Supplemental Digital Content is available in the text.
Introduction:
Inpatient rounding serves numerous roles. The American Academy of Pediatrics recommends a family-centered bedside model. Residents identified physical examination teaching during and satisfaction with rounds as areas for improvement. A resident group developed a project utilizing quality improvement (QI) methodology to address these concerns. We aimed to increase the frequency of bedside physical examination teaching most or every day on a single inpatient unit by 20% over 1 year, with secondary goals to increase the percentage of interns spending one hour or more at bedside per day by 10% and intern satisfaction by 15%, without impacting rounding duration.
Methods:
We developed an organizational structure to complete a long-term resident-led project. Interventions included daily bedside examination teaching on rounds, afternoon examinations, goal communication, topic recording, and a teaching “tip sheet.” Using an institutional QI framework, we utilized iterative plan-do-study-act cycles to implement interventions and surveys to assess outcomes, with rounding efficiency as a balancing measure.
Results:
The survey response rate was 57%. Bedside teaching frequency increased from a mean of 10% to 61%, perceived time at the bedside increased from 37% to 59%, and rounding satisfaction improved from a rating of 6.7/10 to 7.4/10. Efficiency was not impacted.
Conclusions:
We improved inpatient rounds bedside physical examination teaching and satisfaction without sacrificing efficiency. This project demonstrates the feasibility and success of a resident-driven education initiative to successfully motivate fellow residents and colleagues across disciplines to enact change. The organizational structure may serve as a model for resident-led QI projects across institutions.
INTRODUCTION
Problem Description
Inpatient rounding serves numerous roles, including determining the medical plan and creating a shared mental model amongst the multidisciplinary team, patient, family, and trainee education. The American Academy of Pediatrics recommends a family-centered approach, recognizing that patients’ and families’ perspectives are integral to clinical decision-making and optimal medical care.1 Although there is no standard for conducting family-centered rounds (FCRs), they generally occur either inside or outside the patient room with the medical team and the patient and/or their caregivers.
The education of trainees has historically been a critical component of inpatient rounds. Rounds conducted at the bedside offer an additional opportunity for physical examination teaching; however, this does not always occur.2,3 At our institution, residents expressed dissatisfaction with the current rounding model, specifically regarding the frequency of bedside physical examination teaching.
The majority of studies exploring patient, caregiver, and nursing attitudes toward FCR have been observational. Perceptions are overall favorable; families express that hearing the discussion of the medical plan is beneficial.4–6 FCRs are associated with increased nursing involvement7 and a sense of teamwork among the interdisciplinary team.8
Several studies have evaluated the educational experience of FCR, but few have attempted to intervene to improve rounds. In a study of pediatric residents at multiple institutions, the majority of residents agreed that the quality of nonlecture-based teaching improved with FCR.9 Similarly, 2 studies found that residents thought FCR improved their education through increased patient exposure, physical examination findings, and modeling of communication skills.10,11 The only intervention-level study evaluated using a web-based physical examination teaching toolkit, including visual aids, audio, and video clips of normal and abnormal physical examination findings. This tool increased self-reported physical examination teaching at the bedside.12
We sought to determine the impact of multiple rounding interventions to increase bedside physical examination teaching, time at the bedside, and rounding satisfaction.
At our institution, a survey distributed to the postgraduate year (PGY) 1 class in 2016 demonstrated that only 8% of the first-year residents (38 responses with 73% response rate) were satisfied with the current rounding paradigm. Lack of physical examination teaching on rounds was noted as a key driver of dissatisfaction felt to be modifiable by the study team.
Therefore, we posited that increasing bedside physical examination teaching on rounds could improve resident satisfaction with FCRs.
Specific Aims
The project aimed to increase the percentage of interns reporting bedside physical examination teaching with the team most or every day on a single inpatient unit over one year by 20%, with secondary goals of increasing the percentage of interns reporting spending 1 hour or more at bedside per day by 10%, and intern satisfaction with the current rounding model by 15%, without impacting our balancing measure of rounding duration.
METHODS
Context
This study was conducted from January 2018 through June 2019 at a large, urban, quaternary care children’s hospital on a single 23-bed inpatient unit. We chose this unit based on a strong QI culture, a large volume of general pediatric patients, and consistent nursing staff.
This unit’s team structure includes 1 attending, 2 daytime senior residents (PGY2-4), 4–6 interns (PGY1), 0-1 subinterns, and 2 clerkship students. The interdisciplinary team also includes nurses, dieticians, and pharmacists. Social workers and case managers meet with the team after rounds. A care team assistant (CTA) is present to notify nurses of rounds for their patients and assist with nonclinical tasks.
We invite families to join rounds, provide input, and discuss the care plan. An intern or medical student presents the patient’s interval history, relevant examination findings, laboratories and imaging, and the day’s plan. The senior resident and attending then provide feedback and teaching for each patient. Before our intervention, entering the room to see the patient at the bedside and perform a physical examination during rounds was at the team’s discretion and occurred infrequently.
Intervention
A group of 10 residents led the formation of a multidisciplinary team consisting of nurses, patient-family liaisons, faculty, and administrators.
Although most prior studies evaluating the quality and frequency of bedside examinations have been driven by attending physicians, this project was resident-driven, which required additional attention to long-term sustainability. We identified the challenge of creating and sustaining change, given the transient nature of the residency and frequently changing schedules. We created a novel organizational structure to enable resident leadership of a robust, longitudinal QI initiative (Fig. 1). The project spanned from the end of the team’s PGY1–PGY3 years.
Fig. 1.
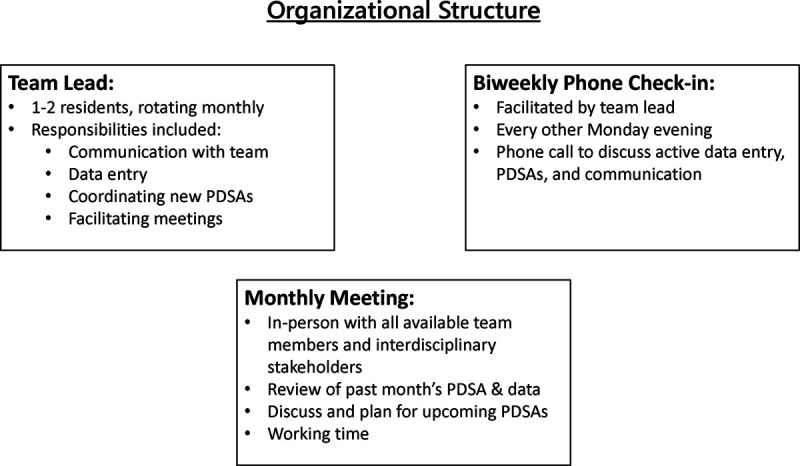
Depiction of the organizational structure of the resident leadership team and workflow. Note: not all team members are depicted here.
We utilized an institutional QI framework adapted from the Six Sigma, Lean, and Model for Improvement frameworks, which uses iterative plan-do-study-act (PDSA) cycles to implement changes and assess outcomes simultaneously. We surveyed interns weekly regarding their rounding satisfaction and teaching practices. We recorded the total duration of rounds and the number of patients on rounds (Figure 1, Supplemental Digital Content 1, http://links.lww.com/PQ9/A254). We collected baseline data over 4 months, starting in January 2018. We introduced interventions through December 2018, and we present the results sustained for 6 months after the last intervention.
Key drivers were identified through group discussion among the project leaders and key stakeholders, including attending physicians, bedside nurses, and nursing leadership and family liaisons (Fig. 2). The majority of interventions were education-focused: asking the senior resident or attending to institute daily, team-wide bedside physical examinations on 1 patient per day during rounds (our primary intervention); transitioning the examination to the afternoon; weekly communication of project goals and current intervention to the team; senior resident recording of daily physical examination teaching topics/goals, and providing a bedside physical examination teaching “tip sheet.” One intervention (incentivizing survey completion) targeted data collection (Figs. 3–6). We communicated interventions through weekly reminder emails and personal conversations with the senior residents and attendings on service. Decisions to adopt or discontinue PDSA interventions were made based on feedback from the floor residents and attendings, reviewing the data, and discussion among the study team. The CTA was a consistent presence on the unit and provided reminders as well. We encouraged a prerounds huddle between the senior resident and attending physician to discuss an appropriate patient for bedside physical examination.
Fig. 2.
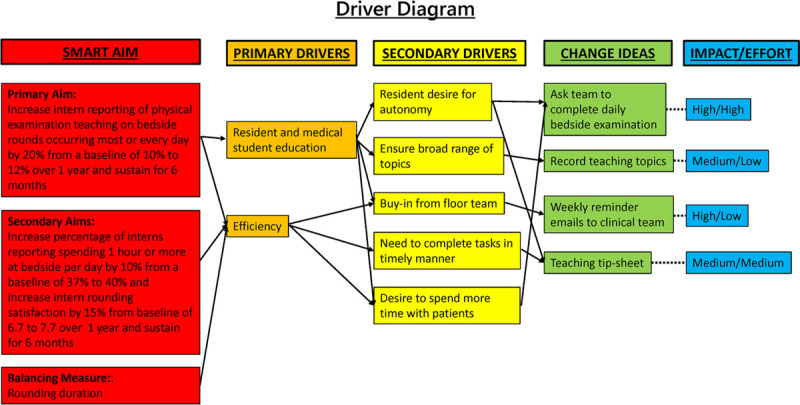
Driver diagram. Key driver diagram used to identify interventions. Key drivers were identified through discussion with key stakeholders, including residents (members of the project leadership team and others), attending physicians, bedside nurses, nursing leadership, and family liaisons.
Fig. 3.
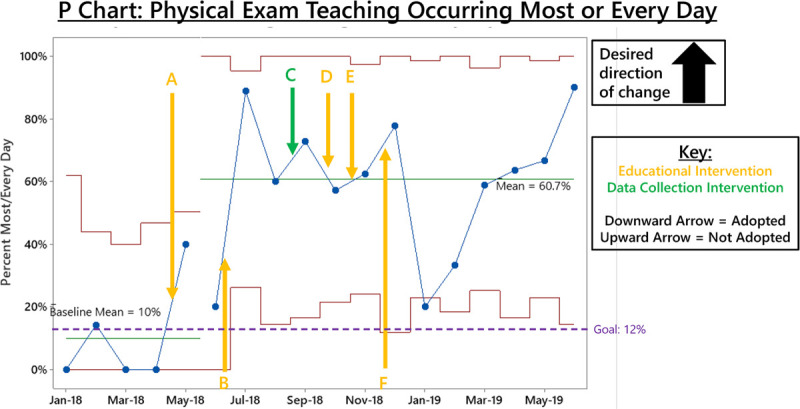
P-Chart of bedside physical examination teaching occurring most or every day interventions. A, Daily bedside physical examination during rounds. B, Afternoon examination with attending (not adopted). C, Coffee cards to incentivize survey completion. D, Regular email communication of expectations. E, Documentation of teaching goal. F, Bedside teaching tip sheet (not adopted).
Fig. 6.
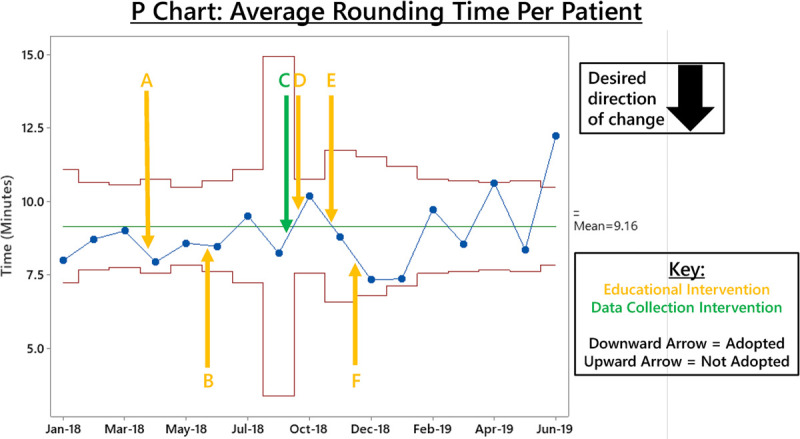
P-chart of average duration of rounds per patient interventions. A, Daily bedside physical examination during rounds. B, Afternoon examination with attending (not adopted). C, Coffee cards to incentivize survey completion. D, Regular email communication of expectations. E, Documentation of teaching goal. F, Bedside teaching tip sheet (not adopted).
Study of the Intervention
To gauge the response to the PDSA cycles, we surveyed interns and senior residents on the unit weekly with surveys distributed by the CTA or a member of the project team. We incentivized survey completion with gift cards to the hospital coffee shop beginning in July 2018 to improve response rates. We entered the survey results into a Research Electronic Data Capture (REDCap) database every 2 weeks and reviewed them monthly.13,14
CTAs recorded the duration of rounds, and the number of patients rounded on; we calculated an average duration of rounding time per patient.
The group met monthly to discuss implementation. A team member visited the unit 1–2 times per week to discuss ongoing PDSA cycles and elicit feedback from the resident and nursing teams. Interventions were adopted or not adopted based on qualitative feedback from residents, attendings, and nursing and quantitative evaluation of survey data.
Measures
Survey measures targeted 3 related outcomes: bedside teaching, rounding efficiency, and resident satisfaction. Administering weekly surveys allowed for frequent assessments of PDSA cycles. The project team developed the surveys, which were reviewed and revised with faculty mentors’ assistance and approved by the residency program leadership before distribution (Figure 1, Supplemental Digital Content 1, http://links.lww.com/PQ9/A254).
Our survey measured the quantity and quality of the educational experience on rounds and self-reported measures of satisfaction.
Measuring rounding efficiency was critical to assess our interventions because it enabled effective bedside rounding and was an essential balancing metric. Data from daily rounds included average time spent per patient and the total length of rounds. Rounds were timed daily by the CTA.
Analysis
We managed study data using REDCap (a secure, web-based software platform designed to support data capture for research studies) tools hosted at The Children’s Hospital of Philadelphia (CHOP). We analyzed data using IBM SPSS Statistics, Version 24.0. (IBM Corp, Armonk, N.Y.). We used control charts to assess improvement in the frequency of bedside physical examination teaching, perceived time spent at the bedside, and intern satisfaction with rounds. We grouped data from resident survey responses monthly. The baseline period is January–April 2018. To identify special cause variation in the data, we applied 2 probability-based run chart rules: we defined a shift as ≥8 consecutive points above or below the mean, and we defined a trend as ≥6 consecutive points that increased or decreased.15
Ethical Considerations
The CHOP Institutional Review Board reviewed the study and determined it to be Institutional Review Board exempt. We periodically checked in with families and nursing staff to see how they perceived the changes. Before examining a patient as a group, we always asked permission with proper personal protective equipment. Although we did not explicitly study this, anecdotally, families were supportive of the team-based physical examination and felt included as part of the team.
In this report, we have adhered to the SQUIRE 2.0 QI reporting standards.16
RESULTS
We recorded 193 survey responses: 25 in the baseline data collection period and 168 in the intervention period. Based on the average team composition, we expected 336 survey responses for a response rate of 57%.
Bedside physical examination teaching occurred most or every day (Fig. 3; preintervention mean 10%), at least 1 hour of perceived time spent at the bedside (Fig. 4; preintervention mean 36.7%), and intern rounding satisfaction (Fig. 5; preintervention mean rating 6.7/10) improved from baseline with the implementation of our PDSA cycles.
Fig. 4.
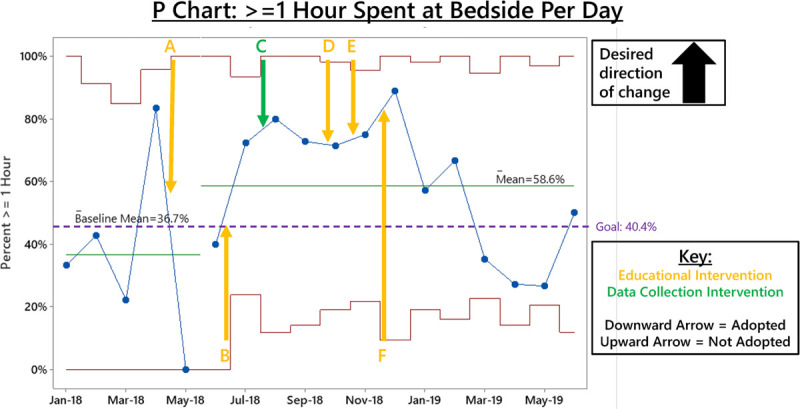
P-chart of ≥1 hour spent at the bedside per day interventions. A, Daily bedside physical examination during rounds. B, Afternoon examination with attending (not adopted). C, Coffee cards to incentivize survey completion. D, Regular email communication of expectations. E, Documentation of teaching goal. F, Bedside teaching tip sheet (not adopted).
Fig. 5.
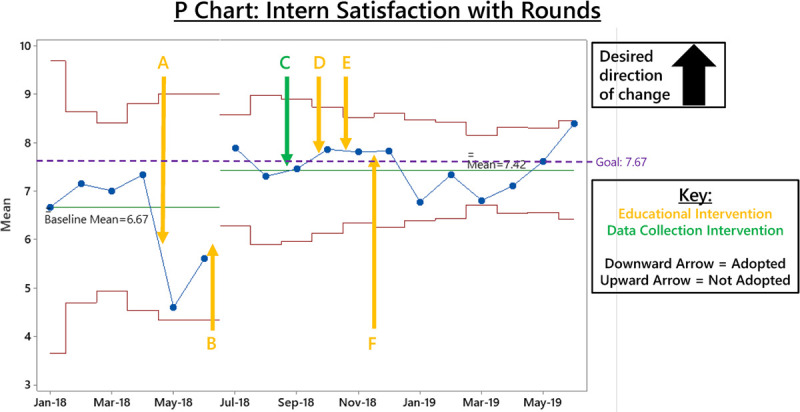
P-chart of intern satisfaction with rounds interventions. A, Daily bedside physical examination during rounds. B, Afternoon examination with attending (not adopted). C, Coffee cards to incentivize survey completion. D, Regular email communication of expectations. E, Documentation of teaching goal. F, Bedside teaching tip sheet (not adopted).
The percentage of interns reporting beside physical examination teaching occurring most or every day improved from a baseline mean of 10% to above our goal (60.7%) with a positive shift starting in June 2018 after our first intervention (daily bedside physical examination on rounds) and remained sustained at or above our goal for the study duration. The percentage of interns reporting at least 1 hour of perceived time spent at the bedside improved from a baseline mean of 36.7% to above our goal (58.6%) with a positive shift starting in June 2018. Intern satisfaction improved from a baseline mean rating of 6.7/10 to 7.4/10 with a positive shift starting in June 2018, though this fell short of our goal increase (Fig. 5).
There was no impact on the balancing measure of the average duration of rounds per patient (Fig. 6) following the introduction of daily bedside physical examinations and the PDSAs to sustain this change, with normal random variation observed post-intervention. In June 2019, 3 outlier patients may account for the increase in rounding time.
DISCUSSION
Using a standardized system for developing and implementing a resident-run QI project, we successfully increased bedside physical examination teaching on rounds, perceived time at the bedside, and rounding satisfaction, without significantly increasing the length of rounds.
We demonstrated improvement in our primary and secondary outcomes without sacrificing efficiency. Physical examination teaching on rounds met our goal improvement and demonstrated a sustained change, remaining above that the level for the study period’s duration. Perceived time at bedside improved above our goal but did not demonstrate sustained change throughout the entire study. Although it may be related to a higher rounding time per patient and/or increased census on the general pediatric service, it is unclear why.
Resident satisfaction improved but did not meet our goal; there are several potential reasons for this. There may have been an insufficient sample of residents to detect such an increase in satisfaction since overall satisfaction was, at baseline, high (though this is in contrast to the survey data before implementation, which was cross-sectional rather than longitudinal). Additionally, the PDSA cycles focused primarily on education rather than efficiency. This trade-off was purposeful; we decided to focus on education to change the institutional culture to promote physical examination teaching on rounds before tackling the myriad factors that influence rounding efficiency. Although there was no significant change in rounding duration per patient with our interventions, there are potential opportunities to shorten rounds to optimize resident educational opportunities. Additionally, we report an average rounding time per patient to account for varying floor census during our study period. Still, higher census and longer overall rounds may have impacted satisfaction as well.
We created a model organizational structure for other residents to emulate on longitudinal projects during their training. Despite a busy and rapidly changing schedule, with proper planning and strong handoffs, residents can start and follow through with a project requiring buy-in from multiple stakeholders. We have since transitioned this project’s leadership to PGY1 and PGY2s at our institution; they are currently working on devising and implementing their interventions using this foundation.
Our interventions impacted the specific floor on which the QI interventions took place and other floors in our institution. As residents rotate throughout the hospital, they have brought physical examination teaching elements elsewhere and informally expanded the program throughout the hospital.
Additional barriers to implementation were identified through survey comments and team observation and multiple reasons why interventions were not adopted (for instance, afternoon examinations were not adopted based on attending preference). Most importantly, sustaining this intervention required a culture shift. We found that involving an interdisciplinary team in our PDSA design was critical. Other significant barriers included patient volume and acuity, as well as attending and nursing preferences. Minor barriers included large team size and the group’s requirement to don contact precautions to enter individual rooms. We also found that we needed reminders and incentives to encourage senior residents to continue to bedside round and junior residents to complete surveys.
Strength of our study was the ability to measure the impact of various interventions on bedside teaching. There have been numerous qualitative studies evaluating perceptions of FCR, although most focus primarily on communication and other aspects of rounding rather than education. One interventional study evaluated a toolkit for physical examination teaching similar to our bedside teaching tip sheet. It demonstrated that residents’ perceptions of bedside physical examination teaching frequency increased, although it was not quantified and was not the study’s primary aim.12 A future project could specifically look at this tool’s effect, our tip sheet, or others on bedside teaching quality.
Limitations
The project took place on a single hospital unit that historically participated in other QI initiatives, and more broadly, within an institution with an established QI infrastructure. This existing culture likely assisted in our efforts and facilitated stakeholder buy-in and may limit our findings’ reproducibility. The sample size was limited by small team size, resulting in only 3–5 data points per week, and our preintervention period was short. The project was also subject to a hospital setting’s inherent variability, including the frequent turnover of attending physicians and resident teams, differences in resident experience at different points in the academic calendar, variable patient diagnoses, and unit census. Notably, the intervention of daily bedside examinations took place a few weeks before the start of a new academic year. These factors may have limited the validity of data trends and the significance of findings. Attempts to limit this variability included performing the intervention on a single unit, focusing on general pediatric patients, introducing the intervention at the beginning of the residency year to limit differences between residency class years, and gathering data over 1.5 years, including a sustained change period of 6 months. Additionally, group bedside physical examination may not be generalizable if personal protective equipment is limited, or disease transmission concerns exist.
Survey measures directly assessed the resident perception of rounding frequency and time with patients. We based these measures on survey results rather than direct timing due to the difficulty of activity measurement outside of rounds. No validated surveys exist to assess the specific aspects of rounding on which we focused. Nevertheless, we measured total rounding time effectively and extrapolated actual time at the bedside from perceived time. We conducted no formal assessments of physical examination skills. This project’s longitudinal nature made it difficult to separate our interventions’ impact from the expected improvement due to natural intern progression throughout the year. We did not assess patient outcomes. Although we took feedback ad hoc, we did not utilize a standard survey to study feedback from nursing, attendings, or families. We initially surveyed nurses regarding their satisfaction with rounds as a balancing measure. Still, these data were inconsistent and infrequent, so we ultimately stopped it, and it is not presented here.
CONCLUSIONS
This project demonstrates the successful creation and implementation of an organizational structure that can allow resident-driven, interdisciplinary projects to succeed despite the heavy clinical load, competing priorities, and varying schedules. We developed and sustained a structured QI project and motivated fellow residents and colleagues across disciplines to implement this change. We hope that this model can be used for future projects both within our institution and similarly sized residency programs in other institutions.
In the current inpatient environment, with multiple competing goals and learners of different levels, creating a rounding environment that allows for education while maintaining efficiency is crucial. This project successfully implemented structured bedside physical examination teaching and a shift in the rounding culture on a busy inpatient unit, meeting our goals of demonstrating sustained improvement in frequency of bedside physical examination teaching and rounding satisfaction and improvement in perceived time at the bedside, without sacrificing efficiency. We are currently trialing our interventions on general pediatric teams on other units in our institution, and there is potential for spread to other subspecialties. Unstudied interventions include family preference on joining rounds, limiting computers, and providing additional teaching tools to senior residents.
ACKNOWLEDGMENTS
We thank the CHOP Pediatric Residency leadership, the Department of Pediatrics Office of Practice Innovation and Improvement, general pediatrics attendings, our nursing colleagues, and the ACGME Back to Bedside program for their support. We also acknowledge Drs. Tara Bamat, Jacqueline Meadow, Jessica Winters for their assistance in conceptualizing the project, Drs. Christopher Bonafide, and Kathy Shaw for providing feedback on the manuscript, and most importantly, Brenna Aredas for guiding us through the publication process.
Supplementary Material
Footnotes
Published online May 19, 2021
Presented at the CHOP 2nd Annual Interprofessional Education Day, Philadelphia, PA [Frosch O, & Argraves M (January 2019). Project SPHERE: Shaping a Patient and Housestaff Engaged Rounding Environment Oral Presentation]; the ACGME Annual Educational Conference, Orlando, FL [Krass P, Frosch O, Argraves M, Becker A, Carroll B, Christiano J, Kamsheh A, Meadow J, Mehta S, Wild T (March 2019). Project SPHERE: Shaping a Patient and Housestaff Engaged Rounding Environment Poster]; the Pediatric Academic Societies; Baltimore, MD [Argraves M, Becker A, Carroll B, Christiano J, Frosch O, Kamsheh A, Krass P, McCloskey M, Meadow J, Mehta S, Salazar E, Wild T, Taylor A, Bamat T, Hart J (April 2019). A Resident-Driven Initiative to Increase Bedside Teaching on Interdisciplinary Rounds Poster]; and the Pediatric Hospital Medicine Annual Conference; Seattle, WA [Frosch O, & Carroll B (July 2019). A Resident-Driven Initiative to Increase Bedside Teaching on Interdisciplinary Rounds. Oral Platform].
A grant from the Accreditation Committee for Graduate Medical Education (ACGME) “Back to Bedside” initiative awarded in December 2017 supported this project.
Drs Becker and Frosch contributed equally to this work and should be considered co-first authors.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
To cite: Becker A, Frosch O, Argraves M, Carroll B, Kamsheh A, Krass P, Mehta S, Salazar E, Taylor A, Hart J. A Resident-driven Initiative to Increase Bedside Teaching on Interdisciplinary Rounds. Pediatr Qual Saf XXXX;X:XXXX.
Disclosure The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Committee on Hospital Care And Institute For Patient- And Family-Centered Care. Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012; 129:394–404. [DOI] [PubMed] [Google Scholar]
- 2.Beck J, Kind T, Meyer R, et al. Promoting resident autonomy during family-centered rounds: a qualitative study of resident, hospitalist, and subspecialty physicians. J Grad Med Educ. 2016; 8:731–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rabinowitz R, Farnan J, Hulland O, et al. Rounds today: a qualitative study of internal medicine and pediatrics resident perceptions. J Grad Med Educ. 2016; 8:523–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aronson PL, Yau J, Helfaer MA, et al. Impact of family presence during pediatric intensive care unit rounds on the family and medical team. Pediatrics. 2009; 124:1119–1125. [DOI] [PubMed] [Google Scholar]
- 5.Rappaport DI, Ketterer TA, Nilforoshan V, et al. Family-centered rounds. Clin Pediatr (Phila). 2011; 51:260–266. [DOI] [PubMed] [Google Scholar]
- 6.Rea KE, Rao P, Hill E, et al. Families’ experiences with pediatric family-centered rounds: a systematic review. Pediatrics. 2018; 141:e20171883. [DOI] [PubMed] [Google Scholar]
- 7.Mittal VS, Sigrest T, Ottolini MC, et al. Family-centered rounds on pediatric wards: a PRIS network survey of US and Canadian hospitalists. Pediatrics. 2010; 126:37–43. [DOI] [PubMed] [Google Scholar]
- 8.Rosen P, Stenger E, Bochkoris M, et al. Family-centered multidisciplinary rounds enhance the team approach in pediatrics. Pediatrics. 2009; 123:e603–e608. [DOI] [PubMed] [Google Scholar]
- 9.Pinto JM, Chu D, Petrova A. Pediatric residents’ perceptions of family-centered rounds as part of postgraduate training. Clin Pediatr (Phila). 2013; 53:66–70. [DOI] [PubMed] [Google Scholar]
- 10.Mittal V, Krieger E, Lee BC, et al. Pediatrics residents’perspectives on family-centered rounds: a qualitative study at 2 children’s hospitals. J Grad Med Educ. 2013; 5:81–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sandhu AK, Amin HJ, McLaughlin K, et al. Leading educationally effective family-centered bedside rounds. J Grad Med Educ. 2013; 5:594–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patel A, Unaka N, Holland D, et al. Increasing physical exam teaching on family-centered rounds utilizing a web-based tool. Pediatr Qual Saf. 2017; 2:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harris PA, Taylor R, Thielke R, et al. Journal of biomedical informatics. J Biomed Inform. 2009; 42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris PA, Taylor R, Minor BL, et al. ; REDCap Consortium. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019; 95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003; 12:458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ogrinc G, Davies L, Goodman D, et al. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2016; 25:986–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


