board memberships: Pretzel Therapeutics and Khondrion.
GR: was principal investigator in Wallace 2019, supported by the National Institute for Health Research (NIHR Research for Patient Benefit funding stream, Grant reference PB‐PG 0711‐25151) and University College London Hospitals Biomedical Research Centre. CSL Behring organised and funded her travel and accommodation at the Peripheral Nerve Society meeting in Baltimore 2018. She has published an opinion piece on targeting the sedentary behaviour epidemic in neurological disease. She is a Consultant Allied Health Professional working with people with neuromuscular disease and a committee member of the British Myology Society (unpaid).
Mental Health and Neuroscience Network to 31 March 2021
Edited (no change to conclusions)
References
References to studies included in this review
Andersen 2015 {published data only}
- Andersen G, Prahm KP, Dahlqvist JR, Citirak G, Vissing J. Aerobic training and postexercise protein in facioscapulohumeral muscular dystrophy: RCT study. Neurology 2015;85(5):396-403. [DOI: 10.1212/WNL.0000000000001808] [DOI] [PubMed] [Google Scholar]
Andersen 2017 {published data only}
- Andersen G, Heje K, Buch AE, Vissing J. High-intensity interval training in facioscapulohumeral muscular dystrophy type 1: a randomized clinical trial. Journal of Neurology 2017;264(6):1099-106. [DOI: 10.1007/s00415-017-8497-9] [DOI] [PubMed] [Google Scholar]
- NCT02156141. High intensity training in patients with spinal and bulbar muscular atrophy. Clinicaltrials.gov/show/NCT02156141 (first received 5 June 2014).
Elsworth 2011 {published data only}
- Elsworth C, Winward C, Sackley C, Meek C, Freebody J, Esser P, et al. Supported community exercise in people with long-term neurological conditions: a phase II randomized controlled trial. Clinical Rehabilitation 2011;25(7):588-98. [DOI: 10.1177/0269215510392076] [DOI] [PubMed] [Google Scholar]
- ISRCTN95992791. Long term individual fitness enablement. www.isrctn.com/ISRCTN95992791 (first received 18 October 2007).
- Winward C, LIFE group. Supporting community-based exercise in long-term neurological conditions: experience from the Long-term Individual Fitness Enablement (LIFE) project. Clinical Rehabilitation 2011;25(7):579-87. [DOI: 10.1177/0269215510392075] [DOI] [PubMed] [Google Scholar]
Grewal 2015 {published data only}
- Grewal GS, Schwenk M, Lee-Eng J, Parvaneh S, Bharara M, Menzies RA, et al. Sensor-based interactive balance training with visual joint movement feedback for improving postural stability in diabetics with peripheral neuropathy: a randomized controlled trial. Gerontology 2015;61(6):567-74. [DOI: 10.1159/000371846] [DOI] [PubMed] [Google Scholar]
Koopman 2016 {published data only}
- Koopman FS, Beelen A, Gerrits KH, Bleijenberg G, Abma TA, Visser M, et al. Exercise therapy and cognitive behavioural therapy to improve fatigue, daily activity performance and quality of life in postpoliomyelitis syndrome: the protocol of the FACTS-2-PPS trial. BMC Neurology 2010;10:8. [DOI: 10.1186/1471-2377-10-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koopman FS, Voorn EL, Beelen A, Bleijenberg G, Visser M, Brehm MA, et al. No reduction of severe fatigue in patients with postpolio syndrome by exercise therapy or cognitive behavioral therapy: results of an RCT. Neurorehabilitation and Neural Repair 2016;30(5):402-10. [DOI: 10.1177/1545968315600271] [DOI] [PubMed] [Google Scholar]
- NTR1371. Exercise therapy and cognitive behavioural therapy in postpoliomyelitis syndrome: effects on fatigue, activities and quality of life. www.trialregister.nl/trial/669 (first received 8 July 2008).
Lemaster 2008 {published data only}
- Kruse RL, Lemaster JW, Madsen RW. Fall and balance outcomes after an intervention to promote leg strength, balance, and walking in people with diabetic peripheral neuropathy: "feet first" randomized controlled trial. Physical Therapy 2010;90(11):1568-79. [DOI: 10.2522/ptj.20090362] [DOI] [PubMed] [Google Scholar]
- Lemaster JW, Mueller MJ, Reiber GE, Mehr DR, Madsen RW, Conn VS. Effect of weight-bearing activity on foot ulcer incidence in people with diabetic peripheral neuropathy: feet first randomized controlled trial. Physical Therapy 2008;88(11):1385-98. [DOI: 10.2522/ptj.20080019] [DOI] [PubMed] [Google Scholar]
- NCT00286598. Feet First: promoting physical activity among people with diabetes mellitus and insensate feet. clinicaltrials.gov/show/NCT00286598 (first received 3 February 2006).
Mueller 2013 {published data only}
- Mueller MJ, Tuttle LJ, Lemaster JW, Strube MJ, McGill JB, Hastings MK, et al. Weight-bearing versus nonweight-bearing exercise for persons with diabetes and peripheral neuropathy: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2013;94(5):829-38. [DOI: 10.1016/j.apmr.2012.12.015] [DOI] [PMC free article] [PubMed] [Google Scholar]
Okkersen 2018 {published data only}
- Jimenez-Moreno AC, Wood L, Lochmuller H, Gorman G. OPTIMISTIC: observational prolonged trial in myotonic dystrophy type 1 to improve quality of life-standards, a target identification collaboration. Neuromuscular Disorders 2015;25(Suppl 1):S40. [Google Scholar]
- Okkersen K, Jimenez-Moreno C, Wenninger S, Daidj F, Glennon J, Cumming S, et al. Cognitive behavioural therapy with optional graded exercise therapy in patients with severe fatigue with myotonic dystrophy type 1: a multicentre, single-blind, randomised trial. Lancet Neurology 2018;17(8):671-80. [DOI: 10.1016/S1474-4422(18)30203-5] [DOI] [PubMed] [Google Scholar]
- Van Engelen B, OPTIMISTIC Consortium. Cognitive behaviour therapy plus aerobic exercise training to increase activity in patients with myotonic dystrophy type 1 (DM1) compared to usual care (OPTIMISTIC): study protocol for randomised controlled trial. Trials 2015;16:224. [DOI: 10.1186/s13063-015-0737-7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shrader 2015 {published data only}
- Shrader JA, Kats I, Kokkinis A, Zampieri C, Levy E, Joe GO, et al. A randomized controlled trial of exercise in spinal and bulbar muscular atrophy. Annals of Clinical and Translational Neurology 2015;2(7):739-47. [DOI: 10.1002/acn3.208] [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Groenestijn 2019 {published data only}
- NTR1616. Aerobic exercise therapy and cognitive behavioural therapy in amyotrophic lateral sclerosis: effects on activities and quality of life. www.trialregister.nl/trial/1545 (first received 6 January 2009).
- Van Groenestijn A, Schroder C, Van Eijk R, Veldink J, Visser-Meily A, Van den Berg LH. Aerobic exercise therapy in patients with amyotrophic lateral sclerosis (FACTS-2-ALS): a randomized clinical trial. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration 2016;17(1):44-5. [Google Scholar]
- Van Groenestijn AC, Schröder CD, Van Eijk RP, Veldink JH, Kruitwagen-van Reenen ET, Groothuis JT, et al. Aerobic exercise therapy in ambulatory patients with ALS: a randomized controlled trial. Neurorehabilitation and Neural Repair 2019;33(2):153-64. [DOI: 10.1177/1545968319826051] [DOI] [PubMed] [Google Scholar]
- Van Groenestijn AC, Van de Port IG, Schröder CD, Post MW, Grupstra HF, Kruitwagen ET, et al. Effects of aerobic exercise therapy and cognitive behavioural therapy on functioning and quality of life in amyotrophic lateral sclerosis: protocol of the FACTS-2-ALS trial. BMC Neurology 2011;11:70. [DOI: 10.1186/1471-2377-11-70] [DOI] [PMC free article] [PubMed] [Google Scholar]
Voet 2014 {published data only}
- Janssen B, Voet N, Geurts A, Van Engelen B, Heerschap A. Quantitative MRI reveals decelerated fatty infiltration in muscles of active FSHD patients. Neurology 2016;86(18):1700-7. [DOI: 10.1212/WNL.0000000000002640] [DOI] [PubMed] [Google Scholar]
- Van Engelen BG, Janssen B, Voet N, Nabuurs C, Padberg GW, Geurts A, et al. Physical activity decreases fatty infiltration in FSHD, a quantitative muscle MR study. Neuromuscular Disorders 2012;22(9-10):896. [Google Scholar]
- Van Engelen BG, Voet N, Janssen B, Bleijenberg G, Hendriks J, De Groot I, et al. Aerobic exercise and cognitive behavior therapy reduce fatigue and slow progression of muscle MR fatty infiltration in FSHD. Neuromuscular Disorders 2014;24(9-10):798-9. [Google Scholar]
- Voet N, Bleijenberg G, De Groot I, Padberg G, Van Engelen B, Geurts A, et al. Both aerobic exercise training and cognitive behavior therapy reduce chronic fatigue in patients with facioscapulohumeral muscular dystrophy: a randomized controlled trial. Annals of Physical and Rehabilitation Medicine 2014;57(Suppl 1):e96. [Google Scholar]
- Voet N, Bleijenberg G, Hendriks J, De Groot I, Padberg G, Van Engelen B, et al. Both aerobic exercise and cognitive-behavioral therapy reduce chronic fatigue in FSHD: an RCT. Neurology 2014;83(21):1914-22. [DOI: 10.1212/WNL.0000000000001008] [DOI] [PubMed] [Google Scholar]
- Voet NB, Bleijenberg G, Hendriks JC, De Groot IJ, Padberg GW, Van Engelen BG, et al. Both aerobic exercise and cognitive-behavioral therapy reduce fatigue in FSHD: an RCT. Nederlands Tijdschrift voor Geneeskunde 2015;159(12):A8806. [DOI] [PubMed] [Google Scholar]
- Voet NB, Bleijenberg G, Padberg GW, Van Engelen BG, Geurts AC. Effect of aerobic exercise training and cognitive behavioural therapy on reduction of chronic fatigue in patients with facioscapulohumeral dystrophy: protocol of the FACTS-2-FSHD trial. BMC Neurology 2010;10:56. [DOI: 10.1186/1471-2377-10-56.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wallace 2019 {published data only}
- Wallace A, Dewar E, Skorupinska M, Laura M, Morrow JM, Sterr A, et al. Evaluating the benefits of community based aerobic training on the physical health and well-being of people with neuromuscular diseases: a pilot study. Journal of the Peripheral Nervous System 2013;18(Suppl 2):S123. [Google Scholar]
- Wallace A, Dewar L, Pietrusz A, Dudziec M, Sterr A, Laura M, et al. Evaluating the benefits of community based aerobic training on the physical health and well-being of people with neuromuscular diseases: a pilot study. Neuromuscular Disorders 2015;25(Suppl 2):S273-4. [Google Scholar]
- Wallace A, Pietrusz A, Dewar E, Dudziec M, Jones K, Hennis P, et al. Community exercise is feasible for neuromuscular diseases and can improve aerobic capacity. Neurology 2019;92(15):e1773-85. [DOI: 10.1212/WNL.0000000000007265] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace A, Pietrusz A, Dewar E, Dudziec M, Jones K, Hennis P, et al. Evaluating the benefits of community based aerobic training on the physical health and well-being of people with Charcot-Marie-Tooth disease type 1A: a pilot randomised controlled trial. Journal of the Peripheral Nervous System 2017;22(3):408. [Google Scholar]
- Wallace A, Pietrusz A, Dewar E, Dudziec M, Jones K, Hennis P, et al. Evaluating the benefits of community based aerobic training on the physical health and well-being of people with Charcot-Marie-Tooth disease type 1A. Journal of the Peripheral Nervous System 2016;21(3):309. [Google Scholar]
- Wallace A, Pietrusz A, Dewar E, Dudziec M, Jones K, Hennis P, et al. Evaluating the benefits of community based aerobic training on the physical health and well-being of people with neuromuscular disease. Muscle & Nerve 2016;54(Suppl 1):S5. [Google Scholar]
White 2016 {published data only}
- White C, Hadden RD, McCrone P, Roberts-Lewis S, Petty J. Observer-blind randomised controlled trial to evaluate the efficacy of a twelve week tailored home exercise programme in the management of inflammatory neuropathy. Journal of the Peripheral Nervous System 2016;21(3):225-6. [Google Scholar]
- White CM, Hadden RD, Robert-Lewis SF, McCrone PR, Petty JL. Observer blind randomised controlled trial of a tailored home exercise programme versus usual care in people with stable inflammatory immune mediated neuropathy. BMC Neurology 2015;15:147. [DOI: 10.1186/s12883-015-0398-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Adams 2019 {published data only}
- Adams AS, Schmittdiel JA, Altschuler A, Bayliss EA, Neugebauer R, Ma L, et al. Automated symptom and treatment side effect monitoring for improved quality of life among adults with diabetic peripheral neuropathy in primary care: a pragmatic, cluster, randomized, controlled trial. Diabetic Medicine 2019;36(1):52-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ahlstrom 2006 {published data only}
- Ahlstrom G, Lindvall B, Wenneberg S, Gunnarsson LG. A comprehensive rehabilitation programme tailored to the needs of adults with muscular dystrophy. Clinical Rehabilitation 2006;20(2):132-41. [DOI] [PubMed] [Google Scholar]
Alemdaroglu 2015 {published data only}
- Alemdaroglu I, Karaduman A, Yilmaz OT, Topaloglu H. Different types of upper extremity exercise training in Duchenne muscular dystrophy: effects on functional performance, strength, endurance, and ambulation. Muscle & Nerve 2015;51(5):697-705. [DOI] [PubMed] [Google Scholar]
Andrews 2018 {published data only}
- Andrews AW, Middleton A. Improvement during inpatient rehabilitation among older adults with Guillain-Barre syndrome, multiple sclerosis, Parkinson disease, and stroke. American Journal of Physical Medicine and Rehabilitation 2018;97(12):879-84. [DOI] [PubMed] [Google Scholar]
Armon 2008 {published data only}
- Armon C. A randomized controlled trial of resistance exercise in individuals with ALS. Neurology 2008;71(11):864-6. [DOI] [PubMed] [Google Scholar]
Bauer 2017 {published data only}
- Bauer V, Wang CH, Goodman N, Craig TL, Glosner S, Juhn M, et al. Text messaging to improve outcomes in patients with painful diabetic peripheral neuropathy (PDPN). Journal of General Internal Medicine 2017;32(2 (Suppl 1)):S328. [Google Scholar]
Bauer 2018 {published data only}
- Bauer V, Goodman N, Lapin B, Cooley C, Wang E, Craig TL, et al. Text messaging to improve disease management in patients with painful diabetic peripheral neuropathy. Diabetes Educator 2018;44(3):237-48. [DOI] [PubMed] [Google Scholar]
Bogdanovic 2015 {published data only}
- Bogdanovic G, Stojanovich L, Djokovic A, Stanisavljevic N. Physical activity program is helpful for improving quality of life in patients with systemic lupus erythematosus. Tohoku Journal of Experimental Medicine 2015;237(3):193-9. [DOI] [PubMed] [Google Scholar]
Buch 2015 {published data only}
- Buch A, Andersen G, Borup Heje Pedersen K, Vissing J. High intensity training in patients with facioscapulohumeral muscular dystrophy. Neuromuscular Disorders 2015;25(Suppl 2):S215. [Google Scholar]
Cazares Miranda 2017 {published data only}
- Cazares Miranda V, Solis Flores L, Granados Rangel MG, Mendoza Hernandez F, Lopez Alvarenga JC. Benefits of personalised nurse counselling in neurological patients. Revista Cientifica de la Sociedad Espanola de Enfermeria Neurologica 2017;46:18-25. [Google Scholar]
Cejudo 2000 {published data only}
- Cejudo P, Ainchez CS, Villagamez R, Bautista J, Montemayor T, Ortega F, et al. Rehabilitation program for mitochondrial myopathies. European Respiratory Journal 2000;16:330s. [Google Scholar]
Cejudo‐Ramos 2000 {published data only}
- Cejudo-Ramos P, Villagomez-Cerrato R, Bautista-Lorite J, Montemayor-Rubio T, Ortega-Ruiz F, Sanchez-Riera H. Application of a rehabilitation program of mitochondrial myopathies. Archivos de Bronconeumologia 2000;36(Suppl 2):18. [Google Scholar]
Chetlin 2004a {published data only}
- Chetlin RD, Gutmann L, Tarnopolsky M, Ullrich IH, Yeater RA. Resistance training effectiveness in patients with Charcot-Marie-Tooth disease: recommendations for exercise prescription. Archives of Physical Medicine and Rehabilitation 2004;85(8):1217-23. [DOI] [PubMed] [Google Scholar]
Chetlin 2004b {published data only}
- Chetlin RD. The Effects of Resistance Training and Oral Creatine Supplementation on Muscle Fiber Morphology, Strength and Activities of Daily Living in Patients with Charcot-Marie-Tooth Disease [dissertation]. Morgantown (WV): West Virginia University, 2004. [Google Scholar]
Connolly 2015 {published data only}
- Connolly B, Thompson A, Douiri A, Moxham J, Hart N. Exercise-based rehabilitation after hospital discharge for survivors of critical illness with intensive care unit-acquired weakness: a pilot feasibility trial. Journal of Critical Care 2015;30(3):589-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
Drory 2001a {published data only}
- Drory VE, Goltsman E, Goldman-Reznick J, Mosek A. The value of muscle exercise in patients with amyotrophic lateral sclerosis. Journal of the Neurological Sciences 2001;187(Suppl 1):S125. [DOI] [PubMed] [Google Scholar]
Drory 2001b {published data only}
- Drory VE, Goltsman E, Reznik JG, Mosek A, Korczyn AD. The value of muscle exercise in patients with amyotrophic lateral sclerosis. Journal of the Neurological Sciences 2001;191(1-2):133-7. [DOI] [PubMed] [Google Scholar]
Evans 1984 {published data only}
- Evans RL, Fox HR, Pritzl DO, Halar EM. Group treatment of physically disabled adults by telephone. Social Work in Health Care 1984;9(3):77-84. [DOI] [PubMed] [Google Scholar]
Favejee 2015 {published data only}
- Favejee MM, Van den Berg LE, Kruijshaar ME, Wens SC, Praet SF, Pim Pijnappel WW, et al. Exercise training in adults with Pompe disease: the effects on pain, fatigue, and functioning. Archives of Physical Medicine and Rehabilitation 2015;96(5):817-22. [DOI] [PubMed] [Google Scholar]
Flannery 2014 {published data only}
- Flannery M, Roscoe J, Heckler C, Janelsins M, Peppone L, Kamen C, et al. Exploratory analysis of chemotherapy induced peripheral neuropathy (CIPN), concurrent symptoms and interference with walking and general activity: a URCC CCOP research base Study. Supportive Care in Cancer 2014;22(1 (Suppl 1)):S216-7. [Google Scholar]
Gagnon 2018 {published data only}
- Gagnon C, Gallais B, Laberge L. Myotonic dystrophy type 1: reasons to be OPTIMISTIC. Lancet Neurology 2018;17(8):652-3. [DOI] [PubMed] [Google Scholar]
Ghavami 2018 {published data only}
- Ghavami H, Radfar M, Soheily S, Shamsi SA, Khalkhali HR. Effect of lifestyle interventions on diabetic peripheral neuropathy in patients with type 2 diabetes, result of a randomized clinical trial. Journal of the Turkish Society of Algology 2018;30(4):165-70. [DOI] [PubMed] [Google Scholar]
Henke 2012 {published data only}
- Henke C, Cabri J, Fricke L, Kandilakis G, Wulf P, Feyer PC, et al. Enhanced physical activity intervention in lung cancer patients during palliative chemotherapy – a randomized controlled trial. Onkologie 2012;35(Suppl 6):139. [Google Scholar]
Katz 2004 {published data only}
- Katz J. AVP-39: a successful randomized clinical trial on a supportive therapy for ALS. Neurology 2004;63(8):1345. [Google Scholar]
Khan 2011 {published data only}
- Khan F, Pallant JF, Amatya B, Ng L, Gorelik A, Brand C. Outcomes of high- and low-intensity rehabilitation programme for persons in chronic phase after Guillain-Barre syndrome: a randomized controlled trial. Journal of Rehabilitation Medicine 2011;43(7):638-46. [DOI] [PubMed] [Google Scholar]
Kierkegaard 2011 {published data only}
- Kierkegaard M, Harms-Ringdahl K, Widen Holmqvist L, Edstrom L, Tollback A. Compliance and feasibility of a physical exercise programme in adults with myotonic dystrophy type 1. Physiotherapy 2011;97(Suppl 1):eS608-9. [DOI] [PubMed] [Google Scholar]
Kierkegaard 2012 {published data only}
- Kierkegaard M, Widen Holmqvist L. Effects of a physical exercise programme in adults with myotonic dystrophy type 1 – a one-year follow-up study. Neuromuscular Disorders 2012;22(9-10):895-6. [Google Scholar]
Kitano 2018 {published data only}
- Kitano K, Asakawa T, Kamide N, Yorimoto K, Yoneda M, Kikuchi Y. Effectiveness of home-based exercises without supervision by physical therapists for patients with early-stage amyotrophic lateral sclerosis: a pilot study. Archives of Physical Medicine and Rehabilitation 2018;99(10):2114-7. [DOI] [PubMed] [Google Scholar]
Kleckner 2016 {published data only}
- Kleckner I, Kamen CS, Peppone LJ, Janelsins MC, Asare M, Heckler CE. A URCC NCORP nationwide randomized controlled trial investigating the effect of exercise on chemotherapy-induced peripheral neuropathy in 314 cancer patients. Journal of Clinical Oncology 2016;34(15 (Suppl)):10000. [Google Scholar]
Kluding 2017 {published data only}
- Kluding PM, Singleton JR, Pasnoor M, Dimachkie MM, Barohn RJ, Smith AG. Activity for Diabetic Polyneuropathy (ADAPT): study design and protocol for a 2-site randomized controlled trial. Physical Therapy 2017;97(1):20-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Landon‐Cardinal 2018 {published data only}
- Landon-Cardinal O, Bachasson D, Guillaume P, Vautier M, Champtiaux N, Hervier B. Physical activity monitoring using wrist-worn accelerometer in the assessment and follow-up of patients with myositis. Arthritis and Rheumatology 2018;70(Suppl 9):416. [Google Scholar]
Landon‐Cardinal 2019 {published data only}
- Landon-Cardinal O, Bachasson D, Guillaume-Jugnot P, Vautier M, Champtiaux N, Hervier B, et al. Physical activity monitoring using wrist-worn accelerometer in the assessment of patients with myositis. Neuromuscular Disorders 2019;29(Suppl 1):S106. [Google Scholar]
Lehmann 1994 {published data only}
- Lehmann ED. The diabetes control and complications trial (DCCT): a role for computers in patient education? Diabetes, Nutrition & Metabolism - Clinical & Experimental 1994;7(5):308-16. [Google Scholar]
Longstreth 1998 {published data only}
- Longstreth WT Jr, McGuire V, Koepsell TD, Wang Y, Van Belle G. Risk of amyotrophic lateral sclerosis and history of physical activity: a population-based case-control study. Archives of Neurology 1998;55(2):201-6. [DOI] [PubMed] [Google Scholar]
Lustenhouwer 2019 {published data only}
- Lustenhouwer R, Van Alfen N, Cameron IG, Toni I, Geurts AC, Helmich RC. NA-CONTROL: a study protocol for a randomised controlled trial to compare specific outpatient rehabilitation that targets cerebral mechanisms through relearning motor control and uses self-management strategies to improve functional capability of the upper extremity, to usual care in patients with neuralgic amyotrophy. Trials 2019;20(1):482. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mishra 2012 {published data only}
- Mishra SK, Singh P, Bunch, S, Zhang R. The therapeutic value of yoga in neurological disorders. Annals of Indian Academy of Neurology 2012;15(4):247-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Monini 2017 {published data only}
- Monini S, Buffoni A, Romeo M, Di Traglia M, Filippi C, Atturo F, et al. Kabat rehabilitation for Bell's palsy in the elderly. Acta Oto-laryngologica 2017;137(6):646-50. [DOI] [PubMed] [Google Scholar]
Mori 2016 {published data only}
- Mori L, Francini L, Prada V, Signori A, Pareyson D, Padua L. Aerobic exercise in patients affected by Charcot-Marie-Tooth (CMT) neuropathy: results of a randomized, single blind, controlled study. Journal of the Peripheral Nervous System 2016;21(3):282. [Google Scholar]
Mori 2017 {published data only}
- Mori L, Francini L, Prada V, Signori A, Pareyson D, Padua L. Aerobic exercise for subjects affected by Charcot Marie Tooth (CMT) neuropathy: results of a multicenter, prospective, randomized, single blind, controlled clinical trial. Journal of the Peripheral Nervous System 2017;22(3):343-4. [Google Scholar]
Mosforth 1958 {published data only}
- Mosforth J, Taverner D. Physiotherapy for Bell's palsy. British Medical Journal 1958;13(5097):675-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Oksuz 2011 {published data only}
- Oksuz C, Akel BS, Bumin G. Effect of occupational therapy on activity level and occupational performance in patients with neuromuscular disease. Fizyoterapi Rehabilitasyon 2011;22(3):231-9. [Google Scholar]
Otterman 2011 {published data only}
- Otterman N. An exercise programme for patients with diabetic complications: a study on feasibility and preliminary effectiveness. Physiotherapy 2011;97(Suppl 1):eS950-1. [DOI] [PubMed] [Google Scholar]
Ozalevli 2004 {published data only}
- Ozalevli SS, Bayir N, Cavusoglu YH, Cakmak O. Is physical exercise necessary in the treatment of the congenital muscular torticollis? Pediatrik Cerrahi Dergisi 2004;18(1):22-4. [Google Scholar]
Phillips 2009 {published data only}
- Phillips M, Flemming N, Tsintzas K. An exploratory study of physical activity and perceived barriers to exercise in ambulant people with neuromuscular disease compared with unaffected controls. Clinical Rehabilitation 2009;23(8):746-55. [DOI] [PubMed] [Google Scholar]
Phillips 2012 {published data only}
- Phillips MF, Robertson Z, Killen B, White B. A pilot study of a crossover trial with randomized use of ankle-foot orthoses for people with Charcot-Marie-tooth disease. Clinical Rehabilitation 2012;26(6):534-44. [DOI] [PubMed] [Google Scholar]
Ramdharry 2012 {published data only}
- Ramdharry GM, Pollard AJ, Anderson CA, Laura M, Murphy SM, Hutton EJ. Strengthening hip flexors to improve walking distance in people with Charcot-Marie-Tooth disease. Neuromuscular Disorders 2012;22(Suppl 1):S21. [Google Scholar]
Rideau 1995 {published data only}
- Rideau Y, Duport G, Delaubier A, Guillou C, Renardel-Irani A, Bach JR. Early treatment to preserve quality of locomotion for children with Duchenne muscular dystrophy. Seminars in Neurology 1995;15(1):9-17. [DOI] [PubMed] [Google Scholar]
Schenone 2010 {published data only}
- Schenone A, Padua L, Monti Bragadin M, Maggi G, Pareyson D, Fabrizi GM. A multicenter study to evaluate the effects on Charcot-Marie-Tooth neuropathy type 1A of a composite treadmill, stretching and proprioceptive exercise (TreSPE) rehabilitation program. Journal of the Peripheral Nervous System 2010;15(Suppl 1):34. [Google Scholar]
Schenone 2015 {published data only}
- Schenone A, Francini L, Signori A, Maggi G, Bragadin MM, Bolla S, et al. Treadmill, stretching and proprioceptive (TRESPE) rehabilitation program in CMT1A: the role of 6-MWT in the evaluation of patients at baseline. Journal of the Peripheral Nervous System 2015;20(2):227. [Google Scholar]
Schonsteiner 2015 {published data only}
- Schonsteiner S, Kirchner E, Mack S, Bauder-Misbach H, Hamel T, Furnis T, et al. A randomized phase-3 study in patients with chemotherapy induced sensorimotor polyneuropathy evaluating an integrated program including massage, structured kinesthetic three-dimensional mobilization, physical exercises with or without whole-body vibration. Oncology Research and Treatment 2015;38(Suppl 5):189. [Google Scholar]
Scott 1981 {published data only}
- Scott OM, Hyde SA, Goddard C, Jones R, Dubowitz V. Effect of exercise in Duchenne muscular dystrophy. A controlled six-month study of the effects of two different regimes of exercises in children with Duchenne muscular dystrophy. Physiotherapy 1981;67(6):174-6. [PubMed] [Google Scholar]
Sendhilkumar 2013 {published data only}
- Sendhilkumar R, Gupta A, Nagarathna R, Taly AB. Effect of pranayama and meditation as an add-on therapy in rehabilitation of patients with Guillain-Barre syndrome – a randomized control pilot study. Disability and Rehabilitation 2013;35(1):57-62. [DOI] [PubMed] [Google Scholar]
Spencer 2016 {published data only}
- Spencer T, Williams G, Fahey M. The effectiveness of a running group program in children with a neurological condition. Developmental Medicine and Child Neurology 2016;58(Suppl 3):49-50. [Google Scholar]
Terpstra Lindeman 1992 {published data only}
- Terpstra Lindeman E, Leffers P, Spaans F, Drukker J, Reulen J, Kerckhoffs M, et al. Strength training in patients with neuromuscular diseases – a randomized clinical trial. Clinical Rehabilitation 1992;6(Suppl 6):76. [DOI] [PubMed] [Google Scholar]
Tomas 2011 {published data only}
- Tomas MT, Santa-Clara H, Monteiro E, Gil J, Bruno PM, Barroso E, et al. A supervised versus home-based exercise program effects on liver transplanted familial amyloidotic polyneuropathy patients: walking, fatigue and quality of life. Physiotherapy 2011;97(1):eS1241-2. [Google Scholar]
Van Puymbroeck 2016 {published data only}
- Van Puymbroeck M, Atler K, Portz J, Willis L, Phillips C, Schmid AA. Less neuropathy after yoga: qualitative perspectives on improvements following an 8-week trial. Archives of Physical Medicine and Rehabilitation 2016;97(10):e39-40. [Google Scholar]
Veenhuizen 2015 {published data only}
- Veenhuizen Y, Cup EH, Groothuis JT, Hendriks JC, Adang EM, Van Engelen BG. Effectiveness and cost-effectiveness of a self-management group program to improve social participation in patients with neuromuscular disease and chronic fatigue: protocol of the Energetic study. BMC Neurology 2015;15:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Veenhuizen 2019 {published data only}
- Veenhuizen Y, Cup EH, Jonker MA, Voet NB, Van Keulen BJ, Maas DM, et al. Self-management program improves participation in patients with neuromuscular disease: a randomized controlled trial. Neurology 2019;93(18):e1720-31. [DOI] [PubMed] [Google Scholar]
Wiesinger 1998 {published data only}
- Wiesinger GF, Quittan M, Graninger M, Seeber A, Ebenbichler G, Sturm B. Benefit of 6 months long-term physical training in polymyositis/dermatomyositis patients. British Journal of Rheumatology 1998;37(12):1338-42. [DOI] [PubMed] [Google Scholar]
Zhang 2005 {published data only}
- Zhang X, Zhi AH, Liu RL, Cheng XZ. Alcoholic peripheral neuropathy. Chinese Journal of Clinical Rehabilitation 2005;9(5):138-40. [Google Scholar]
Zilliox 2018 {published data only}
- Zilliox L, Kumar P, Russell J. A randomized, blinded, lifestyle intervention study improves the expiration: inspiration ration in diabetic neuropathy. Journal of the Peripheral Nervous System 2018;23(4):329-30. [Google Scholar]
Zilliox 2019 {published data only}
- Zilliox L, Ilieva N, Zhan M, Russell J. A randomized lifestyle intervention study improves mobility and neuropathy in diabetes. Neurology 2019;92(15 (Suppl 1)):P3.4-018. [Google Scholar]
References to studies awaiting assessment
ChiCTR‐IPR‐15006127 {published data only}
- ChiCTR-IPR-15006127. Effect of peer support on physical activity of patients with diabetic peripheral neuropathy. www.chictr.org.cn/hvshowproject.aspx?id=11741 (first received 22 March 2015).
NCT00866112 {published data only}
- NCT00866112. A randomized exercise trial for wheelchair users. clinicaltrials.gov/show/NCT00866112 (first received 20 March 2009).
References to ongoing studies
ACTRN12617000543381 {published data only}
- ACTRN12617000543381. Do different shoe insole surfaces affect balance and walking in adults with diabetes and foot nerve damage? www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=372682 (first received 18 April 2017).
NCT02089880 {published data only}
- NCT02089880. Comparing functional outcomes in individuals using micro-processor controlled orthosis versus stance control orthosis. clinicaltrials.gov/show/NCT02089880 (first received 18 March 2014).
NCT02790931 {published data only}
- NCT02790931. Effects of foot muscle strengthening in daily activity in diabetic neuropathic patients. clinicaltrials.gov/ct2/show/NCT02790931 (first received 6 June 2016).
NCT03515356 {published data only}
- NCT03515356. Exercise to reduce chemotherapy-induced peripheral neuropathy. clinicaltrials.gov/show/NCT03515356 (first received 3 May 2018).
NCT03531788 {published data only}
- NCT03531788. Use of dynamic arm supports to promote activities of daily living in individuals with DMD. clinicaltrials.gov/show/NCT03531788 (first received 22 May 2018).
Additional references
ACSM 2010
- Thompson WR, Gordon NF, Pescatello LS, editor(s). ACSM's Guidelines for Exercise Testing and Prescription. 8th edition. Philadelphia (PA): Wolters Kluwer Lippincott Williams & Wilkins, 2010. [Google Scholar]
Aitkens 2005
- Aitkens S, Kilmer DD, Wright NC, McCrory MA. Metabolic syndrome in neuromuscular disease. Archives of Physical Medicine and Rehabilitation 2005;86(5):1030-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Apabhai 2011
- Apabhai S, Gorman GS, Sutton L, Elson JL, Plötz T, Turnbull DM, et al. Habitual physical activity in mitochondrial disease. PloS One 2011;6(7):e22294. [DOI: 10.1371/journal.pone.0022294] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ashworth 2005
- Ashworth NL, Chad KE, Harrison EL, Reeder BA, Marshall SC. Home versus center based physical activity programs in older adults. Cochrane Database of Systematic Reviews 2005, Issue 1. Art. No: CD004017. [DOI: 10.1002/14651858.CD004017.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Baker 2015
- Baker PR, Francis DP, Soares J, Weightman AL, Foster C. Community wide interventions for increasing physical activity. Cochrane Database of Systematic Reviews 2015, Issue 1. Art. No: CD008366. [DOI: 10.1002/14651858.CD008366.pub3] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bartels 2019
- Bartels B, Montes J, Van der Pol WL, De Groot JF. Physical exercise training for type 3 spinal muscular atrophy. Cochrane Database of Systematic Reviews 2019, Issue 3. Art. No: CD012120. [DOI: 10.1002/14651858.CD012120.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Covidence [Computer program]
- Covidence. Melbourne, Australia: Veritas Health Innovation, 2020. Available at covidence.org.
Dal Bello‐Haas 2013
- Dal Bello-Haas V, Florence JM. Therapeutic exercise for people with amyotrophic lateral sclerosis or motor neuron disease. Cochrane Database of Systematic Reviews 2013, Issue 5. Art. No: CD005229. [DOI: 10.1002/14651858.CD005229.pub3] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2020
- Deeks JJ, Higgins JP, Altman DG. Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane, 2020. Available from training.cochrane.org/handbook/archive/v6.1.
Deenen 2015
- Deenen JC, Horlings CG, Verschuuren JJ, Verbeek AL, Van Engelen BG. The epidemiology of neuromuscular disorders: a comprehensive overview of the literature. Journal of Neuromuscular Diseases 2015;2(1):73-85. [PMID: ] [PubMed] [Google Scholar]
Dobbins 2015
- Dobbins M, Husson H, DeCorby K, LaRocca RL. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database of Systematic Reviews 2015, Issue 2. Art. No: CD007651. [DOI: 10.1002/14651858.CD007651.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ekelund 2016
- Ekelund U, Steen-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016;388(10051):1302-10. [DOI: 10.1016/S0140-6736(16)30370-1] [PMID: 27475271] [DOI] [PubMed] [Google Scholar]
Foster 2005
- Foster C, Hillsdon M, Thorogood M, Kaur A, Wedatilake T. Interventions for promoting physical activity. Cochrane Database of Systematic Reviews 2005, Issue 1. Art. No: CD003180. [DOI: 10.1002/14651858.CD003180.pub2] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Foster 2013
- Foster C, Richards J, Thorogood M, Hillsdon M. Remote and web 2.0 interventions for promoting physical activity. Cochrane Database of Systematic Reviews 2013, Issue 9. Art. No: CD010395. [DOI: 10.1002/14651858.CD010395.pub2] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fowler 2002
- Fowler WM Jr. Consensus conference summary. Role of physical activity and exercise training in neuromuscular diseases. American Journal of Physical Medicine and Rehabilitation 2002;81(11 Suppl):S187-95. [EMBASE: 35192978] [DOI] [PubMed] [Google Scholar]
Freak‐Poli 2020
- Freak-Poli R, Cumpston M, Albarqouni L, Clemes SA, Peeters A. Workplace pedometer interventions for increasing physical activity. Cochrane Database of Systematic Reviews 2020, Issue 7. Art. No: CD009209. [DOI: 10.1002/14651858.CD009209.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT. Hamilton (ON): McMaster University (developed by Evidence Prime), 2020. Available at gradepro.org.
Heutinck 2017
- Heutinck L, Van Kampen N, Jansen M, De Groot IJ. Physical activity in boys with Duchenne muscular dystrophy is lower and less demanding compared to healthy boys. Journal of Child Neurology 2017;32(5):450-7. [DOI: 10.1177/0883073816685506] [PMID: 28112012 ] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Altman DG, Sterne JA. Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Higgins 2020
- Higgins JP, Eldridge S, Li T. Chapter 23: Including variants on randomized trials. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane, 2020. Available from training.cochrane.org/handbook/archive/v6.1.
Jimenez‐Moreno 2017
- Jimenez-Moreno AC, Newman J, Charman SJ, Catt M, Trenell MI, Gorman GS, et al. Measuring habitual physical activity in neuromuscular disorders: a systematic review. Journal of Neuromuscular Diseases 2017;4(1):25-52. [DOI: 10.3233/JND-160195] [PMID: 28269791 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Joseph 2015
- Joseph PD, Craig JC, Caldwell PH. Clinical trials in children. British Journal of Pharmacology 2015;79(3):357-69. [DOI: 10.1111/bcp.12305] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kilmer 2005
- Kilmer DD, Zhao HH. Obesity, physical activity, and the metabolic syndrome in adult neuromuscular disease. Physical Medicine and Rehabilitation Clinics of North America 2005;16(4):1053-62. [PMID: ] [DOI] [PubMed] [Google Scholar]
Koopman 2015
- Koopman FS, Beelen A, Gilhus NE, Visser M, Nollet F. Treatment for postpolio syndrome. Cochrane Database of Systematic Reviews 2015, Issue 5. Art. No: CD007818. [DOI: 10.1002/14651858.CD007818.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lu 2020
- Lu Y, Xing P, Cai X, Luo D, Li R, Lloyd C, et al. Prevalence and risk factors for diabetic peripheral neuropathy in type 2 diabetic patients from 14 countries: estimates of the INTERPRET-DD study. Frontiers in Public Health 2020;8:534372. [DOI: 10.3389/fpubh.2020.534372] [DOI] [PMC free article] [PubMed] [Google Scholar]
McCrory 1998
- McCrory MA, Kim HR, Wright NC, Lovelady CA, Aitkens S, Kilmer DD. Energy expenditure, physical activity, and body composition of ambulatory adults with hereditary neuromuscular disease. American Journal of Clinical Nutrition 1998;67(6):1162-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
McDonald 2002
- McDonald CM. Physical activity, health impairments, and disability in neuromuscular disease. American Journal of Physical Medicine and Rehabilitation 2002;81(Suppl):S108-20. [PMID: ] [DOI] [PubMed] [Google Scholar]
MDUK 2014
- Muscular Dystrophy UK. Exercise advice for adults with muscle-wasting conditions. www.musculardystrophyuk.org/wp-content/uploads/2015/05/Exercise-advice-for-adults.pdf (accessed 5 May 2021).
Mehrholz 2015
- Mehrholz J, Pohl M, Kugler J, Burridge J, Mückel S, Elsner B. Physical rehabilitation for critical illness myopathy and neuropathy. Cochrane Database of Systematic Reviews 2015, Issue 3. Art. No: CD010942. [DOI: 10.1002/14651858.CD010942.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Medicine 2009;6(7):e1000097. [DOI: 10.1371/journal.pmed1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nary 2011
- Nary DE, Froehlich-Grobe K, Aaronson L. Recruitment issues in a randomized controlled exercise trial targeting wheelchair users. Contemporary Clinical Trials 2011;32(2):188-95. [DOI: 10.1016/j.cct.2010.10.010] [DOI] [PMC free article] [PubMed] [Google Scholar]
Öksüz 2011
- Öksüz Ç, Akel BS, Bumin G. Effect of occupational therapy on activity level and occupational performance in patients with neuromuscular disease. Fizyoterapi Rehabilitasyon 2011;22(3):231-9. [EMBASE: 365493900] [Google Scholar]
Page 2021
- Page MJ, Higgins JP, Sterne JA. Chapter 13: Assessing risk of bias due to missing results in a synthesis. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, 2021. Available from training.cochrane.org/handbook.
Quinlivan 2011
- Quinlivan R, Vissing J, Hilton-Jones D, Buckley J. Physical training for McArdle disease. Cochrane Database of Systematic Reviews 2011, Issue 12. Art. No: CD007931. [DOI: 10.1002/14651858.CD007931.pub2] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ramdharry 2017
- Ramdharry GM, Pollard AJ, Grant R, Dewar EL, Laurá M, Moore SA, et al. A study of physical activity comparing people with Charcot-Marie-Tooth disease to normal control subjects. Disability and Rehabilitation 2017;39(17):1753-8. [DOI: 10.1080/09638288.2016.1211180] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Review Manager 2020 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.4. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2020.
RevMan Web 2020 [Computer program]
- Review Manager Web (RevMan Web). Version 2.2.1. The Cochrane Collaboration, 2020. Available at revman.cochrane.org.
Richards 2013a
- Richards J, Hillsdon M, Thorogood M, Foster C. Face-to-face interventions for promoting physical activity. Cochrane Database of Systematic Reviews 2013, Issue 9. Art. No: CD010392. [DOI: 10.1002/14651858.CD010392.pub2] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Richards 2013b
- Richards J, Thorogood M, Hillsdon M, Foster C. Face-to-face versus remote and web 2.0 interventions for promoting physical activity. Cochrane Database of Systematic Reviews 2013, Issue 9. Art. No: CD010393. [DOI: 10.1002/14651858.CD010393.pub2] [PMID: 24085593 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Saeedi 2019
- Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Diabetes Atlas Committee. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Research and Clinical Practice 2019;157:107843. [DOI: 10.1016/j.diabres.2019.107843] [DOI] [PubMed] [Google Scholar]
Schünemann 2011a
- Schünemann HJ, Oxman AD, Higgins JP, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and 'Summary of findings' tables. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Schünemann 2011b
- Schünemann HJ, Oxman AD, Vist GE, Higgins JP, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Slade 2016
- Slade SC, Dionne CE, Underwood M, Buchbinder R, Beck B, Bennell K, et al. Consensus on Exercise Reporting Template (CERT): modified Delphi study. Physical Therapy 2016;96(10):1514-24. [DOI: 10.2522/ptj.20150668] [DOI] [PubMed] [Google Scholar]
Stefanetti 2020
- Stefanetti RJ, Blain A, Jimenez-Moreno C, Errington L, Ng YS, McFarland R, et al. Measuring the effects of exercise in neuromuscular disorders: a systematic review and meta-analyses. Wellcome Open Research 2020;5(84):eCollection. [DOI: 10.12688/wellcomeopenres.15825.1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stoyanov 2015
- Stoyanov SR, Hides L, Kavanagh DJ, Zelenko O, Tjondronegoro D, Mani M. Mobile app rating scale: a new tool for assessing the quality of health mobile apps. Journal of Medical Internet Research 2015;3(1):e27. [DOI: 10.2196/mhealth.3422] [DOI] [PMC free article] [PubMed] [Google Scholar]
The EQUATOR Network
- The EQUATOR Network. The TIDieR (Template for Intervention Description and Replication) checklist. www.equator-network.org/wp-content/uploads/2014/03/TIDieR-Checklist-PDF.pdf (accessed 5 May 2021).
Voet 2013
- Voet NB, Van der Kooi EL, Riphagen II, Lindeman E, Van Engelen BG, Geurts AC. Strength training and aerobic exercise training for muscle disease. Cochrane Database of Systematic Reviews 2013, Issue 7. Art. No: CD003907. [DOI: 10.1002/14651858.CD003907.pub4] [PMID: ] [DOI] [PubMed] [Google Scholar]
Voet 2019
- Voet NB, Van der Kooi EL, Van Engelen BG, Geurts AC. Strength training and aerobic exercise training for muscle disease. Cochrane Database of Systematic Reviews 2019, Issue 12. Art. No: CD003907. [DOI: 10.1002/14651858.CD003907.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Walklet 2016
- Walklet E, Muse K, Meyrick J, Moss T. Do psychosocial interventions improve quality of life and wellbeing in adults with neuromuscular disorders? A systematic review and narrative synthesis. Journal of Neuromuscular Diseases 2016;3(3):347-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Warburton 2006
- Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ : Canadian Medical Association Journal 2006;174(6):801-9. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Warburton 2017
- Warburton DE, Bredin SS. Health benefits of physical activity: a systematic review of current systematic reviews. Current Opinion in Cardiology 2017;32(5):541-56. [DOI: 10.1097/HCO.0000000000000437] [DOI] [PubMed] [Google Scholar]
White 2004
- White CM, Pritchard J, Turner-Stokes L. Exercise for people with peripheral neuropathy. Cochrane Database of Systematic Reviews 2004, Issue 4. Art. No: CD003904. [DOI: 10.1002/14651858.CD003904.pub2] [PMID: ] [DOI] [PubMed] [Google Scholar]
WHO 2020a
- World Health Organization. WHO guidelines on physical activity and sedentary behavior. Geneva: WHO Press, 2020. [ISBN: 9789240015128] [Google Scholar]
WHO 2020b
- World Health Organization. Physical activity fact sheet. www.who.int/news-room/fact-sheets/detail/physical-activity (accessed 5 May 2021).
References to other published versions of this review
Jones 2020
- Jones K, Hawke F, Newman J, Miller JAL, Burns J, Jakovljevic DG, et al. Interventions for promoting physical activity in people with neuromuscular disease. Cochrane Database of Systematic Reviews 2020, Issue 3. Art. No: CD013544. [DOI: 10.1002/14651858.CD013544] [DOI] [PMC free article] [PubMed] [Google Scholar]


