Abstract
Robotic-assisted total knee arthroplasty (RA-TKA) has shown improved reproducibility and precision in mechanical alignment restoration, with improvement in early functional outcomes and 90-day episode of care cost savings compared to conventional TKA in some studies. However, its value is still to be determined.
Current studies of RA-TKA systems are limited by short-term follow-up and significant heterogeneity of the available systems.
In today’s paradigm shift towards an increased emphasis on quality of care while curtailing costs, providing value-based care is the primary goal for healthcare systems and clinicians. As robotic technology continues to develop, longer-term studies evaluating implant survivorship and complications will determine whether the initial capital is offset by improved outcomes.
Future studies will have to determine the value of RA-TKA based on longer-term survivorships, patient-reported outcome measures, functional outcomes, and patient satisfaction measures.
Cite this article: EFORT Open Rev 2021;6:252-269. DOI: 10.1302/2058-5241.6.200071
Keywords: RA-TKA, robotic-assisted total knee arthroplasty, total knee arthroplasty
Introduction
As value in healthcare has shifted to a measurement of quality relative to the cost, there is a greater emphasis on improving clinical and functional outcomes and patient satisfaction.1 This is especially relevant in elective primary total knee arthroplasty (TKA), which is one of the most commonly performed surgical procedures in the United States and has projected exponential growth in the upcoming decade.2–5 Increased long-term survival, functional outcomes and satisfaction following TKA are therefore becoming more important to both the patient and the healthcare system as a whole. Despite marked advances in implant designs, surgical techniques, and postoperative rehabilitation programmes, multiple studies demonstrate that nearly 20% of patients remain dissatisfied with their overall outcomes after primary TKA.6–15
Dissatisfaction is believed to be multifactorial and secondary to component malposition, patient selection and establishing expectation management preoperatively.16 Since component positioning, alignment and equal soft tissue balance are critical for a successful TKA,17 malalignment in the coronal, sagittal and rotational planes continues to increase implant failure rates and cause poor clinical outcomes.16–19 Bone cutting inaccuracies up to 4° in the coronal plane and 11° in the sagittal plane have been reported to occur during conventional primary TKA, with guide movement contributing to 10–40% of the total cutting error.17,20–22 Therefore, TKA technological development, including computer-assisted navigation (CAN), has focused on surgical technique improvement to reliably identify overall limb alignment and to assist in guide placement for bony cuts. However, medium-term and long-term CAN-TKA clinical function outcomes and survivorship have been shown to be similar to conventional TKA despite improved radiographic alignment and fewer outliers achieved with navigation assistance.23–26
The global medical robotic market that was valued at $7.24 billion in 2015 is projected to grow to $20 billion by 2023.27 The most important factor fuelling the market growth is the overall superior economic and social advantage of medical robots over traditional human operators with added procedural value.27 Robotic-assisted TKA (RA-TKA) has gained momentum within the past 10 years to better control surgical variables by mitigating technical errors caused by insecure cutting guides and imprecise bone cuts.28 Studies have also shown superior results with RA-TKA versus CAN-TKA, with shorter operative duration, less coronal/sagittal deviation and increased accuracy of mechanical axis alignment restoration.16,29,30 Newer robotic platforms have further evolved to allow clinicians to track patient experience and outcomes throughout the perioperative period with the collection of validated patient-reported outcome measures (PROMs).31–33 This comprehensive review investigates the advent of robotic navigation, historical and commercially available systems, learning curve, clinical outcomes, cost-analysis and limitations to better understand the value of RA-TKA.
Robotic total knee arthroplasty systems
History
Since the first CAN arthroplasty procedure in 1997, the use of technology in TKA has grown tremendously in an attempt to improve surgical technique for more reliable component placement and alignment.34 CAN technology utilizes either infrared (IR) or electromagnetic (EM) registration signalling that facilitated real-time feedback for instrumentation positioning and bony resection.35–37 However, both modalities had limitations with line of sight and metal intereference.16,35–37 Despite these innovations, long-term study of the first 26 CAN-TKA demonstrated only 85% patient satisfaction without significant improvement in implant survivorship compared to conventional TKA at 10-year mean follow-up.38
The first surgical robot system was introduced in 1985 based on computed tomography (CT) imaging for neurosurgical biopsies.39 This robot’s initial success sparked interest in other surgical fields with robotic transurethral prostate resections in 1989.39 The hypothesized advantages included an increase in three-dimensional (3D) accuracy, increased reproducibility of commonly performed procedures, and increased precision of movements mimicking the motion of the operating surgeon.40 By the late 1980s, surgeons began to appreciate the potential advantages of surgical robots compared with computer navigation alone, with the most potential in neurosurgery and orthopaedic surgery. The first orthopaedic robotic-assisted system, the ROBODOC system (THINK Surgical Inc., Fremont, CA, USA), was developed in 1986 and was used for cementless total hip arthroplasty (THA) in 1992.41 During the past two decades, enthusiasm for robotic-assisted total joint arthroplasty (TJA) has grown tremendously.16
Passive, active and semi-active
CAN-TKA systems delineate patient anatomical data and provide objective real-time feedback on guide placement for optimal bone resection and implant placement. However, CAN does not actively control or restrain the surgeon in performing any aspect of the procedure. RA-TKA systems utilize computer software while incorporating advanced imaging to provide a virtual patient-specific 3D reconstruction of the knee. The surgeon calculates the optimal bony resection and final component placement and alignment on the robotic computer software. An intraoperative robotic device physically assists the surgeon in executing the preoperative plan with a high level of precision and accuracy.42–48 Every robotic design has a different level of constraint and haptic feedback, and designs are classified as either passive, active or semi-active systems.
Passive modalities are under direct and continuous surgeon control. Contrarily, active robotic platforms perform a designated task completely independent of the surgeon. Semi-active systems provide the surgeon with tactile feedback with procedural safe-guards to ensure accuracy and safety against iatrogenic soft tissue or neurovascular injury.16,49 Semi-active modalities utilize haptic feedback through auditory, tactile or visual cues that alert the surgeon about deviations from the preoperatively defined parameters.16,49 This helps mitigate excessive or uneven bony resection and component malpositioning. Semi-active robots also self-regulate instrumentation to either slow down or completely stop when deviation outside the computer-generated volume or depth of a defined bone resection occurs. The main robotic-assisted systems historically used are summarized in Table 1.
Table 1.
Historical robotic-assisted TKA systems.
| Name | Manufacturer | Introduction year | Manufacturer acquisition | Platform | Indication | Type | Technique | Image | Results |
|---|---|---|---|---|---|---|---|---|---|
| CASPAR | Orto-Maquet URS, Schwerin, Germany |
1997 | Smith & Nephew (Memphis, TN) acquired in 2001 | Open | THA TKA |
Active | • Milling • CASPAR’s active system utilized preoperative CT scans which occurred after an index procedure to place self-tapping bicortical screws as fiducial markers.57 • The robotic arm performed bony preparation with bone milling based on the preoperative template, fiducial markers and intraoperative anatomic registration. |
CT | • Seibert et al57 were the first to report this technology and compared 70 CASPAR TKA patients with a historical control group of 50 conventional TKA patients and found the postoperative tibiofemoral alignment was within 0.8° (0–4.1°) of the preoperative template compared to 2.6° (0–7°) in the conventional historical control cohort.57
• After initial success, CASPAR’s TKA platform had poor early clinical outcomes with a high incidence of complications and is no longer commercially available.57,58 |
| Acrobot | Imperial College of London | 1988 | Stanmore Sculptor System (London, England) acquired in 2010 MAKO Surgical acquired the technology in 2013 |
Closed | UKA TKA |
Semi-active | • Saw • Acrobot’s robotic arm attached to the operative bed and used haptic feedback to allow the surgeon to make precise bone cuts. • This was the first system to introduce haptic response, which paved the way for more contemporary robotic systems. |
CT | • In a randomized control trial, Cobb et al63compared 13 UKA performed with Acrobot versus 14 UKA patients performed conventionally. All of the Acrobot UKA patients had coronal tibiofemoral alignment within 2 degrees of the planned position while only 40% of the conventional cohort achieved similar accuracy. • The authors also found a trend towards but not achieving statistically significant functional outcome improvement with better Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and Knee Society Scores (KSS) at six weeks and three months (p > 0.05).63 • Although preliminary TKA found similar accurate results, Stanmore Sculptor System withdrew from robotic platforms when MAKO Surgical acquired the technology in 2013.58 |
| PiGalileo | Plus Orthopedics AG, Rotkreuz, Switzerland | – | Smith & Nephew acquired technology in 2007 | Closed | TKA | Passive | • Cutting guide • The passive robotic system was computer-controlled and motor operated two-axis positioning device was mounted onto the medial and lateral distal femoral shaft to aide in jig placement.58,60,61 |
CT | • Matziolis et al62 examined the spatial implant positioning of 28 TKAs performed traditionally versus 32 TKAs using an imageless computer-assisted system with a mini robot (PiGalileo System, Plus Orthopedics AG, Smith & Nephew, Rotkreuz, Switzerland). |
| • The mini robotic unit did not itself actively perform any cutting operations, but positioned the saw guide for a conventional oscillating saw.61
• The platform was also accompanied with a motorized ligament balancer to aid in soft tissue balancing for surgeons who performed TKA using a gap-balancing technique. |
• The overall mechanical axis was between 4.8° of valgus and 6.6° of varus alignment in the coronal plane for conventional TKA compared with a smaller range (2.9° of valgus and 3.1° of varus alignment) for the computer navigation with a robot cohort (p = 0.004). • The authors further concluded that CAN with a mini robot improved coronal and sagittal femoral component alignment but showed no difference in tibial implant positioning. • Other studies using the PiGalileo system using both measured resection and gap-balancing showed no difference in implant survivorship or functional outcomes with equivocal KSS, Functional KSS (FKSS) and Oxford Knee Scores (OKS) at mid-term follow-up (p > 0.05).105,106 • Plus Orthopedics was acquired by Smith & Nephew in 2007 and the PiGalileo system was subsequently discontinued. |
Note. CASPAR, computer-assisted surgical planning and robotics; Acrobot, The Active Constraint robot; UKA, unicompartmental knee arthroplasty; TKA, total knee arthroplasty; THA, total hip arthroplasty; CT, computed tomography; CAN, computer-assisted navigation; KSS, Knee Society Score.
Image-based versus imageless
Each robotic system requires preoperative plain radiographs or advanced imaging such as CT scan or magnetic resonance imaging (MRI) scans to use in a mapping process to virtually recreate the knee for preoperative and intraoperative planning. The desired resection angle, resection depth, overall limb alignment and implant positioning can be predetermined and set preoperatively onto the robot’s computer software. The robot implements the predetermined surgical plan to either position cutting guides or to assist in bony cuts. Preoperative imaging allows consideration of the patient’s distinct anatomy which serves as a checkrein for accurate implant placement and allows template adjustment as needed. However, additional increased cost, burden of obtaining additional imaging and increased radiation exposure are potential drawbacks. Furthermore, preoperative CT exposure can have a radiation effective doses greater than 100 mSv, which is significantly greater than the Food and Drug Administration (FDA)’s warning of increased malignancy with effective radiation doses greater than 10 mSv.16,50 CT-based robotic platforms often require lengthy preoperative planning, potential inconvenience to both patients and providers along with the reliance on an external engineer for preoperative planning and formatting. However, the advancements of imageless systems as well as the adoption of low-dose CT protocols may help mitigate these risks and further streamline the process.
Though imageless modalities reduce overall operative time and radiation exposure, as well as being more convenient for patients compared to image-based systems, imageless systems are only as accurate as the operator’s bony landmark registration and may introduce an error margin. Patients with significant deformity or bone loss may have altered anatomic landmarks which can pose a challenge during registration for the robotic software. However, studies comparing imageless versus CT-based imaging robotic platforms demonstrate no difference in reliability with landmarking and implant positioning.51–53 There are only two systems in the US that utilize an imageless robotic platform: Navio Surgical System (Smith & Nephew, Memphis, TN, USA)54 and OMNIBotics for gap balancing (Corin, Raynham, MA, USA).55
Open versus closed platforms
The majority of available robotic systems in the US are regarded as closed platforms. Closed platform systems are only compatible with specific vendor implants.47 This may hinder some surgeons in adopting robotic technology if they have a preference towards an implant that does not have a robotic platform. Open platform systems are more appealing due to accommodation of a wide variety of prosthesis designs from multiple different manufacturers. Although open platforms provide a convenience for incorporated 3D implant data for numerous implant systems, they may lack the depth of biomechanical kinematic data present in closed platforms that use proprietary implants.56 Currently, TSolution-One (THINK Surgical Inc, Fremont, CA, USA) is the only RA-TKA system on the market with an open platform.56
Historical TKA robotic systems
Early generation RA-TKA systems were introduced in Europe in the late 1980s as active systems. After surgical exposure was performed, the active robots completed the predefined plans without operator intervention. However, the older generation robots added tremendous surgical time and were associated with higher blood loss.57,58 These early systems had poor early clinical outcomes with high rates of failure and subsequently fell out of favour.57,58 Tactile systems with haptic feedback and overall technological improvements addressed some of the mechanisms of failure of older active platforms, such as soft tissue protection.59 Early generation tactile systems demonstrated increased implant alignment and placement accuracy with more consistent ligament soft tissue balance.60–62 Radiological and clinical outcome improvement increased the popularity and paved the way for newer generation modern RA-TKA platforms.58,63 Historical robotic-assisted systems are summarized in Table 1.
Contemporary TKA robotic systems
Active systems
TSolution-One® (active system – milling/requires CT imaging)
ROBODOC®(Curexo Technology, Fremont, CA, USA), the earliest active robot system used in arthroplasty, was the first FDA-approved robotic technology in orthopaedic surgery.16 In 2014, THINK Surgical Inc. acquired Curexo Technology and introduced the next generation open robotic system, TSolution-One Surgical System, which successfully obtained FDA clearance for TKA in 2019. TSolution-One is an active-autonomous, CT-based system that helps recreate overall desired limb alignment through an image-based preoperative planning system (Fig. 1). The open platform system helps the surgeon design a preoperative template based on the surgeon’s desired prosthesis.56
Fig. 1.

TSolution-One® System, THINK Surgical Inc, Fremont, California.
Source: Adapted from Liow MHL, Chin PL, Pang HN, Tay DK, Yeo SJ. THINK surgical TSolution-One (Robodoc) total knee arthroplasty. SICOT J 2017;3:63.
ROBODOC’s robot-assisted arm and 3D planning workstation were rebranded as TCAT® and TPLAN® respectively.56 The system retains the active bone milling functionality of the ROBODOC and a rigid mating framework has been incorporated to minimize outside reference range errors due to patient positioning (Fig. 2).56 Compared with its predecessor, TSolution-One is fiducial free and uses a digitizer to locate the exact position of the patient’s anatomy to mill joint surfaces for component placement.16 The TCAT® robotic-assisted tool proceeds to complete all femoral and tibia bone cuts with a robotic milling device.56 Although the surgeon maintains control over the milling tool with a manual override button and is responsible for soft tissue protection, the robot completes the bony preparation steps independently with consistent water cooling irrigation and removal of milling debris without the ability for intraoperative adjustments while the preoperative plan is executed.16,56
Fig. 2.
TCAT® bone milling tool preparing the femur.
Source: Adapted from Liow MHL, Chin PL, Pang HN, Tay DK, Yeo SJ. THINK surgical TSolution-One (Robodoc) total knee arthroplasty. SICOT J 2017;3:63.
Earlier studies demonstrate increased risk of complications during the learning phase of active robotic systems. Although ROBODOC had greater mechanical axis alignment restoration accuracy compared to conventional TKA, Park and Lee42 reported six of their initial 32 active robotic TKA procedures had short-term complications including superficial infection, patellar tendon ligament rupture, patella dislocation, supracondylar fracture and patellar fracture and common peroneal injury. Compared with ROBODOC, TSolution-One has shown improved preliminary clinical outcomes with excellent radiological results.56 Multiple studies comparing TSolution-One TKA and conventional TKA demonstrate 0% mechanical axis deviators in the robotic cohort.47,56 However, there are no published long-term clinical outcomes of TSolution-One TKA, with short and medium-term studies demonstrating no significant difference in functional outcomes when compared to conventional TKA.47,48,56
ROSA® (active system – cutting guide/requires X-ray imaging)
ROSA® Knee System (Zimmer-Biomet, Warsaw, IN, USA) is an active, closed platform robotic arm that aides in placement of the cutting block and dynamic ligament balancing.64 Preoperative full-length lower-extremity radiographs are converted intraoperatively to 3D images using X-Atlas™ software that has a reported accuracy of within 1 mm for the resection thickness and 0.4 mm for angle measurement.64,65 After bony registration, the native flexion and extension gaps are assessed to determine depth of bony resection and planned implant positioning and alignment (Fig. 3). The plan is executed with the robotic arm locking the cutting jig in the desired position for manual bone resection with a conventional oscillating saw.64,65 This system received FDA clearance in 2019 and a strategic roll-out of the robot has limited further clinical studies.
Fig. 3.
(A) ROSA for total knee arthroplasty. (B) ROSA’s computer software for preoperative and intraoperative planning based on implant positioning and soft tissue tensioning. (C) ROSA arm attaching cutting block for femoral cut.
Source: Adapted from Zimmer-Biomet, Warsaw, IN, USA.
Semi-active systems
Mako® (semi-active system – saw/requires CT imaging)
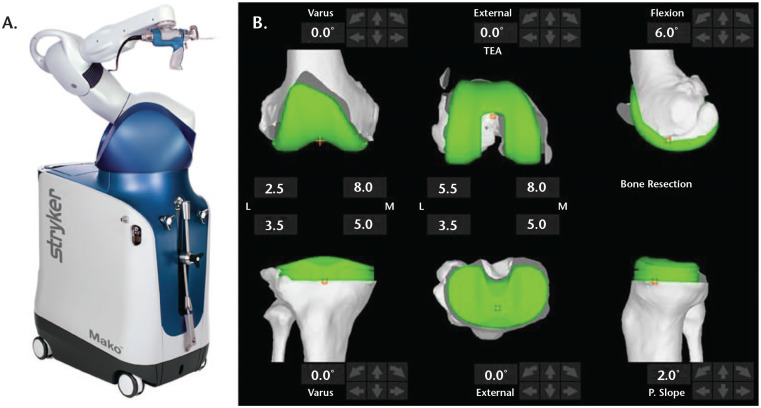
The Mako® robotic-arm closed platform system (Stryker Orthopaedics, Mahwah, NJ, USA) was introduced in 2005 and was acquired by Stryker Orthopaedics with Mako Surgical Corporation in 2013.66 The CT-based TKA system integrates the robotic-arm-guided saw blade and the preoperative plan with set implant position and alignment with anticipated bony resection thicknesses (Fig. 4). The intraoperative bony registration does not require rigid stabilization that may be needed in other robotic designs and allows for dynamic femur and tibia tracking.67 After landmark registration, implant positions are adjusted on the computer software to target equal flexion and extension gaps and overall limb alignment. The robotic arm is used to perform bony cuts with haptic feedback if the saw deviates beyond the predetermined cutting zones.58,63,67
Fig. 4.
(A) Mako robot for total knee arthroplasty. (B) Mako’s computer software for preoperative templating that allows the surgeon to position the implant over the preoperative CT scan to obtain optimal positioning and alignment. The central numbers are the bony depth of resection in millimetres from the medial and lateral distal femur and posterior condyles.
Source: Adapted from Stryker Orthopedics, Mahwah, NJ, USA.
Most of the literature evaluating RA-TKA efficacy involves Mako studies reporting radiological and clinical outcomes, surgical efficiency and cost-effectiveness as it was one of the earliest newer generation systems to receive FDA clearance for unicompartmental knee arthroplasty (UKA), TKA and THA.68 Medium-term and long-term studies are warranted to continue to evaluate implant longevity, complications, functional outcomes and patient satisfaction after Mako TKA.
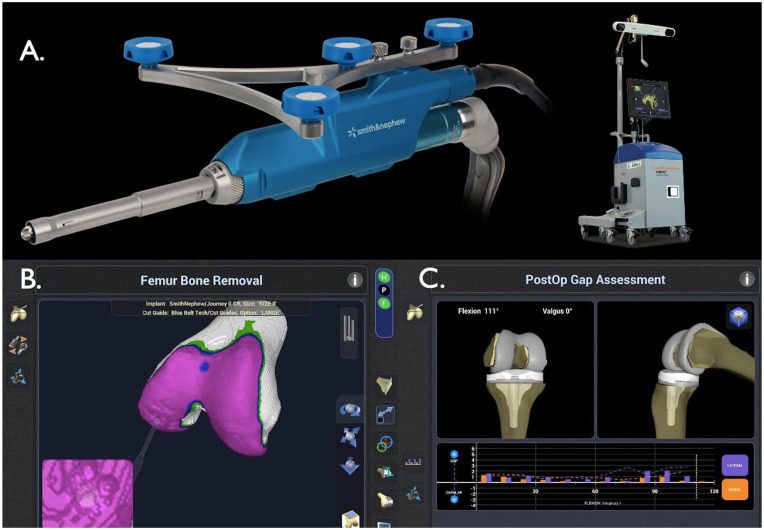
Navio® surgical system (semi-active system – burring/image free)
Blue Belt Technologies (Plymouth, MN, USA) introduced and received FDA clearance for Navio® Surgical System (Smith & Nephew, Memphis, TN, USA) for UKA and patellofemoral arthroplasty (PFA) in 2012. Shortly after being acquired by Smith & Nephew in 2016, the robotic platform acquired FDA approval for TKA in 2017.16 Navio is a closed platform, semi-autonomous, hand-held end-cutting burr that allows the surgeon to perform predefined bone cuts using imageless registration digital-based reference points (Fig. 5).58 Similar to Mako, preset boundaries prevent excessive resection while the robotic tool alters the burr speed and retracts the burr tip to prevent errors; however, a potential lag time between burr tip retraction and speed change may pose problems.16,58 The imageless system eliminates preoperative imaging cost and associated radiation exposure.
Fig. 5.
(A) Navio and its computer software for total knee arthroplasty. (B) Burring for femoral component preparation. (C) Intraoperative gap assessment while trialling implants.
Source: Adapted from Smith & Nephew, Memphis, TN, USA.
Although there are few studies on Navio UKA demonstrating improved alignment without any difference in revision rates,54,69 there are currently no reports, to our knowledge, on short or long-term data for Navio TKA. Currently, there is an ongoing prospective randomized controlled trial evaluating conventional versus Navio TKA with an estimated completion date of December 2022.70
OMNIBotic® (semi-active system – cutting guide/requires CT imaging)
OMNIBotic® (Corin, Tampa, FL, USA) closed platform system, previously known as PRAXIM Robotic-assisted navigation, was FDA approved for TKA in 2017. After intraoperative registration, the OMNIbot robotic cutting guide is mounted onto the bone, similar to the ROSA (Zimmer-Biomet, Warsaw, IN, USA). The BalanceBot is used in conjunction with the cutting guide and is the first and only robotic soft tissue balancer available on the market (Fig. 6).71 The robotic lamina spreader measures soft tissue tension throughout the range of motion after the tibial cut and prior to any femoral cuts.71 The robot consists of two autonomous motorized actuators with integrated force sensors.71,72 The soft tissue tension data help plan femoral component rotation and position that optimizes symmetric flexion and extension gaps with minimal soft tissue releases. The main robotic-assisted systems currently used are summarized in Table 2.
Fig. 6.
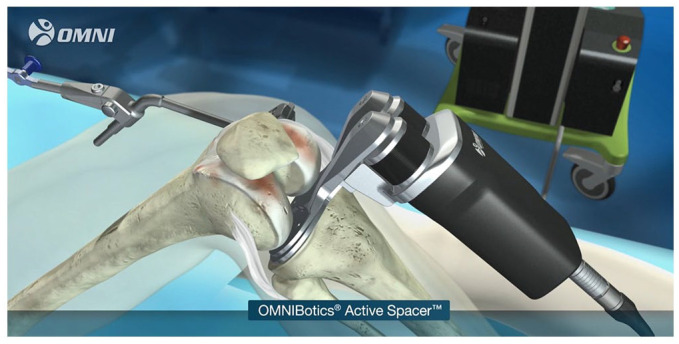
BalanceBot robotic soft tissue balancer (formerly OMNIBotics active spacer).
Source: Adapted from Siddiqi A, Smith T, Mcphilemy JJ, Ranawat AS, Sculco PK, Chen AF. Soft-tissue balancing technology for total knee arthroplasty. JBJS Rev 2020;8:e0050.
Table 2.
Main robotic-assisted TKA systems in the United States.
| Name | Manufacturer | Introduction year | Platform | Indication | FDA clearance | Type | Technique | Image | Current Status |
|---|---|---|---|---|---|---|---|---|---|
| TSolution-One | THINK Surgical Inc. Fremont, CA |
2015 | Open | THA, TKA |
THA: 2015 TKA: 2019 |
Active | Milling | CT | Currently used |
| ROSA | Zimmer Biomet Warsaw, IN |
2018 | Closed | TKA | 2019 | Active | Cutting guide | XR | Limited release |
| Mako | Stryker Mahwah, NJ |
2005 | Closed | UKA PFA TKA THA |
2015 | Semi-active | Saw burr |
CT | Currently used |
| Navio | Smith & Nephew Memphis, TN |
2012 | Closed | UKA PFA TKA |
2017 | Semi-active | Burring | Image Free | Currently used |
| OMNIBotic BalanceBot | Corin Tampa, FL |
2004 | Closed | TKA | 2017 | Semi-active | Cutting guide | CT | Currently used |
| Orthotaxy | DePuy Synthes Warsaw, IN |
– | Closed | UKA TKA |
– | Semi-active | Saw | N/A | Awaiting product launch |
| CORI | Smith & Nephew Memphis, TN |
– | Closed | UKA TKA |
– | Semi-active | Burring | Image free | Awaiting product launch; TKA release planned fall 2020 |
Note. UKA, unicompartmental knee arthroplasty; PFA, patellofemoral arthroplasty; TKA, total knee arthroplasty; THA, total hip arthroplasty; CT, computed tomography; NJ, New Jersey; TN, Tennessee; FL, Florida; CA, California; IN, Indiana; XR, X-ray.
Learning curve
The RA-TKA learning curve is critical to understand the impact on surgical workflow and duration. Kayani et al73 reported on the RA-TKA learning curve by assessing surrogate operative and radiological markers in 60 conventional TKAs followed by 60 RA-TKA, and found the learning curve was seven cases for operative times (p = 0.01) and surgical team anxiety levels (p = 0.02). There was no learning curve effect for achieving planned femoral and tibial positioning (p < 0.001) and limb alignment (p < 0.001) without additional risk of postoperative complications. Similarly, Sodhi et al74 found the operative times for RA-TKA were increased for an initial 20 cases in two fellowship-trained arthroplasty surgeons but comparable to conventional TKA afterwards in both surgeons. Although operative times are increased in the learning phase of RA-TKA, surgical workflow appears to be comparable to traditional TKA after proficiency has been achieved.60
Clinical outcomes
Regardless of the improved accuracy of robotic-assisted TKA, it is important to determine whether the improved precision impacts functional outcomes and implant survivorship. Although robotic technology has been present for over a decade with an increasing market penetration, there are relatively few medium-term or long-term studies assessing the impact of robotic assistance on these outcome measures. However, comparative short-term findings are promising.46,75–80 In a retrospective study, Siebert et al57 compared 70 RA-TKA patients versus 50 conventional TKA patients and observed reduced postoperative soft tissue swelling in the robotic cohort. Periarticular soft tissue preservation with minimal releases and decreased surrounding tissue injury in RA-TKA may limit local inflammatory response resulting in decreased pain and postoperative swelling.60,81–83 Similarly, Kayani et al84 found RA-TKA patients to have less postoperative pain, decreased perioperative analgesia requirements, and reduced physical therapy duration compared to conventional TKA.
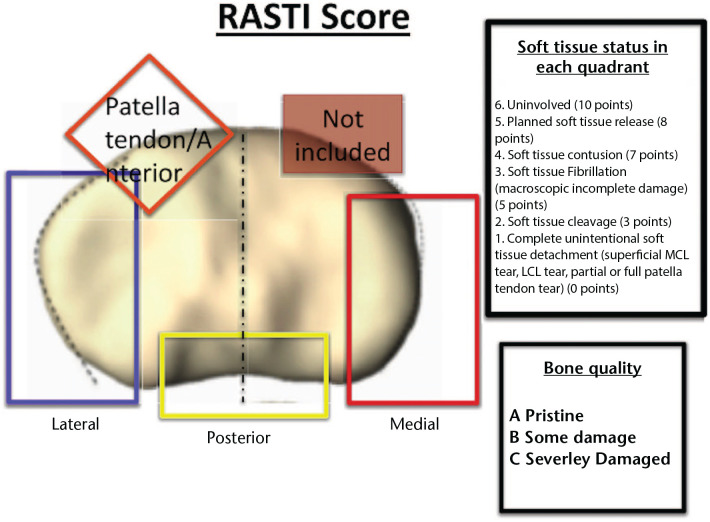
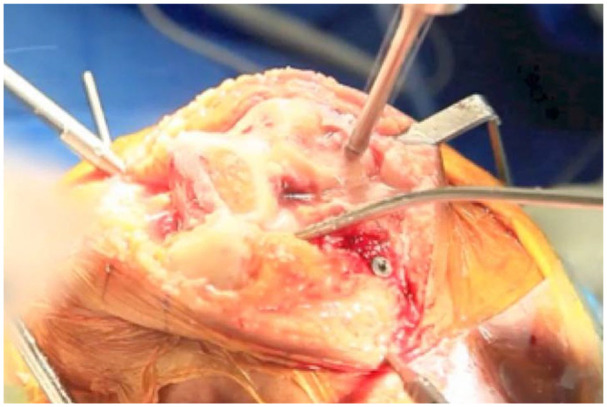
Another study comparing 30 conventional TKA with 30 RA-TKA demonstrated that RA-TKA had reduced medial soft tissue injury in passively correctable (p < 0.05) and fixed varus deformities (p < 0.05), more accurate femoral and tibia bone cuts (p < 0.05), and less macroscopic soft tissue injury (MASTI) compared with conventional TKA (Fig. 7).85 This decreased swelling after RA-TKA may be an implication of greater initial postoperative range of motion compared to conventional TKA. A multicentre study found that patients undergoing RA-TKA experienced a significant 4.5-fold decrease in manipulation under anaesthesia rates (p = 0.032).86 Subsequently, a systematic review and meta-analysis of five studies with 323 RA-TKAs and 251 traditional TKAs, Ren et al87 reported improved Knee Society Score (KSS) functional scores and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores in the robotic group at six-month follow-up.
Fig. 7.
Diagrammatic representation of the macroscopic soft tissue injury (RASTI) score showing tibial plateau in the axial plane.
Source: Adapted from Kayani B, Konan S, Pietrzak JRT, Haddad FS. Iatrogenic bone and soft tissue trauma in robotic-arm assisted total knee arthroplasty compared with conventional jig-based total knee arthroplasty: a prospective cohort study and validation of a new classification system. J Arthroplasty 2018;33:2496–2501.
However, improved implant positioning and alignment with robotic TKA have not rendered any difference in medium-term to long-term functional outcomes compared to conventional TKA.60 Song et al47 and Liow et al88 both reported no difference in Hospital for Special Surgery (HSS), WOMAC, Oxford Knee Score (OKS) and KSS scores between robotic TKA and traditional TKA at minimum two-year follow-up. Similarly, recent long-term studies found no difference in HSS, WOMAC, OKS or Short-Form 12 (SF-12) scores at minimum 10-year follow-up.89,90 A recent prospective, randomized controlled trial also found no differences between RA-TKA and conventional TKA in terms of functional outcome scores, aseptic loosening, overall survivorship and complications at minimum 10-year follow-up.91 Current studies regarding clinical outcomes after RA-TKA are summarized in Table 3.
Table 3.
Clinical outcomes after robotic-assisted total knee arthroplasty.
| Study | Year | Studies (#) | System | Robotic cases (#) | Conventional cases (#) | Follow-up in months | Conclusions | Level of evidence | Grade of recommendation |
|---|---|---|---|---|---|---|---|---|---|
| Song et al47 | 2013 | 1 | ROBODOC | 50 | 50 | 41 | No differences in postoperative ROM, WOMAC scores, and HSS knee score. | 1 | A |
| Liow et al28 | 2014 | 1 | ROBODOC | 31 | 29 | 6 | At 6-month follow-up, there was no overall difference in terms of clinical outcome measures, except in SF-36 vitality scores, where the robot-assisted group reported higher vitality scores. | 1 | A |
| Liow et al88 | 2017 | 1 | ROBODOC | 31 | 29 | 24 | Both robotic and conventional TKA displayed significant improvements in majority of the functional outcome scores at 2 years. Despite having a higher rate of complications, the robotic-assisted group displayed a trend towards higher scores in SF-36 QoL measures, with significant differences in SF-36 vitality (p = 0.03), role emotional (p = 0.02) and a larger proportion of patients achieving SF-36 vitality MCID (48.4% vs. 13.8%, p = 0.009). No significant differences in KSS, OKS or satisfaction/expectation rates were noted. | 1 | A |
| Kim et al91 | 2020 | 1 | ROBODOC | 975 | 990 | 120 | At a minimum follow-up of 10 years, there were no differences between robotic-assisted TKA and conventional TKA in terms of functional outcome scores, aseptic loosening, overall survivorship, and complications. Considering the additional time and expense associated with robotic-assisted TKA, we cannot recommend its widespread use. | 1 | A |
| Kayani et al107 | 2018 | 1 | Mako | 40 | 40 | 1 | Robotic-arm assisted TKA was associated with reduced postoperative pain (p < 0.001), decreased analgesia requirements (p < 0.001), decreased reduction in postoperative haemoglobin levels (p < 0.001), shorter time to straight leg raise (p < 0.001), decreased number of physiotherapy sessions (p < 0.001) and improved maximum knee flexion at discharge (p < 0.001) compared with conventional jig-based TKA. Median time to hospital discharge in robotic TKA was 3.2 days compared with 4.4 days in conventional TKA (p < 0.001). | 2 | B |
| Khlopas et al76 | 2020 | 1 | Mako | 150 | 102 | 3 | This prospective, non-randomized, open-label, multicentre comparative cohort study found robotic TKA patients to have equal or greater improvements in 9 out of 10 of the Knee Society Scoring System components assessed at 3 months postoperatively, though not all findings were statistically significant. | 2 | B |
| Ren et al87 | 2019 | 7 | ROBODOC CASPAR |
315 | 262 | 16–120 | Seven studies with a total of 577 knees undergoing TKA were included. Compared with conventional surgery, active robotic TKA showed better outcomes in precise mechanical alignment (p < 0.05) and implant position, with lower outliers (p < 0.05), better functional score (WOMAC functional score) and less drainage (p < 0.05). | 2 | B |
| Siebert et al57 | 2002 | 1 | CASPAR | 70 | 50 | – | The mean difference between preoperatively planned and postoperatively achieved tibiofemoral alignment was 0.8 degrees (0–4.1 degrees) in the robotic group vs. 2.6 degrees (0–7 degrees) in a manually operated historical control group of 50 patients. The authors observed reduced postoperative soft tissue swelling in the robotic cohort. | 3 | B |
| Park et al42 | 2007 | 1 | ROBODOC | 32 | 30 | 45 | Roughly 70% of conventional TKA gives a MA alignment of less than ± 3° as compared to more than 90% with navigation TKA. Six of the 32 active robotic TKA procedures had short-term complications including superficial infection, patellar tendon ligament rupture, patella dislocation, supracondylar fracture and patellar fracture and common peroneal injury. | 3 | B |
| Song et al48 | 2011 | 1 | ROBODOC | 15 | 15 | 16 | Radiographic results showed significantly more postoperative leg alignment outliers of conventional sides than robotic-assisted sides (mechanical axis, coronal inclination of the femoral prosthesis, and sagittal inclination of the tibial prosthesis). Robotic-assisted sides had non-significantly better postoperative knee scores (HSS, WOMAC, side preference) and ROMs. | 3 | B |
| Clark et al30 | 2013 | 1 | OMNIBotic | 52 | 29 | 1 | Robotic navigation times were, on average, 9.0 minutes shorter compared to computer navigation. The average absolute intraoperative malalignment was 0.5° less in the robotic procedures compared to the computer-navigation procedures. Patients in the robotic TKA group tended to be discharged 0.6 days earlier compared to patients in the computer-navigated TKA. | 3 | B |
| Yang et al89 | 2017 | 1 | ROBODOC | 71 | 42 | 120 | Clinical outcomes and long-term survival rates were similar between the two groups. Regarding the radiological outcomes, the robotic TKA group had significantly fewer postoperative leg alignment outliers (femoral coronal inclination, tibial coronal inclination, femoral sagittal inclination, tibial sagittal inclination, and mechanical axis) and fewer radiolucent lines than the conventional TKA group. | 3 | B |
| Marchand et al108 | 2017 | 1 | Mako | 20 | 20 | 6 | The mean physical function scores for the manual and robotic cohorts were 9 ± 5 and 4 ± 5, p = 0.055, respectively. The mean total patient satisfaction scores for the manual and robotic cohorts were 14 points and 7 points, p < 0.05, respectively. The results from this study highlight the potential of the Mako to improve short-term pain, physical function, and total satisfaction scores. | 3 | B |
| Kayani et al85 | 2018 | 1 | Mako | 30 | 30 | – | Patients undergoing RA-TKA had reduced medial soft tissue injury in both passively correctible (p < 0.05) and fixed varus deformities (p < 0.05); more accurate femoral (p < 0.05) and tibial (p < 0.05) bone resection cuts; and improved macroscopic soft tissue injury (MASTI) scores compared to conventional TKA (p < 0.05). | 3 | B |
| Cho et al90 | 2019 | 1 | ROBODOC | 155 | 196 | 132 | All clinical assessments showed excellent improvements in both robotic and conventional TKA cohorts (all p < 0.05), without any significant differences between the groups (p > 0.05). The conventional TKA group showed a significantly higher number of outliers compared with the robotic TKA group (p < 0.05). The cumulative survival rate was 98.8% in robotic TKA and 98.5% in the conventional group (p = 0.563). | 3 | B |
| Cool et al95 | 2019 | 1 | Mako | 519 | 2595 | 3 | Overall 90-day episode-of-care costs were US$2,391 less for robotic TKA (p < 0.0001). Over 90% of patients in both cohorts utilized post-acute services, with robotic TKA accruing fewer costs than manual TKA. Savings were driven by fewer readmissions and an economically beneficial discharge destination. | 3 | B |
| Malkani et al86 | 2020 | 1 | Mako | 188 | 188 | 24 | Patients undergoing RA-TKA experienced a significant, 4.5-fold decrease in rates of MUA (p = 0.032). Given that MUAs can be a marker of knee stiffness following total knee arthroplasty, the lower rate indicates that study cohort patients had less knee stiffness and, therefore, greater initial postoperative ROM than the control cohort. | 3 | B |
| Marchand et al75 | 2019 | 1 | Mako | 53 | 53 | 12 | The RA-TKA cohort had significantly improved mean total (6 ± 6 vs. 9 ± 8 points, p = 0.03) and physical function scores (4 ± 4 vs. 6 ± 5 points, p = 0.02) when compared with the manual cohort. The mean pain score for the RA-TKA cohort (2 ± 3 points [range, 0–14 points]) was also lower than that for the manual cohort (3 ± 4 points [range, 0–11 points]) (p = 0.06). RA-TKA was found to have the strongest association with improved scores when compared with age, gender, and BMI. This study suggests that RA-TKA patients may have short-term improvements at minimum 1-year postoperatively. | 3 | B |
| Sultan et al46 | 2019 | 1 | Mako | 43 | 39 | 1.5 | RA-TKA patients had smaller mean differences in posterior condylar offset ratio which has been previously shown to correlate with better joint ROM at one year following surgery. In addition, these patients were less likely to have values outside of normal Insall-Salvati Index, which means they are less likely to develop patella baja, leading to restricted flexion and overall decreased ROM. | 3 | B |
| Khlopas et al76 | 2020 | 1 | Mako | 150 | 102 | 3 | At 4 to 6 weeks postoperatively and at 3 months, RA-TKA patients were also found to have larger improvements in walking and standing, standard activities, advanced activities, functional activities total score, pain with walking, total symptoms score, satisfaction score, expectations score when compared with manual TKA patients. | 3 | B |
| Bellemans et al43 | 2007 | 1 | CASPAR | 25 | – | 66 | Results demonstrate excellent implant positioning and alignment was achieved within the 1° error of neutral alignment in all three planes in all cases. Despite this technical precision, the excessive operating time required for the robotic implantation, the technical complexity of the system, and the extremely high operational costs have led the authors to abandon the robotic system. | 4 | C |
| Marchand et al80 | 2018 | 1 | Mako | 330 | – | – | All 132 knees with initial varus deformity of less than 7° were corrected to neutral (mean 1°, range –1–3°). A total of 82 knees (64%) with 7° or greater varus deformity were corrected to neutral (mean 2°, range 0–3°). However, roughly 30% of patients with severe deformity who were not corrected to neutral were still corrected within a couple of degrees of neutral. There were seven knees with 7° or greater valgus deformity, and all were corrected to neutral (mean 2°, range 0–3°). This study demonstrated that all knees were corrected in the appropriate direction within a few degrees of neutral, and no knees were overcorrected. | 4 | C |
| Sodhi et al74 | 2018 | 1 | Mako | 20 | 20 | – | Surgeon 1: First and last robotic cohort operative times were 81 and 70 minutes (p < 0.05). Mean operative times for the first 20 robotic-assisted cases and manual cases were 81 versus 68 minutes (p < 0.05). Mean operative times for the last 20 robotic-assisted cases and manual cases were 70 versus 68 minutes (p > 0.05). Surgeon 2: First and last robotic cohort operative times were 117 and 98 minutes (p < 0.05). Mean operative times for the first 20 robotic-assisted cases and manual cases were 117 versus 95 (p < 0.05). Mean operative times for the last 20 robotic-cohort cases and manual cases were 98 versus 95 (p > 0.05). The data from this study effectively create a learning curve for the use of robotic-assisted TKA. As both surgeons completed their total cases numbers within similar time frames, these data imply that within a few months, a board-certified orthopaedic joint arthroplasty surgeon should be able to adequately perform robotic TKA without adding any operative times. | 4 | C |
| Sodhi et al77 | 2019 | 1 | Mako | 3 | – | – | Three cases (femoral and tibial fracture malunion, proximal tibial fracture nonunion, healed tibial plateau fracture) of patients who underwent RA-TKA in the setting of preoperative extra-articular deformities were identified. Utilizing preoperative CT scans with a 3D plan for robotic-arm assisted surgery allowed for appropriate assessment of the deformity preoperatively and execution of a plan for a balanced and aligned total knee arthroplasty. The study reported excellent results utilizing RA-TKA in these complex cases. |
4 | C |
| Marchand et al78 | 2019 | 1 | Mako | 335 | – | 1 | For 98% of prostheses, RA-TKA software predicted within 1 implant size the actual tibial or femoral implant size used. The mean length of stay was found to be 2 days. No patients suffered from superficial skin infection, pin site infections or fractures, soft tissue damage, and no robotic cases were converted to manual TKA due to intraoperative complications. A total of 8 patients (2.2%) were readmitted; however, none were directly related to robotic use. The robotic software and use of a preoperative CT substantially helped with intraoperative planning and accurate prediction of implant sizes. | 4 | C |
| Khlopas et al83 | 2017 | 1 | Mako | 6 | 6 | – | During bone resections, the tibia in RA-TKA procedures did not require subluxation, which may reduce ligament stretching or decrease complication rates. Potential patient benefits for short-term recovery and decreased morbidity to reduce operative complications should be studied in a clinical setting. Since RA-TKA uses a stereotactic boundary to constrain the sawblade, which is generated based on the implant size, shape, and plan, and does not have the ability to track the patient’s soft tissue structures, standard retraction techniques during cutting are recommended. Therefore, the retractor placement and potential for soft tissue protection needs to be further investigated. RA-TKA has the potential to increase soft tissue protection when compared to manual TKA. | 5 | I |
| Parratte et al65 | 2019 | 1 | ROSA | 15 | 15 | – | 15 cadaveric specimens were used with 15 knees undergoing TKA with computer navigation and 15 knees undergoing robotic TKA with ROSA. The target angles obtained from the intraoperative planning were then compared to the angles of the bone cuts performed using the robotic system and measured with the computer-assisted system considered to be the gold standard. All angle mean differences were below 1° and standard deviations below 1°. For all 6 angles, the mean differences between the target angle and the measured values were not significantly different from 0 except for the femoral flexion angle which had a mean difference of 0.95°. The mean hip-knee-ankle axis difference was –0.03° ± 0.87°. All resection mean differences were below 0.7 mm and standard deviations below 1.1 mm. | 5 | I |
| Hampp et al81 | 2019 | 1 | Mako | 12 | 12 | – | Significantly less damage occurred to the PCLs in the RA-TKA versus the manual TKA specimens (p < 0.001). RA-TKA specimens had non-significantly less damage to the deep medial collateral ligaments (p = 0.149), iliotibial bands (p = 0.580), poplitei (p = 0.248), and patellar ligaments (p = 0.317). The remaining anatomical structures had minimal soft tissue damage in all manual TKA and RA-TKA specimens. These findings are likely due to the enhanced preoperative planning with the robotic software, the real-time intraoperative feedback, and the haptically bounded saw blade, all of which may help protect the surrounding soft tissues and ligaments. | 5 | I |
Note. TKA, total knee arthroplasty; (#), number; ROM, range of motion; KSS, Knee Society score; WOMAC, Western Ontario and McMaster Universities osteoarthritis index; SF-36, Short Form-36; RA-TKA, robotic-assisted TKA; PCL, posterior cruciate ligament; HSS, Hospital for Special Surgery; QoL, quality of life; MCID, minimal clinically important difference; OKS, Oxford Knee Score; MA, mechanical axis; MUA, manipulation under anesthesia; BMI, body mass index; CT, computed tomography
Cost analysis
In today’s cost-conscious healthcare environment that has transitioned towards value-based care, the future of robotics in TJA depends heavily on the value it provides and its associated cost-effectiveness. Robotic technology is associated with substantial installation and maintenance costs in addition to preoperative imaging, increased operating times during the learning phase, and computer software updates.60 Depending on the hospital contracts, each robotic device may range in cost from $400,000 to $1.5 million.60 The upfront expenditure may be partly offset with cost savings from reduced analgesia consumption, decreased hospital length of stay (LOS), readmission rates and greater home discharges for robotic TKA.60
In a Markov model analysis, Moschetti et al92 found robotic UKA to be more cost-effective compared to traditional UKA if case volume exceeded 94 cases per year, two-year failure rates were below 1.2%, and total system costs were less than $1.4 million and not cost-effective in low to medium-volume centres. Similarly, another Markov decision analysis showed robotic UKA to be cost-effective in terms of quality-adjusted life years (QALY) at centres with greater than 200 annual cases a LOS less than two days.93 Although there are no Markov model cost-analysis RA-TKA studies, many models are theoretical as prospective outcome studies are needed to substantiate the role of robotics.
Wide acceptance of new technologies should be coupled with the anticipated short and long-term benefits, outcomes and reduction in postoperative complications beyond the cost of the robotic technology. Revision TKA has an annual burden of $2.3 billion in hospital charges with the burden on the healthcare system to surpass $13 billion by 2030.94 In an era of value-based care and bundled payments, Cool et al95 evaluated 90-day episode-of-care costs associated with 519 RA-TKA versus propensity score matched 2,595 manual TKA amongst Medicare patients. Overall, 90-day episode-of-costs were $2,391 less costly for RA-TKA (p < 0.0001) driven by fewer readmission (5.2% versus 7.8%) and greater home discharges (56.7% versus 46.7%).95 However, the study highlights that as diagnosis-related group payments vary by hospital, the ability to determine claims costs versus true hospital facility costs are difficult to elucidate across the overall population.
Currently, these short-term outcome studies suggest that the initial capital investment has the potential to be offset by improved PROMs, LOS, readmission rates, and home discharge. However, since there are no long-term RA-TKA studies demonstrating distinct advantages and cost-savings over conventional techniques, insurance companies do not always authorize RA-TKA including preoperative advanced imaging as medical necessities.96 Though RA-TKA has shown short-term success, longer-term evaluation of implant survivorship, patient satisfaction, and rates of revision arthroplasty will determine the value of robotic technology in TKA. Cost-effectiveness and the value added with robotic procedures remains a dynamic and important factor as the field of robotics in arthroplasty continues to evolve.
Ergonomic health
Operating room physical stresses are known potential causes of musculoskeletal overuse injuries amongst surgeons, especially those who perform arthroplasty, due to ergonomically challenging postures.96 Other studies have reported neck injuries to be one of the highest incidences amongst arthroplasty surgeon work-related injuries.97,98 In a cadaver study, movement and electromyography (EMG) sensors were secured to two surgeons performing manual TKA and RA-TKA to monitor shoulder and low back movements and muscle activities. Overall, there were more high-risk shoulder than lower back activities in both manual and RA-TKA. Highest risk tasks for shoulder and low back stimulation were during bone cut preparation and cutting, with a higher risk for manual TKA compared to RA-TKA.96 RA-TKA can further help reduce physical stress on an individual’s neck by providing an eye-level computer display to improve cervical and thoracic spine posture.99 Robotic technology requires less demanding physical work with more ergonomic friendly postures which may prove to have a beneficial impact on long-term physical health.99 However, studies specifically evaluating medium and long-term impact on surgeon health are warranted to determine robotic technology’s additional value.
Limitations
Many robotic devices are compatible with a limited number of implant designs, and different application systems need to be purchased for THA, UKA and TKA. Additionally, RA-TKA may require additional incisions for insertion of the femoral and tibial registration pins to enable optical motion-capture tracking, and image guidance that increases patient radiation exposure.60 Despite improvement of workflow and efficiency, there are inherent time delays both preoperatively for implant templating and intraoperative plan adjustment. This is especially relevant as every 20-minute increase in operative time is associated with nearly a 25% increased risk of subsequent periprosthetic joint infection.100 Furthermore, similar to CAN, robotic systems can require percutaneous pins for optical tracking arrays which creates stress risers and risk for periprosthetic fractures, especially if placed in diaphyseal bone.101 Inadvertent pin placement can also theoretically cause neurovascular laceration.101 It is, therefore, critical that optical array pins be placed meticulously in metaphyseal bone without extensively breaching the second cortex. Finally, although robotic platforms are designed to make precise bone cuts without deviation from the planned template, some systems such as the older ROBODOC did not routinely recognize periarticular soft tissue, as studies have reported a 5% incidence of patella tendon rupture.102 Although newer designs have evolved to become more cognizant of surrounding soft tissues, it is still imperative to place retractors in the appropriate position to prevent any iatrogenic ligamentous or neurovascular compromise.
Conclusion
Robotic TKA has shown improved reproducibility and precision in mechanical alignment restoration with improvement in early functional outcomes and 90-day episode-of-care cost savings compared to conventional TKA; however, its added value is still to be determined. Technology-assisted TKA helps execute a preoperative templated plan while minimizing variation and maximizing reliability and reproducibility compared to conventional methods. Therefore, the usefulness of robotic platforms is the decreased variability in execution of an action, not necessarily to improve the expected outcome from an already well executed procedure.103 In today’s paradigm shift towards increased emphasis on quality of care while curtailing costs, providing value-based care is the primary goal for healthcare systems and clinicians.104 As robotic technology continues to develop, longer-term studies evaluating implant survivorship and complications will determine whether the initial capital is offset with improved outcomes. More importantly, evaluation of patient functional outcomes, satisfaction and overall surgeon health will determine whether robotic technology has added value in TKA.
Footnotes
ICMJE Conflict of interest statement: AS reports consultancy for the Zimmer Biomet robot discussed in the paper, outside the submitted work.
MRB reports consultancy for Stryker Orthopaedics, outside the submitted work.
NSP reports consultancy for Stryker Orthopaedics and grants/grants pending with OREF, RegenLab and Zimmer, all outside the submitted work.
The authors declare no conflict of interest relevant to this work.
OA licence text: This article is distributed under the terms of the Creative Commons Attribution-Non Commercial 4.0 International (CC BY-NC 4.0) licence (https://creativecommons.org/licenses/by-nc/4.0/) which permits non-commercial use, reproduction and distribution of the work without further permission provided the original work is attributed.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Schwartz AJ, Bozic KJ, Etzioni DA. Value-based total hip and knee arthroplasty: a framework for understanding the literature. J Am Acad Orthop Surg 2019;27:1–11. [DOI] [PubMed] [Google Scholar]
- 2. Sloan M, Premkumar A, Sheth NP. Projected volume of primary total joint arthroplasty in the US, 2014 to 2030. J Bone Joint Surg Am 2018;100:1455–1460. [DOI] [PubMed] [Google Scholar]
- 3. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg – Ser A 2007;89:780–785. [DOI] [PubMed] [Google Scholar]
- 4. Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Jt Surg - Ser A 2005;87:1487–1497. [DOI] [PubMed] [Google Scholar]
- 5. Kurtz SM, Ong KL, Schmier J, Zhao K, Mowat F, Lau E. Primary and revision arthroplasty surgery caseloads in the United States from 1990 to 2004. J Arthroplasty 2009;24:195–203. [DOI] [PubMed] [Google Scholar]
- 6. Choi Y-J, Ra HJ. Patient satisfaction after total knee arthroplasty. Knee Surg Relat Res 2016;28:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bryan S, Goldsmith LJ, Davis JC, et al. Revisiting patient satisfaction following total knee arthroplasty: a longitudinal observational study. BMC Musculoskelet Disord 2018;19:423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Neogi T. The epidemiology and impact of pain in osteoarthritis. Osteoarthr Cartil 2013;21:1145–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Anderson JG, Wixson RL, Tsai D, Stulberg SD, Chang RW. Functional outcome and patient satisfaction in total knee patients over the age of 75. J Arthroplasty 1996;11:831–840. [DOI] [PubMed] [Google Scholar]
- 10. Chesworth BM, Mahomed NN, Bourne RB, Davis AM; OJRR Study Group. Willingness to go through surgery again validated the WOMAC clinically important difference from THR/TKR surgery. J Clin Epidemiol 2008;61:907–918. [DOI] [PubMed] [Google Scholar]
- 11. Dunbar MJ, Robertsson O, Ryd L, Lidgren L. Appropriate questionnaires for knee arthroplasty. J Bone Jt Surg - Ser B 2001;83:339–344. [DOI] [PubMed] [Google Scholar]
- 12. Hawker G, Wright J, Coyte P, et al. Health-related quality of life after knee replacement. J Bone Jt Surg 1998;80:163–173. [DOI] [PubMed] [Google Scholar]
- 13. Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 2006;452:35–43. [DOI] [PubMed] [Google Scholar]
- 14. Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 2010;468:57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schroer WC, Berend KR, Lombardi AV, et al. Why are total knees failing today? Etiology of total knee revision in 2010 and 2011. J Arthroplasty. 2013;28:116–119. [DOI] [PubMed] [Google Scholar]
- 16. Siddiqi A, Hardaker WM, Eachempati KK, Sheth NP. Advances in computer-aided technology for total knee arthroplasty. Orthopedics 2017;40:338–352. [DOI] [PubMed] [Google Scholar]
- 17. Banerjee S, Cherian JJ, Elmallah RK, Jauregui JJ, Pierce TP, Mont MA. Robotic-assisted knee arthroplasty. Expert Rev Med Devices 2015;12:727–735. [DOI] [PubMed] [Google Scholar]
- 18. Manzotti A, Cerveri P, De Momi E, Pullen C, Confalonieri N. Relationship between cutting errors and learning curve in computer-assisted total knee replacement. Int Orthop 2010;34:655–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement: its effect on survival. Clin Orthop Relat Res 1994;299:153–156. [PubMed] [Google Scholar]
- 20. Thienpont E, Fennema P, Price A. Can technology improve alignment during knee arthroplasty. Knee 2013;20:S21–S28. [DOI] [PubMed] [Google Scholar]
- 21. Mont MA, Urquhart MA, Hungerford DS, Krackow KA. Intramedullary goniometer can improve alignment in knee arthroplasty surgery. J Arthroplasty 1997;12:332–336. [DOI] [PubMed] [Google Scholar]
- 22. Plaskos C, Hodgson AJ, Inkpen K, McGraw RW. Bone cutting errors in total knee arthroplasty. J Arthroplasty 2002;17:698–705. [DOI] [PubMed] [Google Scholar]
- 23. Lee DY, Park YJ, Hwang SC, Park JS, Kang DG. No differences in mid- to long-term outcomes of computer-assisted navigation versus conventional total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2020;28:3183–3192. [DOI] [PubMed] [Google Scholar]
- 24. Kim YH, Park JW, Kim JS. The clinical outcome of computer-navigated compared with conventional knee arthroplasty in the same patients: a prospective, randomized, double-blind, long-term study. J Bone Joint Surg Am 2017;99:989–996. [DOI] [PubMed] [Google Scholar]
- 25. Zhang GQ, Chen JY, Chai W, Liu M, Wang Y. Comparison between computer-assisted-navigation and conventional total knee arthroplasties in patients undergoing simultaneous bilateral procedures: a randomized clinical trial. J Bone Joint Surg Am 2011;93:1190–1196. [DOI] [PubMed] [Google Scholar]
- 26. Roberts TD, Frampton CM, Young SW. Outcomes of computer-assisted surgery compared with conventional instrumentation in 19,221 total knee arthroplasties: results after a mean of 4.5 years of follow-up. J Bone Joint Surg Am 2020;102:550–556. [DOI] [PubMed] [Google Scholar]
- 27. Credence Research. Medical robotics market size, share, trend and forecast to 2022. https://www.credenceresearch.com/report/medical-robotics-market (date last accessed 27 April 2020).
- 28. Liow MHL, Xia Z, Wong MK, Tay KJ, Yeo SJ, Chin PL. Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis: a prospective randomised study. J Arthroplasty 2014;29:2373–2377. [DOI] [PubMed] [Google Scholar]
- 29. Koulalis D, O’Loughlin PF, Plaskos C, Kendoff D, Cross MB, Pearle AD. Sequential versus automated cutting guides in computer-assisted total knee arthroplasty. Knee 2011;18:436–442. [DOI] [PubMed] [Google Scholar]
- 30. Clark TC, Schmidt FH. Robot-assisted navigation versus computer-assisted navigation in primary total knee arthroplasty: efficiency and accuracy. ISRN Orthop 2013;2013:794827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Squitieri L, Bozic KJ, Pusic AL. The role of patient-reported outcome measures in value-based payment reform. Value Heal 2017;20:834–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. McLawhorn AS, Buller LT. Bundled payments in total joint replacement: keeping our care affordable and high in quality. Curr Rev Musculoskelet Med 2017;10:370–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cleveland O, Piuzzi NS, Strnad G, et al. ; OME Cleveland Clinic Orthopaedics. Implementing a scientifically valid, cost-effective, and scalable data collection system at point of care: the Cleveland Clinic OME Cohort. J Bone Joint Surg Am 2019;101:458–464. [DOI] [PubMed] [Google Scholar]
- 34. Saragaglia D, Picard F, Leitner F. An 8- to 10-year follow-up of 26 computer-assisted total knee arthroplasties. Orthopedics 2007;30:S121–S123. [PubMed] [Google Scholar]
- 35. Lionberger DR. The attraction of electromagnetic computer-assisted navigation in orthopaedic surgery. In: Stiehl JB, Konermann WH, Haaker RG, DiGioia AM, Navigation and MIS in Orthopaedic Surgery. Heidelberg: Springer, 2007. [Google Scholar]
- 36. Stulberg DD, Picard F, Saragaglia D. Computer-assisted total knee replacement arthroplasty. Oper Tech Orthop 2000;10:25-39. [Google Scholar]
- 37. Lionberger DR, Weise J, Ho DM, Haddad JL. How does electromagnetic navigation stack up against infrared navigation in minimally invasive total knee arthroplasties? J Arthroplasty 2008;23:573–580. [DOI] [PubMed] [Google Scholar]
- 38. Anderson KC, Buehler KC, Markel DC. Computer assisted navigation in total knee arthroplasty: comparison with conventional methods. J Arthroplasty 2005;20:132–138. [DOI] [PubMed] [Google Scholar]
- 39. Davies B. A review of robotics in surgery. Proc Inst Mech Eng Part H J Eng Med 2000;241:129–140. [DOI] [PubMed] [Google Scholar]
- 40. Challacombe BJ, Khan MS, Murphy D, Dasgupta P. The history of robotics in urology. World J Urol 2006;24:120–127. [DOI] [PubMed] [Google Scholar]
- 41. Bargar WL, Bauer A, Börner M. Primary and revision total hip replacement using the ROBODOC® system. Clin Orthop Relat Res 1998;354:82–91. [DOI] [PubMed] [Google Scholar]
- 42. Park SE, Lee CT. Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty 2007;22:1054–1059. [DOI] [PubMed] [Google Scholar]
- 43. Bellemans J, Vandenneucker H, Vanlauwe J. Robot-assisted total knee arthroplasty. Clin Orthop Relat Res 2007;464:111–116. [DOI] [PubMed] [Google Scholar]
- 44. Hampp EL, Chughtai M, Scholl LY, et al. Robotic-arm assisted total knee arthroplasty demonstrated greater accuracy and precision to plan compared with manual techniques. J Knee Surg 2019;32:239–250. [DOI] [PubMed] [Google Scholar]
- 45. Moon YW, Ha CW, Do KH, et al. Comparison of robot-assisted and conventional total knee arthroplasty: a controlled cadaver study using multiparameter quantitative three-dimensional CT assessment of alignment. Comput Aided Surg 2012;17:86–95. [DOI] [PubMed] [Google Scholar]
- 46. Sultan AA, Samuel LT, Khlopas A, et al. Robotic-arm assisted total knee arthroplasty more accurately restored the posterior condylar offset ratio and the Insall-Salvati Index compared to the manual technique: a cohort-matched study. Surg Technol Int 2019;34:409–413. [PubMed] [Google Scholar]
- 47. Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA knee. Clin Orthop Relat Res 2013;471:118–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Song E-K, Seon J-K, Park S-J, Jung WB, Park H-W, Lee GW. Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surgery, Sport Traumatol Arthrosc 2011;19:1069–1076. [DOI] [PubMed] [Google Scholar]
- 49. Buza JA, III, Wasterlain AS, Thakkar SC, Meere P, Vigdorchik J. Navigation and robotics in knee arthroplasty. JBJS Rev 2017;5:01874474-201702000-00001. [DOI] [PubMed] [Google Scholar]
- 50. Ponzio DY, Lonner JH. Preoperative mapping in unicompartmental knee arthroplasty using computed tomography scans is associated with radiation exposure and carries high cost. J Arthroplasty 2015;30:964–967. [DOI] [PubMed] [Google Scholar]
- 51. Foley KA, Muir JM, Epi C. Improving accuracy in total knee arthroplasty: a cadaveric comparison of a new surgical navigation tool, Intellijoint KNEE, with computed tomography imaging, 2019. www.intellijointsurgical.com (date last accessed 13 December 2020).
- 52. Nam D, Maher P, Ranawat A, Padgett D, Mayman D. CT-based, robotic-arm assisted navigation versus an imageless, computer-assisted surgery system in total hip arthroplasty: a comparison of radiographic results | Orthopaedic proceedings. Bone Jt J, 2018. https://online.boneandjoint.org.uk/doi/abs/10.1302/1358-992X.95BSUPP_34.ISTA2013-136 (date last accessed 13 December 2020).
- 53. Kalteis T, Handel M, Bäthis H, Perlick L, Tingart M, Grifka J. Imageless navigation for insertion of the acetabular component in total hip arthroplasty: is it accurate as CT-based navigation? J Bone Jt Surg - Ser B 2006;88:163–167. [DOI] [PubMed] [Google Scholar]
- 54. Leelasestaporn C, Tarnpichprasert T, Arirachakaran A, Kongtharvonskul J. Comparison of 1-year outcomes between MAKO versus NAVIO robot-assisted medial UKA: nonrandomized, prospective, comparative study. Knee Surg Relat Res 2020;32:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Shalhoub S, Lawrence JM, Keggi JM, Randall AL, DeClaire JH, Plaskos C. Imageless, robotic-assisted total knee arthroplasty combined with a robotic tensioning system can help predict and achieve accurate postoperative ligament balance. Arthroplast Today 2019;5:334–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Liow MHL, Chin PL, Pang HN, Tay DK-J, Yeo S-J. THINK surgical TSolution-One® (Robodoc) total knee arthroplasty. SICOT J 2017;3:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Siebert W, Mai S, Kober R, Heeckt PF. Technique and first clinical results of robot-assisted total knee replacement. Knee 2002;9:173–180. [DOI] [PubMed] [Google Scholar]
- 58. Jacofsky DJ, Allen M. Robotics in arthroplasty: a comprehensive review. J Arthroplasty 2016;31:2353–2363. [DOI] [PubMed] [Google Scholar]
- 59. Lang JE, Mannava S, Floyd AJ, et al. Robotic systems in orthopaedic surgery. J Bone Jt Surg - Ser B 2011;93:1296–1299. [DOI] [PubMed] [Google Scholar]
- 60. Kayani B, Konan S, Ayuob A, Onochie E, Al-Jabri T, Haddad FS. Robotic technology in total knee arthroplasty: a systematic review. EFORT Open Rev 2019;4:611–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Ritschl P, MacHacek F, Fuiko R. Modern navigated ligament balancing in total knee arthroplasty with the PiGalileo system. In: Stiehl JB, Konermann WH, Haaker RG, DiGioia AM, Navigation and MIS in Orthopaedic Surgery. Heidelberg: Springer, 2007. [Google Scholar]
- 62. Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C. A prospective, randomized study of computer-assisted and conventional total knee arthroplasty: three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am 2007;89:236–243. [DOI] [PubMed] [Google Scholar]
- 63. Cobb J, Henckel J, Gomes P, et al. Hands-on robotic unicompartmental knee replacement: a prospective, randomised controlled study of the Acrobot system. J Bone Joint Surg Br 2006;88:188–197. [DOI] [PubMed] [Google Scholar]
- 64. Scholes C, Sahni V, Lustig S, Parker DA, Coolican MRJ. Patient-specific instrumentation for total knee arthroplasty does not match the pre-operative plan as assessed by intra-operative computer-assisted navigation. Knee Surg Sports Traumatol Arthrosc 2014;22:660–665. [DOI] [PubMed] [Google Scholar]
- 65. Parratte S, Price AJ, Jeys LM, Jackson WF, Clarke HD. Accuracy of a new robotically assisted technique for total knee arthroplasty: a cadaveric study. J Arthroplasty 2019;34:2799–2803. [DOI] [PubMed] [Google Scholar]
- 66. Stryker. Stryker announces definitive agreement to acquire MAKO Surgical Corp. for $1.65 billion. https://investors.stryker.com/press-releases/news-details/2013/Stryker-Announces-Definitive-Agreement-to-Acquire-MAKO-Surgical-Corp-for-165-Billion/default.aspx (date last accessed 25 April 2020).
- 67. Pearle AD, van der List JP, Lee L, Coon TM, Borus TA, Roche MW. Survivorship and patient satisfaction of robotic-assisted medial unicompartmental knee arthroplasty at a minimum two-year follow-up. Knee 2017;24:419–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Lee K, Goodman SB. Current state and future of joint replacements in the hip and knee. Expert Rev Med Devices 2008;5:383–393. [DOI] [PubMed] [Google Scholar]
- 69. Batailler C, White N, Ranaldi FM, Neyret P, Servien E, Lustig S. Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. Knee Surgery, Sport Traumatol Arthrosc 2019;27:1232–1240. [DOI] [PubMed] [Google Scholar]
- 70. Navio robotic versus conventional total knee arthroplasty. ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT03519269 (date last accessed 26 April 2020).
- 71. Siddiqi A, Smith T, McPhilemy JJ, Ranawat AS, Sculco PK, Chen AF. Soft-tissue balancing technology for total knee arthroplasty. JBJS Rev 2020;8:e0050. [DOI] [PubMed] [Google Scholar]
- 72. Shalhoub S, Moschetti WE, Dabuzhsky L, Jevsevar DS, Keggi JM, Plaskos C. Laxity profiles in the native and replaced knee: application to robotic-assisted gap-balancing total knee arthroplasty. J Arthroplasty 2018;33:3043–3048. [DOI] [PubMed] [Google Scholar]
- 73. Kayani B, Konan S, Huq SS, Tahmassebi J, Haddad FS. Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surgery, Sport Traumatol Arthrosc 2019;27:1132–1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Sodhi N, Khlopas A, Piuzzi NS, et al. The learning curve associated with robotic total knee arthroplasty. J Knee Surg 2018;31:17–21. [DOI] [PubMed] [Google Scholar]
- 75. Marchand RC, Sodhi N, Anis HK, et al. One-year patient outcomes for robotic-arm-assisted versus manual total knee arthroplasty. J Knee Surg 2019;32:1063–1068. [DOI] [PubMed] [Google Scholar]
- 76. Khlopas A, Sodhi N, Hozack W, et al. Patient-reported functional and satisfaction outcomes after robotic-arm-assisted total knee arthroplasty: early results of a prospective multicenter investigation. J Knee Surg 2020;33:685–690. [DOI] [PubMed] [Google Scholar]
- 77. Sodhi N, Khlopas A, Ehiorobo JO, et al. Robotic-assisted total knee arthroplasty in the presence of extra-articular deformity. Surg Technol Int 2019;34:497–502. [PubMed] [Google Scholar]
- 78. Marchand RC, Sodhi N, Bhowmik-Stoker M, et al. Does the robotic arm and preoperative CT planning help with 3D intraoperative total knee arthroplasty planning? J Knee Surg 2019;32:742–749. [DOI] [PubMed] [Google Scholar]
- 79. Khlopas A, Sodhi N, Sultan AA, Chughtai M, Molloy RM, Mont MA. Robotic arm-assisted total knee arthroplasty. J Arthroplasty 2018;33:2002–2006. [DOI] [PubMed] [Google Scholar]
- 80. Marchand RC, Sodhi N, Khlopas A, et al. Coronal correction for severe deformity using robotic-assisted total knee arthroplasty. J Knee Surg 2018;31:2–5. [DOI] [PubMed] [Google Scholar]
- 81. Hampp EL, Sodhi N, Scholl L, Deren ME, Yenna Z, Westrich G, et al. Less iatrogenic soft-tissue damage utilizing robotic-assisted total knee arthroplasty when compared with a manual approach: a blinded assessment. Bone Joint Res 2019;8:495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Sultan AA, Piuzzi N, Khlopas A, Chughtai M, Sodhi N, Mont MA. Utilization of robotic-arm assisted total knee arthroplasty for soft tissue protection. Expert Rev Med Devices 2017;14:925–927. [DOI] [PubMed] [Google Scholar]
- 83. Khlopas A, Chughtai M, Hampp EL, et al. Robotic-arm assisted total knee arthroplasty demonstrated soft tissue protection. Surg Technol Int 2017;30:441–446. [PubMed] [Google Scholar]
- 84. Kayani B, Konan S, Tahmassebi J, Rowan FE, Haddad FS. An assessment of early functional rehabilitation and hospital discharge in conventional versus robotic-arm assisted unicompartmental knee arthroplasty. Bone Jt J 2019;101:24–33. [DOI] [PubMed] [Google Scholar]
- 85. Kayani B, Konan S, Pietrzak JRT, Haddad FS. Iatrogenic bone and soft tissue trauma in robotic-arm assisted total knee arthroplasty compared with conventional jig-based total knee arthroplasty: a prospective cohort study and validation of a new classification system. J Arthroplasty 2018;33:2496–2501. [DOI] [PubMed] [Google Scholar]
- 86. Malkani AL, Roche MW, Kolisek FR, et al. Manipulation under anesthesia rates in technology-assisted versus conventional-instrumentation total knee arthroplasty. Surg Technol Int 2020;36:336–340. [PubMed] [Google Scholar]
- 87. Ren Y, Cao S, Wu J, Weng X, Feng B. Efficacy and reliability of active robotic-assisted total knee arthroplasty compared with conventional total knee arthroplasty: a systematic review and meta-analysis. Postgrad Med J 2019;95:125–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Liow MHL, Goh GSH, Wong MK, Chin PL, Tay DKJ, Yeo SJ. Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surgery, Sport Traumatol Arthrosc 2017;25:2942–2951. [DOI] [PubMed] [Google Scholar]
- 89. Yang HY, Seon JK, Shin YJ, Lim HA, Song EK. Robotic total knee arthroplasty with a cruciate-retaining implant: a 10-year follow-up study. Clin Orthop Surg 2017;9:169–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Cho KJ, Seon JK, Jang WY, Park CG, Song EK. Robotic versus conventional primary total knee arthroplasty: clinical and radiological long-term results with a minimum follow-up of ten years. Int Orthop 2019;43:1345–1354. [DOI] [PubMed] [Google Scholar]
- 91. Kim YH, Yoon SH, Park JW. Does robotic-assisted TKA result in better outcome scores or long-term survivorship than conventional TKA? A randomized, controlled trial. Clin Orthop Relat Res 2020;478:266–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Moschetti WE, Konopka JF, Rubash HE, Genuario JW. Can robot-assisted unicompartmental knee arthroplasty be cost-effective? A Markov decision analysis. J Arthroplasty 2016;31:759–765. [DOI] [PubMed] [Google Scholar]
- 93. Clement ND, Deehan DJ, Patton JT. Robot-assisted unicompartmental knee arthroplasty for patients with isolated medial compartment osteoarthritis is cost-effective: A Markov decision analysis. Bone Jt J 2019;101-B:1063–1070. [DOI] [PubMed] [Google Scholar]
- 94. Bhandari M, Smith J, Miller LE, Block JE. Clinical and economic burden of revision knee arthroplasty. Clin Med Insights Arthritis Musculoskelet Disord 2012;5:89–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Cool CL, Jacofsky DJ, Seeger KA, Sodhi N, Mont MA. A 90-day episode-of-care cost analysis of robotic-arm assisted total knee arthroplasty. J Comp Eff Res 2019;8:327–336. [DOI] [PubMed] [Google Scholar]
- 96. Scholl L, Hampp E, Alipit V, Chen A, Mont M, Bhave A. Does the use of robotic technology improve surgeon ergonomic safety during TKA? 2019. https://easychair.org/publications/open/62mV (date last accessed 1 February 2021).
- 97. Alqahtani SM, Alzahrani MM, Tanzer M. Adult reconstructive surgery: a high-risk profession for work-related injuries. J Arthroplasty 2016;31:1194–1198. [DOI] [PubMed] [Google Scholar]
- 98. Abdollahzade F, Mohammadi F, Dianat I, Asghari E, Asghari-Jafarabadi M, Sokhanvar Z. Working posture and its predictors in operating room nurses. Health Promot Perspect 2016. 31;6:17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Mont MA, Khlopas A, Chughtai M, Newman JM, Deren M, Sultan AA. Value proposition of robotic total knee arthroplasty: what can robotic technology deliver in 2018 and beyond? Expert Rev Med Devices 2018;15:619–630. [DOI] [PubMed] [Google Scholar]
- 100. Wang Q, Goswami K, Shohat N, Aalirezaie A, Manrique J, Parvizi J. Longer operative time results in a higher rate of subsequent periprosthetic joint infection in patients undergoing primary joint arthroplasty. J Arthroplasty 2019;34:947–953. [DOI] [PubMed] [Google Scholar]
- 101. Lonner JH, Fillingham YA. Pros and cons: a balanced view of robotics in knee arthroplasty. J Arthroplasty 2018;33:2007–2013. [DOI] [PubMed] [Google Scholar]
- 102. Chun YS, Kim KI, Cho YJ, Kim YH, Yoo MC, Rhyu KH. Causes and patterns of aborting a robot-assisted arthroplasty. J Arthroplasty 2011;26:621–625. [DOI] [PubMed] [Google Scholar]
- 103. Bini S. The (surgical) robots are coming! Run for the hills or for the robots? LinkedIn. 2019. https://www.linkedin.com/pulse/surgical-robots-coming-run-hills-stefano-bini (date last accessed 9 May 2020).
- 104. Porter ME. What is value in health care? N Engl J Med 2010;363:2477–2481. [DOI] [PubMed] [Google Scholar]
- 105. Singh VK, Varkey R, Trehan R, Kamat Y, Raghavan R, Adhikari A. Functional outcome after computer-assisted total knee arthroplasty using measured resection versus gap balancing techniques: a randomised controlled study. J Orthop Surg (Hong Kong) 2012;20:344–347. [DOI] [PubMed] [Google Scholar]
- 106. Kamat YD, Aurakzai KM, Adhikari AR, Matthews D, Kalairajah Y, Field RE. Does computer navigation in total knee arthroplasty improve patient outcome at midterm follow-up? Int Orthop 2009;33:1567–1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Kayani B, Konan S, Pietrzak JRT, Tahmassebi J, Haddad FS. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty. Bone Jt J 2018;100-B:930–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Marchand RC, Sodhi N, Khlopas A, et al. Patient satisfaction outcomes after robotic arm-assisted total knee arthroplasty: a short-term evaluation. J Knee Surg 2017;30:849–853. [DOI] [PubMed] [Google Scholar]