SUMMARY
Oral cancer is a heterogeneous disease that develops through a complex, multi-step process. Precision medicine should help to better understand its molecular basis, integrate traditional classifications and have a positive impact on cancer management. To apply this information in clinical practice, we need to define its histology and identify biomarkers expressed by the tumour that provide useful information for planning tailored treatment. The most reliable information currently derives from evaluation of biomarkers on post-operative samples. To plan personalised treatment, oncologists need to assess these markers on biopsy samples. We reviewed the recent literature and identified 6 of 184 publications that compared markers measured on biopsy and post-operative samples or assessed their predictivity for the development of lymph node metastases. Data from these studies suggest that markers measured on biopsy samples can provide useful indications for tailoring treatments. However, due to their heterogeneity and low level of evidence, these results need to be confirmed by clinical studies on a large population to standardise and validate biomarkers in biopsies and to assess their reliability in other diagnostic mini-invasive procedures such as radiomics and liquid biopsy.
KEY WORDS: surgical biopsy, liquid biopsy, radiomics, depth of invasion, precision medicine
RIASSUNTO
Il cancro orale è una malattia eterogenea che origina ed evolve con un processo complesso e multifasico. La medicina di precisione permette di pianificare un trattamento personalizzato sulla base delle caratteristiche biologiche e molecolari delle singole neoplasie. Le informazioni oggi più affidabili sono fornite dalla valutazione post-operatoria dei biomarcatori, ma per pianificare un trattamento personalizzato è necessario valutare questi marcatori sulla biopsia. Per questo abbiamo rivisto la letteratura dell’ultimo quinquennio ed abbiamo identificato 6/184 articoli che valutano i marcatori sulla biopsia confrontandone i valori con quelli misurati sul pezzo operatorio di ciascun paziente o valutandone la predittività per lo sviluppo di metastasi linfonodali. I dati che emergono da questi studi suggeriscono che la valutazione dei marcatori sul campione bioptico potrebbe fornire indicazioni utili per programmare trattamenti personalizzati. Tuttavia, a causa della eterogeneità e del basso livello di evidenza dei lavori considerati, questi risultati devono essere confermati da studi clinici su un’ampia popolazione per standardizzare e validare i biomarcatori e la loro affidabilità in altre procedure mini-invasive, ad esempio radiomica e biopsia liquida.
PAROLE CHIAVE: biopsia chirurgica, biopsia liquida, radiomica, profondità di invasione, medicina di precisione
Introduction
Cancer of the oral cavity is the eighth most common cancer worldwide: GLOBOCAN reported an estimated 354,900 new cases in 2018; about 90% of these tumours are oral squamous cell carcinomas (OSCCs) with a 5-year survival of < 60% 1. OSCCs can arise from the oral tongue, which is the most common sub-site and has the worse prognosis 2-4, followed by the floor of mouth, buccal mucosa, alveolar mucosa, and hard palate. Historically, OSCC affects older people, mainly men, smokers and alcohol drinkers. Recent clinical and epidemiological studies have reported an overall decline in the incidence of tobacco-related OSCCs, probably due to the anti-smoking campaigns 5-7, but an increasing trend of tongue and oropharyngeal cancers in younger patients, women and individuals with no exposure to traditional risk factors 8-10. While infection with human papillomavirus accounts for an increasing number of patients with oropharyngeal cancers, risk factors, especially viruses, in OSCC non-smokers and non-drinkers, are unclear 11,12. Head and neck cancer (HNC), including OSCC, is a heterogeneous disease that develops through a complex, multi-step process involving genetic alterations, growth regulation, apoptosis, angiogenesis, invasion and metastasis; moreover, it is influenced by the individual’s genetic predisposition and environmental exposure to carcinogens 13,14. This heterogeneity is confirmed in daily practice by the observation that patients with clinically similar tumours have different treatment responses and outcomes 15,16.
Precision medicine
To address this heterogeneity, the Cancer Genome Atlas project 17, classifications based on molecular pathology 18, and the Precision Medicine Initiative 19 have been proposed. These efforts should help to better understand the molecular basis of cancer, integrate traditional classifications and have a positive impact on cancer management 20. Given this complexity, both the diagnosis and therapy of OSCCs should be planned by a highly specialised multidisciplinary team that is able to globally assess the disease and patient 21,22. Such personalised diagnostic and treatment strategies which precisely target molecular alterations refer to Precision Medicine or Genomics-Driven Cancer Medicine 23-25. To apply precision medicine in clinical practice, we need to identify biomarkers expressed by tumours that reflect their individual characteristics 26-28.
Tissue biomarkers validated on post-operative surgical specimens
Many prognostic/predictive biomarkers have been taken into account and tested, such as c-erbB2, EGFR (Epidermal Growth Factor Receptor), tumour infiltrating lymphocytes, c-met, etc., and currently the most reliable information on high-risk patients derives from assessment of tissue biomarkers on post-operative samples. In 2004, two trials by the European Organization for Research and Treatment of Cancer (EORTC), and the United States Radiation Therapy Oncology Group (RTOG) compared adjuvant radiation alone vs chemoradiation in advanced head and neck cancers. The results showed that the addition of concurrent chemotherapy was associated with better oncologic outcomes compared to radiation alone in a subset of high risk patients. They evaluated pathological classification of the primary tumour, positive margins, tumour depth, positive nodes, extranodal extension (ENE), lympho-vascular invasion (LVI), perineural invasion (PNI) and histology grade 29,30. A subsequent comparative analysis of data pooled from these two trials showed that ENE and/or microscopically involved surgical margins were the only risk factors for which the impact of post-operative chemo-radiotherapy was significant in both trials 31. Cooper et al. in 2012 confirmed these data by evaluating the long-term results of patients enrolled in the RTOG study. They found that at 10 years, local recurrence and disease-free survival rates were significantly better only in patients included in the chemo-radiotherapy arm for ENE and/or microscopically involved margins 32. Subsequently, other studies confirmed these data and proposed risk classes for effective post-operative therapeutic planning 33-36. The 8th edition of the TNM staging system 20 suggests that HPV and depth of invasion (DOI) as well as specific biomarkers expressed by HNCs should be assessed. OSCCs are rarely related to HPV, while DOI is useful to evaluate biological behaviour, because prognosis worsens when the tumour is deeper 37,38. In the past, the DOI of early-stage tongue tumours (T1-T2) was considered a predictor of occult lymph node metastases, as in skin carcinomas, and was used to plan neck dissection 39,40. Before the publication of the TNM, 8th Edition, the terms “Tumour Thickness (TT)” and “Depth of Invasion (DOI)” were often considered synonymous. However, DOI, as defined in the AJCC (American Joint Committee on Cancer) Cancer Staging Manual 8th Edition, has a better predictive value than TT 38,41. Recent studies based on this definition suggest that DOI > 4 mm (range: 3.4 mm-6.6 mm) is a strong predictor of locoregional recurrence, and survival together with two or more markers such as PNI, LVI and Worst Pattern Of Invasion (WPOI-5) 42-44 which have been integrated into the 8th TNM edition. In addition, several studies have highlighted tumour budding (BD) and tumour-stroma ratio (TSR), considered in other non-TNM-based staging systems, as predictive factors for lymphatic diffusion and disease-free survival (DFS) 15,45-47. Table I shows the definition and purpose of these markers 2,15,37,38,42,45,46,48-57.
Table I.
Pathological markers predictive of loco-regional recurrence and prognosticators.
| Marker | Definition | Notes |
|---|---|---|
| Depth of Invasion (DOI) | DOI is measured from the level of the basement membrane of the closest adjacent normal mucosa. A “plumb line” is dropped from this plane to the deepest point of tumour invasion 38,42 | Included in T1-3 Categories for Oral Cavity Cancer, TNM Staging Manual 8th Edition 37 The T category increases with every interval of 5 mm |
| Tumour Thickness (TT) |
TT is measured from the surface of the tumour to the deepest point of invasion. In exofitic and ulcerated lesions TT is measured from the imaginary line reconstructing the intact mucosa to the deepest point of invasion 42,48 TT1 is measured from the level of adjacent mucosa to the deepest point of tumour invasion 49 TT2 is the distance from the bottom of most adjacent dysplastic abnormal rete pegs to the deepest point of invasion 49 TT3 is measured as distance from the epithelial junction of the most adjacent dermal papillae to the deepest point of tumour invasion 49 |
As defined before publication of the 8th TNM Edition 42,48 or defined as an alternative to the proposed classification 49 Rete pegs: epithelial extensions in the connective tissue underlying the mucosa 49 |
| Radiological Depth of Invasion (rDOI) | rDOI is measured by drawing a perpendicular line from the reference line to the deepest point of the tumour 50 | Radiological definition of DOI is also reported in TNM 8th Edition 37. The reference line connects the junction of the tumour surfaces and of the normal mucosa on both sides 50 |
| Tumour Budding (TB) | TB is defined as the presence of either isolated single cells or small-cell clusters comprising fewer than five cells scattered in the stroma ahead of the invasive tumour front 15,45,48,51-54 | TB is speculated to be the result of interactions between cancer cells and tumour microenvironments. It is expression of loss of cohesion and active invasive cellular movement 55. It is considered the first step in metastasis of a solid tumour |
| Pattern of Invasion (POI) | POI at the tumour-host interface of oral cancer is graded 1 to 5. | Tumour dispersion is assessed at the advancing tumour edge. The most common WPOI-5 phenotype is tumor dispersion through soft tissue. Dispersed extratumoral peri-neural invasion, or extratumoral lymphovascular invasion, also can qualify for classification as WPOI-5 37 |
| Worst Pattern of Invasion (WPOI) | WPOI-5 (POI Grade 5) consists of dispersed, discontinuous growth pattern, with a defined tumour dispersion cutoff of 1 mm 37,54 | |
| Tumour-Stroma Ratio (TSR) | TSR defines the interactions between cancer cells and intra-tumoural stroma, which is the main component of the microenvironment 46,56,57 | These interactions are important for both cancer initiation and progression: the proportion of this stroma acts as a key regulator in cancer biology and could provide strategies for biological cancer treatment |
| Peri Neural Invasion (PNI) | PNI is defined as the tumour cell infiltration in any layer of the nerve sheath or tumour in close proximity involving more than one-third of the nerve circumference 49 | PNI should be subclassified as either intratumoral or extratumoral, and as focal or multifocal. Extensive multifocal PNl is usually extratumoral and frequently associated with a “strand-like” tumour phenotype 37 |
| Lympho Vascular Invasion (LVI) | LIV is defined as the detection of tumour epithelial cells within or attached to the endothelial cell lining of the vascular space 49 | LIV should be reported as either intratumoral or extratumoral, as well as focal or multifocal 37 |
To plan personalised treatment, oncologists need to assess these markers, including DOI, on biopsy samples according to the AJCC TNM (8th edition) recommendations 38. Herein, we review the literature in order to evaluate the concordance between the values of tissue biomarkers measured in both pre-operative and post-operative samples from the same patient.
Methods
For this purpose, we reviewed the recent literature published in English (January 2015-December 2019) by consulting the PubMed, Medline, Web of Science, Embase and Cochrane databases. We used the following keywords (strings): oral biopsy and depth of infiltration/DOI; oral biopsy and tumour/tumor budding; oral cancer diagnosis and depth of infiltration/DOI; oral cancer diagnosis and tumour/tumor budding. Only peer-reviewed papers were considered. We thus identified 184 papers (Fig. 1); 90 of these were duplicates. The remaining 94 were evaluated based on the abstracts. Inclusion criteria were: A) histologically proven squamous cell carcinomas (SCC) of the oral cavity; B) both prospective and retrospective studies; C) papers that compared biopsy and post-operative samples from the same patient; D) papers that evaluated predictivity of biomarkers on biopsy specimens; E) articles based on a retrospective series whose biopsy and post-operative slides were reviewed by the authors. Exclusion criteria: a) reviews, case reports, abstracts; b) histology other than SCC; c) studies that did not review histological samples. As a result of this analysis, we discarded 72 papers unrelated to our aim; for 12 studies, criteria for patient selection or study design were not reported in detail. Fourteen papers (the 10 selected articles and 4 others identified through a manual search) were evaluated on the complete text. Following this analysis, 8 more papers were considered unsuitable for our purpose as they were reviews or the study design did not fall within the selection criteria.
Figure 1.
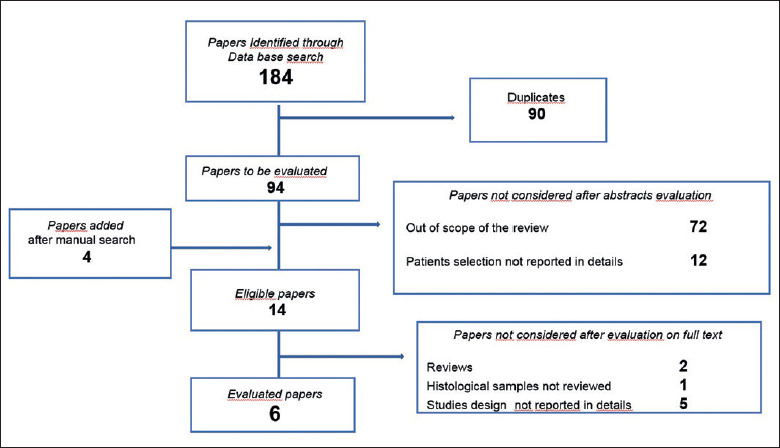
Flow chart showing selection of papers.
Results
All six papers included were retrospective, and were divided into two groups based on the aim of the study (Tab. II) 48,49,58-61:
Table II.
Evaluation of pathological markers on biopsy and postoperative samples in the 6 papers selected.
| Author | Study design Time period | Site Stage or TNM teatment | No. patients Biopsy technique | Aim of the study | Markers | Results | Notes |
|---|---|---|---|---|---|---|---|
| Almangush, 2018 58 | Retrospective 1981-2016 | Mobile oral tongue Stage I-II = 81% Stage III-IV = 19% Surgery = 100% |
100 Incisional biopsy |
Analysis of the sensitivity and specificity of BD scores on biopsy and postoperative samples | TB TT BD model score |
BD model score preo-op vs post-op - Sensitivity 59.1% - Specificity = 100% - Agreement pre/post op = 83% Depth values (mm) pre-op (mean) = 4.1 (0.5-10 mm) post-op (mean) = 6.3 (0.5-23 mm) |
17% = non-representative biopsies (badly fragmented, too superficial, technical artifacts) TB and TT (Tab. I) Budding model score (Tab. II) |
| Seki, 2016 59 | Retrospective 2009-2013 |
Tongue, floor of the mouth T1 = 43% T2-T4 = 57% Preop CT = 52% Surgery = 48% |
91 Not described |
Detection of histopathologic parameters predictive for lympho nodal metastases in preoperative biopsy specimens |
Histologic Grading TT INF LIV Budding score |
Tumour depth: higher in resection specimens than in biopsy samples. It is predictive of lymph node metastases on resection specimens, not on biopsy samples Budding score: good correlation between biopsy and postop specimens BD = > 3 and Tumour depth > 3 mm significantly predictive of lymph node metastases, OS and RFS BD = > 3 and INFa/INFb: predictive of early or late lymph node metastases or late in many cases |
TT (Tab. I) INF (Tab. I) Budding score (Tab. IIb) Comparison between TB, TT, and INF status on lymph node metastases was assessed on 33 patients who underwent resection and neck dissection |
| Seki Soda, 2019 60 | Retrospective 2009-2015 |
Oral cavity Stage not reported Preop CT = 57% Surgery = 43% |
248 Incisional biopsy |
Evaluation of relashionship between tumour budding score in biopsy and resected specimens and the effect of pre-op chemotherapy on tumour budding | Budding score | Mean budding scores: no significant differences in both groups; but tended to increase in resected patients without preop CT Preoperative CT-S1 treatment is effective for suppressing relapse and lowering the budding scores |
Budding score (Tab. II) |
| Seki, 2017 48 | Retrospective 2009-2014 |
Mobile tongue, buccal mucosa, palate, lip T1-T2 = 76% T3-T4 = 24% Preop CT and resection +/- ND = 53% Resection+/- ND = 47% |
209 Incisional biopsy |
Evaluation of the relashionship between tumour budding in biopsy specimen and lymphnode metastases | TB INF Tumour grade TT |
TB => 3 predictive of Lymphnode metastases and poor prognosis P < 0.01 (mainly T1-T2 cN0) The budding score (high) together with INF and LIV were found to be independent risk factors for lymphnode metastases at multivariate analyses Strong correlation (p < 0.01) between the budding score and tumour grade, tumour depth, INF, and blood vessels invasion TB in early OSCC can be used as a reliable parameter for stratifying patients with different risks of lymph node metastases |
Authors describe biopsy technique; Tumour budding can be detected using routine haematoxylin and eosin-stained slides or cytokeratin-stained slides. Results may differ significantly depending on the staining used |
| Nayanar, 2019 61 | Retrospective 2014-2016 |
Oral cavity (lips, buccal mucosa, tongue, hard palate, retromolar trigone, floor of the mouth) Stage II = 48% Stage III = 20% Stage IV = 32% Wide excision with Neck dissection |
160 Incision or wedge biopsy |
Identification of clinical and histopathological predictors of lymphnode metastases Development of a predictive scoring system |
Shape of rete pegs Pattern of invasion Depth of invasion (TT) Histologic differentiation Site of cancer |
Risk score (4-18) Score 4: predictive of N+ = 5% Score 18: predictive of N+ = 91% |
The risk score needs to be tested and validated in other patient populations Rete pegs (Tab. I) Risk score (Tab. II) |
| Sahoo, 2020 49 | Retrospective 2014-2016 |
Oral cavity (GB sulcus, tongue, floor of the mouth, retromolar and maxilla) cT1/T2 Resection and elective neck dissection |
150 Excisional biopsy |
Comparison of prognostic performance of TT and of DOI (TT2 and TT3) in predicting lymphnode metastases. Predictive potential of PNI and LVI |
TT1, TT2, TT3, DOI PNI, LVI |
TT2 and LVI correlate with lymph node metastases | TT1, TT2, TT3, DOI (Tab. I) |
Comparison of tissue markers on biopsy and post-operative samples
Three papers 58-60 compared the values of biomarkers measured on patient’s biopsy and post-operative samples from the same patients in order to evaluate their concordance and reliability. Almangush et al. 58 reviewed the slides of 100 patients (81 = Stage I-II) with SCC of the mobile tongue treated with surgical excision. They measured TT and found that mean values were 4.1 mm (0.5-10 mm) in biopsy samples vs 6.3 mm (0.5-23 mm) in the corresponding post-operative specimens. They also evaluated TB (Tab. I) and their prognostic score (BD Model, Tab. III), and documented a sensitivity and specificity of pre-operative vs post-operative values of 59% and 100%, respectively, showing a 83% pre-operative/post-operative agreement. Seki et al. 59, among 91 OSCC patients treated with surgery alone or preoperative chemotherapy and resection, analysed 44 undergoing exclusive surgery. They evaluated TT, TB Score (TBS, Tab. III), infiltrative pattern (INF, Tab. III) and LVI, and found that the depth of infiltration measured on biopsies was lower than that on post-operative samples, while there was a good correlation of budding score in pre-treatment and post-treatment samples. Seki Soda et al. 60 recently analysed the relationship between TBS in biopsies and in resected specimens of 248 patients with OSCC and the effect of pre-operative chemotherapy on TBS. The authors did not report staging, but pointed out that 141 of 248 patients received preoperative chemotherapy. The mean TBS in biopsy and resected specimens showed no significant difference between patients with and without preoperative chemotherapy. Moreover, they found that pre-operative chemotherapy is effective in lowering the budding score and suppressing relapses.
Table III.
Different scores for prognostic evaluation.
| Author | Definition | Score |
|---|---|---|
| Almangush, 2018 58 | BD Model Score (BDM): N° of buds and depth of invasive front (IF, mm) |
0: < 5 buds at the IF and depth < 4 mm 1: =/> 5 buds at the IF or depth > 4 mm 2: =/> 5 buds at the IF and depth > 4mm |
| Seki, 2017 48 | Tumour Budding Score (TBS): Number of buds |
Low: < 3 cells Intermediate: 3-4 cells High: => 5 cells |
| Seki, 2017 48 | INF (Infiltrative Pattern): Cancer growth and mode of invasion |
INFa: Expanding growth with a distinct border from surrounding tissue; INFb: Intermediate pattern between INFa and INFc; INFc: Infiltrative growth with no distinct border from the surrounding tissue |
| Nayanar, 2019 61 | Risk Score: Sum of single score of clinical and pathologic parameters |
Shape of rete pegs: Slender and fused = 1, Bulbous and uniform = 2; Irregular = 3 Pattern of invasion: Pushing = 1; Minimally invasive = 2; Frankly invasive = 5 Depth of invasion (TT, mm): 0-3 = 1; > 3 = 3 Histogic differentiation: Well = 1; Moderate = 3; Poor = 5 Site of cancer: Buccal mucosa = 0; Tongue = 1; Others = 2 |
Predictive value of pathological markers in biopsy samples
Four papers 48,49,59,61 evaluated whether markers assessed on biopsy samples were predictive of lymph node metastases (Tab. II). Seki et al. 59 examined 33 patients with tongue and floor SCC treated with tumour resection and neck dissection. They found that BD score ≥ 3 and TT > 3 mm was significantly predictive of nodal metastases, overall survival (OS) and relapse-free survival (RFS), while TT alone measured on biopsy samples was not. The same team 48 evaluated TBS on a larger series of 209 OSCC patients (76% cT1) treated with resection or with pre-operative chemotherapy and resection, without stratifying the patients according to treatment modalities. They found that ≥ 3 buds in the biopsy samples was predictive of lymph node metastases, and that TBS was significantly correlated with INF, Grading and LVI (p < 0.01). The authors pointed out that the TB cut-off point needs to be defined, and that the evaluation of TBS and TT needs to be standardised. Nayanar et al. 61 analysed 160 patients with oral cancer (Stage II = 48%) treated with wide excision and neck dissection and proposed a predictive score based on selected pathological features (rete pegs, pattern of invasion, TT, histologic differentiation) and site of tumour (buccal mucosa, tongue, other). The score ranged from 4 to 18; the authors found that a score of 4 is predictive of risk for lymph node metastasis of 5%; for scores of 10, 14 and 18, the risk was 31%, 67% and 91%, respectively. Sahoo et al. 49 studied 150 cT1-T2 patients treated with resection and neck dissection for OSCC. They compared three measurement modalities of the depth of invasion: TT1, TT2 (DOI) and TT3 (alternative DOI); according to the authors, TT2 corresponds to DOI, as defined in the TNM 8th Edition 37,38. They found that TT2 (DOI) and LVI correlate with nodal metastases.
Discussion
To our knowledge, this is the first comprehensive review correlating biological tumour characteristics between biopsy and corresponding pathologic specimen with an evidence-based method. Unfortunately, the studies that met the inclusion criteria had a level of evidence of 3 and 4 according to the AJCC on Cancer Levels of Evidence classification 20. It is worth stressing a criticality common to all: namely that they differ in the design of the study, selection of patients, oral subsite of cancer and in choice of pathological markers such as DOI, TT and budding score; for this reason, the results are not comparable. Furthermore, many authors have measured the depth of the invasion differently than what is foreseen in the TNM 8th Edition, even when published after its release. In this regard, the paper of Driven et al. that quantified the impact of the stage migration on patients’ prognosis using TT and DOI in a retrospective cohort of 456 OSCC patients is interesting. They found similar stage category and prognosis regardless of the measurement used 62. This review highlights several other critical issues.
Biopsy technique
The patients evaluated by Almangush 58, Seki 48 and Seki-Soda 60 underwent incisional biopsy; those studied by Nayanar 61 had an incisional or wedge biopsy; those in the study of Sahoo 49 were treated with an excisional biopsy. The authors did not provide more details on the procedures applied to perform the incisional/excisional biopsy. This information is important since the reliability of the biopsy sample strictly depends on the quality and quantity of the tissue taken. Seki et al. 59 did not specify the biopsy modalities in their first report, but in a later study aimed to evaluate the relationship between TBS assessed in OSCC biopsy specimens and lymph node metastases (LNM), recommending that incisional biopsy be performed peripherally to the cancer so as to obtain a significant amount of non-necrotic tissue from the centre of the tumour 48.
Depth of biopsy
It should also be stressed that the biopsy sample should be deep enough to possibly include the entire tumour infiltration front and underlying healthy tissue 48. Reliability of biopsy (incisional, wedge, punch, excisional) is influenced by the depth of the sample because it is unlikely that specimens always include tumour stroma on the invasive front, which is adequate to evaluate the relationships between the various components of the tumour microenvironment (TME) 48,58,59. In fact, tissue biomarkers are the morphological expression of the TME, or the field in which the immune system and the tumour interplay. Inside TME cancer cells, non-tumour cells and stroma are in a continuous and dynamic relationship, and any change within the TME may reflect changes of the balance between the immune system and tumour 63. In this context, the role of biopsy is not only diagnostic, but also predictive, since biopsies should include the invasive front, the behaviour of tumour cells in the TME interface and biomarkers that provide useful information to guide the therapeutic choice 15,64,65-67. Leite et al. 66, in a recent preliminary study on biopsy samples from 56 OSCC cases, highlighted the possible importance of the correlation between grading, predominant mode of invasion and TB intensity. The authors classified the mode of invasion in 4 degrees, similar to the proposal of Shimuzu 54; they also graded TB as low-intensity (5 buds in one single x200 power field) and high- intensity (≥ 5 buds in one single x200 power field). The majority of cases studied (66.1%) were high-intensity TB; all cases with the worst mode of invasion showed high-intensity TB, while no association was found between TB and histopathological grading. They concluded that both TB and mode of invasion in OSCC diagnostic specimens could help to select patients who could benefit from more aggressive treatment. This paper has some critical issues, such as the biopsy performed in the central part of the tumour, which is rich in necrotic tissue that must be eliminated, and the lack of follow-up. Therefore, these promising data require confirmation on larger series with a longer follow-up. A large biopsy on the surface (at least 8 mm) and depth (at least 5 mm) could allow an assessment of the microenvironment in early cancers, but does not solve the problem 48,64. In this regard, Dhanda 64 compared TT measurement on biopsies and the corresponding post-operative samples reported in the medical records of 93 patients operated on for oral cancer; we have not included this paper in our review according to the exclusion criteria (point c) because those specimens were not revised by a pathologist. However, measurements reported in medical charts provide interesting information because in this series 20% of tumours had a tumour depth > 10 mm on post-operative specimens; on biopsies only 28% of samples had a thickness greater than the DOI calculated on the post-operative specimens. They therefore suggested performing a 10 mm deep punch biopsy, which should potentially include the invasive front in up to 80% of the cases analysed in this paper 64.
Additional biopsy related issues
It should also be pointed out that 17% of biopsy samples are not representative of the cancer due to technical errors such as fragmented, superficial, non-orientable samples and artifacts in the preparation of slides 58. For this reason, how the specimen is sectioned and oriented is important: slides are evaluable if sections are perpendicular and include all mucous, submucosal and muscle layers. On the contrary, tangential sectioning does not allow the evaluation of infiltration depth 68. In addition, biopsy and surgical procedures can sometimes make it difficult to measure the depth of invasion on post-operative specimens. This critical point is underlined by Berdugo who analysed the post-operative samples of 239 glossectomies 69: 5% had only a minimal residual of cancer and in 14% no tumour was found. He also emphasised that in 21/183 (11.5%) pT2 OSCCs the DOI was underestimated due to positivity of deep resection margins. Finally, it should be kept in mind that a large surgical biopsy may create an inflammatory reaction which alters the microenvironment and could promote the regional spread of cancer 70,71.
Changing the aim of biopsy
To plan the best treatment of a tumour, one must know its histopathological diagnosis, site, size and biological aggressiveness. Currently, the risk of developing lymph node metastases can be evaluated by measuring biomarkers such as Grading, PNI, LVI, positive resection margins, depth and mode of invasion and tumour budding on post-operative specimens. On the basis of this information, high-risk patients can be identified for treatment with post-operative radiotherapy or chemoradiotherapy. It is hoped that this predictive and prognostic information will be available for all patients, even those candidates for non-surgical therapies, at the end of the diagnostic process, so as to personalise the therapy for each. This review documents the possibility to reliably test these tissue biomarkers on biopsy samples. However, it is necessary that the biopsy technique and the methods of evaluation of biomarkers are standardised and validated in clinical trials on large case series before they can be used in clinical practice. For these reasons, the role of biopsy is changing and evaluation of a biopsy sample will allow not only to define the morphology of a tumour, but also to guide the therapeutic choice.
Clinical and imaging evaluation of depth of infiltration
The 8th edition of TNM suggests that the DOI of oral cancer is assessed pre-operatively with clinical and imaging investigations 38. It should be emphasised that clinical evaluation is subjective, depends on the experience and ability of each physician and is limited by anatomical conditions such as trismus and/or the patient’s intolerance to palpation for pain 72. Recently, prospective studies comparing pre-operative clinical and magnetic resonance imaging (MRI) evaluation 72, or MRI alone 50,73,74 with post-operative DOI have documented a good correlation of these investigations, especially in tumours with infiltration > 5 mm. On the contrary, other authors have reported an overestimation of T2 lesions and under-estimation of T4 cancers when clinical T staging is compared with histopathological data 75,76. These papers also highlight several critical issues related to imaging (MRI/computed tomography, CT) such as artifacts due to movement and dental fillings; the evaluation of peritumoural oedema and inflammation, and timing between imaging and biopsy (first imaging or biopsy? If imaging is performed after biopsy, how long does it take to get reliable information from MRI/CT?) 50,76,77. Tumour shrinkage of formalin-fixed post-operative specimens may interfere with comparing the DOI between MRI pre-operative imaging and post-operative specimens 72,78. A recent meta-analysis 79 documented a high correlation of TT measured by intraoral ultrasound and histopathology mainly in T1-2 tongue cancers (p < 0.001), although it is operator-dependent and often overestimates exophytic tumours 80,81.
Future directions
Other non-invasive diagnostic modalities are being considered to support evidence-based clinical decision-making, in particular radiomics and liquid biopsy.
Radiomics is an emerging translational field of research. Thanks to the extraction of mathematically defined parameters from routine medical images it is possible to generate large-scale sets of information that can be correlated with OS and treatment-related toxicity and can also be used to identify new biomarkers to be implemented in daily clinical practice 82. Currently, there are few but promising published studies on the application of radiomics in oral cancer with CT or MRI 83-85. Probably, if the role of radiomics will be confirmed with standardised methodology on a large number of patients, these results would help to promote cancer treatment towards personalised precision medicine 82,86.
Liquid biopsy is particularly promising as an alternative to surgical biopsy. It allows assessment of biomarkers in fluids (serum, saliva, urine, etc.) such as circulating tumour cells (CTC), DNA and RNA fragments (miRNA), exosomes that originate from cancerous cells, and their characteristics, particularly mutations and number of somatic alterations 87-90. Liquid biopsy theoretically provides the individual molecular profile of each cancer over time, and could allow physicians to diagnose a tumour, plan tailored therapy and monitor cancer evolution 91,92. Unfortunately, no circulating biomarker has yet been validated for routine use in clinical practice for OSCC, because alongside the promising potentials, there are also considerable critical issues 93,94. For example, the levels of circulating DNA fragments derived from the tumour (cfDNA) represent a small fraction (up to 10%) of the total cfDNA and variations between patients related to cancer stage, tumour vascularisation, tumour burden and apoptosis rate can compromise the accuracy of the tests 92,95-97.
Conclusions
The traditional role of biopsy is evolving; in the future, a single procedure will allow to define the histology of a tumour and to identify predictive and prognostic biomarkers. The data emerging from this review of the literature, even if heterogeneous and fragmented, suggest that the evaluation of markers on biopsy samples, mainly the DOI and growth characteristics of the invasive front (INF, TB) could provide useful indications for planning tailored treatments. Minimally invasive procedures such as liquid biopsy are also promising, although only preliminary results are currently available which require further confirmation. Further clinical studies are needed to standardise and validate clinical and imaging evaluation, surgical and liquid biopsy technique, sampling of specimens, and choice of biomarkers and their assessment before introducing these diagnostic and predictive modalities in daily clinical practice.
Figures and tables
References
- 1.Ferlay J, Colombet M, Soerjomaratam I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 2019;144:1941-1953. https://doi.org/10.1002/ijc.31937 10.1002/ijc.31937 [DOI] [PubMed] [Google Scholar]
- 2.Wu K, Wei J, Liu Z, et al. Can pattern and depth of invasion predict lymph node relapse and prognosis in tongue squamous cell carcinoma. BMC Cancer 2019;9:714. https://doi.org/10.1186/s12885-019-5859-y 10.1186/s12885-019-5859-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fitzmaurice C, Abate D, Abbasi N, et al. Global burden of disease cancer collaboration global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability and disability-adjusted life-years for 29 cancer groups. 1990 to 2017. Jama Oncol 2019;5:1749-1768. https://doi.org/10.1001/jamaoncol.2019.2996 10.1001/jamaoncol.2019.2996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen SW, Zhang Q, Guo ZM, et al. Trends in clinical features and survival of oral cavity cancer: fifty years of experience with 3,362 consecutive cases from a single institution. Cancer Manag Res 2018;10:4523-4535. https://doi.org/10.2147/CMAR.S171251 10.2147/CMAR.S171251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paderno A, Morello R, Piazza C. Tongue carcinoma in young adults: a review of the literature. Acta Otorhinolaryngol Ital 2018;38:175-180. https://doi.org/10.14639/0392-100X-1932 10.14639/0392-100X-1932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kharwala SS, Hatsukami DK, Stepanov I, et al. Patterns of tobacco cessation attempts and symptoms experienced among smokers with head and neck squamous cell carcinoma. JAMA Otolaryngol Head Neck Surg 2018;144:477-482. https://doi.org/10.1001/jamaoto.2018.0249 10.1001/jamaoto.2018.0249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bala MM, Strzeszynski L, Topor-Madry R, et al. Mass media interventions for smoking cessation in adults. Cochrane Database Syst Rev 2013;6:CD004704. https://doi.org/10.1002/14651858.CD004704.pub3 10.1002/14651858.CD004704.pub3 [DOI] [PubMed] [Google Scholar]
- 8.Challapalli SD, Simpson MC, Adjei Boakye E, et al. Head and neck squamous cell carcinoma in adolescents and young adults: survivorship patterns and disparities. J Adolesc Young Adult Oncol 2018;7:472-479. https://doi.org/10.1089/jayao.2018.0001 10.1089/jayao.2018.0001 [DOI] [PubMed] [Google Scholar]
- 9.Ng HJ, Iyer NG, Tan MH, et al. Changing epidemiology of oral squamous cell carcinoma of the tongue: a global study. Head Neck 2017;39:297-304. https://doi.org/10.1002/hed.24589 10.1002/hed.24589 [DOI] [PubMed] [Google Scholar]
- 10.Hussein AA, Helder MN, de Visscher JG, et al. Global incidence of oral and oropharynx cancer in patients younger than 45 years versus older patients: a systematic review. Eur J Cancer 2017;82:115-127. https://doi.org/10.1016/j.ejca.2017.05.02.6 10.1016/j.ejca.2017.05.02.6 [DOI] [PubMed] [Google Scholar]
- 11.Yete S, D’Souza W, Saranath D, et al. High-risk human papillomavirus in oral cancer: clinical implications. Oncology 2018;94:133-141. https://doi.org/10.1159/000485322 10.1159/000485322 [DOI] [PubMed] [Google Scholar]
- 12.Hübbers CU, Akgül B. HPV and cancer of the oral cavity. Virulence 2015;6:244-248. https://doi.org/10.1080/21505594.2014.999570 10.1080/21505594.2014.999570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Russo D, Merolla F, Varricchio S, et al. Epigenetics of oral and oropharyngeal cancers (Review). Biomed Rep 2018;9:275-283. https://doi.org/10.3892/br.2020.1290 10.3892/br.2020.1290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lam DK, Schmidt BL. Molecular biology of head and neck cancer: therapeutic implications. Bagheri SC, Bell RB, Khan HA, editors. Current therapy in oral and maxillofacial surgery. Amsterdam: Elsevier Inc; 2012. pp. 92-101. https://doi.org/10.1016/B978-1-4160-2527-6.00010-4 10.1016/B978-1-4160-2527-6.00010-4 [DOI] [Google Scholar]
- 15.Zhu Y, Liu H, Xie N, et al. Impact of tumour budding in head and neck squamous cell carcinoma: a meta-analysis. Head Neck 2019;41:542-550. https://doi.org/10.1002/hed.25462 10.1002/hed.25462 [DOI] [PubMed] [Google Scholar]
- 16.Naruse T, Yanamoto S, Matsushita Y, et al. Cetuximab for the treatment of locally advanced and recurrent/metastatic oral cancer: an investigation of distant metastasis. Mol Clin Oncol 2016;5:246-252. https://doi.org/10.3892/mco.2016.928 10.3892/mco.2016.928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weinstein JN, Collisson EA, Mills GB, et al. The Cancer Genome Atlas pan-cancer analysis project. Nat Genet 2013;45:113-120. https://doi.org/10.1038/ng.2764 10.1038/ng.2764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leichsering J, Horak P, Kreutzfeldt S, et al. Variant classification in precision oncology. Int J Cancer 2019;145:2996-3010. https://doi.org/10.1002/ijc.32358 10.1002/ijc.32358 [DOI] [PubMed] [Google Scholar]
- 19.Sankar PL, Parker LS. The Precision Medicine Initiative’s All of Us Research Program: an agenda for research on its ethical, legal, and social issues. Genet Med 2017;19:743-750. https://doi.org/10.1038/gim.2016.183 10.1038/gim.2016.183 [DOI] [PubMed] [Google Scholar]
- 20.Amin MB, Greene FL, Edge SB, et al. The Eighth Edition AJCC Cancer Staging Manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. Ca Cancer J Clin 2017;67:93-99. https://doi.org/10.3322/caac.21388 10.3322/caac.21388 [DOI] [PubMed] [Google Scholar]
- 21.NCCN Clinical Practice Guidelines in Oncology. Head and Neck Cancers v 1-2020 - February 12, 2020. NCCN.org.
- 22.Orlandi E, Alfieri S, Simon C, et al. Treatment challenges in and outside a network setting: head and neck cancers. Eur J Surg Oncol 2019;45:40-45. https://doi.org/10.1016/j.ejso.2018.02.007 10.1016/j.ejso.2018.02.007 [DOI] [PubMed] [Google Scholar]
- 23.Orlandi E, Licitra L. Personalized medicine and the contradictions and limits of first-generation deescalation trials in patients with Human Papillomavirus-positive oropharyngeal cancer. JAMA Otolaryngol Head Neck Surg 2018;144:99-100. https://doi.org/10.1001/jamaoto.2017.2308 10.1001/jamaoto.2017.2308 [DOI] [PubMed] [Google Scholar]
- 24.Coyle KM, Boudreau JE, Marcato P. Genetic mutations and epigenetic modifications driving cancer and informing Precision Medicine. Biomed Res Int 2017;2017:9620870. https://doi.org/10.1155/2017/9620870 10.1155/2017/9620870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Garraway LA, Verweij J, Ballman KV. Precision oncology: an overview. J Clin Oncol 2013;31:1803-1805. https://doi.org/10.1200/JCO.2013.49.4799 10.1200/JCO.2013.49.4799 [DOI] [PubMed] [Google Scholar]
- 26.Zhong L, Liu Y, Wang K, et al. Biomarkers: paving stones on the road towards the personalized precision medicine for oral squamous cell carcinoma. BMC Cancer 2018;18:911. https://doi.org/10.1186/s12885-018-4806-7 10.1186/s12885-018-4806-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nor JE, Gutkind JS. Head and neck cancer in the new era of precision medicine. J Dent Res 2018;97:601-602. https://doi.org/10.1177/0022034518772278 10.1177/0022034518772278 [DOI] [PubMed] [Google Scholar]
- 28.Giefing M, Wierzbicka M, Szyfter K, et al. Moving towards personalized therapy in head and neck squamous cell carcinoma through analysis of next generation sequencing data. Eur J Cancer 2016;55:147-157. https://doi.org/10.1016/j.ejca.2015.10.070 10.1016/j.ejca.2015.10.070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bernier J, Domenge C, Ozsahin M, et al. Postoperative irradiation with or without concomitant chemotherapy for locally advanced head and neck cancer. N Engl J Med. 2004;350:1945-1952. https://doi.org/10.1056/NEJMoa032641 10.1056/NEJMoa032641 [DOI] [PubMed] [Google Scholar]
- 30.Cooper JS, Pajak TF, Forastiere AA, et al. Postoperative concurrent radiotherapy and chemotherapy for high-risk squamous-cell carcinoma of the head and neck. N Engl J Med. 2004;350:1937-1944. https://doi.org/10.1056/NEJMoa032646 10.1056/NEJMoa032646 [DOI] [PubMed] [Google Scholar]
- 31.Bernier J, Cooper JS, Pajak TF, et al. Defining risk levels in locally advanced head and neck cancers: a comparative analysis of concurrent postoperative radiation plus chemotherapy trials of the EORTC (#22931) and RTOG (#9501). Head Neck 2005;27:843-850. https://doi.org/10.1002/hed.20279 10.1002/hed.20279 [DOI] [PubMed] [Google Scholar]
- 32.Cooper JS, Zhang Q, Pajak TF, et al. Long-term follow-up of the RTOG 9501/intergroup phase III trial: postoperative concurrent radiation therapy and chemotherapy in high-risk squamous cell carcinoma of the head and neck. Int J Radiat Oncol Biol Phys 2012;84:1198-1205. https://doi.org/10.1016/j.ijrobp.2012.05.008 10.1016/j.ijrobp.2012.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen WC, Lai CH, Fang CC, et al. Identification of high-risk subgroups of patients with oral cavity cancer in need of postoperative adjuvant radiotherapy or chemo-radiotherapy. Medicine (Baltimore) 2016;95(22):e3770. https://doi.org/10.1097/MD.0000000000003770 10.1097/MD.0000000000003770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fan KH, Chen YC, Lin CY, et al. Postoperative radiotherapy with or without concurrent chemotherapy for oral squamous cell carcinoma in patients with three or more minor risk factors: a propensity score matching analysis. Radiat Oncol 2017;12:184. https://doi.org/10.1186/s13014-017-0910-0 10.1186/s13014-017-0910-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cheraghlou S, Schettino A, Zogg CK, et al. Changing prognosis of oral cancer: an analysis of survival and treatment between 1973 and 2014. Laryngoscope 2018;128:2762-2769. https://doi.org/10.1002/lary.27315 10.1002/lary.27315 [DOI] [PubMed] [Google Scholar]
- 36.Ribeiro IP, Caramelo F, Esteves L, et al. Genomic and epigenetic signatures associated with survival rate in oral squamous cell carcinoma patients. J Cancer 2018;9:1885-1895. https://doi.org/10.7150/jca.23239 10.7150/jca.23239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Amin MB, Edge S, Greene F, et al. AJCC Cancer Staging Manual. Eigth Edition. New York: Springer International Publishing; 2017. [Google Scholar]
- 38.Lydiatt WM, Patel SG, O’Sullivan B, et al. Head and neck cancers. Major changes in the American Joint Committee on Cancer eighth edition Cancer Staging Manual. Ca Cancer J Clin 2017;67:122-137. https://doi.org/10.3322/caac.21389 10.3322/caac.21389 [DOI] [PubMed] [Google Scholar]
- 39.Fakih AR, Rao RS, Borges AM, et al. Elective versus therapeutic neck dissection in squamous carcinoma of tongue a prospective randomized trial. Am J Surg 1989;158:309-313. https://doi.org/10.1016/0002-9610(89)90122-0 10.1016/0002-9610(89)90122-0 [DOI] [PubMed] [Google Scholar]
- 40.Fukano H, Matsuura H, Hasegawa Y, et al. Depth of invasion as a predictive factor for cervical lymph node metastasis in tongue carcinoma. Head Neck 1997;19:205-10. https://doi.org/10.1002/(sici)1097-0347(199705)19:3<205::aid-hed7>3.0.co;2-6 [DOI] [PubMed] [Google Scholar]
- 41.Kukreja P, Parekh D, Roy P. Practical challenges in measurement of invasion in oral squamous cell carcinoma: pictographical documentation to improve consistency of reporting per the AJCC 8th Edition recommendations. Head Neck Pathol 2020;14:419-427. https://doi.org/10.1007/s12105-019-01047-9 10.1007/s12105-019-01047-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Almangush A, Bello IO, Coletta RD, et al. For early-stage oral tongue cancer, depth of invasion and worst pattern of invasion are the strongest pathological predictors for locoregional recurrence and mortality. Virchows Arch 2015;467:39-46. https://doi.org/10.1007/s00428-015-1758-z 10.1007/s00428-015-1758-z [DOI] [PubMed] [Google Scholar]
- 43.Larson AR, Kemmer J, Formeister E, et al. Beyond depth of invasion: adverse pathologic tumour features in early oral tongue squamous cell carcinoma. Laryngoscope 2020;130:1715-1720. https://doi.org/10.1002/lary.28241. 10.1002/lary.28241 [DOI] [PubMed] [Google Scholar]
- 44.den Toom IJ, Janssen LM, van Es RJJ, et al. Depth of invasion in patients with early stage oral cancer staged by sentinel node biopsy. Head Neck 2019;41:2100-2106. https://doi.org/10.1002/hed.25665 10.1002/hed.25665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Almangush A, Pirinen M, Heikkinen I, et al. Tumour budding in oral squamous cell carcinoma: a meta-analysis. Br J Cancer 2018:118:577-586. https://doi.org/10.1038/bjc.2017.425 10.1038/bjc.2017.425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Almangush A, Heikkinen I, Bakhti N, et al. Prognostic impact of tumour –stroma ratio in early-stage oral tongue cancers. Histopathology 2018;72:1128-1135. https://doi.org/10.1111/his.13481 10.1111/his.13481 [DOI] [PubMed] [Google Scholar]
- 47.Hori Y, Kubota A, Yokose T, et al. Association between pathological invasion patterns and late lymph node metastases in patients with surgically treated clinical N0 early tongue carcinoma. Head Neck 2020;42:238-243. https://doi.org/10.1002/hed.25994 10.1002/hed.25994 [DOI] [PubMed] [Google Scholar]
- 48.Seki M, Sano T, Yokoo S, et al. Tumour budding evaluated in biopsy specimens is a useful predictor of prognosis in patients with cN0 early stage oral squamous cell carcinoma. Histopathology 2017;70:869-879. https://doi.org/10.1111/his.13144 10.1111/his.13144 [DOI] [PubMed] [Google Scholar]
- 49.Sahoo A, Panda S, Mohanty N, et al. Perineural, lymphovascular and depths of invasion in extrapolating nodal metastasis in oral cancer. Clin Oral Investig 2020;24:747-755. https://doi.org/10.1007/s00784-019-02921-0 10.1007/s00784-019-02921-0 [DOI] [PubMed] [Google Scholar]
- 50.Vidiri A, Panfili M, Boellis A, et al. The role of MRI-derived depth of invasion in staging oral tongue squamous cell carcinoma: inter-reader and radiological-pathological agreement. Ann Radiol 2020;61:344-352. https://doi.org/10.1177/0284185119862946 10.1177/0284185119862946 [DOI] [PubMed] [Google Scholar]
- 51.Prall F. Tumour budding in colorectal carcinoma. Histopathology 2007;50;151-162. https://doi.org/10.1111/j.1365-2559.2006.02551.x 10.1111/j.1365-2559.2006.02551.x [DOI] [PubMed] [Google Scholar]
- 52.Jensen DH, Dabelsteen E, Specht L, et al. Molecular profiling of tumour budding implicates TGFb-mediated epithelial-mesenchymal transition as a therapeutic target in oral squamous cell carcinoma. J Pathol 2015;236:505-516. https://doi.org/10.1002/path.4550 10.1002/path.4550 [DOI] [PubMed] [Google Scholar]
- 53.Attramadal CG, Kumar S, Boysen ME, et al. Tumour budding, EMT and cancer stem cells in T1-2/N0 oral squamous cell carcinomas. Anticancer Res 2015; 35:6111-6120. [PubMed] [Google Scholar]
- 54.Shimizu S, Miyazaki A, Sonoda T, et al. Tumour budding is an independent marker in early stage oral squamous cell carcinoma: with special reference to the mode of invasion and worst pattern of invasion. Plos One 2018;13:e0195451. https://doi.org/10.1371/journal.pone.0195451 10.1371/journal.pone.0195451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Almangush A, Youssef O, Pirinen H, et al. Does evaluation of tumour budding in diagnostic biopsies have a clinical relevance? A systematic review. Histopathology 2019;74:536-544. https://doi.org/10.1111/his.13793 10.1111/his.13793 [DOI] [PubMed] [Google Scholar]
- 56.Wang K, Ma W, Wang J, et al. Tumour-stroma ratio is an independent predictor for survival in esophageal squamous cell carcinoma. J Thorac Oncol 2012;7:1457-1461. https://doi.org/10.1097/JTO.0b013e318260dfe8 10.1097/JTO.0b013e318260dfe8 [DOI] [PubMed] [Google Scholar]
- 57.Wu J, Liang C, Chen M, et al. Association between tumour-stroma ratio and prognosis in solid tumour patients: a systematic review and meta-analysis. Oncotarget 2016;7:68954-68965. https://doi.org/10.18632/oncotarget.12135 10.18632/oncotarget.12135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Almangush A, Leivo I, Siponen M, et al. Evaluation of the budding and depth of invasion (BD) model in oral tongue cancer biopsies. Virchows Arch 2018;472:231-236. https://doi.org/10.1007/s00428-017-2212-1 10.1007/s00428-017-2212-1 [DOI] [PubMed] [Google Scholar]
- 59.Seki M, Sano T, Yokoo S, et al. Histologic assessment of tumour budding in preoperative biopsies to predict nodal metastasis in squamous cell carcinoma of the tongue and floor of the mouth. Head Neck 2016;38:E1582-1590. https://doi.org/10.1002/hed.24282 10.1002/hed.24282 [DOI] [PubMed] [Google Scholar]
- 60.Seki-Soda M, Sano T, Koshi H, et al. Histopathological changes in tumour budding between biopsy and resected specimens from patients treated with preoperative S-1 chemotherapy for oral cancer. J Oral Pathol Med 2019;48:880-887. https://doi.org/10.1111/jop.12923 10.1111/jop.12923 [DOI] [PubMed] [Google Scholar]
- 61.Nayanar SK, Tripathy JP, Duraisamy K, et al. Prognostic efficiency of clinicopathologic score to predict cervical ymph node metastasis in oral squamous cell carcinoma. J Oral Maxillofac Pathol 2019;23:36-42. https://doi.org/10.4103/jomfp.JOMFP_132_17 10.4103/jomfp.JOMFP_132_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dirven R, Ebrahimi A, Moeckelmann N, et al. Tumour thickness versus depth of invasion – Analysis of the 8th edition American Joint Committee on Cancer Staging for oral cancer. Oral Oncol 2017;74:30-33. https://doi.org/10.1016/j.oraloncology.2017.09.007 10.1016/j.oraloncology.2017.09.007 [DOI] [PubMed] [Google Scholar]
- 63.Merlano MC, Abbona A, Denaro N, et al. Knowing the tumour microenvironment to optimise immunotherapy. Conference Paper. Acta Otorhinolaryngol Ital 2019;39:18-21. https://doi.org/10.14639/0392-100X-2481 10.14639/0392-100X-2481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dhanda J, Uppal N, Chowlia H, et al. Features and prognostic utility of biopsy in oral squamous cell carcinoma. Head Neck 2016;38:E1857-1862. https://doi.org/10.1002/hed.24335 10.1002/hed.24335 [DOI] [PubMed] [Google Scholar]
- 65.Kolenda T, Przybyla W, Kapalczynska M, et al. Tumour microenvironment - Unknown niche with powerful therapeutic potential. Rep Pract Oncol Radiother 2018;23:143-153. https://doi.org/10.1016/j.rpor.2018.01.004 10.1016/j.rpor.2018.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Leite CF, Silva KDD, Horta MCR, et al. Can morphological features evaluated in oral cancer biopsies influence in decision-making? A preliminary study. Pathol Res Pract 2020;216:153138. https://doi.org/10.1016/j.prp.2020.153138. 10.1016/j.prp.2020.153138 [DOI] [PubMed] [Google Scholar]
- 67.Elseragy A, Salo T, Coletta RD, et al. A proposal to revise the histopathologic grading system of early oral tongue cancer incorporating tumour budding. Am J Surg Pathol 2019;43:703-709. https://doi.org/10.1097/PAS.0000000000001241 10.1097/PAS.0000000000001241 [DOI] [PubMed] [Google Scholar]
- 68.Heerema MGJ, Melchers LJ, Roodenburg JNL, et al. Reproducibility and prognostic value of pattern of invasion scoring in low-stage oral squamous cell carcinoma. Histopathology 2016;68:338-397. https://doi.org/10.1111/his.12754 10.1111/his.12754 [DOI] [PubMed] [Google Scholar]
- 69.Berdugo J, Thompson LDR, Purgina B, et al. Measuring depth of invasion in early squamous cell carcinoma of the oral tongue: positive deep margin, extratumoural perineural invasion, and other challenges. Head Neck Pathol 2019;13:154-161. https://doi.org/10.1007/s12105-018-0925-3 10.1007/s12105-018-0925-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Seppala M, Tervo S, Pohjola K, et al. The association and prognostic relevance of cancerous inhibitor of protein phosphatase 2A and inflammation in tongue squamous cell carcinoma. APMIS 2015;123:1007-1015. https://doi.org/10.1111/apm.12462 10.1111/apm.12462 [DOI] [PubMed] [Google Scholar]
- 71.Lundqvist L, Stenlund H, Laurell G, et al. The importance of stroma inflammation in squamous cell carcinoma of the tongue. J Oral Pathol Med 2012;41:379-383. https://doi.org/10.1111/j.1600-0714.2011.01107.x 10.1111/j.1600-0714.2011.01107.x [DOI] [PubMed] [Google Scholar]
- 72.Alsaffar HA, Goldstein DP, King EV, et al. Correlation between clinical and MRI assessment of depth of invasion in oral tongue squamous cell carcinoma. J Otolaryngol Head Neck Surg 2016;45:61. https://doi.org/10.1186/s40463-016-0172-0 10.1186/s40463-016-0172-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jayasankaran SC, Chelakkot PG, Karippaliyil M, et al. Magnetic resonance imaging: a predictor of pathological tumour dimensions in carcinoma of the anterior two-thirds of tongue. Prospective evaluation. Indian J Cancer 2017;54:508-513. https://doi.org/10.4103/ijc.IJC_319_17 10.4103/ijc.IJC_319_17 [DOI] [PubMed] [Google Scholar]
- 74.Morand GB, Ikenberg K, Vital DG, et al. Preoperative assessment of CD44-mediated depth of invasion as predictor of occult metastases in early oral squamous cell carcinoma. Head Neck 2019;41:950-958. https://doi.org/10.1002/hed.25532 10.1002/hed.25532 [DOI] [PubMed] [Google Scholar]
- 75.Goel V, Parihar PS, Parihar A, et al. Accuracy of MRI in prediction of tumour thickness and nodal stage in oral tongue and gingivobuccal cancer with clinical correlation and staging. J Clin Diagn Res 2016;10:TC01-5. https://doi.org/10.7860/JCDR/2016/17411.7905 10.7860/JCDR/2016/17411.7905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mao MH, Wang S, Feng ZE, et al. Accuracy of magnetic resonance imaging in evaluating the depth of invasion of tongue cancer. A prospective cohort study. Oral Oncol 2019;91:79-84. https://doi.org/10.1016/j.oraloncology.2019.01.021 10.1016/j.oraloncology.2019.01.021 [DOI] [PubMed] [Google Scholar]
- 77.Franceschi L, Santo JM, Abreu AM, et al. Staging of oral cavity cancer in the 8th edition of the TNM classification: the role of computed tomography in the assessment of depth of invasion and extranodal extension. Arch Head Neck Surg 2018;47:e0869. https://doi.org/10.4322/ahns.2018.0869 10.4322/ahns.2018.0869 [DOI] [Google Scholar]
- 78.Chen CH, Hsu MY, Jiang RS, et al. Shrinkage of head and neck cancer specimens after formalin fixation. J Chin Med Assoc 2012;75:109-113. https://doi.org/10.1016/j.jcma.2012.02.006 10.1016/j.jcma.2012.02.006 [DOI] [PubMed] [Google Scholar]
- 79.Klein Nulent TJW, Noorlag R, Van Cann EM, et al. Intraoral ultrasonography to measure tumour thickness of oral cancer: a systematic review and meta-analysis. Oral Oncol 2018;77:29-36. https://doi.org/10.1016/j.oraloncology.2017 10.1016/j.oraloncology.2017 [DOI] [PubMed] [Google Scholar]
- 80.Tarabichi O, Bulbul MG, Kanamuri VV, et al. Utility of intraoral ultrasound in managing oral tongue squamous cell carcinoma: systematic review. Laryngoscope 2019;129:662-670. https://doi.org/10.1002/lary.27403 10.1002/lary.27403 [DOI] [PubMed] [Google Scholar]
- 81.Iida Y, Kamijo T, Kusafuka K, et al. Depth of invasion in superficial oral tongue carcinoma quantified using intraoral ultrasonography. Laryngoscope 2018;128:2778-2782. https://doi.org/10.1002/lary.27305 10.1002/lary.27305 [DOI] [PubMed] [Google Scholar]
- 82.Rizzo S, Botta F, Raimondi S, et al. Radiomics: the facts and the challenges of image analysis. Eur Radiol Exp 2018;2:36. https://doi.org/10.1186/s41747-018-0068-z 10.1186/s41747-018-0068-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Haider SP, Burtness B, Yarbrough WG, et al. Applications of radiomics in precision diagnosis, prognostication and treatment planning of head and neck squamous cell carcinomas. Cancers Head Neck 2020;5:6. https://doi.org/10.1186/s41199-020-00053-7 10.1186/s41199-020-00053-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mes SW, van Velden FHP, Peltenburg B, et al. Outcome prediction of head and neck squamous cell carcinoma by MRI radiomic signatures. Eur Radiol 2020;30:6311-6321. https://doi.org/10.1007/s00330-020-06962-y 10.1007/s00330-020-06962-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pan X, Zhang T, Yang Q, et al. Survival prediction for oral tongue cancer patients via probabilistic genetic algorithm optimized neural network models. Br J Radiol 2020;93:20190825. https://doi.org/10.1259/bjr.20190825 10.1259/bjr.20190825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Romeo V, Cuocolo R, Ricciardi C, et al. Prediction of tumor grade and nodal status in oropharyngeal and oral cavity squamous-cell carcinoma using a radiomic approach. Anticancer Res 2020;40:271-280. https:/doi.org/10.21873/anticanres.13949 10.21873/anticanres.13949 [DOI] [PubMed] [Google Scholar]
- 87.Castagnola M, Scarano E, Passali GC, et al. Salivary biomarkers and proteomics: future diagnostic and clinical utilities. Acta Otorhinolaryngol Ital 2017;37:94-101. https://doi.org/10.14639/0392-100x-1598 10.14639/0392-100x-1598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Xiao C, Song F, Zheng YL, et al. Exosomes in head and neck squamous cell carcinoma. Front Oncol 2019;9:894. https://doi.org/10.3389/fonc.2019.00894 10.3389/fonc.2019.00894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Cree IA, Uttley L, Buckley Woods H, et al. The evidence base for circulating tumour DNA blood-based biomarkers for the early detection of cancer: a systematic mapping review. BMC Cancer 2017;17:697. https://doi.org/10.1186/s12885-017-3693-7 10.1186/s12885-017-3693-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mazunder S, Datta S, Ray JG, et al. Liquid biopsy: miRNA as a potential biomarker in oral cancer. Cancer Epidemiol 2019;58:137-145. https://doi.org/10.1016/j.canep.2018.12.008 10.1016/j.canep.2018.12.008 [DOI] [PubMed] [Google Scholar]
- 91.Lousada-Fernandez F, Rapado-Gonzalez O, Lopez-Cedrun JL, et al. Liquid biopsy in oral cancer. Int J Mol Sci 2018;19:1704. https://doi.org/10.3390/ijms19061704 10.3390/ijms19061704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Arneth B. Update on the types and usage of liquid biopsies in the clinical setting: a systematic review. BMC Cancer 2018;18:527. https://doi.org/10.1186/s12885-018-4433-3 10.1186/s12885-018-4433-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ribeiro IP, Barbosa de Melo J, Carreira IM. Head and neck cancer: searching for genomic and epigenetic biomarkers in body fluids – the state of art. Mol Cytogenet 2019;12:33. https://doi.org/10.1186/s13039-019-0447-z 10.1186/s13039-019-0447-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hussein AA, Forouzanfar T, Bloemena E, et al. A review of the most promising biomarkers for early diagnosis and prognosis prediction of tongue squamous cell carcinoma. Br J Cancer 2018;119:724-736. https://doi.org/10.1038/s41416-018-0233-4. 10.1038/s41416-018-0233-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Economopoulou P, Kotsanti I, Kyrodimos E, et al. Liquid biopsy: an emerging prognostic and predictive tool in head and neck squamous cell carcinoma (HNSCC). Focus on circulating tumour cells (CTCs). Oral Oncol 2017;74:83-89. https://doi.org/10-1016/j.oraloncology.2017.09.012 10.1016/j.oraloncology.2017.09.012 [DOI] [PubMed] [Google Scholar]
- 96.Spector ME, Farlow JL, Haring CT, et al. The potential for liquid biopsies in head and neck cancer. Discover Med 2018;25:251-257. [PMC free article] [PubMed] [Google Scholar]
- 97.Van Ginkel JH, Huibers MMH, Noorlag R, et al. Liquid biopsy: a future tool for posttreatment surveillance in head and neck cancer? Pathobiology 2017;84:115-120. https://doi.org/10.1159/00045286 10.1159/00045286 [DOI] [PubMed] [Google Scholar]


