INTRODUCTION
The recently validated Pittsburgh Fatigability Scale (PFS) Mental subscale improves upon shortfalls in existing global fatigue measures by standardizing mental fatigue to intensity and duration across a range of activities/tasks, thus eliminating self-pacing.1 A next step is to describe the prevalence and severity of perceived mental fatigability by age and sex to foster comparisons across cohorts and health conditions. We hypothesized that prevalence of perceived mental fatigability would be greater with advancing age and PFS Mental scores would be higher for women than men.
METHODS
Of the 2906 long life family study (LLFS) participants from Visit 2 (2014–2017), N = 2361 completed the PFS. Study eligibility, screening, and measurements are published elsewhere.2 The PFS is a self-administered, 10-item tool that measures fatigue anchored to demand tasks in separate physical and mental subscales. The PFS asks participants to indicate the level of tiredness/exhaustion one expects/imagines they would feel after completing activities on a scale from 0 (“no fatigue”) to 5 (“extreme fatigue”). Responses were summed to derive PFS Mental scores (0–50), higher score = more severe fatigability.3 Missing scores were imputed (n = 140).4 Established cut points were applied to construct PFS Mental score severity strata: 0–3, 4–7, 8–12, 13–15, 16–19, and ≥20.5 Participants with PFS Mental scores ≥13 were classified as having greater perceived mental fatigability.5
We examined age and sex differences using generalized estimating equations (GEEs) with an exchangeable covariance matrix accounting for family relatedness and adjusted for field center.2 Linear trends for PFS Mental scores and prevalence of greater perceived mental fatigability were evaluated across age strata (60–69, 70–79, 80–89, and 90–108 years) and by sex and education. Differences in sample characteristics across PFS Mental score severity strata were tested using GEEs.
RESULTS
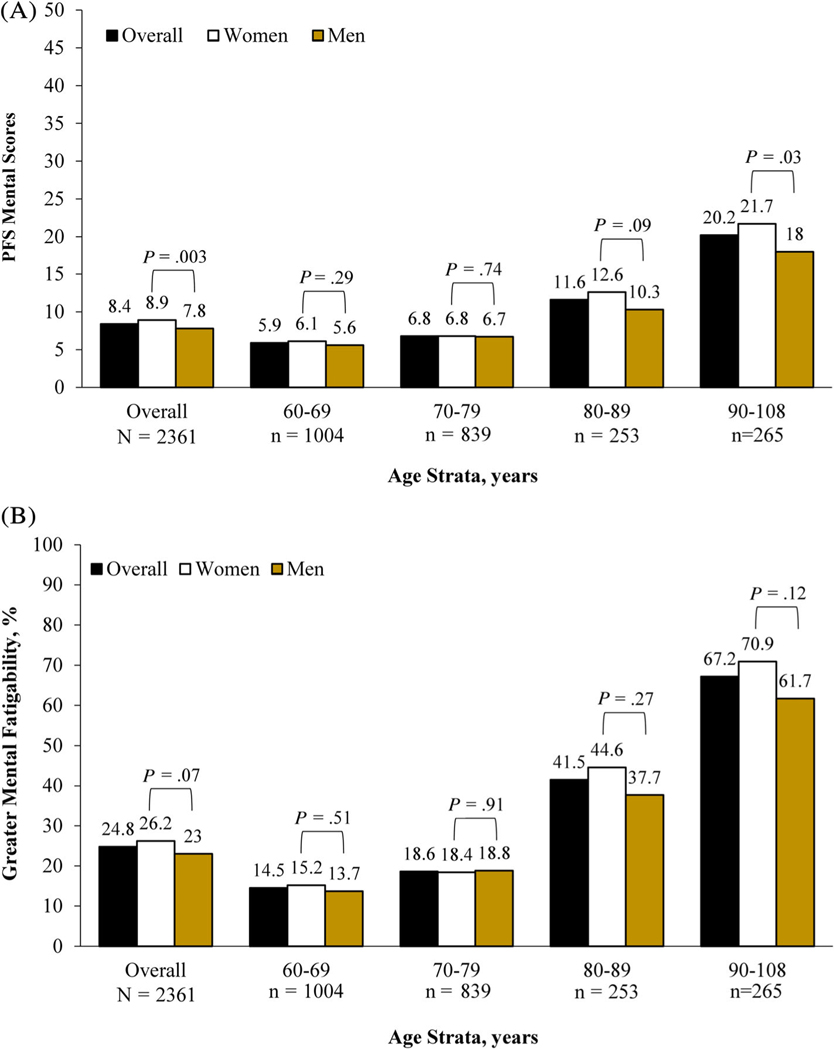
Overall, the sample was 73.6 ± 10.5 years (range 60–108 years), 99.6% white, and 55% women (Table S1). Those with the most severe mental fatigability (PFS Mental score ≥ 20) were less educated, had lower physical activity, slower gait speed, worse cognitive function, and greater depressive symptomatology (p < 0.001 for all) after adjustment (Tables S1 and S2). PFS Mental scores skewed right (Figure S1) and were 3.4-fold higher from the youngest (60–69 years) to the oldest (90–108 years) age strata (p < 0.001, Figure 1A and Table S2). When stratified by age and sex, mean PFS Mental scores were higher for women compared with men both overall (p = 0.003) and in the oldest age strata (p = 0.03, Figure 1A and Table S2). Prevalence of perceived mental fatigability (PFS ≥ 13) was greater with advanced age (14.5% for 60–69 years to 67.2% for those 90–108 years, p < 0.001) and was similar between women and men, although sex differences in prevalence widened across older age strata (Figure 1B).
FIGURE 1.
Pittsburgh Fatigability Scale (PFS) mental scores and prevalence of greater perceived mental fatigability across age strata and by sex: the long life family study (N = 2361). A, Mean PFS Mental scores across age strata and by sex. B, Prevalence of greater perceived mental fatigability (PFS mental scores ≥13) across age strata and by sex.
Note: p-values between sex account for family relatedness and are adjusted for field center. p-value for linear trend >0.001 for PFS Mental scores and greater perceived mental fatigability across age strata, overall and for women and men
DISCUSSION
The prevalence of perceived mental fatigability was strikingly greater with age, and women in the oldest age strata were most at risk for the highest PFS Mental scores. Overall mean PFS Mental scores for LLFS (8.4 points) were lower than those from two small studies of healthy older adults by Burke et al.6 (mean age = 74.1 years, N = 35, PFS = 14.0 points) and Carlozzi et al.7 (mean age = 53.4 years, N = 86, PFS = 10.2 points). Overall prevalence of greater perceived mental fatigability (24.8%) was comparable with the Baltimore Longitudinal Study of Aging (22.6%),5 despite LLFS having a larger proportion of the oldest-old. The trend of higher PFS Mental scores with age was expected, as aging is associated with decreased physical function that may cause increased cognitive strain due to higher energy expenditure when performing tasks of fixed intensity and duration.8 The appearance of sex-based differences for PFS Mental scores only in the oldest age strata corroborates and extends previous work that found no sex differences among younger age strata ranging from 25 to 75 years.9
We are the first to report prevalence and severity of perceived mental fatigability across age and sex, including a large sample of the oldest-old. Generalizability is limited due to LLFS participants being predominantly white, well-educated, and potential for selection bias in the oldest-old, possibly resulting in more conservative prevalence estimates. As the PFS is included in several large epidemiologic studies worldwide, forthcoming studies will evaluate perceived mental fatigability by race/ethnicity. Other future directions include examining consequences and prognostic value of this common patient-reported outcome on health conditions and mortality, with the goal of developing targeted interventions to reduce mental fatigue in order to slow phenotypic aging.10 Longitudinal examination of perceived mental fatigability is also warranted, as understanding trajectories with advancing age will aid in determining older adults most at risk for aging-related functional and cognitive decline.
Supplementary Material
Data S1 Supporting Information.
ACKNOWLEDGMENTS
FINANCIAL DISCLOSURE
This work was supported by the National Institute on Aging (U19 AG063893, U01 AG023712, U01 AG023744, U01 AG023746, U01 AG023749, and U01 AG023755). In addition, the Claude D. Pepper Older Americans Independence Center, Research Registry and Developmental Pilot Grant (NIH P30 AG024827), and the Intramural Research Program, National Institute on Aging supported N.W.G. to develop the Pittsburgh Fatigability Scale. The Epidemiology of Aging training grant at the University of Pittsburgh (NIA T32 AG000181) supported T.G.
Funding information
Intramural Research Program, National Institute on Aging; National Institute of Health Claude D. Pepper Older Americans Independence Center, Research Registry and Developmental Pilot Grant, Grant/Award Number: P30 AG024827; National Institute on Aging, Grant/Award Numbers: T32 AG000181, U01 AG023712, U01 AG023744, U01 AG023746, U01 AG023749, U01 AG023755, U19 AG063893
SPONSOR’S ROLE
None.
Footnotes
SUPPORTING INFORMATION
Additional supporting information may be found online in the Supporting Information section at the end of this article.
CONFLICT OF INTEREST
The authors declare that they have no conflicts of interest.
REFERENCES
- 1.Renner SW, Bear TM, Brown PJ, Andersen SL, Cosentino S, Gmelin T, Boudreau RM, Cauley JA, Qiao YS, Simonsick EM, Glynn NW. Validation of Perceived Mental Fatigability Using the Pittsburgh Fatigability Scale. J Am Geriatr Soc. 2021. January 20. doi: 10.1111/jgs.17017. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.LaSorda KR, Gmelin T, Kuipers AL, et al. Epidemiology of perceived physical fatigability in older adults: the long life family study. J Gerontol A Biol Sci Med Sci. 2020;75(9):e81–e88. 10.1093/gerona/glz288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Glynn NW, Santanasto AJ, Simonsick EM, et al. The Pittsburgh fatigability scale for older adults: development and validation. J Am Geriatr Soc. 2015;63(1):130–135. 10.1111/jgs.13191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cooper R, Popham M, Santanasto AJ, Hardy R, Glynn NW, Kuh D. Are BMI and inflammatory markers independently associated with physical fatigability in old age? Int J Obes (Lond). 2019;43(4):832–841. 10.1038/s41366-018-0087-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simonsick EM, Schrack JA, Santanasto AJ, Studenski SA, Ferrucci L, Glynn NW. Pittsburgh fatigability scale: one-page predictor of mobility decline in mobility-intact older adults. J Am Geriatr Soc. 2018;66(11):2092–2096. 10.1111/jgs.15531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burke SE, Babu Henry Samuel I, Zhao Q, et al. Task-based cognitive fatigability for older adults and validation of mental fatigability subscore of Pittsburgh fatigability scale. Front Aging Neurosci. 2018;10:327. 10.3389/fnagi.2018.00327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carlozzi NE, Boileau NR, Murphy SL, Braley TJ, Kratz AL. Validation of the Pittsburgh fatigability scale in a mixed sample of adults with and without chronic conditions. J Health Psychol. 2019: 1359105319877448. 10.1177/1359105319877448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moreh E, Jacobs JM, Stessman J. Fatigue, function, and mortality in older adults. J Gerontol A Biol Sci Med Sci. 2010;65(8): 887–895. 10.1093/gerona/glq064. [DOI] [PubMed] [Google Scholar]
- 9.Engberg I, Segerstedt J, Waller G, Wennberg P, Eliasson M.Fatigue in the general population- associations to age, sex, socioeconomic status, physical activity, sitting time and self-rated health: the northern Sweden MONICA study 2014. BMC Public Health. 2017;17(1):654. 10.1186/s12889-017-4623-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schrack JA, Simonsick EM, Glynn NW. Fatigability: a prognostic indicator of phenotypic aging. J Gerontol A Biol Sci Med Sci. 2020;75(9):e63–e66. 10.1093/gerona/glaa185. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1 Supporting Information.