Abstract
Metallosis is a well-known complication at the site of total hip and knee arthroplasty. Vascular involvement of this complication is rare and generally results from vascular compression by a mass or pseudotumor. In the present report, we have described a case of lower limb acute arterial ischemia due to arterial injury as a complication of metallosis with a fatal outcome.
Keywords: Adverse local tissue reaction, ALTR, Femoral artery, Metallosis, Pseudotumor, Vascular complications
Vascular complications in prosthetic hip surgery are rare and have generally been related to the surgical procedure. They can be clear and evident early, such as hemorrhage due to direct vessel injury or ischemia related to traumatic arterial thrombosis. However, they can also develop in the late postoperative period, such as the formation of pseudoaneurysms and arteriovenous fistulas. Metallosis has been described as a complication at the site of total hip and knee arthroplasty, and, very infrequently, metallosis has been responsible for a vascular injury, generally resulting from compression by a mass or pseudotumor.1, 2, 3, 4
In the present report, we have described the case of acute lower limb arterial ischemia due to arterial injury as a complication of metallosis. The patient's family provided written informed consent for the report of the patient's case.
Case report
A 74-year-old woman was admitted to the emergency department of our hospital because of severe pain in her left thigh. She was stable on admission, with normal blood and chemistry parameters. In 1999, she had undergone total left hip arthroplasty to treat degenerative damage to the hip joint. Later, in 2012, she had undergone left hip osteosynthesis for a femur fracture to realign and secure the fragments in a position that would promote callus formation (Fig 1). She was then lost to follow-up. However, the patient reported that 2 months previously, she had undergone surgery at another hospital (without providing a surgical report). Since then, she had experienced several episodes of severe pain. The radiograph at admission showed the absence of a hip joint and increased amorphous densities in the periprosthetic soft tissue (Fig 2). It was observed that the prosthetic material had been removed but without replacement.
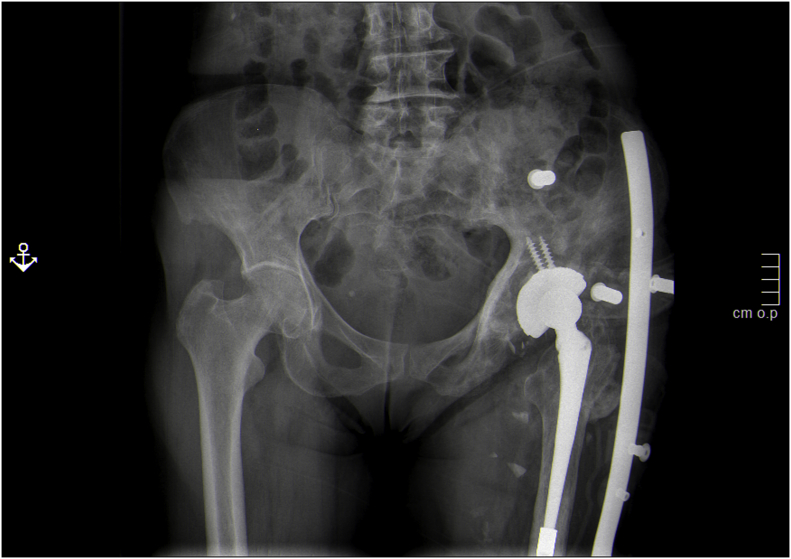
Fig 1.
Abdominal radiograph after surgery in 2012 showing total right hip replacement without signs of osteolysis of the cup but with moderate metaphyseal osteolytic involvement at the femoral level. A pelvic basket can also be seen (antiluxation system).
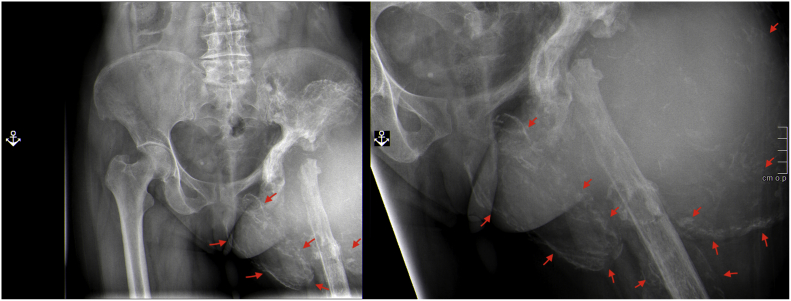
Fig 2.
Abdominal pelvis radiograph at admission in 2020. Red arrows indicate numerous signs of increased amorphous densities in the periprosthetic soft tissues. The prosthetic material was removed but without replacement.
At 24 hours after admission, an increase in size and distension was observed at the left thigh, with the absence of femoral, popliteal, and distal pulses, and functional impotence of the limb was evident. Of the blood and chemistry parameters evaluated, a significant decrease in hemoglobin (from 12.7 g/dL at admission to 6.1 g/dL), the occurrence of renal failure (2.31 mg/dL), and acidosis (pH. 7.31) were observed. A computed tomography (CT) scan showed a large mass with increased density areas inside, at the left side of the pelvis and thigh, with resorption of both the proximal femur and the left acetabular area. This mass encompassed vessels, causing occlusion of the left common femoral artery, with distal recanalization through the collateral vessels and a hematoma with active bleeding (Fig 3). Emergency surgery was decided for hemostatic control and vascular repair because of rupture of the common femoral artery, which was evident on its posterior aspect. The rupture required surgical repair using an iliofemoral bypass (external iliac artery to superficial femoral artery) and reimplantation of the deep femoral artery to the graft (Fig 4, A). Intraoperative open biopsy of a part of the pseudotumor showed a blackish mass with metallic remnants (Fig 4, B). Microbiologic study of the samples resulted in negative findings. In the postoperative period, she was hemodynamically unstable, requiring high doses of inotropic drugs. She developed anuria, liver failure, and, finally, multiorgan failure, and died 48 hours after surgery.
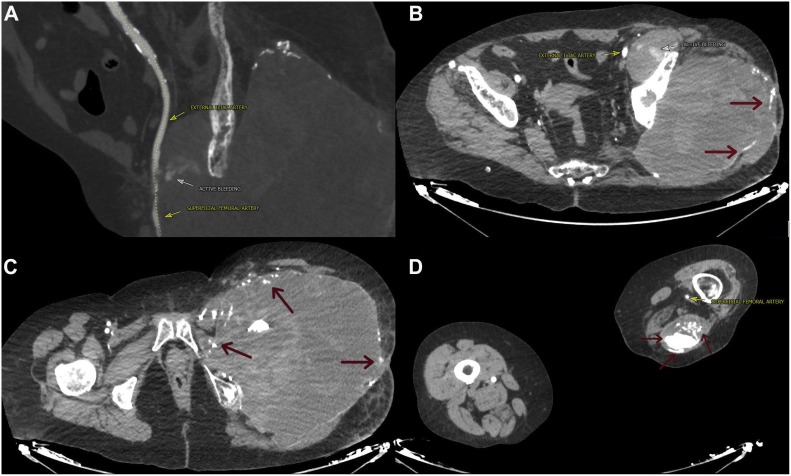
Fig 3.
A, Active bleeding from the femoral artery. Craniocaudal sequences of computed tomography scans of the abdomen, pelvis, and lower limbs: active bleeding from the femoral artery (B), absence of the left femoral artery (C), and patency of the distal superficial femoral artery (D). Red arrows indicate numerous signs of increased amorphous densities inside and at the edges of the pseudotumors.
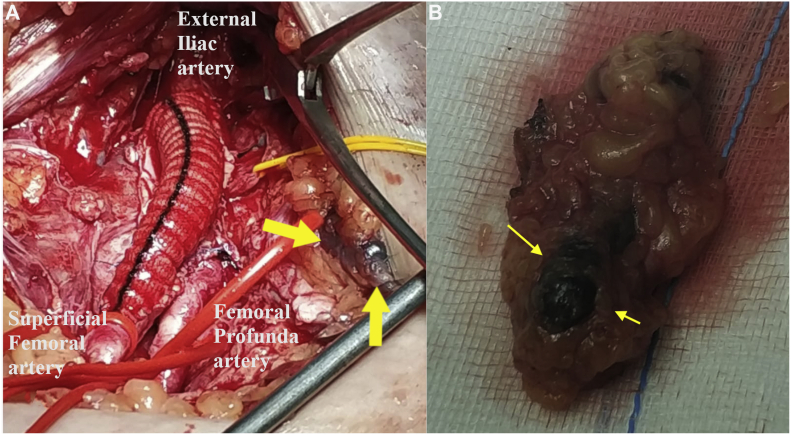
Fig 4.
A, Photograph of the iliofemoral bypass (external iliac artery to superficial femoral artery) and reimplantation of the deep femoral artery to the graft. Yellow arrow indicates some black debris in the background. B, Photograph of fragment of the surgical bed. Yellow arrow indicates a blackish mass.
Discussion
Metallosis refers to the deposition and accumulation of metallic debris in the periprosthetic area that originates by abrasion of metallic components and is a part of what is known at present as an adverse local tissue reaction (ALTR). An ALTR is a chronic inflammatory process caused by metallic debris that appears as a consequence of wear of the joint prosthesis or corrosion of the metallic osteosynthesis material. The accumulation of microscopic metallic debris in the soft tissues incites a foreign body inflammatory reaction with a histiocytic infiltrate and multinucleated giant cells. In an attempt to isolate the immunogen, a fibrotic response occurs, and the histiocytes that surround the particles release inflammatory cytokines, which are responsible for local effects such as synovial hyperplasia, periprosthetic osteolysis, implant loosening, tissue necrosis, lesion-associated aseptic lymphocytic vasculitis, and the presence of a mass or pseudotumor.5 Pseudotumors are defined as noninfectious and non-neoplastic masses that arise from an inflammatory exudate encapsulated by fibrosis.6 The local inflammatory process causes infiltration of the bone and periprosthetic soft tissues (ie, ALTR) but is also responsible for systemic involvement. Systemic involvement is referred to as an adverse reaction to metal debris. Systemic findings can include cognitive, visual, and auditory symptoms, cardiomyopathy, neuropathy, and depression. ALTR will occur in 30% to 60% of symptomatic and asymptomatic patients with metal-to-metal hip implants.7,8 Symptoms can include pain, mass or pseudotumor formation with or without cystic changes, joint effusion, metallic friction noises, and functional limitations. In radiographs, we can observe some signs that can guide the diagnosis of metallosis, because amorphous increases in the density of the periprosthetic soft tissues could reflect the presence of metallic debris deposited in the joint, together with the inflammatory process. Depending on their appearance, they have been described as the “bubble sign” (areas of curvilinear densities that resemble bubbles),9 the “cloud sign” (higher density, amorphous, and uniform areas that resemble clouds),10 and the “metal line sign” (a rim of linear increased radiodensity outlining a portion of the joint capsule).11 These signs will not always be present and could depend on the extent and duration of the metallosis. However, they are useful for the diagnosis when they are evident.
Color Doppler ultrasound has been the initial imaging method of choice in our practice for the assessment of vascular lesions. However, for the present patient, owing to the severity of the clinical presentation and location of the injury, a CT scan was performed. CT evaluation of metallosis provides a better assessment of the densities that delineate the joints and metals and can identify and quantify the areas of osteolysis. In cases of suspected arterial injury, CT allows for an assessment of the severity, location, and status of the inflow and runoff to determine the treatment required. In our patient, the CT findings also revealed a serious situation responsible for the hemodynamic shock: a source of active bleeding. Treatment of metallosis includes surgical intervention to prevent progressive joint destruction. Surgery should consist of debridement, subtotal synovectomy, removal of all visible metallic debris, and removal of the prosthesis.12 Depending on the specific cause, metallosis can develop at any point postoperatively, from a few weeks to many years later. Serologic tests, including ion levels, will not provide useful information. Thus, the diagnosis can only be confirmed intraoperatively by macroscopic evaluation of the site and/or subsequent histologic examination. In agreement with other investigators, in our patient, we observed the accumulation of a blackish material in the surgical bed.13,14
Women have had eight times the rate of surgical revision for pseudotumors compared with men. Because the histologic findings of ATLR samples were similar to the type IV hypersensitivity reaction mediated by T lymphocytes, it has been proposed that the increased sensitivity to metal by women is related to the habitual use of jewelry.15 However, allergic mechanisms alone cannot explain all the responses to metal exposure. The individual susceptibility of the patients would play a fundamental role.5 ATLR poses a risk of irreversible soft tissue damage, which increases over time; thus, early diagnosis is essential.16
Conclusions
Injury to the femoral vascular bundle due to metallosis, either by compression or, as in our patient, by direct injury, is a rare complication after total hip replacement. However, owing to its anatomic proximity, it should be considered.
Footnotes
Author conflict of interest: none.
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal Policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Zink T.M., McGrory B.J. Mechanically assisted crevice corrosion in a metal-on-polyethylene total hip presenting with lower extremity vascular compromise. Arthroplast Today. 2020;6:445–450. doi: 10.1016/j.artd.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Algarni A.D., Huk O.L., Pelmus M. Metallosis-induced iliopsoas bursal cyst causing venous obstruction and lower-limb swelling after metal-on-metal THA. Orthopedics. 2012;35:e1811–e1814. doi: 10.3928/01477447-20121120-30. [DOI] [PubMed] [Google Scholar]
- 3.Grote C.W., Cowan P.C., Anderson D.W., Templeton K.J. Pseudotumor from metal-on-metal total hip arthroplasty causing unilateral leg edema: case presentation and literature review. Biores Open Access. 2018;7:33–38. doi: 10.1089/biores.2017.0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lencioni A., Ellis B., Dean C.S., Lendrum J., Hogan C.A. Metal-on-metal total hip arthroplasty adverse local tissue reaction with intermittent unilateral vascular claudication. Arthroplast Today. 2019;5:389–393. doi: 10.1016/j.artd.2019.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.U.S. Food and Drug Administration Biological responses to metal implants. https://www.fda.gov/media/131150/download September 2019. Available at:
- 6.Pandit H., Glyn-Jones S., McLardy-Smith P., Gundle R., Whitwell D., Gibbons C.L.M. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br. 2008;90:847–851. doi: 10.1302/0301-620X.90B7.20213. [DOI] [PubMed] [Google Scholar]
- 7.Williams D.H., Greidanus N.V., Masri B.A., Duncan C.P., Garbuz D.S. Prevalence of pseudotumor in asymptomatic patients after metal-on-metal hip arthroplasty. J Bone Joint Surg Am. 2011;93:2164–2171. doi: 10.2106/JBJS.J.01884. [DOI] [PubMed] [Google Scholar]
- 8.Sutphen S.A., MacLaughlin L.H., Madsen A.A., Russell J.H., McShane M.A. Prevalence of pseudotumor in patients after metal-on-metal hip arthroplasty evaluated with metal ion analysis and MARS-MRI. J Arthroplasty. 2016;31:260–263. doi: 10.1016/j.arth.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 9.Su E.P., Callander P.W., Salvati E.A. The bubble sign: a new radiographic sign in total hip arthroplasty. J Arthroplasty. 2003;18:110–112. doi: 10.1054/arth.2003.50007. [DOI] [PubMed] [Google Scholar]
- 10.Paydar A., Chew F.S., Manner P.A. Severe periprosthetic metallosis and polyethylene liner failure complicating total hip replacement: the cloud sign. Radiol Case Rep. 2007;2:1–6. doi: 10.2484/rcr.v2i4.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weissman B.N., Scott R.D., Brick G.W., Corson J.M. Radiographic detection of metal-induced synovitis as a complication of arthroplasty of the knee. J Bone Joint Surg Am. 1991;73:1002–1007. [PubMed] [Google Scholar]
- 12.Sanchis-Alfonso V. Severe metallosis after unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2007;15:361–364. doi: 10.1007/s00167-006-0207-6. [DOI] [PubMed] [Google Scholar]
- 13.Cooper H.J., Della Valle C.J., Berger R.A. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am. 2012;94:1655–1661. doi: 10.2106/JBJS.K.01352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hussey D.K., McGrory B.J. Ten-year cross-sectional study of mechanically assisted crevice corrosion in 1352 consecutive patients with metal-on-polyethylene total hip arthroplasty. J Arthroplasty. 2017;32:2546–2551. doi: 10.1016/j.arth.2017.03.020. [DOI] [PubMed] [Google Scholar]
- 15.Glyn-Jones S., Pandit H., Kwon Y.M., Doll H., Gill H.S., Murray D.W. Risk factors for inflammatory pseudotumor formation following hip resurfacing. J Bone Joint Surg Br. 2009;91:1566–1574. doi: 10.1302/0301-620X.91B12.22287. [DOI] [PubMed] [Google Scholar]
- 16.Morlock M.M. The taper disaster—how could it happen? Hip Int. 2015;25:339–346. doi: 10.5301/hipint.5000269. [DOI] [PubMed] [Google Scholar]