Abstract
Background
Tecfidera® (dimethyl fumarate [DMF]) is an approved product for the treatment of relapsing forms of multiple sclerosis. Monomethyl fumarate (MMF) is the only active metabolite of DMF and is responsible for its therapeutic efficacy.
Objective
The objective of this study was to determine whether two Bafiertam™ capsules each containing 95 mg of MMF is bioequivalent to one Tecfidera® capsule containing 240 mg of DMF, a prodrug of MMF.
Methods
This was a single-dose, open-label, randomized, two-way crossover study evaluating two treatments over two periods with a washout interval between treatments. Fifty healthy subjects were randomized to receive a single dose of the test drug MMF 190 mg as 2 × 95 mg delayed-release capsules or the reference drug DMF 240 mg as a 1 × 240-mg delayed-release capsule. Blood samples were obtained prior to dosing and at prespecified time points through 24 h post-dose to determine plasma concentrations of MMF. The pharmacokinetic parameters of MMF were calculated including maximum observed concentration, time to reach maximum observed concentration, apparent half-life of the drug in plasma, AUC0–t which is the area under the plasma concentration–time curve (AUC) from time zero (dosing time) to the last time point, t, with measurable analyte concentration, and AUC0–inf, which is AUC0–t plus the extrapolated AUC from time t to infinity.
Results
The geometric least-squares mean ratios (90% confidence interval) of the test drug MMF vs the reference drug DMF were 96.80% (92.18–101.64), 96.35% (91.81–101.12), and 104.84% (95.54–115.05) for AUC0–t, AUC0–inf, and maximum observed concentration, respectively. Two capsules of Bafiertam™ was safe and generally well tolerated. The most common adverse event for both products was flushing, 60% and 51%, for Bafiertam™ and Tecfidera®, respectively.
Conclusions
Based on the statistical analysis results of the pharmacokinetic parameters of MMF, a single oral dose of two Bafiertam™ DR 95 mg capsules is bioequivalent to a single oral dose of one Tecfidera® DR 240 mg capsule.
Clinical Trial Registration
This study was retrospectively registered with ClinicalTrials.gov (NCT04570670) on 30 September, 2020.
Key Points
| This was a phase I bioequivalence study evaluating if a single oral 190 mg dose of two Bafiertam™ capsules (2 × 95 mg) produced equivalent plasma exposures of monomethyl fumarate to those achieved with a 240 mg dose of one Tecfidera® capsule (1 × 240 mg). |
| This study established pharmacokinetic bioequivalence of Bafiertam™ to the reference product Tecfidera® in terms of exposure to the active moiety, and therefore established the safety and therapeutic efficacy of Bafiertam™ for the treatment of relapsing forms of multiple sclerosis. |
Introduction
Tecfidera® (dimethyl fumarate [DMF]) was initially approved in the USA in 2013 and Europe in 2014 for the treatment of patients with relapsing forms of multiple sclerosis (MS). Efficacy and safety were established based on a statistically significant treatment effect for the primary endpoint, positive results for most secondary outcome measures, and an acceptable safety profile in the two phase III studies, DEFINE and CONFIRM [1, 2].
The mechanism by which DMF exerts its therapeutic effect in MS is unknown; however, after oral administration of Tecfidera®, DMF undergoes rapid and extensive pre-systemic hydrolysis by esterases and is substantially converted to its only active metabolite, monomethyl fumarate (MMF) [3]. Dimethyl fumarate and MMF have been shown to activate the nuclear factor (erythroid-derived 2)-like 2 pathway in vitro and in vivo in animals and humans. The nuclear factor (erythroid-derived 2)-like 2 pathway elicits both antioxidant and anti-inflammatory responses. Additionally, MMF has been identified as a nicotinic acid receptor agonist of hydroxycarboxylic acid receptor 2, a Gi-protein coupled membrane receptor specifically involved in anti-inflammatory and/or protective responses [4, 5]. MMF is metabolized by the tricarboxylic cycle pathway and about 60% of the DMF dose is excreted as exhaled CO2 [6].
Following the rapid conversion of DMF to its active metabolite MMF by hydrolysis after oral administration of Tecfidera®, plasma DMF concentrations are not quantifiable and it is MMF that confers therapeutic efficacy. Pharmacokinetic (PK) studies following administration of Tecfidera® were performed by evaluating plasma MMF concentrations in both healthy subjects and subjects with MS. Thus, regulatory guidance for approval of Bafiertam™ (containing MMF) was to establish bioequivalence between Bafiertam™ and Tecfidera® capsules based on plasma MMF concentrations [7]. Additionally, a relative bioavailability study conducted under fed and fasted conditions supports the guidance for administration of Bafiertam™ with or without food [8].
Therefore, this study was designed to assess the bioequivalence of a single oral dose of Bafiertam™ (MMF [previously referred to as BLS-11 by Banner Life Sciences]) and Tecfidera® (DMF) based on PK parameters of MMF in healthy subjects. With equivalent plasma exposure to MMF, the active moiety, the safety and efficacy of Bafiertam™ can then be inferred based on the established clinical safety and efficacy of Tecfidera®.
Methods
Subjects
Healthy male and female subjects 18–55 years of age were eligible for enrollment. Subjects were required to have a body mass index ≥ 18.5 to ≤ 29.9 kg/m2 and were excluded for any clinically significant medical condition. Subjects who were not surgically sterile, or female subjects who were not postmenopausal for ≥ 1 year and of childbearing potential, were required to follow protocol-specified contraceptive methods. Subjects were required to refrain from the use of any drug with potential for drug–drug interactions affecting the pharmacokinetics, including prescription and non-prescription medications, or herbal remedies, within 14 days prior to the first dose of the study drug.
Study Design
This was a single-dose, open-label, randomized, two-way crossover study evaluating the pharmacokinetics of MMF after a single dose of the test product vs the reference product under fasting conditions over two dose periods separated by 2 days. Healthy subjects were randomized to one of two treatment sequences prior to the first dose to minimize the period effect in a crossover study. In each period, subjects received one of the two treatments based on the treatment sequence: (1) test: a single oral dose of MMF 190 mg administered as two Bafiertam™ 95 mg delayed-release (DR) capsules, and (2) reference: DMF 240 mg administered as one Tecfidera® 240 mg DR capsule. Each dose of study drug was administered with 240 mL of water after an overnight fast, which continued for another 4 h post-dose. Blood samples for measurement of plasma MMF concentrations were collected in each period within 15 min prior to dosing, and at 0.5, 1, 1.5, 2, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, 8, 9, 10, 11, 12, and 24 h post-dose. Blood samples were collected into prechilled Vacutainer® tubes containing sodium fluoride and potassium oxalate as the stabilizer and anticoagulant, respectively. The stabilizer (sodium fluoride) was used to quench the hydrolysis of DMF, if any, to MMF immediately upon blood collection. Prior to the clinical study, the selected anticoagulant and stabilizer were verified by validation experiments conducted by BioPharma Services to be sufficient to stop the esterase hydrolysis. Immediately upon blood collection, the collection tubes were gently inverted to allow mixing of the blood, anticoagulant, and the stabilizer, and were then cooled in an ice bath and centrifuged (approximately at 2056 × gravity for 7 min) under refrigeration (approximately 4 °C) as soon as possible and no later than 60 min after blood collection. Plasma samples were stored at approximately − 70 °C or lower until analysis.
This study was conducted in accordance with the US Food and Drug Administration (FDA) guidance for bioavailability and bioequivalence studies for orally administered drug products [9]. The study received institutional review board approval and all subjects provided written informed consent prior to the conduct of study-related procedures. The study was conducted at Celerion’s phase I clinical research unit (Tempe, AZ, USA) in compliance with the protocol, Good Clinical Practice guidelines, the ethical principles of the Declaration of Helsinki, and all applicable regulatory requirements.
PK Endpoints and Analysis
The primary endpoints for bioequivalence assessment are AUC0–inf and C max of MMF between the two treatments (MMF 190 mg vs DMF 240 mg). The AUC0–t was also compared between treatments as supportive information. The definitions of these PK parameters are as follows: C max is the maximum observed plasma concentration, AUC0–t is the area under the plasma concentration–time curve (AUC) from time zero (dosing time) to the last time point, t, with measurable analyte concentration, and AUC0–inf is AUC0–t plus the extrapolated AUC from time t to infinity. Additional PK parameters including the percent of AUC0–inf that is extrapolated (AUC%extrap), time to reach C max (tmax), and the apparent half-life of the drug in plasma (t 1/2) of MMF were computed for each treatment but not compared between treatments. Pharmacokinetic parameters of MMF were determined by a noncompartmental analysis of individual plasma concentration–time data using Phoenix® WinNonlin® Version 6.3 or higher (Certara, Princeton, NJ, USA).
Sample Size
A sample size of 44 subjects was calculated according to Hauschke et al. [10] using a power of at least 95% and an alpha error of 5%. The power was defined as the probability of having a 90% CI for the geometric least-squares mean (GLSM) ratio, test/reference, for each primary PK parameter to fall within the acceptance criteria of 80.00–125.00%. A true GLSM ratio between 95 and 105% was assumed and an intra-subject coefficient of variation (CV) of 24% was used for estimating the sample size. To ensure having 44 subjects in the study with evaluable PK data (e.g., exposure to treatment, availability and validity of measurements, and absence of major protocol violations), six additional subjects were enrolled with a total of 50 subjects dosed to account for potential dropouts. Statistical analysis was performed on all subjects contributing PK parameters of MMF (Cmax, AUC0–inf, and AUC0–t). However, statistical analysis for bioequivalence assessment was based on PK parameter data from subjects who completed the study and had sufficient data for a pairwise comparison (i.e., from both treatments).
Plasma Concentrations of MMF
The analysis of plasma MMF concentrations was conducted using a validated method to determine MMF in human plasma containing NaF/K-oxalate/1.0% phosphoric acid using high-performance liquid chromatography with tandem mass spectrometry. The method was developed and validated by BioPharma Services (Toronto, ON, Canada). Sample treatment involves protein precipitation and filtration from 100 μL of human plasma; MMF-d5 was used as the internal standard. The compounds were identified and quantified by liquid chromatography with tandem mass spectrometry over a theoretical concentration range of 25–2500 ng/mL, with a lower limit of quantitation of 25 ng/mL. This method met acceptance criteria with respect to specificity, sensitivity, precision, accuracy, matrix effect, linearity, percent extraction yields, and dilution integrity according to the FDA/CVM Guidance 145: Bioanalytical Method Validation (September 2013 and May 2001). Stability evaluations in matrix and solutions also met acceptance criteria, demonstrating no significant degradation of MMF and MMF-d5 (internal standard) over the storage durations for the clinical samples and conditions examined during the method validation. This method was fully validated in conformance with current FDA Regulations (21 CFR Part 58), the FDA/CVM Guidance 145: Bioanalytical Method Validation (September 2013 and May 2001), and the principles, as they apply to bioanalysis, of the OECD Series on Principles of Good Laboratory Practice (1997).
Safety and Tolerability
Safety and tolerability were assessed by analysis of treatment-emergent adverse events (TEAEs) reported from the time of the first dose through follow-up (telephone or e-mail contact approximately 7 days after the last dose of the study drug). Treatment-emergent adverse events were coded using the Medical Dictionary for Regulatory Activities (MedDRA®) Version 19.1. All TEAEs were graded as mild (event was easily tolerated and did not interfere with daily activity), moderate (event interfered with daily activity, but the subject was still able to function; medical intervention may have been considered), or severe (event was incapacitating and required medical intervention). Laboratory parameters (hematology, chemistry, and urinalysis) and vital signs were collected through day 2 of period 2. No inferential statistics were performed for safety assessments.
Statistical Analyses
Summary statistics (arithmetic mean; standard deviation; %CV, geometric %CV, standard error of the mean; median, minimum, maximum) were determined for continuous variables and number and percent for categorical variables and were summarized by treatment. Statistical analysis of PK parameters was performed on natural log (ln)-transformed AUC0–t, AUC0–inf, and Cmax using analysis of variance (ANOVA). The ANOVA model included sequence, treatment, and period as fixed effects, and subject nested within a sequence as a random effect. The ANOVA included calculation of least-squares means of the ln-transformed parameter as well as the least-squares mean difference between treatments.
Ratios of GLSM, test vs reference, were calculated by exponentiating the least-squares mean difference between treatments from the ANOVA on the ln-transformed data. The 90% CIs for the GLSM ratios were derived similarly as the GLSM. Bioequivalence criteria are met if the 90% CIs for the ratios of GLSMs of both C max and AUC0–inf of the test (Bafiertam™, MMF) to the reference (Tecfidera®, DMF) fall within the boundaries of 80.0% and 125%. Statistical analysis was performed using SAS Version 9.3 or higher (SAS Institute Inc., Cary, NC, USA).
Results
The study was conducted at a single site in the USA. Enrollment began on 6 January, 2017 and the last subject completed the study on 16 February, 2017.
Subject Disposition and Baseline Demographics
Fifty subjects were randomized and dosed and one subject discontinued early; the subject, randomized to the treatment sequence of Bafiertam™ followed by Tecfidera®, withdrew consent (for personal reasons) and discontinued on day 1 after being dosed with MMF. Most subjects were male (72%), white (76%), and the mean age (standard deviation) was 36.2 (9.17) years. All subjects met eligibility criteria.
Pharmacokinetics
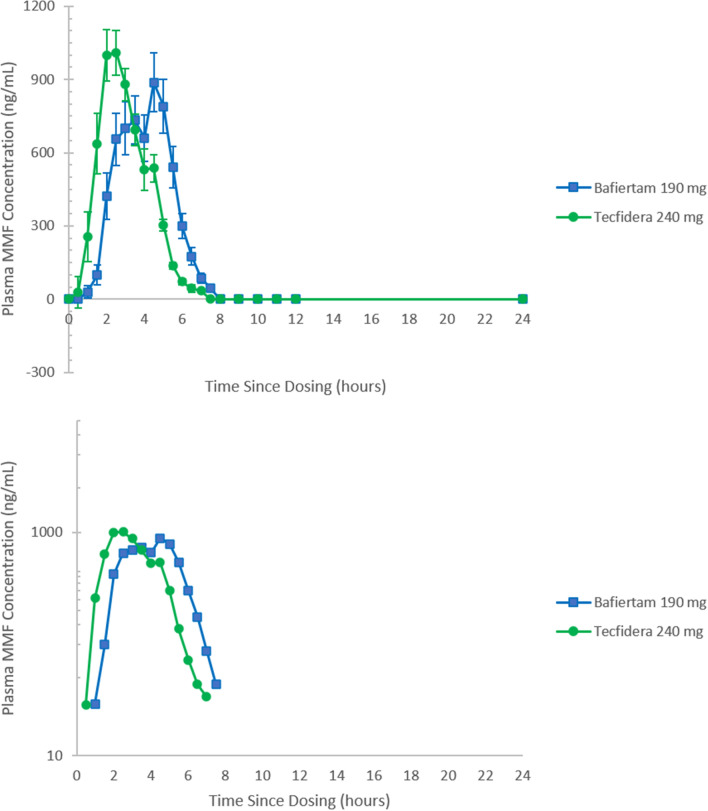
Linear and semi-log plots of the mean (± standard error of mean) plasma concentration–time curves after a single oral dose of MMF 190 mg (2 × 95 mg) and a single oral dose of DMF 240 mg (1 × 240 mg) under fasting conditions are presented in Fig. 1. All PK parameters of MMF are summarized in Table 1 and results of the statistical comparison of AUC0–t, AUC0–inf, and C max of MMF are presented in Table 2.
Fig. 1.
Mean plasma monomethyl fumarate (MMF) concentration-time profiles following a single oral dose of Bafiertam™ 190 mg (2 × 95 mg) and a single oral dose of Tecfidera® 240 mg. Mean ± standard error of the mean linear and semi-log are displayed in the upper and lower panels, respectively. The lower limit of quantitation−upper limit of quantitation for MMF in plasma was 25–2500 ng/mL. Plasma samples from all 50 subjects and from 49 subjects were assayed and included for Bafiertam™ and Tecidera®, respectively
Table 1.
Summary of MMF pharmacokinetics following a single oral dose of Bafiertam™ (MMF) 2 × 95 mg or Tecfidera® (DMF) 1 × 240 mg
| PK parameters | Bafiertam™ (MMF 2 × 95 mg) (test) |
Tecfidera® (DMF 1 × 240 mg) (reference) |
||
|---|---|---|---|---|
| n | n | |||
| AUC0–t (ng*h/mL) |
AM: 3051 (26.3%) GM: 2952 (26.4%) |
49 |
AM: 3145 (25.3%) GM: 3051 (25.0%) |
49 |
| AUC0–inf (ng*h/mL) |
AM: 3081 (26.0%) GM: 2984 (25.9%) |
49 |
AM: 3203 (24.3%) GM: 3116 (23.9%) |
48 |
| AUC%extrap (%) | 1.29 ± 0.27 | 49 | 1.27 ± 0.35 | 48 |
| C max (ng/mL) |
AM: 1860 (32.5%) GM: 1760 (34.8%) |
49 |
AM: 1770 (32.7%) GM: 1680 (33.8%) |
49 |
| t max (h) | 4.03 (1.02, 6.01) | 49 | 2.50 (1.01, 5.04) | 49 |
| t ½ (h) | 0.566 ± 0.154 | 49 | 0.591 ± 0.185 | 48 |
AM arithmetic mean, AUC area under the concentration–time curve, AUC 0–inf AUC from time 0 extrapolated to infinity, AUC 0–t AUC from time 0 to the time of the last measured non-zero analyte concentration, AUC %extrap percent of AUC0–inf extrapolated, C max maximum observed concentration, CV coefficient of variation, DMF dimethyl fumarate, GM geometric mean, MMF monomethyl fumarate, PK pharmacokinetic, SD standard deviation, t 1/2 apparent half-life of the drug in plasma, t max time to reach C max
AUC and C max values are presented as arithmetic mean (CV%) and geometric mean (geometric CV%)
t max values are presented as median (minimum, maximum)
Other parameters are presented as arithmetic mean (± SD)
Note: Subject 11 who discontinued from the study because of personal reasons 6.5 h after a single dose of Bafiertam™ was excluded from all PK parameter calculations and the subsequent statistical analysis for bioequivalence. Subject 9 was excluded from the Tecfidera® AUC0–inf and t ½ calculations because of missing or unreportable values and was excluded from the statistical analysis. The terminal elimination phase was not clearly defined for Subject 9 following treatment with Tecfidera®. In this instance, because the terminal elimination constant could not be reliably estimated, AUC0–inf, t ½, and AUC%extrap were reported as missing. As only AUC0–-inf values were obtained following treatment with Bafiertam™ for Subject 9, the PK data were not used in the statistical analysis for bioequivalence because the subject did not fit the description of the statistical population for bioequivalence (i.e., did not have sufficient data for a pairwise comparison, i.e., from both treatments)
Table 2.
Statistical analysis of PK parameters of MMF following a single oral dose of Bafiertam™ (MMF) 2 × 95 mg or Tecfidera® (DMF) 1 × 240 mg
| Parameter | Bafiertam™ (MMF 2 × 95 mg) (test) | Tecfidera® (DMF 1 × 240 mg) (reference) | Statistical analysis results Test vs reference |
||||
|---|---|---|---|---|---|---|---|
| GLSM | n | GLSM | n | GLSM ratio (%) | 90% confidence interval | Intra-subject CV% |
|
| AUC0–t (ng*h/mL) | 2955 | 49 | 3053 | 49 | 96.80 | 92.18–101.64 | 14.48 |
| AUC0–inf (ng*h/mL) | 3002 | 48 | 3116 | 48 | 96.35 | 91.81–101.12 | 14.16 |
| C max (ng/mL) | 1760 | 49 | 1680 | 49 | 104.84 | 95.54–115.05 | 27.93 |
ANOVA analysis of variance, AUC area under the concentration–time curve, AUC 0–inf AUC from time 0 extrapolated to infinity, AUC 0–t AUC from time 0 to the time of the last measured non-zero analyte concentration, C max maximum observed concentration, CV coefficient of variation, DMF dimethyl fumarate, GLSM geometric least-squares mean, LSMs least-square means, MMF monomethyl fumarate, PK pharmacokinetic
Statistical analysis for bioequivalence was based on PK parameter data from subjects who completed the study and contributed PK parameter values for a pairwise comparison (i.e., from both treatments)
GLSMs were calculated by exponentiating the LSMs derived from the ANOVA
GLSM ratio = 100% × (test/reference)
Intra-subject CV% was calculated as 100% × square root(exp[MSE]−1), where MSE = residual variance from the ANOVA
The mean AUC%extrap values were approximately 1.3% for both treatments, suggesting that the sampling time was sufficiently long to fully characterize the plasma profile of MMF. Following Bafiertam™ administration (190 mg MMF), t max of MMF was prolonged by approximately 1.5 h (compared with the reference DMF), although the mean C max and t 1/2 were comparable between treatments. Inter-subject variability (geometric CV%) for AUC and C max were 26% and 35%, respectively, following administration of Bafiertam™ capsules. Comparable inter-subject variability for each parameter of MMF was also observed after administration of the Tecfidera® capsule. The higher inter-subject variability observed in C max than in AUC following Bafiertam™ administration is consistent with Tecfidera® data, which is expected for DR dosage forms. The 90% CIs of the GLSM ratio of AUC0–t, AUC0–inf, and Cmax of MMF fell entirely within the 80–125% boundaries, indicating that a single oral dose of MMF 190 mg (2 × 95 mg Bafiertam™ DR capsules) is bioequivalent to DMF 240 mg (1 × 240 mg Tecfidera® DR capsule).
Safety
A single oral dose of MMF 190 mg was safe and generally well tolerated with no subject discontinuing because of a TEAE, and no serious adverse events or deaths reported. All TEAEs were mild in severity. No clinically significant laboratory or vital sign abnormalities were observed.
A summary of TEAEs occurring by treatment is presented in Table 3. A total of 42 TEAEs were reported by 31 subjects (62%) treated with MMF and 37 TEAEs reported by 29 subjects (59%) treated with DMF. The most common TEAE was flushing for both treatments. All events of flushing were assessed by the investigator as likely related to the study drug. The following events occurring in more than one subject were assessed as at least possibly related to study drug: diarrhea, nasal congestion, and skin fissures (verbatim term, chapped lips).
Table 3.
Incidence of TEAEs by treatment (percent of subjects randomized and treated)
| Treatment | ||
|---|---|---|
| System organ class Preferred term, n (%) |
Bafiertam™ (MMF 2 × 95 mg) N = 50 |
Tecfidera® (DMF 1 × 240 mg) N = 49 |
| Number of subjects reporting at least 1 TEAEa | 31 (62%) | 29 (59%) |
| Number of TEAEs | 42 | 37 |
| Gastrointestinal tolerabilityb | 1 (2%) | 2 (4%) |
| Abdominal pain (pooled) | 1 (2%) | 1 (2%) |
| Diarrhea | 0 (0%) | 2 (4%) |
| Gastrointestinal disorders | 1 (2%) | 2 (4%) |
| Diarrhea | 0 (0%) | 2 (4%) |
| Respiratory, thoracic, and mediastinal disorders | 1 (2%) | 2 (4%) |
| Nasal congestion | 0 (0%) | 2 (4%) |
| Skin and subcutaneous tissue disorders | 2 (4%) | 1 (2%) |
| Skin fissures | 1 (2%) | 1 (2%) |
| Vascular disorders | 30 (60%) | 25 (51%) |
| Flushing | 30 (60%) | 25 (51%) |
DMF dimethyl fumarate, MMF monomethyl fumarate, TEAEs treatment-emergent adverse events
aAdverse events were coded using the Medical Dictionary for Regulatory Activities (MedDRA®) Version 19.1. Treatment-emergent adverse events by System Order Class with Preferred Terms occurring in at least 2 subjects are presented
bGastrointestinal tolerability was defined as all adverse events pertaining to abdominal pain (abdominal pain, abdominal pain upper, abdominal distension), nausea, vomiting, and diarrhea
Discussion
Results of this pivotal bioequivalence study showed that MMF 190 mg administered as two Bafiertam™ 95 mg DR capsules under fasting conditions was bioequivalent (i.e., equivalent MMF plasma exposure) to the approved product DMF 240 mg administered as a single Tecfidera® 240 mg DR capsule for the treatment of relapsing forms of MS. Following administration of two 95-mg Bafiertam™ capsules under fasting conditions, MMF plasma profiles were consistent with those expected from a DR dosage form. MMF was readily absorbed from Bafiertam™ capsules with a median t max occurring at approximately 4 h post-dose. Although the median t max of MMF after Bafiertam™ administration occurred about 1.5 h later than that after Tecfidera® administration, C max of MMF was comparable between the Bafiertam™ 190 mg dose and the Tecfidera® 240 mg dose. A higher inter-subject variability in MMF C max was observed than in MMF AUC for both Bafiertam™ and Tecfidera® capsules, which is also an expected phenomenon for DR capsules, potentially owing to inter-subject variability in gastric emptying time. However, the inter-subject variability (expressed as CV%) for both C max and AUC following Bafiertam™ administration was lower than what has been observed overall for Tecfidera® (i.e., CV% of 33–67% for C max and about 30% for AUC) [7]. Systemic MMF was rapidly eliminated from plasma with a mean t 1/2 of about 30 min following administration of either Bafiertam™ capsules or the Tecfidera® capsule. Although in vitro testing during the development of the Bafiertam™ formulation had shown that the dissolution performance and the release profiles are similar between one capsule and two capsules, the apparent double peak observed in the Bafiertam™ curve may arise from variable gastric emptying times when dosing with two capsules of Bafiertam™ vs the single Tecfidera® capsule.
In this single-dose study, the safety profile of Bafiertam™ (MMF) was similar to the safety profile of Tecfidera® (DMF). Mild non-serious flushing was the most common TEAE observed in this open-label study; in 60% of subjects treated with Bafiertam™ (MMF) and 51% of subjects treated with Tecfidera® (DMF). The relatively small number of subjects enrolled, the open-label design, and administration of either product under fasting conditions likely contributed to an overall higher incidence observed in this small study relative to the phase III studies for Tecfidera® (i.e., 76% v. 40%), as well as a recent 5-week tolerability study evaluating Bafiertam™ vs Tecfidera® [6, 11]. In the latter study, mild flushing was reported in 43% and 54% of subjects, respectively. The only other events that occurred in more than two subjects in this study were gastrointestinal (GI) and cutaneous events, both common events observed with Tecfidera® [6].
MMF is the sole active moiety of DMF that is measurable in plasma following DMF administration, which unequivocally contributes to the efficacy of DMF. By showing bioequivalence based on PK parameters of MMF, the therapeutic equivalence of MMF (two Bafiertam™ capsules) to the approved DMF product (one Tecfidera® capsule) was accepted by the FDA and Bafiertam™ was approved for relapsing forms of MS in April 2020. The test product of MMF in this study was formulated as a DR Bafiertam™ capsule containing MMF 95 mg. By directly delivering the active drug, MMF, there is potential for reducing the tolerability issues associated with DMF, particularly GI events. Gastrointestinal tolerability issues have persistently resulted in treatment discontinuation of about 6% of patients in the long-term extension studies of DEFINE and CONFIRM [12]. Even higher rates of GI events (about 88% of whom 54% used symptomatic treatment) and discontinuation because of GI events (about 7%) have been observed in the post-marketing setting [13]. These GI tolerability issues of Tecfidera® may be related to the known cutaneous/mucosal irritant properties of DMF [14–16].
Recently, in 2019, another prodrug of MMF, diroximel fumarate, was approved for the treatment of relapsing forms of MS. As with Bafiertam™, diroximel fumarate was approved by establishing bioequivalence to Tecfidera®. In a 5-week tolerability study in patients with MS (EVOLVE study), diroximel fumarate had improved GI tolerability with less severe GI events and fewer days of self-assessed GI symptoms, fewer GI adverse events, and a lower rate of discontinuation because of GI events [17]. More recently, we have shown that treatment with Bafiertam™ (MMF), compared to its prodrug, Tecfidera® (DMF), for 5 weeks in healthy subjects showed a trend for a reduction in incidence, severity, and duration of GI symptoms favoring MMF [11]. Our data suggest that GI tolerability may be improved with direct MMF administration via Bafiertam™, which potentially eliminates any local irritation of the GI mucosa by DMF, while offering a bioequivalent dose of MMF.
Conclusions
Based on the PK results of this study, it was concluded that a 190 mg dose of Bafiertam™ produced equivalent plasma exposure to MMF, the active moiety, as compared to that achieved with a 240 mg dose of Tecfidera®, and therefore the safety and therapeutic efficacy of Bafiertam™ are established for the treatment of relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults.
Acknowledgements
Jane Anderson (J Anderson Solutions, LLC) provided medical writing support and was paid by Banner Life Sciences.
Declarations
Funding
This study was supported in its entirety by Banner Life Sciences. Banner Life Sciences paid the open access fee.
Conflict of interest
Thomas W. Lategan, Tiffany N. Sprague, and Franck S. Rousseau are employees of Banner Life Sciences. Laurene Wang is a paid consultant to Banner Life Sciences.
Ethics approval
All pertinent study documents were reviewed, and the study protocol approved by the Chesapeake Institutional Review Board prior to study initiation.
Consent to participate
All subjects provided written informed consent prior to the conduct of study-related procedures.
Consent for publication
Not applicable.
Availability of data and material
This phase I study was retrospectively registered with ClinicalTrials.gov (NCT04570670) on 30 September, 2020.
Code availability
Not applicable.
Author contributions
TWL: conceptualization, writing, original draft preparation; LW: study design, conduct and oversight, clinical research organization selection, sample size estimation, study result review, and data analysis, interpretation, and presentation; FR: conceptualization, supervision; TNS: project administration. All authors have read, commented on the manuscript, and approved the final manuscript. The authors were responsible for all content and editorial decisions.
References
- 1.Gold R, Kappos L, Arnold D, Bar-Or A, Giovannoni G, Selmaj K, et al. Placebo-controlled phase 3 study of oral BG-12 for relapsing multiple sclerosis. N Engl J Med. 2012;367(12):1098–1107. doi: 10.1056/NEJMoa1114287. [DOI] [PubMed] [Google Scholar]
- 2.Fox R, Miller D, Phillips J, Hutchinson M, Havrdova E, Kita M, et al. Placebo controlled phase 3 study of oral BG-12 or glatiramer in multiple sclerosis. N Engl J Med. 2012;367(12):1087–1097. doi: 10.1056/NEJMoa1206328. [DOI] [PubMed] [Google Scholar]
- 3.Werdenberg D, Joshi R, Wolffram S, Merkle H, Langguth P. Presystemic metabolism and intestinal absorption of antipsoriatic fumaric acid esters. Biopharm Drug Dispos. 2003;24:259–273. doi: 10.1002/bdd.364. [DOI] [PubMed] [Google Scholar]
- 4.Chen H, Assmann JC, Krenz A, Rahman M, Grimm M, Christian M, et al. Hydroxycarboxylic acid receptor 2 mediates dimethyl fumarate’s protective effect in EAE. J Clin Investig. 2014;124(5):2188–2192. doi: 10.1172/JCI72151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parodi B, Rossi S, Morando S, Cordano C, Bragoni A, Motta C, et al. Fumarates modulate microglia activation through a novel HCAR2 signaling pathway and rescue synaptic dysregulation in inflamed CNS. Acta Neuropathol. 2015;130(2):279–295. doi: 10.1007/s00401-015-1422-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Biogen. Tecfidera® (dimethyl fumarate) prescribing information and patient information. 2020. https://www.tecfiderahcp.com/content/dam/commercial/tecfidera/hcp/en_us/pdf/Tecfidera_PI.pdf. Accessed 22 June 2020.
- 7.US Food and Drug Administration, Center for Drug Evaluation and Research. Clinical pharmacology and biopharmaceutics review. 2013. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2013/204063Orig1s000ClinPharmR.pdf. Accessed 9 July 2020.
- 8.Banner Life Sciences. Biafertam™ (monomethyl fumarate) prescribing information and patient information. 2020. https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=a161f9d4-70f1-4097-957a-eafb35d3274f. Accessed 2 Nov 2020.
- 9.US Food and Drug Administration, Center for Drug Evaluation and Research. Guidance for industry: bioavailability and bioequivalence studies submitted in NDAs or INDs: general considerations (draft March 2014). https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM389370.pdf. Accessed 9 July 2020.
- 10.Hauschke D, Steinijans VW, Diletti E, Burke M. Sample size determination for bioequivalence assessment using a multiplicative model. J Pharmacokinet Biopharm. 1992;20(5):557–561. doi: 10.1007/BF01061471. [DOI] [PubMed] [Google Scholar]
- 11.Wynn D, Lategan TW, Sprague TN, Rousseau FS, Fox EJ. Monomethyl fumarate has better gastrointestinal tolerability profile compared with dimethyl fumarate. Mult Scler Relat Disord. 2020;45:102335. doi: 10.1016/j.msard.2020.102335. [DOI] [PubMed] [Google Scholar]
- 12.Gold R, Arnold DL, Bar-Or A, Hutchinson M, Kappos L, Havrdova E, et al. Long-term effects of delayed-release dimethyl fumarate in multiple sclerosis: Interim analysis of ENDORSE, a randomized extension study. Mult Scler J. 2017;23(2):253–265. doi: 10.1177/1352458516649037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fox EJ, Vasquez A, Grainger W, Ma TS, von Hehn C, Walsh J, et al. Gastrointestinal tolerability of delayed-release dimethyl fumarate in a multicenter, open-label study of patients with relapsing forms of multiple sclerosis (MANAGE) Int J MS Care. 2016;18:9–18. doi: 10.7224/1537-2073.2014-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCullough T, Annamalai T, Wustrow D, Cundy K. Comparative gastric irritation of the fumaric acid esters dimethyl fumarate (DMF) and XP23829 in rat and monkey. Neurology. 2013;80(7 Suppl.):P01.159.
- 15.Rantanen T. The cause of the Chinese sofa/chair dermatitis epidemic is likely to be contact allergy to dimethylfumarate, a novel potent contact sensitizer. Br J Dermatol. 2008;159(1):218–221. doi: 10.1111/j.1365-2133.2008.08622.x. [DOI] [PubMed] [Google Scholar]
- 16.Silvestre JF, Mercader P, De la Cuadra J, Ballester I, Gallardo F, Pujol RM, et al. Shoe contact dermatitis from dimethyl fumarate: clinical manifestations, patch test results, chemical analysis, and source of exposure. Contact Dermatitis. 2009;61(5):249–260. doi: 10.1111/j.1600-0536.2009.01628.x. [DOI] [PubMed] [Google Scholar]
- 17.Naismith RT, Wundes A, Ziemssen T, Jasinska E, Freedman MS, Lembo AJ, et al. Diroximel fumarate demonstrates an improved gastrointestinal tolerability profile compared with dimethyl fumarate in patients with relapsing-remitting multiple sclerosis: results from the randomized, double-blind, phase III EVOLVE-MS-2 study. CNS Drugs. 2020;34:185–196. doi: 10.1007/s40263-020-00700-0. [DOI] [PMC free article] [PubMed] [Google Scholar]