Abstract
Emergency department (ED) crowding is recognized as a critical threat to patient safety, while sub‐optimal ED patient flow also contributes to reduced patient satisfaction and efficiency of care. Provider in triage (PIT) programs—which typically involve, at a minimum, a physician or advanced practice provider conducting an initial screening exam and potentially initiating treatment and diagnostic testing at the time of triage—are frequently endorsed as a mechanism to reduce ED length of stay (LOS) and therefore mitigate crowding, improve patient satisfaction, and improve ED operational and financial performance. However, the peer‐reviewed evidence regarding the impact of PIT programs on measures including ED LOS, wait times, and costs (as variously defined) is mixed. Mechanistically, PIT programs exert their effects by initiating diagnostic work‐ups earlier and, sometimes, by equipping triage providers to directly disposition patients. However, depending on local contextual factors—including the co‐existence of other front‐end interventions and delays in ED throughput not addressed by PIT—we demonstrate how these features may or may not ultimately translate into reduced ED LOS in different settings. Consequently, site‐specific analysis of the root causes of excessive ED LOS, along with mechanistic assessment of potential countermeasures, is essential for appropriate deployment and successful design of PIT programs at individual EDs. Additional motivations for implementing PIT programs may include their potential to enhance patient safety, patient satisfaction, and team dynamics. In this conceptual article, we address a gap in the literature by demonstrating the mechanisms underlying PIT program results and providing a framework for ED decision‐makers to assess the local rationale for, operational feasibility of, and financial impact of PIT programs.
Keywords: emergency department boarding, emergency department crowding, emergency department physician in triage, emergency department provider in triage, hospital capacity, patient flow, patient safety, patient satisfaction
1. INTRODUCTION
Organizations, including The Joint Commission and the American College of Emergency Physicians, have long recognized the need to mitigate emergency department (ED) crowding as an urgent patient safety priority. 1 , 2 ED crowding, which occurs when the number of patients receiving care exceeds treatment space capacity, has been associated with delayed antibiotic administration, a higher likelihood of adverse events, prolonged wait times, and increasing rates of patients who leave without being seen (LWBS), among other deleterious effects. 3 , 4 , 5 , 6 , 7 Prolonged patient length of stay (LOS) in the ED both contributes to, and is exacerbated by, ED crowding. 8 , 9 , 10 Many causes of prolonged ED LOS—such as boarding of patients admitted from the ED due to inpatient bed unavailability—require hospital‐wide countermeasures to address. 11 , 12 , 13 However, there also is interest in mitigating ED crowding by accelerating patient flow within the ED itself. Provider in triage (PIT)—which typically involves a physician or advanced practice provider conducting an initial screening examination and potentially initiating diagnostic testing and treatment at triage—has been proposed as one ED‐controllable mechanism to reduce ED LOS.
PIT programs often are endorsed as a mechanism to mitigate ED crowding, 2 , 14 , 15 , 16 , 17 yet the peer‐reviewed evidence regarding their impact on measures, including ED LOS, wait times, and costs (as variously defined), is mixed. Existing systematic reviews have demonstrated significant heterogeneity in study design, PIT program design, and results, which they attribute in part to the critical influence of local contextual factors, without elucidating these factors in depth. 18 , 19 , 20 Although these findings are important for characterizing the literature on PIT programs, they are not generalizable to—and therefore are of limited use for—local decision‐makers contemplating, designing, or assessing performance of PIT programs in individual EDs.
Consequently, we seek in this conceptual article to fill a gap in the literature by providing a structured resource to guide ED decision‐makers in their initial evaluation of PIT programs in the context of their local operations. Specifically, our objectives are to (1) illustrate the primary mechanisms underlying PIT programs, and (2) provide a framework for ED decision‐makers to assess the local rationale for feasibility of and financial impact of PIT programs, accounting for their potential influence on patient flow, patient safety, patient satisfaction, and team dynamics.
2. LITERATURE REVIEW
Working with a medical librarian (A.T.N.), we queried PubMed for peer‐reviewed literature related to PIT programs (Appendix 1). We hand‐searched selected reference lists to identify additional citations. The objective of our evidence synthesis was to identify major ideas and models related to PIT, rather than provide an exhaustive review of the literature. We included articles in our synthesis if they (1) reported outcomes of 1 or more PIT implementations, or (2) offered perspectives related to PIT. A reviewer (B.J.F.) used our data extraction form to evaluate articles against the aforementioned eligibility criteria and categorize their content. Themes were determined by co‐authors’ review and discussion.
Our search yielded 504 unique articles, of which 64 met our criteria for review. Eight articles were systematic reviews, including 3 meta‐analyses. The remaining 56 articles primarily described individual PIT implementations or offered perspectives regarding PIT. The literature demonstrates significant heterogeneity in both the design (Figure 1) and outcomes of PIT programs. Key differences among existing PIT programs include provider and clinical support staffing models, scope of work, patients and acuity levels seen, and type of space repurposed, remodeled, or added. Table 1 summarizes evidence from the three systematic reviews with meta‐analysis.
FIGURE 1.
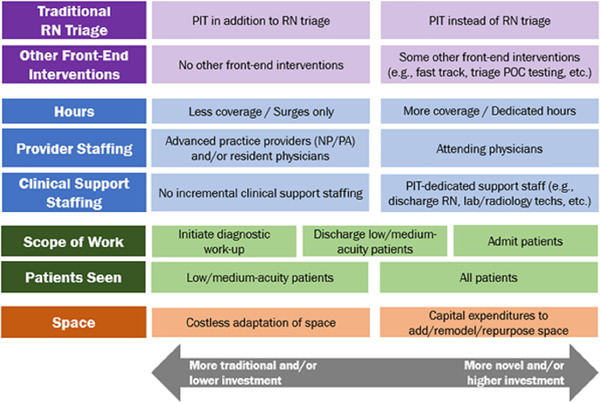
Provider in triage program design variables. NP, nurse practitioner; PA, physician assistant; POC, point of care; RN, registered nurse
TABLE 1.
Summary of results of systematic reviews with meta‐analysis of provider in triage programs
| Reference | No. of studies reviewed, by country of origin | Wait time (arrival to provider evaluation) | LWBS/LWTC | ED LOS | Adverse events | Patient satisfaction | Return on investment |
|---|---|---|---|---|---|---|---|
| Benabbas et al18 | United States (12) | NR |
In 10 studies, RR of LWBS ranged from 0.15 to 0.95 (results too heterogenous to pool data) In 2 studies, RR of LWTC was 0.60 (95% CI, 0.57–0.64) |
In 9 studies, mean difference of ED LOS pre‐ and post‐PIT ranged from −82 to +20 min (results too heterogenous to pool data). Stratification of studies by disposition (admit vs discharge) did not decrease heterogeneity. | NR | NR | NR |
| Ming et al19 | Canada (2), United States (1), United Kingdom (1) | 1 study reported a reduction in wait time of 26 min (P < 0.001) 21 | NR | 2 of 4 studies reported a statistically significant reduction in LOS ranging from 24 to 36 min 21 , 22 | NR | NR | NR |
| Abdulwahid et al20 | United States (12), Australia (5), Canada (2), United Kingdom (2), Hong Kong (1), Jamaica (1), Singapore (1), Sweden (1) |
2 of 2 RCTs demonstrated a significant reduction in WT (WMD −26.17 minutes, 95% CI, −31.68 to −20.65) 9 of 11 non‐RCTs demonstrated a significant reduction in WT with median difference of −15 min (IQR = −7.5 to −18) |
2 of 2 RCTs demonstrated a significant reduction in LWBS (RR = 0.79, 95% CI, 0.66–0.94) 8 of 12 non‐RCTs demonstrated statistically significant reduction in LWBS 1 of 1 RCTs did not demonstrate a significant reduction in LWTC 3 of 3 non‐RCTs demonstrated a significant reduction in LWTC rates |
2 of 4 RCTs reported a significant reduction in LOS 21 , 22 |
1 observational study demonstrated a statistically significant reduction in mortality (P < 0.001) 23 1 study demonstrated a significant improvement in unplanned reattendance 23 |
1 of 3 RCTs demonstrated a significant improvement in Press Ganey overall rating of ED care from 4.22 to 4.38 (P = 0.013) 24 | 1 study reported a positive return on investment (as quantified by net present value of $2.82 M and breakeven time of 13 months) 25 |
Abbreviations: CI, confidence interval; ED, emergency department; LOS, length of stay; LWBS, left without being seen; LWTC, left without treatment complete (seen by a provider but left the ED before completion of treatment); NR, not reported; PIT, provider in triage; RCT, randomized controlled trial; RR, risk ratio; WMD, weighted mean difference; WT, wait time (arrival to provider evaluation).
3. RATIONALE TO IMPLEMENT PIT
PIT is deployed to mitigate ED crowding by targeting ED throughput and output. 26 Two major goals for implementing PIT are reducing LWBS and reducing ED LOS (Figure 2).
FIGURE 2.
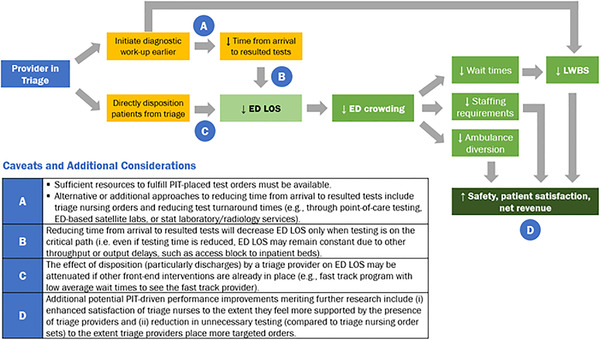
Mechanisms by which PIT programs may improve ED performance. ED, emergency department; LOS, length of stay; LWBS, left without being seen
Additional rationales for implementing PIT may include enhancing patient satisfaction, patient safety, and team dynamics, as further discussed below. Finally, the COVID‐19 pandemic may renew interest in interventions, including PIT, designed to increase ED capacity. Solutions targeting ED crowding are particularly relevant because facilitating physical distancing in waiting and treatment areas, which is difficult to achieve in EDs operating at extremely high occupancy, may influence patient perceptions of safety and willingness to seek in‐person care. 27 , 28
Next, we discuss the mechanisms by which PIT theoretically promotes reduced LWBS and ED LOS, factors counteracting PIT efficacy, alternatives or complements to PIT (Table 2), and a framework for assessing cost‐effectiveness.
TABLE 2.
Examples of other countermeasures targeting LWBS and/or ED LOS
| Countermeasure | Directly targets | |
|---|---|---|
| LWBS | ED LOS | |
| Immediate bedding | ✓ | ✓ |
| Fast track/split‐flow | ✓ | ✓ |
| Triage nursing orders | ✓ | |
| Rapid medical evaluation a | ✓ | ✓ |
Improving test turnaround times
|
✓ | |
| Bedside registration | ✓ | |
4. REDUCING LEFT WITHOUT BEING SEEN RATES
4.1. Motivations
The desire to reduce LWBS is motivated by concerns related to patient safety, patient satisfaction, and foregone revenue. Prolonged wait times drive ED patient elopement and the risk of certain unseen patients experiencing adverse outcomes after leaving. 31 , 32 Financially, increased LWBS results in foregone revenue and exposes health systems to medicolegal risk, though PIT introduces its own medicolegal considerations related to screening exam adequacy. 33 , 34
4.2. Mechanisms and evidence
Unless an ED has an immediate bedding policy and treatment spaces are routinely available, placing a provider at triage is likely to reduce the time from arrival to provider evaluation. In turn, as wait times drive elopement, reducing time from arrival to provider evaluation drives reduced LWBS (Figure 2). As shown in Table 1, a majority of studies reviewed by Abdulwahid et al 20 and Ming et al 19 demonstrate significant reductions in time from arrival to provider evaluation following PIT implementation. Additionally, a majority of these studies demonstrate significant reductions in LWBS.
5. REDUCING ED LENGTH OF STAY
Although PIT is likely to reduce time from arrival to provider (and therefore LWBS), the mechanisms and evidence base supporting PIT as a technique to reduce ED LOS are significantly more context‐dependent. PIT is thought to promote reduced ED LOS by (1) decreasing time from patient arrival to resulted tests by ordering tests earlier, and/or (2) decreasing time from patient arrival to disposition by permitting triage providers to directly treat and disposition certain patients (eg, discharge low‐acuity patients and/or admit medium‐acuity patients) (Figure 2). In Benabbas et al's systematic review, 11 of the 11 studies reviewed reported triage providers initiated diagnostic testing and treatment, 5 of 11 studies reported triage providers discharged patients, and 4 of 11 studies reported triage providers both admitted and discharged patients. 18
5.1. Arrival to resulted tests
Intuitively, PIT facilitates earlier test ordering, which—assuming sufficient resources exist to fulfill these orders—generally leads to earlier test results. However, whether accelerating test results ultimately reduces ED LOS—and whether PIT is the most optimal means of doing so—depends on local contextual factors. For example, after implementing PIT, Han et al 35 reported a modest decrease in ED LOS for discharged patients, but no decrease in ED LOS for admitted patients. Concurrently, boarding times—the time elapsed between inpatient bed request and patient exit from the ED—for admitted patients increased by 9 minutes during the intervention period.
This finding demonstrates how, for EDs in hospitals facing inpatient bed capacity constraints, accelerating a patient's workup and disposition may not ultimately reduce their ED LOS. Figure 3 illustrates a hypothetical scenario in which the next inpatient bed becomes available at 4:00 PM regardless of when admission orders are placed (ignoring the nuance that requesting a bed earlier may provide more time for the hospital to address capacity—for example, by summoning additional resources, accelerating discharges, or activating a surge plan). In this scenario, accelerating the patient's workup and admission merely results in boarding beginning earlier, with no effect on ED LOS.
FIGURE 3.
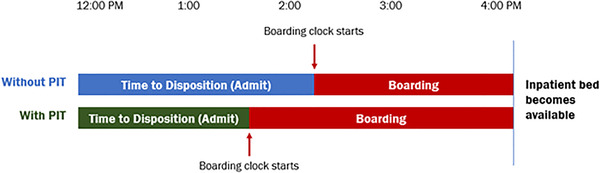
Reducing time to disposition does not decrease ED LOS in the event of inpatient bed capacity constraint
Stated more generally, accelerating time to resulted tests will not decrease ED LOS if testing is not on the critical path. In project management, the critical path is defined as the longest path from project start (patient arrival) to finish (patient exit from the ED); the sum of activities on the critical path is the minimum time necessary to complete the entire project. 36 As Figure 4 illustrates, in this simplified hypothetical scenario, the critical path (depicted in red) is 135 minutes and involves waiting for specialty consultation. Even if time from arrival to resulted tests (currently 75 minutes) is shortened, because the consultant will not be available to evaluate test results any earlier (ie, because testing is not on the critical path), the patient's ED LOS will remain unchanged.
FIGURE 4.
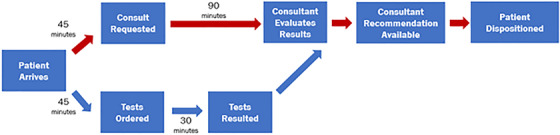
Reducing time to resulted tests does not decrease ED LOS if testing time is not on the critical path (depicted in red)
5.2. Alternative approaches to achieving earlier resulting of tests
5.2.1. Triage nursing orders
PIT facilitates earlier ordering of tests. An alternative approach to accelerating test ordering is equipping registered nurses (RNs) at triage with standard order sets for laboratory or imaging studies based on chief complaint, ideally informed by evidence‐based testing protocols. A variety of studies have documented reduced ED LOS, treatment time, or time to disposition after implementing triage nursing orders (TNOs). 37 , 38 , 39 , 40 , 41 , 42 When comparing PIT against TNOs, ED decision‐makers should consider whether a high proportion of patients could have an appropriate work‐up initiated by a triage RN, which may obviate the role of PIT in accelerating test ordering.
Balance measures to consider when ordering tests at triage based on minimal history and exam—whether through TNOs or PIT—include the percentage of tests ordered at triage that prove to be clinically irrelevant, along with the percentage of patients who have a separate diagnostic work‐up initiated by the treating clinician because the initial work‐up was insufficient or inappropriate (thus paradoxically negating the benefit of earlier resulting of those tests, and ultimately leading to over‐testing). 43 , 44 An alternative hypothesis is that PIT could actually reduce unnecessary testing compared to TNOs to the extent triage providers place more targeted orders. 45
5.2.2. Improving test turnaround times
Another approach to decreasing ED LOS involves reducing test order‐to‐result turnaround times, which can account for a significant proportion of LOS. 46 Strategies to reduce ED testing turnaround times including point‐of‐care testing (at triage or bedside), ED‐based satellite laboratories, and “stat,” ED‐dedicated laboratory and radiology services. 37 , 38 , 47 , 48 , 49 Costs and benefits of these alternative strategies should be compared against those of PIT.
5.3. Discharge from triage
Multiple studies have described PIT programs in which triage clinicians directly disposition patients. 18 However, as with reducing time to resulted tests, evidence regarding direct disposition of patients on ED LOS is mixed. For example, in contrast to Han et al, 35 who reported PIT decreased ED LOS only for discharged patients, Imperato et al 50 reported much more pronounced reductions in ED LOS for admitted patients, with minimal impact on LOS for discharged patients. Although in Imperato et al the triage physician was permitted to directly discharge patients, this study also involved concurrent use of a fast track area staffed by a physician assistant (ie, a split‐flow model 2 ), which may have siphoned off many low‐acuity, easily discharged patients. Nestler et al 51 , 52 found PIT in combination with a fast track area was associated with reduced ED LOS, whereas these benefits were lost when PIT alone was trialed. An area for future research relates to potential benefits and costs of assigning non‐provider support for PIT programs. 53 For example, could a dedicated triage treatment/discharge nurse, charged with frequently reassessing patient progress and test results, allow the triage provider to focus on decision‐making, reduce non‐value‐added time, and facilitate faster patient disposition?
Neither Imperato et al nor Nestler et al comment on average wait time for the fast track area. Generally, however, if a fast track area exists, the effect of PIT on fast track patients conceptually depends on the average wait time to see the fast track provider. If there are typically lengthy wait times to see a fast track provider, then PIT may decrease ED LOS by either (1) initiating diagnostic workups earlier (as previously discussed), or (2) directly dispositioning patients (essentially serving as another fast track provider). If, alternatively, there is minimal wait time to see a fast track provider, then having a triage provider order diagnostic testing may have little effect on ED LOS for fast track patients. The expected site‐specific effects of PIT must be considered in the context of other front‐end interventions, including fast track.
6. TELE‐INTAKE
Some EDs have deployed telemedicine to place virtual providers at triage, who may perform tasks equivalent to those of their in‐person PIT counterparts (initial screening exam and order placement), though with potential differences in billability for these services. 54 , 55 , 56 , 57 Other than differences in team dynamics resulting from virtual (vs physical) collaboration and unfamiliar co‐workers (in the case of contracted providers), these tele‐intake programs may influence patient flow and safety by the same mechanisms as in‐person PIT programs. The COVID‐19 pandemic has renewed interest in tele‐intake given its potential to reduce contacts among patients and caregivers. 58 , 59
7. ASSESSING FINANCIAL IMPACT
PIT programs may involve annualized expenditures of hundreds of thousands of dollars, depending on incremental staffing requirements. To ensure organizational viability and value for patients, assessing quantitative and qualitative return on investment (ROI) of PIT programs is critical.
Assessing quantitative ROI involves evaluating annual cash flows from PIT, including those noted in Table 3. 25 Contribution margin is calculated as collected revenues from patient care less direct costs of providing that care. In a fee‐for‐service environment, collected revenues are a function of the number of incremental patients, charges per patient (based on payer mix and intensity of care), collection rate, and participation in value‐based payment programs. Specific methods for approaching these calculations are beyond the scope of this paper. Generally, however, return on investment may be quantified using methods including payback period, net present value, and internal rate of return. Soremekun et al 25 illustrate these assessments (although depreciation expense should be excluded from net present value calculations). Kezirian et al 60 and Cheng et al 61 describe additional approaches to quantify ROI.
TABLE 3.
PIT program cash flows
| Positive cash flows | Negative cash flows |
|---|---|
|
|
Abbreviations: LWBS, left without being seen; PIT, provider in triage.
Contribution margin is calculated as collected revenues from patient care less direct costs of providing that care. Collected revenues are a function of factors including the number of incremental patients, charges per patient (which depends on payer mix and intensity of care), collection rate, and participation in value‐based payment programs.
If no net additional hours are paid (ie, if existing staff are redeployed to the PIT program), then this figure should be calculated as the opportunity cost associated with the full‐time equivalent personnel allocated to the PIT program.
For EDs considering PIT in a fee‐for‐service environment, the most complex—and essential—component of assessing quantitative ROI is estimating the number of patients likely to be recaptured from LWBS and ambulance diversions, along with any incremental patients seen due to increased ED capacity. These estimates require considerable local analysis because they rely on understanding the site‐specific mechanistic drivers of how PIT would—or would fail to—lead to the desired outcomes illustrated in Figure 2. Overall, regardless of payment model, when contemplating PIT programs, it is critical for ED decision‐makers to:
articulate the problem(s) they are attempting to solve (eg, excessive LWBS or ED LOS),
undertake rigorous analysis (eg, using A3 problem solving 62 ) to identify the local root causes of these problems, and
assess mechanistically and quantitatively the extent to which PIT would address these root causes.
8. LIMITATIONS OF LITERATURE AND OTHER IMPORTANT CONSIDERATIONS
Further important considerations regarding PIT feasibility, which may not be easily quantified, include potential influence of PIT programs on the following:
Patient safety and outcomes: PIT may facilitate earlier recognition and treatment of time‐sensitive conditions (eg, myocardial infarction, stroke, sepsis, etc.) and pain, as well as guard against patient deterioration in the waiting room. 23
Patient satisfaction: by reducing time from arrival to evaluation (and potentially reducing ED LOS), PIT may enhance the patient experience. 24 , 63
Clinician satisfaction and teamwork: triage nurses may feel more supported by the presence of triage providers when managing busy waiting rooms.
Graduate medical education: while serving as a triage provider might confer new learning opportunities to residents, in cases where residents do not work in triage, PIT programs might reduce opportunities for residents to formulate their own assessments and plans. 64 , 65
Medicolegal considerations: PIT may introduce medicolegal considerations related to screening exam adequacy. 34 Further literature elucidating these considerations would help inform PIT program design and potentially enhance providers’ buy‐in.
Although challenging to measure and apparently addressed by only a narrow body of literature, these factors must be considered in combination with the quantitative ROI to determine whether PIT is worthwhile at any single site.
9. CONCLUSION
PIT programs are frequently endorsed as a mechanism to reduce ED LOS and therefore mitigate ED crowding, yet evidence regarding their effectiveness is mixed. Existing systematic attribute the significant heterogeneity in PIT program results to local contextual factors, without elucidating these factors in depth. Mechanistically, PIT programs exert their effects by reducing time from arrival to resulted tests and by equipping triage providers to directly disposition patients. However, depending on local contextual factors—including the coexistence of other front‐end interventions and delays in ED throughput not addressed by PIT—we illustrate how these features may or may not ultimately translate into reduced ED LOS. Consequently, site‐specific analysis of the root causes of excessive ED LOS and mechanistic assessment of potential countermeasures is essential for appropriate deployment and successful design of PIT programs. Additional motivations for implementing PIT programs may include their potential to facilitate enhanced patient safety, patient satisfaction, and team dynamics. In this conceptual article, we address a gap in the literature by demonstrating the mechanisms underlying PIT program results and providing a framework for ED decision‐makers to assess the site‐specific rationale for, operational feasibility of, and cost‐effectiveness of PIT programs.
AUTHOR CONTRIBUTIONS
BJF, DMS, KYL, and NLH conceptualized the project. ATN and BJF developed the literature search strategy. BJF screened articles for inclusion. BJF assumes responsibility for the article as a whole. All authors provided analysis and interpretation of the data, developed thematic concepts, and provided critical feedback related to the research and manuscript.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
APPENDIX 1. PUBMED SEARCH STRATEGY
1.1.
(“Emergency service, hospital”[mesh] OR trauma centers[mesh] OR emergency medicine[mesh] OR “emergency”[tiab])
AND
(((Triage[mesh] OR triage[ti]) AND (provider*[tiab] OR physician*[tiab] OR team*[tiab] OR doctor*[tiab] OR practitioner*[tiab])) OR “Provider in triage”[tiab] OR “Physician in triage”[tiab] OR “Physician at triage”[tiab] OR “triage liaison provider”[tiab] OR “Triage liaison physician”[tiab] OR “Team triage”[tiab])
AND
(Length of stay[mesh] OR “length of stay”[tiab] OR Time‐to‐treatment[mesh] OR “time to treatment”[tiab] OR “leave without being seen”[tiab] OR “left without being seen”[tiab] OR “left before being seen”[tiab] OR “leave before being seen”[tiab] OR LWBS[tiab] OR Crowding[mesh] OR crowding[tiab] OR patient satisfaction[mesh])
Franklin BJ, Li KY, Somand DM, et al. Emergency department provider in triage: assessing site‐specific rationale, operational feasibility, and financial impact. JACEP Open. 2021;2:e12450. 10.1002/emp2.12450
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Christian Tomaszewski, MD, MS.
REFERENCES
- 1. The Joint Commission . Approved: standards revisions addressing patient flow through the emergency department.Jt Comm Perspect. 2012;32(7):1‐5. https://www.jointcommission.org/-/media/tjc/documents/standards/jc-requirements/stds_rev_patient_flowpdf.pdf?db=web&hash=32FD460560C35C7FBC8D69C9F783232B. [PubMed] [Google Scholar]
- 2. Emergency Department Crowding: High‐Impact Solutions. American College of Emergency Physicians; 2016. https://www.acep.org/globalassets/sites/acep/media/crowding/empc_crowding‐ip_092016.pdf Accessed July 11, 2020.
- 3. Peltan ID, Bledsoe JR, Oniki TA, et al. Emergency department crowding is associated with delayed antibiotics for sepsis. Ann Emerg Med. 2019;73(4):345‐355. [DOI] [PubMed] [Google Scholar]
- 4. Pines JM, Localio AR, Hollander JE, et al. The impact of emergency department crowding measures on time to antibiotics for patients with community‐acquired pneumonia. Ann Emerg Med. 2007;50(5):510‐516. [DOI] [PubMed] [Google Scholar]
- 5. Mccarthy ML, Zeger SL, Ding R, et al. Crowding delays treatment and lengthens emergency department length of stay, even among high‐acuity patients. Ann Emerg Med. 2009;54(4):492‐503. [DOI] [PubMed] [Google Scholar]
- 6. Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust. 2006;184 (5):213–216. 10.5694/j.1326-5377.2006.tb00204.x. [DOI] [PubMed] [Google Scholar]
- 7. Carter EJ, Pouch SM, Larson EL. The Relationship Between Emergency Department Crowding and Patient Outcomes: A Systematic Review. J Nurs Scholarsh. 2014;46(2):106–115. 10.1111/jnu.12055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Morley C, Unwin M, Peterson GM, Stankovich J, Kinsman L. Emergency department crowding: A systematic review of causes, consequences and solutions. PLOS ONE. 2018;13(8):e0203316. 10.1371/journal.pone.0203316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pines JM, Prabhu A, Hilton JA, et al. The effect of emergency department crowding on length of stay and medication treatment times in discharged patients with acute asthma. Acad Emerg Med. 2010;17(8):834‐839. [DOI] [PubMed] [Google Scholar]
- 10. Mccarthy ML, Zeger SL, Ding R, et al. Crowding delays treatment and lengthens emergency department length of stay, even among high‐acuity patients. Ann Emerg Med. 2009;54(4). [DOI] [PubMed] [Google Scholar]
- 11. Rutherford PA, Provost LP, Kotagal UR, et al. Achieving Hospital‐wide Patient Flow. IHI White Paper. Cambridge, Massachusetts: Institute for Healthcare Improvement; 2017. http://www.ihi.org/resources/Pages/IHIWhitePapers/Achieving-Hospital-wide-Patient-Flow.aspx. Accessed August 1, 2020. Available at www.ihi.org.
- 12. Driesen BEJM, van Riet BHG, Verkerk L, Bonjer HJ, Merten H, Nanayakkara PWB. Long length of stay at the emergency department is mostly caused by organisational factors outside the influence of the emergency department: A root cause analysis. PLoS One. 2018;13(9):e0202751. 10.1371/journal.pone.0202751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mohr NM, Wessman BT, Bassin B, et al. Boarding of Critically Ill Patients in the Emergency Department. Crit Care Med. 2020;48(8):1180–1187. 10.1097/ccm.0000000000004385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Approaching Full Capacity in the Emergency Department: An Information Paper. American College of Emergency Physicians. https://www.acep.org/globalassets/uploads/uploaded‐files/acep/clinical‐and‐practice‐management/resources/crowding/approach_full_capacity.pdf Published 2006. Accessed July 13, 2020.
- 15. Emergency Department Operations Management and Patient Flow. Envision Healthcare. https://www.envisionphysicianservices.com/campaigns/breakthrough‐series/presentation‐materials/playbooks/ed‐operations‐management‐and‐patient‐flow‐playbook.pdf Published 2017. Accessed July 13, 2020.
- 16. Flow Improvement Strategies: Provider‐In‐Triage (PIT). Common Sense ‐ American Academy of Emergency Medicine. https://www.aaem.org/UserFiles/file/OMCArticleJanFeb19.pdf Published 2019. Accessed July 13, 2020.
- 17. PhysicianFirst Emergency Department Management Model: Decreases Walk‐outs and Improves Patient Satisfaction. https://www.usacs.com/physicianfirst‐program Accessed July 13, 2020.
- 18. Benabbas R, Shah R, Zonnoor B, Mehta N, Sinert R. Impact of triage liaison provider on emergency department throughput: A systematic review and meta‐analysis. Am J Emerg Med. 2020;38(8):1662–1670. 10.1016/j.ajem.2020.04.068. [DOI] [PubMed] [Google Scholar]
- 19. Ming T, Lai A, Lau P‐M. Can Team Triage Improve Patient Flow in the Emergency Department? A Systematic Review and Meta‐Analysis. Adv Emerg Nurs J. 2016;38(3):233–250. 10.1097/tme.0000000000000113. [DOI] [PubMed] [Google Scholar]
- 20. Abdulwahid MA, Booth A, Kuczawski M, Mason SM. The impact of senior doctor assessment at triage on emergency department performance measures: systematic review and meta‐analysis of comparative studies. Emerg Med J. 2016;33(7):504–513. 10.1136/emermed-2014-204388. [DOI] [PubMed] [Google Scholar]
- 21. Cheng I, Lee J, Mittmann N, et al. Implementing wait‐time reductions under Ontario government benchmarks (Pay‐for‐Results): a Cluster Randomized Trial of the Effect of a Physician‐Nurse Supplementary Triage Assistance team (MDRNSTAT) on emergency department patient wait times. BMC Emerg Med. 2013;13(1): 10.1186/1471-227x-13-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Holroyd BR, Bullard MJ, Latoszek K, et al. Impact of a triage liaison physician on emergency department overcrowding and throughput: a randomized controlled trial. Acad Emerg Med. 2007;14(8):702‐708. 10.1197/j.aem.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 23. Burström L, Nordberg M, Örnung G, et al. Physician‐led team triage based on lean principles may be superior for efficiency and quality? A comparison of three emergency departments with different triage models. Scand J Trauma, Resusc Emerg Med. 2012;20(1):57. 10.1186/1757-7241-20-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Imperato J, Morris DS, Sanchez LD, et al. Improving patient satisfaction by adding a physician in triage.J Hosp Adm. 2014;3(1):7‐13. [Google Scholar]
- 25. Soremekun OA, Biddinger PD, White BA, et al. Operational and financial impact of physician screening in the ED. Am J Emerg Med. 2012;30(4):532‐539. [DOI] [PubMed] [Google Scholar]
- 26. Asplin BR, Magid DJ, Rhodes KV, Solberg LI, Lurie N, Camargo CA. A conceptual model of emergency department crowding. Ann Emerg Med. 2003;42 (2):173–180. 10.1067/mem.2003.302. [DOI] [PubMed] [Google Scholar]
- 27. Wong LE, Hawkins JE, Murrell KL, et al. Where are all the patients? Addressing Covid‐19 fear to encourage sick patients to seek emergency care. NEJM Catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0193. [Internet] 2020; [Google Scholar]
- 28. Patel S, Lorenzi N, Smith T, et al. Critical insights from patients during the covid‐19 pandemic. NEJM Catalyst. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0299. Accessed August 1, 2020. [Google Scholar]
- 29. Jesionowski M. Emergency department left without being seen rates and staff perceptions post‐implementation of a rapid medical evaluation and a provider in triage. J Emerg Nurs. 2019;45(1):38‐45. [DOI] [PubMed] [Google Scholar]
- 30. Koenig R, Mehta S, How to Use Teamwork to Transform Your ED (Part 2). Vituity. https://www.vituity.com/blog/how-to-use-teamwork-to-transform-your-ed-part-2/ Published August 17, 2018. Accessed March 20, 2021.
- 31. Rowe BH, Channan P, Bullard M, et al. Characteristics of patients who leave emergency departments without being seen. Acad Emerg Med. 2006;13(8):848‐852. [DOI] [PubMed] [Google Scholar]
- 32. Baker DW. Patients Who Leave a Public Hospital Emergency Department Without Being Seen by a Physician. JAMA. 1991;266 (8):1085. 10.1001/jama.1991.03470080055029. [DOI] [PubMed] [Google Scholar]
- 33. Clarey AJ, Cooke MW. Patients who leave emergency departments without being seen: literature review and English data analysis. Emerg Med J. 2011;29(8):617‐621. [DOI] [PubMed] [Google Scholar]
- 34. Reyes C, At your defense: physician‐at‐triage no protection against… : Emergency Medicine News. LWW. https://journals.lww.com/em‐news/fulltext/2012/07000/at_your_defense__physician_at_triage_no_protection.10.aspx. Published July 2012. Accessed August 4, 2020.
- 35. Han JH, France DJ, Levin SR, Jones ID, Storrow AB, Aronsky D. The Effect of Physician Triage on Emergency Department Length of Stay. J Emerg Med. 2010;39(2):227–233. 10.1016/j.jemermed.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 36. Girija VR, Bhat MS. Process Flow Analysis in the Emergency Department of a Tertiary Care Hospital using Program Evaluation and Review Technique (PERT). J Health Manag. 2013;15(3):353–359. 10.1177/0972063413492042. [DOI] [Google Scholar]
- 37. Zaboli A, Pfeifer N, Solazzo P, et al. Blood sampling during nurse triage reduces patient length of stay in the emergency department: a propensity score‐weighted, population‐based study. Int Emerg Nurs. 2020;49:100826. [DOI] [PubMed] [Google Scholar]
- 38. Singer AJ, Taylor M, LeBlanc D, et al. Early Point‐of‐Care Testing at Triage Reduces Care Time in Stable Adult Emergency Department Patients. J Emerg Med. 2018;55(2):172–178. 10.1016/j.jemermed.2018.04.061. [DOI] [PubMed] [Google Scholar]
- 39. Lee WW, Filiatrault L, Abu‐Laban RB, Rashidi A, Yau L, Liu N. Effect of Triage Nurse Initiated Radiography Using the Ottawa Ankle Rules on Emergency Department Length of Stay at a Tertiary Centre. CJEM. 2016;18(2):90–97. 10.1017/cem.2015.67. [DOI] [PubMed] [Google Scholar]
- 40. Tambimuttu J, Hawley R, Marshall A. Nurse‐initiated x‐ray of isolated limb fractures in the emergency department: Research outcomes and future directions. Aust Crit Care. 2002;15(3):119–122. 10.1016/s1036-7314(02)80052-2. [DOI] [PubMed] [Google Scholar]
- 41. Douma MJ, Drake CA, O'Dochartaigh D, Smith KE. A Pragmatic Randomized Evaluation of a Nurse‐Initiated Protocol to Improve Timeliness of Care in an Urban Emergency Department. Ann Emerg Med. 2016;68(5):546–552. 10.1016/j.annemergmed.2016.06.019. [DOI] [PubMed] [Google Scholar]
- 42. Rowe BH, Villa‐Roel C, Guo X, et al. The role of triage nurse ordering on mitigating overcrowding in Emergency Departments: a systematic review. Acad Emerg Med. 2011;18(12):1349‐1357. [DOI] [PubMed] [Google Scholar]
- 43. Corl K, New emergency department triage system compromises care. STAT. https://www.statnews.com/2019/09/05/triage-system-boost-profits-compromises-care/. Published September 6, 2019. Accessed August 4, 2020.
- 44. Corl K, New emergency department triage system compromises care. STAT. https://www.statnews.com/2019/09/05/triage-system-boost-profits-compromises-care/. Published September 6, 2019. Accessed July 29, 2020.
- 45. ED revamp: Team approach to care reduces errors, boosts patient and clinician satisfaction. ED Management. https://www.reliasmedia.com/articles/130956-ed-revamp-team-approach-to-care-reduces-errors-boosts-patient-and-clinician-satisfaction. Published July 1, 2011. Accessed August 15, 2020. [PubMed]
- 46. Wang DC, Parry CR, Feldman M, Tomlinson G, Sarrazin J, Glanc P. Acute Abdomen in the Emergency Department: Is CT a Time‐Limiting Factor?. Am J Roentgenol. 2015;205(6):1222–1229. 10.2214/ajr.14.14057. [DOI] [PubMed] [Google Scholar]
- 47. Jang JY, Shin SD, Lee EJ, Park CB, Song KJ, Singer AJ. Use of a Comprehensive Metabolic Panel Point‐of‐Care Test to Reduce Length of Stay in the Emergency Department: A Randomized Controlled Trial. Ann Emerg Med. 2013;61(2):145–151. 10.1016/j.annemergmed.2012.07.021. [DOI] [PubMed] [Google Scholar]
- 48. Lee‐Lewandrowski E, Nichols J, Van Cott E, et al. Implementation of a Rapid Whole Blood D‐Dimer Test in the Emergency Department of an Urban Academic Medical Center. Am J Clin Pathol. 2009;132(3):326–331. 10.1309/ajcp6us3ilgearee. [DOI] [PubMed] [Google Scholar]
- 49. Singer AJ, Viccellio P, Thode HC, et al. Introduction of a stat laboratory reduces emergency department length of stay. Acad Emerg Med. 2008;15(4):324‐328. [DOI] [PubMed] [Google Scholar]
- 50. Imperato J, Morris DS, Binder D, et al. Physician in triage improves emergency department patient throughput. Internal Emerg Med. 2012;7(5):457–462. 10.1007/s11739-012-0839-0. [DOI] [PubMed] [Google Scholar]
- 51. Nestler DM, Fratzke AR, Church CJ, et al. Effect of a physician assistant as triage liaison provider on patient throughput in an Academic Emergency Department. Acad Emerg Med. 2012;19(11):1235‐1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Nestler DM, Halasy MP, Fratzke AR, et al. Patient throughput benefits of triage liaison providers are lost in a resource‐neutral model: a prospective trial. Acad Emerg Med. 2014;21(7):794‐798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Considine J, Lucas E, Payne R, Kropman M, Stergiou HE, Chiu H. Analysis of three advanced practice roles in emergency nursing. Aust Emerg Nurs J. 2012;15(4):219–228. 10.1016/j.aenj.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 54. Joshi AU, Randolph FT, Chang AM, et al. Impact of Emergency Department Tele‐intake on Left Without Being Seen and Throughput Metrics. Academic Emergency Medicine. 2020;27(2):139–147. 10.1111/acem.13890. [DOI] [PubMed] [Google Scholar]
- 55. Rademacher NJ, Cole G, Psoter KJ, et al. Use of Telemedicine to Screen Patients in the Emergency Department: Matched Cohort Study Evaluating Efficiency and Patient Safety of Telemedicine. JMIR Med Infor. 2019;7(2):e11233 10.2196/11233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Hsu Hanson, Greenwald Peter W., Clark Sunday, Gogia Kriti, Laghezza Matthew R., Hafeez Baria, Sharma Rahul. Telemedicine Evaluations for Low‐Acuity Patients Presenting to the Emergency Department: Implications for Safety and Patient Satisfaction. Telemedicine and e‐Health. 2020;26 (8):1010–1015. 10.1089/tmj.2019.0193. [DOI] [PubMed] [Google Scholar]
- 57. Envision Physician Services Tele‐Triage/Intake Program. Envision Physician Services. https://www.envisionphysicianservices.com/explore-solutions/virtual-health/virtual-health-services/tele-triage-intake-program.pdf
- 58. Hollander JE, Carr BG. Virtually perfect? telemedicine for Covid‐19. N Engl J Med. 2020;382(18):1679‐1681. [DOI] [PubMed] [Google Scholar]
- 59. Joy K, How 'tele‐triage' models work to keep patients and clinicians safe. Technology solutions that drive healthcare. https://healthtechmagazine.net/article/2020/04/how-tele-triage-models-work-keep-patients-and-clinicians-safe-perfcon. Published May 1, 2019. Accessed March 28, 2021.
- 60. Kezirian J, Muhammad WT, Wan JY, Godambe SA, Pershad J. Cost Analysis and Provider Satisfaction With Pediatrician in Triage. Pediatr Emerg Care. 2012;28(10):971–976. 10.1097/pec.0b013e31826c6dc4. [DOI] [PubMed] [Google Scholar]
- 61. Cheng I, Castren M, Kiss A, Zwarenstein M, Brommels M, Mittmann N. Cost‐effectiveness of a physician‐nurse supplementary triage assessment team at an academic tertiary care emergency department. CJEM. 2016;18(3):191–204. 10.1017/cem.2015.88. [DOI] [PubMed] [Google Scholar]
- 62. Cindy J. A3 Problem Solving for Healthcare: A Practical Method for Eliminating Waste. CRC Press, 2007. [Google Scholar]
- 63.(September 1, 2007). 'PIT' more than triples ED's satisfaction rates. Emergency Department Management. Retrieved from. https://www.emsworld.com/news/10408630/pit-more-triples-eds-satisfaction-rates [PubMed]
- 64. Nicks B, Mahler S, Manthey D. Impact of a physician‐in‐triage process on resident education. West J Emerg Med. 2014;15(7):902‐907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Ullo M, Alexander A, Sugalski G. Perceived impact of physician‐in‐triage on resident education. Am J Emerg Med. 2019;37(6):1208–1210. 10.1016/j.ajem.2018.11.036. [DOI] [PubMed] [Google Scholar]


