1. Introduction
Disruptive mood dysregulation disorder (DMDD), a new diagnosis of the DSM-5 (Diagnostic and Statistical Manual of Mental Disorder, 5th edition) (American Psychiatric Association, 2013; Stringaris et al., 2012b), is characterized by severe, developmentally inappropriate temper outbursts and chronic/persistent irritable mood lasting for 12 months or more across situations. To address the issues of inadequate treatment of patients with chronic irritability as well as the misdiagnosis of bipolar disorder in chronically irritable youth (Blader and Carlson, 2007; Leibenluft, 2011), a syndrome named “severe mood dysregulation” was ever proposed for research use to examine the differences between chronic irritability and pediatric bipolar disorder (Leibenluft, 2011). A series of studies have shown that severe mood dysregulation (chronic irritability) is different from pediatric bipolar disorder (episodic irritability) in terms of longitudinal outcomes (Leibenluft et al., 2006; Brotman et al., 2006; Stringaris and Goodman, 2009; Stoddard et al., 2014), pathophysiology (Rich et al., 2007; Stringaris et al., 2012a; Thomas et al., 2012), and family history (Brotman et al., 2007; Propper et al., 2017). For example, severe mood dysregulation was associated with later anxiety and depression but not bipolar disorder (Leibenluft et al., 2006; Stringaris et al., 2009; Brotman et al., 2006; Stringaris, 2011). These findings provided the basis for the new DSM-5 diagnosis ‘DMDD’ (Roy et al., 2014).
Since the publication of the DSM-5, there has been a growing number of studies on DMDD. Based on retrospective diagnoses using existing datasets, the lifetime prevalence of DMDD was estimated to be 0.8~3.3 % (depending on age) in the Great Smoky Mountains Study sample (Copeland et al., 2013) and 0.12~5.26 % (depending on the stringency of the diagnostic threshold) in a representative population-based survey in youth aged 13–18 (Althoff et al., 2016). Another population-based study in children aged 6 years reported a 3-month prevalence rate of 8.2% (Dougherty et al., 2014). More recently, an adult population-based study in Switzerland showed that the prevalence of elevated DMDD symptoms was 0.79% during the primary school period by the recall and 0.5% during adulthood (Grau et al., 2018). The rates of DMDD are much higher in the clinical samples. For instance, in the Longitudinal Assessment of Manic Symptoms study, which recruited children (6–12.9 years) with significant mood liability, 26% of children met the DMDD criteria (Axelson et al., 2012). In a study from a large community mental health clinic, approximately 31% of youth met the operational definition of DMDD (Freeman et al., 2016). All of the abovementioned studies were conducted in Western countries. Only one study to date has examined the prevalence of DMDD in Asia, reporting a rate of < 1% in a large population-based sample of youth in Taiwan (Chen et al., 2019).
It is a rule rather than the exception that patients with DMDD have comorbid psychiatric disorder(s). It was reported that as high as 92.8% of patients with DMDD met the criteria for other psychiatric disorders (Copeland et al., 2013; Althoff et al., 2016), including attention-deficit/hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), conduct disorder, and anxiety and depressive disorders. Given the high rate of comorbidities, questions were raised about the necessity of creating a new diagnosis of DMDD. For example, a recent population-based epidemiological study found that DMDD was similar to ODD in symptomatology (Mayes et al., 2016). Studies with clinical samples also reported that DMDD overlapped largely with ODD in psychiatric comorbidities (Freeman et al., 2016; Axelson et al., 2012). The DSM-5 specifies that DMDD cannot co-exist with ODD, i.e., for those who met criteria for both DMDD and ODD, only the DMDD diagnosis should be given. Taking a different approach, the ICD-11, published in 2018, incorporates chronic irritability into the diagnosis of ODD by adding an ODD subtype with chronic irritability-anger (Evans et al., 2017). The different conceptualizations of chronic irritability call for more empirical data to clarify the relationship between DMDD and ODD.
Individuals with DMDD tend to have significant difficulties in several areas, e.g., social impairments with parents, siblings, and teachers and increased rate of service use and school suspension during childhood (Copeland et al., 2013) and adverse health outcomes, low educational attainment and high rate of police contact during adulthood (Copeland et al., 2014). DMDD was also found to increase the burden of ADHD in social functioning (Mulraney et al., 2016). Deficits of emotional self-regulation partially mediated the association between ADHD and functional impairments and service use in children (Leibenluft, 2017); and were associated with significantly increased school dysfunctions, unemployment, financial problems, and driver license suspension in adults with ADHD (Brotman et al., 2017). A recent study also demonstrated that DMDD, as compared to major depressive disorder (MDD) and persistent depressive disorders (PDD), tend to cause more complicated pregnancy, persistent peer-relationship, and school difficulties (Benarous et al., 2020). Given the highly impairing nature of emotional dysregulation and chronic irritability, either in isolation or in combination with other psychiatric disorders, it is critical to assess the functional deficits associated with DMDD.
Taken together, the aim of this study was to examine the correlates, psychiatric comorbidities, and social adjustment difficulties in children with DMDD from a national epidemiological study in Taiwan. Specifically, we compared children with DMDD to those with other psychiatric disorders and controls without any psychiatric disorder in demographic variables, psychiatric comorbidities, and social adjustment difficulties. We also compared social impairments among those with DMDD-only, ODD-only, DMDD+ODD, and controls without psychiatric disorders.
2. Methods
2.1. Participants and procedures
Taiwan’s National Epidemiological Study of Child Mental Disorders (NESCMD) is a school-based national epidemiological study focusing on common mental disorders among children in Taiwan (Chen et al., 2019; Chen et al., 2017). We used the stratified clustering sampling scheme to select a representative sample. The school sampling frame of this study was constructed using the school lists of 2012 from the Taiwan’s Ministry of Education. Nineteen counties in Taiwan were stratified into seven major geographic clusters based on population density, population ratio of people with educational levels of college or above, population ratio of people over the age of 65, population ratio of agricultural workers, and the number of physicians per 100,000 people (Chen et al., 2019). Cluster 1 represents the highest and cluster 7 the least urbanicity (Liu et al., 2006). Overall, of 10118 eligible children, 9560 (94.4%) children, 6846 (67.6%) parents, and 9759 (96.3%) teachers provided written informed consent to the study and completed the questionnaire-based survey from June 1, 2015 to January 31, 2017. With written consents to the psychiatric interviews from the participants and their parents, 4816 (47.6%; 2520 boys, 52.3%) children in grade 3 (n=1352, 28.1%; 693 boys, 51.2%), grade 5 (n=1297, 26.9%; 666 boys, 51.4%), and grade 7 (n=2167, 45.0%; 1161 boys, 53.6%) received psychiatric interview of the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Epidemiologic (K-SADS-E) for DSM-5 (Chen et al., 2017) by trained interviewers (Chen et al., 2019). Thirty children were diagnosed with DMDD (both full and subthreshold) based on the K-SADS-E, including 23 boys (76.67%) and 7 girls. The weighted prevalence was 0.3 (full criteria) to 0.76% (full + subthreshold) in Taiwan (Chen et al., 2019). Subthreshold DMDD was defined as whose temper outbursts and/or irritable mood last only for 6–12 months.
2.2. Measures
2.2.1. The Mandarin version of the K-SADS-E was revised in accordance with DSM-5 diagnoses.
The K-SADS-E is a semistructured clinical interview to assess lifetime and current episodes of mental disorders in children and adolescents (Ambrosini, 2000). The Mandarin version of the K-SADS-E for DSM-IV was developed by the Child Psychiatry Research Group in Taiwan (Gau et al., 2005), and was further prepared for the DSM-5 (Chen et al., 2017). The K-SADS-E consists of a screener and full supplements of each of the disorders included. The interviewers first completed the entire set of screening questions. If symptoms were endorsed on the screeners, the interviewers then went on to complete the full supplements of the disorders, inquiring about the symptoms, course, age of onset, impairments, specifiers, and exclusion for each psychiatric disorder. Our previous study has demonstrated good interrater reliability (prevalence adjusted bias-adjusted kappa = .80–1.00) and convergent and divergent validity of the Mandarin version of the K-SADS-E (Chen et al., 2017).
2.2.2. Social Adjustment Inventory for Children and Adolescents (SAICA).
The SAICA is a 77-item scale designed to assess adaptive functioning in children and adolescents aged 6–18 years (John et al., 1987). Participating children and their parents reported on the child’s behaviors and functions in multiple domains, including school, spare time, peer relations, and home behaviors. A higher mean score (items rated on a 4-point Likert scale from 1 to 4) indicates either more reduced social functions or more severe social problems. The SAICA has been widely used in studies of social outcomes for youth with ADHD with good validity (Biederman et al., 1993). The Chinese version of SAICA has been shown to be a reliable and valid instrument to measure adjustment problems in youth in Taiwan (Gau et al., 2006).
2.3. Interviewer training and fieldwork
Prior to conducting the K-SADS-E interviews, eight interviewers, who earned a bachelor’s or master’s degree in psychology with extensive experience working with children and families, received intensive clinical training in childhood mental disorders and in conducting clinical and psychiatric interviews with children and their parents. The training, lasting at least six months, included reading, observation, practice, case presentation and discussion, and structured and semistructured interviews using the K-SADS-E. Each interviewer was required to interview ten clinical subjects independently. They qualified as the interviewers for this study only when their ratings showed at least 90% agreement with those conducted by the corresponding author.
The Research Ethics Committee of National Taiwan University Hospital approved this study prior to its implementation (approval number: 201411056RINA). After the representative schools were chosen, we sent a letter with descriptions of the purpose and procedure of this study to the schools through Taiwan’s Ministry of Education. With permission from school principals, we obtained written informed consent from both the children and their parents. Children were interviewed with the K-SADS-E at school, and parents were asked to complete a questionnaire (including the SAICA) brought home by the child. Participating children/families received compensation of NT$200 (approximately US$7).
2.4. Statistical analyses
Statistical analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC, USA). Weighted prevalence rate and 95% confidence interval were analyzed using the PROC SURVEYFREQ to address the complex survey design. We conducted logistic regressions for categorical outcome variables using the PROC SURVEYLOGISTC and linear regressions for continuous outcome variables using PROC SURVEYREG to examine between-group differences that controlled for stratification and clustering. We divided the participants into three groups: children with DMDD (n = 30), children with other psychiatric disorders but not DMDD (n = 1573), and children without any psychiatric disorders (n = 3213) and examined group differences in demographics and social adjustment while controlling for age and sex. Weighted odds ratios of psychiatric comorbidities were calculated for children with DMDD against those without DMDD. To compare between DMDD and ODD on social adjustment, we categorized children with DMDD and/or ODD into three groups: (1) those with DMDD and ODD (DMDD+ODD); (2) those with DMDD only (DMDD-only); (3) those with ODD only (ODD-only). For research purposes, the DSM-5 exclusion of ODD when diagnosing DMDD was not applied. Additional comparisons were performed among these three DMDD and/or ODD groups for demographic data and psychiatric comorbidities. Social adjustment was compared among these three groups and the control group after adjusting for age and sex (and the diagnosis of ADHD and the statistical result controlling for age, sex, and ADHD was presented in the supplementary Table). Bonferroni method was used for the correction of multiple group comparisons for continuous variables in post-hoc comparisons. We set the significance level at alpha = 0.05.
3. Results
3.1. Demographics
There were significantly more males in the DMDD group than in the other two groups (i.e., those with other psychiatric disorders and those without any disorders). There were no significant group differences in participants’ age and parents’ age. Parents of children with DMDD and other psychiatric disorders had lower educational levels than parents of those without any psychiatric disorders. The mean age of onset of DMDD symptoms was 5 years old (Table 1).
Table 1.
Demographic data
| N (%) or mean (SD) | DMDD (n = 30) | Other psychiatric disorder (n = 1573) | No psychiatric disorder (n = 3213) | Statistics Wald χ2 or F (p) |
|---|---|---|---|---|
| Gender, male | 23 (76.67) | 888 (56.45) | 1615 (50.08) | 24.37 (< .001) |
| Age | 11.31 (1.66) | 11.42 (1.67) | 11.30 (1.68) | 1.06 (0.35) |
| School grade | ||||
| Grade 3 | 9 (30.00) | 418 (26.57) | 925 (28.79) | 8.18 (0.09) |
| Grade 5 | 10 (33.33) | 403 (25.62) | 884 (27.51) | |
| Grade 7 | 11 (36.67) | 752 (47.81) | 1404 (43.70) | |
| Age of onset of DMDD, years (Age range, years) | 5 (2.79) (1–8) | |||
| Father’s age | 43.43 (6.21) | 44.03 (5.69) | 43.86 (5.70) | 1.23 (0.30) |
| Mother’s age | 39.83 (4.93) | 40.60 (5.05) | 40.40 (4.93) | 0.64 (0.53) |
| Father’s education | ||||
| Junior high school or below | 5 (20.00) | 178 (14.42) | 295 (11.05) | 21.15 (0.002) |
| Senior high school | 11 (44.00) | 622 (50.41) | 1276 (47.81) | |
| College | 8 (32.00) | 312 (25.28) | 753 (28.21) | |
| Postgraduate | 1 (4.00) | 122 (9.89) | 345 (12.93) | |
| Mother’s education | ||||
| Junior high school and below | 4 (14.81) | 160 (13.07) | 278 (10.35) | 15.74 (0.02) |
| Senior high school | 13 (48.15) | 679 (55.47) | 1413 (52.59) | |
| College | 9 (33.33) | 322 (26.31) | 817 (30.40) | |
| Postgraduate | 1 (3.70) | 63 (5.15) | 179 (6.66) |
Note. DMDD: disruptive mood dysregulation disorder; SD: standard deviation
3.2. Psychiatric comorbidities
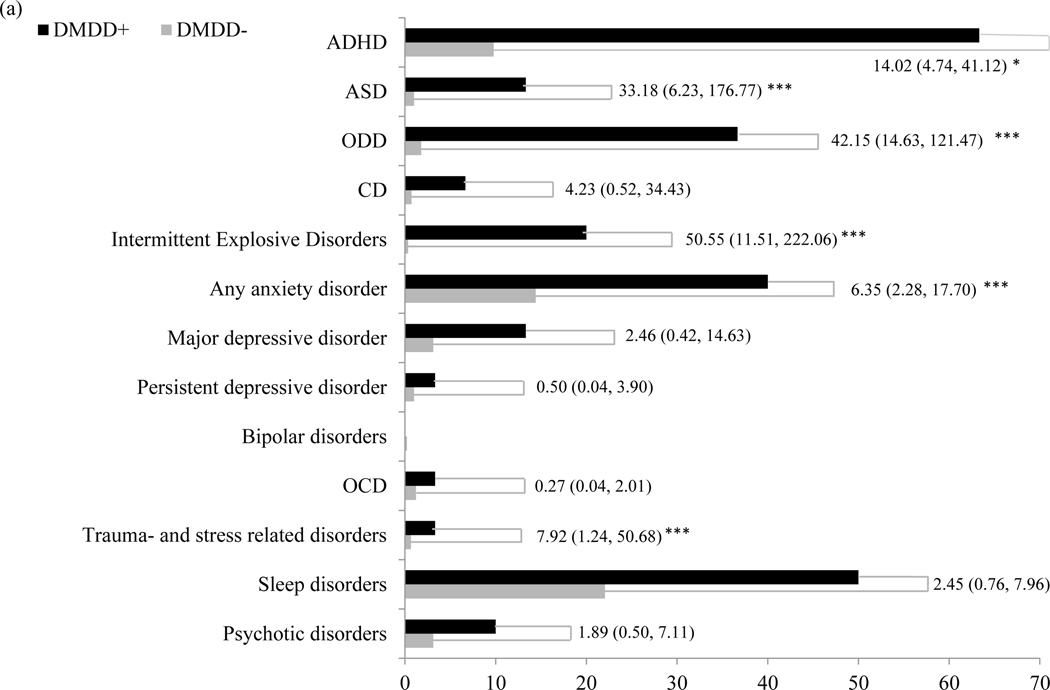
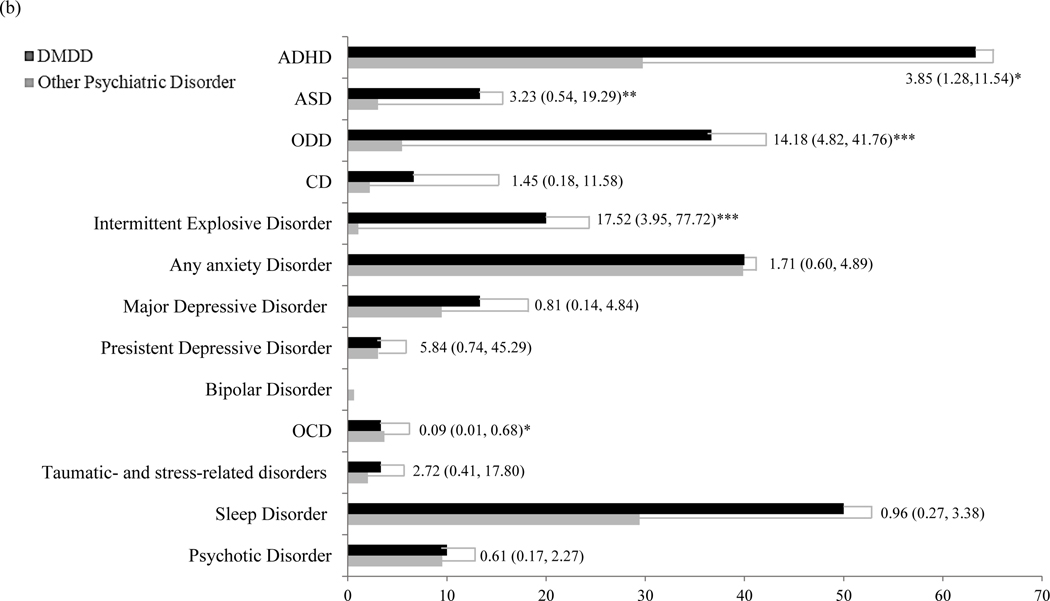
Among the 30 children with DMDD, 29 (96.67%) had at least one psychiatric comorbidity. Compared to children without DMDD, those with DMDD had significantly higher risks of having other psychiatric comorbidities, including ADHD, autism spectrum disorder (ASD), ODD, intermittent explosive disorder, anxiety disorders, and trauma- and stress-related disorders (Figure 1a, Supplementary Table S1). Surprisingly, children with DMDD did not have a significantly higher risk for mood disorders than those without. Compared to children with other psychiatric disorders, those with DMDD had significantly higher risks of having ADHD, ASD, ODD, intermittent explosive disorder, and a lower risk of obsessive-compulsive disorder (Figure 1b, Supplementary Table S2).
Figure 1.
Psychiatric Comorbidities. 1a: Comparison between subjects with DMDD and without DMDD. 1b: Comparison between subjects with DMDD and subjects with other psychiatric disorders. Weighted odds ratio is presented with 95% confidence interval. * P < 0.05, ** P < 0.01, *** P < 0.001. DMDD = Disruptive Mood Dysregulation Disorder, ADHD = Attention-Deficit/Hyperactivity Disorder, ASD = Autism Spectrum Disorder, ODD = Oppositional Defiant Disorder, CD = Conduct Disorder, OCD = Obsessive Compulsive Disorder.
Eight children with DMDD (26.67% of all children with DMDD) had one psychiatric comorbidity, including ADHD (n = 2), ASD (n =1), anxiety disorders (n = 3) and sleep disorders (n = 2). Ten children with DMDD (33.33%) had two psychiatric comorbidities, 4 children (13.33%) had three, 3 children (10%) had four, 2 (6.67%) had five and 2 (6.67%) had six psychiatric comorbidities. Only one child with DMDD had no other psychiatric disorders.
3.3. Social adjustment difficulties
Compared to children without any psychiatric disorders, children with DMDD had more difficulties in overall school functions, particularly behavioral problems at school (e.g., “does not pay attention or listen,” “is disruptive/bothers others in the class,” “is excluded by others”) by parent reports, and in various domains of school functioning (except academic performance) and overall home functioning, particularly sibling interaction, by self-reports. Children with other psychiatric disorders had significantly more difficulties in all areas of functioning than children without any psychiatric disorders, regardless of informants (Table 2).
Table 2.
Group Comparisons of maternal- and self-reports of social adjustment difficulties
| Variables | 1.DMDD (n = 30) | 2.Other psychiatric disorder (n = 1573) | 3.No psychiatric disorder (n = 3213) | Comparison | Statistical analysis | ||||
|---|---|---|---|---|---|---|---|---|---|
| 1 VS. 2 | 1 VS. 3 | 2 VS. 3 | F | p | Post-hoc comparison | ||||
| Mean (SD) | Cohen d | ||||||||
| Parent-report | |||||||||
| School function | 1.66 (0.42) | 1.50 (0.4) | 1.34 (0.31) | 3.00 | 1.03 | 0.47 | 18.54 | <.001 | 1,2>3 |
| Academic performance | 2.03 (0.8) | 1.93 (0.76) | 1.71 (0.67) | 0.13 | 0.48 | 0.31 | 8.45 | 0.001 | 2>3 |
| Attitude toward school | 1.8 (0.91) | 1.7 (0.79) | 1.5 (0.67) | 0.13 | 0.45 | 0.28 | 5.14 | 0.009 | 2>3 |
| Peer interaction | 1.75 (0.41) | 1.53 (0.37) | 1.4 (0.31) | 0.59 | 1.13 | 0.39 | 12.90 | <.001 | 2>3 |
| School behavior | 1.57 (0.39) | 1.38 (0.38) | 1.23 (0.28) | 0.50 | 1.21 | 0.48 | 25.21 | <.001 | 1,2>3 |
| Home behavior | 1.38 (0.31) | 1.4 (0.36) | 1.31 (0.3) | −0.06 | 0.23 | 0.28 | 12.81 | <.001 | 2>3 |
| Sibling interaction | 1.26 (0.25) | 1.3 (0.37) | 1.21 (0.29) | −0.11 | 0.17 | 0.28 | 5.49 | <.001 | 2>3 |
| Parent-child interaction | 1.44 (0.38) | 1.47 (0.42) | 1.37 (0.36) | −0.07 | 0.19 | 0.26 | 10.02 | <.001 | 2>3 |
| Self-report | |||||||||
| School function | 1.84 (0.62) | 1.55 (0.38) | 1.34 (0.29) | 0.75 | 1.70 | 0.65 | 90.09 | <.001 | 1,2>3 |
| Academic performance | 2.05 (0.76) | 2.05 (0.78) | 1.8 (0.69) | 0.00 | 0.36 | 0.35 | 22.07 | <.001 | 2>3 |
| Attitude toward school | 2.14 (0.99) | 1.81 (0.82) | 1.52 (0.67) | 0.40 | 0.92 | 0.40 | 35.03 | <.001 | 1,2>3 |
| Peer interaction | 1.95 (0.66) | 1.58 (0.41) | 1.4 (0.32) | 0.89 | 1.69 | 0.51 | 45.52 | <.001 | 1,2>3 |
| School behavior | 1.79 (0.67) | 1.42 (0.39) | 1.22 (0.28) | 0.93 | 1.99 | 0.62 | 76.06 | <.001 | 1,2>3 |
| Home behavior | 1.64 (0.6) | 1.42 (0.39) | 1.27 (0.31) | 0.56 | 1.18 | 0.44 | 25.00 | <.001 | 1,2>3 |
| Sibling interaction | 1.77 (0.82) | 1.38 (0.47) | 1.24 (0.36) | 0.82 | 1.45 | 0.35 | 12.78 | <.001 | 1>2>3 |
| Parent-child interaction | 1.57 (0.57) | 1.44 (0.43) | 1.29 (0.35) | 0.30 | 0.79 | 0.40 | 24.82 | <.001 | 2>3 |
Note. Analyses controlled for age and sex. Group comparisons were corrected by Bonferroni method.
DMDD: disruptive mood dysregulation disorder; SD: standard deviation
3.4. Comparisons between those with ODD and/or DMDD
There were 11, 19, and 86 children in the DMDD+ODD, DMDD-only, and ODD-only groups. There were no between-group differences in age, sex, parental ages, and parental education. Children with ODD+DMDD had an earlier onset of DMDD symptoms than those with DMDD-only (Supplementary Table S3). In general, children with DMDD+ODD were more likely to have psychiatric comorbidities, including ADHD, anxiety, and depressive disorders than those with ODD- or DMDD-only (Supplementary Table S4). Children with ODD-only had slightly higher risks of conduct disorder, depressive disorders, and bipolar disorder than those with DMDD-only. Parents reported that children with ODD, with or without DMDD, had more problems at school and home (except for peer/sibling interaction) than children with DMDD-only. The children with ODD+/−DMDD themselves felt that they had more problems in academic performance, attitude, and behavior problems at school than those with DMDD-only. No significant differences were noted in peer interaction at school or parent-child relationships at home between the ODD-only and DMDD-only groups. Still, parents reported more problems at home with their children with ODD than DMDD (Table 3). There was a trend of dose-dependent effect of school functions in the three groups, i.e., children with DMDD+ODD had worst school functions, followed by those with ODD-only and then those with DMDD-only. After adjusting for ADHD, the significance of parent-reported problems diminished significantly in the ODD-only group, whereas the significant differences noted in self-reported problems remained mostly substantial (Supplementary Table S5).
Table 3.
Maternal- and self-reports of social adjustment difficulties by DMDD and/or ODD
| Variables | 1.DMDD+ODD (n = 11) | 2.DMDD-only (n = 19) | 3.ODD-only (n = 86) | 4.No psychiatric disorder (n = 3213) | Statistical analysis | ||
|---|---|---|---|---|---|---|---|
| Mean (SD) | F | p | Post-hoc comparison | ||||
| Parent-report | |||||||
| School function | 1.82 (0.45) | 1.56 (0.38) | 1.8 (0.59) | 1.34 (0.31) | 17.89 | <.001 | 1,3>4; 1>2 |
| Academic performance | 2.31 (0.45) | 1.88 (0.91) | 2.24 (0.93) | 1.71 (0.67) | 11.64 | <.001 | 1>2,4 |
| Attitude toward school | 2.25 (1.04) | 1.59 (0.8) | 2.06 (0.89) | 1.5 (0.67) | 9.09 | <.001 | 1,3>2,4 |
| Peer interaction | 1.89 (0.4) | 1.66 (0.4) | 1.66 (0.42) | 1.4 (0.31) | 5.88 | 0.0013 | 1>4 |
| School behavior | 1.72 (0.45) | 1.48 (0.33) | 1.67 (0.56) | 1.23 (0.28) | 3.84 | 0.03 | 1>2,4; 3>4 |
| Home behavior | 1.51 (0.35) | 1.29 (0.26) | 1.59 (0.46) | 1.31 (0.3) | 4.05 | 0.03 | 3>2,4 |
| Sibling interaction | 1.35 (0.29) | 1.21 (0.23) | 1.43 (0.44) | 1.21 (0.29) | 1.22 | 0.31 | |
| Parent-child interaction | 1.54 (0.42) | 1.38 (0.36) | 1.7 (0.53) | 1.37 (0.36) | 4.79 | 0.005 | 3>2,4 |
| Self-report | |||||||
| School function | 2.19 (0.8) | 1.66 (0.42) | 1.84 (0.47) | 1.34 (0.29) | 14.08 | <.001 | 1,3>2,4 |
| Academic performance | 2.4 (0.82) | 1.86 (0.68) | 2.51 (0.93) | 1.8 (0.69) | 16.73 | <.001 | 1,3>2,4 |
| Attitude toward school | 2.8 (1.14) | 1.79 (0.71) | 2.16 (1.02) | 1.52 (0.67) | 14.39 | <.001 | 1>2,3,4; 3>4 |
| Peer interaction | 2.01 (0.84) | 1.92 (0.56) | 1.75 (0.46) | 1.4 (0.32) | 7.94 | <.001 | 3>4 |
| School behavior | 2.12 (0.85) | 1.61 (0.5) | 1.72 (0.54) | 1.22 (0.28) | 14.58 | <.001 | 1>2,3,4; 3>4 |
| Home behavior | 1.75 (0.86) | 1.58 (0.4) | 1.6 (0.46) | 1.27 (0.31) | 8.16 | <.001 | 2,3>4 |
| Sibling interaction | 1.91 (0.92) | 1.68 (0.77) | 1.57 (0.58) | 1.24 (0.36) | 4.17 | 0.01 | 1>4 |
| Parent-child interaction | 1.67 (0.89) | 1.51 (0.3) | 1.65 (0.51) | 1.29 (0.35) | 15.53 | <.001 | 3>4 |
Note. Statistical analysis adjusted for age and sex. Group comparisons were corrected by Bonferroni method.
DMDD: disruptive mood dysregulation disorder; ODD: oppositional defiant disorder; SD: standard deviation
4. Discussion
As one of a few studies on the expressions and comorbidities of DMDD, we found that the weighted prevalence of DMDD was 0.3~0.76% (depending on the stringency of diagnostic criteria) in Taiwan (Chen et al., 2019) with male vs. female ratio as 3:1 in our sample. Parents of children with DMDD or other psychiatric comorbidities had lower educational levels than parents of children without any psychiatric disorder. Children with DMDD had a wide variety of psychiatric comorbidities and social impairments at home and school as compared to controls. Relative to those with other psychiatric disorders, children with DMDD had significantly higher risks of having ADHD, ASD, ODD, intermittent explosive disorder, and more self-reported problematic interactions with siblings. Children with DMDD+ODD had more anxiety disorders than those with ODD-only and more major depressive and separation anxiety disorders and ADHD than those with DMDD-only. Based on parent- and self-reports, children with ODD+/−DMDD had more problematic behaviors at home and school than those with DMDD-only, and children with DMDD-only had more problems in self-reported home behavior as compared to controls without any psychiatric comorbidity.
The prevalence of DMDD in Taiwan was consistent with other Western community studies (Copeland et al., 2013), which also reported 0.3~5% depending on the stringency of the criteria used. It is possible that DMDD is rare in the community when the criteria are strictly applied and that the prevalence in late childhood and adolescence is lower than that in early childhood (Copeland et al., 2013). Given that irritability is among the most common reasons that children and adolescents are referred to the clinic (Stringaris et al., 2018) and that the rate of DMDD is substantially higher in clinical samples (Baweja et al., 2016), it raises the question of whether the current DSM-5 DMDD criteria are too strict, as many youths who fail to meet the full DMDD criteria are significantly impaired due to irritability.
Most of the previous Western studies reported equal sex distribution of DMDD in the community samples (Copeland et al., 2013; Dougherty et al., 2014; Althoff et al., 2016), yet the male-dominant tendency in clinical samples (Benarous et al., 2020). We found a male predominant ratio in the community survey, which may possibly be due to cultural differences. Based on a previous study, the variance of irritability is largely explained by the non-shared environmental factors (70%) (Stringaris et al., 2012a). Furthermore, the non-shared environmental factors play a more critical role in the development of irritability in girls during late childhood to adolescence than early childhood. In contrast, the non-shared environmental influences weaken as boys develop from early childhood to adolescence (Wiggins et al., 2016). In Chinese culture, girls are socialized and expected to suppress their anger and outburst relative to boys. Therefore, non-shared environmental factors such as socialization in emotion expression may limit the presentation of anger and irritability in girls, resulting a male predominant rate of DMDD in Taiwan. More data from Asian countries with similar cultures are required to test this hypothesis and replicate our findings.
We found that parents of children with DMDD had lower educational attainment than those without DMDD, consistent with one study (Althoff et al., 2016) but not with another (Copeland et al., 2013). There were no differences in parental education levels between children with DMDD and children with ODD. Because severe irritability might be inherited (Coccaro et al., 1997) and was found to predict low education and income attainment (Vidal-Ribas et al., 2016), parental educational levels and the occurrence of DMDD in the offspring might have a common genetic basis. On the other hand, based on the model of aberrant reward and threat processing in severe irritability, environmental factors also play a role here through instrumental learning (Thomas et al., 2012). Parents with lower educational levels, relative to those with higher educational levels, maybe more inconsistent in parenting and have more difficulties in managing their anger and their children’s emotional problems effectively due to a lack of skills or time, thereby exacerbating the children’s irritability.
Similar to other community studies (Copeland et al., 2013; Althoff et al., 2016), DMDD is comorbid with various psychiatric disorders, especially disruptive behavior disorders (i.e., ADHD, ODD) as well as ASD and anxiety disorders. The association between DMDD and neurodevelopmental disorders is not new (Mayes et al., 2016; Copeland et al., 2013). We did not find a higher rate of depressive disorders in children with DMDD than those without, possibly due to a small sample size of DMDD and the relatively young age of our sample. The high correlation of childhood irritability and later depression/anxiety in adolescence and adulthood has been reported (Vidal-Ribas et al., 2016). It was proposed that these symptoms (i.e., depressive/anxious behavior and chronic irritability) might share common genetic and environmental factors (Savage et al., 2015). DSM-5, therefore, put DMDD in the category of depressive disorder. Nevertheless, during young adolescence, the overlap of DMDD, MDD, and PDD might not be high (Benarous et al., 2020). Furthermore, a recent study provided a different perspective. Using the Genome-wide polygenic risk scores, Nigg et al. (2020) found that irritability-anger was more related to ADHD-related genetic risk and not mood-related genetic risk. If the mood dysregulation in ADHD was closer to ADHD per se and not mood factors, how about the DMDD without comorbid ADHD? Are the correlations between DMDD and later depressive/anxiety disorders based on a common genetic basis, a shared environmental adversity, or DMDD as the risk factor for later depressive disorders? It requires further genetic and longitudinal familial studies incorporating comprehensive psychiatric evaluations and carefully dissecting the psychiatric disorders to answer this question.
In addition to the complex correlations between DMDD and internalizing problems, the overlapping symptoms (i.e., chronic irritability and temper outbursts) of DMDD and ODD also raised questions about the necessity of creating a new diagnosis (Mayes et al., 2016), leading to different diagnostic strategies in chronic irritability between ICD and DSM. In our analyses comparing psychiatric comorbidities of DMDD+ODD, DMDD-only, and ODD-only, it was not surprising that DMDD+ODD had higher rates of psychiatric comorbidities than DMDD- and ODD-only. Generally speaking, the DMDD and ODD groups had similar rates of psychiatric comorbidities, except a slightly higher rate of MDD and bipolar disorder in the ODD-only than in the DMDD-only group and a trend of more phobic disorders in the DMDD-only than in the ODD group. There was no comorbidity of conduct disorder in the DMDD-only group, compared to 15–18 % in the DMDD+ODD and ODD-only group, implying that the construct of DMDD is less of a “behavioral/externalizing” disorder and more of a “mood/internalizing” disorder. Hence, the hierarchical exclusion of ODD while DMDD is diagnosed in the DSM-5 might overlook the behavioral (i.e., hurtful and headstrong) dimensions of ODD (Stringaris and Goodman, 2009; Benarous et al., 2020).
Although parents did not report DMDD having more problems at home than controls, parents and children with DMDD themselves rated more difficulties at school. While further comparing the impact of ODD and DMDD on these functions, the impairment in the DMDD-only group was less than that in the ODD-only group even after accounting for the influence of ADHD, especially in the attitude toward school and academic performance. DMDD and ODD had a similar impact on peer interactions both at school and at home. In summary, children with DMDD, unlike ODD, were able to behave well at school and had non-inferior academic performance as compared to controls. The problems of them were in the broken relationship, especially with peers. A trend of dose-dependent influence on social adjustment was found such that those with DMDD+ODD had worst school functions, followed by those with ODD-only and then those with DMDD-only. Other community studies found that DMDD by itself is associated with significant impairment (Copeland et al., 2013) and poor adult outcomes after adjusting for comorbidities (Copeland et al., 2014). These two studies only adjusted the overall psychiatric disorders but not specific psychiatric disorders, such as ADHD or ODD. In a recent comparison of impairment of DMDD and ADHD, the authors suggested that the higher impairment of DMDD than ADHD was due to a higher comorbid rate of ODD in DMDD than ADHD (Uran and Kılıç, 2020). In their study, they also found a dose-dependent tendency of impairment (i.e., the more the psychiatric diagnoses, the higher the impairments). Future studies are needed to elucidate whether the impairment of DMDD is largely due to DMDD symptoms or other common comorbid disorders. On the other hand, it is consistently found that comorbid DMDD with other psychiatric disorders would further impair functions of the affected ones without DMDD.
Our findings should be interpreted in the context of the following limitations. First, the diagnostic interview using the K-SADS-E should ideally be conducted with both children and their parents. In this school-based study, we only interviewed the child because it was not feasible to ask the parents to participate in the interview at school. This limitation may partially explain why the prevalence of DMDD is low in this sample, as youths tend to under-report their temper outbursts and irritability (Stringaris et al., 2012b; Wakschlag et al., 2012). Second, this survey is completely voluntary. Of the eligible potential participants, only 50.4% participated in the diagnostic interview. Thus, our results might suffer from some degree of non-response bias. That is, children who underwent the clinical interview (with informed consent provided) may have more emotional and behavioral problems compared with children whose parents did not consent to the clinical interview. Nevertheless, the non-response bias might have little impact on our results of the prevalence rates of mental disorders because the prevalence rates before and after the adjustment of inverse probability censoring weighting did not differ significantly. Hence, it is suggested that our results provided robust estimates of the national prevalence of mental disorders in children. Third, because the prevalence of DMDD in our sample was low and we did not want to miss any potential case of DMDD, we included the children with subthreshold DMDD in the analysis. Such approach may have influenced the estimates of the impairment caused by DMDD and the rates of psychiatric comorbidities. Even after including subthreshold DMDD, the overall sample size for DMDD was still small, and thus, our analyses may be underpowered to detect significant associations and differences. Further studies with a large sample size are warranted to validate our findings.
5. Conclusions
DMDD, strictly defined based on the full DSM-5 criteria, is not a common disorder (prevalence 0.3~0.76%) in the community, at least in Taiwan, and has a high rate of psychiatric comorbidities such as ADHD, ASD, ODD, intermittent explosive disorder, and anxiety disorders. DMDD alone without any psychiatric comorbidity is rare, and the impairment of DMDD might be confounded by impairment due to other comorbid disorders or symptoms such as ODD or ADHD. However, the overlap of DMDD and ODD in our study was not as high as other studies (Mayes et al., 2016), raising whether ODD with a specifier of chronic irritability-anger in the ICD is adequate to represent all youth with DMDD. In contrast, the hierarchical exclusion of ODD in subjects diagnosed with DMDD in the DSM-5 might overlook the behavioral component of ODD (headstrong/hurtful), which had been demonstrated to predict later conduct disorder. Given the strong correlation with later depressive and anxiety disorders and often add more impairment to other psychiatric disorders, chronic irritability, which the DMDD diagnosis is intended to capture, has important clinical implications. DMDD itself might not directly influence the school achievement on children but had a significant impact on peer relationships. However, there is currently a lack of standard, effective treatment for irritability or DMDD. Recent studies suggest that a combination of citalopram and stimulants may be efficacious in treating youth with severe, chronic irritability (Shaw et al., 2014) and that exposure-based cognitive behavioral therapy may also be a promising approach (Towbin et al., 2020). There has been an increase in research on chronic irritability since the inception of DMDD, more research on the behavioral correlates and neurobiological and genetic underpinnings are essential to guide the development of effective treatment for chronic irritability and DMDD.
Supplementary Material
Acknowledgments
We thank all the participants, their parents, and school teachers who participated in our study. We also thank the research assistants for their help in data collection.
Funding
This work was supported by grants from the Ministry of Health and Welfare (M03B3374), National Health Research Institute (NHRI-EX104–10404PI, NHRI-EX105–10404PI, NHRI-EX106–10404PI), and Ministry of Science and Technology (MOST 103–2314-B-002–021-MY3). Wan-Ling Tseng has received grant support from the National Institute of Mental Health (R00MH110570).
Footnotes
Declaration of Conflicting Interests
All authors declare no conflicts of interest about the design, implementation of the study, and the publication of the results.
References
- Althoff RR, Crehan ET, He JP, et al. , 2016. Disruptive Mood Dysregulation Disorder at Ages 13–18: Results from the National Comorbidity Survey-Adolescent Supplement. J Child Adolesc Psychopharmacol. 26 (2), 107–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ambrosini PJ, 2000. Historical development and present status of the schedule for affective disorders and schizophrenia for school-age children (K-SADS). J Am Acad Child Adolesc Psychiatry. 39 (1), 49–58. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, 2013. Diagnostic and Statistical Manual of Mental Disorders. 5 ed. Washington, DC: American Psychiatric Press. [Google Scholar]
- Axelson D, Findling RL, Fristad MA, et al. , 2012. Examining the proposed disruptive mood dysregulation disorder diagnosis in children in the Longitudinal Assessment of Manic Symptoms study. J Clin Psychiatry. 73 (10), 1342–1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baweja R, Mayes SD, Hameed U, et al. , 2016. Disruptive mood dysregulation disorder: current insights. Neuropsychiatr Dis Treat. 12, 2115–2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benarous X, Renaud J, Breton JJ, et al. , 2020. Are youths with disruptive mood dysregulation disorder different from youths with major depressive disorder or persistent depressive disorder? J Affect Disord. 265, 207–215. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV and Chen WJ, 1993. Social Adjustment Inventory for Children and Adolescents: concurrent validity in ADHD children. J Am Acad Child Adolesc Psychiatry. 32 (5), 1059–1064. [DOI] [PubMed] [Google Scholar]
- Blader JC and Carlson GA, 2007. Increased Rates of Bipolar Disorder Diagnoses among U.S. Child, Adolescent, and Adult Inpatients, 1996–2004. Biol Psychiatry. 62 (2), 107–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brotman MA, Kassem L, Reising MM, et al. , 2007. Parental diagnoses in youth with narrow phenotype bipolar disorder or severe mood dysregulation. Am J Psychiatry. 164 (8), 1238–1241. [DOI] [PubMed] [Google Scholar]
- Brotman MA, Kircanski K, Stringaris A, et al. , 2017. Irritability in Youths: A Translational Model. Am J Psychiatry. 174 (6), 520–532. [DOI] [PubMed] [Google Scholar]
- Brotman MA, Schmajuk M, Rich BA, et al. , 2006. Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biol Psychiatry. 60 (9), 991–997. [DOI] [PubMed] [Google Scholar]
- Chen YL, Chen WJ, Lin KC, et al. , 2019. Prevalence of DSM-5 mental disorders in a nationally representative sample of children in Taiwan: methodology and main findings. Epidemiol Psychiatr Sci. 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen YL, Shen LJ and Gau SS, 2017. The Mandarin version of the Kiddie-Schedule for Affective Disorders and Schizophrenia-Epidemiological version for DSM-5 - A psychometric study. J Formos Med Assoc. 116 (9), 671–678. doi: 10.1016/j.jfma.2017.1006.1013. Epub 2017 Jul 1011. [DOI] [PubMed] [Google Scholar]
- Coccaro EF, Bergeman CS, Kavoussi RJ, et al. , 1997. Heritability of aggression and irritability: a twin study of the Buss-Durkee aggression scales in adult male subjects. Biol Psychiatry. 41 (3), 273–284. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Angold A, Costello EJ, et al. , 2013. Prevalence, comorbidity, and correlates of DSM-5 proposed disruptive mood dysregulation disorder. Am J Psychiatry. 170 (2), 173–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Shanahan L, Egger H, et al. , 2014. Adult diagnostic and functional outcomes of DSM-5 disruptive mood dysregulation disorder. Am J Psychiatry. 171 (6), 668–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty LR, Smith VC, Bufferd SJ, et al. , 2014. DSM-5 disruptive mood dysregulation disorder: correlates and predictors in young children. Psychol Med. 44 (11), 2339–2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans SC, Burke JD, Roberts MC, et al. , 2017. Irritability in child and adolescent psychopathology: An integrative review for ICD-11. Clin Psychol Rev. 53, 29–45. [DOI] [PubMed] [Google Scholar]
- Freeman AJ, Youngstrom EA, Youngstrom JK, et al. , 2016. Disruptive Mood Dysregulation Disorder in a Community Mental Health Clinic: Prevalence, Comorbidity and Correlates. J Child Adolesc Psychopharmacol. 26 (2), 123–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gau SS, Chong MY, Chen TH, et al. , 2005. A 3-year panel study of mental disorders among adolescents in Taiwan. Am J Psychiatry. 162 (7), 1344–1350. [DOI] [PubMed] [Google Scholar]
- Gau SS, Shen HY, Soong WT, et al. , 2006. An open-label, randomized, active-controlled equivalent trial of osmotic release oral system methylphenidate in children with attention-deficit/hyperactivity disorder in Taiwan. J Child Adolesc Psychopharmacol. 16 (4), 441–455. [DOI] [PubMed] [Google Scholar]
- Grau K, Plener PL, Hohmann S, et al. , 2018. Prevalence Rate and Course of Symptoms of Disruptive Mood Dysregulation Disorder (DMDD). Z Kinder Jugendpsychiatr Psychother. 46 (1), 29–38. [DOI] [PubMed] [Google Scholar]
- John K, Gammon GD, Prusoff BA, et al. , 1987. The Social Adjustment Inventory for Children and Adolescents (SAICA): testing of a new semistructured interview. J Am Acad Child Adolesc Psychiatry. 26, 898–911. [DOI] [PubMed] [Google Scholar]
- Leibenluft E, 2011. Severe mood dysregulation, irritability, and the diagnostic boundaries of bipolar disorder in youths. Am J Psychiatry. 168 (2), 129–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leibenluft E, 2017. Pediatric Irritability: A Systems Neuroscience Approach. Trends Cogn Sci. 21 (4), 277–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leibenluft E, Cohen P, Gorrindo T, et al. , 2006. Chronic versus episodic irritability in youth: a community-based, longitudinal study of clinical and diagnostic associations. J Child Adolesc Psychopharmacol. 16 (4), 456–466. [DOI] [PubMed] [Google Scholar]
- Liu CY, Hung YT, Chuang YL, et al. , 2006. Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey [in Chinese, with English abstract]. J Health Manag. 4, 1–22. [Google Scholar]
- Mayes SD, Waxmonsky JD, Calhoun SL, et al. , 2016. Disruptive Mood Dysregulation Disorder Symptoms and Association with Oppositional Defiant and Other Disorders in a General Population Child Sample. J Child Adolesc Psychopharmacol. 26 (2), 101–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulraney M, Schilpzand EJ, Hazell P, et al. , 2016. Comorbidity and correlates of disruptive mood dysregulation disorder in 6–8-year-old children with ADHD. Eur Child Adolesc Psychiatry. 25 (3), 321–330. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Karalunas SL, Gustafsson HC, et al. , 2020. Evaluating chronic emotional dysregulation and irritability in relation to ADHD and depression genetic risk in children with ADHD. J Child Psychol Psychiatry. 61 (2), 205–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Propper L, Cumby J, Patterson VC, et al. , 2017. Disruptive mood dysregulation disorder in offspring of parents with depression and bipolar disorder. Br J Psychiatry. 210 (6), 408–412. [DOI] [PubMed] [Google Scholar]
- Rich BA, Schmajuk M, Perez-Edgar KE, et al. , 2007. Different psychophysiological and behavioral responses elicited by frustration in pediatric bipolar disorder and severe mood dysregulation. Am J Psychiatry. 164 (2), 309–317. [DOI] [PubMed] [Google Scholar]
- Roy AK, Lopes V and Klein RG, 2014. Disruptive mood dysregulation disorder: a new diagnostic approach to chronic irritability in youth. Am J Psychiatry. 171 (9), 918–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage J, Verhulst B, Copeland W, et al. , 2015. A genetically informed study of the longitudinal relation between irritability and anxious/depressed symptoms. J Am Acad Child Adolesc Psychiatry. 54 (5), 377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw P, Stringaris A, Nigg J, et al. , 2014. Emotion dysregulation in attention deficit hyperactivity disorder. Am J Psychiatry. 171 (3), 276–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoddard J, Stringaris A, Brotman MA, et al. , 2014. Irritability in child and adolescent anxiety disorders. Depress Anixety. 31 (7), 566–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringaris A, 2011. Irritability in children and adolescents: a challenge for DSM-5. Eur Child Adolesc Psychiatry. 20 (2), 61–66. [DOI] [PubMed] [Google Scholar]
- Stringaris A, Cohen P, Pine DS, et al. , 2009. Adult outcomes of youth irritability: a 20-year prospective community-based study. Am J Psychiatry. 166 (9), 1048–1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringaris A and Goodman R, 2009. Longitudinal outcome of youth oppositionality: irritable, headstrong, and hurtful behaviors have distinctive predictions. J Am Acad Child Adolesc Psychiatry. 48 (4), 404–412. [DOI] [PubMed] [Google Scholar]
- Stringaris A, Goodman R, Ferdinando S, et al. , 2012a. The Affective Reactivity Index: a concise irritability scale for clinical and research settings. J Child Psychol Psychiatry. 53 (11), 1109–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringaris A, Vidal-Ribas P, Brotman MA, et al. , 2018. Practitioner Review: Definition, recognition, and treatment challenges of irritability in young people. J Child Psychol Psychiatry. 59 (7), 721–739. [DOI] [PubMed] [Google Scholar]
- Stringaris A, Zavos H, Leibenluft E, et al. , 2012b. Adolescent irritability: phenotypic associations and genetic links with depressed mood. Am J Psychiatry. 169 (1), 47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas LA, Brotman MA, Muhrer EJ, et al. , 2012. Parametric modulation of neural activity by emotion in youth with bipolar disorder, youth with severe mood dysregulation, and healthy volunteers. Arch Gen Psychiatry. 69 (12), 1257–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Towbin K, Vidal-Ribas P, Brotman MA, et al. , 2020. A Double-Blind Randomized Placebo-Controlled Trial of Citalopram Adjunctive to Stimulant Medication in Youth With Chronic Severe Irritability. J Am Acad Child Adolesc Psychiatry. 59 (3), 350–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uran P and Kılıç BG, 2020. Family Functioning, Comorbidities, and Behavioral Profiles of Children With ADHD and Disruptive Mood Dysregulation Disorder. J Atten Disord. 24 (9), 1285–1294. [DOI] [PubMed] [Google Scholar]
- Vidal-Ribas P, Brotman MA, Valdivieso I, et al. , 2016. The Status of Irritability in Psychiatry: A Conceptual and Quantitative Review. J Am Acad Child Adolesc Psychiatry. 55 (7), 556–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wakschlag LS, Choi SW, Carter AS, et al. , 2012. Defining the developmental parameters of temper loss in early childhood: implications for developmental psychopathology. J Child Psychol Psychiatry. 53 (11), 1099–1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiggins JL, Brotman MA, Adleman NE, et al. , 2016. Neural Correlates of Irritability in Disruptive Mood Dysregulation and Bipolar Disorders. Am J Psychiatry. 173 (7), 722–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.