Abstract
Objective
This study examined the impact of lockdown for SARS-CoV-2 on breast cancer management via an online survey in a French multicentre setting.
Material and methods
This is a multicentre retrospective study, over the strict lockdown period from March 16th to May 11th, 2020 in metropolitan France. 20 centres were solicited, of which 12 responded to the survey.
Results
50% of the centres increased their surgical activity, 33% decreased it and 17% did not change it during containment. Some centres had to cancel (17%) or postpone (33%) patient-requested interventions due to fear of SARS-CoV-2. Four and 6 centres (33% and 50%) respectively cancelled and postponed interventions for medical reasons. In the usual period, 83% of the centres perform their conservative surgeries on an outpatient basis, otherwise the length of hospital stay was 24 to 48 h. All the centres except one performed conservative surgery on an outpatient basis during the lockdown period, for which. 8% performed mastectomies on an outpatient basis during the usual period. During lockdown, 50% of the centres reduced their hospitalization duration (25% outpatient /25% early discharge on Day 1).
Conclusion
This study explored possibilities for management during the first pandemic lockdown. The COVID-19 pandemic required a total reorganization of the healthcare system, including the care pathways for cancer patients.
Keywords: COVID-19, Containment, Epidemic disease, Survey
1. Introduction
Initially described in December 2019 in China, SARS-CoV-2, responsible for the COVID-19 pandemic, affected more than 200 countries in just a few months and caused more than 3000,000 deaths worldwide, including 100,000 in France (gouvernement.fr data, as of 23/04/2021).
SARS-CoV-2 has a global impact on the healthcare system due to the severity of cases overwhelming intensive car units with repercussions on the management of other patients requiring sometimes equally urgent care.
It is recognized that SARS-CoV-2 is more severe in elderly patients or patients with co-morbidities [1].
According to the analysis of the first cases in China [2], the rate of SARS-CoV-2 infection appeared to be higher in cancer patients than in the general population (1% vs. 0.29%).
Other results suggested that patients with a history of cancer or cancer in treatment have a five-fold risk of developing secondary complications, and a four-fold risk of death more related to the infection than to the cancer itself. Mehta V, Goel S, Kabarriti R et al. case fatality rate of cancer patients with COVID-19 in a New York hospital system. Cancer Discov 10;2020 p 2,020,953-41.
Different ways of reorganizing the healthcare system have been observed around the world to limit human contact [3] that affected the delivery of routine cancer care and supportive services secondary to a reduction in healthcare personnel and available resources.
The American College of Surgeons [4], recommended postponing surgeries if there are too many covid-positive cases in the concerned institution. Numerous recommendations have been made for cancer management in the COVID-19 pandemic context, depending on the number of cases in different countries and available resources.
The French Government enforced a strict lockdown from March 16th 2020 to May 11th 2020 with reorganization of the public health services with suspension of “non-essential” medical and surgical activity ton increase the capacity of managing patients with SARS-CoV-2 infections. [5].
The aim of this study was to evaluate the impact of the strict lockdown for the COVID-19 pandemic on the therapeutic management of women with breast cancer in France.
2. Materials and methods
This is a multicentre retrospective study, about breast cancer management concerning the first lockdown in France from March 16th 2020 to May 11th 2020.
Twenty centres were solicited (Francogyn study group and different hospital in centre region), of which 12 responded to the questionnaire. Responding centres, were: the University Hospital of Tours, La Pitié Salpétrière Hospital, University Hospital of Angers, University Hospital of Lille, University Hospital of Limoges and the Hospitals of Créteil, Poissy, Orléans, Dreux, Bourges, Croix Saint Simon and Tenon.
A multiple-choice and short answer online survey was sent to all centres, to evaluate the impact of the initial lockdown on medical care in these different centres. The questionnaire was sent by email to one referring physician per centre. Non-responding centres were solicited 3 times. (One-month interval).
We assessed the number of women managed for breast cancer during this period compared to the same period in 2019 (from March 16th 2019 to May 11th 2019), changes in management (consultation, additional examinations, organization of multidisciplinary consultation meetings), postponement of interventions, surgical modifications (primary surgery, genomic tests, breast reconstruction, etc.), changes in hospitalization conditions, adaptation of adjuvant and neoadjuvant chemotherapy and radiotherapy.
3. Results
A total of twelve centres participated to the study.
3.1. Changes in activity volume
Among the participating centres, annual surgical activity 2019 varied from 21 to 334 operated breast cancer patients per year (average of 196 patients per year).
An average of 29 women were operated from March 16th 2020 to May 11th 2020 compared to 27 women over the same period in 2019.
50% of the included centres increased their surgical activity, 33% decreased it and 17% observed no change during lockdown.
First-time Consultations: All the twelve centres included, continued to perform "first time" breast cancer consultations. Only two centres out of twelve, i.e. 16%, carried out these consultations by “teleconsultation”. The only changes were those taken to limit human contact: hygiene rules (wearing a mask, disinfection of the rooms, no accompanying person).
Follow-up consultations: Nine centres (75%) continued the follow-up consultations by “teleconsultation”, and two centres postponed these consultations to the period after lockdown.
Surgical interventions: some centres (n = 2) had to cancel (17%) or postpone (n = 4 (33%)) interventions due to a patient-request for fear of SARS-CoV-2.
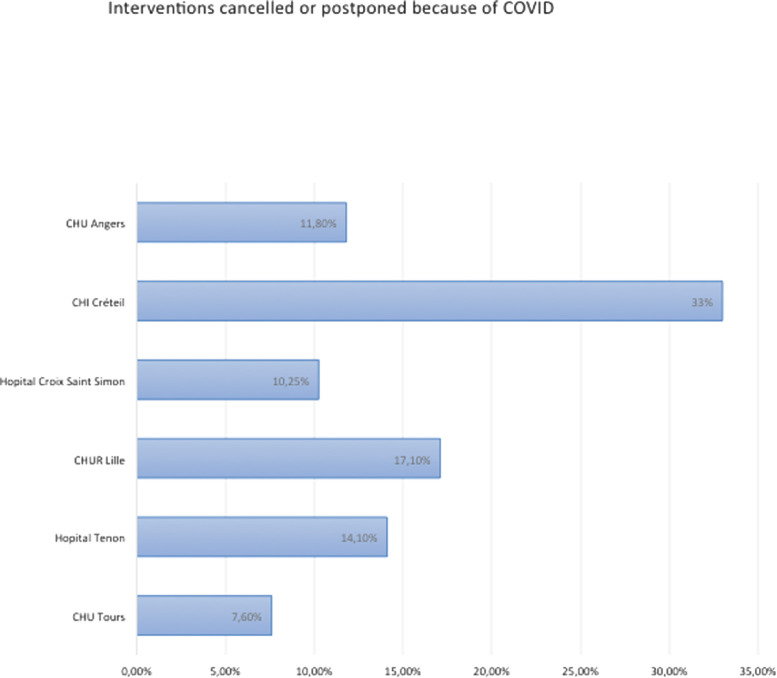
Four and 6 centres (33% and 50%) respectively cancelled and postponed interventions for medical reasons (suspicion of COVID-19 infection, significant co-morbidities or type of cancer allowing the implementation of primary medical care). These represented up to 30% of the breast surgical activity of the most affected centres (Fig. 1 ).
Fig. 1.
Interventions cancelled or postponed because of covid 19.
In these cases, the management of invasive carcinomas was shifted in favour of primary hormone therapy in case of positive hormone receptors.
Surgeries were reserved for invasive carcinomas (management of DCIS was postponed in all centres).
3.2. Radiological investigations
Five of the 12 centres (41%) encountered difficulties in organizing complementary examinations, secondary to the fact that radiologists were mobilized for COVID-19 cases, necessitating sending patients to another radiology centre (this was not the case in university teaching hospitals).
3.3. Immediate breast reconstruction
Nine centres (81%) either postponed immediate breast reconstructions to the period after lockdown or limited surgeries to prosthesis placements.
3.4. Outpatient activity
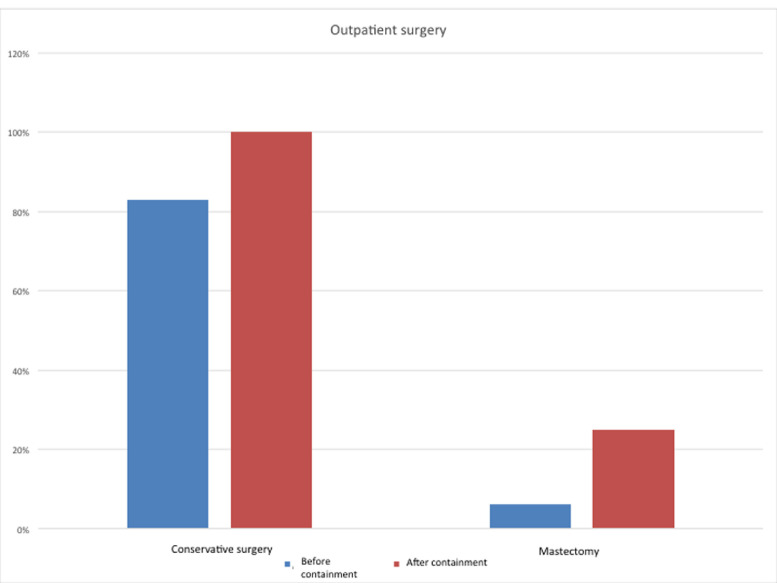
In the usual period, 83% of the centres performed their conservative surgeries on an outpatient basis; otherwise the length of stay was 24 to 48 h. All the centres performed conservative surgery on an outpatient basis during the lockdown period in question except one (a peripheral hospital), for which the hospitalization service had closed.
8% of the centres performed the mastectomies on an outpatient basis during the usual period, while the others had hospitalization length ranging from one to four days, with an average of two days. During lockdown, 50% of the centres reduced their hospitalization length durations (25% outpatient /25% early discharge on Day 1). (Fig. 2 ).
Fig. 2.
Outpatient breast surgery before and after the first lockdown for covid 19.
3.5. Multidisciplinary meetings
100% of the centres modified their organizational multidisciplinary meetings practices with the implementation of videoconferences, restriction of medical presence to one referent specialist per specialty.
3.6. Genomic tests
Indications for the use of genomic testing (endopredict, oncotype, etc.) have not been modified during lockdown period.
3.7. Management of triple negative and HER2 positive breast cancers
Only one centre (8%) has modified their management by not performing upfront primary surgery if indicated.
Neoadjuvant chemotherapy (NAC): One centre (8%) limited indications of NAC in case of elderly patients (>75 years).
Adjuvant chemotherapy: One centre (8%) limited indications in case of elderly patients (>75 years).
3.8. Radiotherapy
41% of centres have changed their practices regarding adjuvant radiotherapy.
50% of centres reported a delay of one to two weeks (66%) or two to four weeks (33%) for radiotherapy initiation.
3.9. Attitude when revision surgery was mandatory
Three centres (25%) have modified their indications for revision surgery: no revision surgery if insufficient margins for associated ductal carcinoma in situ (DCIS) (<2 mm), or interventions were postponed to the post-chemotherapy period in case of adjuvant chemotherapy.
3.10. Covid-19 positive cases
Four centres have been affected by the coronavirus within the medical breast cancer surgical team.
Three centres had patients affected in the preoperative period and two in the 15 days following surgery.
3.11. Post lockdown plan
83% of the centres planned to preoperatively test their patients after the lockdown period with PCR within 48 h before surgery.
4. Discussion
The aim of this study was to detail the impact of the first French COVID-19 lockdown on breast cancer management. Our survey concerned hospitals with variable surgical activity.
There was no single attitude towards the COVID-19 pandemic and care varied according to the pre-existing surgical activity and the means available in the different centres.
However, many recommendations have been published.
The reorganization of the healthcare system imposed reduced access to hospitals and operating theatres, implying establishment of priorities, determined according to the histological type, the time required for treatment, the patient's co-morbidities and to take into account limitation of the detrimental impact on patient care and the risk of COVID-19 infection during management.
The French recommendations [6] for the management of breast cancer during the pandemic period favoured any equivalent treatment option limiting the length of hospital stay.
For radiological exams: suspension of breast screening programs was advised, controls were allowed for ACR 3 lesions in a high-risk of breast cancer context and management of ACR 4–5 lesions was pursued.
For surgery: recommendations favoured postponement of surgical management of benign lesions and immediate breast reconstructions (IBR) (IBR with prosthesis or expander were authorized function of centre means).
Management of Ductal carcinomas in situ (DCIS) was delayed up to 3 months.
In case of significant co-morbidities and low-grade, hormone-dependent cancer, a neoadjuvant hormone therapy was favoured, as found in the different centres surveyed.
For radiotherapy: postponement (3 to 6 months) was favoured in case of DCIS without invasive component. An alternative was to propose hypo-fractional radiotherapy.
If adjuvant chemotherapy was indicated, a postponement of 6 weeks in initiation of treatment was tolerated.
It was recommended to maintain fertility-preservation consultations.
The French Haut Conseil de Santé Publique (HCSP) considered that cancer patients under treatment were at increased risk of developing a severe form of COVID-19 infection [5].
Several expert opinions have been issued based on different recommendations (NAPBC, NCCN, CoC …), to prioritize different scenarios [7].
The Spanish recommendations also advocated limiting access to hospitals, performing conservative surgery or postponing it, postponing radiotherapy (12 weeks after surgery), if possible postponing or spacing out chemotherapy sessions by favouring less immunosuppressive molecules. No changes in terms of neoand/or adjuvant chemotherapy in triple negative or HER2 positive cancers [3].
The EUBREAST study [8] aimed to analyse changes in practices during the COVID-19 pandemic. Treatment was delayed in 20% of institutions (2 to 4 weeks in 60% of cases).
There was an increase in neoadjuvant treatments, and a 10% increase in primary surgery for triple negative and HER2 positive cancers (T1), contrary to what was found in our study.
67% of respondents believed that chemotherapy increases the risk of complications.
31% have changed chemotherapy protocols (more spaced, less immunosuppressive).
20% increased the use of genomic testing to assess the need for neoadjuvant chemotherapy, whereas no modification was found in our study.
20% postponed adjuvant radiotherapy, 50% did not modify the sequences (similar to our results).
20% treated COVID-19-affected patients when recommendations favoured treatment suspension.
The ESMO (European Society for Medical Oncology) stressed that non-coronavirus related priorities need to be defined; with prioritization methods in the face of limited resources [9].
It was recommended to prioritize: avoid visits or perform triage at admission, perform outpatient biology check-ups if the patient was asymptomatic, postpone consultations, postpone mammograms if patient was asymptomatic, reschedule breast reconstruction surgery, prioritize triple negative for neoadjuvant chemotherapy, suspend hormone therapy if case covid-19 infection to prevent thromboembolic risk. Defined as high priority: diagnosis of invasive cancer, ACR5 lesions, self-examination of a breast mass medium priority: non-invasive cancer, ACR4 lesions.
For high-risk cancers, surgery was maintained (few associated complications and major prognosis impact), or neoadjuvant treatment should be considered prior to surgery.
For low-risk cancers, delay surgery for 12 weeks. In the case of luminal cancer, hormone therapy should be preferred while waiting for surgery.
The American Society of Clinical Oncology (ASCO) reported an increase in neoadjuvant chemotherapy in response to a decrease in first surgeries, resulting in an increase in genomic testing [4].
They recommended delaying elective surgeries, increasing home therapies and telemedicine.
For DCIS lesions they advised to delay treatment (except in the case of a micro invasive component or strong suspicion of associated invasive carcinoma) up to 3–6 months. Delay was 6 months after hormone therapy in case of hormone dependant cancers.
Radiotherapy could be delayed or abandoned in case of positive hormone receptors and lesions <2.5 cm.
For triple negative cancers, prefer surgery if T1N0 lesions, no neoadjuvant chemotherapy for T1a-bN0. When chemotherapy was necessary, avoid anthracyclines and prefer cyclophosphamide, which require fewer control visits.
For stages II-III, surgery was recommended to be scheduled within 4–6 weeks after neoadjuvant chemotherapy followed by radiotherapy.
For HER 2 positive lesions, prefer surgery if T1N0 or T2<3cmN0 lesions, and do not defer radiotherapy.
Concerning the impact of COVID-19 infection in breast cancer patients, no association was found between a history of radiotherapy and coronavirus-related lung damage. We did not found any cases of coronavirus and breast cancer in our study.
According to a cohort study in these patients, coronavirus-related deaths are greater in patients with associated co-morbidities, including high blood pressure and an age greater than 70 years, but are not increased by prior radiotherapy or combination with adjuvant therapy.
Breast cancer does not appear to be a risk factor for coronavirus complications in this study, however, this finding may be induced by higher barrier measures that are better applied in this context [10].
In another cohort study, the authors analysed coronavirus mortality in cancer patients, it appeared that those with breast and prostate cancer were at higher risk. The initial hypothesis is that cancer-related treatments lead to a decrease in immunity; the subjects were also older with more comorbidity. The risk factors associated with increased mortality were age, male sex, smoking, co-morbidities, > WHO 2 status, active cancer and hydroxychloroquine intake. The following were not found to be risk factors: ethnicity, obesity, type of chemotherapy or recent surgery [11, 12].
The patients most at risk of going to the intensive care units were smoking patients, obese, with haematological cancer, WHO status 2.
In this study, the absence of complications in patients treated with chemotherapy or primary surgery suggested that they might be safely continued during the pandemic [11].
Conversely, another Chinese study found a higher risk of severe complications and rapid worsening in cancer patients [2], especially if chemotherapy or surgery in the previous months, with 38% of deaths in patients with breast cancer and coronavirus (compared to 15% of deaths per year from breast cancer) [12].
A multicentre comparative study evaluated the differences between patients with coronavirus, whether or not associated with cancer. The results showed that patients with metastatic cancer, who have undergone surgery, are more at risk of severe complications. This was not the case in non-metastatic patients, or who have only received radiotherapy.
The association between cancer (of any type) and coronavirus is also associated with a higher death rate, more intensive care unit admissions, increased need for invasive mechanical ventilation [13].
This study explored possibilities for breast cancer management during the COVID-19 pandemic. The situation during the first lockdown required a total reorganization of the healthcare system, including the care pathways for cancer patients. This involved prioritizing surgical, oncological and follow-up management according to their degree of urgency and necessity in the treatment plan, while at the same time making patients feel safe with regard to COVID-19 and their disease.
References
- 1.Verity R., Okell L.C., Dorigatti I., Winskill P., Whittaker C., Imai N., et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20(6):669‑77. doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liang W., Guan W., Chen R., Wang W., Li J., Xu K., et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335‑7. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Martin M., Guerrero-Zotano A., Montero Á., Jara C., Filipovich E., Rojo F., et al. GEICAM guidelines for the management of patients with breast cancer during the COVID-19 pandemic in Spain. Oncologist. 2020 doi: 10.1634/theoncologist.2020-0363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sheng J.Y., Santa-Maria C.A., Mangini N., Norman H., Couzi R., Nunes R., et al. Management of breast cancer during the COVID-19 pandemic: a stageand subtype-specific approach. JCO Oncol Pract [Internet] 2020 doi: 10.1200/OP.20.00364. https://ascopubs.org/doi/pdf/10.1200/OP.20.00364 [cité 6 août 2020]; Disponible sur. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.HCSP Avis provisoire Recommandations relatives à la prévention et à la prise en charge du COVID-19 chez les patients à risque de formes sévères [Internet] Rapport de l'HCSP. Paris: Haut Conseil de la Santé Publique; 2020 https://www.hcsp.fr/explore.cgi/avisrapportsdomaine?clefr=776 mars [cité 6 août 2020]. Disponible sur. [Google Scholar]
- 6.Gligorov J., Bachelot T., Pierga J.-.Y., Antoine E.-.C., Balleyguier C., Barranger E., et al. COVID-19 et personnes suivies pour un cancer du sein : recommandations françaises pour la pratique clinique de Nice-St Paul de Vence, en collaboration avec le Collège Nationale des Gynécologues et Obstétriciens Français (CNGOF), la Société d'Imagerie de la Femme (SIFEM), la Société Française de Chirurgie Oncologique (SFCO), la Société Française de Sénologie et Pathologie Mammaire (SFSPM) et le French Breast Cancer Intergroup-UNICANCER (UCBG) Bull Cancer. 2020;107(5):528‑37. doi: 10.1016/j.bulcan.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dietz J.R., Moran M.S., Isakoff S.J., Kurtzman S.H., Willey S.C., Burstein H.J., et al. Recommendations for prioritization, treatment, and triage of breast cancer patients during the COVID-19 pandemic. the COVID-19 pandemic breast cancer consortium. Breast Cancer Res Treat. 2020;181(3):487‑97. doi: 10.1007/s10549-020-05644-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gasparri M.L., Gentilini O.D., Lueftner D., Kuehn T., Kaidar-Person O., Poortmans P. Changes in breast cancer management during the Corona Virus Disease 19 pandemic: an international survey of the European breast cancer research association of surgical trialists (EUBREAST) Breast. août. 2020;52:110‑5. doi: 10.1016/j.breast.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de A.E, D T., Loibl S., Delaloge S., Senkus E., Criscitiello C., et al. ESMO Management and treatment adapted recommendations in the COVID-19 era: Breast Cancer. ESMO Open. 2020;5(3) doi: 10.1136/esmoopen-2020-000793. Suppl. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Institut Curie Breast Cancer and C.O.V.I.D. Group. Vuagnat P., Frelaut M., Ramtohul T., Basse C., Diakite S., et al. COVID-19 in breast cancer patients: a cohort at the Institut Curie hospitals in the Paris area. Breast Cancer Res. 2020;22(1):55. doi: 10.1186/s13058-020-01293-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuderer N.M., Choueiri T.K., Shah D.P., Shyr Y., Rubinstein S.M., Rivera D.R., et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020;395(10241):1907‑18. doi: 10.1016/S0140-6736(20)31187-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mehta V., Goel S., Kabarriti R., Cole D., Goldfinger M., Acuna-Villaorduna A., et al. Case fatality rate of cancer patients with COVID-19 in a New York hospital system. Cancer Discov [Internet] 2020 doi: 10.1158/2159-8290.CD-20-0516. https://cancerdiscovery.aacrjournals.org/content/early/2020/04/29/2159-8290.CD-20-0516 [cité 6 août 2020]; Disponible sur. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dai M., Liu D., Liu M., Zhou F., Li G., Chen Z., et al. Patients with cancer appear more vulnerable to SARS-COV-2: a multi-center study during the COVID-19 outbreak. Cancer Discov. 2020;20:0422. doi: 10.1158/2159-8290.CD-20-0422. CD. [DOI] [PMC free article] [PubMed] [Google Scholar]