Abstract
Objective
Building on the original taxonomy of hospital‐based health systems from 20 years ago, we develop a new taxonomy to inform emerging public policy and practice developments.
Data Sources
The 2016 American Hospital Association's (AHA) Annual Survey; the 2016 IQVIA Healthcare Organizations and Systems (HCOS) database; and the 2017‐2018 National Survey of Healthcare Organizations and Systems (NSHOS).
Study Design
Cluster analysis of the 2016 AHA Annual Survey data to derive measures of differentiation, centralization, and integration to create categories or types of hospital‐based health systems.
Data Collection
Principal components factor analysis with varimax rotation generating the factors used in the cluster algorithms.
Principal Findings
Among the four cluster types, 54% (N = 202) of systems are decentralized (−0.35) and relatively less differentiated (−0.37); 23% of systems (N = 85) are highly differentiated (1.28) but relatively decentralized (−0.29); 15% (N = 57) are highly centralized (2.04) and highly differentiated (0.65); and approximately 9 percent (N = 33) are least differentiated (−1.35) and most decentralized (−0.64). Despite differences in calculation, the Highly Centralized, Highly Differentiated System Cluster and the Undifferentiated, Decentralized System Cluster were similar to those identified 20 years ago. The other two system clusters contained similarities as well as differences from those 20 years ago. Overall, 82 percent of the systems remain relatively decentralized suggesting they operate largely as holding companies allowing autonomy to individual hospitals operating within the system.
Conclusions
The new taxonomy of hospital‐based health systems bears similarities as well as differences from 20 years ago. Important applications of the taxonomy for addressing current challenges facing the healthcare system, such as the transition to value‐based payment models, continued consolidation, and the growing importance of the social determinants of health, are highlighted.
Keywords: centralization, cluster analysis, differentiation, healthcare systems, integration
What is Already Known
A hospital‐based health system taxonomy developed approximately 20 years ago found five cluster types of systems based on varying degrees of differentiation, centralization, and integration.
The taxonomy was used to examine cost, quality of care, and related performance measures in subsequent years.
What This Study Adds
Using recent data and modified measures, the new taxonomy identifies four cluster types of hospital‐based health systems – two similar to the previous taxonomy and two somewhat different.
The new taxonomy is partially validated with independent measures from the National Survey of Health Systems and Organizations (NSHOS) fielded by the Dartmouth Institute.
Most systems are relatively decentralized operating largely as holding companies for individual hospitals.
The new taxonomy can be used to address a number of continuing and emerging health care delivery, payment, and policy issues.
1. INTRODUCTION
The health care sector is undergoing an unprecedented period of change. This is reflected in the horizontal and vertical consolidation of hospitals, health systems, and physician organizations, an increase in physicians joining medical groups, an overall growth in the size and complexity of health care organizations, 1 the emergence of value‐based payments, increased use of new technologies such as telehealth, growing recognition of the importance of the social determinants of care and the challenges posed by the Covid‐19 pandemic and its’ consequences.
These developments have raised a host of issues ranging from whether consolidated hospital and health systems provide any advantages in access or quality of care to offset the evidence that they raise prices 2 , 3 to the ability of various types of healthcare organizations to eliminate waste and respond to the value‐based payment arrangements. 4 , 5 In what ways are hospitals and the systems to which they belong responding to these developments in terms of the number and types of services they offer; the extent to which they are centralized or decentralized in their service offerings and various arrangements with physicians and health plans; and the extent to which they integrate the services and arrangements through ownership and direct provision or contract them out to other organizations? In this paper, we develop a new taxonomy based on updated data that addresses these questions. The taxonomy builds on the foundational taxonomy of hospital‐based health systems developed by Bazzoli et al 6 20 years ago. We suggest that the new taxonomy can be used by the research community, policymakers, and practitioners to help track hospitals and health system operating in the current environment of rapid change.
Using the American Hospital Association's (AHA) Annual Survey data, the original taxonomy was grounded in industrial organization economics and organization theory drawing on the key concepts of differentiation, centralization, and structural integration. These three concepts remain relevant today. Differentiation refers to the number of different types of services or products that an organization provides. As competition among hospitals and health systems has increased along with pressure to avoid penalties for readmissions and advances in technology, hospitals are changing their service mix. This is reflected in the growth of outpatient care, community‐based services addressing the social determinants of health and high technology services, and new arrangements with physicians and health plans.
Centralization refers to where in an organization decisions are made and a given service is provided. As healthcare systems have become more complex with many having owner subsidiaries, the issue of centralization grows in importance. Structural integration refers to the mechanisms used to coordinate services. As hospitals and health systems have changed their service mix and become more differentiated, parallel demands are placed on the need for integration. This becomes particularly salient for hospital and health systems participating in Accountable Care Organizations (ACOs) and related risk‐based payment arrangements where providers are financially at risk and accountable for the entire continuum of care delivered to patients.
The original taxonomy resulted in five systems clusters labeled as Centralized Health Systems, Moderately Centralized Health Systems, Centralized Physician/Insurance Health Systems, Decentralized Health Systems, and Independent Health Systems and four network clusters with similar designations. 6 The taxonomy was updated and further validated in 2004. 7
The taxonomy provided a foundation for examining the evolution of health systems over time and for subsequent research on the relationship of the system/network types to performance on a variety of cost, quality, and related measures. For example, hospitals in systems that were more tightly integrated had better financial performance than those less integrated. Further, hospitals belonging to more centralized networks had better financial performance than those belonging to more decentralized networks. 8 Those hospitals in systems that were less differentiated experienced the poorest financial performance. 8 Centralized physician/insurance health systems have been shown to be more likely to adopt patient safety practices such as computerized physician order entry while independent hospital systems had a negative adoption rate. 9 Hospitals in centralized health systems were found to be associated with lower acute myocardial infarction (AMI), congestive heart failure (CHF), and preventive mortality. 10 As expected, hospitals belonging to systems exchanged more patient data with other hospitals in the same system than with hospitals outside the system, but there were no differences by type of system 11 Burns et al and Walker et al summarize much of the recent research on systems noting an upward trend in centralized “hub and spoke” and regional health systems driven mostly by system size and geography. 12 , 13 At the same time, there has been growing concern over the impact of increased consolidation of hospitals and systems on increasing hospital prices due to decreasing competition in local markets. 2 , 3 , 14 , 15
2. METHODS
2.1. Overall Approach
Our overall approach was to use the 2016 American Hospital Association (AHA) annual survey data of general medical/surgical hospitals excluding all specialty hospitals including children's hospitals and all Veteran Administration hospitals. The survey provides data on services offered, physician arrangements, and health plan arrangements. We used two different listings of hospital ownership. The first was the IQVIA Health Care Organizations and Systems (HCOS) database. The second was the AHA data base list. This was followed by drawing on selected variables from an independent National Survey of Healthcare Organizations and Systems (NSHOS) to provide preliminary validation of the resulting taxonomy. In the following sections, we introduce the data sets; define the key variables; describe our handling of data challenges such as non‐response and outliers; and note where our measurement and analytic approach differs from the original work.
2.2. Data
Consistent with the AHA and prior work, we defined a system as owning two or more hospitals. Alternative definitions also exist such as including only one hospital as long as it has an ownership relationship with a medical group providing comprehensivecare. 1
The 2016 IQVIA Health Care Organizations and Systems (HCOS) database was first used to attribute hospitals to systems in our primary analysis because it contains detailed information on financial relationships between healthcare organizations and the physicians they employ and was the basis of the National Survey of Health Care Organizations and Systems (NSHOS). The 2016 AHA database was used to attribute hospitals as a sensitivity analysis that provided an alternative attribution of hospitals to systems consistent with the previous taxonomy but not necessarily identifying the same systems indicated by HCOS. For both the HCOS and AHA attribution of hospitals to systems, the 2016 AHA survey data on services offered, physician arrangements and health plan arrangements were used. The NSHOS hospital survey provided additional data that we used for validation on characteristics such as degree of physician influence, use of electronic health records, and organizational culture.
Reflecting the increasing complexity of the health sector in 2016, we found that many hospitals in the AHA database reported being part of both a network (contractual relationship) and a system (asset ownership). We visually inspected the AHA provider system and network names and found in many instances the network names indicated affiliation with the overall system, likely as owner subsidiaries. We also compared system and network names against the names contained in the HCOS database and found that most listed as part of a network were also listed as a member of a system. Only 349 hospitals (8.2%) reported that they were part of a network only. As such, we diverged from the original taxonomy by excluding these network‐only hospitals from analyses.
2.3. Construction of key variables
2.3.1. Services and physician, insurance organizational arrangements
The list of services used to define differentiation, centralization, and integration were nearly identical to those in the 1995 survey upon which the 1999 taxonomy was based although some new high‐tech services, such as proton therapy, were added. In addition, in 1995 a question that asked about the hospital's involvement in community activities such as conducting a community health needs assessment was not asked in 2016. Instead, we used the 11 services from the overall list that represented community‐oriented outreach services such as adult day health centers, retirement housing, and meals on wheels.
The services were grouped into 16 general categories as in the original taxonomy 6 (see Table 1 in the Appendix S2 for details about each service category). The pediatric service category also included birthing services. Within each category, we calculated the percentage of affirmative responses with the denominator being the number of non‐missing values. When less than 50% of questions in a service category were answered, we set the value to missing.
There are eight formal physician organizational arrangements with hospitals provided in the AHA survey. These included having a voluntary medical staff appointment, a group practice “without walls,” a management service organization, an independent practice association, an open physician‐hospital organization, a closed physician‐hospital organization, a foundation model, an equity model, and an integrated salary model. Insurance arrangements included whether or not a hospital had an ownership relationship with an HMO or PPO plan.
2.3.2. Differentiation, centralization, and integration
To measure differentiation, we calculated the number of services each hospital offered and whether or not they owned or had a joint venture with a health plan. Then we averaged across all hospitals in a given system to yield our measure of system differentiation. This is different from the original taxonomy that counted a service as being provided if any hospital in the system provided the service. We did not want to privilege larger systems for which because of their size would be more likely to have at least one hospital offering the service.
Centralization was measured by the proportion of the hospitals reporting that the service was provided by the system even if it was also provided by the responding hospital. We then averaged across the hospitals in the system. The original taxonomy only counted the service as centralized if it was only provided by the system and not the hospital. The new measure provides a more granular measure of centralization by allowing for some services within a service category to be provided by others within the system as well. Services integration was measured by the average number of services that the hospital contracted out with such contracting representing less integration than if the hospital itself directly provided the service. Hospital‐physician integration was measured differently from the original taxonomy by making full use of the information available on the relative degree of integration of the various models ranging from 1 (loose‐ voluntary medical staff) to 8 (high‐ integrated salary model). The original taxonomy used a simple count of the number of loose versus tight arrangements. Given that the majority of hospitals had only one arrangement, the ordinal measure of degree of integration of that model provides a more granular and accurate measure. Where two or more arrangements were checked, we averaged the integration scores. Health plan integration was measured by the average across the hospitals in the system of the indicator variables of whether each hospital owned a health plan versus contracted out.
2.4. Taxonomy development
The 16 service measures plus the hospital‐physician arrangement measure and the hospital‐health plan arrangement measure were computed corresponding to the definitions of differentiation, centralization, and integration respectively yielding three groups of 18 measures. In the original taxonomy, the service measures were examined and factored analyzed separately from the physician arrangements and health plan measures. Given the close relationship between the services a hospital offers and the physicians who are either employed or admit patients to the hospital and similar close relationship between the services a hospital offers and those being covered by a hospital's health plan, we included them as an entire set in the subsequent analysis.
We then examined the correlation matrix of the 18 measures for the three concepts of differentiation, centralization, and integration across the systems and applied principal components factor analysis to each of the correlation matrices. We used varimax rotation to facilitate the identification of which service or physician or health plan arrangement loaded on which factor. Our criteria for determining the number of factors was that at least 50% of the total variance had to be explained. We standardized the resulting factors to have a mean of zero and a variance of one.
We accounted for outliers resulting from the factor analysis of the integration items by winsorizing the values in the extreme tails of the distribution. The values more extreme than the 2.5th and 97.5th percentiles were substituted with the quantiles corresponding to these percentiles.
This resulted in the factor variables having distributions that were more evenly spread and, thus, more informative in the clustering analysis.
2.5. Taxonomy clustering
To partition the systems into groups, we used unsupervised hierarchical clusters analysis based on the factors obtained from the three factor analyses. We identified the optimal number of clusters via visual inspection of the dendrogram (see Figure 1) obtained from the cluster analysis. One‐way Analysis of Variance (ANOVA) was used to check the equality of means in the different cluster groups. P‐values below .05 were considered significant, although such inferences are reported solely as a description of the data as opposed to being confirmatory. A discriminant analysis was employed for internal validation. We used the 18 components of the measures of differentiation, centralization, and integration to develop classification rules for assigning the systems to one of the four clusters that emerged. We provide the percentage of correct classified systems as a measure of overall internal consistency. All statistical analyses were performed with R (www.r‐project.org).
FIGURE 1.
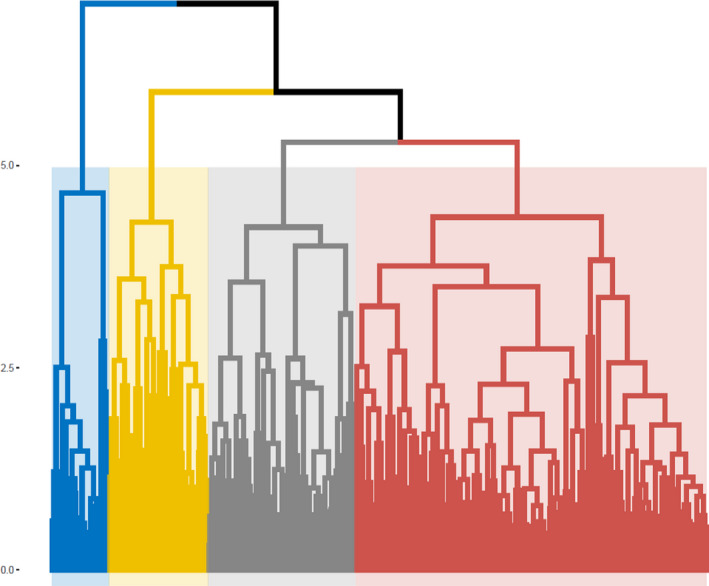
Dendrogram resulting in the unsupervised cluster analysis. *Y‐axis is the relative differential distances on which the clusters are built. Colored areas reflect the four‐cluster solution. X‐axis has no scale or meaning—there's one observation for each system
To evaluate the reproducibility of the cluster solution, we randomly split the systems into two groups and then repeated both the dimension reduction and clustering steps for each group, constraining the solutions to four‐factor solutions. The resulting clusters were compared in terms of their agglomerative coefficient, a measure of the tightness of the cluster solution with smaller values implying tighter clusters in the sense that variation in Mahalanobis distance between systems in the same cluster exceeds that between clusters. Similar values of the agglomerative coefficient between the halves imply that the structure of cluster solutions is similar providing evidence that the results are robust in that random permutations of the sample did not change the results appreciably.
2.6. Validation and robustness of the taxonomy
To validate the new taxonomy and provide a test of sensitivity, as earlier noted, we developed an independent taxonomy based on AHA attribution (instead of HCOS) of hospitals to systems. This allowed us to test the robustness of the primary HCOS attribution method. Given that it was not possible to form a complete cross‐listing of systems between HCOS and AHA systems, we evaluated concordance at the hospital level. Specifically, for each pair of hospitals (“dyad”), we evaluated whether they were in the same or different clusters of systems for both the HCOS and AHA. We then compare the agglomerative coefficients for the two sets of clusters and report the Kappa index as a measure of dyadic concordance across the HCOS and AHA‐based clusters.
The system clusters were further validated by drawing on the recent 2017‐2018 National Survey of Healthcare Organizations and Systems (NSHOS) in which hospitals were assigned to systems based on the HCOS data. 11 The survey yielded 739 hospitals within systems, representing a 47% response rate. The survey included an additional measure of centralization asking about the degree of influence that physicians had on decisions within the system on the scale 4 = none (most centralized); 3‐very little; two = some; and one = a lot (most decentralized). We expected that more centralized systems would score more toward reporting that physicians have none or very little influence.
We also examined two additional measures of integration. The first was whether a single electronic record existed for all hospitals in the system or not (one = yes and zero = no) with an additional point given if they were also linked to primary care practices. Therefore, this scale went from zero to two. The second measure of integration was whether the hospital owned or managed physician practices (one = yes and zero = no). We expected the “Less differentiated, low integration” systems would score lower on these measures.
From the NSHOS survey, we were also able to measure the reported culture of the hospital using the competing values framework measuring the extent to which the organization's culture is group‐oriented, developmental or innovation oriented, hierarchical/bureaucratic; or rational/efficiency oriented. 16 , 17 We expected that highly centralized systems would have a more bureaucratic/hierarchical culture while the low differentiated systems composed of smaller hospitals would score lowest on the bureaucratic/hierarchical culture dimension and highest on the group‐oriented culture dimension. We expected that other decentralized system hospitals would report having a culture that is more group oriented.
3. RESULTS
3.1. Taxonomy
We identified 4278 community hospitals in the AHA database that were also in the HCOS database. Of these, 2911 of these hospitals were members of systems using our definition of two or more hospitals under common ownership. The factor analyses reduced the 16 service categories, hospital‐physician arrangements and hospital‐insurance arrangement variables to six factors or dimensions: two for differentiation, one for centralization and three for integration. These were used as the inputs to the clustering analysis.
As shown in the Figure 1 (dendrogram) and Table 1, we partitioned the systems into four clusters of size 202, 85, 57, and 33. The first cluster is best described as being relatively decentralized with a standardized mean of −0.349 for the Centralization factor with 0 being the threshold for above or below the mean. It is also less differentiated particularly about offering fewer pediatric, ICU, and cardiology services. We call this cluster of systems “Decentralized, Less Differentiated.” The second cluster of systems is highly differentiated particularly about pediatric, ICU, and cardiology services (standardized mean of 1.279).
TABLE 1.
Distribution of factors for the systems in each of the four clusters using the HCOS definition
|
Cluster 1 n = 202 |
Cluster 2 n = 85 |
Cluster 3 n = 57 |
Cluster 4 n = 33 |
P‐value | |
|---|---|---|---|---|---|
| # Hospitals, median | 4 | 3 | 5 | 3 | |
| Differentiation | |||||
| Factor 1 | ‒0.367 | 1.279 | ‒0.057 | ‒0.95 | <0.001 |
| Factor 2 | 0.079 | ‒0.103 | 0.654 | ‒1.351 | <0.001 |
| Centralization | |||||
| Factor 1 | ‒0.349 | ‒0.291 | 2.039 | ‒0.637 | <0.001 |
| Integration [Wz] | |||||
| Factor 1 a | ‒0.090 | ‒0.105 | ‒0.053 | ‒0.020 | 0.692 |
| Factor 2 | ‒0.140 | ‒0.232 | 0.037 | ‒0.336 | 0.002 |
| Factor 3 a | ‒0.169 | ‒0.121 | ‒0.040 | ‒0.31 | 0.128 |
Abbreviation: Wz, Winsorized measures.
Non‐significant differences. Numbers represent the mean value of the factors, which are centered on 0 and scaled to have standard deviation of 1, in the clusters indicated by the column headings.
We label this cluster “Highly Differentiated, Decentralized.” The third cluster is extremely highly centralized (standardized mean of 2.039). It is also relatively highly differentiated in women and community‐oriented services and to some extent in high technology, general acute care, and ambulatory care services. We call this cluster “Highly Differentiated, Highly Centralized.” Cluster four is the least differentiated in its’ service offerings and least integrated (all standardized means below 0). We call this cluster “Undifferentiated, Decentralized, Low Integration.” Thus, other than the cluster 3 systems, 82% of the systems (320/377) are relatively decentralized suggesting that, although “hub and spoke” models may be growing, the majority of systems in the United States may still be operating largely as holding companies allowing autonomy to their individual hospitals to set their own strategic direction in the local markets in which they operate.
Using discriminant analysis, we used a simple rule based on a linear combination of the six factor scores for classifying the systems into clusters of four. We found an overall correct classification percentage of 88.1—this value may be compared to the same value obtained for the alternative AHA‐based approach for forming the taxonomy in the Validation section of the Results.
Table 2A–C provide further information on the clusters about their degree of differentiation, centralization, and integration for each of the service provision categories, hospital‐physician arrangements, and hospital‐health plan arrangements. The higher the mean values of the variable the greater the extent to which the corresponding factor is characterized by high values of that variable; when the variable is binary, the resulting means are proportions although we express them as percentages. In Table 2A on differentiation, all of the P‐values are significant (implying the extent to which each variable varies across the clusters is beyond what could reasonably be expected by chance) with cluster 4 systems being most different from the other clusters. Table 2B shows that cluster 3 systems are most centralized on all services while cluster 4 (all means below 12.2) is the least centralized of all. Table 2C summarizing the integration measures shows somewhat fewer differences among the clusters but with cluster 3 hospital systems being somewhat more integrated on most service categories while cluster 4 hospital systems are least integrated on nine of the 16 service categories and on physician arrangements (Table 2C).
TABLE 2.
Means for the (A) differentiation (B) centralization (C) integration measures for the systems in each cluster a
|
Cluster 1 n = 202 |
Cluster 2 n = 85 |
Cluster 3 n = 57 |
Cluster 4 n = 33 |
P‐value | |
|---|---|---|---|---|---|
| (A) | |||||
| General acute services | 81.63 | 88.03 | 87.35 | 64.52 | <.001 |
| Pediatric services b | 42.46 | 74.14 | 48.01 | 21.58 | <.001 |
| Women Services | 69.59 | 77.21 | 77.31 | 44.70 | <.001 |
| Surgery | 77.09 | 83.55 | 85.69 | 51.49 | <.001 |
| Specialty | 42.61 | 60.79 | 56.83 | 18.91 | <.001 |
| Psychiatric | 43.91 | 57.11 | 49.94 | 25.48 | <.001 |
| Geriatric/LTC/home health | 25.27 | 35.79 | 27.81 | 19.61 | <.001 |
| Cardiology | 66.78 | 84.73 | 73.57 | 31.18 | <.001 |
| Diagnostic | 69.27 | 74.01 | 72.67 | 54.42 | <.001 |
| Emergency care | 50.83 | 60.84 | 56.36 | 41.52 | <.001 |
| Community services | 55.94 | 65.19 | 65.81 | 37.11 | <.001 |
| Other | 17.01 | 52.74 | 30.66 | 14.03 | <.001 |
| ICU beds | 24.57 | 36.68 | 36.63 | 7.612 | <.001 |
| Hi‐Tech | 48.07 | 82.84 | 56.37 | 31.52 | <.001 |
| Ambulatory services | 61.11 | 69.18 | 68.28 | 35.94 | <.001 |
| Transplant services | 8.501 | 19.66 | 21.88 | 0.306 | <.001 |
| MD employment arrangement (hierarchical 1‐8) | 4.782 | 5.129 | 5.894 | 4.144 | .009 |
| Insurance (mean # of insurance plans) | 0.181 | 0.208 | 0.109 | 0.184 | .758 |
| (B) | |||||
| General acute services | 16.28 | 17.85 | 87.63 | 9.541 | <.001 |
| Pediatric services b | 15.45 | 17.90 | 65.01 | 7.783 | <.001 |
| Women Services | 18.91 | 20.93 | 85.94 | 12.17 | <.001 |
| Surgery | 17.71 | 18.36 | 88.19 | 10.18 | <.001 |
| Specialty | 13.52 | 14.81 | 66.25 | 6.642 | <.001 |
| Psychiatric | 22.41 | 20.30 | 71.71 | 8.751 | <.001 |
| Geriatric/LTC/home health | 19.14 | 21.83 | 60.19 | 9.74 | <.001 |
| Cardiology | 16.91 | 16.25 | 81.99 | 9.438 | <.001 |
| Diagnostic | 10.29 | 13.38 | 74.24 | 5.281 | <.001 |
| Emergency care | 10.68 | 13.91 | 63.76 | 4.246 | <.001 |
| Community services | 15.20 | 18.57 | 74.84 | 7.325 | <.001 |
| Other | 8.855 | 12.33 | 44.20 | 3.041 | <.001 |
| ICU beds | 10.43 | 10.70 | 50.71 | 4.532 | <.001 |
| Hi‐Tech | 17.18 | 17.85 | 68.15 | 9.115 | <.001 |
| Ambulatory services | 24.02 | 25.81 | 82.93 | 12.02 | <.001 |
| Transplant services | 7.336 | 7.364 | 32.01 | 2.268 | <.001 |
| MD employment arrangement (hierarchical 1‐8) | 2.59 | 2.871 | 5.681 | 1.779 | <.001 |
| Insurance (mean # of insurance plans) | 0.293 | 0.332 | 0.429 | 0.248 | .293 |
| (C) | |||||
| General acute services | 2.805 | 4.093 | 6.637 | 1.63 | .031 |
| Pediatric services b | 5.504 | 3.437 | 12.43 | 0.641 | <.001 |
| Women Services | 3.669 | 5.076 | 8.431 | 1.616 | .004 |
| Surgery | 0.942 | 1.059 | 3.354 | 2.877 | .106 |
| Specialty | 7.932 | 8.555 | 11.38 | 6.87 | .057 |
| Psychiatric | 5.424 | 5.572 | 9.267 | 4.204 | .259 |
| Geriatric/LTC/home health | 4.553 | 8.184 | 10.59 | 2.1 | <.001 |
| Cardiology | 3.116 | 2.632 | 7.481 | 1.176 | .003 |
| Diagnostic | 3.199 | 4.026 | 9.557 | 3.336 | .001 |
| Emergency care | 1.073 | 0.704 | 5.922 | 1.465 | <.001 |
| Community services | 5.439 | 4.292 | 10.46 | 4.875 | .001 |
| Other | 1.067 | 2.076 | 1.831 | 0.14 | .440 |
| ICU beds | 4.933 | 6.011 | 9.581 | 2.228 | .001 |
| Hi‐Tech | 3.007 | 1.576 | 6.525 | 0.228 | .003 |
| Ambulatory services | 3.022 | 3.206 | 8.611 | 1.025 | .001 |
| Transplant services | 5.225 | 5.902 | 6.098 | 1.002 | .538 |
| MD employment arrangement (hierarchical 1‐8) | 0.466 | 0.727 | 1.218 | 0.276 | .005 |
| Insurance (mean # of insurance plans) | 0.045 | 0.092 | 0.087 | 0.005 | .233 |
Service‐dimension values represent the percentages of the service in each dimension provided by each hospital and aggregated by system (range 0‐100), MD arrangement ranges 1‐8, and Insurance plan take the values of 0‐2. Same explanation of values as in Table 2.
Includes birthing services.
TABLE 3.
Distributions of differentiation, centralization and integration factors across the four clusters of systems as using the AHA definition a
|
Cluster 1 n = 42 |
Cluster 2 n = 149 |
Cluster 3 n = 75 |
Cluster 4 n = 58 |
P‐value | |
|---|---|---|---|---|---|
| # Hospitals, median | 5 | 4 | 5 | 3 | |
| Differentiation | |||||
| Factor 1 | 0.885 | ‒0.641 | 0.907 | ‒0.168 | <.001 |
| Factor 2 | ‒1.243 | ‒0.185 | 0.486 | 0.746 | <.001 |
| Centralization | |||||
| Factor 1 | ‒0.545 | ‒0.44 | ‒0.098 | 1.651 | <.001 |
| Integration [Wz] | |||||
| Factor 1 a | ‒0.114 | ‒0.107 | ‒0.074 | ‒0.148 | .571 |
| Factor 2 | ‒0.262 | ‒0.131 | ‒0.334 | 0.102 | <.001 |
| Factor 3 a | 0.032 | ‒0.125 | ‒0.195 | ‒0.295 | .013 |
Abbreviation: Wz, Winsorizated measures.
Non‐significant differences. Numbers represent the mean values of the centered and scaled factors for the systems in the Cluster indicated by the column heading. These are comparable to the numbers in Table 1 with the greater similarity of the values indicating greater similarity of the taxonomy implied by the clusters.
Using largely the AHA survey data, the clusters differ in varying degrees by size, system complexity, ownership, whether or not they contain critical access hospitals, teaching activity, urban versus rural location and region of the country. Regarding size, there is relatively little difference across the clusters in the median number of hospitals in the system with a range of three to five. This median is higher than the two hospitals per system reported in the AHRQ Compendium due to the differences in the definition of a system (eg, the requirement to have at least two hospitals as opposed to the lesser requirement of only needing one hospital). Cluster 1 has the highest average number of hospitals per system with ten. Cluster 4 has the smallest average bed size of 108 versus 368 for cluster 2 and 299 for cluster 3. Examining complexity, 34% of cluster 1 systems have an owner subsidiary vs only 6%‐15% for the other clusters. Fourty eight (48%) of cluster 4 system hospitals are critical access hospitals versus only 13%‐20% for the other clusters. Clusters 2 and 3 have higher percentages of systems with teaching hospitals than one and four; with the latter having virtually none. Cluster 3 has the highest percentage of not‐for‐profit hospitals while clusters 1 and 4 have a relatively higher percentage of for‐profit hospitals and cluster 2 has a relatively higher percentage of government or public hospitals. Cluster 4 system hospitals are primarily located in rural areas and small towns; cluster 1 hospitals are commonly in suburban and large towns; and clusters 2 and 3 are commonly located in more urban areas. The clusters do not differ greatly by region of the country although cluster 4 systems are somewhat preferentially located in the South and cluster 3 in the Midwest. As also documented in the AHRQ Compendium, most systems hospitals are located in a single state, although more than one‐third of systems in cluster 4 have hospitals in multiple states.
The above descriptions are generally consistent with expectations. For example, in cluster 4 (low differentiation system) hospitals are small, rural, and non‐ teaching, with many being composed of critical access hospitals and more likely to be located in more than one state. The more highly differentiated systems, clusters 2 and 3, have greater involvement in teaching activities, have larger size hospitals, and are more likely to be located in urban areas and in a single state. Cluster 1 has the most complex systems as well as a higher percent of hospitals that belong to owner subsidiaries of the main corporate parent. This likely accounts for the high average number 10 of hospitals in the cluster 4 systems. It may also help explain why cluster 1 systems were relatively decentralized in that with more owner subsidiaries more autonomy is given to the subsidiaries on what services to offer and what arrangements to make with physicians and health plans.
As with the original taxonomy, we found that differentiation and centralization were the most informative in categorizing hospital‐based health systems. Similar to the original taxonomy, the "Centralized” cluster 3 systems are also highly differentiated. In addition, the original “Independent Hospital Systems” cluster is similar to the present “Undifferentiated, low integration” cluster 4 systems in being composed primarily of smaller hospitals located in largely rural areas.
Finally, when we performed a split halves analysis we obtain agglomerative coefficients of 0.796 and 0.808 for the clusters obtained from the two halves. These values are smaller than for clusters built for the full sample because it is easier to get closer to a cleaner partition of systems with a smaller sample. The similarity of the agglomerative coefficients suggests that there is consistency to the cluster solutions across the two halves and thus that the taxonomy formed on the full sample is self‐reproducing (ie, can be reproduced on subsets of the data) and so in this sense is robust.
3.2. Validation using a different data set for forming clusters
Using the AHA hospital assignments to systems, we redid the analysis to create new clusters that could be compared to the primary HCOS‐based clusters. Using the same criteria, we also found a 4‐cluster solution as shown in Table 3. Discriminant analysis revealed a correct classification compared to the actual clusters of 88.6% similar to the 88.1% for the primary analysis based on HCOS. Furthermore, the agglomerative coefficient of the cluster solution based on the relationships in the AHA data was 0.842, which is nearly identical to the 0.837 obtained for the primary analysis based on the HCOS‐reported relationship. The coefficient of concordance assessing whether hospital dyads are classified in the same cluster within each taxonomy produced a Kappa coefficient value of 0.50. Given the lack of agreement between the AHA and HCOS on the alignment of hospitals with systems, finding even a modest consistency between the two taxonomies provides some further validation that the taxonomy is a meaningful and useful partitioning of systems.
3.3. Validation using independent national survey data
As shown in Table 4, the most centralized cluster 3 systems do report that physicians have somewhat less influence as predicted than reported by hospitals belonging to other clusters although the differences are not statistically significant. In addition, as predicted, the low differentiated, low integration cluster 4 system hospitals are less likely to have a single integrated electronic health record and to have it linked to physician practices. Contrary to prediction, Table 3 shows that the more centralized cluster 3 system hospitals do not score highest on the bureaucratic/hierarchical culture dimension but, rather, score highest on the innovation‐oriented culture dimension (mean of 25.7 versus next highest of 20.4) reflecting their broad differentiation of services ranging from community‐oriented services to high technology services. However, as predicted, the cluster 4 system hospitals score the lowest on the bureaucratic/hierarchical culture dimension (10.1) and the highest on the group‐oriented culture dimension (59.3).
TABLE 4.
NSHOS system and hospital respondent characteristics by cluster a
|
Cluster 1 n = 117 |
Cluster 2 n = 48 |
Cluster 3 n = 33 |
Cluster 4 n = 15 |
P‐value | |
|---|---|---|---|---|---|
| Degree of MD influence (1 = a lot −4 = none) | 1.6 | 1.51 | 1.63 | 1.55 | .52 |
| Single EHR(0,1) and EHR connects to practices(0,1) | 1.08 | 1.38 | 1.18 | 0.99 | .06 |
| Own or manage PCP practices (%) | 80.1 | 85.6 | 75.9 | 80.0 | .59 |
| Hospital culture (sums to 100) | |||||
| Hospital group oriented | 46.9 | 38.6 | 43.4 | 59.1 | <.01 |
| Innovation oriented | 19.9 | 20.4 | 25.6 | 18.0 | .02 |
| Bureaucratic | 16.2 | 19.0 | 14.2 | 10.1 | .06 |
| Rational | 17.0 | 21.9 | 16.8 | 12.8 | .02 |
Weighted by combined sampling non‐response weights at the hospital level.
3.4. Limitations
A major advantage of the taxonomy is its basis on the 16 services, hospital‐ physician arrangements, and hospital‐insurance arrangement measures obtained by the AHA Annual Survey, which has a high response rate from all the nations’ general acute medical/surgical hospitals. At the same time, it is limited by missing data on various questions requiring imputation or decisions on whether a skipped question should be considered as a “no” response; for example, not offering the service. The taxonomy is also limited to hospital‐based health systems and does not consider systems based on medical groups or physician organizations that do not own hospitals or, as in the case of the AHRQ Compendium definition, have only one hospital involved. It also cannot be directly compared with the original taxonomy given the differences in the calculation of the differentiation, centralization, and integration concepts. (See the Appendix S1 for a taxonomy based on the originally calculated measures and analytic approach). Given available data, the taxonomy also does not take into account the intensity or degree to which the various services are offered as it only counts if it is offered. Thus, hospitals in two systems may each score similarly on offering ICU or cardiology services, for example, but these services might comprise 50% of all admissions for hospitals in one system versus 25% in another. Linking the taxonomy to claims‐based or related sources of data on admissions and service intensity can provide such refinement. One could also, for example, calculate the ratio of outpatient visits to inpatient admissions by service categories of interest. Such calculations may potentially provide a more nuanced taxonomy that policymakers could use in assessing the benefits as well as negative aspects of potential mergers. Finally, as with the original taxonomy, the survey‐based measures of centralization and integration are broad‐based structural measures that do not necessarily fully capture these dimensions of being a hospital system. The usefulness of the taxonomy may be enhanced when coupled with more fine grained largely qualitative data collection that may provide a more nuanced understanding of these and related dimensions of health systems. 18
4. DISCUSSION/IMPLICATIONS
The new taxonomy of hospital‐based systems can be used as in the past 8 , 9 , 10 , 11 , 12 , 13 to examine important public policy issues. By linking to Medicare and commercial claims data issues involving cost containment, reducing unnecessary admissions and readmissions, improving quality, patient safety and the patient experience, and improving access to care can be addressed. The taxonomy can also be used to examine the growing trend toward increased vertical integration of hospitals and physician practices 14 , 19 and hospital and health system consolidation relevant to the growing concern over increased prices 2 , 20 , 21 with mixed evidence of offering any offsetting advantages in quality of care. 14 , 22 The more centralized cluster 3 systems, for example, might be examined for potential anti‐competitive behavior depending on the degree to which the markets in which they are located are concentrated. Attention might also be given to the potential anti‐competitive effects of hospitals that merge across clusters.
The taxonomy can also be used to assess the types of systems that are most likely to participate or expand their participation in the newly evolving value‐based payment models from CMS and commercial insurers. These models provide incentives for hospitals to become more involved in quality improvement initiatives and provide performance feedback to physicians. This raises the question of what types of systems are more or less likely to do so? For example, the cluster 2 system hospitals with a more bureaucratic and rational oriented culture were more likely to share electronic health records (EHRs). EHRs can help to facilitate the use of standardized care guidelines and related care management processes needed to succeed under risk‐based payment models. Existing taxonomies of ACOs and hospitals participating in ACOs 23 , 24 could also be merged or overlaid with the present system taxonomy to assess differences in involvement in such payment related innovations and the implications for performance.
Given the growing importance of the social determinants of health, the taxonomy may also prove useful in assessing patterns of involvement with community‐based organizations (CBOs) in the education, housing, transportation, and social services sectors. For example, cluster 3 systems are the most differentiated in offering more community‐oriented and related services. Therefore, one might expect cluster 3 system hospitals to be further advanced in developing partnerships with such CBOs.
The taxonomy may also help in identifying hospitals that were better able to address the Covid‐19 pandemic. The pandemic caused nearly all hospitals to rapidly adjust treatments for an influx of patients. These changes included use of personal protective equipment (PPE), ICU bed availability, use of ventilators, and staffing among others. As such, the cluster 3 system hospitals being centralized and with more integrated physician arrangements, but also having a more innovation‐oriented culture may have fared best. The taxonomy can be used to assess long run hospital recovery from the pandemic. The cluster 4 systems composed primarily of small, rural, and critical hospitals highlight the need for continued investment and innovation in how best to deliver value‐based care to people living in the rural areas of the United States. A crosscutting question is the extent to which systems that appear to still be operating largely as holding companies can provide the locus for change that the emerging health care reforms require?
5. CONCLUSION
The new taxonomy of hospital‐based health systems, despite differences in calculating the underlying concepts, bears similarities as well as differences to the original taxonomy of 20 years ago. There remains a cluster of systems that are highly centralized and highly differentiated. There also remains a cluster that is much less differentiated. These are composed of small, largely rural, and critical access hospitals. Overall, the majority of systems are decentralized and may be operating largely as holding companies. Going beyond data available in the past, predictions of how hospitals belonging to the different types of systems would respond to questions from the independent NSHOS were largely confirmed. The taxonomy holds promise for examining a variety of issues related to the cost, quality and patient experience of care, value‐based payment reform, vertical and horizontal consolidation, biomedical and care delivery innovations, linkage of systems to community‐based organizations (CBOs), recovery from Covid‐19, and for addressing the special challenges of rural hospital‐based systems.
Supporting information
Supplementary Material
Supplementary Material
Supplementary Material
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: This research was supported by Grant # 1U19HS024075 from the Agency for Healthcare Research and Quality (AHRQ) Center of Excellence Program on Comparative Health System Performance. We thank Ellen Meara for her comments on an earlier draft of this manuscript and Elliott Fisher, Taressa Fraze, Marisha Palm, Maia Crawford, Dora Mairena, and all those who were involved in the development and execution of the National Survey of Healthcare Organizations and Systems (NSHOS) upon which some of the analysis in this paper is based. The statements, findings, conclusions, viewpoints, and opinions contained and expressed herein are not necessarily those of IQVIA Inc or any of its' affiliated or subsidiary entities.
The only financial support for the project relevant to this paper is the grant from the Agency for Heath Research and Quality as noted in the Acknowledgment section. As noted all authors were involved in nearly all aspects of the paper. Other contributors noted above played various supportive roles in managing the overall grant upon which this paper is based. There is nothing else to disclose.
Shortell SM, Gottlieb DJ, Martinez Camblor P, O’Malley AJ. Hospital‐based health systems 20 years later: A taxonomy for policy research and analysis. Health Serv Res.2021;56:453–463. 10.1111/1475-6773.13621
REFERENCES
- 1. Furukawa MF, Machta RM, Barrett KA, et al. Landscape of health systems in the United States. Med Care Res Rev. 2020;77(4):357‐366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gaynor M. Examining the Impact of Health Care Consolidation: Statement before the Beaulieu ND , Beaulieu ND,, et al. Changes in quality of care after hospital mergers and acquisitions. N Engl J Med. 2020;382(1):51‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Beaulieu ND, Dafny LS, Landon BE, Dalton JB, Kuye I, McWilliams MJ. Changes in quality of care after hospital mergers and acquisitions. N Engl J Med. 2020;382(1):51‐59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shrank WH, Rogstad TL, Parekh N. Waste in the US health care system: estimated costs and potential cost savings. JAMA. 2019;322(15):1501‐1509. [DOI] [PubMed] [Google Scholar]
- 5. Burns LR, Pauly MV. Transformation of the Health care industry: curb your enthusiasm? Milbank Q. 2018;96(1):57‐109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bazzoli GJ, Shortell SM, Dubbs N, Chan C, Kralovec P. A taxonomy of health networks and systems: bringing order out of Chaos. Health Serv Res. 1999; 33(6):1683‐1717. [PMC free article] [PubMed] [Google Scholar]
- 7. Dubbs NL, Bazzoli GJ, Shortell SM, Kralovec PD. Reexamining organizational configurations: an update, validation, and expansion of the taxonomy of health networks and systems. Health Serv Res. 37(1):207‐220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bazzoli GJ, Chan B, Shortell M, D’Aunno T. The financial performance of hospitals belonging to health networks and systems. Inquiry. 2000;37:234‐252. [PubMed] [Google Scholar]
- 9. Ford EW, Short JC. The impact of health system membership on patient safety initiatives. Healthc Manage Rev. 2008;33(1):13‐20. [DOI] [PubMed] [Google Scholar]
- 10. Chukmaitov AS, Bazzoli GJ, Harless DW, Hurley RE, Devers KJ, Zhao ME. Variations in inpatient mortality among hospitals in different system types, 1995 to 2000. Med Care. 2009; 47(4):466‐473. [DOI] [PubMed] [Google Scholar]
- 11. Opoku‐Agyeman W. Are there differences in health information exchange by health system type? Healthc Manage Rev. 2016;41(4):325‐333. [DOI] [PubMed] [Google Scholar]
- 12. Burns LR, McCullough JS, Wholey DR, Kruse G, Kralovec P, Muller R. Is the system really the solution? Operating costs in hospital systems. Med Care Res Rev. 2015;72(3):247‐272. [DOI] [PubMed] [Google Scholar]
- 13. Walker DM, Mora AM, Hogan TH, Diana ML, McLearney AS. Assessing trends in hospital system structures from 2018 to 2015. Med Care. October, 2018; 56(10): 831‐839.2.2. Gaynor M. Examining the Impact of Health Care Consolidation: Statement before the Committee on Energy and Commerce Oversight and Investigations Subcommittee. Washington, DC: US House of Representatives. February 14, 2018.30113422 [Google Scholar]
- 14. Post B, Buchmueller T, Ryan AM. Vertical integration of hospitals and physicians: economic theory and empirical evidence on spending and quality. Med Care Res Rev. 2018;75(4):399‐433. [DOI] [PubMed] [Google Scholar]
- 15. Scheffler RM, Arnold DR, Whaley CM. Consolidation trends in California’s health care system: impacts On ACA premiums and outpatient visit prices. Health Aff. 2018;37(9):1409‐1416. [DOI] [PubMed] [Google Scholar]
- 16. Quinn RE, Rohrbaughh J. A competing values approach to organizational effectiveness. Public Prod Rev. 1981;5:122‐140. [Google Scholar]
- 17. Zazzali JL, Alexander JA, Shortell SM, Burns LR. Organizational culture and physician satisfaction with dimensions of group practice. Health Serv Res. 2006;42(3):1150‐1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ridgely SM, Duffy E, Wolf L, et al. Understanding the U.S. health systems: using mixed methods to unpack organizational complexity. J Electronic Health Data Methods. 2019;7(1):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Baker LC, Bundorf KM, Devlin AM, Kessler DP. Hospital ownership of physicians: hospital versus physician perspectives. Med Care Res Rev. 2018;75(1):88‐99. 10.1177/1077558716676018 [DOI] [PubMed] [Google Scholar]
- 20. Cutler DM, Scott MF. Hospitals, market share, and consolidation. JAMA. 2013;310(18):1964‐1970. [DOI] [PubMed] [Google Scholar]
- 21. Frakt AB. Hospital consolidation isn’t the key to lowering cots and raising quality. JAMA. 2015;313(4):345. [DOI] [PubMed] [Google Scholar]
- 22. Fisher ES, Shortell SM, O’Malley AJ, et al. Do integrated systems adopt more care delivery and payment reforms? results from a national Survey. Health Aff. 2020;39(8):1‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wu FM, Shortell SM, Lewis VA, Colla CH, Fisher ES. Assessing differences between early and later adopters of accountable care organizations’ using taxonomic analysis. Health Serv Res. 2016; 51(6):2318‐2329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bazzoli GJ, Harless DW, Chukmaitov AS. A taxonomy of hospitals participating in Medicare accountable care organizations. Health Care Manage Rev. 2019;44(2):93‐103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Supplementary Material
Supplementary Material


