Abstract
Since its outbreak in China at the end of 2019, the new coronavirus disease (COVID-19) was characterized by both easy spreading and high mortality. The latter proved to be way more elevated in the North of Italy -with a peak of 18.4% in region Lombardia and even 31% in the city of Bergamo and surrounding county- than in the rest of the world. In an attempt to conceptualize the reasons for such a dramatic situation, four key elements have been identified: COVID-19 itself, old age, lung disease, and heart failure. Their harmful combination has been named “The deadly quartet”. The underlying risk factors, among which a lot of them are distinctive features of the population in northern Italy, have been summarized as “unmodifiable”, “partially modifiable”, and “modifiable”, for the sake of clarity. Up-to-date scientific evidence in this field has been described in the form of a narrative and easy-to-read review.
Keywords: COVID-19, coronavirus, Italy, mortality, lung, heart
1. INTRODUCTION
In early December 2019, a new coronavirus, identified by the Chinese Center for Disease Control and Prevention and named 2019-nCoV or SARS-CoV-2 by WHO, was described to induce severe acute respiratory syndrome (COronaVIrus Disease 2019 or COVID-19) in Wuhan, China. SARS-CoV-2 later spread to Italy, other European countries, and the US experiencing much fear and concern. The WHO, on March 11th, 2020 called the disease a pandemic [1].
COVID-19 is transmitted by airborne droplets and is very contagious. Its usual clinical signs and symptoms involve the respiratory system and include high temperature, cough, shortness of breath, (usually bilateral) pneumonia with ground glass opacities at a computed tomography scan [2]. However, even the cardiovascular system can be involved in around 15% of the cases. Patients with additional extrapulmonary complications often have underlying cardiovascular diseases and/or one or more cardiovascular risk factors. Features associated with mortality include male gender, elderly, and presence of comorbidities such as high blood pressure, diabetes, smoking, and previous myocardial infar- ction or stroke. As a general rule, the higher the number of cardiovascular risk factors, the higher and earlier the mortality due to COVID-19. Acute cardiac injury, detected by a rise in high-sensitivity troponin blood levels, is commonly observed in severe cases and is strongly linked with mortality. The higher the level of troponin, the higher the risk of death. Severe acute respiratory distress is strongly related to mortality as well. On balance, COVID-19 leads to a high inflammatory burden, which in turn can cause vascular inflammation, myocarditis, and potentially life-threatening arrhythmias [3].
2. SEARCH STRATEGY
Pubmed/Medline, Scopus, and Web of Sciences databases were searched electronically utilizing Boolean operators and combinations of word variants for “coronavirus” and “SARS-CoV-2” and “COVID-19” and“death” and “mortality” and “Italy”. The search and selection criteria were restricted to the English language (at least the abstract). A total of 1,123 papers were identified, 435 duplicated included. The titles and abstracts of the remaining 688 papers were screened for subject importance. After a discussion between six reviewers (GC, PPB, FB, DS, MC, and FR), a complete intra-examiner agreement was obtained. In the case of disagreement over study inclusion, a discussion was held with the seventh reviewer (JLM) to reach an agreement. Finally, 9 suitable papers were identified. Additional 18 papers were included after checking the references of the relevant selected reviews and studies. As the selection process included heterogeneous study designs and sources, the results and key information obtained were summarized by means of a narrative approach.
3. SCIENTIFIC EVIDENCE
With regard to COVID-19 mortality, the current reports in the literature show some fluctuations among the different countries involved in the pandemic. Chinese scientists were the first to gather data and submit the related reports. So, in Wuhan, the epicenter of the outbreak in China, the reported overall mortality was 4.3% [4]. However, mortality was higher among COVID-19 patients with cardiovascular manifestations, than in those without cardiac involvement. When analyzing the entire population enrolled in their retrospective study, Guo and Coll. found that hypertension, coronary heart disease, and cardiomyopathy were the most common underlying cardiac conditions. Mortality during admission to hospital was 7.6% for patients without underlying cardiac conditions and normal troponin, 13.3% for those with underlying cardiac conditions and normal troponin, 37.5% for those without underlying cardiac conditions but elevated troponin, and 69.4% for those with underlying cardiac conditions and elevated troponin. Patients with underlying cardiac conditions were more likely to display elevation of troponin compared with individuals without them. Blood troponin values showed a strong direct correlation with C-reactive protein and N-terminal pro-brain natriuretic peptide. Blood troponin and N-terminal pro-brain natriuretic peptide were higher in patients who passed away. Furthermore, during their stay in the intensive care unit, patients with high troponin had more frequently malignant arrhythmias, and the administration of corticosteroids as well as the need for mechanical ventilation was more common compared to those with normal troponin levels. The mortality rates of patients with and without the use of angiotensin-converting enzyme inhibitors/angiotensin receptor blockers were 36.8% and 25.6%, respectively [5].
In the first few reports coming from the US, the severity of the disease in terms of mortality was analyzed by age group among COVID-19 cases that occurred from February 12thto March 16th, 2020. Overall mortality was 9.1%. When focusing on age, 80% of deaths were among subjects older than 65 years, with the highest percentage of severe outcomes among those aged 85 years or more. A lot of cases occurred among very old adults living in nurses' houses. Conversely, no deaths were reported among young people aged less than 19 years [6]. In another survey carried out in the New York City area, outcomes were assessed in patients who were discharged from the hospital or had died at the study endpoint. In this respect, 21% of them passed away, while mortality for those requiring mechanical ventilation was 88.1% [7].
Conversely, the mortality rate in Italy was way scarier than in the rest of the world. Overall, the death rate there was 12.2% among positive cases and even higher in the North of Italy. In region Lombardia -whose capital is Milan- and related counties like Bergamo, mortality rates were 18.4% and 31% respectively, thus generating a public hue and cry. In fact, northern Italian regions Lombardia, Emilia-Romagna, and Veneto had by far the highest number of infected individuals, accounting for 76% of all cases in Italy. The most affected counties were Bergamo, Brescia, Milan, and Cremona, which taken together accounted for 33% of all cases in Italy [8]. These numbers cannot be explained simply owing to the epidemic starting in Italy earlier than in the other countries besides China [9].
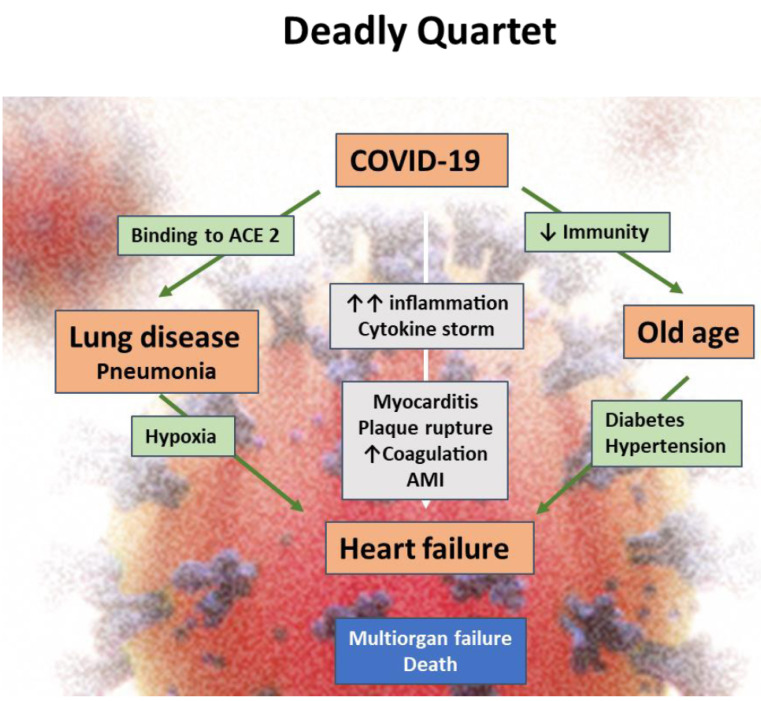
In an attempt to conceptualize the reasons for such a dramatic situation, four key elements have been identified: COVID-19 itself, old age, lung disease, and heart failure. The term “The deadly quartet” has been coined to name their harmful combination.
4. CORONAVIRUS (COVID-19)
The first animal model showing that viruses belonging to the Coronavirus family can jump from animals to humans, thus inducing myocarditis and congestive heart failure, dates back to 1992 [10]. Regarding SARS-CoV-2, it binds the carboxypeptidase angiotensin-converting enzyme 2 (ACE2) receptor in the pulmonary epithelium and myocardial cells surface, and is responsible for the pulmonary pathology. ACE2 activity has been shown to be regulated by renin-angiotensin-system blockers in some but not all clinical studies [11]. ACE2 polymorphisms have been linked to diabetes mellitus, cerebral stroke, and hypertension as well [12].
5. OLD AGE
While a vast majority of patients with COVID-19 infection require minimal care, others with moderate and severe disease require intensive care, primarily to support their pulmonary and cardiac functions. The risk for hospitalization also increases with age; specifically, 11.8% of patients in their 60s require admission, with 16.6% of patients in their 70s, and 18.4% of patients in their 80s or older [13]. Those with severe disease have reduced immunity to fight the burden of the infectious process and often suffer from hypertension and diabetes as well. The risk for death from COVID-19 is 1.0 to 1.50% overall, but rises with age from < 1% among children aged 9 years or less to nearly 8% for subjects aged 80 years or older [13]. Higher mortality in Italy has been attributed to a much higher (23%) number of older folks (65 years or higher) in the general population. Conversely, the proportion of the population older than 65 years is 9.5% in Alaska and 19.1% in Florida [14]. As to the first four months of the disease, 84.1% of those who passed away in Italy were over 70 years (29.7% between 70 and 79 years; 40.5% between 80 and 89 years) [15]. Regarding China, where COVID-19 started, available data are less precise. What is known is that about 55% of the deceased had more than 49 years. The Chinese Center for Disease Control and Prevention reported a case fatality rate (i.e. the ratio between the number of deceased patients and that of patients diagnosed with Covid-19) of 14.8% in those over 80 years [15].
6. SEVERE PNEUMONIA
A vast majority of patients with COVID-19 infection present with acute and severe respiratory distress, develop pneumonia, and many require mechanical or assisted ventilation. Patients with pre-existing pulmonary disease are prone to develop extensive interstitial alveolar pneumonia. Further, there is intense inflammation in the lungs, which is also reflected in the systemic circulation as high white blood cell count and high CRP levels [16].
7. CARDIAC INJURY AND HEART FAILURE
The demographic and clinical profile of hospitalized patients with COVID-19 shows a high (20-50%) prevalence of cardiac involvement [17, 18]. Many patients have acute myocarditis as a result of direct viral infiltration but also from intense systemic inflammation and cytokine storm. In some patients, particularly the elderly with diabetes and hypertension and pre-existing coronary atherosclerosis, there may be instability of atherosclerotic plaque followed by rupture, in situ clotting and acute coronary syndrome. Cardiac involvement is characterized by ST-segment elevation and elevated levels of C-reactive protein, creatinine kinase-MB, N-terminal pro-B-type natriuretic peptide, and cardiac dysfunction and arrhythmias. In one report, patients with cardiac injury were generally older than those without (median age 74 vs. 60 years), had more frequent acute respiratory distress syndrome (58.5% vs 14.7%) and acute kidney injury (8.5% vs 0.3%), and suffered from higher mortality (51.2% vs. 4.5%). Other studies in different groups of patients confirmed these findings [5, 18].
In addition to the deadly quartet, which can apply worldwide, a few peculiar Italian factors are likely to have contributed to such a high mortality. Again, for the sake of clarity, we have tried to summarise them as:
1). Unmodifiable factors: Male gender and cold weather.
2). Partially modifiable factors: These include the extreme burden of incidence of the disease, shortage of medical personnel, weakness in the national health care system especially with regard to the availability of ventilators and pharmacological guidelines as to the use of anti-viral/anti-inflammatory/anti-malarial drugs in old patients [1]. Overall, 5,090 intensive care unit beds with a ventilator (8.4 per 100,000 population) are available in Italy, and 2,601 beds in coronary care units (4.3 per 100,000 population), while they are too much higher numbers in the US (36 ICU beds per 100,000 population) [19].
3). Modifiable factors: These include avoidance of highly transmissible viral infection and high air pollution. In this respect, the Champions League soccer match on February 19th, 2020 (Atalanta vs Valencia), which was attended in Milan by more than a third of the population of Bergamo, who continued partying overnight thereafter, acted as ‘infective bomb of transmission‘. Italian people have a marked tendency to socialise with frequent congregations and clustering. It is also possible that in early stages, there was not much adoption of standard hygienic measures, and instructions to lockdown proved difficult to be accepted [9]. The burden of air pollution in the Val Padana land (corresponding to regions Lombardia and Emilia-Romagna) is overwhelming. Based on the air quality index (comprising PM10, PM2.5, O3, SO2 and NO2), Lombardia and Emilia Romagna are among the most polluted areas in Italy, even worse than some regions in China [20]. There is evidence that people living in territories with high levels of air pollution and with long-term exposure to it are more prone to develop chronic respiratory and cardiovascular diseases [21, 22]. In a recently published paper, a strong link between exposure to NO2 and coronavirus fatality was detected. In fact, 78% of deaths were in five regions located in northern Italy and central Spain. Interestingly, the same five regions had the highest NO2 concentrations combined with downwards airflow, which prevent an efficient dispersion of air pollution. Coronavirus might hitch a ride from air pollution [23].
CONCLUSION
We suggest that old age, lung disease and heart failure play an interactive role in multiorgan failure and resultant death in patients with COVID-19 infection (Fig. 1). Concomitant specific Italian features are contributing factors. Severe inflammation and cytokine storm in the elderly patients with compromised immune response and diabetes and hypertension contribute to the failure of the heart, lungs and other organs and eventually to death [24, 25]. In particular, myocardial injury is significantly linked with a worse outcome of COVID-19, since it is associated with the appearance of cardiac dysfunction and arrhythmias. So, aggressive treatment should be considered for patients at high risk of myocardial damage and differential diagnosis with other infective pathologies, including endocarditis, should be done [26].
Fig. (1).
The deadly quartet, i.e., the combination of COVID-19, old age, lung disease (pneumonia), and heart failure. Abbreviations: AMI: acute myocardial infarction (A higher resolution / colour version of this figure is available in the electronic copy of the article).
Further, the pandemic of COVID 19 is an exceptional challenge to ascertain effective drugs for prevention and treatment [27].
ACKNOWLEDGEMENTS
Declared none.
CONSENT FOR PUBLICATION
The consent was provided by all the authors.
FUNDING
None.
CONFLICT OF INTEREST
The authors have no conflicts of interest, financial or otherwise.
REFERENCES
- 1.Romeo F., Calcaterra G., Barilla F., Mehta J.L. Coronavirus disease 2019 infection and the cardiovascular system. J. Cardiovasc. Med. (Hagerstown) 2020;21(6):403–405. doi: 10.2459/JCM.0000000000000980. [DOI] [PubMed] [Google Scholar]
- 2.Li H., Liu Z., Ge J. Scientific research progress of COVID-19/SARS-CoV-2 in the first five months. J. Cell. Mol. Med. 2020;24(12):6558–6570. doi: 10.1111/jcmm.15364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Madjid M., Safavi-Naeini P., Solomon S.D., Vardeny O. Potential effects of coronaviruses on the cardiovascularsystem: A review. JAMA Cardiol. 2020;5(5):831–840. doi: 10.1001/jamacardio.2020.1286. [DOI] [PubMed] [Google Scholar]
- 4.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Wang B., Xiang H., Cheng Z., Xiong Y., Zhao Y., Li Y., Wang X., Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;23(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guo T., Fan Y., Chen M., Wu X., Zhang L., He T., Wang H., Wan J., Wang X., Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(7):811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19) - United States, February 12-March 16, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69(12):343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W., Barnaby D.P., Becker L.B., Chelico J.D., Cohen S.L., Cookingham J., Coppa K., Diefenbach M.A., Dominello A.J., Duer-Hefele J., Falzon L., Gitlin J., Hajizadeh N., Harvin T.G., Hirschwerk D.A., Kim E.J., Kozel Z.M., Marrast L.M., Mogavero J.N., Osorio G.A., Qiu M., Zanos T.P. and the Northwell COVID-19 Research Consortium. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the new york city area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. https://www.statista.com/statistics/1099389/coronavirus-deaths-by-region-in-italy/
- 9.Boccia S., Ricciardi W., Ioannidis J.P.A. What other countries can learn from italy during the COVID-19 pandemic. JAMA Intern. Med. 2020;180(7):927–928. doi: 10.1001/jamainternmed.2020.1447. [DOI] [PubMed] [Google Scholar]
- 10.Edwards S., Small J.D., Geratz J.D., Alexander L.K., Baric R.S. An experimental model for myocarditis and congestive heart failure after rabbit coronavirus infection. J. Infect. Dis. 1992;165(1):134–140. doi: 10.1093/infdis/165.1.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vaduganathan M., Vardeny O., Michel T., McMurray J.J.V., Pfeffer M.A., Solomon S.D. Renin–angiotensin–aldosterone system inhibitors in patients with Covid-19. N. Engl. J. Med. 2020;382(17):1653–1659. doi: 10.1056/NEJMsr2005760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fang L., Karakiulakis G., Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir. Med. 2020;8(4):e21. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Verity R, Okell LC, Dorigatti I, Winskill P, Whittaker C, Imai N, Cuomo-Dannenburg G, Thompson H, Walker PGT, Fu H, Dighe A, Griffin JT, Baguelin M, Bhatia S, Boonyasiri A, Cori A, Cucunubá Z, FitzJohn R, Gaythorpe K, Green W, Hamlet A, Hinsley W, Laydon D, Nedjati-Gilani G, Riley S, van Elsland S, Volz E, Wang H, Wang Y, Xi X, Donnelly CA, Ghani AC, Ferguson NM. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect Dis. 2019;S1473-3099(20):30243–30247. doi: 10.1016/S1473-3099(20)30243-7.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in Italy JAMA. 2020 doi: 10.1001/jama.2020.4683.. [DOI] [PubMed] [Google Scholar]
- 15.Casti G., Bassareo P.P., Limone M., Pistolesi F., Fanos V., Marcialis M.A. Epidemiology of SARS-CoV-2: Numbers matter! J Pediatr Neonat Individual Med. 2020;9(2):e090203. doi: 10.7363/090203. [DOI] [Google Scholar]
- 16.Li R., Tian J., Yang F., Lv L., Yu J., Sun G., Ma Y., Yang X., Ding J. Clinical characteristics of 225 patients with COVID-19 in a tertiary Hospital near Wuhan, China. J. Clin. Virol. 2020;127:104363. doi: 10.1016/j.jcv.2020.104363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F., Gong W., Liu X., Liang J., Zhao Q., Huang H., Yang B., Huang C. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5(7):802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alderighi C., Rasoini R., Ambrosio G., Valente S., Gensini G.F. New insights into the seriousness of acute myocardial injury during COVID-19. G. Ital. Cardiol. (Rome) 2020;21(5):328–331. doi: 10.1714/3343.33128. [DOI] [PubMed] [Google Scholar]
- 19.Epidemia COVID-19, aggiornamento nazionale. 2020 Available from: https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_30-marzo-2020.pdf.
- 20.Qin C., Zhou L., Hu Z., Zhang S., Yang S., Tao Y., Xie C., Ma K., Shang K., Wang W., Tian D.S. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin. Infect. Dis. 2020;71(15):762–768. doi: 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peng L., Zhao X., Tao Y., Mi S., Huang J., Zhang Q. The effects of air pollution and meteorological factors on measles cases in Lanzhou, China. Environ. Sci. Pollut. Res. Int. 2020;27(12):13524–13533. doi: 10.1007/s11356-020-07903-4. [DOI] [PubMed] [Google Scholar]
- 22.Grande G., Ljungman P.L.S., Eneroth K., Bellander T., Rizzuto D. Association between cardiovascular disease and long-term exposure to air pollution with the risk of dementia. JAMA Neurol. 2020;77(7):801–809. doi: 10.1001/jamaneurol.2019.4914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to coronavirus (COVID-19) fatality. Sci. Total Environ. 2020;726:138605. doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Damaskos C., Garmpis N., Kollia P., Mitsiopoulos G., Barlampa D., Drosos A., Patsouras A., Gravvanis N., Antoniou V., Litos A., Diamantis E. Assessing cardiovascular risk in patients with diabetes: An update. Curr. Cardiol. Rev. 2020;16(4):266–274. doi: 10.2174/1573403X15666191111123622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mene-Afejuku T.O., Pernia M., Ibebuogu U.N., Chaudhari S., Mushiyev S., Visco F., Pekler G. Heart failure and cognitive impairment: clinical relevance and therapeutic considerations. Curr. Cardiol. Rev. 2019;15(4):291–303. doi: 10.2174/1573403X15666190313112841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Calcaterra G., Crisafulli A., Guccione P., Di Salvo G., Bassareo P.P. Infective endocarditis triangle. Is it the time to revisit infective endocarditis susceptibility and indications for its antibiotic prophylaxis? Eur. J. Prev. Cardiol. 2019;26(16):1771–1774. doi: 10.1177/2047487319856126. [DOI] [PubMed] [Google Scholar]
- 27.Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;323(18):1824–1836. doi: 10.1001/jama.2020.6019.. [DOI] [PubMed] [Google Scholar]