Background:
The distinction between race and ethnicity should be carefully understood and described for demographic data collection. Racial healthcare differences have been observed across many orthopaedic subspecialties. However, the frequency of reporting and analyzing race and ethnicity in orthopaedic clinical trials has not been determined. Therefore, the primary purpose of this systematic review was to determine how frequently race and ethnicity are reported and analyzed in orthopaedic clinical trials.
Methods:
The top 10 journals by impact factor in the field of orthopaedics were manually screened from 2015 to 2019. All randomized controlled trials related to orthopaedics and assessing clinical outcomes were included. Eligible studies were evaluated for bias using the Cochrane risk-of-bias tool and for whether the trial reported and analyzed several demographics, including age, sex, height, weight, race, and ethnicity. The frequency of reporting and analyzing by each demographic was accessed. In addition, comparisons of reporting and analyzing race/ethnicity were made based on orthopaedic subspecialty and journal of publication.
Results:
A total of 15,488 publications were screened and 482 met inclusion criteria. Of these 482 trials, 460 (95.4%) reported age and 456 (94.6%) reported sex, whereas 35 (7.3%) reported race and 15 (3.1%) reported ethnicity for the randomized groups; 79 studies (16.4%) analyzed age and 72 studies (14.9%) analyzed sex, whereas 6 studies (1.2%) analyzed race and 1 study (0.2%) analyzed ethnicity. The orthopaedic subspecialty of spine was found to report race (23.5%) and ethnicity (17.6%) more frequently than all the other subspecialties, whereas sports medicine reported race and/or ethnicity in only 3 of 150 trials (2.0%).
Conclusions:
Race and ethnicity are not frequently reported or analyzed in orthopaedic randomized controlled trials. Social context, personal challenges, and economic challenges should be considered while analyzing the effect of race and ethnicity on outcomes.
The distinction between race and ethnicity is complex, and a proper understanding of the differences between them is vital for demographic data collection.1 Race is a socially constructed term that associates individuals based on shared physical characteristics, whereas ethnicity is also a socially constructed term but instead categorizes people based on shared cultural identity and expression. In the United States, race categories often include American Indian or Alaska Native, Asian, Black, or African American, Native Hawaiian or Pacific Islander, and White or Caucasian, whereas ethnicity is defined as either Hispanic/Latino or not Hispanic/Latino.2 The National Institutes of Health guidelines require that minority patients be included in National Institutes of Health–funded research and that researchers collect patient-reported race and ethnicity.3 However, if previous research has shown that race and ethnicity do not affect the outcomes of an intervention, then race and ethnicity are not required as patient selection criteria, whereas their reporting and analysis are still strongly encouraged.3
Racial healthcare differences are driven heavily by the social determinants of health or factors outside of medicine that affect one's health, such as social norms, attitudes, and economic stability.4 These proximate factors may then lead to worse healthcare because of an inability to access care, a lack of health insurance, and provider biases. Racial health differences have been observed in several orthopaedic subspecialties, such as joint arthroplasty and spine surgery.5 In joint arthroplasty, Adelani et al6 controlled for comorbidities to more accurately evaluate the effects of race. They found that Black patients have an increased rate of complications and mortality after hip and knee arthroplasty, including postoperative infection, deep vein thrombosis, embolism, myocardial infarction, and stroke.6 Similar results have been observed in spine surgery, with Black patients having higher rates of mortality and complications after spine surgery than White patients.7,8 Because of these notable healthcare differences in patient populations among hospitals,9 orthopaedic research may benefit from frequent reporting of race and ethnicity demographics in publications.
According to CONSORT guidelines, randomized controlled trials (RCTs) should include all relevant demographic information in Table 1; 10however, what demographics are considered “relevant” is not clearly stated. Age and sex are almost always reported, whereas race and ethnicity are much less common. In a sample from four top medical journals, age and sex were reported in 99% of RCTs, whereas ethnicity was only reported in 37%.11 Similarly, Geller et al12 assessed the frequency of reporting race and ethnicity in prominent medical journals focusing on internal medicine, infectious disease, cardiology, oncology, and obstetrics and gynecology. They found that of 86 RCTs from 2009, 79% reported participants' race/ethnicity, whereas only 14% provided analysis by race/ethnicity.
Table 1.
Reporting Rates of Age, Sex, Height, Weight, Race, and Ethnicity Among Seven Orthopaedic Surgery Subspecialties and One Nonsurgical Category
| % of Papers Reporting Demographic | Foot/Ankle (n = 16) | Hand (n = 12) | Shoulder/Elbow (n = 12) | Spine (n = 17) | Sports (n = 150) | Total Joint (n = 137) | Trauma (n = 56) | Nonsurgical (n = 82) |
| Age | 100.0 | 100.0 | 100.0 | 100.0 | 97.3 | 95.6 | 96.4 | 86.7 |
| Sex | 93.8 | 100.0 | 100.0 | 100.0 | 96.7 | 95.6 | 92.9 | 86.7 |
| Height | 31.3 | 0.0 | 16.7 | 11.8 | 14.0 | 19.7 | 7.1 | 22.9 |
| Weight | 37.5 | 0.0 | 25.0 | 23.5 | 26.7 | 44.5 | 7.1 | 28.9 |
| Race | 0.0 | 8.3 | 8.3 | 23.5 | 2.0 | 8.8 | 8.9 | 6.0 |
| Ethnicity | 0.0 | 0.0 | 0.0 | 17.6 | 0.7 | 3.6 | 1.8 | 6.0 |
The frequency of reporting race and ethnicity in orthopaedic RCTs has not been determined. Therefore, the primary purpose of this systematic review was to determine how frequently race and ethnicity are reported and analyzed in orthopaedic clinical trials. Our secondary purpose was to determine if reporting and analysis rates of race and ethnicity differ based on orthopaedic subspecialty and journal. Finally, our tertiary purpose was to evaluate how the included studies defined and analyzed both race and ethnicity.
Methods
Search Strategy and Criteria
This systematic review was done according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.13 Only journals related to orthopaedics, sports, bones, joints, and arthroscopy were considered. The journals with the 10 highest impact factors according to the 2019 Journal Citation Reports were selected. These journals were as follows: British Journal of Sports Medicine, Bone Research, Sports Medicine, Journal of Bone and Mineral Research, American Journal of Sports Medicine, Journal of Sport and Health Science, Journal of Bone and Joint Surgery—American Volume, Clinical Orthopaedics and Related Research, Journal of Arthroscopy, and Bone & Joint Journal. The publications from 2015 to 2019 were manually screened by two independent researchers (R.W.P. and D.L.) in September 2020, and any disagreements were settled by a third investigator (K.B.F.). A broad definition of orthopaedics was used, including orthopaedic surgery and topics related to injury prevention and exercise science.
Inclusion and Exclusion Criteria
Studies were only included if a RCT study design was used, if a full-text publication was present, and if the topic was related to orthopaedics. Articles were excluded if they did not use a RCT design. Publications not related to orthopaedics were also excluded. Finally, studies that were basic science, a secondary analysis, or cluster randomized, were excluded.
Assessment of Study Quality
Each article was evaluated for potential bias by the Cochrane risk-of-bias14 tool. The Cochrane risk-of-bias tool evaluates the bias of RCTs using seven categories: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. The risk of bias in each category was classified as high, low, or unclear.
Data Collection and Abstraction
Age and sex served as frequently reported controls, whereas height and weight were used as infrequently reported controls. Full-texts were assessed to determine whether age, sex, height, weight, race, and ethnicity were reported for the study groups in each trial. Reporting a demographic variable was considered, providing a mean for continuous variables (age, height, and weight) or a sample size and/or percentage of the study population for categorical variables (sex, race, and ethnicity). Statistical analysis of demographics was also assessed as whether significant statistical analysis was done based on these variables relative to the study outcomes of interest. Comparing baseline demographics was not considered significant statistical analysis, whereas multivariate analyses or comparing subgroups divided based on one of these variables was considered significant analysis.
The following categories were used to classify subspecialty of orthopaedics: oncology, total joint and adult reconstructive surgery, spine, foot, and ankle, sports medicine, trauma, hand, and shoulder and elbow, and nonsurgical. The following race categories were used to guide our analysis: American Indian or Alaska Native, Asian, Black, or African American, Native Hawaiian or Pacific Islander, and White or Caucasian.2 Similarly, Hispanic and Latino were the considered ethnic categories of our review.2
The outcomes of interest were the frequency of reporting and analyzing race and ethnicity compared with other demographic variables (age, sex, height, and weight). Subspecialty category, whether the study reported and analyzed each demographic (0 = no and 1 = yes), and Cochrane Risk-of-Bias scores (0 = low, 1 = unclear, and 2 = high) were collected in Microsoft Excel. Assessments were completed among all orthopaedic RCTs and based on orthopaedic subspecialty.
Results
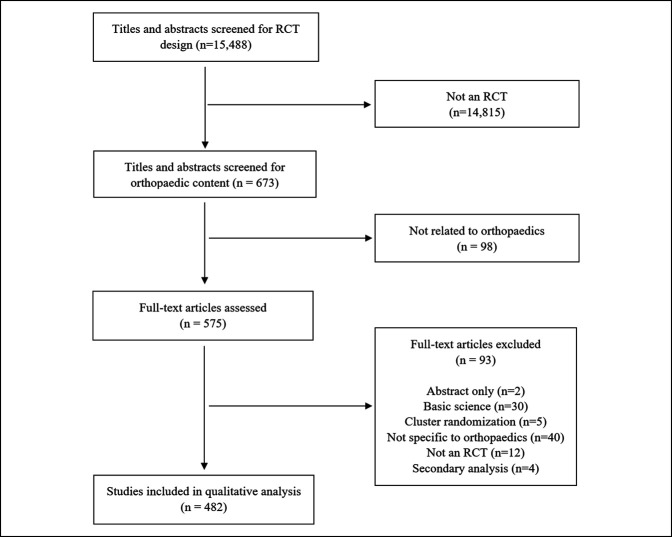
Details of paper inclusion/exclusion are presented in Figure 1. A total of 15,488 studies across 10 journals were screened for RCT design; 673 papers were then screened for relevance to orthopaedics. In total, 575 publications were fully assessed, and after excluding 93 studies for various reasons (Figure 1), 482 studies were included in the final qualitative analysis.
Figure 1.
Flow chart showing the Preferred Reporting Items for Systematic Reviews and Meta-Analyses of study inclusion and exclusion, with 482 randomized controlled trials (RCTs) included in the qualitative analysis.
Rates of Reporting Demographics
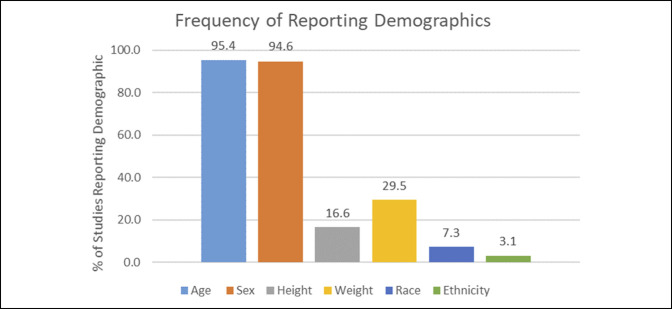
Of the 482 studies, 460 (95.4%) reported age and 456 (94.6%) reported sex for the randomized groups. Eighty (16.6%) reported height, and 142 (29.5%) reported weight for the randomized groups. Furthermore, 35 (7.3%) reported race, and 15 (3.1%) reported ethnicity for the randomized groups (Figure 2).
Figure 2.
Bar diagram showing the percentage of orthopaedic randomized controlled trials that reported age, sex, height, weight, race, and ethnicity.
Rates of Analyzing Demographics
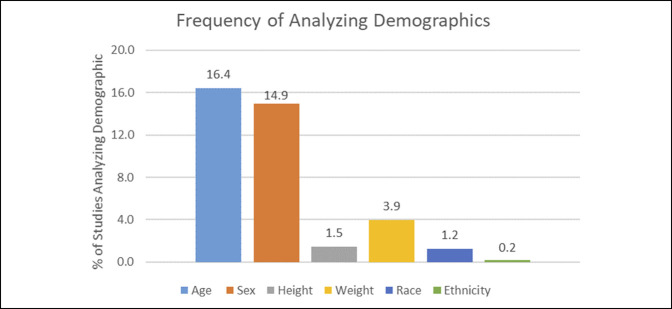
Of 482 studies, 79 studies (16.4%) analyzed age and 72 studies (14.9%) analyzed sex (Figure 3). Seven studies (1.5%) analyzed height, and 19 studies (3.9%) analyzed weight. Furthermore, six studies (1.2%) analyzed race, and only one study (0.2%) analyzed ethnicity (Figure 3).
Figure 3.
Bar diagram showing the percentage of orthopaedic randomized controlled trials that analyzed age, sex, height, weight, race, and ethnicity.
Included Studies that Reported and Analyzed Race and Ethnicity
Of the 35 RCTs that reported race, five studies15,16,17,18,19 only included one race (Table A1, http://links.lww.com/JG9/A133). The percentage of the participants that were White/Caucasian ranged from 29.9%20 to 98.3%,21 Black/African American ranged from 2.2%22 to 68.7%,20 Asian ranged from 0.8%23 to 60%,24 and Hispanic ranged from 0.9%25 to 39.6%26 (Table A1, http://links.lww.com/JG9/A133). In total, 20,686 patients in the 30 RCTs reported a study population of mixed race/ethnicity. Of these 20,686 patients, 130 (0.6%) were Asian, 1692 (8.2%) were Black/African American, 3590 (17.4%) were Hispanic, and 8933 (43.2%) were White/Caucasian.
Orthopaedic Subspecialties
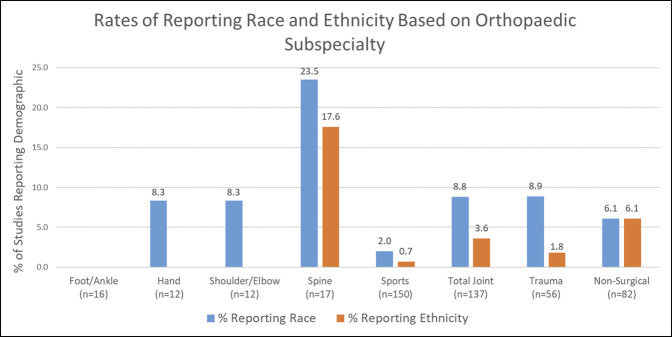
Sixteen publications were categorized as foot/ankle, 12 hand, 12 shoulder and elbow, 17 spine, 150 sports medicine, 137 total joint reconstruction and replacement, 56 trauma, and 82 nonsurgical. Spine reported both race (23.5%) and ethnicity (17.6%) more frequently than all other subspecialties (Table 1; Figure 4). Sports medicine, total joint reconstruction and replacement, and trauma reported race in 2.0%, 8.8%, and 8.9% of RCTs, respectively (Table 1; Figure 4). In addition, these subspecialties only reported ethnicity in 0.7%, 3.6%, and 1.8% of trials (Table 1; Figure 4). As for analysis, no spine and sports medicine RCTs analyzed race or ethnicity (Table 2). One total joint reconstruction and replacement RCT and two trauma RCTs analyzed race (Table 2). Finally, four nonsurgical RCTs analyzed race and one nonsurgical study analyzed ethnicity (Table 2).
Figure 4.
Bar diagram showing the rates of reporting race (blue) and ethnicity (orange) among seven orthopaedic surgery subspecialties and one nonsurgical category.
Table 2.
Analysis Rates of Age, Sex, Height, Weight, Race, and Ethnicity Among Seven Orthopaedic Surgery Subspecialties and One Nonsurgical Category
| % of Papers Analyzing Demographic | Foot/Ankle (n = 16) | Hand (n = 12) | Shoulder/Elbow (n = 12) | Spine (n = 17) | Sports (n = 150) | Total Joint (n = 137) | Trauma (n = 56) | Nonsurgical (n = 82) |
| Age | 6.3 | 25.0 | 16.7 | 17.6 | 12.0 | 15.3 | 30.4 | 16.9 |
| Sex | 6.3 | 25.0 | 8.3 | 23.5 | 11.3 | 11.7 | 17.9 | 24.1 |
| Height | 0.0 | 0.0 | 0.0 | 0.0 | 1.3 | 0.7 | 1.8 | 3.6 |
| Weight | 0.0 | 0.0 | 0.0 | 11.8 | 1.3 | 4.4 | 1.8 | 9.6 |
| Race | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.7 | 1.8 | 4.9 |
| Ethnicity | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 1.2 |
Orthopaedic Journals
All journals reported age and sex more frequently than height, weight, race, and ethnicity (Table 3). Of all the journals, Sport and Health reported height and weight the most frequently (both 50.0%), whereas Journal of Bone and Mineral Research reported height least frequently (8.3%) and American Journal of Sports Medicine reported weight least frequently (23.6%). Journal of Bone and Mineral Research reported race and ethnicity most frequently (both 16.7%) (Table 3). Arthroscopy and British Journal of Sports Medicine did not report either race or ethnicity in any RCTs (Table 3). Analysis rates of these six demographics based on journal are also available in Table A2 (http://links.lww.com/JG9/A134).
Table 3.
Reporting Rates of Demographics Based on Orthopaedic Journal
| Journal | Reporting Age (%) | Reporting Sex (%) | Reporting Height (%) | Reporting Weight (%) | Reporting Race (%) | Reporting Ethnicity (%) |
| American Journal of Sports Medicine (n = 106) | 98.1 | 99.1 | 13.2 | 23.6 | 6.6 | 2.8 |
| Arthroscopy (n = 60) | 93.3 | 91.7 | 13.3 | 25.0 | 0.0 | 0.0 |
| Bone & Joint Journal(n = 94) | 94.7 | 92.6 | 14.9 | 31.9 | 4.3 | 0.0 |
| British Journal of Sports Medicine (n = 29) | 96.6 | 96.6 | 37.9 | 37.9 | 0.0 | 0.0 |
| Bone Research (n = 2) | 100.0 | 100.0 | 50.0 | 0.0 | 0.0 | 0.0 |
| Clinical Orthopaedics and Related Research (n = 51) | 98.0 | 98.0 | 19.6 | 31.4 | 11.8 | 3.9 |
| Journal of Bone and Joint Surgery—American Volume (n = 112) | 94.6 | 94.6 | 11.6 | 29.5 | 11.6 | 7.1 |
| Journal of Bone and Mineral Research (n = 12) | 100.0 | 100.0 | 8.3 | 25.0 | 16.7 | 16.7 |
| Sport and Health (n = 12) | 75.0 | 58.3 | 50.0 | 50.0 | 25.0 | 0.0 |
| Sports Medicine (n = 4) | 100.0 | 100.0 | 50.0 | 75.0 | 0.0 | 0.0 |
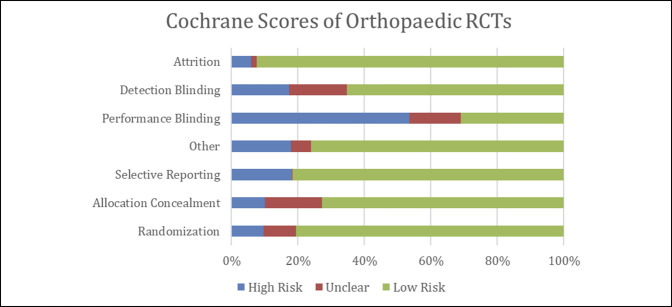
Cochrane Risk-of-Bias
The least amount of bias was present in the attrition category of the Cochrane risk-of-bias tool, with 92% of RCTs describing exclusion criteria and their participant dropout rates (Figure 5). The highest amount of bias was in the performance blinding category, with 53% of RCTs not blinding patients and intervention providers (Figure 5).
Figure 5.
Diagram showing the Cochrane Risk-of-Bias scores of all included randomized controlled trials (RCTs). Green = low risk of bias, red = unclear, blue = high risk of bias.
Discussion
The primary purpose of our study was to evaluate the frequency of both reporting and analyzing race and ethnicity in orthopaedic RCTs. Race and ethnicity were rarely reported in orthopaedic RCTs, with only 7.3% of publications documenting race and 3.1% of publications documenting ethnicity. Race and ethnicity were also rarely analyzed, with only 1.2% of papers analyzing race and 0.2% of papers analyzing ethnicity. By evaluating orthopaedic subspecialties, we also found that the orthopaedic subspecialty of spine reported race and ethnicity more frequently than all the other subspecialties, whereas sports medicine reported race and ethnicity in only 3 of 150 RCTs and foot/ankle did not report either race or ethnicity in any of the included studies. Finally, by evaluating the reported demographics of included studies, we found that the racial and ethnic demographics of included patients ranged tremendously, and only two of six studies that analyzed race/ethnicity found differences based on race/ethnicity.
Of the six studies20,27,28,29,30,31 that analyzed race/ethnicity, two30,31 showed differences based on race/ethnicity. Warwick et al30 found through a logistic regression multivariable analysis that White patients were slightly more likely to respond to patient-reported outcome surveys compared with Black patients (odds ratio of 2.03) after orthopaedic surgery. Johnson et al31 calculated hazard ratios that found that African-American patients with type 2 diabetes mellitus may be at an increased long-term risk of fracture because of an intentional weight loss intervention (hazard ratio of 1.64), whereas White and Hispanic patients with type 2 diabetes mellitus are not (hazard ratios of 0.97 and 0.87, respectively). Interestingly, it should be noted that even with an intentional weight loss intervention, African-American patients still had a lower incidence of fractures (9.75%) than White patients (15.92%) and Hispanic patients (10.88%).31 However, racial and ethnic differences should not automatically be considered disparities.32 According to Rathore and Krumholz,32 a racial difference should only be considered a racial disparity if the difference cannot be explained by other patient factors. If a racial difference is shown not to be due to eligibility, clinical exclusion (contraindications), patient preferences, or confounding variables (demographic, clinical, and social) and the racial difference is associated with poorer patient outcomes, then the difference should be deemed a disparity.32
It is important to report and identify racial and ethnic differences throughout orthopaedics so that further examination can identify its root cause. For example, racial and ethnic differences have been clearly documented in total joint arthroplasty.33,34 Minority patients have been shown to have worse postoperative function and outcomes,35 and increased mortality rates.36 Despite these differences and their persistence throughout the years,36 RCTs have failed to frequently report these demographics, with RCTs in the total joint arthroplasty subspecialty reporting race and ethnicity in 8.8% and 3.6% of publications, respectively. Several proximal factors may contribute to these low rates, such as a lack of race/ethnicity data collection, a belief that reporting race/ethnicity is not clinically relevant, or a lack of emphasis to report race/ethnicity by medical journals. Educating researchers about the value of reporting and analyzing race and ethnicity, regardless of whether their studies identify or deny racial differences, may help improve reporting and analysis rates. In addition, medical journals may emphasize the reporting and analysis of race and ethnicity for prospective publications.
The complexity of interpreting findings regarding racial/ethnic differences may also lead to decreased reporting and analysis rates. It has been debated whether race and ethnicity are meaningful demographics in medical research.37-39 Race and ethnicity capture a lifetime of social experiences that may never be adequately controlled for40,41; thus, the effect of biological versus social factors cannot competently be discerned. According to a viewpoint by Cooper et al,37 medicine faces the challenge of needing to collect patient subgroup data to recognize and reduce inequities, while avoiding the misinterpretation and exaggeration of the effect race has on health. To combat this, clinicians and researchers should improve their understandings of social context and personal/economic challenges and should consider how social forces may have affected their data.37 Ultimately, research literature should become more effective at identifying differences and disparities, and clinicians may more effectively counsel patients before and after treatment.
This study is not without limitations. First, only RCTs related to orthopaedics were included. Studies regarding racial and ethnic differences are often cohort studies with a large sample size, but we did not include cohort studies. Second, no comparisons were made with fields outside of orthopaedics. It would be beneficial for future research to compare orthopaedics with other fields of medicine regarding rates of reporting and analyzing race/ethnicity and relate these findings to relevant social forces. Third, we did not evaluate other socioeconomic factors. Without evaluating additional social factors, an adequate evaluation of whether race/ethnicity should be reported and analyzed more frequently is not possible. Fourth, several subspecialties of orthopaedics were not included adequately. Foot and ankle, hand, shoulder and elbow, and spine surgery all had less than 18 RCTs included in this systematic review. Finally, this review did not isolate topics with notable health differences. It is possible that the included studies evaluated interventions where racial/ethnic differences are nonexistent or minimal, so reporting and analyzing race and/or ethnicity is not necessary.
In conclusion, race and ethnicity are not frequently reported or analyzed in orthopaedic RCTs. Orthopaedic spine surgery reported and analyzed race the most frequently of orthopaedic subspecialties, whereas all other orthopaedic subspecialties rarely reported race and ethnicity. Racial and ethnic demographics varied markedly among the RCTs that reported patient race and ethnicity. Social context, personal challenges, and economic challenges should be carefully considered while analyzing the effect of race and ethnicity on outcomes.
Footnotes
Dr. Tjoumakaris or an immediate family member serves as a board or committee member of American Academy of Orthopaedic Surgeons, American Board of Orthopaedic Surgery, and American Orthopaedic Society for Sports Medicine and has stock or stock options held in Franklin/Keystone Biosciences, LLC and Trice Medical. Dr. Ciccotti or an immediate family member serves as a board or committee member of American Orthopaedic Society for Sports Medicine and Orthopaedic Learning Center. Dr. Freedman or an immediate family member serves as a board or committee member of American Orthopaedic Society for Sports Medicine; serves as a paid consultant to DePuy, A Johnson & Johnson Company, and Vericel. None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Mr. Paul, Mr. Lee, and Mr. Brutico.
Contributor Information
Ryan W. Paul, Email: Ryan.Paul@rothmanortho.com.
Donghoon Lee, Email: Donghoon.Lee@rothmanortho.com.
Joseph Brutico, Email: Joseph.Brutico@rothmanortho.com.
Fotios P. Tjoumakaris, Email: Fotios.Tjoumakaris@rothmanortho.com.
Michael G. Ciccotti, Email: Michael.Ciccotti@rothmanortho.com.
References
- 1.Standards for maintaining, collecting, and presenting federal data on race and ethnicity. Fed Regist 2016. https://www.federalregister.gov/documents/2016/09/30/2016-23672/standards-for-maintaining-collecting-and-presenting-federal-data-on-race-and-ethnicity. Accessed November 9, 2020. [Google Scholar]
- 2.Revisions to the Standards for the Classification of Federal Data on Race and Ethnicity. White House. https://obamawhitehouse.archives.gov/node/15626. Accessed November 9, 2020. [Google Scholar]
- 3.NIH Policy and Guidelines on The Inclusion of Women and Minorities as Subjects in Clinical Research | grants.nih.gov. https://grants-nih-gov.libproxy.temple.edu/policy/inclusion/women-and-minorities/guidelines.htm. Accessed November 9, 2020. [Google Scholar]
- 4.Catalyst N: Social determinants of health (SDOH). NEJM Catal 2017. https://catalyst-nejm-org.proxy1.lib.tju.edu/doi/full/10.1056/CAT.17.0312. Accessed March 8, 2021. [Google Scholar]
- 5.Schoenfeld AJ, Tipirneni R, Nelson JH, Carpenter JE, Iwashyna TJ: The influence of race and ethnicity on complications and mortality after orthopedic surgery: A systematic review of the literature. Med Care 2014;52:842-851. [DOI] [PubMed] [Google Scholar]
- 6.Adelani MA, Archer KR, Song Y, Holt GE: Immediate complications following hip and knee arthroplasty: Does race matter? J Arthroplasty 2013;28:732-735. [DOI] [PubMed] [Google Scholar]
- 7.Alosh H, Riley LH, Skolasky RL: Insurance status, geography, race, and ethnicity as predictors of anterior cervical spine surgery rates and in-hospital mortality: An examination of United States trends from 1992 to 2005. Spine 2009;34:1956-1962. [DOI] [PubMed] [Google Scholar]
- 8.Sanford Z, Taylor H, Fiorentino A, et al. : Racial disparities in surgical outcomes after spine surgery: An ACS-NSQIP analysis. Glob Spine J 2019;9:583-590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beletsky A, Lu Y, Patel BH, et al. : Should we question the external validity of database studies? A comparative analysis of demographics. Arthroscopy 2019;35:2686-2694. [DOI] [PubMed] [Google Scholar]
- 10.Consort—Welcome to the CONSORT Website. http://www.consort-statement.org/. Accessed November 9, 2020.
- 11.Furler J, Magin P, Pirotta M, van Driel M: Participant demographics reported in “Table 1” of randomised controlled trials: A case of “inverse evidence”? Int J Equity Health 2012;11:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geller SE, Koch A, Pellettieri B, Carnes M: Inclusion, analysis, and reporting of sex and race/ethnicity in clinical trials: Have we made progress? J Womens Health 2011;20:315-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moher D, Shamseer L, Clarke M, et al. ; PRISMA-P Group: Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Higgins JPT, Altman DG, Gøtzsche PC, et al. : The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abula K, Gröpel P, Chen K, Beckmann J: Does knowledge of physical activity recommendations increase physical activity among Chinese college students? Empirical investigations based on the transtheoretical model. J Sport Health Sci 2018;7:77-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koh IJ, Kim MS, Sohn S, Song KY, Choi NY, In Y: Duloxetine reduces pain and improves quality of recovery following total knee arthroplasty in centrally sensitized patients: A prospective, randomized controlled study. J Bone Joint Surg Am 2019;101:64-73. [DOI] [PubMed] [Google Scholar]
- 17.van Tilburg CWJ, Stronks DL, Groeneweg JG, Huygen FJPM: Randomised sham-controlled double-blind multicentre clinical trial to ascertain the effect of percutaneous radiofrequency treatment for lumbar facet joint pain. Bone Joint J 2016;98-B:1526-1533. [DOI] [PubMed] [Google Scholar]
- 18.Zhu Q, Huang L, Wu X, et al. : Effects of tai Ji Quan training on gait kinematics in older Chinese women with knee osteoarthritis: A randomized controlled trial. J Sport Health Sci 2016;5:297-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vina ER, Richardson D, Medvedeva E, Kent Kwoh C, Collier A, Ibrahim SA: Does a patient-centered educational intervention affect African-American access to knee replacement? A randomized trial. Clin Orthop Relat Res 2016;474:1755-1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Egekeze N, Dubin J, Williams K, Bernhardt M: The age of OrthoInfo: A randomized controlled trial evaluating patient comprehension of informed consent. J Bone Joint Surg Am 2016;98:e81. [DOI] [PubMed] [Google Scholar]
- 21.van der Meijden OA, Houwert RM, Hulsmans M, et al. : Operative treatment of dislocated midshaft clavicular fractures: Plate or intramedullary nail fixation? A randomized controlled trial. J Bone Joint Surg Am 2015;97:613-619. [DOI] [PubMed] [Google Scholar]
- 22.Kon E, Engebretsen L, Verdonk P, Nehrer S, Filardo G: Clinical outcomes of knee osteoarthritis treated with an autologous protein solution injection: A 1-year pilot double-blinded randomized controlled trial. Am J Sports Med 2018;46:171-180. [DOI] [PubMed] [Google Scholar]
- 23.Westenberg RF, Zale EL, Heinhuis TJ, et al. : Does a brief mindfulness exercise improve outcomes in upper extremity patients? A randomized controlled trial. Clin Orthop Relat Res 2018;476:790-798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Greiner S, Ide J, Van Noort A, et al. : Local rhBMP-12 on an absorbable collagen sponge as an adjuvant therapy for rotator cuff repair—A phase 1, randomized, standard of care control, multicenter study: Safety and feasibility. Am J Sports Med 2015;43:1994-2004. [DOI] [PubMed] [Google Scholar]
- 25.Goytizolo EA, Lin Y, Kim DH, et al. : Addition of adductor canal block to periarticular injection for total knee replacement: A randomized trial. J Bone Joint Surg Am 2019;101:812-820. [DOI] [PubMed] [Google Scholar]
- 26.Lewiecki EM, Dinavahi RV, Lazaretti-Castro M, et al. : One year of romosozumab followed by two years of denosumab maintains fracture risk reductions: Results of the FRAME extension study. J Bone Miner Res 2019;34:419-428. [DOI] [PubMed] [Google Scholar]
- 27.Simpson AHRW, Keenan G, Nayagam S, Atkins RM, Marsh D, Clement ND: Low-intensity pulsed ultrasound does not influence bone healing by distraction osteogenesis: A multicentre double-blind randomised control trial. Bone Joint J 2017;99-B:494-502. [DOI] [PubMed] [Google Scholar]
- 28.Aung KK, Wu WK, Tokumi A, Kuo P, Day CS: Does a directive to an internet site enhance the doctor-patient interaction? A prospective randomized study for patients with carpal tunnel syndrome. J Bone Joint Surg Am 2015;97:1112-1118. [DOI] [PubMed] [Google Scholar]
- 29.Jules-Elysee KM, Goon AK, Westrich GH, et al. : Patient-controlled epidural analgesia or multimodal pain regimen with periarticular injection after total hip arthroplasty: A randomized, double-blind, placebo-controlled study. J Bone Joint Surg Am 2015;97:789-798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Warwick H, Hutyra C, Politzer C, et al. : Small social incentives did not improve the survey response rate of patients who underwent orthopaedic surgery: A randomized trial. Clin Orthop Relat Res 2019;477:1648-1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson KC, Bray GA, Cheskin LJ, et al. : The effect of intentional weight loss on fracture risk in persons with diabetes: Results from the look AHEAD randomized clinical trial. J Bone Miner Res 2017;32:2278-2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rathore SS, Krumholz HM: Differences, disparities, and biases: Clarifying racial variations in health care use. Ann Intern Med 2004;141:635-638. [DOI] [PubMed] [Google Scholar]
- 33.Shahid H, Singh JA: Racial/ethnic disparity in rates and outcomes of total joint arthroplasty. Curr Rheumatol Rep 2016;18:20. [DOI] [PubMed] [Google Scholar]
- 34.Pierce TP, Elmallah RK, Lavernia CJ, et al. : Racial disparities in lower extremity arthroplasty outcomes and use. Orthopedics 2015;38:e1139-e1146. [DOI] [PubMed] [Google Scholar]
- 35.Mehta BY, Bass AR, Goto R, et al. : Disparities in outcomes for blacks versus whites undergoing total hip arthroplasty: A systematic literature review. J Rheumatol 2018;45:717-722. [DOI] [PubMed] [Google Scholar]
- 36.Singh JA, Lu X, Rosenthal GE, Ibrahim S, Cram P: Racial disparities in knee and hip total joint arthroplasty: An 18-year analysis of national Medicare data. Ann Rheum Dis 2014;73:2107-2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cooper RS, Nadkarni GN, Ogedegbe G: Race, ancestry, and reporting in medical journals. JAMA 2018;320:1531-1532. [DOI] [PubMed] [Google Scholar]
- 38.Peck BM, Denney M: Disparities in the conduct of the medical encounter: The effects of physician and patient race and gender. SAGE Open 2012;2:2158244012459193. [Google Scholar]
- 39.Burchard EG, Ziv E, Coyle N, et al. : The importance of race and ethnic background in biomedical research and clinical practice. N Engl J Med 2003;348:1170-1175. [DOI] [PubMed] [Google Scholar]
- 40.Caulfield T, Fullerton SM, Ali-Khan SE, et al. : Race and ancestry in biomedical research: Exploring the challenges. Genome Med 2009;1:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kaufman JS, Cooper RS: Race in epidemiology: New tools, old problems. Ann Epidemiol 2008;18:119-123. [DOI] [PubMed] [Google Scholar]