Abstract
Introduction:
Individuals with multimorbidity in deprived areas experience worse health outcomes and fragmented care. Research suggests that primary care-based link workers providing social prescribing have potential to improve health and well-being. This paper reports the results of a pilot study conducted in preparation for a randomised controlled trial (RCT) that aims to test the effectiveness of primary care-based link workers providing social prescribing in improving health outcomes for people with multimorbidity who attend general practices in deprived areas in Ireland.
Methods:
An uncontrolled pilot study of an intervention based on the Glasgow Deep End links worker programme, in a single general practice, tested the feasibility and acceptability of planned processes for a RCT. Outcomes were recruitment and retention rates and acceptability of the trial processes and intervention to patients, general practitioners (GPs) and the link worker. Structured interviews were conducted with six patients, the link worker and two GPs within the practice and analysed using descriptive qualitative analysis. Feedback from a Public Patient Involvement group and an Implementation Advisory Group of key stakeholders was incorporated into the evaluation process.
Results:
Twelve out of 14 patients completed the intervention. Selection and recruitment processes were lengthier than expected. GPs recommended including psychosocial need in the selection process. Interviewed patients, the GPs and the link worker were positive about the intervention.
Conclusion:
A range of adaptations were identified for the main trial, mainly considering psychosocial need in the selection process to reflect normal referral pathways. This has resulted in a pragmatic RCT design.
Keywords: Link worker, social prescribing, multimorbidity, complex intervention, primary care, general practice, social deprivation
Introduction
Although many definitions of multimorbidity exist, it is generally recognised as a person having two or more chronic physical and/or mental health conditions. Multimorbidity is recognised as a significant challenge for individuals and health systems internationally, particularly in areas of social deprivation1 and is estimated to affect 66% of individuals over 50 attending Irish General Practice.2 There are strong associations between multimorbidity and education, employment status and household income3 with higher proportions of individuals with complex multimorbidity living in deprived areas.4 Interventions that facilitate engagement in health promoting activities among people with multimorbidity living in deprived areas may be appropriate, though there is limited evidence to support their effectiveness.5
Social prescribing enables general practitioners (GPs), and other health professionals, to refer individuals to a range of non-clinical services provided by the voluntary and community sector.6 The majority of social prescribing models involve patients meeting with a non-health or social care professional, commonly known as a link worker, with extensive knowledge of local community resources and services. A primary care-based link worker providing social prescribing is a potential intervention to support people with multimorbidity to access activities and services in their community to facilitate the self-management of physical and mental health conditions, and may improve health outcomes.
Link workers providing social prescribing services have been gaining popularity internationally, but few have been formally evaluated.6 There have also been a number of pilots in Ireland.7,8 The limited number of RCTs conducted internationally have not reported improved health outcomes.9,10 A quasi-experimental evaluation of the Glasgow Deep End links worker programme in GP practices in areas of deprivation reported improvements in health related quality of life and mental health for patients who met the link worker at least 3 times, but no difference in the intention to treat analysis. They concluded that there remained inadequate evidence to support link workers, but acknowledged the difficulty of finding suitable matched controls, which could be overcome with randomisation at the individual patient level.11
The Deep End Group in Ireland have also emphasised the potential value of this model of care.12 We are conducting a pragmatic randomised trial in 10 Deep End general practices in Ireland using an adapted version of the Glasgow Deep End links worker intervention, with link workers embedded in practices in deprived urban areas, and specifically targeting adults with multimorbidity. The trial was originally scheduled to take place between April and September 2020. In line with the Medical Research Council Guidance on evaluating complex interventions we piloted the intervention to test feasibility and trial processes.13 In this uncontrolled pilot study the feasibility of delivering this adapted intervention was tested within a single practice in relation to selection, recruitment, data collection and intervention processes to ensure they were timely and acceptable. The results informed the protocol for the definitive pragmatic randomised controlled trial (RCT) and economic evaluation.14
Specifically the objectives of the pilot study were to
To assess if selection processes correctly identified intended trial participants without undue workload burden on GPs
To investigate the feasibility and acceptability of trial recruitment and data collection processes
To investigate the acceptability of the intervention with the GPs, a link worker and study participants
To test usability of a client management database specifically designed for the intervention
Methods
An uncontrolled pilot study collecting quantitative and qualitative data was conducted in a single GP practice over a 6-week period from November 2019 to January 2020 with 12 patients. The results were then presented to a Public and Patient Involvement group and an Implementation Advisory group affiliated with this research who made suggestions for adjustments to recruitment materials and selection processes for the main trial protocol. Ethical approval was granted by the Irish College of General Practitioners Research Ethics committee.
Sample
A single practice, located in an area of deprivation (defined as serving two or more small areas rated as disadvantaged by the Pobal Deprivation Index,15 took part in the pilot. Due to inconsistent coding methods for chronic diseases, the presence of polypharmacy (a recognised proxy for multimorbidity) was used to search for potentially eligible participants.16 The lead GPs were initially asked to generate a list of all patients on ≥5 regular medications. However, this produced an unmanageable list due to medication lists not being updated, so for the purposes of this pilot having ≥8 regular medications was used. This returned a list of 823 potentially eligible patients. The practice used a random number generator in Excel to select 15 patients and their medical records were double-checked by the GPs against the eligibility criteria including verifying that they had two or more chronic conditions
Recruitment
Following identification of 15 eligible patients, the GP sent each one an invitation letter, the patient information leaflet and a consent form. The GP telephoned each potential participant 4–5 days later to explain the study. Those who consented were sent baseline questionnaires with a follow-up phone call several days later from the research team to see if assistance was required with questionnaire completion. Once baseline data collection was completed, patients were referred to the link worker.
Intervention
The primary care-based link worker intervention is based on the Glasgow Deep End links worker programme in Scotland.11 Patients were invited to meet the link worker at the GP practice. At the first meeting the link worker explained their role, discussed patient’s health and social care needs and provided them with a relevant list of community resources that could potentially help them to address these needs. The link worker then engaged with them over a 6-week period to support them to access recommended community resources. The intensity of the support offered was tailored to the individual needs of the patient, and this varied from a simple follow up phone call to accompanying the person to community activities. Support was classified into instrumental (doing things for patients), informational (passing on information), emotional (listening and supporting) or appraisal (helping people to assess situations and make plans).17
Data collection
Data on numbers of eligible patients invited was collected from the GP. The research team monitored number of patients who consented, returned baseline questionnaires and the time it took for this. Demographics of patients and baseline patient reported outcome measures (PROMs), were obtained from self-reported questionnaires mailed to patients and completed prior to the intervention. Follow up questionnaires were mailed on completion of the 6 week intervention. The questionnaires collected basic demographic information and the following PROMs:
Health related quality of life as measured by EQ-5D-5L18
Mental health as measured by Hospital Anxiety and Depression Scale19
Activities of daily living as measured by the Frenchay Activity Index20
Self-management as measured by the Patient Activation Measure21
Burden of treatment measured by Multimorbidity Burden of Treatment Questionnaire22
Social Connectedness Scale23
Interactions with the link worker were recorded in a specifically designed client management database using Microsoft Access.24 The database allows collection of data on the frequency and nature of link worker support (instrumental, informational, emotional or appraisal type support17), issues facing patients that they discussed with the link worker and the community resources to which patients were referred.
Feedback on acceptability and feasibility of the trial processes and interventions was obtained using structured interviews with the two principal GPs at the practice, the link worker and a convenience sample of six patients. (Two patients were too unwell, one had dropped out, one declined an interview and two were not available within the time frame of the research). Interviews were conducted over the phone and lasted 10 to 15 minutes. A written record of responses was kept and direct quotes noted where relevant.
Data analysis
Simple descriptive statistics were used to describe patient demographic details and recruitment processes. Data generated through the structured interviews were analysed using a qualitative descriptive approach. This approach to qualitative data analysis is considered suitable for design of complex interventions as the focus of analysis is descriptive rather than interpretive.25
Public and Patient Involvement (PPI)
This study had PPI embedded in it by the engagement of a multimorbidity patient advisory group. Table 2 outlines the input and outcomes of PPI based on the GRIPP-2 guidelines for reporting PPI.26
Table 2.
Public patient involvement reported according to GRIPP 2 short form.
| 1: Aim |
| The aim of the PPI was to provide the perspective of people living with multimorbidity on specific issues identified during the pilot study |
| 2: Methods |
| An advisory panel of 12 people living with multimorbidity was recruited via existing networks of students on a PhD programme in multimorbidity. The panel meets quarterly to provide input on issues brought to them by the PhD students. The members are voluntary but receive a voucher to acknowledge their time and associated costs attending. The panel had been meeting for a year prior to providing input on this study. The meeting at which this study was discussed took place at the Royal College of Surgeons in Ireland, lasted 2 hours in total including a break and was facilitated by BK and 2 other PhD students on the multimorbidity PhD programme. There was 1 hour to discuss issues with them and so their input was sought on three areas only outlined below. For this study BK asked the panel to read the patient information leaflet and comment on their understanding of the link worker intervention. They also provided feedback on the wording and layout of the patient information leaflet. The group tested a revised version of the community resources costs questionnaire by filling it in and feeding back suggestions to BK. They were asked how best to phrase the reason they had been invited by their GP to be part of the study. |
| 3: Study results |
| The PPI advisory group reviewed the patient information leaflet and made suggestions to improve it including reordering of sections to prioritise information about the intervention, adjusting language, and reducing repetition. They gave feedback on what they felt the essential information was and contributed to a brochure summarising this. They found the revised version of the patient costs section of the questionnaire straightforward to fill in. Their opinion was sought on informing patients why they had been chosen to take part in the research. They approved the wording in the leaflet informing people that they had been invited due to having two or more ongoing health conditions and that their GP felt they may benefit from meeting the link worker. |
| 4: Discussion and conclusions |
| The input of this group led to changes to recruitment materials which will hopefully lead to a better understanding of the intervention and enhance recruitment. Notably the PPI group felt the term ‘multimorbidity’ and ‘chronic condition’ were negative and recommended removing these from any literature. They also felt that the information leaflets were overly cautious and read more like the small print in an insurance policy rather than a research study. The group unprompted brought up changing the name. Ultimately, the researchers did not act on the groups suggestion to rename as the link worker concept was already familiar to many GPs and community resource providers. |
| 5: Reflections/critical perspective |
| The PPI group gave useful feedback on the recruitment material, but it will not be possible to objectively test the impact this has on recruitment. The PPI group composition differed slightly from that of the target group for the intervention in that they came from all socioeconomic backgrounds. However, all members of the PPI group had experience of multimorbidity. The group have developed a relationship with the researcher over time and this allowed for a frank and productive conversation. Ultimately it would have been preferable to get the PPI group input prior to the pilot and again afterwards, but research team time constraints and capacity issues for the group, as they advise on 3 other projects, meant this was not possible. |
Implementation advisory group
The implementation advisory group consisted of four GPs working in deprived areas with and without prior experience of social prescribing, a GP with experience of running a trial of a complex intervention in primary care and a social prescribing coordinator from a well-established social prescribing project in a deprived inner-city area. They were presented with the results of the pilot and then they provided advice on the selection and recruitment in practice for the main trial.
Results
Feasibility of selection, recruitment and data collection processes
Fourteen out of 15 selected eligible patients returned consent forms. Twelve (80%) of the 14 patients who consented to participate completed the intervention, but only 11 (73%) returned the baseline questionnaire. One person who had consented, but had not completed baseline data collection, was referred to the link worker in error. The process of recruitment and baseline data collection took 6 weeks. Eight of the 14 consented participants (57%) returned the follow up questionnaire within an average of 1 week. There was no second mailing of follow-up questionnaires or no follow-up calls to boost the final response rate due to time constraints for completion of the pilot study. See Table 1 for demographics and baseline scores of patient-reported outcome measures.
Table 1.
Patient characteristics at baseline.
| Characteristic | Value |
|---|---|
| Age γ (SD) | 63 (9.9) |
| Female % | 70 |
| Primary education only % | 45 |
| Employed % | 18 |
| Lives alone % | 36 |
| GMS Card 1 % | 64 |
| Number of self-reported health conditions γ (SD) | 2.6 (1.1) |
| EQ-5D-5L γ (SD) | 0.513 (0.21) |
| HADS A γ (SD) | 8.4 (4.6) |
| HADS D γ (SD) | 7.5 (5.1) |
| Multimorbidity Burden of Treatment: Medium or above % | 54 |
| Patient Activation Measure: Level 2 or below % | 54 |
| Activity Level: Inactive % | 9 |
1 The general medical service (GMS) card entitles holders to free primary care services and reduced medication fees. It is means tested and about 40% of the Irish population hold one. EQ-5D-5L = a standardised measure of self-reported health-related quality of life that assesses 5 dimensions at 5 levels of severity where 1 is the preferred state of health; HADS-A = Hospital Anxiety and Depression Scale, Anxiety, where a score above 8 indicates possible caseness; HADS-D = Hospital Anxiety and Depression Scale, Depression, where a score above 8 indicates possible caseness; Multimorbidity burden of treatment questionnaire categorises burden as none, low, medium or high; Patient Activation Measure categorises activation from level 1 to 4 with 1 being least activated; Frenchay activity index categorises people as inactive, moderately active or very active based on work, leisure and domestic activity.
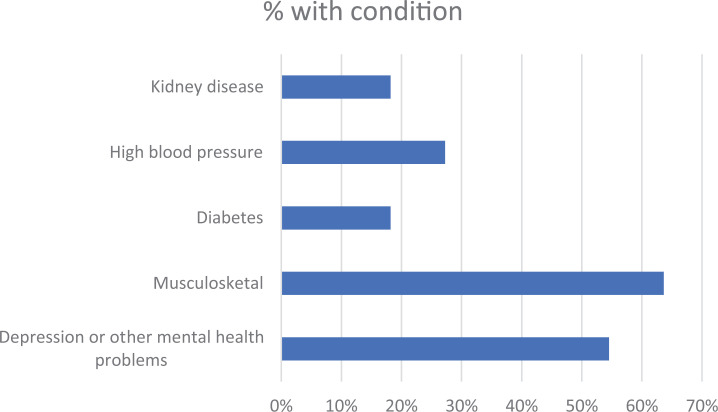
Figure 1 outlines the most common self-reported health issues to the link worker. Priority health issues reported to the link worker were either mental health (50%) or musculoskeletal problems. The majority of people were not members of community clubs or groups, and had no reported social or leisure activities in the previous month.
Figure 1.
Self-reported health conditions.
Patients who completed the structured interviews reported that the PROM questionnaires were easy to complete because of their tick box nature, appropriate and not onerous. They did however note some difficulty completing certain sections of the questionnaires;, in particular details about distance and journeys to the GP or community resources. Returned PROM questionnaires had few missing data except for the Social Connectedness scale23 with 4 out of 11 questionnaires returned missing more than one data item. Self-reported GP attendances had missing data for 7 of 11 questionnaires and 5 of 11 on distance from GP. The community resource costs questionnaire was only filled in by three patients.
The two GPs from the pilot practice reported that the use of the threshold of ≥8 medications as a proxy for multimorbidity led to younger patients being excluded. These GPs also noted that some participants did not have significant psychosocial issues of which they were aware, and were recruited at the expense of patients regarded by the GPs as having higher psychosocial needs. They believed that the patient selection process did not reflect how such a service would work in practice, as it did not include any marker of perceived patient need or suitability for a link worker intervention. They also expressed concern at the lengthy patient information leaflet, and reported that their follow-up phone calls to potentially eligible patients was critical for recruitment. Structured interviews with patients also confirmed that the GP phone call was important in explaining and providing reassurance regarding the study. The link worker agreed that a few of the patients referred required very little support but that around two thirds of them had significant psychosocial issues, whereas the GPs estimated only around half had.
Feasibility and acceptability of the link worker intervention
Intervention implementation
Twelve of the 14 patients who consented to participate met with the link worker. One person was uncontactable, and one was too unwell to continue to participate. Six patients had three or more follow-up contacts with the link worker. The majority of follow-up contacts were by telephone and initiated by the link worker. Appraisal and informational support were the most common types of support provided. Common resources that the link worker shared with patients were chronic disease self-management courses, addiction services and local exercise classes.
Feasibility and acceptability: Participants
When asked why they had taken part, most patients cited the GP phone call as a critical step, either to encourage or reassure. One person reported that they ‘hadn’t thought it was for me, but went along as the GP recommended it’ (P3, Male 70). Interviewees described being unsure as what to expect from the initial meeting with the link worker, with a common misconception that it was to do with medication as this was the reason they had been selected to participate and ‘prescribing’ was in the study title. All reported understanding the process fully after meeting the link worker.
All patients were positive about the experience, describing the link worker as ‘down to earth’ (P2, Male 78) and one said the link worker ‘played a very valid role in helping me to get out of the house and do other things instead of feeling lonely and isolated in this world’ (P6, Female 65). One patient said the link worker was the ‘kick start’ needed to get him moving again (P3, Male 70). No one was uncomfortable with any of the questions the link worker asked them, which included questions about housing, employment, personal supports, leisure activities smoking and alcohol consumption.
All bar one were happy with the resources provided and the support the link worker gave to access them, usually providing details or making initial contact for them. One patient said the resources that were suggested for them were too expensive and the timing of an exercise class didn’t suit. The GP practice was considered a familiar and private place to meet face-to-face with the link worker. Appendix 1 contains a table with interview participants’ demographic details.
Feasibility and acceptability: GPs and link worker
Feedback from the GPs was positive and no practical challenges hosting the link worker identified. The practice invited the link worker to their monthly primary care team meetings and reported that she made helpful suggestions about resources that could support patients not involved in the study. The link worker was positive about being based within the general practice, apart from an issue with suitable room availability at times. Prior to meeting patients, the link worker compiled a list of local community resources. She reported that this mapping of, and networking with, local community service providers was time consuming but essential in order to support participants’ health and social needs.
The client management database was easy to use according to the link worker and could easily generate participant-related information. The pilot study did allow some minor technical issues with the database to be identified and corrected in advance of the main trial.
Implementation advisory group
The Implementation Advisory Group were presented with the results of the pilot and provided advice on selection and recruitment in practice. While they agreed that a formalised, health electronic records based recruitment strategy to identify patients would be more efficient compared to prospective recruitment during clinical encounters, they felt that GP knowledge of their patients psychosocial problems would normally underpin a referral to a link worker, and that without the incorporation of this factor the trial conditions would not be reflective of real life conditions. They agreed with the pilot study GPs that using ≥8 medications as a finder would exclude younger people with multimorbidity.
Public Patient Involvement
The panels input was first sought after the pilot had been completed and after consultation with the implementation advisory group. At this stage challenges with explaining the intervention, the patient information leaflets, completion of self-reported health care use and community resource questionnaires were known. Details of PPI methods and outcomes are in Table 2
The research team made the decision to add the Investigating Choice Experiments for the preference of older people CAPability measure for Adults (ICE-CAP A)27 and remove the Social Connectedness Scale. This was in an effort to shorten the PROM questionnaire, yet still capture potential social and wellbeing effects. Furthermore the ICECAP-A can be used as an economic measure and is recommended by NICE for use in evaluations of interventions that have non-health elements.28
Summary of modifications to the RCT protocol as a result of the pilot, the PPI group and the implementation advisory group input
A stage was added to the selection process that involved GPs identifying all patients on their list who they believed could benefit from the intervention. This will form a register of eligible patients for the RCT. Trial patients will then be randomly selected from this list to minimise selection bias.
Additional time was allocated to the recruitment phase to allow screening of lists of all patients on ≥5 medications with psychosocial needs, with recruitment to start 1 month in advance of the intervention.
Recruitment packs were modified to include a summary brochure as the lengthy information leaflet was initially off putting.
The patient questionnaires were modified to clarify sections on costs related to the intervention. The social connectedness scale was replaced by ICE-CAP A.27
A research assistant will provide support with baseline and follow up data collection where necessary, including reminder phone calls, repeat mail outs and support to fill in the questionnaires if required.
Discussion
This paper describes a rapid uncontrolled pilot project of a link worker intervention and subsequent adjustments to the trial protocol for a planned pragmatic randomised trial of a primary care based link worker intervention targeting patients with multimorbidity living in disadvantaged communities. The selection and recruitment processes were lengthier than expected and aspects were unacceptable to the GPs involved. The patients had poor understanding of the intervention before meeting the link worker. Patients, GPs and the link worker were positive about the intervention processes.
The patients in this pilot study were older than in other studies where mean age of participants was approximately 10 years younger than our sample.9–11 Compared to participants in the Glasgow Links worker study, which also targeted areas of deprivation, the patients in this pilot had higher EQ-5D-5L scores indicating better health related quality of life, lower HADS scores indicating less depression and anxiety and were less likely to live alone. This resonates with the GPs perception that our original participant selection methods were not identifying participants who they perceived as needing the intervention most. We were confident, however, that it was identifying people with multimorbidity as our participants had an average of 2.6 self-reported chronic conditions. To our knowledge, all evaluations of link workers providing social prescribing in the UK and Ireland have incorporated a referral element, either self-referral or referral by a health care professional, based on perceived potential to benefit from a link worker.
The fact that 73% of the potential participants identified for involvement agreed to take part was high compared to other published studies. This was possibly due to the relationship between the GPs and the participants, the follow up phone calls made by the GPs, and the GPs commitment to the link worker concept. Qualitative evaluations of social prescribing programmes suggested that there is variation in the level of GP commitment and this can affect implementation.29,30 Our follow up rate of 57% was lower than other trials,9–11 but this could potentially be improved with reminders by post and phone.
Our findings on the acceptability of the link worker intervention are consistent with the current literature where such interventions are broadly perceived very positively by participants, with the ability of the link worker to listen and support being emphasised as important.31–33 The importance of available community resources is also reported as key to success and co-location of link workers in primary care recommended.32
Finally, the use of a PPI panel at this early pilot stage of the research is fast becoming recognised as international best practice for the conduct of high quality intervention studies.
Strengths and limitations
By building on the Glasgow Deep End links worker evaluation, we were able to carry out a rapid uncontrolled pilot study focusing on exploring the feasibility and acceptability of trial processes, and the intervention, within an Irish primary care setting. The timeline of 1 year for completion of the pilot and full RCT which was imposed by the funders of the study meant there was insufficient time to conduct a randomised pilot study. However, trials of similar interventions9,10 have shown that individual patient randomisation is possible for this type of intervention. A rapid pilot was possible given that we were modifying an existing intervention rather than designing a new one.
The pilot resulted in several important issues being identified and, with focused input from a multimorbidity PPI advisory group and implementation advisory group of frontline practitioners, important adjustments were made to these elements of the main trial protocol.
While there was some discrepancy in the GPs and link worker’s perception of participants’ psychosocial needs it was ultimately decided with input from the implementation advisory group to include GP perception of psychosocial need in the selection process. The latter approach, while raising the potential of selection bias, is closer to the reality of day-to-day decision making within general practice, which is important in a pragmatic randomised trial and improves external validity of the trial The input from the two advisory groups also helped achieve buy-in to recruitment and intervention processes with GPs who are taking part in the definitive trial.
The pilot also tested the client management database designed specifically for the trial using Microsoft Access24 which allowed collection of detailed information on link worker activity. This information has often been lacking in previous evaluations34 and will be reported separately as part of the parallel process evaluation for the main trial.
The short timeline of 3-months for the pilot resulted in several limitations to the methods. There was a very limited number of participants and even fewer responded to interviews. The demographic findings cannot be taken to represent the population as a whole. Given the small sample size, we did not do any statistical analyses of the patient reported outcome measures. It was not possible to do a thematic analysis of interview data and so only descriptive analysis was done. There was not sufficient time to chase non-responders to the initial mail out of follow up questionnaires. More involvement from the PPI panel, ideally before the pilot and afterwards more input on outcomes measures would have been desirable.
Conclusion
In conclusion, the pilot and patient and implementation group input allowed trial processes and acceptability to be tested and adjusted accordingly. These changes have led to a pragmatic RCT approach with adjusted timelines and additional support for recruitment and data collection, which will enhance the conduct of the planned definitive trial of primary care based link workers delivering social prescribing interventions to patients with multimorbidity living in disadvantaged communities. Evaluating complex interventions to improve outcomes for people with multimorbidity is very challenging and previous RCTs have not shown an improvement in their primary outcomes evaluated through quantitative approaches.35,36 Similar to these studies we are also conducting a parallel process evaluation including qualitative methods to explore the implementation of the intervention and potential mechanisms of action. Combined, the pragmatic RCT and process evaluation will contribute to the evidence base on link worker interventions and interventions to improve outcomes for people with multimorbidity.
Supplemental material
Supplemental Material, sj-docx-1-cob-10.1177_26335565211017781 for Primary care-based link workers providing social prescribing to improve health and social care outcomes for people with multimorbidity in socially deprived areas (the LinkMM trial): Pilot study for a pragmatic randomised controlled trial by Bridget Kiely, Deirdre Connolly, Barbara Clyne, Fiona Boland, Patrick O’Donnell, Eamon O Shea and Susan M Smith in Journal of Comorbidity
Supplemental Material, sj-docx-2-cob-10.1177_26335565211017781 for Primary care-based link workers providing social prescribing to improve health and social care outcomes for people with multimorbidity in socially deprived areas (the LinkMM trial): Pilot study for a pragmatic randomised controlled trial by Bridget Kiely, Deirdre Connolly, Barbara Clyne, Fiona Boland, Patrick O’Donnell, Eamon O Shea and Susan M Smith in Journal of Comorbidity
Supplemental Material, sj-docx-3-cob-10.1177_26335565211017781 for Primary care-based link workers providing social prescribing to improve health and social care outcomes for people with multimorbidity in socially deprived areas (the LinkMM trial): Pilot study for a pragmatic randomised controlled trial by Bridget Kiely, Deirdre Connolly, Barbara Clyne, Fiona Boland, Patrick O’Donnell, Eamon O Shea and Susan M Smith in Journal of Comorbidity
Appendix 1.
Demographics of interview participants.
| Interview participants characteristics | |
|---|---|
| Characteristic | Value |
| Age γ (SD) | 66.3 (8.82) |
| Female % | 66 |
| Primary education only % | 33 |
| Employed % | 18 |
| Lives alone % | 33 |
| GMS Card 1 % | 66 |
| Number of self reported health conditions γ (SD) | 2.8 (1.16) |
| EQ5D5L γ (SD) | 0.519 (0.21) |
| HADS A γ (SD) | 7.5 (3.01) |
| HADS D γ (SD) | 7.3 (4.81) |
| Multimorbidity Burden of Treatment: Medium or above % | 33 |
| Activity Level: Inactive % | 18 |
1 The general medical service (GMS) card entitles holders to free primary care services and reduced medication fees. It is means tested and about 40% of the Irish population hold one. EQ-5D-5L = a standardised measure of self-reported health-related quality of life that assesses 5 dimensions at 5 levels of severity where 1 is the preferred state of health; HADS-A = Hospital Anxiety and Depression Scale, Anxiety, where a score above 8 indicates possible caseness; HADS-D = Hospital Anxiety and Depression Scale, Depression, where a score above 8 indicates possible caseness; Multimorbidity burden of treatment questionnaire categorises burden as none, low, medium or high; Patient Activation Measure categorises activation from level 1 to 4 with 1 being least activated; Frenchay activity index categorises people as inactive, moderately active or very active based on work, leisure and domestic activity.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The research was funded the Health Research Board Ireland Collaborative Doctoral Award in Multimobidity CDA-2018-003) and the Department of Health Slaintecare Integration fund. (PC-24).
ORCID iDs: Bridget Kiely  https://orcid.org/0000-0002-5752-0432
https://orcid.org/0000-0002-5752-0432
Fiona Boland  https://orcid.org/0000-0003-3228-0046
https://orcid.org/0000-0003-3228-0046
Susan M Smith  https://orcid.org/0000-0001-6027-2727
https://orcid.org/0000-0001-6027-2727
Supplemental material: Supplemental material for this article is available online.
References
- 1. Fortin M, Soubhi H, Hudon C, et al. Multimorbidity’s many challenges. BMJ 2007; 334(7602): 1016–1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Glynn LG, Valderas JM, Healy P, et al. The prevalence of multimorbidity in primary care and its effect on health care utilization and cost. Fam Prac 2019; 28(5): 516–523. [DOI] [PubMed] [Google Scholar]
- 3. Palladino R, Tayu Lee J, Ashworth M, et al. Associations between multimorbidity, healthcare utilisation and health status: evidence from 16 European countries. Age Ageing 2016; 45(3): 431–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012; 380(9836): 37–43. [DOI] [PubMed] [Google Scholar]
- 5. Smith SM, Wallace E, O’Dowd T, et al. Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Sys Rev 2016; 3(3): CD006560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bickerdike L, Booth A, Wilson PM, et al. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open 2017; 7(4): e013384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. HSE. Donegal Social Prescribing Service: HSE.ie, https://www.hse.ie/eng/health/hl/selfmanagement/donegal/programmes-services/social-prescribing/social-prescribing.html (2019, accessed 31 December 2020).
- 8. HSE. Waterford Social Prescribing Service: Waterford Libraries, http://waterfordlibraries.ie/waterford-social-prescribing-service/ (2018, updated 2018, accessed 31 December 2020).
- 9. Grant C, Goodenough T, Harvey I, et al. A randomised controlled trial and economic evaluation of a referrals facilitator between primary care and the voluntary sector. BMJ 2000; 320(7232): 419–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kangovi S, Mitra N, Norton L, et al. Effect of community health worker support on clinical outcomes of low-income patients across primary care facilities: a randomized clinical trial. JAMA Int Med 2018; 178(12): 1635–1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mercer SW, Fitzpatrick B, Grant L, et al. Effectiveness of community-links practitioners in areas of high socioeconomic deprivation. Annal Fam Med 2019; 17(6): 518–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Smith S, O’Donnell P. Deep End Ireland 2018: role of links workers & social prescribing: Deep End Ireland, http://deepend.ie/wp-content/uploads/2018/04/DE-link-worker-meet-report-25.4.18.pdf (2018, accessed 31 December 2020).
- 13. Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new medical research council guidance. BMJ 2008; 337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kiely B, Clyne B, Boland F, et al. Link workers providing social prescribing and health and social care coordination for people with multimorbidity in socially deprived areas (the LinkMM trial): protocol for a pragmatic randomised controlled trial. BMJ Open 2021; 11(2): e041809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Haase T. The 2016 Pobal HP Deprivation Index (SA) trutzhaase.eu2016, http://trutzhaase.eu/deprivation-index/the-2016-pobal-hp-deprivation-index-for-small-areas/ (accessed 31 December 2020).
- 16. Wallace E, McDowell R, Bennett K, et al. Comparison of count-based multimorbidity measures in predicting emergency admission and functional decline in older community-dwelling adults: a prospective cohort study. BMJ Open 2016; 6(9): e013089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Langford CPH, Bowsher J, Maloney JP, et al. Social support: a conceptual analysis. J Adv Nur 1997; 25(1): 95–100. [DOI] [PubMed] [Google Scholar]
- 18. Gusi N, Olivares PR, Rajendram R. The EQ-5D health-related quality of life questionnaire. In: Preedy VR, Watson RR. (eds) Handbook of disease burdens and quality of life measures. New York, NY: Springer New York, 2010, pp. 87–99. [Google Scholar]
- 19. Brennan C, Worrall-Davies A, McMillan D, et al. The hospital anxiety and depression scale: a diagnostic meta-analysis of case-finding ability. J Psychosom Res 2010; 69(4): 371–378. [DOI] [PubMed] [Google Scholar]
- 20. Schuling J, Haan RD, Limburg M, et al. The Frenchay Activities Index. Assessment of functional status in stroke patients. Stroke 1993; 24: 1173–1177. [DOI] [PubMed] [Google Scholar]
- 21. Hibbard JH, Stockard J, Mahoney ER, et al. Development of the patient activation measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004; 39(4 Pt 1): 1005–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Duncan P, Murphy M, Man M-S, et al. Development and validation of the multimorbidity treatment burden questionnaire (MTBQ). BMJ Open 2018; 8(4): e019413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lee R, Robbins S. Measuring belongingness: the social connectedness and the social assurance scales. J Counsel Psychol 1995; 42(2): 232–241. [Google Scholar]
- 24. Microsoft. Access. 16 ed. Microsoft, 2016. [Google Scholar]
- 25. Neergaard MA, Olesen F, Andersen RS, et al. Qualitative description – The poor cousin of health research? BMC Med Res Methodol 2009; 9: 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Staniszewska S, Brett J, Simera I, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. BMJ 2017; 358: j3453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Al-Janabi H, N Flynn T, Coast J. Development of a self-report measure of capability wellbeing for adults: the ICECAP-A. Quality Life Res 2012; 21(1): 167–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. NICE. Developing NICE Guidelines: the manual London: National Institute for Health and Care Excellence, https://www.nice.org.uk/process/pmg20/chapter/incorporating-economic-evaluation (2014, updated 15 October 2020, accessed 28 February 2021). [PubMed]
- 29. Mercer S, Wyke S, Fitzpatrick B, et al. Evaluation of the Glasgow ‘Deep End’ links worker programme. NHS Scot University Glasgow 2017; 7(1): 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Aughterson H, Baxter L, Fancourt D. Social prescribing for individuals with mental health problems: a qualitative study of barriers and enablers experienced by general practitioners. BMC Fam Prac 2020; 21(1): 194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Moffatt S, Steer M, Lawson S, et al. Link worker social prescribing to improve health and well-being for people with long-term conditions: qualitative study of service user perceptions. BMJ Open 2017; 7(7): e015203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Carnes D, Sohanpal R, Frostick C, et al. The impact of a social prescribing service on patients in primary care: a mixed methods evaluation. BMC Health Ser Res 2017; 17: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Payne K, Walton E, Burton C. Steps to benefit from social prescription: a qualitative interview study. Br J General Pract J Royal College Gen Pract 2019; 70(690): e36–e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Husk K, Blockley K, Lovell R, et al. What approaches to social prescribing work, for whom, and in what circumstances? A realist review. Health Soc Care Community 2020; 28(2): 309–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Salisbury C, Man M-S, Bower P, et al. Management of multimorbidity using a patient-centred care model: a pragmatic cluster-randomised trial of the 3D approach. Lancet London Eng 2018; 392(10141): 41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fortin M, Stewart M, Ngangue P, et al. Scaling up patient-centered interdisciplinary care for multimorbidity: a pragmatic mixed-methods randomized controlled trial. Ann Family Med 2021; 19(2): 126. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-docx-1-cob-10.1177_26335565211017781 for Primary care-based link workers providing social prescribing to improve health and social care outcomes for people with multimorbidity in socially deprived areas (the LinkMM trial): Pilot study for a pragmatic randomised controlled trial by Bridget Kiely, Deirdre Connolly, Barbara Clyne, Fiona Boland, Patrick O’Donnell, Eamon O Shea and Susan M Smith in Journal of Comorbidity
Supplemental Material, sj-docx-2-cob-10.1177_26335565211017781 for Primary care-based link workers providing social prescribing to improve health and social care outcomes for people with multimorbidity in socially deprived areas (the LinkMM trial): Pilot study for a pragmatic randomised controlled trial by Bridget Kiely, Deirdre Connolly, Barbara Clyne, Fiona Boland, Patrick O’Donnell, Eamon O Shea and Susan M Smith in Journal of Comorbidity
Supplemental Material, sj-docx-3-cob-10.1177_26335565211017781 for Primary care-based link workers providing social prescribing to improve health and social care outcomes for people with multimorbidity in socially deprived areas (the LinkMM trial): Pilot study for a pragmatic randomised controlled trial by Bridget Kiely, Deirdre Connolly, Barbara Clyne, Fiona Boland, Patrick O’Donnell, Eamon O Shea and Susan M Smith in Journal of Comorbidity