Abstract
Background and aim:
Vulvar hematoma is often puerperal. A case of non-puerperal vulvovaginal hematoma is rare in the literature. There is no consensus on the management of vulvovaginal hematoma. In this study, we discussed the approach to a rare case of non-puerperal vulvar hematoma.
Case:
We present the case of a 14-year-old adolescent female with a severe vulvar non-obstetric hematoma that occurred after she had been illegally and voluntarily married.
Conclusions:
In conclusion; vulvar hematoma is the most common non-obstetric cause of perineal trauma and carries the risk of mortality by causing hypovolemic shock. The conservative approach is preferred for small and non-growing hematomas; however, surgical hematoma drainage is used for large and enlarging hematomas. Selective arterial embolization procedure is not common as the required equipment is not available in all healthcare facilities.
Keywords: Adolescent, vulva, hematoma, trauma
Introduction
Hematoma is a soft mass caused by the accumulation of blood due to trauma in subcutaneous soft tissue. Vulva, supported by a rich vascular structure. Vulvar hematoma is often puerperal and non-puerperal causes are rare. A puerperal vulvar hematoma usually was seen within 24 hours after birth. Non-puerperal causes include straddle injury, sexual abuse, rape, water skiing and coagulopathies (1-7). Also, spontaneous rupture of the internal iliac artery has been reported in the literature due to atherosclerosis (8).
A case of non-puerperal vulvovaginal hematoma is rare in the literature. Therefore, there is no consensus on the management of vulvovaginal hematoma.
Case
In this article, we present the case of a 14-year-old Syrian female refugee with a severe vulvar non-obstetric hematoma that occurred after she had been illegally and voluntarily married. A 14-year-old adolescent girl with gravida 0 and para 0 and no other disease and allergy history. She has presented to our hospital with complaints of vaginal bleeding, vulvar mass, and pain on the second day after first coitus and urinary retention for 24 hours. The patient was transferred from the emergency unit to our clinic and hospitalized. In her perineum examination, there was generalized edema in the vulva and vagina, and approximately 12x10 cm deviated mass consistent with hematoma, covering the right labium minus and labium majus and the urethra. Generalize edema was observed in the periurethral region and a vesical globe was seen. There was an actively bleeding 2x2 cm laceration extending from 9 o’clock position in the hymen to the vagina. Cervix was nulliparous, clean and consistent with the patient’s age. The findings of her physical examination were 110 beats/min heart rate and 100/60 mmHg blood pressure. No macroscopic hematuria was observed in bladder catheterization with a 14F Foley catheter. Hemoglobin was 12.3 g/dL, hematocrit was 36.7%, platelet was 172.000 x 10^3/uL and coagulation parameters were normal. Hematoma area was evacuated and irrigated with physiological saline solution, then hemostasis was achieved with bleeding vessel ligation and by repairing the vaginal laceration area covering the hymen. The operation was completed after the insertion of a hemovac drain into the hematoma region.
In her post-operative follow-up, the drain was removed on the postoperative first day. Intravenous antibiotic cefazolin sodium 1g IV and anti-inflammatory treatment diclofenac sodium 75mg IM were administered twice a day, cold compression and dressing with Eau de Goulard solution were applied to the perineum thrice a day and the patient was discharged in a healthy condition on the postoperative fifth day. In the follow-up of the patient, hemoglobin levels and vital signs were normal; therefore, no blood transfusion was performed.
Figure 1.

Pre-operative edematous vulva, and vulvar hematoma covering the right labium minus and majus and the urethra
Figure 2.
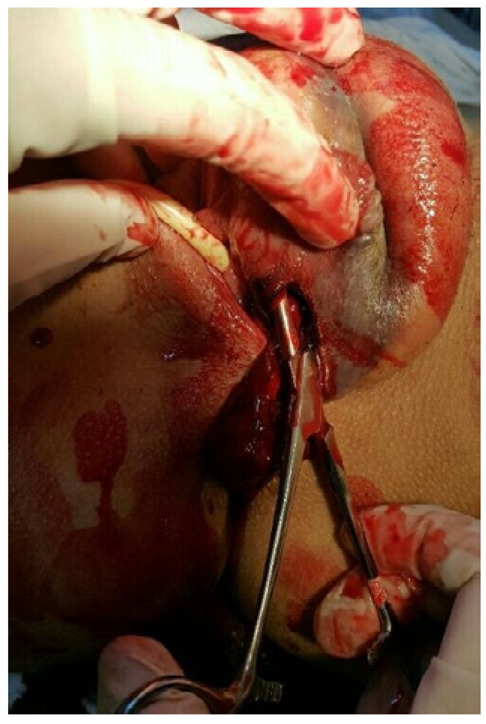
Evacuation of the vulvar hematoma with the incision to the interior of left labium majus
Discussion
The vulva mostly consists of loose connective tissue and smooth muscle, and it has a rich vascular structure. The external genital area is fed by a vascular structure rich in internal and external pudendal arteries (9). The venous drainage is provided by labial veins, and labial veins drain into the external and internal pudendal veins (9). Damages that the injury to labial branches of the internal pudendal artery in this vascular network easily hematoma developments. Vulvar hematoma can develop due to delivery or trauma. These may be located in one of two anatomic areas, often referred to as the anterior and posterior triangles. The frequency of sexual injuries in general gynecology practice has been reported in various publications ranging from 0.05% to 0.7% (5,10,11). However, the actual frequency is estimated to be much higher than reported (10).
Figure 3.

Post-operative 12th hour
Most of the female reproductive system injuries are caused by obstetric traumas, while sexual trauma is the most common non-obstetric cause. (12). Virginity, hard sexual intercourse, sexual assault and harassment, penovaginal disproportion, premenarchal and postmenopausal period, puerperium, inadequate emotional and physical preparation of women for sexual intercourse, previous vulvovaginal surgery, foreign body use with pelvic radiotherapy are predisposing etiologic factors for vulva laceration and hematoma (13,14).
There are no specific guidelines of surgical intervention, surgical management, the surgical outcome in vulvar hematoma. In the treatment of vulvar hematomas; conservative treatment (ice bags, pressure clothing, and analgesia is sufficient, etc), surgery, and arterial embolization. Although some authors suggested that obstetric vulvar hematomas could be managed conservatively (ice bags, pressure clothing, and analgesia is sufficient, etc) (15,16), surgical drainage reduces prolonged morbidity and hospital stay (3,17). Conservative treatment is possible in small and chronic vulvar hematomas but is not possible in acute and large vulvar hematomas. Surgical drainage and primary repair can be performed in acute large hematomas (1,3,5,7,18). If possible, the incision should be opened through the vagina and bleeding foci should be repaired with eight-shape absorbable sutures. It may be necessary to insert a drain into the hematoma cavity for at least 24 hours, insert a tampon into the vagina, and insert a foley catheter.
Recently, selective arterial embolization has been preferred as an alternative to surgery in puerperal and non-puerperal hematomas (2,19-22). In the selective artery embolization technique, these vessels are initially examined by transfemoral arteriography. Embolization is then performed using gel foam (gelatin) pledgets. Although it appears less risky than surgery, deaths due to sepsis and multiple organ failure have been reported (22). Selective arterial embolization is not yet common, as it requires equipment and staff.
In our case, there was a large vulvar hematoma obstructing the external urethra. Therefore, as conservative treatment would not be sufficient, surgical approach was preferred. Hemostasis was achieved by ligation of the bleeding arteries during exploration after evacuation. Our patient had short post-operative hospitalization and a good treatment response.
Conclusion
In conclusion, vulvar hematoma is the most common non-obstetric cause of perineal trauma and carries the risk of mortality by causing hypovolemic shock. Sexual trauma, in particular, increases the risk of non-obstetric vulvar hematoma. The conservative approach is preferred for small and non-growing hematomas; however, surgical hematoma drainage is used for large and enlarging hematomas. Selective arterial embolization procedure is not common as the required equipment is not available in all healthcare facilities.
Conflict of Interest:
Each author declares that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
Informed Consent:
Informed consent was obtained from all individual participants included in the study.
Contributors’ statements:
Dr. Gölbaşı, C. designed the study, drafted the initial manuscript and approved the final manuscript as submitted. Dr. Gölbaşı, H. carried out the initial analyses, critically reviewed the manuscript and approved the final manuscript as submitted. Dr. Bayraktar designed the data collection instruments, and coordinated data collection at hospital information system, made statistical analysis, critically reviewed the manuscript, and approved the final manuscript as submitted. Dr. Ertaş conducted the literature search and data extraction and contributed sections of the text, critically reviewed the manuscript and approved the final manuscript as submitted.
References
- 1.Virgili A, Bianchi A, Mollica G, Corazza M. Serious hematoma of the vulva from a bicycle accident. A case report. J Reprod Med. August 2000;45(8):662–4. [PubMed] [Google Scholar]
- 2.Kunishima K, Takao H, Kato N, Inoh S, Ohtomo K. Transarterial embolization of a nonpuerperal traumatic vulvar hematoma. Radiat Med. 30 April 2008;26(3):168. doi: 10.1007/s11604-007-0208-5. [DOI] [PubMed] [Google Scholar]
- 3.Kanai M, Osada R, Maruyama K, Masuzawa H, Shih H-C, Konishi I. Warning from Nagano: Increase of Vulvar Hematoma and/or Lacerated Injury Caused by Snowboarding. J Trauma Acute Care Surg. February 2001;50(2):328–31. doi: 10.1097/00005373-200102000-00021. [DOI] [PubMed] [Google Scholar]
- 4.Habek D, Kulaš T. Nonobstetrics vulvovaginal injuries: mechanism and outcome. Arch Gynecol Obstet. 01 February 2007;275(2):93–7. doi: 10.1007/s00404-006-0228-x. [DOI] [PubMed] [Google Scholar]
- 5.Sau AK, Dhar KK, Dhall GI. Nonobstetrie Lower Genital Tract Trauma. Aust N Z J Obstet Gynaecol. 1993;33(4):433–5. doi: 10.1111/j.1479-828x.1993.tb02132.x. [DOI] [PubMed] [Google Scholar]
- 6.Bechtel K, Santucci K, Walsh S. Hematoma of the Labia Majora in an Adolescent Girl. Pediatr Emerg Care. June 2007;23(6):407–8. doi: 10.1097/01.pec.0000278399.47999.0b. [DOI] [PubMed] [Google Scholar]
- 7.Dash S, Verghese J, Nizami DJ, Awasthi RT, Jaishi S, Sunil M. Severe haematoma of the vulva--a report of two cases and a clinical review. Kathmandu Univ Med J KUMJ. June 2006;4(2):228–31. [PubMed] [Google Scholar]
- 8.Egan E, Dundee P, Lawrentschuk N. Vulvar hematoma secondary to spontaneous rupture of the internal iliac artery: clinical review. Am J Obstet Gynecol. 01 January 2009;200(1):e17–8. doi: 10.1016/j.ajog.2008.09.024. [DOI] [PubMed] [Google Scholar]
- 9.Anderson JR, Genadry R. Anatomy and Embryology. In: Berek JS, editor. Berek & Novak’s Gynecology. 13th ed. Philadelphia,PA: Lippincott Williams & Wilkins; 2002. pp. 69–121. [Google Scholar]
- 10.Danso KA, Turpin CA. Vulvo-vaginal injuries: analysis of 170 cases at Komfo Anokye Teaching Hopital, Kumasi, Ghana. Ghana Med J. 2004;38(3):116–9. [Google Scholar]
- 11.Rush R, Milton PJ. Injuries of the vagina. South Afr Med J Suid-Afr Tydskr Vir Geneeskd. 28 July 1973;47(29):1325–6. [PubMed] [Google Scholar]
- 12.Fallat ME, Weaver JM, Hertweck SP, Miller FB. Late follow-up and functional outcome after traumatic reproductive tract injuries in women. Am Surg. September 1998;64(9):858–61. [PubMed] [Google Scholar]
- 13.Jeng C-J, Wang L-R. Vaginal Laceration and Hemorrhagic Shock during Consensual Sexual Intercourse. J Sex Marital Ther. 15 May 2007;33(3):249–53. doi: 10.1080/00926230701267910. [DOI] [PubMed] [Google Scholar]
- 14.Sloin MM, Karimian M, Ilbeigi P. Nonobstetric Lacerations of the Vagina. J Am Osteopath Assoc. 01 May 2006;106(5):271–3. [PubMed] [Google Scholar]
- 15.Propst A, Thorp J. Traumatic Vulvar Hematomas: Conservative Versus Surgical Management. South Med J. February 1998;91(2):144–6. doi: 10.1097/00007611-199802000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Vermesh M, Deppe G, Zbella E. Non-puerperal traumatic vulvar hematoma. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet. June 1984;22(3):217–9. doi: 10.1016/0020-7292(84)90009-2. [DOI] [PubMed] [Google Scholar]
- 17.Benrubi G, Neuman C, Nuss R, Thompson R. Vulvar and Vaginal Hematomas: A Retrospective Study of Conservative Versus Operative Management. South Med J. August 1987;80(8):991–4. doi: 10.1097/00007611-198708000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Hong HR, Hwang KR, Kim SA, Kwon JE, Jeon HW, Choi JE. A case of vulvar hematoma with rupture of pseudoaneurysm of pudendal artery. Obstet Gynecol Sci. 15 March 2014;57(2):168–71. doi: 10.5468/ogs.2014.57.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heffner LJ, Mennuti MT, Rudoff JC, McLean GK. Primary management of postpartum vulvovaginal hematomas by angiographic embolization. Am J Perinatol. July 1985;2(3):204–7. doi: 10.1055/s-2007-999949. [DOI] [PubMed] [Google Scholar]
- 20.Villella J, Garry D, Levine G, Glanz S, Figueroa R, Maulik D. Postpartum angiographic embolization for vulvovaginal hematoma. A report of two cases. J Reprod Med. January 2001;46(1):65–7. [PubMed] [Google Scholar]
- 21.Chen T-H, Chen C-H, Hong Y-C, Chen M. Puerperal Pelvic Hematoma Successfully Treated by Primary Transcatheter Arterial Embolization. Taiwan J Obstet Gynecol. 01 June 2009;48(2):200–2. doi: 10.1016/S1028-4559(09)60289-8. [DOI] [PubMed] [Google Scholar]
- 22.Lédée N, Ville Y, Musset D, Mercier F, Frydman R, Fernandez H. Management in intractable obstetric haemorrhage: an audit study on 61 cases. Eur J Obstet Gynecol Reprod Biol. 01 February 2001;94(2):189–96. doi: 10.1016/s0301-2115(00)00349-3. [DOI] [PubMed] [Google Scholar]


