Abstract
There is growing evidence that pre-exposure prophylaxis (PrEP) prevents HIV acquisition. However, in the United States, approximately only 4% of people who could benefit from PrEP are currently receiving it, and it is estimated only 1 in 5 physicians has ever prescribed PrEP. We conducted a scoping review to gain an understanding of physician-identified barriers to PrEP provision. Four overarching barriers presented in the literature: Purview Paradox, Patient Financial Constraints, Risk Compensation, and Concern for ART Resistance. Considering the physician-identified barriers, we make recommendations for how physicians and students may work to increase PrEP knowledge and competence along each stage of the PrEP cascade. We recommend adopting HIV risk assessment as a standard of care, improving physician ability to identify PrEP candidates, improving physician interest and ability in encouraging PrEP uptake, and increasing utilization of continuous care management to ensure retention and adherence to PrEP.
Keywords: HIV, pre-exposure prophylaxis, PrEP, medical curriculum
What do we already know about this topic?
Men and transgender women (TGW) who have sex with men have a greater incidence of Human Immunodeficiency Virus (HIV) infection compared to TGW and gay, bisexual and other men who have sex with men (GBMSM) are at an increased risk from the HIV infection. Though pre-exposure prophylaxis (PrEP), a combination antiretroviral medication has been shown to reduce the risk of infection, the uptake is far below most national targets. To implement PrEP effectively, it should be addressed in the medical curriculum and the best practices in PrEP training employed in medical schools as part of the National HIV/AIDS prevention strategy to reduce the incidence of HIV.
How does your research contribute to the field?
Our review findings provide important information for clinicians, caregivers, healthcare administrators, and health policy makers as these findings highlight the need for the above-mentioned TGW and GBMSM to adhere to PrEP. Additionally, clinical faculty, residents, and physicians may work together to increase PrEP knowledge and competence in clinical settings by updating the graduate medical education curriculum and training methods.
What are your research’s implications toward theory, practice, or policy?
Our findings may inform how to enhance physician ability to identify PrEP candidates, encouraging PrEP uptake and utilize continuous care management to encourage adherence to PrEP. We envision a greater role played by practicing physicians in mitigating the HIV infections through increased PrEP usage eventually contributing to enhanced patient care.
Background
Despite the decline in the number of individuals diagnosed over the past decade with Human Immunodeficiency Virus (HIV), approximately 50 000 new cases continue to be identified annually in the United States.1 Pre-exposure prophylaxis (PrEP), a once-daily combination antiretroviral medication (tenofivir and emtricitabine) has been shown to reduce the risk of infection by between 44% and 86%2 and, with greater medication adherence, reduction rates are found to be even higher.3,4 While it is estimated that 1.2 million people could benefit from PrEP, currently only 70,395 are taking this regimen.5 This extremely low rate—under 5% (4.4%)—is of particular concern and may indicate a need to enhance primary care education to increase prescribing. The efficacy of PrEP among those with adherence was reported to be over 80%.6
Since the inception of the HIV epidemic, men, and TGW who have sex with men have had higher rates of HIV infection in the United States7-9 compared with GBMSM. Despite accounting for as little as 2% of the U.S. population, men who have sex with men (MSM) make up 58% of people living with HIV/AIDS (PLWHA) nationwide,10 and trends demonstrate that while infection rates are declining among heterosexual populations, they are either stable or reduced for all MSM with the exception of American Indian/Alaska Native and Native Hawaiian men who inject drugs among the MSM sub-population.10 While few data are available on HIV disparities among transgender women who have sex with men, 2 available studies have reported higher rates among the male to female transgender (MTF) population than among heterosexual men or women.8,9 In the U.S., while women account for only 19% of all new HIV infections, Black women including multipartnering women are second only to MSM in new infection rates.11 A summary of 4 national household surveys revealed that the percent of people who inject drugs (PWID) in the U.S. ranged from 0.24 to 0.59% across surveys.12 The small sample size, exclusion of unstably housed, and incarcerated persons, missing key populations and self-report of data were recognized as limitations by Bradley et al.12 Furthermore, PWID account for approximately 8% of new HIV infections in the U.S.13 All of the aforementioned populations could benefit from PrEP and should be addressed in any curriculum designed to implement PrEP effectively.
The efficacy of PrEP as a preventive measure has been tested in multiple studies14-19 and meta-analyses20,21 and findings suggest that, when used consistently, PrEP results in significantly decreased rates of HIV infection. A meta-analysis study of PrEP efficacy confirmed that PrEP was equally effective for men and women.18,22,23 Nevertheless, physicians remain less likely to prescribe PrEP to women than to men. While no studies of PrEP for PWID have been conducted in the U.S., the Bangkok Tenofivir Study found a reduction in HIV infection of 49% to 74%19 among PWID. However, uptake of prescribing PrEP for PWIDs has been slow, and may be in part due to lack of government support (providing needles and syringes, condoms, HIV testing, and counselling etc.) for PrEP with this population24 and stigma related to injection drug use.25
Though empirical support for the effectiveness of PrEP is well established, medication adherence mediates the impact the drug can have. Adherence rates have been found to vary widely across studies depending on how adherence is measured.26,27 In 3 studies where blood levels of Tenofovir were used to measure adherence, the HIV infection rates were strikingly lower (84%-92%) for people with the drug detected compared with placebo.28 While some factors such as heavy alcohol use and younger age have been found to attenuate adherence,28 other factors including partner support and increased perception of risk are associated with increased adherence.29
In order for PrEP to reach its full potential in reducing HIV, those individuals at greatest risk must have widespread access. A predominant way to achieve this is by increasing the pool of willing and able prescribing physicians. While barriers to prescribing PrEP to at-risk populations have been noted in the literature,30-50 training primary care medical students appropriately to engage individuals at elevated risk in prescribing the medication is understudied, and recommendations for effective training are needed.
The aim of this scoping review was twofold: to determine: (a) what are the barriers to PrEP prescribing among practicing primary care physicians, and (b) what are the best practices in PrEP training employed in medical schools. The need to develop curricula that include PrEP training is directly in line with the National HIV/AIDS prevention strategy to provide doctors with the skills needed to reduce the incidence of HIV. The findings of this scoping review are organized using the PrEP cascade model,31 and provide recommendations for both content and educational delivery methods.
Methods
Search Strategy and Study Selection
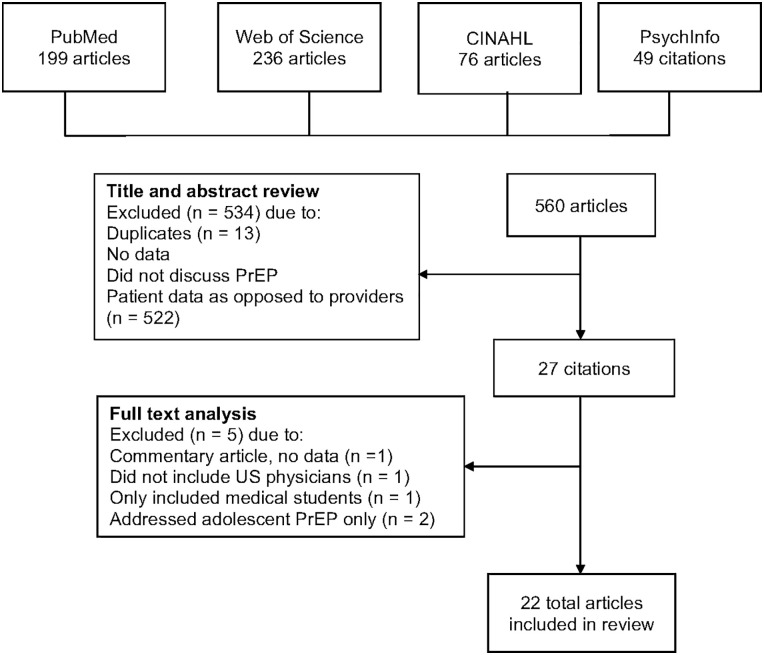
Four authors conducted a scoping review of articles retrieved from PubMed, Web of Science, CINAHL, and PsychInfo, using the following search terms: (HIV) plus any of the following: (Prevention OR Pre Exposure prophylaxis (PrEP) OR Biomedical HIV prevention OR oral preexposure prophylaxis OR Pre-exposure prophylaxis OR Healthcare provider OR primary care providers OR early adopters OR primary care OR health services research OR education, medical OR implementation OR Medical Field Training OR Training, Medical Field OR Studies, Medical Field). Title and abstracts were reviewed to determine relevance (whether the studies examine provider views of PrEP, or examine medical school training outcomes for PrEP) and articles were excluded due to the following criteria: (a) was a duplicate; (b) missing primary data (qualitative or quantitative); (c) did not discuss PrEP, reducing the total number of articles from 560 to 27.
The full texts of the remaining articles were examined and eliminated if they were commentaries and non-empirical, did not include US physicians, only included medical students or only addressed adolescent PrEP. Studies only of providers practicing outside the U.S. were excluded, as the barriers and facilitators to PrEP in other countries have been found to vary based on local context. Furthermore, studies examining provider views of PrEP for adolescents were excluded, as these barriers often pertain to consent and assent and involvement of family members and guardians that are often specific to individual state guidelines. Finally, commentaries and non-empirical articles were omitted. An additional 5 articles were excluded for relevance, reducing the number of studies from 27 to 22 total articles included in the review.
The full review process to demonstrate article exclusion is illustrated in Figure 1. Sixteen of the articles were cross-sectional surveys while a further 6 were qualitative interviews.
Figure 1.
Schematic of literature search process.
Quality Assessment
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist51 was employed to evaluate the 16 cross-sectional surveys. In previous studies the quality assessment tools have been summed and percentages calculated to indicate the degree to which the study had sufficient rigor to be included in a systematic review52
For the 6 qualitative studies, the Consolidated Criteria for Reporting Qualitative Research (CORE-Q) checklist53 was utilized to assess the quality of reporting.53 These studies, while well reported, were missing key items from the CORE-Q, specifically in reporting relationships with the participants and reporting non-participation, including dropout rates. The setting, date of data collection, description of the subjects, study design, and quality scores from both STROBE and CORE-Q are presented, and summaries of the findings and conclusions from all the studies are presented in Table 1.
Table 1.
Summary of Systematic Review Findings.*
| Source | Setting/date of data collection | Subjects/participants | Design | Quality % | Findings | Implications |
|---|---|---|---|---|---|---|
| Smith et al41 | National Multiple years: 2009, 2010, 2012, 2013, 2014, and 2015 |
2009: Recruited 1500 physicians and nurse practitioners (NPs) 2010: 1504 physicians and NPs 2012: 1503 physicians and NPs 2013: 1507 physicians and NPs 2014: 1508 physicians and NPs 2015: 1501 physicians and NPs 2009, 2010, and 2012 recruits were from Epocrates panel of physicians 2014-2015 were recruited from SERMO’s Global Medical Panel |
Cross sectional survey designed by Porter Novelli Public Services to assess physician awareness of and attitudes regarding PrEP. | 74 | From 2009 to 2012 1% of clinicians had prescribed PrEP, this rose to 4% in 2013 and 2014, and then rose again to 7% in 2015. PrEP awareness was low in 2009 and 2010 (24% and 29% respectively) and then increased greatly in 2012-2015 (49%, 51%, 61%, 66%). Clinicians were most willing to prescribe PrEP to an uninfected partner in a serodiscordant relationship. | Physician education should focus on generalists who potentially come in contact with a greater number of high HIV risk patients. Education should focus on properly taking a sexual history, identifying patients at risk of HIV transmission, and risk reduction counseling. Raising overall knowledge of Truvada (side effects, dosing, proper candidates) is vital in effectively using antiretroviral’s on a large scale. |
| White et al32 | Massachusetts Pre iPrex: July-December 2010 Post iPrex: December 2010-April 2011 |
Recruited 178 physicians pre-iPrex and 115 physicians post-iPrex through HIV Medical Association, Infectious Disease Society of America, League of Community Health Centers, as well as direct emailing to hospitals, community health centers, physician practice groups and university directories throughout Massachusetts | Cross sectional online survey comparing the knowledge, beliefs, and experience with PrEP before and after the release of iPrex clinical trial data | 74 | Over the 2 time periods knowledge of oral PrEP increased from 79% to 92%, while knowledge of topical microbicides were already high (89%). Only 4% of respondents had prescribed PrEP post-iPrex. Most common barriers to prescribing were toxicities and ARV resistance. Formal guidelines from the CDC and patient’s requesting PrEP were major factors that would influence the likelihood of prescribing. | Educational initiatives should focus on closing the gap of knowledge and awareness of PrEP between HIV specialists and primary care physicians. Physicians need training on the importance of adherence counseling and monitoring. |
| Mimiaga et al33 | Massachusetts December 2010-April 2011 |
Recruited 115 HIV specialists and generalists through the League of Community Health Centers | Cross sectional survey assessing physicians’ knowledge, experiences, and beliefs regarding PrEP after the release of iPrEx. | 55 | Awareness of iPrEx was 64% and CAPRISA was 57%. 70% believed that the gel should be available to all at risk persons compared to 40% for oral PrEP. HIV specialists were more knowledgeable than generalists about iPrEx and CAPRISA. | Medical students and physicians should be educated on the risks and benefits of PrEP to assist patients interested in PrEP. Educational interventions focusing on the efficacy of PrEP and how nonadherence affects efficacy may increase the willingness to prescribe PrEP among generalists. |
| Tellalian et al31 | National April-September 2011 |
Recruited 189 HIV practitioners from the American Academy of HIV Medicine | Cross sectional online survey to evaluate PrEP knowledge, attitudes, perceptions and prescribing practices. | 61 | 90% of respondents were familiar with iPrex and CDC interim guidelines. Only 19% of practitioners had prescribed PrEP, of these 17% prescribed a triple drug HIV regimen as PrEP. 58% of respondents reported that treating serodiscordant couples would most influence their decision to prescribe PrEP. Common concerns were: ARV resistance, risk compensation, non-adherence, and cost. Only 13% thought that PrEP was the most effective method for reducing HIV acquisition. | Even with reported lower risk behaviors in their patient population, providers acknowledged risk compensation as a concern indicating further education on this barrier is needed. Training to serve populations that are candidates for PrEP is needed. |
| Arnold et al46 | California May-December 2011 |
22 in depth interviews with PCPs, HIV specialists, community health clinic providers, and public health officials | In depth interviews were conducted regarding physician knowledge of iPrEx, CDC guidance, cost considerations, capacity of primary care practices, dosing schedules, and toxicity monitoring | Five themes emerged from interviews: little consensus on PrEP target populations, current models of care and skill sets were not always well suited for prescribing PrEP, a need to build capacity to prescribe PrEP, concerns about monitoring adherence side effects and toxicities as well as resistance and risk compensation, there was still a belief in the public health benefits of PrEP even after HPTN 052 (HIV Prevention Trials Network 052; a clinical trial) results. Primary care was discussed as the best location for PrEP, but their models for care would need to be updated to accommodate PrEP. Adherence monitoring, ARV resistance, and risk compensation came up as major concerns for physicians. |
Educational interventions clearly defining the target population’s for PrEP is necessary. Training on how to alter current practice models to provide the full PrEP cascade of care is crucial to enabling scaling up prescribing. Education on monitoring toxicities and renal function are needed. | |
| Castel et al35 | Miami, Florida and Washington D.C. March 2012-March 2013 |
Recruited 142 HIV providers from physician societies, training centers, and health departments | Cross sectional online survey of HIV providers evaluating PrEP knowledge, experience, and intention to prescribe | 61 | 53% of providers agreed that PrEP was effective or most effective and 24% had prescribed PrEP. A latent class analysis was used identifying 2 unique classes (Class 1: PrEP less effective and with barriers, Class 2: PrEP moderately effective with few barriers). Class 1 showed to have less PrEP knowledge/experience, were less likely to prescribe PrEP to individuals with multiple sex partners and individuals with a history of injection drug use. | Differences in the 2 classes indicate that non-prescribers perceived barriers to implementing PrEP were greater than the reported barriers of prescribers. Getting education early in medical training is vital to overcome these perceived feasibility issues. Early training may increase PrEP prescription as well as increase the populations perceived to be in need including PWID and individuals with multiple sex partners. |
| Hoffman et al45 | NYC Region 2012-2013 |
30 in depth interviews with PCPs and HIV specialists in the NYC region | In depth interviews of physicians and NPs to determine who should prescribe PrEP. | HIV specialists and PCPs indicated that primary care is the appropriate venue in which to deliver PrEP, as these practices come into contact with more HIV negative patients. HIV specialists, however, possess the skills and knowledge needed to deliver PrEP. Most interviewees claimed the need for knowledge of the medications, sexual risk assessments, and the ability to monitor adherence. | While it is believed that PrEP should be available to high-risk HIV negative patients seen in primary care, PCPs tend to not have the skills needed to properly monitor patients on PrEP. Training PCPs with the necessary skills is critical to solving the purview paradox. | |
| Karris et al44 | National includes Canada, conducted June-July 2013 | Recruited 573 of 1175 (48.8%) ID physicians from the Infectious Disease Society of America’s Emerging Infections Network. However, the bulk of the findings report on only 285 respondents. By Region: 68 (24%) New England/ Mid Atlantic 66 (23%) Midwest 81 (28%) South 68 (24%) Pacific and Mountain 2 (1%) Canada |
Cross sectional online survey comparing those who WOULD prescribe PrEP to those who have prescribed. GIS analysis conducted to determine whether prescribers were clustered geographically. |
58 | Most providers (74%) support PrEP, while only 9% have provided. Those who would not prescribe cited non-adherence/resistance, cost, lack of efficacy evidence, and not exposing the healthy to a toxic drug. Among those who would or do prescribe PrEP: most would not use NAT, and some only with acute HIV symptoms. Most monitor adherence through self-report on a quarterly basis. |
With ARV resistance being a concern among many, medical education regarding acute HIV infection is vital as those individuals are at increased risk to build resistance. Teaching this to all medical students should help decrease the concern about ARV resistance. |
| Finocchario-Kessler et al49 | National August 2013-October 2014 |
85 interviews with doctors and NPs By City: Atlanta: 8 Baltimore: 14 Houston: 13 Kansas City: 9 Newark: 8 Philadelphia: 20 San Francisco Bay Area: 13 |
Phone interviews evaluating the use of PrEP for safe conception among serodiscordant couples. | 18.8% of providers had prescribed PrEP for safer conception. 74.2% reported a willingness to consider PrEP for safer conception. 7% were resistant to the idea of PrEP for safer conception. The majority (50%) or providers who had prescribed PrEP were located in Philadelphia. The benefits repeated by respondents were that PrEP gave an added level of protection and a greater sense of control for HIV-negative partner. Concerns included adherence, ARV resistance, side effects, monitoring uninfected partner, insurance restrictions and risk compensation. |
Work with this population may best be done by HIV specialists, as the partner may more easily access this specialist. | |
| Krakower et al47 | Boston September 2013-August 2014 |
31 semi structured interviews with LGBT specialists and generalists | 60 min in person interviews to assess how providers approach decisions about prescribing and the range of provider experiences with PrEP | 39% of providers had prescribed PrEP. Both specialists and generalists used a shared decision making process in whether or not PrEP was prescribed that weighed patient preference and the potential risks. Clinicians would prescribe PrEP to most patients engaged in high risk behaviors. Adherence is a concern and patients that showed little interest were not persuaded to use PrEP. Many clinicians indicated that prescribing PrEP to interested but low risk patients was a misuse of PrEP. Generalists were inexperienced with PrEP but reported interest in learning about it. |
Increased education among generalists is vital for the uptake of PrEP nationally. Creating educational opportunities tailored towards generalists and their role in disease prevention may increase the number of generalists who show interest in learning about PrEP and ultimately prescribe PrEP. Recruiting LGBT and/or HIV specialists to train and work with generalists may increase PrEP knowledge and intent to prescribe among generalists. | |
| Krakower et al34 | New England September to December 2013 |
Recruited 184 practitioners who attended educational programs offered by the NEAETC | Cross sectional survey to assess knowledge, practices, and perceptions about early ART and PrEP | 55 | 89% of practitioners had heard of PrEP however only 19% had prescribed. Of the practitioners who had not prescribed PrEP only 58% were likely or very likely to prescribe PrEP in the future. A minority (6%) strongly agreed or agreed that PrEP was not effective. The major concerns for respondents were side effects, ARV resistance, and risk compensation. | While the majority of clinicians prescribed or would be willing to prescribe PrEP, education on the safety and lack of evidence of widespread drug resistance may be necessary to convince the resistant minority to adopt PrEP. |
| Bacon et al37 | San Francisco Bay Area May 2014 |
Recruited 99 (14%) primary care providers through the San Francisco Bay Area Collaborative Research Network | Cross sectional online survey to assess the association of intention to prescribe PrEP with sociodemographic and practice variables, PreP knowledge, and prior prescribing behavior | 71 | Almost all providers had heard of PrEP (92%) however only 26% had prescribed. Even with the low prescribing numbers 70% were very or somewhat confident in prescribing PrEP. The majority of providers reported that they would prescribe PrEP to MSM with an HIV infected partner (91%), women who have sex with an HIV infected male partner (92%), women with multiple partners (88%), MSM with inconsistent condom use during receptive sex (83%), and MSM with inconsistent condom use during insertive sex (71%). Caring for HIV infected patients was associated with an increase in the willingness to prescribe PrEP. The major concerns for providers were: toxicity/adverse side effects, ARV resistance, and adherence. | More PCPs had prescribed PrEP than in national surveys (25%-10%). Utilizing HIV specialists to expand PrEP to PCPs is a strategy used in the SF Bay area, and seemingly has led to higher prescription rates. Concerns about PrEP remain similar to what has been seen in previous studies. Several training topics for medical students were noted listed in descending order of importance: HIV testing frequency, contraindications for PrEP, non-HIV labs, PrEP eligibility, adherence counseling, types HIV tests, side effects, insurance coverage, and sexual behavior counseling. This hierarchy may change from by area of the country. |
| Adams and Balderson36 | National June 2014 |
Recruited 260 providers through membership with the American Academy of HIV Medicine | Cross sectional online survey assessing PrEP practices and likelihood to prescribe PrEP across patient type | 68 | Likelihood to prescribe PrEP differed across patient types. Providers were more likely to prescribe PrEP for MSM patients with HIV positive partner (78%). Providers were least likely to prescribe to high-risk heterosexuals (47%) and IV drug users (45%). | Guidelines should be developed to aid in determining eligibility for non-MSM. Medical education should include the network aspect of risk and stress sexual and drug use history taking. |
| Walsh and Petroll38 | Providers from 10 U.S. cities with the highest HIV prevalence and located in zip codes with an HIV prevalence of at least 0.5% recruited between July 2014 and May 2015. | Recruited 280 PCPs through professional organizations located in high prevalence zip codes within high prevalence cities in the US. By region: 120 South 56 West 34 Midwest 73 Northeast |
Cross sectional online survey assessing information, motivation, and behavioral skills associated with PrEP discussion and prescription | 74 | 75% of PCPs were familiar with PrEP. On average PCPs answered 67% of the knowledge question correctly. 33% discussed PrEP with patients and 17% had prescribed PrEP. | Factual inaccuracies need to be corrected, attitudes improved, perhaps using success stories, and physicians with PrEP experience should be used to train others. Skills training and role play are recommended for behavioral skills such as sexual history taking. |
| Petroll et al42 | National 10 cities with high HIV prevalence further restricted to high prevalence zip codes. July 2014-May 2015 |
Recruited 525 HIV Physicians and PCPs from American Medical Association, American Association of Nurse Practitioners, and American Academy of HIV Medicine By Region: 184 South 58 Midwest 126 West 163 Northeast |
Cross sectional survey comparing HIVPs and PCPs comfort performing clinical activities regarding PrEP, awareness of PrEP, degree of familiarity with prescribing PrEP, barriers to PrEP, attitudes towards PrEP, and willingness to prescribe PrEP | 84 | HIVPs were more comfortable with clinical activities than PCPs (89%-59%). 98% HIVPs were aware of PrEP compared to 76% of PCPs and 76% of HIVPs were familiar with prescribing PrEP compared to 28% of PCPs. The south had the lowest familiarity with prescribing PrEP. Major concerns with PrEP were completing prior authorizations and concerns about insurance coverage. | A significant drop between physician awareness and knowledge to actual prescribing was noted. Could be attributed to lack of experiencing in sexual history taking, as well as dispelling factual inaccuracies regarding PrEP. Navigation of insurance systems should be included in medical education to increase PrEP. PrEP prescribing seems to lessen the perception of barriers to PrEP. |
| Calabrese et al50 | National September 2014 and February 2015 |
28 semi-structured interviews By region: 1 Midwest 12 Northeast 4 South 1 West |
In person and phone interviews to gain an understating of early adopting providers perspectives to address the risk compensation concerns among other providers | 94% had prescribed PrEP as part of their clinical practice. Participants reported condom usage remained stable before and after PrEP initiation. Three themes emerged from the providers (1) support patient in making informed decision (2) increased risk behavior does not fully offset PrEPs benefits, risk compensation is unfairly stigmatized in healthcare community. |
Findings indicate a need to focus on patient provider relationship to ensure collaboration. Also, implicit bias regarding sexual deviance should be addressed in regards to risk compensation. Discussion regarding PrEP and other risk reduction methods should be included in medical education as PrEP use will still provide some protective benefit to patients even without condoms. Early adopters indicated that with adequate training the majority of physicians would be willing to prescribe, indicating medical education is critical to increasing PrEP. | |
| Krakower et al30 | Boston January to February 2015 |
Recruited 32 PCPs at Fenway Health | Cross sectional survey of PCPs to assess experiences and practices with PrEP provision, as well as perceptions about feasibility and future prescribing intentions | 61 | 100% believed PrEP to be highly efficacious, and 97% had prescribed PrEP to a median of 20 patients. Patient adherence was reported to be high (72% reported very good or excellent). After PrEP initiation, physicians reported of their patients: 42% reported a decrease in condom use, 29% reported more frequent sex with HIV positive persons, and 23% reported more sexual partners. The majority of clinicians described PrEP provision as very or somewhat easy. Only 1 clinician was very unlikely to prescribe PrEP in the future. | Among physicians with experience delivering PrEP they generally acknowledge that prescribing and monitoring are easy. The educational implications of this are the need to expose medical students and residents to PrEP prescribing while in school or residency so that perceived barriers can be dispelled. Screening for STI should be increased among PrEP patients, awareness of drug assistance programs should be included in medical education as well. Risk compensation should not be a reason not to prescribe. |
| Edleman et al43 | National April through May 2015 |
Recruited 250 providers from the Society of General Internal Medicine By region: 123 Northeast 42 West 35 Midwest 49 South |
Cross sectional survey of academic general internists on their willingness to prescribe PrEP through 8 brief patient scenarios. Data was analyzed on high or low willingness to prescribe to individuals with a history of injection drug use | 77 | Providers were most willing to prescribe PrEP to a female or male in a serodiscordant relationship (91%). The lowest willingness to prescribe PrEP was to PWID (74%). The number of HIV-infected clients under physicians care was associated with willingness to prescribe to PWID. | Findings may highlight bias regarding PWID, could also be related to the clear guidelines around MSM prescribing vs hetero and PWID. Again, exposure to treating HIV positive patients seems to increase prescription probability. Actual experience in medical school with HIV positive patients is critical. |
| Krakower et al34 | Boston May-June2012 |
6 focus groups conducted with 39 physicians, physicians assistants and advanced nurse practitioners, all of whom have experience prescribing antiretroviral drugs to HIV infected people. | Semi-structured interview conducted through 6 focus groups. Topic areas included (1) attitudes toward PrEP; (2) barriers and facilitators to prescribing; and (3) influence of guidance for prescribing. |
Participants noted difficulty with adherence, monitoring, and identifying appropriate candidates. Unintended consequences such as resistance and prescription of a potentially toxic drug to a healthy population were noted. The purview paradox was noted as a major barrier to implementation, as well as patients lack of motivation to take the drug. Facilitators of prescription included PrEP efficacy and provision of guidance on prescribing. |
Like previous studies the perceived barriers of PrEP implementation are far greater than the actual barriers. Training needs to focus of having the PCPs that have implemented PrEP in their practice train the ones that have not on what it is actually like to have patients on PrEP and monitoring them for risk compensation, adherence, and side effects. Training PCPs is necessary for the full uptake of PrEP nationally as most patients in need of PrEP do not have access to a specialist. | |
| Blackstock et al40 | National, conducted April-May 2015 | Recruited 246 (8%) PCPs from the Society of General Internal Medicine members of a total of 3093. By region: 39(16%) West 30(12%) Midwest 46(19%) South 117(48%) Northeast 13(5%) Missing |
Cross sectional online survey comparing PrEP adopters to non-adopters. | 87 | Adopters reported higher general PrEP knowledge and knowledge about side effects. Adopters were more likely to report a higher likelihood of prescribing PrEP in the next 6 months, and more likely to perceive PrEP as extremely or moderately safe. Risk compensation also continues to be associated with non-adoption. | Physician education may need to target those without HIV care experience and focus on identifying “clinical champions” that have HIV care experience. Risk compensation and perceived safety should be addressed in medical education to increase PrEP prescribing. |
| Hakre et al39 | National December 2015 |
Recruited 404 United States Air Force PCPs By region: 10 Northeast 187 South 39 Midwest 103 West 63 Outside of Continental US |
Cross sectional online survey assessing PrEP experience, attitudes, and knowledge | 74 | Overall 59% of providers rated their knowledge of PrEP as poor and 72% had never prescribed PrEP or PEP. The majority of providers (64%) believed that PrEP should be offered in the Military Health System. Major concerns were side effects, and discomfort with prescribing drugs for new indications without clear evidence. 55% of patients scored 70% or greater on the knowledge test. | Armed forces physician training could potentially be a new avenue for PrEP prescription. Physicians believe there is a need for PrEP in the Air Force and increasing their knowledge of PrEP and decreasing their erroneous beliefs about the dangers of PrEP may increase prescribing. |
| Blumenthal et al48 | New York, San Diego, and Los Angeles. No dates given |
Recruited 233 HIV providers and non HIV providers from HIV related medical conferences and meetings in 3 high HIV-prevalence cities. By region: 163 West 63 Northeast |
Cross sectional iPad survey comparing HIV providers and non HIV providers’ knowledge, practices, likelihood to prescribe, and barriers and motivators to PrEP | 68 | Average PrEP score was 2.5 (out of 5). Scores were higher for HIV providers than non HIV providers. Northeast providers scored higher than west coast providers (3.0 vs 2.3). 21% of providers had prescribed PrEP and was higher among HIV providers and northeast providers. 64% reported being likely or very likely to prescribe PrEP in the future. Drug toxicity, ARV resistance, and adherence were the major concerns for providers. HIV providers were concerned about risk compensation. More providers reported that HIV clinics should provide PrEP (35%) than non HIV clinics (31%). | Educational interventions involving the use of CME courses may be effective in getting generalists the necessary knowledge to prescribe and monitor patients on PrEP. Training in taking sexual histories is vital to the national implementation of PrEP. Particularly, giving medical students multiple opportunities to collect sexual histories is an important part of increase PrEP prescribing among PCPs. |
For studies prior to 2012, PrEP was prescribed as tenofovir-emtricitabine (TDF-FTC).
Results
Overall, we identified the following 4 overarching barriers to physicians prescribing PrEP: 1. The Purview Paradox (who should prescribe PrEP?), 2. Patient Financial Constraints, 3. Adherence and Fear of ART Resistance, and 4. Perceived Risk Compensation Behavior. The only identified facilitator to PrEP prescribing was physicians serving patients who were seen as high risk. We review each of these areas below.
Purview Paradox
Of greatest significance for primary care physicians is the purview paradox. This barrier refers to the fact that HIV specialists are the most informed and skilled in the delivery of antiretrovirals, whereas primary care physicians are more likely to encounter high risk HIV-negative persons in need of PrEP.31 Primary care physicians often cited the lack of knowledge about antiretroviral medications as a barrier to implementing PrEP in general practice settings.37,40,47
Patient Financial Constraints
Additional barriers to prescribing included perceptions of the lack of financial resources to support prescriptions for PrEP patients,31,42,49 concerns about eliminating the consequences of high-risk behaviors,30,31,34,40,46,48-50 and the need for adherence monitoring.30,34,37,44-49 Prescriptions for PrEP can be expensive, and primary care physicians reported that patients that may benefit most from PrEP often do not have insurance or other means to pay for the prescription without financial assistance.31,42,49 Physicians also expressed concerns about risk compensation, or the idea that patients given PrEP may engage in more risk-taking behaviors as a result of feeling safer from infection30,31,34,40,46,48-50
Adherence and Fear of ART Resistance
Additionally, physician concerns over lack of adherence and subsequent development of drug-resistant strains of HIV were noted as affecting provider prescription behavior in several studies.30-32,34,37,44,46,48,49 In the studies that inquired about prescribing to PWID, lack of adherence specifically due to non-medical drug use was identified as a concern.36,37
Perceived Risk Compensation Behavior
Patients, who fall into elevated-risk group were found to be prioritized for PrEP prescription. An additional finding was a generally higher willingness to prescribe PrEP to sero-discordant couples and/or men identified as MSM. This may be due to a higher rate of these individuals having access to specialized clinics due to partner status or social network access. However, providers expressed less willingness to prescribe PrEP to other known high-risk groups: women with multiple sex partners; people with sexually transmitted infections; and PWID.10,12-14,17 The reviewed studies provide data primarily on barriers to PrEP. Little information regarding facilitators was found, and, to date, no studies provided data on approaches employed in medical schools to train students to prescribe PrEP.
Discussion
The findings of this review indicate the need to address barriers to PrEP provision among physicians practicing medicine in the United States. While knowledge of PrEP as HIV prevention was abundant, the numbers of physicians who had actually prescribed PrEP was low. Many studies reviewed up to 2017 showed <20% of physicians surveyed had ever prescribed PrEP.
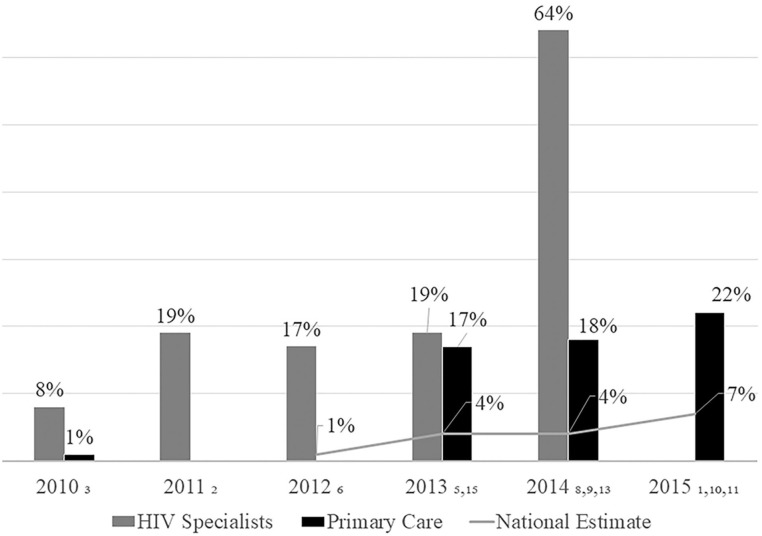
Though there has historically been some confusion over the appropriate purview for PrEP, specialized clinics versus primary care, prescribing rates by primary care physicians have been rising. As noted in Figure 2, a national study of PrEP providers conducted annually from 2009 to 201541 found that HIV specialists are still most likely to prescribe PrEP, but over time, the number of primary care physicians prescribing PrEP has risen steadily. Mirroring this trend, research on barriers faced by primary care physicians to PrEP prescription have also risen.39,40 As these trends continue, it is clear that primary care medical education must address this important preventive tool.
Figure 2.
PrEP prescription by provider type.
Many of the perceptions among primary care physicians limiting their use of PrEP have been found to be misapprehensions. Concern about patient financial constraints was widespread among physicians. However, a wealth of resources is available to support patients who are appropriate candidates for the regimen, including the Patient Advocacy Foundation, Gilead Sciences, and many state-based programs.30 Both medical students and practicing physicians need information about these programs. Additionally, concerns regarding adherence were frequently noted. Adherence must be monitored and encouraged, and regular check-ups should be conducted to identify any adverse consequences from the medication30,34,37,44-49 To achieve this, providers may need to increase their level of non-judgmental patient communication regarding sexual risk.
Other topics that require non-judgmental communication are talking with people about changing desires to use PrEP and experiences with non-adherence. Further, while perceptions of risk compensation and the fear of the development of drug resistant strains of HIV due to inconsistent adherence were identified as major concerns among physicians, neither have been found in the literature of studies of PrEP.18,19,23,24
Patients in sero-discordant couples or self-identified MSM were noted as the most likely to be prescribed PrEP. However, in the U.S., HIV prevalence rates among women with multiple sex partners are second only to MSM, underscoring the potential for women with multiple sex partners to benefit from PrEP.54 In addition, while currently PWID make up a small percentage of the number of new HIV cases, for the latest reporting year (approximately 9% including MSM who also are PWID), 1 in 23 men and 1 in 36 women who inject, respectively will be infected in their lifetime.55 This rate clearly suggests the need for PrEP access among the PWID population. Even though the above-mentioned reports fall within the criteria for HIV PrEP developed by CDC and are currently being implemented in U.S.,55 the CDC guidelines have limitations in supporting PrEP uptake.56 These limitations include incorrect categorization and confounding of sexual orientation, gender identity and risk behavior.56 Education is also needed to ensure that physician stigmatization due to implicit biases of groups that are already marginalized does not create more barriers to health due to limiting PrEP access to these at-risk populations.
Recommendations for Addressing Physician-Identified Barriers
Considering the physician-identified barriers, we make recommendations for how physicians and students may work to increase PrEP knowledge and competence along each stage of the PrEP cascade. We recommend adopting HIV risk assessment as a standard of care, improving physician ability to identify PrEP candidates, improving physician interest and ability in encouraging PrEP uptake, and increasing utilization of continuous care management to ensure retention and adherence to PrEP.
The findings of this review are important to medical education, in that the key barriers to PrEP prescribing identified in the literature can be used to inform the development of PrEP delivery curricula for medical students. In order for PrEP delivery to be improved in real world settings, medical students will need training to identify appropriate candidates for PrEP based on risk assessment, patient data from electronic medical records, and patient preferences for the use of chemoprophylaxis. They will also need to increase their comfort in prescribing and monitoring patient adherence as well as their knowledge about patient assistance programs including: training in cultural humility to address bias towards high-risk HIV populations, practice taking an effective sexual history to identify patients that may be high risk, and overall training in what PrEP is and the benefits of PrEP in order for new physicians to be able to educate and answer patients’ questions surrounding PrEP. Full recommendations have been organized, outlined in Table 2, using the PrEP cascade model,57 to provide medical educators a framework for teaching medical students and residents the requisite knowledge and skills to deliver PrEP in their future practices and for assessing the responsiveness of the health care system for PrEP delivery and adherence. Finally, suggestions as to how to integrate these skills into medical education curricula are offered.
Table 2.
Elements of the PrEP Cascade and Educational Recommendations.
| Steps in PrEP cascade | Educational recommendations |
|---|---|
| At risk for HIV | Utilize health services research projects to familiarize students and residents with local and individual risk. |
| Increase sexual and drug use risk assessment training, make standard of care in teaching hospitals. | |
| Identified as a PrEP candidate | Create algorithms in EHR systems to identify those at high risk for HIV. |
| Address student bias/cultural competence regarding risk populations. | |
| Interest in PrEP | Increase student/resident knowledge of PrEP. |
| Increase community knowledge of PrEP through educational materials, and PrEP testimonials from PrEP users. | |
| Involve students in community education campaigns. | |
| Develop behavioral interventions to increase PrEP interest. | |
| Linked to PrEP | Encourage PrEP delivery by residents, allow students to shadow PrEP delivery sessions. |
| Develop simulated patient encounters to develop student skill in linkage. | |
| Initiate PrEP | Link eligibility criteria based on lab screenings (Cr, Hepatitis B, negative HIV test) to EHR algorithms. |
| Utilize HIV specialist knowledge to train medical students in PrEP delivery. | |
| Disseminate information on patient assistance programs. | |
| Retained in PrEP | Utilize PSR’s and other support staff to ensure retention. |
| Introduce interactive messaging to residents and students as a means to improving retention. | |
| Achieve adherence and persistence | Train students to monitor adherence via self-report adherence measures as standard care. |
| Engage students/residents in having risk reduction counseling with simulated and actual patients. | |
| Increase substance abuse and mental health screening, and referral, perhaps using SBIRT type models. |
Note. Adapted from Liu et al.57
Assessing HIV Risk and Identifying PrEP Candidates
There is an increasing consensus that primary care is the appropriate venue for delivery of this preventive intervention. One key reason for this is that this setting will allow for maximum contact with at-risk patients. This is particularly true in practices that have large populations of MSM, transgender women, sero-discordant couples, women with multiple sex partners, young persons who have multiple partners, and PWID. Delivering PrEP in primary care settings will require provider comfort in obtaining thorough regular sexual histories, frequent HIV testing, and the delivery of HIV prevention messages delivered in culturally appropriate ways to a wider range of patients.
A key factor in the PrEP cascade is the employment of approaches demonstrating cultural humility in working with MSM, transgender, racial/ethnic minorities, and PWID individuals. The impact of intersectionality of race, gender, class, sexuality, and drug use also must be assessed. The outcomes will help individuals, who are discriminated because of layered identities including but not limited to race, gender orientation, social relations, power, oppression etc. Studies of lesbian, gay, bi-sexual, transgender, queer, and intersex (LGBTQI) individuals and PWID individuals seeking medical care have consistently found disparities in health outcomes.24,25,58-62 Patients who identify as LGBTQI frequently report discomfort discussing sex in the health care setting.58,59 One study of medical student responses to at-risk patients found that patient race/ethnicity can play a significant role in the likelihood of students identifying PrEP candidates.60 Combating this will require increased training in sexual history taking, drug use history, cultural humility, and prevention counseling. In addition to the identification of individual risk behaviors, population health data may help identify patients that are part of broader social, sexual, and drug use networks. The addition of algorithms to electronic health records that trigger further screening of at-risk patients for HIV can also be used as a means to help students identify PrEP candidates.
Patient Interest in PrEP
Training in this area builds on risk assessment and identification strategies where physicians are trained to counsel patients effectively about PrEP and engage patients in the process.58-60 Whether training in brief motivational interventions that may assist patients in their increased risk perception and evince individual interest in PrEP is open for speculation.
PrEP Linkage
To facilitate an increase in use of PrEP in primary care settings, medical students must be exposed to training in LGBTQ and PWID affirming health practices. Shadowing PrEP delivery by residents and attending physicians can provide opportunities for medical students to observe PrEP prescribing. Training in this area could include opportunities to observe culturally appropriate language, care provision in a setting that is inviting to MSM, transgender people, and PWID, staff that is knowledgeable about the target populations, as well as opportunities for medical students to identify, reflect on, and address their own implicit and/or explicit biases regarding these populations.
PrEP Initiation
Additional training about antiretrovirals may be necessary for faculty members who are clinical preceptors if primary care is to be the venue for PrEP delivery. PrEP delivery can be discussed as a part of preventive counseling that includes other measures to protect against HIV, HCV, and other STIs. This approach addresses concerns regarding risk compensation, and allows the primary care setting to not only be the hub for PrEP prescription, but also for risk reduction for a broad range of risk-taking behaviors. For students, knowledge of antiretroviral medications can be discussed in year 1 microbiology courses. Pharmacy consultation may be a critical part of this element of training with attention on how resistance to medications is developed. Research describing the actual risk of mutation that weighs this against preventive value can be used in training to diminish this concern.61,62 Rotations through HIV clinics with physicians that have a vast knowledge of antiretrovirals (ARV) can expose medical students to ARV prescribing. This approach is expected to raise awareness of students about the necessary lab tests for PrEP, as well as identifying key issues in maintaining patients on PrEP.
PrEP Retention and Adherence
Medical training in the clinical years should include a focus on regular HIV testing, assessing PrEP side effects, providing ongoing support and risk reduction counseling, monitoring kidney function and conducting regular STI testing as parts of standard care of the PrEP cascade. Monitoring adherence, likewise, is a key element of effective PrEP delivery. Primary care residency training programs might focus on low cost methods (i.e., self-report) for monitoring adherence in the patient-centered medical home (PCMH) clinical settings. This step is expected to keep the PrEP cost low and available and promotes adherence. While self-report surveys have been found to over report adherence, the visual analogue scale has a strong concordance with unannounced pill counts in HIV treatment,63,64 but its validity with PrEP has not yet been demonstrated. On the other hand, dry blood spots which are highly accurate are very costly. As more accurate self-report measures and lower cost, urine and hair assays are developed, medical students should be trained in the most up to date protocols for monitoring patient adherence. Finally, because mental health and substance abuse are factors that affect adherence and retention, medical students should receive training in brief screening and intervention approaches to ensure these barriers do not affect medication adherence. These skills have broad applicability and can easily be integrated into the medical education curriculum in years 1 through 4 along with behavioral health content. The increasing connection between intravenous drug use, sexual risk behavior, and adherence to medication will make this increasingly salient for patients who are on PrEP. It is recommended that clinics, educators and programs ensure representation of people from key populations (TGW and GBMSM) in their cohorts, professional positions and student cohorts. Another recommendation involves working directly in community based, co-development training approaches.
Limitations
The review identified the barriers physicians face in delivering PrEP. At the time of the review (till 2017) no published papers on training efficacy were available. If PrEP is to be a viable preventive measure and realize its potential in ending the HIV epidemic, physicians must be trained to deliver PrEP, and barriers to prescribing PrEP must be addressed in training. Till 2017, few studies have examined the rate of at-risk patients seen by primary care physicians participating in the surveys. Nor do the physicians always know, as members of these groups may not readily identify themselves in a primary care setting. Without asking about physician sexual and drug use history taking, studies assessing rates with which at-risk patients are prescribed PrEP can provide only a rough estimate of the number of people who could benefit from PrEP. Additionally, 2 areas of the PrEP cascade have been neglected in most of the studies: patient interest in PrEP and linkage to PrEP. As a preventive measure, patients may opt out of PrEP even when they may be appropriate candidates, and only 1 of the articles addressed this crucial stage in the PrEP cascade.47 Similarly, only 1 article addressed linkage to PrEP.45 This element of the cascade may be obfuscated by the fact that physicians are not clear on the appropriate venue for delivery and thus may not see linkage as an issue that they must address. Another limitation of our study is that we have stopped our systematic review in 2017 as we had to wrap-up this study and move on to other medical education intervention efforts. Thus, we may have omitted some other studies that may have given us more current information on PrEP. Particularly, contemporary estimates of most training targets (domains) such as knowledge, willingness, comfort, attitude, adherence etc. may have changed in the recent 3 to 4 years since the cessation of our systematic review. Nonetheless, our effort laid a foundation on which further studies could be built to popularize PrEP as an educational intervention in under- and postgraduate medical education and clinical training.
Conclusion
The HIV epidemic will not be halted without innovative approaches that effectively curb HIV transmission rates. While PrEP has become 1 widely available solution, barriers to PrEP provision remain. We present findings from our scoping review as a means for collating physician identified (perceived and actual) barriers and offering up solutions and clarifications for misconceptions that pose as barriers. We recommend adopting HIV risk assessment as a standard of care, improving physician ability to identify PrEP candidates, improving physician interest and ability in encouraging PrEP uptake, and increasing utilization of continuous care management to ensure retention and adherence to PrEP. We hope our actionable recommendations inspire medical educators, students, and practicing physicians to play a greater role in attenuating the HIV epidemic through increased PrEP provision.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UH1HP3048, titled “Academic Units for Primary Care Training and Enhancement.” This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
References
- 1. Prejean J, Song R, Hernandez A, et al. Estimated HIV incidence in the United States, 2006-2009. PLoS One. 2011;6(8):e17502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Spinner CD, Boesecke C, Zink A, et al. HIV pre-exposure prophylaxis (PrEP): a review of current knowledge of oral systemic HIV PrEP in humans. Infection. 2016;44(2):151-158. [DOI] [PubMed] [Google Scholar]
- 3. Anderson PL, Glidden DV, Liu A, et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. 2012;4(151):151ra125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Grant RM, Anderson PL, McMahan V, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14(9):820-829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Siegler AJ, Mouhanna F, Giler RM, et al. The prevalence of pre-exposure prophylaxis use and the pre-exposure prophylaxis-to-need ratio in the fourth quarter of 2017, United States. Ann Epidemiol. 2018;28(12):841-849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Murnane PM, Brown ER, Donnell D, et al. ,; Partners PrEP Study Team. Estimating efficacy in a randomized trial with product nonadherence: application of multiple methods to a trial of preexposure prophylaxis for HIV prevention. Am J Epidemiol. 2015;182(10):848-856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. U.S. CDC. HIV Surveillance Report. CDC; 2013. [Google Scholar]
- 8. Wilson EC, Garofalo R, Harris RD, et al. Transgender female youth and sex work: HIV risk and a comparison of life factors related to engagement in sex work. AIDS Behav. 2009;13:902-913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Garofalo R, Deleon J, Osmer E, Doll M, Harper GW. Overlooked, misunderstood and at-risk: exploring the lives and HIV risk of ethnic minority male-to-female transgender youth. J Adolesc Health. 2006;38(3):230-236. [DOI] [PubMed] [Google Scholar]
- 10. Huang MB, Ye L, Liang BY, et al. Characterizing the HIV/AIDS epidemic in the United States and China. Int J Environ Res Public Health. 2015;13(1):ijerph13010030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas. 2015. Accessed April 5, 2017. https://www.cdc.gov/hiv/statistics/overview/ataglance.html
- 12. Bradley H, Rosenthal EM, Barranco MA, Udo T, Sullivan PS, Rosenberg ES. Use of population-based surveys for estimating the population size of persons who inject drugs in the United States. J Infect Dis. 2020;222(suppl 5):S218-S229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Strathdee SA, Stockman JK. Epidemiology of HIV among injecting and noninjecting drug users: current trends and implications for interventions. Curr HIV/AIDS Rep. 2010;7(2):99106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Abdool Karim Q, Abdool Karim SS, Frohlich JA, et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010;329:1168-1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophy-laxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363:2587-2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Peterson L, Taylor D, Roddy R, et al. Tenofovir disoproxil PrEP Training Systematic Review 16 fumarate for prevention of HIV infection in women: a phase 2, double-blind, randomized, placebo-controlled trial. PLoS Clin Trials. 2007;2:e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Thigpen MC, Kebaabetswe PM, Paxton LA, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367:423-434. [DOI] [PubMed] [Google Scholar]
- 18. Van Damme L, Corneli A, Ahmed K, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med. 2012;367:411-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Choopanya K, Martin M, Suntharasamai P, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo- controlled phase 3 trial. Lancet. 2013;381:2083-2090. [DOI] [PubMed] [Google Scholar]
- 20. Jiang J, Yang X, Ye L, et al. Preexposure prophylaxis for the prevention of HIV infection in high risk populations: a metaanalysis of randomized controlled trials. PLoS One. 2014;9(2):e87674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Okwundu CI, Uthman OA, Okoromah CA. Antiretroviral pre-exposure prophylaxis (PrEP) for preventing HIV in high-risk individuals. Cochrane Database Syst Rev. 2012;7:CD007189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fonner VA, Dalglish SL, Kennedy CE, et al. Effectiveness and safety of oral HIV preexposure prophylaxis for all populations. AIDS. 2016;30(12):1973-1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Marrazzo JM, Ramjee G, Richardson BA, et al. Tenofovir-based pre-exposure prophylaxis for HIV infection among African women. N Engl J Med. 2015;372(6):509-518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mathers BM, Degenhardt L, Ali H, et al. HIV prevention, treatment, and care services for people who inject drugs: a systematic review of global, regional, and national coverage. Lancet. 2010;375(9719):101428. [DOI] [PubMed] [Google Scholar]
- 25. Strathdee SA, Shoptaw S, Dyer TP, Quan VM, Aramrattana A. Towards combination HIV prevention for injection drug users: addressing addictophobia, apathy and inattention. Curr Opin HIV AIDS. 2012;7(4):3205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Campbell JD, Herbst JH, Koppenhaver RT, Smith DK. Antiretroviral prophylaxis for sexual and injection drug use acquisition of HIV. Am J Prev Med. 2013;44(1S2):S63-S69. [DOI] [PubMed] [Google Scholar]
- 27. Koenig LJ, Lyles C, Smith DK. Adherence to antiretroviral medications for HIV pre-exposure prophylaxis: lessons learned from trials and treatment studies. Am J Prev Med. 2013;44(IS2):S91-S98. [DOI] [PubMed] [Google Scholar]
- 28. Ware NC, Wyatt MA, Haberer JE, et al. What’s love got to do with it? Explaining adherence to oral antiretroviral pre-exposure prophylaxis for HIV-serodiscordant couples. J Acquir Immune Defic Syndr. 2012;59(5):463-468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Smith DK, Dearing JW, Sanchez T, Goldschmidt RH. Introducing wicked issues for HIV pre-exposure prophylaxis implementation in the U.S. Am J Prev Med. 2013;44(1 suppl 2):S59-S62. [DOI] [PubMed] [Google Scholar]
- 30. Krakower DS, Maloney KM, Grasso C, Melbourne K, Mayer KH. Primary care clinicians’ experiences prescribing HIV pre-exposure prophylaxis at a specialized community health centre in Boston: lessons from early adopters. J Int AIDS Soc. 2016;19:21165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Tellalian D, Maznavi K, Bredeek UF, Hardy D. Pre-exposure prophylaxis (PrEP) for HIV infection: results of a survey of HIV healthcare providers evaluating their knowledge, attitudes, and prescribing practices. AIDS Patient Care STDs. 2013;27:553-559. [DOI] [PubMed] [Google Scholar]
- 32. White JM, Mimiaga MJ, Krakower DS, Mayer KH. Evolution of Massachusetts physician attitudes, knowledge, and experience regarding the use of antiretrovirals for HIV prevention. AIDS Patient Care STDs. 2012;26:395-405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mimiaga MJ, White JM, Krakower DS, Biello KB, Mayer KH. Suboptimal awareness and comprehension of published pre-exposure prophylaxis efficacy results among physicians in Massachusetts. AIDS Care. 2014;26(6):684-693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Krakower DS, Oldenburg CE, Mitty JA, et al. Knowledge, beliefs and practices regarding antiretroviral medications for HIV prevention: results from a survey of healthcare providers in New England. PLoS One. 2015;10(7):e0132398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Castel AD, Feaster DJ, Tang W, et al. Understanding HIV care provider attitudes regarding intentions to prescribe PrEP. J Acquir Immune Defic Syndr. 2015;70(5):520-528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Adams LM, Balderson BH. HIV providers’ likelihood to prescribe pre-exposure prophylaxis (PrEP) for HIV prevention differs by patient type: a short report. AIDS Care. 2016;28(9):1154-1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bacon O, Gonzalez R, Andrew E, et al. Informing strategies to build PrEP capacity among San Francisco Bay Area clinicians. J Acquir Immune Defic Syndr. 2017;74:175-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Walsh JL, Petroll AE. Factors related to pre-exposure prophylaxis prescription by U.S. primary care physicians. Am J Prev Med. 2017;52(6):e165-e072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hakre S, Blaylock JM, Dawson P, et al. Knowledge, attitudes, and beliefs about HIV pre-exposure prophylaxis among US Air Force Health Care Providers. Medicine. 2016;95(32):e4511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Blackstock OJ, Moore BA, Berkenblit GV, et al. A cross-sectional online survey of HIV pre-exposure prophylaxis adoption among primary care physicians. J Gen Intern Med. 2016;32(1):62-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Smith DK, Mendoza MC, Stryker JE, Rose CE. PrEP awareness and attitudes in a national survey of primary care clinicians in the United States, 2009-2015. PLoS One. 2016;11(6):e0156592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Petroll AE, Walsh JL, Owczarzak JL, McAuliffe TL, Bogart LM, Kelly JA. PrEP awareness, familiarity, comfort, and prescribing experiences among US primary care providers and HIV specialists. AIDS Behav. 2017;21:1256-1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Edelman EJ, Moore BA, Calabrese SK, et al. Primary care physicians’ willingness to prescribe HIV pre-exposure prophylaxis for people who inject drugs. AIDS Behav. 2017;21(4):1025-1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Karris MY, Beekmann SE, Mehta SR, Anderson CM, Polgreen PM. Are we prepped for preexposure prophylaxis (PrEP)? Provider opinions on the real-world use of PrEP in the United States and Canada. Clin Infect Dis. 2014;58(5):704-712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hoffman S, Guidry JA, Collier KL, et al. A clinical home for pre exposure prophylaxis (PrEP): diverse health care providers’ perspectives on the “Purview Paradox”. J Int Assoc Provid AIDS Care. 2016;15(1):59-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Arnold EA, Hazelton P, Lane T, et al. A qualitative study of provider thoughts on implementing pre-exposure prophylaxis (PrEP) in clinical settings to prevent HIV infection. PLoS One. 2012;7(7):e40603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Krakower DS, Ware NC, Maloney KM, Wilson IB, Wong JB, Mayer KH. Differing experiences with pre-exposure prophylaxis in Boston among lesbian, gay, bisexual, and transgender specialists and generalists in primary care: implications for scale-up. AIDS Patient Care STDS. 2017;31(7):297-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Blumenthal J, Jain S, Krakower D, et al. Knowledge is power! Increase provider knowledge scores regarding pre-exposure prophylaxis (PrEP) are associated with higher rates of PrEP prescription and future intent to prescribe PrEP. AIDS Behav. 2015;19(5):802-810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Finocchario-Kessler S, Champassak S, Hoyt MJ, et al. Pre-exposure prophylaxis (PrEP) for safer conception among serodifferent couples: findings from healthcare providers serving patients with HIV in seven US cities. AIDS Patients Care STDs. 2016;30(3):125-133. [DOI] [PubMed] [Google Scholar]
- 50. Calabrese SK, Magnus M, Mayer KH, et al. Support your client at the space that they’re in”: HIV pre-exposure prophylaxis (PrEP) prescribers’ perspectives on PrEP-related risk compensation. AIDS Patient Care STDs. 2017;31(4):196-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573-577. [DOI] [PubMed] [Google Scholar]
- 52. Fortin M, Stewart M, Poitras M-E, Almirall J, Maddocks H. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med. 2012;10(2):142-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32 item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349-357. [DOI] [PubMed] [Google Scholar]
- 54. Adimora AA, Ramirez C, Poteat T, et al. HIV and women in the USA: what we know and where to go from here. Lancet. 2021;397(10279):1107-1115. [DOI] [PubMed] [Google Scholar]
- 55. US Centers for Disease Control and Prevention, US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States–2017 update: a clinical practice guideline. Accessed October 10, 2018. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf
- 56. Calabrese SK, Willie TC, Galvao RW, et al. Current US guidelines for prescribing HIV pre-exposure Prophylaxis (PrEP) disqualify many women who are at risk and motivated to use PrEP. J Acquir Immune Defic Syndr. 2019;81(4):395-405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Liu A, Colfax G, Cohen S, et al. The spectrum of engagement in HIV prevention: proposal for a PrEP cascade. In: 7th International Conference on HIV Treatment and Prevention Adherence, Miami Beach, FL, 2012. Accessed April 5, 2021. http://www.iapac.org/AdherenceConference/presentations/ADH7_80040.pdf [Google Scholar]
- 58. Dilley JA, Simmons KW, Boysun MJ, Pizacani BA, Stark MJ. Demonstrating the importance and feasibility of including sexual orientation in public health surveys: health disparities in the Pacific Northwest. Am J Public Health. 2010;100(3):460-467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Fredriksen-Goldsen KI, Kim HJ, Barkan SE, Muraco A, Hoy-Ellis CP. Health disparities among lesbian, gay, and bisexual older adults: results from a population-based study. Am J Public Health. 2013;103(10):1802-1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Calabrese SK, Earnshaw VA, Underhill K, Hansen NB, Dovidio JF. The impact of patient race on clinical decisions related to prescribing HIV pre-exposure prophylaxis (PrEP): assumptions about sexual risk compensation and implications for access. AIDS Behav. 2014;18(2):226-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Quinn GP, Sanchez JA, Sutton SK, et al. Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning (LGBTQ) populations. CA Cancer J Clin. 2015;65(5):384-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Conron KJ, Mimiaga MJ, Landers SJ. A population-based study of sexual orientation identity and gender differences in adult health. Am J Public Health. 2010;100(10):1953-1960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Lehman DA, Baeten JM, McCoy CO, et al. Risk of drug resistance among persons acquiring HIV within a randomized clinical trial of single- or dual-agent preexposure prophylaxis. J Infect Dis. 2015;211(8):1211-1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Kalichman SC, Amaral CM, Swetzes C, et al. A simple single item rating scale to measure medication adherence: further evidence for convergent validity. J Int Assoc Provid AIDS Care. 2009;8(6):367-374. [DOI] [PMC free article] [PubMed] [Google Scholar]