Abstract
Background:
Alcohol and marijuana/cannabis are frequently used simultaneously (i.e., SAM use). SAM use is complex and the ways in which alcohol and cannabis are simultaneously used may reveal differential effects. The purpose of this study was to examine day-level effects of distinct alcohol and cannabis product combinations on simultaneous use and consequences on that day.
Methods:
College student SAM users (N=274; 50% women; Mage =19.82 years) were recruited to complete 54 days of data collection, including five repeated daily surveys each day. We identified 12 distinct product combinations reported during SAM-use days. We tested four reference groups, with one reflecting the most common use pattern and three potentially risky use patterns. We considered three outcomes (negative consequences, number of drinks, and number of cannabis uses) and used generalized linear mixed-effects models disentangling within- from between-person effects in all analyses.
Results:
Using multiple products (≥ 2) of alcohol was consistently linked to higher odds of experiencing a negative consequence. Combining beer with only one cannabis product (leaf or concentrate) was consistently associated with lower odds of a consequence. Combining cannabis with multiple alcohol products was associated with heavier alcohol consumption. Using dual cannabis products also was associated with heavier cannabis consumption, but this pattern was not significantly different than using concentrate only on a given day.
Conclusion:
This is the first study to examine day-level influences of distinct alcohol and cannabis product combinations on consumption and consequences among young adult SAM users. Findings suggest that mixing alcohol products confers greater risk for negative consequences and heavier consumption, whereas there is little difference in cannabis consumption when using concentrate only vs. two cannabis products on a given day, except for concentrate + beer. Our findings support existing protective strategies of not mixing alcohol products and avoiding use of cannabis concentrate for SAM use as well.
Keywords: daily diary, experience sampling methods, alcohol products, cannabis products, simultaneous use
Introduction
Co-use of alcohol and cannabis is common (Metrik et al., 2018; Subbaraman and Kerr, 2020, 2015; Terry-McElrath and Patrick, 2018; Yurasek et al., 2017), particularly among college students (O’Hara, Armeli, & Tennen, 2016; White et al., 2019). Most alcohol and cannabis co-users have used these two substances simultaneously so that their effects overlapped (i.e., simultaneous alcohol and marijuana [SAM] use), which is problematic (Barrett, Darredeau, & Pihl, 2006; Martin, Clifford, & Clapper, 1992; Sokolovsky, Gunn, Micalizzi, White, & Jackson, 2020; Subbaraman & Kerr, 2015; White et al., 2019). Indeed, decades of research have shown that simultaneous use is particularly risky, relative to co-use and mono-substance use (Bailey et al., 2019; Earleywine and Newcomb, 1997; Li et al., 2013; Martin, 2008). For example, laboratory administration studies have shown that combining alcohol with cannabis results in the greatest impairment levels on most performance tasks and in higher subjective intoxication ratings, compared to participants administered alcohol or cannabis alone (e.g., Chait and Perry, 1994a; Downey et al., 2013; Hartman et al., 2016, 2015; Lukas et al., 1992; Lukas and Orozco, 2001; Perez-Reyes et al., 1988). Additive and/or synergistic effects have also been supported by self-report data from SAM users (Lee et al., 2017). See Yurasek et al. (2017), for a review of effects of combining alcohol and cannabis.
Compared to co-users who do not use both substances together or mono-substance users, SAM users have reported higher levels of consumption (Brière et al., 2011; Gunn et al., 2018; Linden-Carmichael et al., 2019; Metrik et al., 2018; Subbaraman and Kerr, 2015) and more negative consequences (Brière et al., 2011; Jackson et al., 2020; Midanik et al., 2007; Subbaraman and Kerr, 2015; Yurasek et al., 2017). In particular, SAM users were shown to be more likely to endorse nine types of consequences, relative to alcohol-only users, with the strongest effects observed for more acute consequences (e.g., blackouts; Jackson et al., 2020). Likewise, SAM users engage in riskier driving and perceive driving under the influence to be safer than co-users and mono-substance users (Duckworth and Lee, 2019). Increased incidences of motor vehicle accidents were also observed for SAM users (Arterberry et al., 2017; Chihuri et al., 2017; Dubois et al., 2015; Li et al., 2017), which is particularly concerning considering the impact on public health. Overall, it is clear SAM use is consequential; however, it is also complex, as the manner in which alcohol and cannabis are used is evolving, and each substance can be used in a number of different ways (e.g., forms, types). The manner of SAM use on a given day may confer greater (or fewer) risks for use and consequences and understanding these differences could inform harm-reduction approaches.
Extant research has shown that the ways in which alcohol is consumed can influence use and consequences, and this notion is currently reflected in protective behavioral strategies for alcohol use (Martens et al., 2007, 2005). In fact, strategies related to manner of drinking (e.g., avoid taking shots, avoid mixing types of alcohol) are robustly related to reduced drinking and negative consequences at both between- and within-person levels (Linden-Carmichael et al., 2018; Martens et al., 2007; Napper et al., 2014; Pearson et al., 2013). These consistent findings underscore the importance of understanding manners of drinking beyond quantity and frequency, particularly considering that some protective behavioral strategies, such as stopping/limiting drinking, have demonstrated equivocal relations to alcohol-related outcomes (see Pearson, 2013). Similar harm-reduction strategies exist for manner of cannabis use, including avoiding mixing with alcohol and avoiding cannabis concentrates (Pedersen et al., 2017). Thus, some manners of SAM use may lead to more negative outcomes than others, and this may depend on the use of a specific product (e.g., liquor vs. beer) and/or the use of multiple products.
A body of work has examined alcoholic beverage preferences (wine vs. beer vs. liquor) and their relations to various outcomes, including drinking patterns (e.g., Dey et al., 2014; Mochrie et al., 2019), heavy drinking and severity of dependence (e.g., Baltieri et al., 2009; Flensborg-Madsen et al., 2008; Jensen et al., 2002), frequency of driving under the influence (DUI) and risk perception of driving after drinking (Greenfield and Rogers, 1999), and morbidity/mortality (e.g., Chou et al., 1998; Klatsky et al., 2003), with a general conclusion that liquor consumption, compared to beer or wine consumption, is more strongly related to negative consequences, severity of dependence, treatment nonadherence, and severe medical consequences. Some evidence also indicates that individuals consume certain alcohol products for specific reasons (e.g., consuming wine with meals; Callinan and MacLean, 2016; Kuntsche et al., 2006), suggesting within-person variability in alcohol product use.
Comparatively little work has examined how specific cannabis products influence outcomes, with some evidence that using multiple cannabis products (Gunn et al., 2020) or being a concentrate (vs. non-concentrate) user (Bidwell, YorkWilliams, Mueller, Bryan, & Hutchison, 2018) is associated with a greater number of consequences. Some cannabis products may also have greater potential for negative outcomes than others. For example, concentrates often contain very high dosages of delta-9-tetrahydrocannabinol (THC; Chan et al., 2017; Meacham, Paul, & Ramo, 2018; Meier, 2017), and as a result, harm-reduction approaches recommend against their use (Pedersen et al., 2017). That said, recent work has shown that regular concentrate users do not experience greater subjective intoxication or impairment from cannabis concentrate use than regular leaf users experience from their use of cannabis flower (Bidwell et al., 2020), which suggests that cannabis concentrate use itself may not be more problematic than leaf use but instead differences may depend on the regularity of using any one cannabis product. Another example of cannabis product differences is that ingesting (vs. inhaling) cannabis results in delayed onset of the drug’s effect, and edible users may consume more than intended during this latency period and subsequently experience severe nausea, vomiting, and paranoia (Barrus et al., 2016; Freeman and Lorenzetti, 2019). However, the effects of alcohol products in combination with cannabis products (and vice versa) on use and consequences remain unknown. Further, evidence regarding these products to date is limited to the between-person level, and we are unable to extrapolate the effects of using a given product on a given day from this work. Understanding SAM use at this nuanced level may reveal differential effects of certain products or product combinations to inform harm-reduction strategies for SAM use and improve our prediction of use and consequences more broadly.
Present Study
The purpose of the present study was to examine the day-level effects of distinct alcohol and cannabis product combinations on consumption and consequences on that day. We analyzed data from a larger multi-site parent study of college student SAM users that included five repeated daily surveys (RDS) spanning 54 days of assessment. To facilitate comparisons across product combinations, we selected two primary reference groups: (1) leaf + beer (most common) and (2) 2 cannabis + ≥ 2 alcohol products (hypothesized most risky pattern). Regarding the latter combination, we hypothesized this to be the riskiest use pattern, relative to other patterns, on a given day, given research has documented the consequences of using multiple cannabis products (Gunn et al., 2020) and of using multiple alcohol products (Martens et al., 2007, 2005); thus, we presumed using multiple products of both substances on a given day would be the most problematic for consumption and consequences, though no prior work has tested this notion. To further disentangle the effects of using more than one product alongside the most potent forms of each substance (i.e., liquor, concentrate), we then explored two additional reference groups: liquor + 2 cannabis products and concentrate + ≥ 2 alcohol products. In general, we hypothesized that using multiple alcohol and/or two cannabis products would result in greater consumption and higher odds of experiencing negative consequences. Specific comparisons of each product combination are considered exploratory, given no work has examined alcohol and cannabis product usage at the daily level, particularly when used simultaneously.
Materials and Methods
Design and Sample
Screening survey.
Full-time students (ages 18–24) were recruited from three state universities in states with varying recreational cannabis laws (i.e., recreational cannabis illegal, recreational cannabis decriminalized, and recreational cannabis legal for adults 21 and older) to participate in a larger parent study on SAM use. Eight thousand students were randomly chosen from each university’s registrar database stratified by expected year of graduation (total N=24,000) and were emailed an invitation to participate in an online screening survey. Screening completers (N=7,000) included more women, more White students, fewer Black students, more Asian students, more Hispanic/Latinx students, and more younger students (i.e., ages 18–21) than those invited; effect sizes for these differences were small (Cohen’s h=.07-.26). Of those screened, 2,874 (41.1%) were considered eligible to participate based on age, being enrolled in college full-time, and endorsing past-year alcohol and cannabis use. Students who completed the screening survey were eligible for several lotteries to win $100. See White et al. (2019) and Stevens et al. (2020; Supplemental Materials) for further details regarding screening for the parent study.
Baseline survey.
Of students eligible for the larger parent study, a random sample of 2,501 students stratified by university and over-sampled for past-month alcohol and cannabis use was invited via email to participate in the parent study’s baseline survey; 1,524 (60.9%) of invitees completed the baseline survey. We retained 1,390 (91.2%) of these students in the analyses after excluding participants who provided responses inconsistent with baseline survey eligibility criteria (see above) or whose surveys had technological problems. See White et al. (2019) and Stevens et al. (2020; Supplemental Materials) for further details regarding the baseline survey.
Daily survey.
Of students who completed the baseline survey, 693 used alcohol and cannabis at the same time ‘so that their effects overlapped’ (i.e., SAM use) within the past month, which made them eligible to participant in the daily phase of the parent study. Of these, 596 were invited to participate in the daily survey. (The other 97 were not invited due to a pre-established quota.) For daily survey recruitment, we stratified based on frequency of past-month SAM use and assigned sex to ensure roughly equal numbers of men and women and to oversample frequent SAM users. (Enrollment was on a rolling basis until quotas were filled, and therefore, not all of those invited were enrolled in the daily phase.) Data collection for this phase directly followed the longer surveys (baseline and three-month follow-up) and comprised 28 days of RDS at each burst (56 total days) prompted at 9:00 am, 2:00 pm, 5:00 pm, 8:00 pm, and 11:00 pm using a custom smartphone application (see Stevens et al., 2020 for details). At the 9:00 am survey, students were also asked additional retrospective questions assessing yesterday’s behavior through bedtime. Participants were provided four hours to complete the 9:00 am survey and two hours to complete the 2:00 pm, 5:00 pm, 8:00 pm, and 11:00 pm surveys. Reminders were provided to participants 15 minutes before the survey closed. See Stevens et al. (2020) for additional details regarding the parent study’s daily phase. See also Sokolovsky et al. (2020) for a flow chart of data collection for the parent study summarized above.
The daily phase included 343 participants. We retained data from 54 study days due to technical difficulties that occurred during the first two study days. Given two participants only completed the first two study days, our final daily sample comprised 341 students and were distributed approximately equally across schools (53% women; M age = 19.79; 74% White; 10% Hispanic/Latinx). Participants were compensated $25 for the baseline survey, $35 for the follow-up survey, and $1 for each completed daily survey, with weekly and overall bonuses for higher compliance rates. Aggregated across the five recurring daily surveys (RDS), mean RDS compliance equaled 88.4%, and mean morning survey compliance equaled 81.9%. Both compliance rates exceed the pooled compliance rate shown in a recent meta-analysis on EMA and substance use (Jones et al., 2019). As a part of the parent study, all participants were trained on standardized drink equivalences set forth by the National Institute of Alcoholism and Alcohol Abuse (NIAAA; National Institute on Alcohol Abuse and Alcoholism, 2007). All procedures were approved by the coordinating university’s Institutional Review Board. A Certificate of Confidentiality was obtained from the National Institute on Drug Abuse.
Measures
Demographics.
Participants self-reported demographic information at the baseline survey, including age, sex assigned at birth, race, and ethnicity.
Alcohol Products.
At each RDS following endorsement of alcohol use, participants were asked, “What type of alcohol had you been drinking between X and Y?” Options included ‘beer’ (coded into no/yes), ‘wine’ (no/yes), ‘liquor’ (no/yes), and ‘beer alternative’ (no/yes). For the purposes of the present study, beer and beer alternative were collapsed into a single category.
Cannabis Products.
At each RDS survey following endorsement of cannabis use, participants were asked, “In what form was the marijuana you used between X and Y?” Options included ‘dry leaf’ (no/yes), ‘concentrate’ (no/yes) and ‘edible’ (no/yes).
Alcohol Quantity.
Participants indicated the number of drinks consumed since their last RDS using a graphical interface, tapping the screen for each drink consumed (see Stevens et al., 2020, Supplemental Materials, for screenshots): “Tap your finger in the blue box each time you had a drink at the corresponding time.” The sum of drinks reported at each RDS determined the total number of drinks reported on that day. In the parent study, if a participant missed one RDS, they reported on their alcohol consumption since their last completed survey, such that information from one missed RDS was captured at the next RDS. If two RDS were missed on a given day, participants reported on their alcohol consumption for the current survey and the immediate prior survey, which resulted in only one missed survey for that day (see Stevens et al., 2020, Supplemental Materials, for details). See Analytic Strategy for missing data estimation.
Cannabis Use.
Using this same graphical interface, participants also indicated their number of cannabis uses since their last RDS, tapping the screen for each use occasion: “Tap your finger in the blue box each time you used marijuana at the corresponding time.” The sum of cannabis use occasions reported at each RDS determined the total number of uses reported on that day. As with alcohol use, if a participant missed one RDS, they reported on their cannabis consumption since their last completed survey. If two RDS were missed on a given day, participants reported on their cannabis consumption for the current survey and the immediate prior survey, which resulted in only one missed survey for that day (see Stevens et al., 2020, Supplemental Materials, for details).
Negative consequences.
Participants reporting any SAM use the prior day (either on a prior-day RDS or on the 9:00 am report asking about yesterday’s behavior) were then asked on the 9:00 am report: “Which of the following things happened to you because of yesterday’s use of alcohol and marijuana together”: “hangover” (19% of SAM daily observations), “nauseous or vomited” (7%), “injured self” (1%), “drove car high” (7%), “had a blackout” (4%), “rude or aggressive” (1%), and “unwanted sex” (0.50%). Given items were administered via mobile phones, consequence items were necessarily brief. We selected this set of acute consequences from several validated measures administered in the parent study, including the Brief Young Adult Alcohol Consequence Questionnaire (Kahler et al., 2005), Brief Marijuana Consequences Questionnaire (Simons et al., 2012), Young Adult Alcohol Consequences Questionnaire (Read et al., 2006), Rutgers Alcohol Problem Index (White & Labouvie, 1989), and the Rutgers Marijuana Problem Index (White, Labouvie, & Papadaratsakis, 2005). For the present study, we examined any endorsement of the above negative consequences (yes = 31% of SAM days; no = 69%).
Covariates.
In addition to adjusting for demographic information (i.e., age [continuous], sex [male vs. female], school [recruitment site; School A, illegal and School B, decriminalized vs. School C, legal]), we covaried for weekend (i.e., Friday and Saturday vs. weekday [Sunday-Thursday]), any other drug use (“Did you use any drugs other than marijuana between X and Y?”; yes vs. no)1, as well as average number of drinks across the study and average number of cannabis uses across the study in all models.
Analytic Strategy
Data management and analyses were conducted in SAS 9.4™ software (SAS Institute Inc., 2012). Following recommendations by Nakagawa et al. (2017), we used the ‘performance’ package in R to calculate the conditional R2 value (i.e., the proportion of variance explained by both fixed and random effects) for each model (R Core Team, 2020). For the present investigation, we aggregated all RDS to the daily level to match the level of analysis of consequences (assessed once daily). Individual product frequencies indicated edible use on SAM days was low (97 of 2,024 observations; 5% of days), which resulted in very low counts when parsed by product combination with alcohol on a given day.2 Thus, all analyses were restricted to SAM days, excluding those involving edibles resulting in 1,927 observations, and included 274 participants who endorsed at least one SAM-use occasion across the 54 study days (50% women; M age = 19.82; 75% White, 11% Asian, 8% bi- or multi-racial, 3% Black, 0.2% Pacific Islander, 2% other race; 8% Hispanic/Latinx). On average, students consumed five drinks (SD = 4.49) and used cannabis five times3 (SD = 6.24) on each SAM day; other drug use was minimal (9% of observations; see footnote 1).
We first examined the endorsement of each possible alcohol and cannabis product combination, with three products for alcohol and two for cannabis, for a total of 21 possible combinations (see Table 1 for raw combinations). Prior to analysis, we collapsed these categories into 12 unique combinations while maintaining the same set of combination categories for each product (see Table 1, collapsed combinations), which were used in subsequent analyses. We then selected two primary reference groups by which to compare these distinct combinations: leaf + beer (most common; 22% of SAM days) and 2 cannabis + ≥ 2 alcohol products (potentially most risky pattern; 4% of SAM days). To further discern possible differential effects of liquor and cannabis concentrate, which are the most concentrated and potentially most problematic products for their substance, we also explored the following two reference groups: concentrate + ≥ 2 alcohol products (6% of SAM days) and liquor + 2 cannabis products (3% of SAM days).
Table 1.
Alcohol and cannabis product combination types
| Collapsed Combinations | N participants (%) | n observations (%) | Raw Combinations | n observations (%) |
|---|---|---|---|---|
| Leaf + Liquor | 154 (56%) | 379 (19.67) | Leaf + Liquor | 379 (19.67) |
| Leaf + Beer | 138 (50%) | 420 (21.80) | Leaf + Beer | 420 (21.80) |
| Leaf + Wine | 77 (28%) | 173 (8.98) | Leaf + Wine | 173 (8.98) |
| Leaf + ≥2 Alcohol | 159 (58%) | 450 (23.35) | Leaf + Liquor + Beer | 290 (15.05) |
| Leaf + Liquor + Wine | 64 (3.32) | |||
| Leaf + Beer + Wine | 53 (2.75) | |||
| Leaf + Liquor + Beer + Wine | 43 (2.23) | |||
| Concentrate + Liquor | 49 (18%) | 67 (3.48) | Concentrate + Liquor | 67 (3.48) |
| Concentrate + Beer | 34 (12%) | 87 (4.51) | Concentrate + Beer | 87 (4.51) |
| Concentrate + Wine | 22 (8%) | 37 (1.92) | Concentrate + Wine | 37 (1.92) |
| Concentrate + ≥ 2 Alcohol | 53 (19%) | 113 (5.86) | Concentrate + Liquor + Beer | 63 (3.27) |
| Concentrate + Liquor + Wine | 20 (1.04) | |||
| Concentrate + Beer + Wine | 17 (0.88) | |||
| Concentrate + Liquor + Beer + Wine | 12 (0.62) | |||
| Liquor + 2 Cannabis | 38 (14%) | 51 (2.65) | Liquor + Leaf + Concentrate | 51 (2.65) |
| Beer + 2 Cannabis | 32 (12%) | 57 (2.96) | Beer + Leaf + Concentrate | 57 (2.96) |
| Wine + 2 Cannabis | 8 (3%) | 12 (0.62) | Wine+ Leaf + Concentrate | 12 (0.62) |
| 2 Cannabis + ≥ 2 Alcohol | 52 (19%) | 81 (4.20) | Liquor + Beer + Leaf + Concentrate | 58 (3.01) |
| Liquor + Wine + Leaf + Concentrate | 13 (0.67) | |||
| Beer + Wine + Leaf + Concentrate | 5 (0.26) | |||
| Liquor + Beer + Wine + Leaf + Concentrate | 5 (0.26) |
Note. N participants = 274; n daily observations = 1,927 (excluding days involving edible use only due to low endorsement).
To determine the unique effects of each combination on a given day on consumption and consequences, we conducted a series of generalized linear mixed-effects models (GLMMs) using SAS PROC GLIMMIX and Laplace approximation for missing data. GLMMs, an extension of multilevel modeling, are necessary to account for clustering that is inherent for nested data that would violate the assumption of independent errors in ordinary least squares regression (Curran and Bauer, 2011; Hox et al., 2017; Raudenbush and Bryk, 2002; Singer, 1998). For each reference group, we analyzed three outcomes, which were not normally distributed: (1) any negative consequence (binomial distribution), (2) number of drinks (count; negative binomial distribution), and (3) number of cannabis uses (count; negative binomial distribution). To isolate the within-person effect of each product combination, we included in all models the proportion of study days on which each alcohol and cannabis product was used. We also adjusted for the following covariates in all models: age, sex (female=reference group), school (School C=reference group), day of the week (weekday as the reference), other drug use (reference = no), as well as the average number of drinks and cannabis uses across the study. Finally, given potential concerns related to multiple testing, we used a Bonferroni corrected p-value for 12 models (i.e., four reference groups X three outcomes), with a corrected alpha = 0.004. Only findings that are significant with this corrected alpha are interpreted and discussed.
Results
Full model effects with covariate estimates are presented in Supplemental Tables S1–S4. Without covariates, product combinations explained 28% of the variance in the consequence outcome, 35% of the alcohol consumption outcome, and 55% of the cannabis consumption outcome.
Leaf + Beer
Using leaf and multiple alcohol products, concentrate and multiple alcohol products, or dual cannabis products and multiple alcohol products had significantly greater odds of experiencing a negative consequence after adjusting for covariates, relative to using leaf + beer on that day (see Figure 1A). Using leaf + liquor, concentrate + liquor, liquor + 2 cannabis products, or multiple alcohol products, including when combined with dual cannabis products, resulted in a greater number of drinks consumed, relative to using leaf + beer on that day, after adjusting for covariates (see Figure 1B). Most concentrate combinations, except for concentrate + wine, and all combinations involving dual cannabis products, including when combined with multiple alcohol products, resulted in a greater rate of cannabis use, relative to using leaf + beer on that day, after adjusting for covariates (see Figure 1C).
Figure 1:
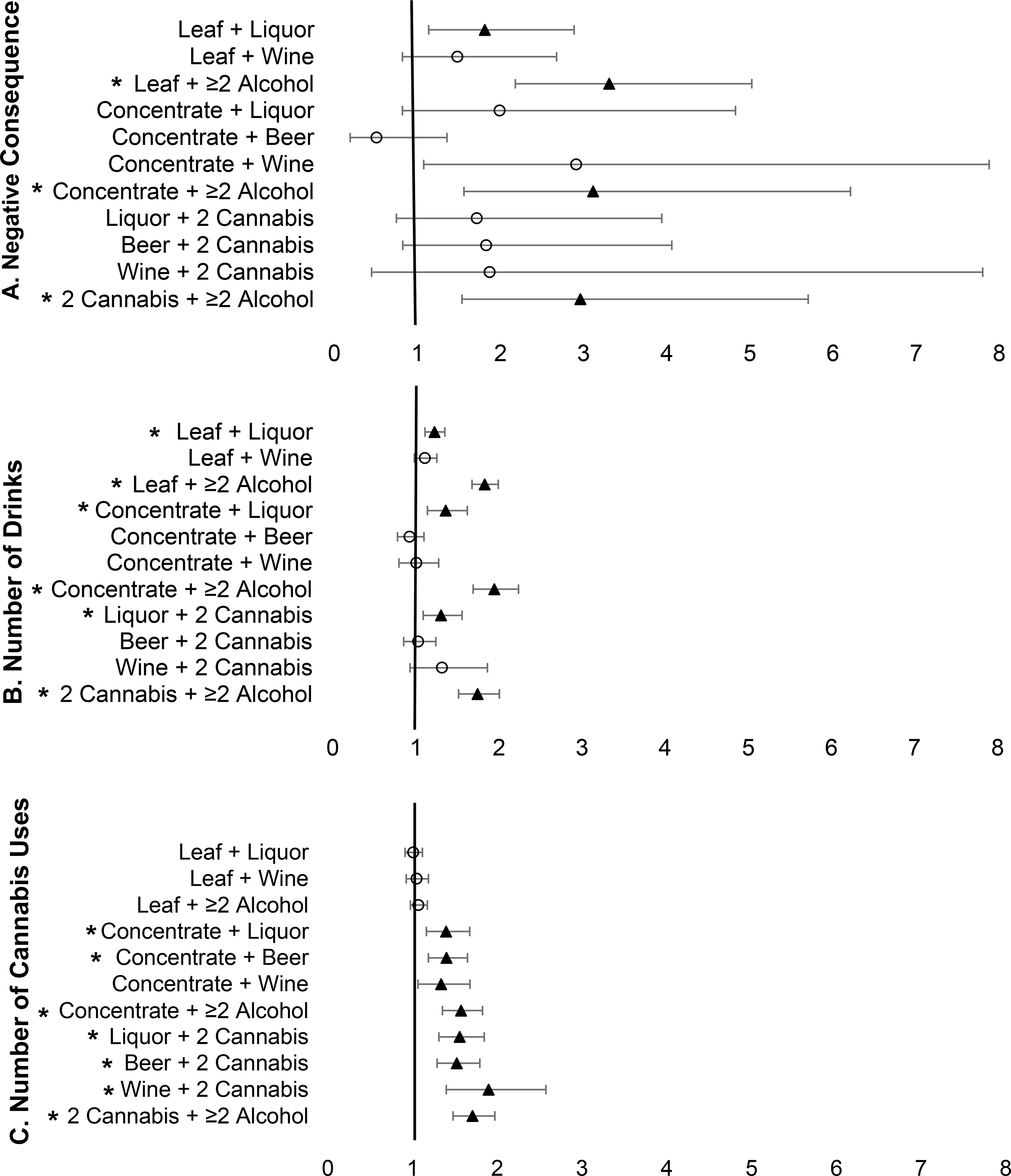
Forest plot of product combination effects relative to using leaf + beer.
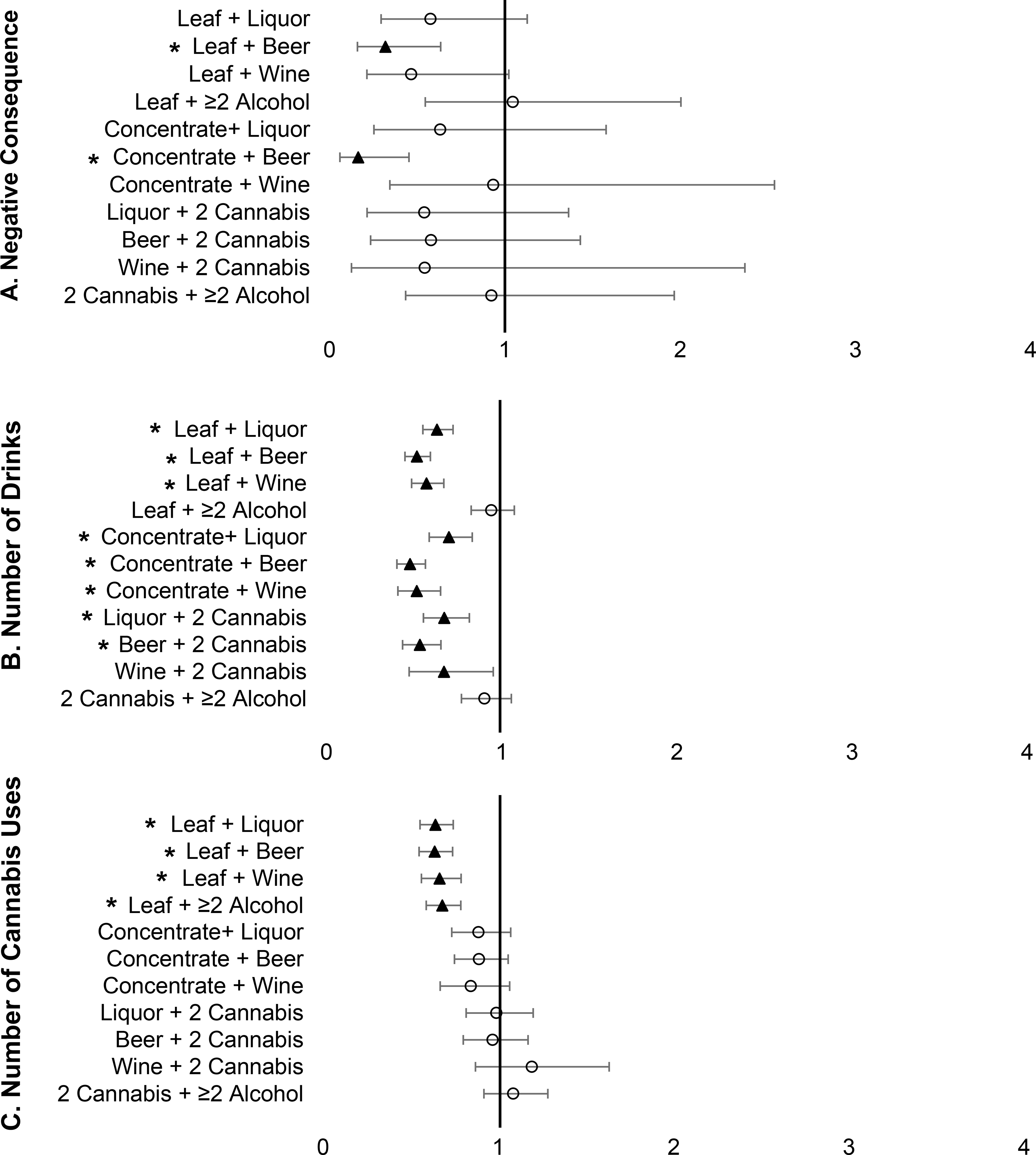
2 Cannabis + ≥ 2 Alcohol Products
Relative to using 2 cannabis + ≥ 2 alcohol products on that day, concentrate + beer and leaf + beer exhibited significantly lower odds of a negative consequence after adjusting for covariates (see Figure 2A). All leaf combinations (except for leaf + ≥ 2 alcohol products), concentrate + beer, concentrate + wine, liquor + 2 cannabis products, and beer + 2 cannabis products had lower rates of drinking after adjusting for covariates, relative to using multiple products of both alcohol and cannabis on that day (see Figure 2B). All leaf combinations had lower rates of cannabis use after adjusting for covariates, relative to using dual cannabis products and multiple alcohol products on that day (see Figure 2C).
Figure 2:

Forest plot of product combination effects relative to using 2 cannabis + ≥ 2 alcohol products.
Concentrate + ≥ 2 Alcohol Products
Only concentrate + beer and leaf + beer had significantly lower odds of experiencing a negative consequence after adjusting for covariates, relative to using concentrate combined with multiple alcohol products on that day (see Figure 3A). All leaf combinations (except for leaf + ≥ 2 alcohol products), all concentrate combinations, liquor + 2 cannabis products, and beer + 2 cannabis products had lower drinking rates, relative to using concentrate combined with multiple alcohol products on that day, after adjusting for covariates (see Figure 3B). All leaf combinations had lower rates of cannabis use, relative to using concentrate and multiple alcohol products on that day, after adjusting for covariates (see Figure 3C).
Figure 3:
Forest plot of product combination effects relative to using concentrate + ≥ 2 alcohol products.
Liquor + 2 Cannabis Products
No combination was significantly different from using liquor + 2 cannabis products on a given day for negative consequences after adjusting for covariates (see Figure 4A). Leaf + ≥ 2 alcohol products, concentrate + beer, concentrate + ≥ 2 alcohol products, and using dual cannabis products and multiple alcohol products were significantly different from using liquor + 2 cannabis products on a given day for rate of drinking. Aside from concentrate + beer, these combinations resulted in significantly greater rates of drinking after adjusting for covariates. By contrast, concentrate + beer resulted in significantly lower rates of drinking (see Figure 4B). All leaf combinations had significantly lower rates of cannabis use, relative to using liquor + 2 cannabis products on that day (see Figure 4C).
Figure 4:
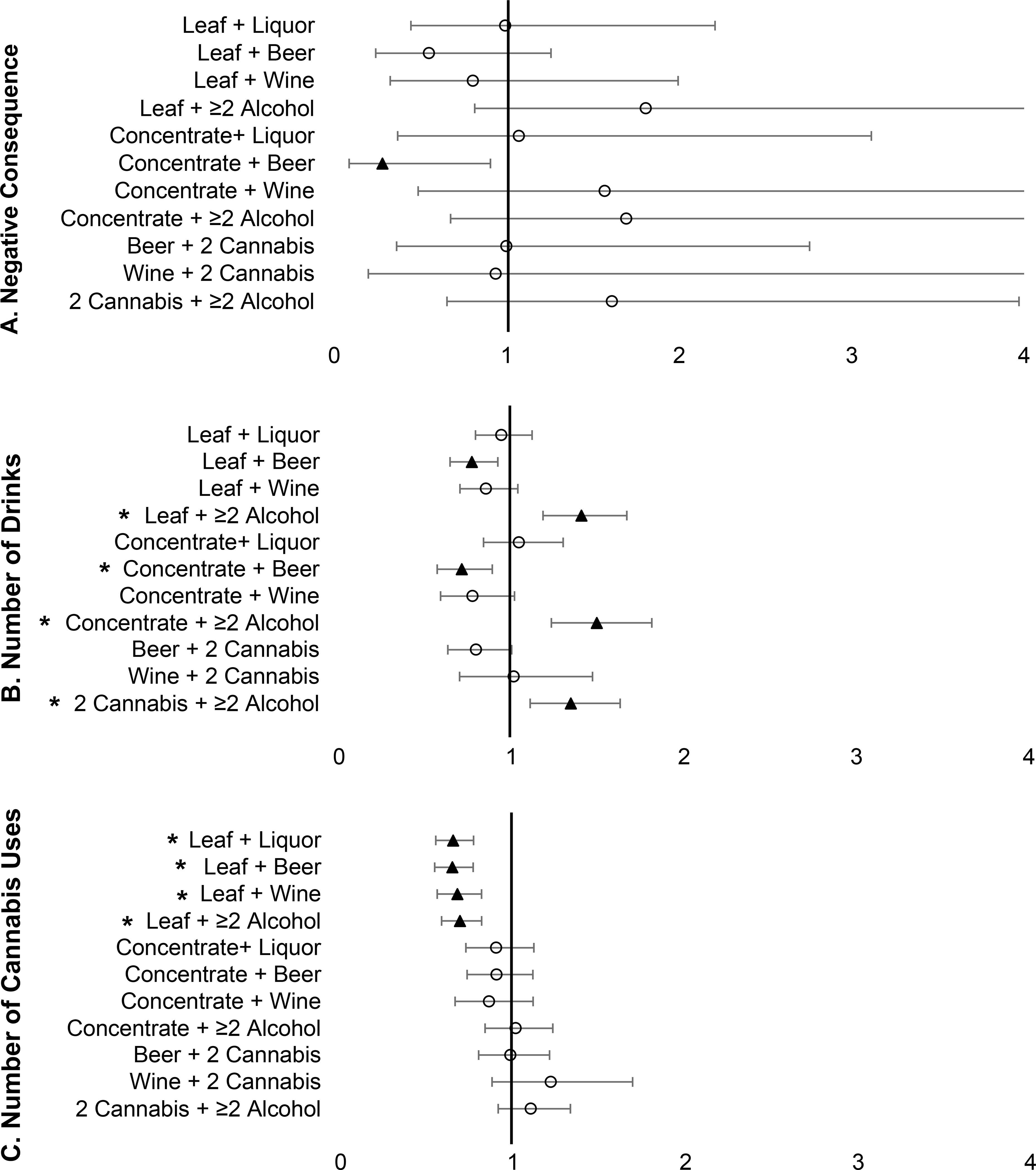
Forest plot of product combination effects relative to using liquor + 2 cannabis products.
Discussion
The present study characterized distinct day-level alcohol and cannabis product combinations and examined their influences on consumption and consequences in a sample of young adult SAM users. Notably, our effects represent using a given product combination on a given day, after accounting for typical product use and consumption across the assessment period for a given individual. This disaggregation of within- and between-person effects provides useful information about the day-level effects of each combination relative to the four tested reference group combinations. These effects are discussed in the context of the larger literature below.
Consequences
Importantly, endorsement of some negative consequences following SAM days was low, and overall, participants endorsed a negative consequence on one-third of the study days (31%). Nonetheless, negative consequences were more likely on days when multiple alcohol products were used, especially compared to the most prevalent category of using leaf + beer. By contrast, negative consequences were not more likely on days when dual cannabis products were used, relative to leaf only + beer. A non-trivial proportion of SAM days involved consuming two cannabis products alongside multiple alcohol products on the same day, which we hypothesized would be the most problematic combination. Yet, combinations involving multiple alcohol products or two cannabis products were equally risky for experiencing negative consequences, relative to the presumed most problematic category (multiple products of both substances). In fact, only using leaf + beer or concentrate + beer evinced significantly lower odds of a negative consequence, relative to using two cannabis products and multiple alcohol products on a given day; no other product combination was significantly different from this multiple-product (of both substances) group.
We explored two comparisons to discern whether there was an increase in consequences associated with a concentrated product (i.e., liquor, cannabis concentrate) when combined with multiple products of the other substance. There were higher odds of experiencing a consequence when using concentrate with multiple alcohol products when compared to leaf + beer and concentrate + beer, but not relative to any other combinations. However, when compared to using two cannabis products with liquor on a given day, no product combination was significantly different regarding the odds of experiencing a negative consequence. Overall, we did not find support for specific concentrated products increasing the odds of a negative consequence; indeed, our most consistent finding was for using multiple alcohol products and negative consequences.
Consumption
Not surprisingly, most single-product combinations resulted in reduced rates of consumption relative to using multiple products on a given day.
Alcohol.
For alcohol consumption, using multiple products of alcohol and two cannabis products on that day was associated with greater consumption compared to all leaf combinations with one alcohol product, concentrate + beer, concentrate + wine, and liquor or beer paired with two cannabis products. Comparisons between concentrate with multiple alcohol products and leaf with multiple alcohol products were not significantly different, suggesting little influence of the cannabis product on alcohol consumption on a given day when combined with multiple alcohol products. Together, these findings highlight that consuming multiple alcohol products on a given day is linked to greater alcohol consumption, rather than any specific alcohol product. At the same time, the combinations of leaf + liquor, concentrate + liquor, and liquor + 2 cannabis products resulted in greater alcohol consumption compared to the most common combination (leaf + beer); thus, liquor may increase quantity consumed above and beyond beer or wine.
Cannabis.
For cannabis consumption, use of two cannabis products and most concentrate combinations each resulted in greater cannabis consumption on that day, especially when compared to consuming leaf + beer. Interestingly, no combination involving cannabis concentrate was significantly different from using two cannabis products on a given day, which emphasizes that cannabis concentrate use may be particularly linked to greater consumption, relative to leaf combinations on a given day. Notably, this is counter to the parallel comparisons with alcohol, where evidence shows that consuming multiple alcohol products on a given day (vs. liquor only) is linked to significantly more consumption.
Implications for Harm Reduction
The comparisons described above demonstrate the effects of using multiple products on consequences and consumption of that substance, as well as provide preliminary empirical support for existing harm-reduction techniques recommending against multiple product use (Martens et al., 2007, 2005). Though speculative, individuals might be more open to altering their specific product usage than their quantity and subsequent subjective effects; this notion should be explored in future research. For example, consuming multiple alcohol products was consistently linked to greater odds of having a negative consequence. “Avoid mixing different types of alcohol” is a recommended protective behavioral strategy related to manner of drinking (Martens et al., 2007, 2005), and our findings support that mixing alcohol products, on a given day for a given person, is linked to negative consequences and heavier consumption. Though these strategies have been recommended for the past two decades, we are the first, to our knowledge, to demonstrate the possible daily-level adverse effects of using multiple alcohol products. Our comparisons also showed that using liquor was not consistently related to heavier alcohol consumption or to greater odds of experiencing a consequence than using multiple alcohol products on that day. Nonetheless, the overwhelming majority of days using multiple alcohol products included liquor as one of those products. It is important to acknowledge that the consequence items included in the present study were heavily weighted toward alcohol-specific consequences, which may also explain the relation between using multiple alcohol products and consequences. More research is needed to determine the replicability of these findings in a sample that assesses more cannabis-specific (e.g., paranoia, lethargy) and SAM-specific consequences, though, to our knowledge, the latter have yet to be identified.
Protective behavioral strategies for cannabis use currently recommend against consuming concentrate (Pedersen et al., 2017, 2016), and our findings support this recommendation, with higher consumption levels of cannabis being linked, in part, to concentrate use in this sample. On the other hand, recent research has shown that regular concentrate users do not report greater impairment or subjective intoxication compared to regular leaf users (Bidwell et al., 2020); thus, it is difficult to determine whether the heavier consumption linked to concentrate use is problematic or due to cannabis tolerance. Though we found greater cannabis consumption on days where two cannabis products were used, we did not find that using concentrate and leaf on a given day, compared to using only concentrate, led a greater chance of experiencing a negative consequence. As indicated above, this may be an artifact of the data, such that the consequence items included in the present study did not contain cannabis-specific consequences, and more research is needed to discern whether the differential effect of multiple alcohol products (but not two cannabis products) on consequences is replicable.
Avoiding the consumption of two vs. one cannabis products on a given day is not currently reflected as a harm-reduction strategy for cannabis use. Consistent with limited prior work from our research group (Gunn et al., 2020), our findings suggest that aiming to reduce the number of cannabis products used on a given day could be beneficial in reducing the amount of cannabis consumed, although not necessarily protective against the set of acute consequences we examined here. Overall, we supported existing literature documenting harms associated with cannabis concentrate use (Bidwell et al., 2018; Meacham et al., 2018; Meier, 2017; Stogner and Miller, 2015), with one notable exception (i.e., concentrate + beer), and provided novel findings detailing the daily-level effects of using multiple alcohol and/or cannabis products, which supports strategies reflected in current harm-reduction approaches for alcohol and cannabis.
Limitations
Despite the strengths of the present study, findings should be interpreted considering limitations. First, data were limited to college students and the majority were White, which limits generalizability to non-college and non-White young adults. Second, the RDS used as part of the larger parent study did not capture behavior in real-time; thus, all reports required a small degree of retrospection, with more retrospection required on a given RDS if the immediately prior survey was missed and collected at the next report. Third, the assessment of cannabis use is complex, and because we lack a standardized metric of cannabis use akin to standardized drink equivalencies for alcohol use, gauging the degree of real-world exposure to psychoactive compounds such as THC remains difficult. For this reason, in the larger parent study, participants were asked to self-define a cannabis use occasion. We believe this limitation is mitigated by our focus on within-person effects that would not be influenced by differences in self-defining cannabis use occasions across individuals. Fourth, the consequence outcome was zero-inflated; thus, we constructed a binary outcome, which obscured any specific relations between product combinations and the number of consequences or specific types of consequences. Fifth, the consequence outcome was heavily weighted toward alcohol-related negative consequences (e.g., hangover), which limits the degree to which our findings can inform effects of alcohol and cannabis product combinations on more cannabis-specific consequences (e.g., paranoia, lethargy). Finally, we did not discern between mixed drinks vs. taking shots, which may have implications for outcomes associated with liquor consumption.
Future Directions
Given the novelty of the present work, findings should be considered preliminary, and future work is needed to examine the replicability of these findings before firm conclusions are drawn. Likewise, to advance our findings, future research should examine the day-level effects of these specific product combinations on negative consequences that are more specific to cannabis and/or SAM use. To further explore the effects of specific product combinations, it would be useful to compare these day-level product patterns in individuals categorized by their cannabis product of choice (e.g., regular leaf users, regular concentrate users) to determine whether day-level effects of a given combination are attenuated or amplified by potential tolerance developed to a given cannabis product. We also recommend that future studies with greater endorsement of individual consequences examine possible specificity between certain product combinations and specific consequences to further inform harm-reduction approaches. Though beyond the scope of the present work, evidence suggests that drinking motives relate to specific beverage preferences (Kuntsche et al., 2006), and the surrounding context may place constraints on products used (e.g., being restricted to products used at a party or informal gathering vs. being at a bar/restaurant). Future research may consider alcohol and cannabis motives, contexts, and availability as precursors to various manners of drinking, including product combinations, which could provide further nuance for interventions targeting reasons for use. Overall, more research regarding the various manners of SAM use at the event-level (e.g., products, modes, rate of consumption, ordering; e.g., Gunn et al., in press) is needed to determine whether these differ on SAM-use occasions (vs. co-use occasions and mono-substance use occasions); if so, protective behavioral strategies specific to SAM use are needed.
Supplementary Material
Acknowledgments
This was worked supported by the National Institute on Drug Abuse (R01 DA040880, MPIs: Jackson and White; T32 DA016184, PI: Rohsenow; K08 DA048137, PI: Sokolovsky; K01DA039311, PI: Aston), the National Institute on Alcohol Abuse and Alcoholism (K23 AA024808, PI: Treloar, K08AA027551, PI: Gunn), and the National Institute on General Medical Sciences (P20GM130414, PL: Aston).
Footnotes
Of the SAM days analyzed in the present study, two other drug use days (1% of 194 other drug use days) involved “other amphetamines,” 100 other drug use days (52%) involved cocaine, 53 other drug use days (27%) involved Ritalin/Adderall, 3 other drug use days (2%) involved opioids, 11 other drug use days (6%) involved sedatives, 12 other drug use days (6%) involved hallucinogens, 2 other drug use days (1%) involved ecstasy, and 24 other drug use days (12%) involved “other drugs.
The following edible combinations were observed: edible and liquor (13 SAM days; 0.64%), edible and beer (18 SAM days; 0.89%); edible and wine (10 SAM days; 0.49%), and edible and multiple alcohol products (10 SAM days; 0.49%).
Given there are limited documented procedures for standardizing a cannabis use occasion, cannabis use was self-defined in the parent study, such that participants were instructed to tap the graphical interface at each time they used cannabis (see Measures).
References
- Arterberry BJ, Treloar H, McCarthy DM (2017) Empirical profiles of alcohol and marijuana use, drugged driving, and risk perceptions. J Stud Alcohol Drugs 78:889–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey AJ, Farmer EJ, Finn PR (2019) Patterns of polysubstance use and simultaneous co-use in high risk young adults. Drug Alcohol Depend 205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baltieri DA, Daró FR, Ribeiro PL, De Andrade AG (2009) The role of alcoholic beverage preference in the severity of alcohol dependence and adherence to the treatment. Alcohol 43:185–195. [DOI] [PubMed] [Google Scholar]
- Barrett SP, Darredeau C, Pihl RO (2006) Patterns of simultaneous polysubstance use in drug using university students. Hum Psychopharmacol 21:255–263. [DOI] [PubMed] [Google Scholar]
- Barrus DG, Capogrossi KL, Cates SC, Gourdet CK, Peiper NC, Novak SP, Lefever TW, Wiley JL (2016) Tasty THC: Promises and challenges of cannabis edibles., Methods Report (RTI Press). NIH Public Access. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bidwell CL, YorkWilliams SL, Mueller RL, Bryan AD, Hutchison KE (2018) Exploring cannabis concentrates on the legal market: User profiles, product strength, and health-related outcomes. Addict Behav Reports 8:102–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bidwell LC, Bidwell LC, Ellingson JM, Ellingson JM, Karoly HC, Yorkwilliams SL, Hitchcock LN, Tracy BL, Klawitter J, Klawitter J, Sempio C, Bryan AD, Hutchison KE, Hutchison KE (2020) Association of naturalistic administration of cannabis flower and concentrates with intoxication and impairment. JAMA Psychiatry 77:787–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobak M, Room R, Pikhart H, Kubinova R, Malyutina S, Pajak A, Kurilovitch S, Topor R, Nikitin Y, Marmot M (2004) Contribution of drinking patterns to differences in rates of alcohol related problems between three urban populations. J Epidemiol Community Health. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brière FN, Fallu JS, Descheneaux A, Janosz M (2011) Predictors and consequences of simultaneous alcohol and cannabis use in adolescents. Addict Behav 36:785–788. [DOI] [PubMed] [Google Scholar]
- Callinan S, MacLean S (2016) “If I wanna get really drunk I would drink vodka”: drink choices associated with acute intoxication for young Australians. Drugs Educ Prev Policy 23:397–403. [Google Scholar]
- Chan GCK, Hall W, Freeman TP, Ferris J, Kelly AB, Winstock A (2017) User characteristics and effect profile of Butane Hash Oil: An extremely high-potency cannabis concentrate. Drug Alcohol Depend 178:32–38. [DOI] [PubMed] [Google Scholar]
- Chihuri S, Li G, Chen Q (2017) Interaction of marijuana and alcohol on fatal motor vehicle crash risk: a case–control study. Inj Epidemiol 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou SP, Grant BF, Dawson DA (1998) Alcoholic beverage preference and risks of alcohol-related medical consequences: A preliminary report from the national longitudinal alcohol epidemiologic survey. Alcohol Clin Exp Res 22:1450–1455. [DOI] [PubMed] [Google Scholar]
- Curran PJ, Bauer DJ (2011) The disaggregation of within-person and between-person effects in longitudinal models of change. Annu Rev Psychol 62:583–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dey M, Gmel G, Studer J, Dermota P, Mohler-Kuo M (2014) Beverage preferences and associated drinking patterns, consequences and other substance use behaviours. Eur J Public Health 24:496–501. [DOI] [PubMed] [Google Scholar]
- Dubois S, Mullen N, Weaver B, Bédard M (2015) The combined effects of alcohol and cannabis on driving: Impact on crash risk. Forensic Sci Int 248:94–100. [DOI] [PubMed] [Google Scholar]
- Duckworth JC, Lee CM (2019) Associations among simultaneous and co-occurring use of alcohol and marijuana, risky driving, and perceived risk. Addict Behav 96:39–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earleywine M, Newcomb MD (1997) Concurrent versus simultaneous polydrug use: Prevalence, correlates, discriminant validity, and prospective effects on health outcomes. Exp Clin Psychopharmacol 5:353–364. [DOI] [PubMed] [Google Scholar]
- Flensborg-Madsen T, Knop J, Mortensen EL, Becker U, Makhija N, Sher L, Grønbaek M (2008) Beverage preference and risk of alcohol-use disorders: A Danish prospective cohort study. J Stud Alcohol Drugs 69:371–377. [DOI] [PubMed] [Google Scholar]
- Freeman TP, Lorenzetti V (2019) ‘Standard THC units’: a proposal to standardize dose across all cannabis products and methods of administration. Addiction (in press):add.14842. [DOI] [PubMed] [Google Scholar]
- Greenfield TK, Rogers JD (1999) Alcoholic beverage choice, risk perception and self-reported drunk driving: Effects of measurement on risk analysis. Addiction 94:1735–1743. [DOI] [PubMed] [Google Scholar]
- Gunn RL, Aston ER, Sokolovsky AW, White HR, Jackson KM (2020) Complex cannabis use patterns: Associations with cannabis consequences and cannabis use disorder symptomatology. Addict Behav 105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunn RL, Norris AL, Sokolovsky A, Micalizzi L, Merrill JE, Barnett NP (2018) Marijuana use is associated with alcohol use and consequences across the first 2 years of college. Psychol Addict Behav 32:885–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunn RL, Sokolovsky AW, Stevens AK, Metrik J, White HR, Jackson KM (n.d.) Ordering in simultaneous alcohol and marijuana use: Impact on daily consumption and consequences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hox J, Moerbeek M, Schoot R Van de (2017) Multilevel analysis: Techniques and applications, Third Edit. ed. Taylor & Francis. [Google Scholar]
- Jackson KM, Sokolovsky AW, Gunn RL, White HR (2020) Consequences of alcohol and marijuana use among college students: Prevalence rates and attributions to substance-specific versus simultaneous use. Psychol Addict Behav 34:370–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen MK, Andersen AT, Sørensen TIA, Becker U, Thorsen T, Grønbæk M (2002) Alcoholic beverage preference and risk of becoming a heavy drinker. Epidemiology 13:127–132. [DOI] [PubMed] [Google Scholar]
- Jones A, Remmerswaal D, Verveer I, Robinson E, Franken IHAA, Wen CKFF, Field M (2019) Compliance with ecological momentary assessment protocols in substance users: a meta-analysis. Addiction 114:609–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler CW, Strong DR, Read JP (2005) Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: the brief young adult alcohol consequences questionnaire. Alcohol Clin Exp Res 29:1180–1189. [DOI] [PubMed] [Google Scholar]
- Klatsky AL, Friedman GD, Armstrong MA, Kipp H (2003) Wine, liquor, beer, and mortality. Am J Epidemiol 158:585–595. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R (2006) “I drink spirits to get drunk and block out my problems...” beverage preference, drinking motives and alcohol use in adolescence. Alcohol Alcohol 41:566–573. [DOI] [PubMed] [Google Scholar]
- Li G, Brady JE, Chen Q (2013) Drug use and fatal motor vehicle crashes: A case-control study. Accid Anal Prev 60:205–210. [DOI] [PubMed] [Google Scholar]
- Li G, Chihuri S, Brady JE (2017) Role of alcohol and marijuana use in the initiation of fatal two-vehicle crashes. Ann Epidemiol 27:342–347.e1. [DOI] [PubMed] [Google Scholar]
- Linden-Carmichael AN, Calhoun BH, Patrick ME, Maggs JL (2018) Are protective behavioral strategies associated with fewer negative consequences on high-intensity drinking days? Results from a measurement-burst design. Psychol Addict Behav 32:904–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden-Carmichael AN, Stamates AL, Lau-Barraco C (2019) Simultaneous use of alcohol and marijuana: Patterns and individual differences. Subst Use Misuse 54:2156–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Ferrier AG, Sheehy MJ, Corbett K, Anderson DA, Simmons A (2005) Development of the Protective Behavioral Strategies Survey. J Stud Alcohol 66:698–705. [DOI] [PubMed] [Google Scholar]
- Martens MP, Pedersen ER, LaBrie JW, Ferrier AG, Cimini MD (2007) Measuring alcohol-related protective behavioral strategies among college students: Further examination of the Protective Behavioral Strategies Scale. Psychol Addict Behav 21:307–315. [DOI] [PubMed] [Google Scholar]
- Martin CS (2008) Timing of alcohol and other drug use. Alcohol Res Health 31:96–9. [PMC free article] [PubMed] [Google Scholar]
- Martin CS, Clifford PR, Clapper RL (1992) Patterns and predictors of simultaneous and concurrent use of alcohol, tobacco, marijuana, and hallucinogens in first-year college students. J Subst Abuse 4:319–326. [DOI] [PubMed] [Google Scholar]
- Meacham MC, Paul MJ, Ramo DE (2018) Understanding emerging forms of cannabis use through an online cannabis community: An analysis of relative post volume and subjective highness ratings. Drug Alcohol Depend 188:364–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier MH (2017) Associations between butane hash oil use and cannabis-related problems. Drug Alcohol Depend 179:25–31. [DOI] [PubMed] [Google Scholar]
- Metrik J, Gunn RL, Jackson KM, Sokolovsky AW, Borsari B (2018) Daily patterns of marijuana and alcohol co-use among individuals with alcohol and cannabis use disorders. Alcohol Clin Exp Res 42:1096–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midanik LT, Tam TW, Weisner C (2007) Concurrent and simultaneous drug and alcohol use: Results of the 2000 National Alcohol Survey. Drug Alcohol Depend 90:72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mochrie KD, Ellis JE, Whited MC (2019) Does it matter what we drink? Beverage type preference predicts specific alcohol-related negative consequences among college students. Subst Use Misuse 54:899–907. [DOI] [PubMed] [Google Scholar]
- Nakagawa S, Johnson PCD, Schielzeth H (2017) The coefficient of determination R2 and intra-class correlation coefficient from generalized linear mixed-effects models revisited and expanded. J R Soc Interface 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Napper LE, Kenney SR, Lac A, Lewis LJ, LaBrie JW (2014) A cross-lagged panel model examining protective behavioral strategies: Are types of strategies differentially related to alcohol use and consequences? Addict Behav 39:480–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIAAA (2007) Helping patients who drink too much: A clinician’s guide: updated 2005 edition (no. 7), US Department of Health and Human Services, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- O’Hara RE, Armeli S, Tennen H (2016) Alcohol and cannabis use among college students: Substitutes or complements? Addict Behav 58:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson MR (2013) Use of alcohol protective behavioral strategies among college students: A critical review. Clin Psychol Rev [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson MR, D’Lima GM, Kelley ML (2013) Daily use of protective behavioral strategies and alcohol-related outcomes among college students. Psychol Addict Behav 27:826–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Huang W, Dvorak RD, Prince MA, Hummer JF, Anthenien AM, Bravo AJ, Conner BT, Correia CJ, Dvorak RD, Egerton GA, Hustad JTP, Kholodkov T, King KM, Liese BS, Messina BG, Murphy JG, Neighbors C, Nguyen XT, Parnes JE, Pearson MR, Pedersen ER, Prince MA, Radomski SA, Ray LA, Read JP (2017) The Protective Behavioral Strategies for Marijuana Scale: Further examination using item response theory. Psychol Addict Behav 31:548–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Hummer JF, Rinker DV, Traylor ZK, Neighbors C (2016) Measuring protective behavioral strategies for marijuana use among young adults. J Stud Alcohol Drugs 77:441–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team (2020) R: A language and environment for statistical computing. [Google Scholar]
- Raudenbush SW, Bryk AS (2002) Hierarchical linear models: Applications and data analysis Methods. SAGE Publications. [Google Scholar]
- Read JP, Kahler CW, Strong DR, Colder CR (2006) Development and preliminary validation of the young adult alcohol consequences questionnaire. J Stud Alcohol 67:169–177. [DOI] [PubMed] [Google Scholar]
- Rogers JD, Greenfield TK (1999) Beer drinking accounts for most of the hazardous alcohol consumption reported in the United States. J Stud Alcohol 60:732–739. [DOI] [PubMed] [Google Scholar]
- Siegel MB, Naimi TS, Cremeens JL, Nelson DE (2011) Alcoholic beverage preferences and associated drinking patterns and risk behaviors among high school youth. Am J Prev Med 40:419–426. [DOI] [PubMed] [Google Scholar]
- Simons JS, Dvorak RD, Merrill JE, Read JP (2012) Dimensions and severity of marijuana consequences: Development and validation of the Marijuana Consequences Questionnaire (MACQ). Addict Behav 37:613–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer JD (1998) Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. J Educ Behav Stat 24:323–355. [Google Scholar]
- Sokolovsky AW, Gunn RL, Micalizzi L, White HR, Jackson KM (2020) Alcohol and marijuana co-use: consequences, subjective intoxication, and the operationalization of simultaneous use. Drug Alcohol Depend [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevens AK, Sokolovsky AW, Treloar Padovano H, White HR, Jackson KM (2020) Heaviness of alcohol use, alcohol problems, and subjective intoxication predict discrepant drinking reports in daily life. Alcohol Clin Exp Res. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stogner JM, Miller BL (2015) Assessing the dangers of “dabbing”: Mere marijuana or harmful new trend? Pediatrics 136:1–3. [DOI] [PubMed] [Google Scholar]
- Strandberg TE, Strandberg AY, Salomaa V V., Pitkälä K, Tilvis RS, Miettinen TA (2007) Alcoholic beverage preference, 29-year mortality, and quality of life in men in old age. Journals Gerontol 62:213–218. [DOI] [PubMed] [Google Scholar]
- Subbaraman MS, Kerr WC (2020) Subgroup trends in alcohol and cannabis co-use and related harms during the rollout of recreational cannabis legalization in Washington state. Int J Drug Policy 75:102508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman MS, Kerr WC (2015) Simultaneous versus concurrent use of alcohol and cannabis in the national alcohol survey. Alcohol Clin Exp Res 39:872–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry-McElrath YM, Patrick ME (2018) Simultaneous alcohol and marijuana use among young adult drinkers: Age-specific changes in prevalence from 1977 to 2016. Alcohol Clin Exp Res 42:2224–2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White HR, Kilmer JR, Fossos-Wong N, Hayes K, Sokolovsky AW, Jackson KM (2019) Simultaneous alcohol and marijuana use among college students: Patterns, correlates, norms, and consequences. Alcohol Clin Exp Res 43:1545–1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White HR, Labouvie EW (1989) Towards the assessment of adolescent problem drinking. J Stud Alcohol 50:30–37. [DOI] [PubMed] [Google Scholar]
- White HR, Labouvie EW, Papadaratsakis V (2005) Changes in substance use during the transition to adulthood: A comparison of college students and their noncollege age peers. J Drug Issues 35:281–305. [Google Scholar]
- Yurasek AM, Aston ER, Metrik J (2017) Co-use of alcohol and cannabis: A review. Curr Addict Reports 4:184–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


