Abstract
Background
Critical care is widely perceived, both within and outside of the speciality, as unremitting and emotionally burdensome. There is a perception of a higher risk to medical staff of burnout than other specialities. Critical care also has considerable emotional and professional rewards. We sought to examine this balance between emotional reward and stress in UK critical care consultants registered with the Faculty of Intensive Care Medicine.
Method
We conducted a Wellbeing survey of the Faculty of Intensive Care Medicine consultant membership utilising the Professional Quality of Life (Pro-QOL) survey tool. The survey was conducted as part of the Annual Workforce Census.
Results
In sum, 799 members completed the Pro-QOL survey, making this one of the largest surveys of physician wellbeing in critical care medicine. Data were analysed in accordance with the Pro-QOL manual.
Conclusions
The results demonstrate moderate risk for burnout and secondary traumatic stress, but this is balanced by moderate compassion satisfaction. No association was demonstrated between age, sex, or size of critical care unit worked in. Further follow-up of this consultant group is warranted to better understand risk factors for burnout and for future mitigation of these risk factors whilst also enhancing the positive aspects of working as a consultant in critical care medicine.
Keywords: Intensive care, wellbeing, burnout, Pro-QOL
Introduction
In recent years, there has been increasing interest into staff experience within healthcare and the wellbeing of the workforce. Average sickness rates in National Health Service England vary across professions and areas, but on average in 2017, the sickness absence for acute Trusts ran at 3.95%.1 Twenty-two percent of these absences were accounted for by stress-related problems.2 By comparison, the UK Office for National Statistics Annual Labour Force Survey finds sickness absence across the UK workforce to run at 1.9% and is overall on the decrease, with between 7 and 10% explained by mental health or stress.3
UK doctors are at greater risk of work-related stress, burnout, depression and anxiety than the general population. The most common causes being high perceived workload, increasing intensity and complexity of the work, rapid change within healthcare, low control and support and personal experiences of bullying and harassment.4 A survey of the medical workforce including 7000 trainees and consultants indicated a quarter of doctors in training and a fifth of consultants feel burnt out. This may be associated with high workloads, rota gaps, the lack of a supportive working environment and significant concerns about the effect burnout has on delivery of good care.5 Intensive care medicine (ICM) provides many clinical challenges. These can be both rewarding and stimulating but may also increase the experience of stress, with staff being exposed to more vicarious trauma and death than many of the general population are likely to witness in a lifetime.
Wellbeing research is an emerging field of research in ICM. Following such interest and concern, a 2016 statement was produced by a collaborative of critical care societies calling for action to mitigate the causes of burnout syndrome in critical care.6 Many researchers have chosen to focus on the concept of burnout: one concept within the wider issue of workforce wellbeing. Table 1 is a summary of recent research in critical care utilising the Maslach Burnout Inventory17 as a measure of burnout syndrome in critical care and also other measures of psychological morbidity such as post-traumatic stress disorder, depression and anxiety.
Table 1.
A summary of studies of BOS and psychological morbidity in critical care settings since 2000.
| Principle author | Country | Population | Psychological distress |
|---|---|---|---|
| Meynaar et al.7 | Netherlands | N = 272 Physicians | 4.4% BOS |
| Colville et al.8 | UK | Paediatric critical care N = 120, physicians and nurses | 61% one + BOS 18% PTSD |
| Teixeira et al.9 | Portugal | N = 300, physicians & nurses | 31% BOS |
| Czaja et al.10 | USA | Paediatric critical care nurses | 82% any psychological morbidity 68% one symptom + BOS |
| Merlani et al.11 | Switzerland | N = 3052, physicians & nurses | 29% BOS |
| Verdon et al.12 | Switzerland | N = 91, nurses | 28% BOS |
| Mealer et al.13 | USA | N = 351 nurses | 24% clinical PTSD in ICU nurses |
| Poncet et al.14 | France | N = 2392 nurses | 33% BOS |
| Embracio et al.15 | France | N = 978 physicians | 46% BOS 25% depression |
| Coomber et al.16 | UK | N = 627 Physicians | 30% psychological distress (General Health Questionnaire) 10% depression |
BOS: burnout syndrome; ICU: intensive care unit; PTSD: post-traumatic stress disorder.
We do not fully understand the predictive factors of burnout. Studies are mainly cross-sectional, with few longitudinal studies able to clearly elucidate the development of burnout. Findings are inconsistent around gender, social support and personality.18 Despite increasing numbers of women in the speciality of ICM, the proportion of men remains high. Age is important in trying to address whether ICM is a career that may impact the individual over a prolonged period of time.
If we do measure burnout alone, we risk ignoring the positive aspects of what keeps people working successfully and healthily in critical care. Maslach, who developed the term burnout into the concept we now understand, currently focuses her research on the area of staff engagement. We have little research into the Professional Quality of Life (Pro-QOL)19 and satisfaction in intensive care staff; hence, the Faculty of Intensive Care Medicine (FICM) has decided to focus on assessing the wellbeing of its consultant workforce. We sought to examine the interplay between work-related stress and emotional rewards that can be experienced working in critical care in the UK. The retention of critical care consultants, alongside the recruitment of doctors to the speciality, is crucial. A better factual understanding of wellbeing might aid both recruitment and retention of medical staff.
FICM is the professional body responsible for the training, assessment and practice of ICM in the UK. It is the largest organisation of critical care medical professionals in the UK. The working group of the Careers, Recruitment and Workforce (CRW) committee have run an annual census of its members since 2013. This census has a standardised set of demographic questions for members, as well as a section on workforce, and patient throughput through the units. This paper describes the results of the 2018 wellbeing survey as a sub-part of the census.
Method
In 2017, the CRW group included a separate section in the census on workforce wellbeing by use of the Pro-QOL in the census as a voluntary section (Pro-QOL – version 5).19,20 The Pro-QOL is the most widely used measure of the positive and negative aspects of helping in the world. It has three subscales, as indicated in Figure 1. Additional data gathered included gender, age, size of unit and most enjoyed area of ICM.
Figure 1.
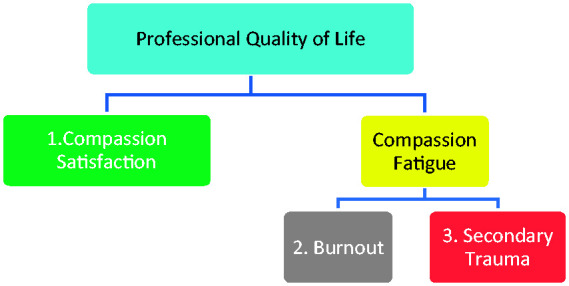
The Pro-QOL subscales.
Statistical analysis
Data were interpreted in accordance with the Pro-QOL Manual and analysed using SPSS. Results from participants with incomplete data were excluded. Continuous variables were not normally distributed; hence, comparisons were drawn using non-parametric tests (the Mann–Witney U test or Kruskall–Wallis tests). P values of < 0.05 were interpreted as significant. Correlations were done through the use of the Chi-square or Fisher’s exact test as appropriate.
Results
The response rate for the census as a whole was 38.5%. Of the 38.5% that completed the census, 90.1% (799 participants) also completed the wellbeing survey in full. Demographic data are summarised, and a comparison of median Pro-QOL scores by declared gender is shown in Table 2. No significant differences were found between genders for each of the subscales.
Table 2.
Demographic characteristics of participants and median Pro-QOL scores by gender.
| N | Average age | Range | Compassion satisfaction | Burnout | Secondary traumatic stress | |
|---|---|---|---|---|---|---|
| Male | 527 | 47.77 | 33–70 | 38 | 26 | 22 |
| Female | 175 | 46.23 | 35–62 | 37 | 27 | 23 |
| Did not say | 97 | 50.31 | 37–64 | 37 | 26 | 22 |
| Total group | 799 | 47.76 | 33–70 |
Pro-QOL: Professional Quality of Life.
Pro-QOL may be categorised into risk groups by percentile. The number of participants within high-risk Pro-QOL categories (low compassion satisfaction, high burnout, high secondary traumatic stress are indicated by shading) is given in Table 3 with respect to male and female gender. The percentages for each of the high-risk Pro-QOL categories are low and did not vary by gender. No participants were present in all three at-risk groups. A high number of participants were in the moderate risk groups for either burnout or secondary traumatic stress.
Table 3.
Proportion of participants in ‘High-Risk’ bracket for each subscale.
| Low (below 25th percentile) | Moderate | High (above 75th percentile) | |
|---|---|---|---|
| Compassion satisfaction | |||
| Female | 4 (2%) | 136 (78%) | 35 (20%) |
| Male | 8 (2%) | 396 (75%) | 121 (23%) |
| Burnout | |||
| Female | 36 (21%) | 137 (78%) | 2 (1) |
| Male | 125 (24%) | 396 (75%) | 4 (1%) |
| Secondary traumatic stress | |||
| Female | 84 (48%) | 91 (52%) | 0 (0%) |
| Male | 274 (52%) | 250 (48%) | 1 (0.1%) |
Note: High-risk category for each subscale is indicated by grey shading.
Correlations between age and Pro-QOL scores found no significant relationships (compassion satisfaction −0.56, p = 0.057; burnout 0.031, p = 0.191; secondary traumatic stress −0.009, p = 0.399). Correlations between reported size of unit by bed number and Pro-QOL scores found no significant relationships (compassion satisfaction 0.159, p = 0.065; burnout −0.141, p = 0.089; secondary traumatic stress −0.024, p = 0.410).
Participants also had the opportunity to report their most enjoyed factor of ICM, with high scores for variable and challenging case mix, supportive colleagues, feeling you make a difference and MDT working. These are reported in Table 4.
Table 4.
Reported most enjoyed factor in ICM.
| Agreement (%) | ICM work factor |
|---|---|
| 87 | Variable and challenging case mix |
| 69 | Supportive colleagues |
| 69 | Feel you make a real difference |
| 77 | Working as part of an MDT |
| 19 | Research |
ICM: intensive care medicine; MDT: multi-disciplinary team.
Discussion
The findings indicate that risk of burnout and secondary traumatic stress is low to moderate, and the prevalence of compassion satisfaction is moderate to high. Pro-QOL scores were not influenced by age, gender or size of unit, indicating that none of these factors is significantly predictive of work-related compassion satisfaction or compassion fatigue.
This aligns with the normative benchmarks reported more recently from an analysis of multiple studies21 and also specific examples from physicians.22–27 There are particular studies where our sample scores were preferably compared to other groups.
These are also significant findings in terms of professional risks: we did not find that either gender or length of experience alone as risk factors. This is important, as professionals should not feel that their gender will deter them from achieving success in ICM. In addition, it may be short sighted to consider that prolonged exposure through length of service predicts poor psychological wellbeing, or that ICM cannot be a lifelong career. There may be other factors to consider as a person ages: people may find this difficult for physical rather than emotional reasons. This means that as the workforce ages, working patterns and job plans will need to have wider considerations as to how an ageing workforce’s needs are best met.
Much of the critical care literature focusses upon the level of burnout. The prevalence of burnout has varied widely, and despite the recommendations to not use the Maslach questionnaire to give total scores of burnout, many papers have chosen this methodology. This reduces the validity of the findings. There are other methodological issues, such as the use of mixed professional groups, especially in mixed settings, which makes it hard to draw conclusions. The use of Pro-QOL with this FICM group was useful as an indicator, as despite a 78% moderate risk of burnout, the study also indicated high levels of work-related compassion satisfaction, with 98% of all participants reporting moderate to high levels of compassion satisfaction. A high number of participants also reported enjoyable aspects of critical care working, such as the variable and challenging workload and supportive colleagues. If only questions related to burnout are asked, the consultant workforce would appear at risk; however, the literature indicates that engagement and job satisfaction are important to wellbeing at work.27 It could be that compassion satisfaction provides some balance to the stress of working in ICM. Clearly, more research is required to understand the mitigating factors for burnout and also what best promotes positive wellbeing at work. A career in ICM does not necessarily increase the risk over other medical careers. The relationship between workplace and wellbeing is more complicated than the area of medicine alone.
Although numbers in the ‘high-risk’ Pro-QOL groups were low, there were a high number of cases within the ‘moderate’ risk group, which might indicate sub-clinical levels of secondary traumatic stress and burnout. In such a point prevalence survey, however, it is not possible to understand whether that will remain the same or develop into a problem in the future. Certainly, the limited evidence available in the wider burnout literature suggests that, at least in healthcare professionals, burnout seems to be stable, at least across three years.28 We do, as a speciality, need to reduce the risk of burnout due to both the effect on the delivery of good care29 as well as the effect on care givers.30
Strengths and weaknesses
The number of people choosing to complete the study is a strength of this study. The age and sex demographic of the sample suggest that the sample is representative of the speciality at the present time.
The nature of a voluntary survey, however, means there will be debate over whether this is a truly representative sample of ICM consultants and their wellbeing. It is possible that those who did not answer did not do so because they are burnt out. Conversely, it is possible that those under most stress and fatigue would want their voice heard loudly and thus participated more.
This is a point prevalence survey and therefore gives no indication of how the scores might change over time.
The authors of the Pro-QOL urge caution in interpreting the categories, as these are based on arbitrary percentile cut-offs. Despite the Pro-QOL being the world’s leading measure of quality of life at work, its accuracy in reflecting compassion fatigue (burnout and secondary traumatic stress scale) has recently come under some scrutiny.31
Conclusion
The data indicate that there are a high number of consultants in ICM who display some of the symptoms of burnout or secondary traumatic stress but very few fell within the highest risk category. The lack of statistical link between gender, age and years of experience or size of the unit currently worked in suggests that these are not significant risk factors. With 98% of the sample, however, scoring above the 25th percentile with moderate or high levels of compassion satisfaction, ICM is a rewarding area to work.
Prospectively monitoring this sample of consultants over time would give a very useful indicator of any loss of consultants from ICM over time to ICM over time due to burnout, and to understand whether this is linked to certain factors, e.g. size of unit, sex, on-call rota, and move to another speciality. We do need more research to better understand some of the predictive factors in work-related wellbeing in ICM and therefore put in place measures to avoid or mitigate any identified risks. This large study of current working intensivists demonstrates that assessing emotional gain and emotional burden gives a more rounded view of those working at the consultant level.
Acknowledgements
The authors would like to thank all the FICM members for their participation in the Pro-QOL survey. The authors especially thank the FICM CRW team led by Dr Danny Bryden.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.NHS Digital, NHS sickness absence rates – April 2018 to June 2018, https://digital.nhs.uk/data-and-information/publications/statistical/nhs-sickness-absencerates/april-2018-to-june-2018 (2018, accessed 19 December 2018).
- 2.NHS digital. Number of days lost by reason for absence and organisation March17 to Feb18, https://digital.nhs.uk/data-and-information/find-data-andpublications/supplementary-information/2018-supplementary-information-files/staffabsence/number-of-days-lost-by-reason-for-absence-and-organisation-mar17-to-feb18 (2018, accessed 19 December 2018).
- 3.Office for National Statistics. Sickness absence falls to the lowest rate on record, www.ons.gov.uk/employmentandlabourmarket/peopleinwork/employmentandemployeetypes/articles/sicknessabsencefallstothelowestratein24years/2018-07-30 (2018, accessed 6 September 2019).
- 4.Kinman G, Teoh K. What could make a difference to the mental health of UK doctors? A review of the research evidence, London: Society of Occupational Medicine, 2018. [Google Scholar]
- 5.General Medical Council. Training environments 2018: key findings from the national training surveys. London: General Medical Council, 2018.
- 6.Moss M, Good VS, Gozal D, et al. An official critical care societies collaborative statement: burnout syndrome in critical care healthcare professionals: a call for action. Crit Care Med 2016; 44: 1414–1421. [DOI] [PubMed] [Google Scholar]
- 7.Meynaar I, van Saase J, Feberwee T, et al. Burnout among Dutch intensivists. Intensive Care Med Exp 2015; 3: A140. [Google Scholar]
- 8.Colville G, Dalia C, Brierley J, et al. Burnout and traumatic stress in staff working in paediatric intensive care: associations with resilience and coping strategies. Intensive Care Med 2015; 41: 364–365. [DOI] [PubMed] [Google Scholar]
- 9.Teixeira C, Ribeiro O, Fonseca AM, et al. Burnout in intensive care units - a consideration of the possible prevalence and frequency of new risk factors: a descriptive correlational multicentre study. BMC Anesthesiol 2013; 13: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Czaja AS, Moss M, Mealer M. Symptoms of posttraumatic stress disorder among pediatric acute care nurses. J Pediatr Nurs Nurs Care Child Fam 2012; 27: 357–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Merlani P, Verdon M, Businger A, et al. Burnout in ICU caregivers: a multicenter study of factors associated to centers. Am J Respir Crit Care Med 2011; 184: 1140–1146. [DOI] [PubMed] [Google Scholar]
- 12.Verdon M, Merlani P, Perneger T, et al. Burnout in a surgical ICU team. Intensive Care Med 2008; 34: 152–156. [DOI] [PubMed] [Google Scholar]
- 13.Mealer ML, Shelton A, Berg B, et al. Increased prevalence of posttraumatic stress disorder symptoms in critical care nurses. Am J Respir Crit Care Med 2007; 175: 693–697. [DOI] [PubMed] [Google Scholar]
- 14.Poncet MC, Toullic P, Papazian L, et al. Burnout syndrome in critical care nursing staff. Am J Respir Crit Care Med 2007; 175: 698–704. [DOI] [PubMed] [Google Scholar]
- 15.Embriaco N, Azoulay E, Barrau K, et al. High level of burnout in intensivists: prevalence and associated factors. Am J Respir Crit Care Med 2007; 175: 686–692. [DOI] [PubMed] [Google Scholar]
- 16.Coomber S, Todd C, Park G, et al. Stress in UK intensive care unit doctors. BJA Br J Anaesth 2002; 89: 873–881. [DOI] [PubMed] [Google Scholar]
- 17.Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual, Palo Alto, CA: Consulting Psychologists Press, 1996. [Google Scholar]
- 18.Briner R, Poppleton S, Owens S, et al. The nature, causes and consequences of harm in emotionally demanding occupations. London: Health and Safety Executive, 2008.
- 19.Pro-Qol April 2018 to June 2018, https://proqol.org/ (accessed 6 September 2019).
- 20.Stamm BH. The concise ProQOL manual, Pocatello, ID: ProQoL, 2010. [Google Scholar]
- 21.De La Rosa GM, Webb-Murphy JA, Fesperman SF, et al. Professional quality of life normative benchmarks. Psychol Trauma 2018; 10: 225–228. [DOI] [PubMed] [Google Scholar]
- 22.Bellolio MF, Cabrera D, Sadosty AT, et al. Compassion fatigue is similar in emergency medicine residents compared to other medical and surgical specialties. West J Emerg Med 2014; 15: 629–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dasan S, Gohil P, Cornelius V, et al. Prevalence, causes and consequences of compassion satisfactio and compassion fatigue in emergency care: a mixed-methods study of UK NHS consultant. Emerg Med J 2015; 32: 588–594. [DOI] [PubMed] [Google Scholar]
- 24.Haik J, Brown S, Liran A, et al. Burnout and compassion fatigue: prevalence and associations among Israeli burn clinicians. Neuropsychiatr Dis Treat 2017; 13: 1533–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Imo UO. Burnout and psychiatric morbidity among doctors in the UK: a systematic literature review of prevalence and associated factors. BJPsych Bull 2017; 41: 197–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huggard P, Dixon R. Tired of caring: the impact of caring on resident doctors. Australas J Disaster Trauma Stud 2011; 3: 105–112. [Google Scholar]
- 27.Maslach C. Burnout and engagement in the workplace: new perspectives. Eur Health Psychol 2011; 13: 44–47. [Google Scholar]
- 28.Schaufeli WB, Maassen GH, Bakker AB, et al. Stability and change in burnout: a 10-year follow-up study among primary care physicians. J Occup Organis Psychol 2011; 84: 248–267. [Google Scholar]
- 29.Cornwell J. Staff care: how to engage staff in the NHS and why it matters, London: The Point of Care Foundation, 2014. [Google Scholar]
- 30.Talbot SG, and Dean WD. Physicians are not burning out they are suffering moral injury. Stat News, https://www.statnews.com/2018/07/26/physicians-not-burning-out-they-are-suffering-moral-injury/ (2018, accessed 26 July 2018).
- 31.Heritage B, Rees CS, Hegney DG. The ProQOL-21: a revised version of the Professional Quality of Life (ProQOL) scale based on Rasch analysis. PLoS One 2018; 13: e0193478. [DOI] [PMC free article] [PubMed] [Google Scholar]


