Introduction
Historical Considerations
To better understand the current landscape of surgery for non-small cell lung cancer (NSCLC), it is helpful to briefly review the history of thoracic surgery before the 1990s. Pulmonary resection in its earliest form, in the 15th to 17th centuries, was performed in rare instances of traumatic wounds with lung herniation or suppurative wounds of the chest wall that left the underlying lung exposed.1–3 The 18th and 19th centuries saw advances in thoracic surgery as surgeons explored surgical methods, including varying degrees of pulmonary resections, to treat tuberculosis and its aftermath. Progressive developments in anesthesia, along with the invention of the endotracheal tube and positive pressure ventilation, allowed thoracic surgery to advance in step. In 1912, Hugh Morriston Davies performed a right lower lobectomy through the sixth intercostal space, using individual hilar dissection and ligation. Unfortunately, the patient died from empyema on postoperative day 8.4 Similar unfavorable outcomes led surgeons to doubt the safety of single-stage pulmonary resection, and two-stage resection, where the lung was compressed or rendered ischemic and then resected at a later phase, was recommended.5
During this time, lung cancer was a rare entity, and the most frequent indications for pulmonary resection were benign, such as infectious or traumatic presentations. The reported mortality for resection ranged from 20% to 100% during this dark era. Most deaths were attributable to air embolism, sepsis, empyema, pneumonitis, and hemorrhage. Until Harold Brunn described complete closure of the chest wall with catheter drainage in 1929,6 the chest was left partially open in most cases, which accounted for much of the associated morbidity and mortality. In 1932, Churchill and Belsey published a series of four patients who underwent surgery for carcinoma of the lung. Only one of these patients was able to undergo a lobectomy and survive beyond postoperative day 3. In 1933, Evarts Graham performed the first pneumonectomy for lung cancer and posited that, “perhaps, if the entire lung is removed, the patient will have less a chance of recurrence than if only one lobe or a smaller portion is removed.”7 However, Churchill and Belsey, while describing the first segmentectomy in 1939, suggested that “the bronchopulmonary segment may replace the lobe as the surgical unit of the lung.”8
Surgical efforts during World War II overcame many technical difficulties and allowed thoracic surgery to become established as a separate, unique specialty shortly thereafter. Streptomycin became available in 1945, which established nonsurgical therapy as the mainstay of tuberculosis treatment. The 1950s saw the first stapling device used for lung resections. In 1962, Salzer published a series that demonstrated oncologically equivalent results for lobectomy and pneumonectomy,9 and further emphasis on lung conservation saw a series of reports on the use of segmentectomy.1, 9–10 However, in the 1980s, reports of competing long-term outcomes for segmentectomy performed for lung cancer emerged,9 fueling a debate whether segmentectomy was oncologically adequate. These debates led to the Lung Cancer Study Group’s 1995 report on a randomized trial comparing sublobar resection to lobectomy,11 which found that sublobar resection was associated with a higher incidence of recurrence and overall mortality and established lobectomy as the standard of care for lung cancer resection.
During the time of these advancements, starting in the 1930s, lung cancer increased rapidly in incidence, overshadowing other indications and finally becoming the most common indication for pulmonary resection in the 1980s. From the 1930s onward, surgery for lung cancer has become more common, with the establishment of surgical principles for the management of NSCLC (Table 1).
Table 1.
Surgical Principles for Management of NSCLC
| Surgically curable NSCLC is treated in a systematic manner with adherence to fundamental oncologic principles. The following key points need to be adhered to during resection. |
|---|
| 1. Completely remove the tumor and all intrapulmonary lymphatic drainage. The standard procedures for NSCLC resection are anatomic lobectomy, sleeve resection, bilobectomy and uncommonly, pneumonectomy. |
| 2. Take care not to transgress the tumor during resection in order to avoid tumor spillage. |
| 3. Make an effort to perform en-bloc resection of adjacent or invaded structures rather than discontinuous resection. |
| 4. Perform frozen section analysis on the bronchial margin and any other margins in close proximity to the tumor. Perform extended resection, whenever possible, if a positive resection margin is encountered. The surgeon needs to play an active role in orienting the pathologist and marking any concerning margins to improve accuracy. |
| 5. Remove or sample all accessible mediastinal lymph node stations for pathologic evaluation. These need to be anatomically and numerically labelled by the surgeon to enable precise pathologic staging in every patient. |
From Pearsons’s Thoracic and Esophageal Surgery 3rd Edition. Patterson GA, Cooper JD, Deslauriers J, Lerut AEMR, Luketich JD, Rice TW (eds.). Philadelphia: Churchill Livingstone; 2008; with permission (requested).
Video-Assisted Thoracoscopic Surgery (VATS)
Although VATS has been an important part of thoracic surgery for nearly three decades, it remains a worthwhile topic of discussion, as it is one of the most commonly offered resection approaches and as it continues to provide a platform for further advancements, most notably in the form of uniportal VATS. It is also worth noting that, while the use of minimally invasive approaches has progressively increased, open thoracotomy remains the most commonly used approach.12
Thoracoscopy was first described by the Swedish physician Han Christian Jacobaeus, who, in the late 19th century, inserted a cystoscope under local anesthesia for diagnostic purposes. He began performing lysis of adhesions using the thoracoscope and a separate second incision, which arguably represents the first VATS procedure. In the mid-1980s, therapeutic laparoscopic surgery took off, irreversibly changing general surgery. Although thoracic surgeons were interested in this new technique, thoracoscopic dissection of hilar structures proved to be challenging, as surgeons initially attempted an approach similar to open surgery, starting with completion of the fissure and control of the vessels. Contributing to the technical challenges of this approach, staplers at this time did not articulate, which made it dangerous to navigate the hilar structures from a small fixed port. Some of the first large series describing VATS techniques used simultaneous stapling of all hilar structures.13 Soon after, additional efforts found that individual hilar structures could be safely dissected and individually controlled,14 and enthusiasm for VATS grew among thoracic surgeons. However, this trend was halted by reports that pain did not differ between VATS and open techniques, concerns over oncologic adequacy, and the wide variability in techniques described in the literature, including the number and size of incisions and the use of a rib spreader.15 An important article from Cancer and Leukemia Group B set the criteria for VATS: avoidance of rib spreading; incision for specimen removal not to exceed 8 cm; individual dissection of the vein, artery, and bronchus; and standardized lymph node sampling.16 With the use of these criteria, research demonstrated that VATS did have advantages over open techniques, including decreased pain, shorter duration of chest tube drainage, shorter length of hospital stay, decreased complications, improved postoperative quality of life, and decreased inflammatory markers.17–18 In addition, long-term oncologic outcomes were equivalent to those following open techniques.19 These favorable reports helped establish VATS and, in a broader sense, minimally invasive thoracic surgery as essential tools in the thoracic surgeon’s arsenal. It is now widely accepted that, when appropriate and with consideration of the surgical principles discussed in Table 1, minimally invasive techniques should be offered to appropriate patients. Although no large-scale randomized controlled trial has compared VATS with open surgery, the feasibility of VATS has been rigorously examined by thoracic surgeons, leading to the widespread acceptance of this minimally invasive technique.
The most common VATS technique involves two to three incisions: usually a camera port in the seventh or eighth intercostal space in the anterior axillary line in a right-sided resection or the posterior axillary line in a left-sided resection, a 4-cm “utility” port directly over the lobar vein to be dissected, and an additional posterior assistant port placed in a location of the surgeon’s choosing (Figure 1). By use of these three incisions, hilar dissection, mediastinal and hilar lymph node sampling or dissection, parenchymal division, and specimen removal are performed. Following maturation and mastery of the technique, segmentectomies, bronchoplasties, sleeve resections, pulmonary arterioplasties, chest wall resections, and pneumonectomies have all been successfully performed using VATS approaches.2
Figure 1.
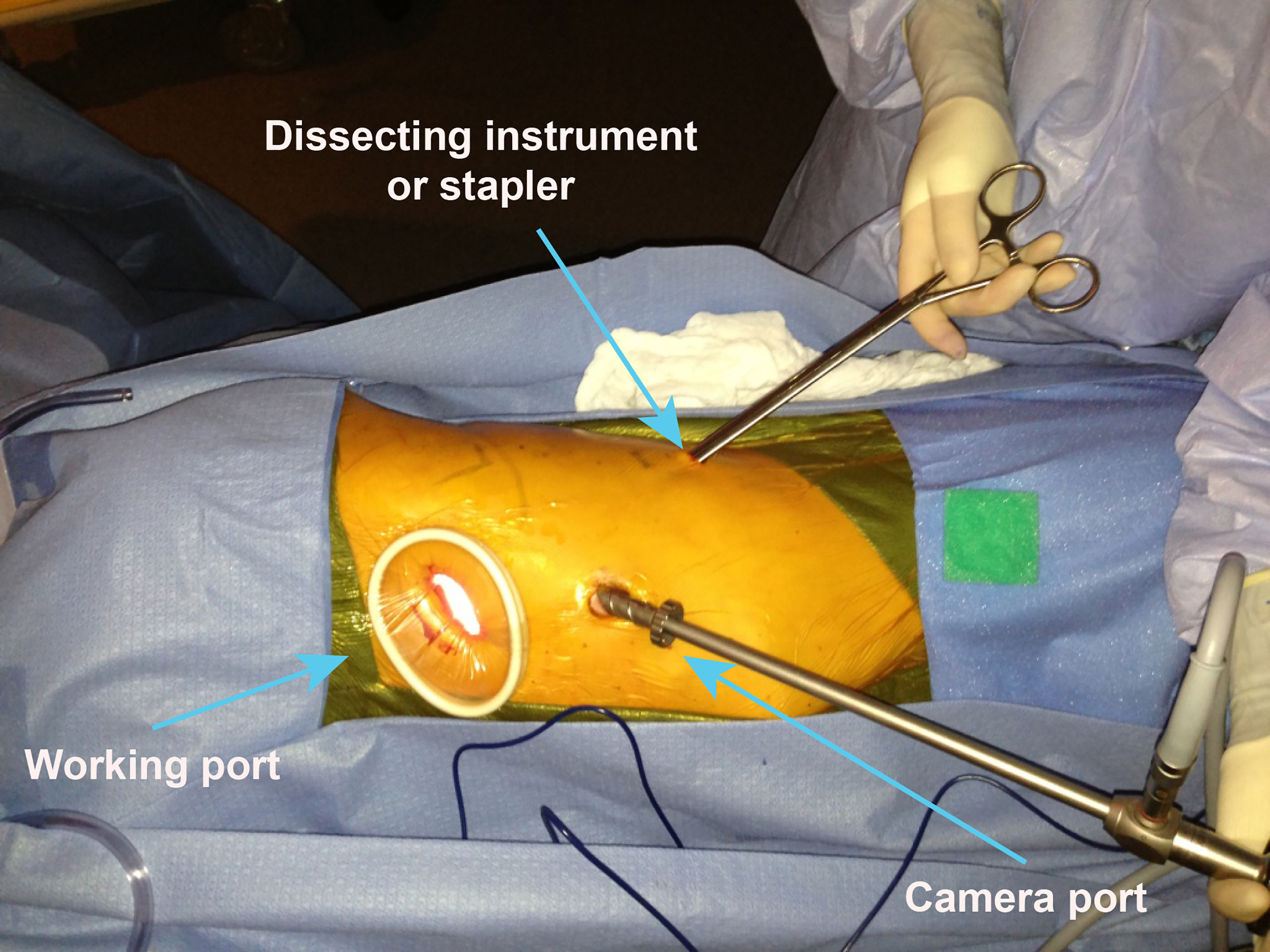
Setup for a VATS procedure.
Robotic-Assisted Thoracoscopic Surgery (RATS)
The concept of robotic surgery—as currently performed, featuring a “master-slave” system—was first explored by NASA in the 1990s as a method to provide possible surgical options for astronauts in space or soldiers on a battlefield. NASA’s Ames Research Center partnered with Stanford University to design the prototypes for telesurgery. This led to commercialization of the first FDA-approved robotic platform for civilian use, called AESOP (Computer Motion, Goleta, CA, USA), which was later replaced by the Zeus platform. Around this time, the da Vinci system (Intuitive Surgical, Sunnyvale, CA, USA) was developed, gaining FDA approval in 2000. Computer Motion and Intuitive merged in 2003, under the Intuitive name, and da Vinci became the only commercially available platform in the United States, and it continues to dominate the market today. While other robotic devices are currently undergoing development, many focus on specific areas of the body, such as the joints, spine, or brain, and no other product has been studied as extensively, with a history of peer-reviewed publications evaluating safety and efficacy. The da Vinci platform’s Si system is designed for laparoscopic and thoracoscopic surgeries and is used by many centers. The most recent iteration of the platform, the Xi system, released in 2014, provides further technological advances, including the ability to more rapidly dock and perform dissections from any angle relative to the patient’s body; smaller, thinner, longer arms; fully robotic staplers; and Firefly Fluorescence Imaging technology designed to provide real-time visualization of tissue perfusion and anatomic details. These advances have led to the wider adoption of robotic surgery approaches among an increasing number of surgeons. The following discussion will focus on the da Vinci platform, which is the most common system used for RATS worldwide.
The da Vinci Xi system comprises three main components: the master console, the surgical cart, and the vision cart. The master console consists of a seated console that can be manipulated to provide ergonomic support for the surgeon, who looks into a high-definition 3-D display, including speakers and a microphone, that was designed to facilitate communication with the bedside personnel. The visual display is magnified up to 10 times, allowing the surgeon to see target structures at the same level as in open procedures using loupe surgical telescopes. The movements of the console’s hand controls are translated to the movements of the surgical arms and instructions. The wristed instruments allow seven degrees of freedom, with tremor cancellation, allowing more range of motion than the native human hand. The surgical cart holds the boom, which consists of four arms, where instruments and the camera are docked and placed into the thoracic cavity via small incisions. The boom can be directed to approach the target from a variety of angles, and preprogrammed surgical arm positioning is used to maximize the surgical capability on the basis of the target. The bedside assistant plays a critical role in docking and deploying the surgical arms in a safe and efficient manner. Finally, the vision cart holds a high-definition monitor, in addition to much of the hardware that connects and controls the three components. The system’s software runs safety checks throughout the entire duration of use to prevent malfunction. One of the downsides of the platform is that it lacks haptic feedback to the surgeon, which can result in tissue injury, especially when a novice to the technique is performing the operation. However, despite the lack of haptic feedback, the ergonomic design of the console, the motion scaling, and the lack of fulcrum effect decrease musculoskeletal fatigue in the surgeon, allowing for consistent performance during longer, difficult cases and possibly resulting in fewer conversions.20–21
Intuitive Surgical has developed simulators that play a critical role in training surgeons to use the platform, and all surgeons seeking certification with the company for independent surgery on the platform are required to qualify on these simulators. Dual consoles further facilitate training by creating a system in which the learner has the same view of the surgical field as the more experienced surgeon and control of the instruments can be exchanged between consoles, allowing the more experienced surgeon to assume control quickly if necessary. On-screen pointers developed specifically to facilitate communication between surgical team members aid in coaching and guiding a training surgeon through a procedure. Operating room personnel, including the bedside assistant, scrub assistant, and circulator, may also need to become familiarized with the platform, and training for these team members is available. These tools have made the process of training to become a robotic surgeon safe and efficient.22
The first robotic lobectomy was reported by Melfi et al.23 in 2002, and since then reports have demonstrated reduced postoperative pain and shorter hospital length of stay, compared with open thoracic surgery. In an analysis of state inpatient databases, Kent et al. found a significant reduction in mortality (0.2% vs 2.0% in open) and reduced mortality, length of stay, and complications (although these differences were not statistically significant) for RATS compared with VATS procedures.24 RATS also appears to have a lower rate of conversion to open procedures25 and allows a minimally invasive approach for many cases that would have previously needed to be done via open thoracotomy. No randomized controlled trial has investigated outcomes between RATS and VATS or open techniques. However, several reports have found comparable long-term outcomes for RATS compared with VATS and open approaches.26–27 When rate of nodal upstaging was examined as a surrogate for completeness of nodal dissection and, therefore, oncologic quality of surgery, RATS was equivalent to open thoracotomy, demonstrating that RATS is an efficacious surgical technique for NSCLC.28
One of the main criticisms of RATS is the cost involved in its use,29 which is no doubt related to the high initial cost of the robotic platform and increased operative time. Its proponents claim that the decreased length of stay and overall complications offset the cost of the operation, but this is still undergoing study. What is clear is that the use of RATS is steadily increasing—in the early 2000s, RATS made up <1% of all major pulmonary surgeries performed; currently, nearly 20% of lobectomies in the United States are performed using RATS. Some reports have found, at least at high-volume centers, no differences in the cost of RATS versus other techniques.30 Moreover, the aforementioned technical advantages have allowed surgeons to provide minimally invasive approaches in difficult cases that would have previously been relegated to an open approach, such as cases including patients who have undergone induction therapy, obese patients with limited intrathoracic space, and patients with locally advanced disease. This capability may offset the cost of the technique, but this topic is difficult to study, as these patients comprise a heterogeneous group. We believe that, although the verdict on RATS is still out, it is a valid tool for thoracic surgery for NSCLC.
Uniportal VATS/RATS
As mentioned earlier, the use of the medical thoracoscope for diagnostic procedures in the 19th century likely represents the first uniportal, or single-port, VATS procedure. However, uniportal minimally invasive thoracic surgery, as it is performed today (wedge resection using a single 2.5-cm incision), was first reported in 2004.31 This technique’s potential was further demonstrated in 2011, when Gonzales-Rivas et al. described the first uniportal lobectomy performed using a 4-cm anterior incision.32 Since then, segmentectomies, pneumonectomies, and more-complex surgeries, including sleeve resections, tracheal resections, and lobectomies with en bloc chest wall resections, have been described. Initially, these more complex procedures were thought to be the work of an exceptional surgeon and unlikely to be replicated by the thoracic surgical community as a whole. However, the uniportal approach was soon excitedly received by surgeons in Europe and Asia, many of whom later demonstrated the efficacy and feasibility of the approach. In contrast, adoption of this approach has been slower in the United States, where multiportal VATS is still much more common. Additionally, surgeons performing uniportal VATS increasingly do so with the patient undergoing spontaneous ventilation33—a throwback to an older anesthesia approach that is now slowly regaining a foothold among surgeons who favor uniportal surgery and is especially useful for patients who are frail and have compromised pulmonary function.
The rapid expansion of the uniportal approach has promoted further innovations of the various tools involved. New thoracoscopes with a range of vision from 0 degrees to 120 degrees have been developed, allowing broad-ranging views without having to torque the scope. Mechanized camera-holding arms allow the surgeon to become truly “unisurgeon,” operating without the need for an assistant, while 3-D–capable thoracoscopes allow further precision. These advances in visualization have occurred in parallel with the development of more-sophisticated instruments, including double-articulated instruments as well as staplers with curved tips or narrower tips and shafts. Magnetic retraction devices and magnetic wireless cameras are being developed, which will further aid in performing a wide range of surgeries through a single small incision.
Although studies investigating outcomes of uniportal VATS have mostly been performed in a single institution with a small number of patients, they have reported that uniportal VATS appears to be associated with less short- and long-term pain and, in experienced hands, less blood loss, shorter duration of surgery, and shorter duration of chest tube drainage, compared with multiportal VATS.34 Data on long-term oncologic outcomes are lacking, and it has been noted that posterior mediastinal nodal dissection is more challenging using a uniportal VATS approach. Although the few data that exist are mostly of a short-term nature, the current findings seem to suggest equivalent results between uniportal VATS and other approaches.35
Intuitive Surgical is currently testing a uniportal robotic platform; however, it is not yet commercially available. By use of a single subxiphoid port, the robot is docked and used for surgery. It remains to be seen what role uniportal RATS may play in the treatment of NSCLC.
Interventional Bronchoscopy
The relationship between interventional pulmonologists and thoracic surgeons is still being defined, as new developments and technologies disrupt previous expectations. These developments include the widespread adoption of endobronchial ultrasound–guided transbronchial nodal biopsies; the ability to reach, biopsy, and localize peripheral lesions via electromagnetic navigational bronchoscopy (ENB); and robotic bronchoscopy. The evolution of these technologies provides an exciting glimpse into the future of minimally invasive approaches for the diagnosis and treatment of NSCLC. Thoracic surgeons and interventional pulmonologists have always worked closely together and will no doubt continue to do so. Among the ongoing technologic advances, ENB and robotic bronchoscopy will be briefly discussed.
In 2004, the FDA approved the use of the superDimension system (Medtronic, St. Paul, MN, US), a minimally invasive image-guidance localization and navigation system that uses electromagnetic guidance to reach peripheral lung lesions. The software superimposes images from a specifically protocoled chest CT onto data collected from a position sensor at the tip of a flexible catheter, allowing navigation of the bronchoscope within the bronchus farther out into the pulmonary parenchyma. This technique has been mostly used for tissue diagnosis of peripheral lesions or placement of fiducials or radioisotope dye to facilitate destruction or resection of hard to locate peripheral tumors. While most studies investigating this technique have been small, the largest to date, which was a short-term interim analysis of a larger prospective multicenter study (NAVIGATE), demonstrated a 94.4% navigation and biopsy completion rate, with a postprocedure pneumothorax rate of 4.9% and an overall 3.2% grade 2 or higher complication rate.36 One criticism of the superDimension system is that it is overly time-consuming to use, as this system requires the protocolized CT to be preloaded, and there is some loss of maneuverability as the endoscope reaches the periphery of the lung.
Robotic bronchoscopy was developed to overcome these issues. Two companies nearly simultaneously began offering robotic bronchoscopy platforms commercially in 2018. The Monarch system (Auris Surgical Robotics, San Carlos, CA, US) and the Ion system (Intuitive Surgical, Sunnyvale, CA, US) both offer robotic platforms using the master-slave configuration. Although they have been designed to address the gaps in ENB technology, the outcomes, safety, and efficacy of these systems remain to be determined.
Localization Techniques
As CT lung-cancer screening became widely accepted and the American Association for Thoracic Surgery, National Comprehensive Cancer Network, American Society of Clinical Oncology, American Lung Association, and American Cancer Society endorsed its use, around 2012, surgeons began seeing an increase in patients with impalpable subsolid lesions not visible from the surface who were referred for diagnostic or therapeutic resection. At the same time, there was renewed interest in the use of sublobar resection for the treatment of NSCLC, which is currently under study in multiple national randomized trials. This change in presentation inspired the development of therapeutic procedures that are able to provide accurate localization of these invisible, impalpable lesions while also preserving as much pulmonary parenchyma as possible. Multiple methods to localize lesions and other anatomic details of the target tissue have been developed (Table 2).
Table 2.
Methods to localize lesions and other anatomic details of the target tissue
| Method | Comments | |
|---|---|---|
| Indocyanine green (ICG) | Percutaneous image–guided or bronchoscopic-guided injection of ICG into lesion. When used for anatomic delineation, frequently intravenous administration is used. Viewed using fluorescence viewing camera using near-infrared light (Firefly [Intuitive], Pinpoint [Stryker], etc.). | Can also delineate segmental parenchymal planes or vascular anatomy. |
| Wire localization | Image (usually CT)–guided placement of conventional mammographic guide wire, usually just before surgery. | Guide wire dislodgement is possible, and certain anatomic locations such as apex, diaphragm, and the great vessels require caution. |
| Radioisotopes (technetium-99m [Tc99m]) | Tc99m-tagged albumin is injected into lesion, usually using CT guidance. Postprocedure scintigraphy is often performed. Intraoperative use of gamma-ray–detecting probe allows for lesion localization. | The radiotracer is stable for 24 h and allows for continued probe use during and after resection to confirm removal of lesion. |
| Ultrasound | Thoracoscopic ultrasound probe (usually 10 mm in diameter) used to detect lesion in deflated lung. | Highly operator-dependent and requires complete collapse of lung. Subsolid lesions may not be as easily detectable. |
| Dye or contrast medium (lipiodol, cyanoacrylate, dyed collagen, barium, methylene blue, etc.) | The dye or contrast medium is injected into the lesion and is either visible to the naked eye or seen with fluoroscopic visualization. | Methylene blue can rapidly diffuse into surrounding tissues, significantly decreasing accuracy. Barium can cause local lung inflammation, influencing the pathologic diagnosis. |
| Fiducial marker or microcoil | Using CT or bronchoscopic guidance, metal microcoils (15–80 mm in length, platinum) or fiducial markers (1.3 × 3 mm, gold) are placed into the lesion. During surgery, the microcoil or fiducial can be directly palpated or located using fluoroscopy. | Less likely to dislodge, compared with guide wire localization, and less discomfort to the patient. |
Often these methods are combined to increase the accuracy and sensitivity of the localization. For instance, technetium-99m may be injected with a dye or wire localization may be combined with a dye injection. Moreover, to improve the patient experience while minimizing procedure time and risk, surgeons are using hybrid operating rooms with built-in imaging capabilities that allow localization and surgery under one anesthetic and without the need to move settings. This has been called image-guided VATS, or iVATS, and is currently under study. At present, hybrid rooms for iVATS are available only in select academic centers, but given the increasing use of hybrid operating rooms for vascular or cardiac surgeries, iVATS may become more prevalent in the future.
3-D Printing
The first 3-D printer was developed in the early 1990s and was used for industrial purposes. Twenty years later, surgeons began exploring the use of this technology, especially for surgical planning for complex anatomical areas in cases in which the patient has a complicated surgical history or the surrounding structures are intricately involved, as well as for education and communication across multiple disciplines. Providing a 3-D model of the patient’s disease and anatomy uniquely promotes patient education, as it does not rely on the ability of the patient to view two-dimensional images and as it enables the surgeon to better explain the complex anatomy involved in surgical decisions. Thoracic surgeons have taken advantage of this technology, most often for use with Pancoast, mediastinal, and chest wall tumors. A team at Mayo Clinic described the use of five dimensions, adding change in tumor size over time during treatment and physiology as measured by PET scan.37 Reports of the use of 3-D printing to aid in surgical planning demonstrate that it can play a role in complex, high-risk surgeries,38 but this technology is not available everywhere and is currently used only in specific high-volume academic centers.
3-D printers have a second fundamental function that relates to the reconstructive and restorative use of 3-D technology. Bioprinting and the creation of custom-made 3-D structures, with the purpose of reconstructing patient-tailored unique tissues and organs, is also being examined.39 For the thoracic surgeon, these tissues may be vascular structures, the airway, or the chest wall. Although this technology is still being developed and is not yet available for mainstream use, we anticipate it will eventually allow more patients to undergo life-saving surgical treatment.
Summary
The field of thoracic surgery has a rich history of innovation and improvement to achieve the best possible outcomes using the technology and knowledge available at the time. While technological advances are constantly being pursued, the core surgical principles of oncologic quality are kept at the forefront of our minds, and any novel approach must be measured against benchmarks that have been established over the course of this history. The thoracic surgeon must stay abreast of these advances to ensure the patient is offered the safest and most efficacious treatment option available. For providers who are not surgeons, being aware of the full breadth of available surgical treatment options will help them counsel patients and refer them appropriately.
Key Points.
VATS allows decreased pain, shorter hospital stays, and lower complication rates coupled with equivalent oncologic outcomes, compared with open surgery.
RATS provides similar outcomes to VATS and serves as a minimally invasive option for patients who otherwise may require an open approach.
Uniportal VATS is safe for most common operations, although it is more popular in Asia and Europe, and is associated with decreased surgical pain, compared with multiportal VATS.
Techniques to localize small invisible and/or impalpable lesions and 3-D printing technology allow surgeons to provide efficacious and safe surgery to more patients.
Synopsis.
Surgery for non-small cell lung cancer has undergone repeated innovations over time. Although medical thoracoscopy has been available for centuries, it was not incorporated into the standard approach until the 1990s, when successful video-assisted thoracoscopic surgery (VATS) techniques were widely reported. Progressive efforts to offer minimally invasive approaches while maintaining oncologic surgical quality led to the development of robotic-assisted thoracic surgery and uniportal VATS, which offer improved pain control, shorter hospital stays, and more patients able to receive adjuvant therapy. Innovations in interventional bronchoscopy, localization methods, and 3-D printing have improved the safety, efficacy, and precision of surgery.
Footnotes
Disclosure Statement: All authors have no relevant disclosures.
References
- 1.Kittle C The history of lobectomy and segmentectomy including sleeve resection. Chest Surg Clin N Am. 2000;10(1):105–130. [PubMed] [Google Scholar]
- 2.Walcott-Sapp S, Sukumar MS. The history of pulmonary lobectomy: two phases of innovation. December 8, 2016. Accessed September 12, 2019. Available at: https://www.CTSnet.org/article/history-pulmonary-lobectomy-two-phases-innovation.
- 3.Antony M Case of extensive caries of the fifth and sixth ribs, and disorganization of the greater part of the right lobe of the lungs; with a description of the operation for the same. London Med Phys J. 1924:51:114–121. [PMC free article] [PubMed] [Google Scholar]
- 4.Meyer JA. Hugh Morriston Davies and lobectomy for cancer, 1912. Ann Thorac Surg. 1988;46(4);472–474. [DOI] [PubMed] [Google Scholar]
- 5.Lilienthal H Resection of the lung for suppurative infections, with a report based on 31 operative cases in which resection was done or intended. Ann Surg. 192;75:257–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brunn H Surgical principles underlying one-stage lobectomy. Arch Surg. 1929;18:490. [Google Scholar]
- 7.Graham EA, Singer JJ. Successful removal of an entire lung for carcinoma of the bronchus. JAMA. 1933;01:1371–1374. [DOI] [PubMed] [Google Scholar]
- 8.Churchill ED, Belsey R. Segmental pneumonectomy in bronchiectasis. Ann Surg. 1939;109:481–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kutschera W Segment resection for lung cancer. Thorac Cardiovasc Surgeon. 1984;32:102–104. [DOI] [PubMed] [Google Scholar]
- 10.Bonfils-Roberts EA, Clagett OT. Contemporary indications for pulmonary segmental resections. J Thorac Cardiovasc Surg. 1972;63:433–438. [PubMed] [Google Scholar]
- 11.Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg. 1995;60(3):615–622. [DOI] [PubMed] [Google Scholar]
- 12.Oh DS, Reddy RM, Gorrepati ML, Mehendale S, Reed MF. Robotic-assisted, video-assisted thoracoscopic and open lobectomy: propensity-matched analysis of recent Premier data. Ann Thorac Surg. 2017;104(5):1773–1740. [DOI] [PubMed] [Google Scholar]
- 13.Lewis RJ, Caccavale RJ, Sisler GE, Mackenzie JW. One hundred consecutive patients undergoing video-assisted thoracic operations. Ann Thorac Surg. 1992;54:421–426. [DOI] [PubMed] [Google Scholar]
- 14.McKenna RJ. Lobectomy by video-assisted thoracic surgery with mediastinal node sampling for lung cancer. J Thorac Cardiovasc Surg. 1994;107:879–882. [PubMed] [Google Scholar]
- 15.Rocco G, Internullo E, Cassivi SD, Van Raemdonck D, Ferguson MK. The variability of practice in minimally invasive thoracic surgery for pulmonary resections. Thorac Surg Clinic. 2008;18(3):235–247. [DOI] [PubMed] [Google Scholar]
- 16.Swanson SJ, Herndon JE 2nd, D’Amico TA, et al. Video-assisted thoracic surgery lobectomy: report of CALGB 39802—a prospective, multi-institution feasibility study. J Clin Oncol. 2007;25:4993–4997. [DOI] [PubMed] [Google Scholar]
- 17.Whitson BA, Groth SS, Duval SJ, Swanson SJ, Maddaus MA. Surgery for early-stage non-small cell lung cancer: a systematic review of the video-assisted thoracoscopic surgery versus thoracotomy approaches to lobectomy. Ann Thorac Surg. 2008;86(6):2008–2016. [DOI] [PubMed] [Google Scholar]
- 18.Flores RM, Alam N. Video-assisted thoracic surgery lobectomy (VATS), open thoracotomy, and the robot for lung cancer. Ann Thorac Surg. 2008;85(2):S710–S715. [DOI] [PubMed] [Google Scholar]
- 19.Lee PC, Nasar A, Port JL, et al. Long-term survival after lobectomy for non-small cell lung cancer by video assisted thoracic surgery versus thoracotomy. Ann Thorac Surg. 2013;96(3):951–960. [DOI] [PubMed] [Google Scholar]
- 20.Choe G, Park B. Robotic-assisted thoracoscopic surgery (RATS) lobectomy. Ann Cardiothorac Surg. 2019;8(2):296–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reddy RM, Gorrepati ML, Oh DS, Mehendale S, Reed MF. Robotic-assisted versus thoracoscopic lobectomy outcomes from high-volume thoracic surgeons. Ann Thorac Surg. 2018;106(3):902–908. [DOI] [PubMed] [Google Scholar]
- 22.Cerfolio RJ, Cichos KH, Wei B, Minnich DJ. Robotic lobectomy can be taught while maintaining quality patient outcomes. J Thorac Cardiovasc Surg. 2016;152(4):991–997. [DOI] [PubMed] [Google Scholar]
- 23.Melfi FM, Menconi GF, Mariani AM, Angeletti CA. Early experience with robotic technology for thoracoscopic surgery. Eur J Cardiothorac Surg. 2002;21(5):864–868. [DOI] [PubMed] [Google Scholar]
- 24.Kent M, Wang T, Whyte R, Curran T, Flores R, Gangadharan S. Open, video-assisted thoracic surgery, and robotic lobectomy: review of a national databases. Ann Thorac Surg. 2014;97(1):236–242. [DOI] [PubMed] [Google Scholar]
- 25.Park BJ, Flores RM, Rusch V. Robotic assistance for video-assisted thoracic surgical lobectomy: technique and initial results. J Thorac Cardiovasc Surg. 2006;131(1):54–59. [DOI] [PubMed] [Google Scholar]
- 26.Park BJ, Melfi F, Mussi A, et al. Robotic lobectomy for non-small cell lung cancer (NSCLC): long-term oncologic results. J Thorac Cardiovasc Surg. 2012;143:383–389. [DOI] [PubMed] [Google Scholar]
- 27.Cerfolio RJ, Ghanim AF, Dylewski M, Veronesi G, Spaggiari L, Park BJ. The long-term survival of robotic lobectomy for non-small cell lung cancer: a multi-institutional study. J Thorac Cardiovasc Surg. 2018;155(2):778–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wilson JL, Louie BE, Cerfolio RJ, et al. The prevalence of nodal upstaging during robotic lung resection in early stage non-small cell lung cancer. Ann Thorac Surg. 2014;97:1901–1906. [DOI] [PubMed] [Google Scholar]
- 29.Singer E, Kneuertz PJ, D’Souza DM, Moffatt-Bruce SD, Merritt RE. Understanding the financial cost of robotic lobectomy: calculating the value of innovation? Ann Cardiothorac Surg. 2019;8(2):194–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kneuertz PJ, Singer E, D’Souza DM, Abdel-Rasoul M, Moffatt-Bruce SD, Merritt RE. Hospital cost and clinical effectiveness of robotic-assisted versus video-assisted thoracoscopic and open lobectomy: a propensity score-weighted comparison. J Thorac Cardiovasc Surg. 2019;157(5):2018–2026. [DOI] [PubMed] [Google Scholar]
- 31.Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg. 2004;77(2):726–728. [DOI] [PubMed] [Google Scholar]
- 32.Gonzalez-Rivas D, de la Torre M, Fernandez R, Mosquera VX. Single-port video-assisted thoracoscopic left upper lobectomy. Interact Cardiovasc Thorac Surg. 2011;13(5):539–541. [DOI] [PubMed] [Google Scholar]
- 33.Guido-Guerrero W, Bolaños-Cubillo A, González-Rivas D. Single-port video-assisted thoracic surgery (VATS)-advanced procedures and update. J Thorac Dis. 2018;10(Suppl 14):S1652–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bourdages-Pageau E, Vieira A, Lacasse Y, Figueroa PU. Outcomes of uniportal vs multiportal video-assisted thoracoscopic lobectomy. Semin Thorac Cardiovasc Surg. 2019. [DOI] [PubMed] [Google Scholar]
- 35.Harris CG, James RS, Tian DH, et al. Systematic review and meta-analysis of uniportal versus multiportal video-assisted thoracoscopic lobectomy for lung cancer. Ann Cardiothorac Surg. 2016;5(2):76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khandhar SJ, Bowling MR, Flandes J, et al. Electromagnetic navigation bronchoscopy to access lung lesions in 1,000 subjects: first results of the prospective, multicenter NAVIGATE study. BMJ Pulm Med. 2017;17(1):59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gillaspie EA, Matsumoto JS, Morris NE, et al. From 3-dimensional printing to 5-dimensional printing: enhancing thoracic surgical planning and resection of complex tumors. Ann Thorac Surg. 2016;101(5):1958–1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.George E, Barile M, Tang A, et al. Utility and reproducibility of 3-dimensional printed models in pre-operative planning of complex thoracic tumors. J Surg Oncol. 2017;116(3):407–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gu BK, Choi DJ, Park SJ, Kim MS, Kang CM, Kim CH. 3-dimensional bioprinting for tissue engineering applications. Biomater Res. 2016;20:12. [DOI] [PMC free article] [PubMed] [Google Scholar]


