Abstract
Objective
Dual Eligible Special Needs Plans (D‐SNPs) were intended to provide better care for beneficiaries eligible for both Medicare and Medicaid through better coordination of these two programs.
Data Sources
671 913 dual eligible (DE) respondents to the 2009‐2019 Medicare Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey.
Study Design
We compared the 2015‐2019 experiences of DE beneficiaries in D‐SNPs relative to fee‐for‐service Medicare (FFS) and non‐SNP Medicare Advantage (MA) using propensity‐score weighted linear regression. Comparisons were made to 2009‐2014. 12 patient experience measures were considered.
Data Collection Methods
Annual mail survey with telephone follow‐up of non‐respondents.
Principal Findings
More than 65% of DE beneficiaries enrolled in FFS. Of 12 measures, D‐SNP performance was higher than non‐SNP MA on two (P < .05), lower than non‐SNP MA on two (P < .05), and higher than FFS on four (P < .01). DE beneficiaries did not report better coordination of care in D‐SNPs. D‐SNP performance was often worse than other coverage types in prior periods.
Conclusions
Relative to FFS Medicare, DE beneficiaries report higher immunization rates in D‐SNPs, but slight or no better performance on other dimensions of patient experience. New requirements in 2021 may help D‐SNPs attain their goal of better care coordination.
Keywords: Medicaid, Medicare, patient experience, special needs plans
What is Known
Beneficiaries eligible for both Medicare and Medicaid are a vulnerable population who account for a disproportionate share of spending in both public programs.
A lack of alignment between the programs has led to reduced health care quality and increased costs.
Dual Eligible Special Needs Plans were intended to better integrate the health benefits of Medicare and Medicaid.
What This Study Adds
Beneficiaries eligible for both Medicare and Medicaid have somewhat better experiences with immunizations and overall ratings of care in Dual Eligible Special Needs Plans than other forms of Medicare coverage.
Beneficiaries eligible for both Medicare and Medicaid do not report better experiences with coordination of care, with doctors, or with receiving care quickly or when needed in Dual Eligible Special Needs Plans than other forms of Medicare coverage.
While Dual Eligible Special Needs Plans have improved over time relative to other coverage types, they are not yet meeting their goal of improved care coordination.
1. INTRODUCTION
Under the Medicare Modernization Act of 2003, Congress established Dual Eligible Special Needs Plans (D‐SNPs) as a new plan type within Medicare Advantage (MA), the private managed care Medicare option, seeking to better integrate the health benefits of dual eligible (DE) beneficiaries eligible for both Medicare and Medicaid. This created a third coverage option for DE beneficiaries, in addition to fee‐for‐service Medicare with stand‐alone prescription drug coverage (FFS + PDP) and non‐SNP MA plans. Enrollment in D‐SNPs has grown steadily from approximately 750 thousand in 2007 to 2.49 million in 2019, 1 , 2 , 3 with the number of D‐SNPs ranging between 210‐440 plans in a given plan year. 4 , 5
DE beneficiaries account for a disproportionate share of spending in both public programs. In 2015, DE beneficiaries were 20% of the Medicare population but accounted for 34% of Medicare spending (169.9 billion dollars). The high medical costs of this population in part reflect their greater disease burden. DE beneficiaries have more chronic conditions and cognitive and functional limitations than non‐DE Medicare beneficiaries and 43% qualify for Medicare through disability rather than age, more than triple the rate for other Medicare beneficiaries. 6 There are concerns that quality of care may be lower and costs unnecessarily high for this medically and financially vulnerable population due to poor coordination between the two complex public insurance programs, Medicare and Medicaid, 7 , 8 which have different enrollment criteria, covered benefits, payment structures, and in some cases, provider networks. Due to the sharing of costs for some types of care between the two programs (eg, hospital care), cost inefficiencies affect both programs. For these reasons, care coordination is crucial, particularly for the many DE beneficiaries whose well‐being depends on the management of complex or advanced conditions. 9 Such concerns prompted the creation of the Medicare and Medicaid Coordination Office under the 2011 Affordable Care Act whose 2016 report stated, “A lack of alignment and cohesiveness between the programs can lead to fragmented or episodic care for Medicare‐Medicaid enrollees and misaligned incentives for both payers and providers, resulting in reduced quality and increased costs to both programs and to enrollees” (page 6). 6
Unlike Medicaid managed care, enrollment in D‐SNPs is voluntary, and most DE beneficiaries continue to select FFS + PDP Medicare coverage instead. In 2008, 80% of DE beneficiaries enrolled in FFS + PDP with the remaining 20% in some form of MA plan. By 2017, DE enrollment in MA had increased to 36%. 10
Unlike non‐SNP MA plans which must accept any Medicare beneficiary, D‐SNPs limit enrollment to DE beneficiaries and are intended to cater their benefits to this population. Most MA plans receive rebates, which are applied to reducing plan premiums and/or providing supplemental medical benefits, similar to the costs and benefits a Medigap plan would cover for a Medicare beneficiary with FFS coverage. Compared with non‐SNP MA plans, D‐SNPs have comparable rebates but spend a much higher proportion of the rebates on supplemental benefits (hearing, vision, and dental) rather than reductions in premiums or cost‐sharing, as those are usually covered by Medicaid for DE beneficiaries. 11
At a minimum, D‐SNPs are responsible for providing or arranging Medicaid benefits, beneficiary cost‐sharing protections, information sharing, and eligibility verification. 12 Between 2006 and 2017, D‐SNPs were re‐authorized by Congress seven times for one to three additional years and often with additional requirements (see Appendix S1). 13 For example, the 2009‐2010 policy environment for D‐SNPs involved (a) a 1‐year moratorium imposed on new D‐SNPs in 2009 by the Medicare, Medicaid, and State Children's Health Insurance Program (SCHIP) Extension Act of 2007, 14 and (b) the Medicare Improvements for Patients and Providers Act (MIPPA) of 2008, which required D‐SNPs to submit “models of care” that provided details about how plans intended to coordinate care for DE beneficiaries. 15 In 2011, the ACA added a new requirement that all D‐SNPs submit quality data to the National Committee on Quality Assurance and be rated on their “models of care,” a quality improvement tool meant to ensure that D‐SNPs meet the needs of their enrollees. The ACA also established Fully Integrated Dual Eligible SNPs (FIDE‐SNPs). To qualify as a FIDE‐SNP, D‐SNPs have to contract with a state Medicaid Agency. 16 , 17 This designation became available in 2012. Further, the American Taxpayer Relief Act (2012) required that all D‐SNPs contract with a state Medicaid Agency by the beginning of 2013. 17 In 2018, D‐SNPs (along with the other types of SNPs) were permanently re‐authorized under the Bipartisan Budget Act of 2018. 18 , 19
Although D‐SNPs have been operating for more than a decade, and their continuation was recently made permanent, little is known about whether they provide better care for DE beneficiaries than other Medicare coverage options. Evaluation efforts have been hampered by data constraints that include incomplete identification of DE beneficiaries and unavailability of detailed service use information in the managed care setting. 20 Most prior research has compared performance in D‐SNPs to performance for Medicare beneficiaries with other coverage types, which is difficult to interpret due to the stark differences between DE and non‐DE beneficiary populations. 21 One exception examined the quality of clinical of care received in 2017 for DE beneficiaries with partial dual benefits, who comprise about 26% of D‐SNP enrollees. Medicaid pays the premiums for this subgroup, but only pays other cost‐sharing for some, and most in this group are not eligible for other Medicaid benefits, such as long‐term care. For this subgroup, clinical performance was similar for D‐SNP enrollees relative to DE enrollees in non‐SNP MA‐PD on all but four of 40 HEDIS measures, with two measures better in D‐SNPs and the other two better in non‐SNP MA‐PD.
We add to the literature on the effectiveness of D‐SNPs by comparing the recent experiences of DE beneficiaries enrolled in D‐SNPs to experiences of otherwise similar DE beneficiaries with FFS + PDP and non‐SNP MA‐PD coverage using beneficiary reports of their experiences with health care, as measured by the nationally representative Medicare Consumer Assessments of Healthcare Providers and Systems (Medicare CAHPS®) survey. Beneficiaries reported their experiences with aspects of care that can best or only be observed by the patient, such as getting needed care, getting care quickly, doctor communication, and care coordination. A recent review found that better patient experiences were associated with better clinical outcomes, higher rates of adherence to recommended prevention and treatment processes, and lower health care utilization. 22 We also compare the most recent period, 2015‐2019, to two earlier periods, 2009‐2010 and 2012‐2014, when D‐SNPs were subject to fewer requirements.
We hypothesize that DE beneficiaries in D‐SNPs will report better experiences with care than DE beneficiaries in both FFS + PDP and non‐SNP MA‐PD on measures related to or requiring care coordination. Relative to the majority of DE beneficiaries in FFS + PDP coverage, we also hypothesize better experiences for DE beneficiaries in D‐SNPs on measures that address aspects of care known to be a strength of managed care (eg, immunization receipt). We expect D‐SNP performance to improve over time as they were subject to additional requirements.
DE beneficiaries are a diverse group and D‐SNPs vary by state. To address this complexity, we also compared experiences of DE beneficiaries younger than 65, who all qualify for Medicare through disability, to those 65 and older, who currently qualify for Medicare by age. The health care needs of these age groups differ, and for those younger than 65 with partial Medicaid eligibility, there can be barriers to obtaining Medigap insurance that make MA‐PD and D‐SNP options potentially lower cost means of obtaining supplemental coverage. We also estimated heterogeneity of experiences across states, focusing on those which have more restrictive eligibility provisions intended to create greater opportunities for care coordination.
2. METHODS
All DE beneficiaries have access to Part D prescription drug coverage through Medicaid payment of Medicare Part D premiums. Thus, coverage options for DE beneficiaries are FFS + PDP or a Medicare Advantage plan with prescription drug coverage (MA‐PD), a category which includes all D‐SNPs.
2.1. Data and measures
We analyzed 10 years of Medicare CAHPS data divided into three time periods: 2009‐2010, 2012‐2014, and 2015‐2019, corresponding to the imposition of additional criteria for D‐SNPs. We omitted 2011 from the analysis because the data field identifying DE respondents was unavailable in that year. We restricted the analysis sample to DE beneficiaries (n = 671 913). All analyses excluded beneficiaries living in Puerto Rico and the Virgin Islands, as health care in these US territories differs from care in the mainland US. 23 We also excluded beneficiaries enrolled in Private FFS, as the sample of DE beneficiaries in this coverage type is quite small (1% or less).
We examined 11 CAHPS measures over the full study period: four health care measures—overall ratings of doctor, specialist, and health care received, and a composite measure of doctor communication; two immunization receipt measures—single items on past year flu immunization and lifetime pneumonia immunization; two access measures —composites regarding ease of getting needed care and getting care quickly; and three Part D prescription drug coverage measures—overall rating of prescription drug plan and composites regarding ease of getting needed drugs and getting information on drugs (this measure was not available in 2018‐2019). We also analyzed a CAHPS composite measure assessing coordination of care, as well as its individual items, which were added to the survey in 2012, and thus are available in the two later periods of data. Although not available for the whole time period, these items are particularly salient, as D‐SNPs were primarily intended to improve coordination of care between Medicare and Medicaid.
Response options for the items comprising each measure were dichotomous, four ordered categories, or 11 ordered categories, see the “MA & PDP CAHPS English Survey Materials ” for item wording, 24 and methods for constructing the composites in the Medicare Advantage and Prescription Drug Plan “Quality Assurance Protocols & Technical Specifications Version 9.0” (page 61). 25 All patient experience measures were recoded to a 0‐100 scale for ease of interpretation.
2.2. Statistical analyses
Sampling weights are applied to make the sample represent the population of community‐dwelling DE beneficiaries. These weights account for sample design and address non‐response by matching weighted sample and enrolled populations in each contract‐by‐county combination on sex, age, race/ethnicity, Medicaid eligibility/low‐income subsidy enrollment status, special needs plan enrollment, and zip‐code level distributions of income, education, and race/ethnicity. 26 , 27 To address systematic differences between DE beneficiaries who do and do not enroll in D‐SNPs, we applied propensity‐score weighting to match observable beneficiary characteristics of non‐SNP MA‐PD or FFS + PDP DE comparison cases to the corresponding distributions for D‐SNP enrollees. These characteristics (see Appendix S2) include sociodemographics (gender, race/ethnicity, age, education, state blocks, and urbanicity) and health characteristics (self‐rated general and mental health, five disease indicators, proxy response). States were pooled into neighboring multi‐state blocks where necessary to obtain adequate sample sizes in D‐SNP and comparison coverage type samples (see Appendix S2). Propensity scores were estimated from multinomial generalized boosted regression, implemented via the twang package in R. 28 Three weighted propensity‐score models were run, one for each time period and each predicting whether a DE beneficiary enrolled in D‐SNP, FFS + PDP, or non‐SNP MA‐PD coverage, where person‐level weights addressed sample design and non‐response. Propensity‐score weights for DE beneficiaries with FFS + PDP coverage and non‐SNP MA‐PD coverage were calculated so the weighted distribution of each group approximated the covariate distribution of the D‐SNP group. To assess the success of the propensity‐score weighting, we compared standardized mean differences of the sociodemographic and health characteristics in each of the three populations (D‐SNPs and the two comparison groups) before and after propensity‐score weighting, by time period. A typical metric of success for balance on covariates is that all or nearly all of the propensity‐score weighted means differ by less than 0.25 of the standard deviation of each covariate. 29
We estimated average differences in the beneficiary experience measures for DE beneficiaries in D‐SNPs vs DE beneficiaries in other coverage types with propensity‐score weighted linear regression models that also included the propensity‐score model predictors as covariates. This “doubly robust” approach assumes only that either the selection model or the regression model is correctly specified, and retains reasonable accuracy even under mild violations of its assumptions. 30 , 31
The primary outcome models tested for differences between the three coverage types in the most recent study period, 2015‐2019. Separate models, which used only data for those enrolled in D‐SNPs and random effects for D‐SNPs, were used to estimate D‐SNP‐level standard deviations (square root of the random effect variance component) for each Medicare CAHPS outcome. These plan‐level standard deviations were used to calculate effect sizes for the D‐SNP performance gap estimates. We also use the patient experience heuristic that differences of 1, 3, and 5 points on the 100‐point scale be considered small, moderate, and large respectively. 32 Secondary analyses tested for trends in the coverage differences over the three study periods by interacting the coverage types with indicators for each of the earlier time periods when different D‐SNP related policies were in place.
To test for different experiences with D‐SNPs for those 64 and younger, we interacted an indicator for <65 with the three coverage types in the main 2015‐2019 models (we also use a single < 65 indicator of younger age in these models instead of the three separate younger age groups used in all other models). Six states (AZ, HI, ID, MA, MN, NJ) had active regulations throughout 2015‐2019 restricting D‐SNP eligibility to DE beneficiaries with full Medicaid benefits, for whom greater coordination of care is feasible. To test for different experiences with D‐SNPs operating in these states, we interacted an indicator for these high‐coordination states with the three coverage types in the main 2015‐2019 models.
3. RESULTS
3.1. Descriptive statistics, selection into D‐SNPs, and propensity‐score weighting to create comparable groups
Between 2015‐2019, relative to those in FFS + PDP, DE beneficiaries who enrolled in D‐SNPs were older, reported slightly better general and mental health status, had lower educational attainment, were more likely to live in urban areas, were more likely to be Black, Hispanic, or Asian/Pacific Islander, and were more likely to have been diagnosed with diabetes and somewhat less likely to have been diagnosed with chronic obstructive pulmonary disease, angina, heart attack or cancer (Table 1). DE beneficiaries who enrolled in other non‐SNP MA‐PD plans were older and in better health than those in either of the other 2 coverage types. The racial/ethnic distribution of DE beneficiaries in non‐SNP MA‐PD plans was similar to that of DE beneficiaries in FFS + PDP, except that a higher proportion of Hispanic beneficiaries enrolled in non‐SNP MA‐PD, though not as high as in D‐SNPs (P < .001 for all differences in this paragraph).
TABLE 1.
Descriptive Characteristics of Dually Eligible Beneficiaries in Fee‐For‐Service Prescription Drug Plans (FFS + PDP), Dual Eligible Special Needs Plans (D‐SNP), and Non‐Special Needs Plan Medicare Advantage‐Prescription Drug Plans (Non‐SNP MA‐PD) (2015‐2019)
| FFS + PDP | D‐SNP | Non‐SNP MA‐PD | Overall | |
|---|---|---|---|---|
| N | 62 872 | 153 258 | 123 064 | 339 194 |
| Age | ||||
| 18‐64 | 47.3% *** | 34.2% | 30.0% *** | 44.3% |
| 65‐79 | 35.7% | 48.3% | 49.0% | 38.3% |
| 80+ | 17.0% | 17.4% | 21.0% | 17.4% |
| Education | ||||
| <High School degree | 32.2% *** | 40.3% | 34.5% *** | 33.2% |
| High School degree or some college | 57.4% | 51.4% | 55.6% | 56.6% |
| College degree+ | 10.4% | 8.3% | 9.8% | 10.1% |
| General health | ||||
| Fair or poor | 50.1% *** | 48.5% | 44.3% *** | 49.4% |
| Good | 31.8% | 32.2% | 34.3% | 32.1% |
| Very good or excellent | 18.0% | 19.3% | 21.4% | 18.5% |
| Mental health | ||||
| Fair or poor | 35.2% *** | 33.1% | 28.7% *** | 34.3% |
| Good | 32.7% | 32.9% | 33.0% | 32.9% |
| Very good or excellent | 32.1% | 34.0% | 38.3% | 32.9% |
| Proxy assistance | ||||
| Any | 28.9% *** | 23.0% | 20.2% *** | 27.5% |
| Answered questions | 10.4% *** | 6.6% | 6.1% | 9 |
| Male gender | 40.3% *** | 37.0% | 37.1% | 39.7% |
| Race/ethnicity | ||||
| White | 56.9% *** | 36.0% | 47.6% *** | 53.9% |
| Black | 18.2% | 24.5% | 19.4% | 19.0% |
| Hispanic | 13.8% | 27.9% | 23.4% | 16.2% |
| Asian/Pacific Islander | 6.7% | 8.1% | 6.6% | 6.9% |
| Native American | 4.3% | 3.4% | 3.0% | 4.1% |
| Urban | ||||
| Metro area of 1 million+ | 43.2% *** | 63.6% | 61.8% *** | 47.1% |
| Chronic conditions | ||||
| Heart attack | 11.6% *** | 10.1% | 10.2% | 11.3% |
| Angina | 14.8% *** | 13.2% | 13.6% | 14.5% |
| Cancer | 11.1% *** | 8.9% | 9.8% *** | 10.8% |
| Chronic Obstructive Pulmonary Disease | 25.7% * | 24.7% | 22.3% *** | 25.3% |
| Diabetes | 33.6% *** | 37.1% | 34.7% *** | 34.0% |
P < .05 for difference vs D‐SNP.
P < .001 for difference vs D‐SNP.
Propensity‐score weighted means of all observed characteristics for DE beneficiaries in FFS + PDP and non‐SNP MA‐PD were similar to those of DE beneficiaries in D‐SNPs and to each other (Appendix S2). After propensity weighting, the largest standardized mean difference across all periods and for both comparison groups was 0.16, well under the conventional criterion “standardized difference < 0.25.” 29
3.2. Differences in DE beneficiary reports of experiences with care between D‐SNPs and other Medicare coverage types 2015‐2019
Table 2 and Figure 1 show the average differences in DE beneficiaries’ experiences when enrolled in D‐SNPs vs the other two coverage types after propensity‐score weighting and regression‐based covariate adjustment (see Appendix S3 for full results).
TABLE 2.
2015‐2019 Differences in Dually Eligible Beneficiary Experiences with Care, Dual Eligible Special Needs Plans (D‐SNP) vs Fee‐For‐Service Prescription Drug Plans (FFS + PDP) and Non‐Special Needs Plan Medicare Advantage‐Prescription Drug Plans (Non‐SNP MA‐PD)
| Patient experience measure |
D‐SNP‐ FFS + PDP |
Non‐SNP MA‐PD‐ FFS + PDP |
D‐SNP‐ Non‐SNP MA‐PD |
D‐SNP Standard Deviation a | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient | Stand. error | Sig | Stand. coefficient | Coefficient | Stand. error | Sig | Stand. coefficient | Coefficient | Stand. error | Sig | Stand. coefficient | ||
| Coordination of care | −0.01 | 0.27 | 0.22 | 0.20 | −0.23 | 0.26 | 3.77 | ||||||
| Rate doctor | 0.41 | 0.24 | 0.63 | 0.26 | * | 0.17 | −0.22 | 0.22 | 3.64 | ||||
| Doctor communication | 0.43 | 0.25 | 0.66 | 0.27 | * | 0.16 | −0.23 | 0.24 | 4.23 | ||||
| Rate specialist | 0.18 | 0.30 | −0.15 | 0.34 | 0.32 | 0.32 | 3.93 | ||||||
| Getting needed care | −0.37 | 0.33 | −0.74 | 0.35 | * | −0.15 | 0.37 | 0.32 | 4.97 | ||||
| Getting care quickly | −0.10 | 0.34 | 0.59 | 0.36 | −0.68 | 0.33 | * | −0.12 | 2.96 | ||||
| Rate care | 1.44 | 0.26 | *** | 0.39 | 1.47 | 0.29 | *** | 0.39 | −0.02 | 0.24 | 3.36 | ||
| Rate prescription drug plan | 1.70 | 0.55 | ** | 0.39 | 0.68 | 0.55 | 0.39 | 1.03 | 0.23 | *** | 0.24 | 4.35 | |
| Getting needed drugs | 0.70 | 0.57 | 0.54 | 0.57 | 0.16 | 0.26 | 4.17 | ||||||
| Getting drug information b | 3.52 | 1.97 | 6.03 | 1.91 | ** | 0.84 | −2.52 | 0.98 | * | −0.35 | 7.19 | ||
| Influenza immunization | 4.62 | 0.62 | *** | 0.41 | 3.34 | 0.67 | *** | 0.29 | 1.29 | 0.54 | * | 0.11 | 11.35 |
| Pneumonia immunization | 2.21 | 0.65 | *** | 0.22 | 1.22 | 0.69 | 0.99 | 0.55 | 10.26 | ||||
Stand. Coefficient is the coefficient standardized by the SNP standard deviation for the corresponding measure, a measure of effect size.
standard deviation is the square root of the D‐SNP benefit package variance component from mixed models.
This measure was not included on the survey after 2016 so the results for this measure are for 2015‐2016 only.
P ≤ .05.
P ≤ .01.
P ≤ .001.
FIGURE 1.
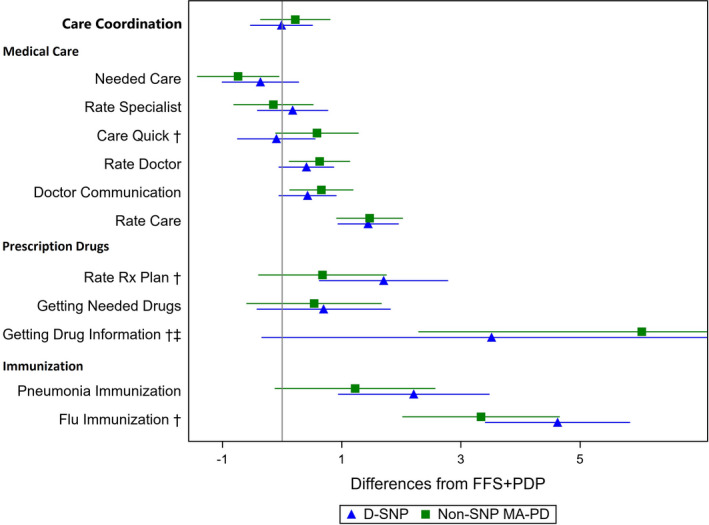
Differences for Dual Eligible Beneficiaries in Fee‐For‐Service Prescription Drug Plan (FFS + PDP, reference) vs Dual Eligible Special Needs Plan (D‐SNP) and non‐Special Needs Plan Medicare Advantage‐Prescription Drug Plan (non‐SNP MA‐PD). Notes: The vertical reference line represents the experiences of Dual Eligible (DE) beneficiaries in fee‐for‐service with Prescription Drug Plan (FFS + PDP) coverage, the dominant coverage type. The green squares, with 95% confidence lines, show the difference between this reference level and the experiences of DE beneficiaries in non‐Special Needs Plan Medicare Advantage‐Prescription Drug Plans (non‐SNP MA‐PD). The blue triangles, with 95% confidence lines, show the difference between the FFS + PDP reference level and the experiences of DE beneficiaries in Dual Eligible Special Needs Plans (D‐SNP). †The differences in patient experiences between D‐SNP and non‐SNP MA‐PD differ significantly (p<0.05) for older vs younger beneficiaries. ‡This measure was available only in 2015‐2016
DE beneficiaries have similar experiences with coordination of care in all 3 coverage types. For all other measures related to medical care, DE beneficiary experiences are also similar (12 of 16 comparisons) or differ by less than 1 point on a 100‐point scale. Despite these similar experiences on four measures, DE beneficiaries rate overall care higher in both forms of managed care than in FFS + PDP (by + 1.4 or + 1.5 points, P < .001 for both), with no difference between the two managed care types.
On prescription drug measures, DE beneficiaries report similar experiences across plan types for four of six comparisons. For getting drug information, experiences are better in “regular” MA than in FFS + PDP (+6.0 points, P < .01) but D‐SNPs do not achieve this improvement (−2.5 relative to non‐SNP MA‐PD, P < .05). On the overall rating of prescription drug plan, ratings for D‐SNPs are higher than for both other coverage types (+1.7 relative to FFS + PDP, +1.0 relative to non‐SNP MA‐PD, P < .01 for both).
On flu immunization, both forms of MA perform better than FFS + PDP and D‐SNPs have additionally higher immunization rates (+3.3 for non‐SNP MA‐PD (P < .001), an additional 1.3 for D‐SNP (P < .05)). DE beneficiaries receive pneumonia immunizations at 2.2 percentage point higher rates in D‐SNPs than in FFS + PDP (P < .001).
To further interpret the magnitude of these differences, we calculated effect sizes relative to the D‐SNP plan‐level standard deviation of MCAHPS scores. Mean D‐SNP performance was between 0.2 and 0.4 plan‐level standard deviations better than FFS + PDP performance on the four measures where it had higher performance. These effect sizes are generally considered to be small to moderate differences. 32 , 33 Two of the differences between D‐SNP and non‐SNP MA‐PD reflect small effect sizes, for getting care quickly and flu immunization, and the other two show moderate effect sizes, rating of PDP (higher in D‐SNPs) and getting drug information (lower in D‐SNPs).
3.3. Trends in D‐SNP performance over time
There is consistent evidence that coordination of care improved in D‐SNPs from 2012‐2014 to 2015‐2019 relative to other coverage types (see Appendix S4); both the composite and its component items. In 2012‐2014, experiences with coordination of care were worse in D‐SNPs than in both FFS + PDP and non‐SNP MA‐PD (P < .05 for both). By the 2015‐2019 period, D‐SNPs had improved relative to other coverage types such that experiences with coordination of care were similar.
While the time patterns varied for other measures, there was often evidence of improvements in D‐SNPs relative to other coverage options, as more stringent requirements for D‐SNPs were enacted (see Appendix S5). For instance, in one or both earlier periods, DE beneficiaries in D‐SNPs reported worse experiences than DE beneficiaries in FFS + PDP on getting care needed, doctor communication, and rating of specialist—all of which D‐SNPs have since improved to where experiences are similar. Figure 2 illustrates this result for rating of specialist. Similarly, DE beneficiaries in D‐SNPs reported worse experiences than those in non‐SNP MA‐PD in one or both earlier periods on getting needed care, getting care quickly, and doctor communication—only one of which remains worse in the most recent period. For the only two measures where DE beneficiaries in D‐SNPs recently reported better experiences than in non‐SNP MA‐PD, rating of care, and flu immunization, experiences were not better in either earlier period (Flu immunization Figure S1 in Appendix S5).
FIGURE 2.
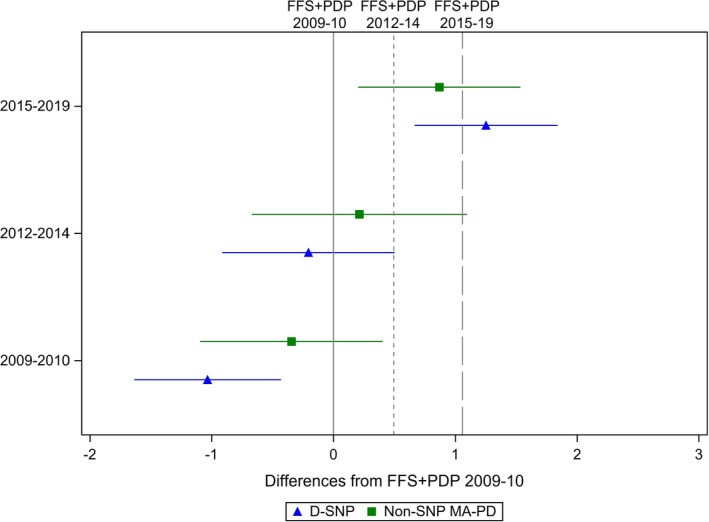
Improvements Over Time for Dual Eligible Beneficiaries in Fee‐For‐Service Prescription Drug Plan (FFS + PDP, reference) vs Dual Eligible Special Needs Plan (D‐SNP) and non‐Special Needs Plan Medicare Advantage‐Prescription Drug Plan (non‐SNP MA‐PD): Rate Specialist
3.4. D‐SNP performance for younger disabled DE beneficiaries vs older DE beneficiaries
Some patterns of D‐SNP performance differed for DE beneficiaries younger than 65, who are eligible for Medicare through disability, and DE beneficiaries 65 and older (see Appendix S6 for key results and Appendix S7 for full results). Relative to FFS + PDP, performance of D‐SNPs was mostly consistent for older vs younger disabled DE beneficiaries.
As shown in Figure 3, there were more differences by age group in comparisons between D‐SNP and non‐SNP MA‐PD. Older DE beneficiaries rated their PDP higher in D‐SNPs than in non‐SNP MA‐PD, but report worse experiences with coordination of care, getting care quickly, getting drug information, and rating of care (P < .05 for all). For younger disabled DE beneficiaries, experiences are largely similar in these two coverage types, with somewhat better experiences on two measures, rating of care and rating of PDP (P < .05 for both).
FIGURE 3.
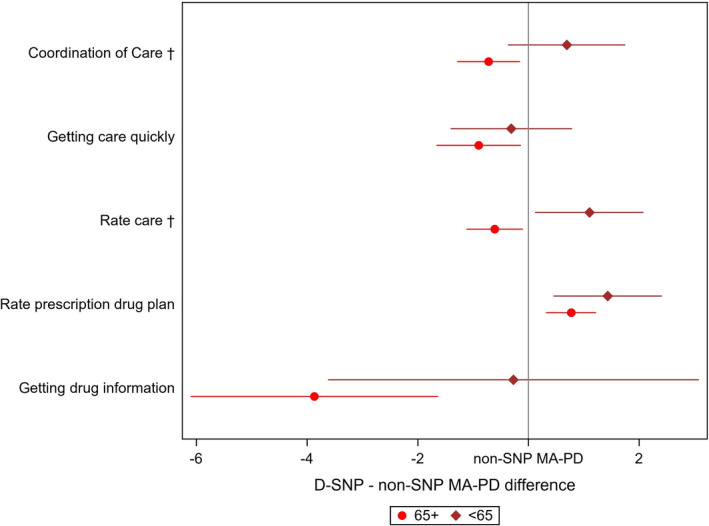
Dual Eligible Special Needs Plan (D‐SNP) Performance Relative to non‐Special Needs Plan Medicare Advantage‐Prescription Drug Plan (non‐SNP MA‐PD) for Older vs Younger Disabled Dually Eligible Beneficiaries
We did not detect different D‐SNP performance relative to other coverage types in the six states where D‐SNP regulations are intended to allow for greater coordination between Medicare and Medicaid (results available by request). However, our statistical power to detect such differences was limited, and these questions should be re‐evaluated as more data accumulates.
4. DISCUSSION
In 2018, Congress permanently re‐authorized D‐SNPs after several rounds of legislation provided greater oversight of the quality of these plans. D‐SNPs were intended to improve care for DE beneficiaries through better coordination of Medicare and Medicaid benefits. Between 2015 and 2019, DE beneficiaries in D‐SNPs have realized some but not all the benefits demonstrated by managed care in non‐SNP MA‐PD. This is notable insofar as D‐SNPs are intended to tailor their MA benefit design to the needs of DE beneficiaries, more so than non‐SNP plans which must accommodate the needs of their non‐DE enrollees as well. As the goal of D‐SNPs was to better coordinate care, it is notable that DE beneficiaries in D‐SNPs did not report better experiences with care coordination than DE beneficiaries in the other coverage types in 2015‐2019 and that in 2012‐2014 they reported worse experiences with coordination of care than DE beneficiaries in both FFS + PDP and non‐SNP MA‐PD. Thus, while D‐SNPs provide some improvements over FFS + PDP, this research suggests they may not meet their intended goal of better coordination of care and may not deliver all the MA benefits of non‐SNP MA‐PD.
Between 2015‐2019, D‐SNPs showed better performance than FFS + PDP for DE beneficiaries on four measures, most of which are areas of strength for MA: rating of care, rating of PDP, and flu and pneumonia immunizations. D‐SNPs also showed better performance than non‐SNP MA‐PD on two of these same measures—rating of PDP and flu immunization. However, D‐SNPs performed worse than non‐SNP MA‐PD on two measures, getting care quickly and getting information about prescription drugs.
Over time, Congress legislated additional requirements for D‐SNPs to support quality improvement. We saw improved D‐SNP performance relative to other coverage options on about half of the patient experience and immunization measures studied here, including coordination of care. This evidence is consistent with the effectiveness of additional requirements in bringing D‐SNP performance at least up to, or occasionally surpassing, the level of FFS + PDP. Further research is needed to determine whether this upward trend continues over time particularly with new requirements for D‐SNPs regarding additional integration (required by the Bipartisan Budget Act of 2018) beginning in 2021.
While evidence about the overall quality of care provided by D‐SNPs remains limited, 34 there is some evidence that some Fully Integrated D‐SNPs are associated with favorable outcomes such as reductions in emergency care visits and hospitalizations. These outcomes were observed in states with operational capitated Medicaid programs that coordinate Medicare and Medicaid benefits and where the same entity receives separate capitated payments by being both a Medicare D‐SNP and a Medicaid managed care organization. 12 These positive findings for D‐SNPs that are highly integrated with Medicaid are promising for Center for Medicare and Medicaid Service's current Financial Alignment Demonstration initiative to better align Medicare and Medicaid financing and to integrate primary, acute, behavioral health, and long‐term services and supports for DE beneficiaries. The evaluations of these demonstrations are underway and some evaluations of early versions of these programs, particularly the Minnesota Senior Health Options program, showed promising results. 35 We did not find evidence of better performance of D‐SNPs in states where greater integration is possible, but this may have been due to limited power.
Some authors have noted that in addition to being vulnerable, DE beneficiaries are quite diverse in their circumstances and health care needs. In particular, we find some evidence that D‐SNPs were more advantageous for DE beneficiaries under the age of 65, who are eligible for Medicare through disability, than for those 65+. Compared to non‐SNP MA‐PD coverage, we find older DE beneficiaries had worse experiences in D‐SNPs on several dimensions, including coordination of care. A “one‐size‐fits‐all” approach thus may not be successful regardless of insurance structure. Some have suggested 11 separate D‐SNP options (or non‐SNP plans) for those with full vs partial dual benefits. Our results may suggest separate plans for older vs younger disabled DE beneficiaries in order to cater to the different needs of these two subgroups.
This study has several limitations. First, since DE beneficiaries were not randomly assigned to coverage types, we cannot rule out selection bias among those enrolling in D‐SNPs despite our efforts to mitigate bias. In particular, we were unable to determine whether DE beneficiaries responding to the Medicare CAHPS survey had full or partial dual benefits and we recommend improved data collection in this regard. A similar proportion of DE beneficiaries in FFS + PDP and D‐SNP have partial dual benefits, approximately 25% (in 2016, 24.5% in FFS + PDP and 26.5% in D‐SNPs) suggesting that these comparisons are unlikely to be affected by selection bias from this source. A larger proportion of DE beneficiaries in non‐SNP MA‐PD have partial dual benefits (58.7% in 2016) and to the extent that the other observed covariates do not account for differences between those with full and partial dual benefits, these comparisons may be affected by selection bias from this source. Second, since response rates for the Medicare CAHPS survey declined over the study period, it is possible that the findings of changes in D‐SNP performance over the study period may be affected by later period response bias, although this may be less likely because the results of interest are within‐period relative differences between coverage types, rather than difference in levels of the patient experience measures over time. We cannot rule out that comparisons between coverage types may be affected by differential non‐response bias although overall response rates in FFS and MA are similar. 36 Third, the results here do not reflect the experiences of the 13% of DE beneficiaries living in nursing homes or other long‐term care facilities. Fourth, some DE beneficiaries in non‐SNP MA‐PD may be enrolled in what some have called “look‐alike plans” 37 that are structured similarly to D‐SNPs but are not designated as D‐SNPs and hence are not subject to the additional requirements of D‐SNPs. These are currently part of the non‐SNP MA‐PD set of comparison plans which may make it more difficult to detect differential performance in D‐SNPs.
In comparison to the more common choice of DE beneficiaries, FFS + PDP coverage, beneficiaries enrolled in D‐SNPs have important dimensions of better experiences: modestly higher immunization rates and slightly higher ratings of prescription drug coverage and care. However, D‐SNPs do not provide better coordination of care, as assessed by DE beneficiaries enrolled in D‐SNPs relative to other Medicare coverage options. Hence, DE beneficiaries considering enrolling in D‐SNPs or other managed care MA plans rather than FFS + PDP coverage should carefully consider their options. D‐SNPs have improved in the last four years relative to prior years and additional work is needed to assess continued change over time as well as other aspects of plan performance such as clinical quality measures, patient safety, and cost containment for this vulnerable, medically complex population. Further research is needed to better understand experiences in D‐SNPs for older vs younger disabled DE beneficiaries as well as those with partial vs full Medicaid benefits as separate D‐SNP plans for these subgroups are considered.
CONFLICTS OF INTEREST
All authors have no potential conflicts of interest.
Supporting information
Author matrix
Appendix S1
Appendix S2
Appendix S3
Appendix S4
Appendix S5
Appendix S6
Appendix S7
Figure S1
ACKNOWLEDGMENT
Joint Acknowledgment/Disclosure Statement: This research was supported by the Centers for Medicare & Medicaid Services under contract / task order number GS‐10F‐0275P / HHSM‐500‐2017‐00083G. The client had no contractual rights to review the manuscript before submission, but there is a requirement that the sponsor/supporter be given a copy of the accepted manuscript prior to publication. The authors do not have any conflicts of interest to disclose. We would like to thank Biayna Darabidian and Fergal McCarthy, M.Phil., for manuscript preparation. No other disclosures.
Haviland AM, Elliott MN, Klein DJ, Orr N, Hambarsoomian K, Zaslavsky AM. Do dual eligible beneficiaries experience better health care in special needs plans?. Health Serv Res. 2021;56:517–527. 10.1111/1475-6773.13620
Funding information
This research was supported by the Centers for Medicare & Medicaid Services under contract/task order number GS‐10F‐0275P / HHSM‐500‐2017‐00083G.
REFERENCES
- 1. Kaiser Family Foundation . Medicare Advantage. 2019. https://www.kff.org/medicare/fact‐sheet/medicare‐advantage/. Accessed July 8, 2020.
- 2. Jacobson G, Damico A, Neuman T, Gold M. Medicare Advantage 2015 Spotlight: Enrollment Market Update. Menlo Park, CA: Kaiser Family Foundation; 2015. [Google Scholar]
- 3. Kaiser Family Foundation . Medicare Advantage: Special Needs Plan (SNP) Enrollment, by SNP Type. 2018. https://www.kff.org/medicare/state‐indicator/snp‐enrollment‐by‐snp‐type/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Accessed July 1, 2020
- 4. Centers for Medicare & Medicaid Services . Details for title: SNP Comprehensive Report. 2018. https://www.cms.gov/Research‐Statistics‐Data‐and‐Systems/Statistics‐Trends‐and‐Reports/MCRAdvPartDEnrolData/Special‐Needs‐Plan‐SNP‐Data‐Items/SNP‐Comprehensive‐Report‐2018‐01.html?DLPage=2&DLEntries=10&DLSort=1&DLSortDir=descending. Accessed July 7, 2019.
- 5. Jacobson G, Gold M, Damico A, et al. Medicare Advantage 2016 Data Spotlight: Overview of Plan Changes. Menlo Park, CA: Kaiser Family Foundation; 2015. [Google Scholar]
- 6. Centers for Medicare & Medicaid Services . Fiscal Year 2015 Report to Congress. Washington, DC: Department of Health and Human Services; 2016. [Google Scholar]
- 7. Adamy J. Overlapping health plans are double trouble for taxpayers. Wall Street Journal. June 27, 2011, 2011. [Google Scholar]
- 8. Medicare Payment Advisory Commission . Report to the Congress: Medicare and the Health Care Delivery System. Washington, DC: Medicare Payment Advisory Commission; 2016. [Google Scholar]
- 9. Kaiser Commission on Medicaid Facts . Dual Eligibles: Medicaid’s Role for Low‐Income Medicare Beneficiaries. Menlo Park, CA: Kaiser Family Foundation; 2010. [Google Scholar]
- 10. Jacobson G, Neuman P, Damico A. Medicare’s Role for Dual Eligible Beneficiaries. Kaiser Family Foundation; 2012. [Google Scholar]
- 11. Medicare Payment Advisory Commission . Promoting integration in dual‐eligible special needs plans. In: Report to the Congress: Medicare and the Health Care Delivery System. Washington, DC; 2019:421‐454.
- 12. Milligan CJ, Woodcock CH. Medicare Advantage Special Needs Plans for Dual Eligibles: A Primer. New York, NY: The Commonwealth Fund; 2008. [PubMed] [Google Scholar]
- 13. Saucier P, Kasten J, Burwell B. Federal Authority for Medicaid Special Needs Plans and their Relationship to State Medicaid Programs. Washington, DC: U.S. Department of Health and Human Services; 2009. [Google Scholar]
- 14. Centers for Medicare & Medicaid Services . Special Needs Plans. 2016. https://www.cms.gov/Medicare/Health‐Plans/SpecialNeedsPlans/index.html. Accessed June 12, 2019
- 15. Gold M, Jacobson G, Damico A, Neuman P. Special Needs Plans: Availability and Enrollment. The Henry J. Kaiser Family Foundation; 2011. [Google Scholar]
- 16. Verdier J, Kruse A, Sweetland Lester R, et al. State Contracting with Medicare Advantage Dual Eligible Special Needs Plans: Issues and Options. Washington, DC: Integrated Care Resource Center; 2015. [Google Scholar]
- 17. Centers for Medicare & Medicaid Services . Chapter 16b: Special Needs Plans. Baltimore, MD: Centers for Medicare & Medicaid Services; 2014. [Google Scholar]
- 18. Larson JB. H.R.1892 ‐ Bipartisan Budget Act of 2018. In: Congress US, ed; 2017.
- 19. Allen K. SNP Provisions of the Bipartisan Budget Act of 2018. 2018. https://www.healthmanagement.com/blog/snp‐provisions‐of‐the‐bipartisan‐budget‐act‐of‐2018/. Accessed July 9, 2019.
- 20. Gold MR, Jacobson GA, Garfield RL. There is little experience and limited data to support policy making on integrated care for dual eligibles. Health Aff (Millwood). 2012;31(6):1176‐1185. [DOI] [PubMed] [Google Scholar]
- 21. Medicare Payment Advisory Commission . Medicare Advantage Special Needs Plans. Washington, DC: Medicare Payment Advisory Commission; 2013. [Google Scholar]
- 22. Anhang Price R, Elliott MN, Zaslavsky AM, et al. Examining the role of patient experience surveys in measuring health care quality. Med Care Res Rev: MCRR. 2014;71(5):522‐554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Elliott MN, Haviland AM, Dembosky JW, et al. Are there differences in the Medicare experiences of beneficiaries in Puerto Rico compared with those in the U.S. mainland? Med Care. 2012;50(3):243‐248. [DOI] [PubMed] [Google Scholar]
- 24. Centers for Medicare & Medicaid Services . Medicare Advantage and Prescription Drug Plan CAHPS® . Survey Instruments 2018. https://www.ma‐pdpcahps.org/en/survey‐instruments/. Accessed July 9, 2019.
- 25. Centers for Medicare & Medicaid Services . MA & PDP CAHPS Survey: Quality Assurance Protocols & Technical Specifications V9.0 ‐ Technical Corrections and Clarifications. 2018. https://www.ma‐pdpcahps.org/globalassets/ma‐pdp/quality‐assurance/2019‐mapdp‐qapts‐v9.0‐manual‐‐‐complete.1‐2.pdf. Accessed June 12, 2019.
- 26. Purcell NJ, Kish L. Postcensal Estimates for Local Areas (Or Domains). Int Stat Rev. 1980;48(1):3‐18. [Google Scholar]
- 27. Deming WE, Stephan FF. On a least squares adjustment of a sampled frequency table when the expected marginal totals are known. Ann Math Stat. 1940;11(4):427‐444. [Google Scholar]
- 28. Ridgeway G, McCaffrey DF, Morral AR, et al. SAS Macros Tutorial. Santa Monica, CA: RAND Corporation; 2020. [Google Scholar]
- 29. Cochran WG, Rubin DB. Controlling bias in observational studies: a review. Indian J Stat Series A. 1973;35(4):417‐446. [Google Scholar]
- 30. Lunceford JK, Davidian M. Stratification and weighting via the propensity score in estimation of causal treatment effects: a comparative study. Stat Med. 2004;23(19):2937‐2960. [DOI] [PubMed] [Google Scholar]
- 31. Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11(5):550‐560. [DOI] [PubMed] [Google Scholar]
- 32. Quigley DD, Elliott MN, Setodji CM, Hays RD. Quantifying magnitude of group‐level differences in patient experiences with health care. Health Serv Res. 2018;53(Suppl 1):3027‐3051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cohen J. Statistical Power Analysis for the Behavioral Sciences (2nd ed.). Abingdon, UK: Routledge; 1988. [Google Scholar]
- 34. Neuman P, Lyons B, Rentas J, Rowland D. Dx for a careful approach to moving dual‐eligible beneficiaries into managed care plans. Health Aff (Millwood). 2012;31(6):1186‐1194. [DOI] [PubMed] [Google Scholar]
- 35. Anderson WL, Feng Z, Long SK. Minnesota Managed Care Longitudinal Data Analysis. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, Department of Health and Human Services; 2016. [Google Scholar]
- 36. Elliott MN, Landon BE, Zaslavsky AM, et al. Medicare prescription drug plan enrollees report less positive experiences than their Medicare Advantage Counterparts. Health Aff (Millwood). 2016;35(3):456‐463. [DOI] [PubMed] [Google Scholar]
- 37. Medicare Payment Advisory Commission . Managed care plans for dual‐eligible beneficiaries. In: Report to the Congress: Medicare and the Health Care Delivery System. Washington, DC; 2018:243‐290.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author matrix
Appendix S1
Appendix S2
Appendix S3
Appendix S4
Appendix S5
Appendix S6
Appendix S7
Figure S1


