Abstract
Introduction:
Onychomatricoma is a rare subungual tumor composed of stroma and nail matrix-like epithelium. Only seven cases of the pigmented variant have been reported in the literature.
Case report:
We present a 62-year-old male patient with a 2-years history of a single fingernail thickening, deformation, and hyperpigmentation. He had been treated for onychomycosis, without improvement. Due to the increasing hyperpigmentation, and to rule out tumoral entities, including melanoma, a color Doppler ultrasound examination of the nail was requested, which showed a hypoechoic tumor of the nail matrix and bed, with hyperechogenic linear images inside, suggesting the diagnosis of onychomatricoma. Onychectomy and partial matricectomy were performed. Histological evaluation confirmed the diagnosis of onychomatricoma.
Discussion and conclusions:
Histological evaluation is the gold standard for the diagnosis of onychomatricoma. However, ultrasonography represents an easily accessible, non-invasive diagnostic tool for the initial evaluation of these tumors, especially in unsuspected atypical clinical presentations. (www.actabiomedica.it)
Keywords: Onychomatricoma, Pigmented onychomatricoma, nail ultrasound, Onychomatricoma ultrasound, dermatologic ultrasound, ultrasound dermatology
Introduction
Onychomatricoma is a benign tumor of the nail matrix, of rare occurrence and few cases documented in the literature, with a real frequency that has not been well stablished (1). It is more frequent in adult patients, with an average age of 47.9 years and the same ratio between men and women, although recent series report a higher incidence in women. It is more frequently described in white individuals, but it can occur in any race (2).
An association between previous local trauma and onychomatricoma development has been proposed, although it remains controversial. The presence of previous onychomycosis might act as a predisposing factor, but a causal relationship has not been well established (3).
Genomic studies suggest that chromosome 11 could play an important role, with a decrease in the activity of the cathepsin C gene, which is involved in the development of the disease (4). Electron microscopy propose a fibroproliferative origin, suggesting that onychomatricomas may be hamartomas of epithelial and connective tissue that resemble the nail matrix, expressing the same pattern of cytokeratins and integrins of the normal matrix (5).
Clinically, onychomatricomas present as a long-standing, slow-growing painless tumor in the nail. It is more common in fingernails than toenails. The classic clinical tetrad is xanthonychia, diffuse nail thickening or longitudinal crests, splinter hemorrhages, and increase of the transverse curvature of the nail plate, which may occasionally present hyperpigmentation (2).
Clinical diagnosis is difficult, as onychomatricoma may mimic both benign or malignant pathologies like common warts, onychomycosis, fibroids, fibrokeratomas, subungual exostosis, Bowen’s disease, keratoacanthoma, squamous cell carcinoma (6-8).
The gold standard for diagnosis and treatment is excision and histopathological analysis, however, since nail biopsies may leave cosmetic sequelae, the ungual surgery is usually complex and the postoperative period usually poorly tolerated, imaging techniques have been increasingly used (5).
Color Doppler ultrasound presents a high axial resolution for studying the skin and the nail, and it has been reported that this technique can support the diagnosis of benign and malignant tumors of the nail (9).
A case of pigmented onychomatricoma is presented, highlighting the use of Color Doppler ultrasound, which suggested the diagnosis before surgery.
Case report
We present the case of a 62-year-old male patient with a history of non-Hodgkin lymphoma treated six years ago and a melanoma in a first-degree relative. He presented a 2-year history of progressive deformation of the nail plate in the middle finger of the left hand, with thickening, discoloration, and hyperpigmentation. He had previously received empirical treatment with oral terbinafine for two months, without improvement. On physical examination, he presented a hard, thickened, highly hyperpigmented nail plate, with lateral deformation and hyperkeratosis, affecting from the nail matrix to the distal free edge of the nail plate (Fig. 1). Direct microscopic examination and fungal culture were negative for fungal infection. Ultrasonographic analysis (8 to 18 MHz multi-frequency linear compact transducer, General Electric Logic E9 XD Clear, General Electric Health Systems, Waukesha; WI), showed a subungual solid hypoechoic structure (1.5 cm x 0.8 cm x 0.5 cm) with hyperechoic lines that involved the proximal segment of the nail bed, including the ulnar wing of the nail matrix, and protruded into the interplate space. Thickening and upward of the nail plate were also noted. On color Doppler, there were low-velocity arterial and venous vessels within the tumor. Thus, the ultrasonographic diagnosis was compatible with onychomatricoma (Fig. 2). Onychectomy and partial matricectomy were performed, and histology confirmed the diagnosis of onychomatricoma. The patient evolved favorably without tumor recurrence in subsequent controls.
Figure 1.

Onychomatricoma. Clinical image. Lateral, hyperkeratotic nail thickening, with increased transverse curvature. Highlights an intense pigmentation of the nail plaque.
Figure 2.
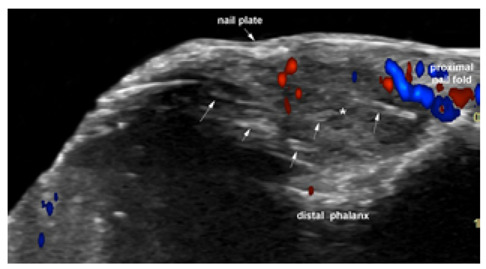
Onychomatricoma. Color Doppler ultrasound (longitudinal axis). Hypoechoic subungual structure (*) with hyperechogenic lines (vertical arrows pointing upward) that involves the proximal segment of the nail bed, including the matrix and its ulnar wing, and protrudes into the interplate space. There are thickening and upward displacement of the nail plate, and a low degree of vascularity within the structure. Slight scalloping of the bony margin of the distal phalanx is also noted.
Discussion
Onychomatricoma is the only tumor originated in the nail matrix that actively produces nail plate (4). It was first described in 1992, and, to date, nearly 200 cases have been published worldwide (10). It is a very rare condition, but it is likely underdiagnosed due to the lack of knowledge or insufficient histopathological studies (1,2). Thus, there must be a high clinical suspicion, since frequently patients have received multiple previous treatments, usually including antifungal drugs, without improvement (11).
The pigmented variant of onychomatricoma is extremely rare, and only 7 cases have been published in the available literature, none of them with ultrasound evaluation (10). This clinical presentation represents an additional diagnostic challenge, which may mimic melanoma or pigmented Bowen’s disease (12,13).
In recent years, the usefulness of complementary techniques to increase the diagnostic accuracy in onychomatricoma has been reported, including dermoscopy, confocal microscopy, ultrasonography, optical coherence tomography, and magnetic resonance imaging (14).
Between the years 2009 and 2010, Soto et al (15) and Wortsman et al (9), described for the first time the ultrasonographic patterns of onychomatricoma, showing a hypoechoic tumoral lesion affecting the matrix zone with hyperechoic linear spots and projections into the interplate nail space; secondary compression with upward displacement of the nail plates and enlargement of the interplate space were also observed. Color Doppler ultrasonographic analysis shows a hypovascular pattern within the lesions. The bone margin of the distal phalanx was unremarkable in all cases according to the authors. Subsequently, only two more cases of non-pigmented onychomatricomas with ultrasonographic evaluation have been reported, whitout published cases of pigmented onychomatricomas in the literature (11,16).
The definitive diagnosis is by histopathologic examination, which reveals a fibroepithelial or biphasic tumor that mimics the normal nail matrix, presenting two anatomical areas: a proximal area that is the base of the tumor (from the root of the nail to below the cuticle), and a distal area composed of multiple fingerlike processes with a fibrous axis covered by matrix epithelium that extend into small cavities filled with serous fluid in the nail plate (5). The diagnosis can be completed with the immunohistochemical study, which is positive for CD34 (17) and AE13 (5).
In 2004, a subclassification for onychomatricoma was proposed based on histological differences in relation to the amount of epithelium, stroma, cellularity and nuclear pleomorphism. Three types of onychomatricoma were defined: unguioblastoma (predominantly epithelial), unguioblast fibroma (predominantly cellular stroma), and atypical unguioblast fibroma (increased mitotic activity and nuclear pleomorphism in the stroma) (18). This classification is conceptual and has no implications in the initial approach, but it can be important in definitive management and follow-up for cases with atypia.
Regarding management, complete surgical excision is recommended, including nail avulsion and removal of the normal nail matrix proximal to the lesion. The presence of finger-like projections to avulsion is highly suggestive of the diagnosis. Mohs micrographic surgery allows removal of the tumor with minimal removal of unaffected matrix, and preserves the potential regeneration of the remaining nail matrix (19).
The clinical course is usually benign, although there are few long-term follow-up studies. Surgical removal generally does not present recurrence in a 2-year follow-up (16,19).
The histopathological evaluation continues to be the gold standard for the diagnosis of onychomatricoma; however, in our case, a highly pigmented variant of onychomatricoma, with a challenging differential diagnosis, the ultrasonographic evaluation suggested the diagnosis conclusively, and helped to decide the optimal management and plan the surgical approach.
Conclusions
The reported case might be clinically relevant, as it highlights the role of ultrasonography in the diagnosis of onychomatricoma, even more so in unsuspected atypical clinical presentations such as the presented pigmented variant of onychomatricoma.
Funding sources:
None
Conflict of Interest:
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- 1.Morales-Cardona CA, Luque-Acevedo ÁA, Bermúdez-Bula LF. Onychomatricoma: an often misdiagnosed tumor of the nails. Cutis. 2015;96(2):121–124. [PubMed] [Google Scholar]
- 2.Di Chiacchio N, Tavares GT, Tosti A, et al. Onychomatricoma: epidemiological and clinical findings in a large series of 30 cases. Br J Dermatol. 2015;173(5):1305–1307. doi: 10.1111/bjd.13900. [DOI] [PubMed] [Google Scholar]
- 3.Mandrell J. Onychomatricoma: a rare case of unguioblastic fibroma of the fingernail associated with trauma. Cutis. 2016;97(4):E15–18. [PubMed] [Google Scholar]
- 4.Cañueto J, Santos-Briz Á, García JL, Robledo C, Unamuno P. Onychomatricoma: genome-wide analyses of a rare nail matrix tumor. J Am Acad Dermatol. 2011;64(3):573–578. doi: 10.1016/j.jaad.2009.07.051. [DOI] [PubMed] [Google Scholar]
- 5.Perrin C, Baran R, Pisani A, Ortonne J-P, Michiels J-F. The onychomatricoma: additional histologic criteria and immunohistochemical study. Am J Dermatopathol. 2002;24(3):199–203. doi: 10.1097/00000372-200206000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Sidhu HK, Patel RV, Goldenberg G. Dermatology clinics: what’s new in dermatopathology: news in nonmelanocytic neoplasia. Dermatol Clin. 2012;30(4):623–641. doi: 10.1016/j.det.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 7.Rushing CJ, Ivankiv R, Bullock NM, Rogers DE, Spinner SM. Onychomatricoma: A Rare and Potentially Underreported Tumor of the Nail Matrix. The Journal of Foot and Ankle Surgery. 2017;56(5):1095–1098. doi: 10.1053/j.jfas.2017.04.008. [DOI] [PubMed] [Google Scholar]
- 8.Richert B, Lecerf P, Caucanas M, André J. Nail tumors. Clin Dermatol. 2013;31(5):602–617. doi: 10.1016/j.clindermatol.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 9.Wortsman X, Wortsman J, Soto R, et al. Benign tumors and pseudotumors of the nail: a novel application of sonography. J Ultrasound Med. 2010;29(5):803–816. doi: 10.7863/jum.2010.29.5.803. [DOI] [PubMed] [Google Scholar]
- 10.Isales MC, Haugh AM, Bubley J, et al. Pigmented onychomatricoma: a rare mimic of subungual melanoma. Clin Exp Dermatol. 2018;43(5):623–626. doi: 10.1111/ced.13418. [DOI] [PubMed] [Google Scholar]
- 11.Joo HJ, Kim MR, Cho BK, Yoo G, Park HJ. Onychomatricoma: A Rare Tumor of Nail Matrix. Ann Dermatol. 2016;28(2):237–241. doi: 10.5021/ad.2016.28.2.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nguyen CV, Moshiri AS, Council ML, Rosman IS, Rubin AI. Pigmented onychomatricoma mimicking nail unit melanoma. J Cutan Pathol. 2019;46(12):895–897. doi: 10.1111/cup.13529. [DOI] [PubMed] [Google Scholar]
- 13.Lobl MB, Santos C, Clarey D, et al. Treatments and associated outcomes of acral lentiginous melanoma: A review. J Am Acad Dermatol. doi: 10.1016/j.jaad.2019.11.021. Published online November 15, 2019. [DOI] [PubMed] [Google Scholar]
- 14.Cinotti E, Veronesi G, Labeille B, et al. Imaging technique for the diagnosis of onychomatricoma. J Eur Acad Dermatol Venereol. 2018;32(11):1874–1878. doi: 10.1111/jdv.15108. [DOI] [PubMed] [Google Scholar]
- 15.Soto R, Wortsman X, Corredoira Y. Onychomatricoma: clinical and sonographic findings. Arch Dermatol. 2009;145(12):1461–1462. doi: 10.1001/archdermatol.2009.312. [DOI] [PubMed] [Google Scholar]
- 16.Di Chiacchio N, Tavares GT, Padoveze EH, Bet DL, Di Chiacchio NG. Onicomatricoma. Surg cosmet dermatol (Impr) Published online 2013:10-14. [Google Scholar]
- 17.Poojary SA, Halwai V. A tumor hidden beneath the nail plate: report of a rare case of onychomatricoma with three-dimensional histopathological analysis and immunohistochemical study. Indian J Dermatol. 2015;60(2):212. doi: 10.4103/0019-5154.152569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ko CJ, Shi L, Barr RJ, Mölne L, Ternesten-Bratel A, Headington JT. Unguioblastoma and unguioblastic fibroma-an expanded spectrum of onychomatricoma. J Cutan Pathol. 2004;31(4):307–311. doi: 10.1111/j.0303-6987.2004.0151.x. [DOI] [PubMed] [Google Scholar]
- 19.Graves MS, Anderson JK, LeBlanc KG, Sheehan DJ. Utilization of Mohs micrographic surgery in a patient with onychomatricoma. Dermatol Surg. 2015;41(6):753–755. doi: 10.1097/DSS.0000000000000372. [DOI] [PubMed] [Google Scholar]


